Psychosocial Characteristics and Vaccine Attitudes in Australia Report
VerifiedAdded on 2022/09/14
|8
|9374
|17
Report
AI Summary
This research report, based on a survey of 4370 Australians, investigates the relationship between vaccine attitudes and various psychosocial and demographic characteristics. The study categorizes participants into five vaccine attitude groups and analyzes how these groups differ in terms of health consumer behavior, trust in the healthcare system, adherence to complementary medicine, conspiracist ideation, political preferences, and demographic factors like gender and religious beliefs. The findings reveal that individuals with negative vaccine attitudes tend to be more informed health consumers, distrustful of the mainstream healthcare system, and more likely to hold conspiratorial beliefs. The research highlights the importance of understanding these psychosocial profiles to tailor communication strategies about vaccination and potentially refine the measurement and classification of vaccine attitudes. The study emphasizes the context-specific nature of vaccine attitudes and the need for granular analysis of hesitancy within the broader spectrum of vaccine acceptance and refusal. This report is a valuable resource for public health professionals and anyone interested in understanding the complexities of vaccine attitudes in Australia.

Psychosocialand demographiccharacteristicsrelating to vaccine
attitudes in Australia
TomasRozbroja,
*, Anthony Lyonsa
, Jayne Luckea,b
aAustralianResearchCentrein Sex,Healthand Society,La TrobeUniversity,Australia
b Schoolof PublicHealth,The Universityof Queensland,Australia
A R T I C L E I N F O
Articlehistory:
Received30 April 2018
Receivedin revised form 13 August 2018
Accepted21 August 2018
Keywords:
Vaccine hesitancy
Vaccine attitude
Vaccine refusal
Vaccine acceptance
Anti-vaccination
Community level
A B S T R A C T
Objective:Distrust in vaccinationis a public health concern.In respondingto vaccinationdistrust, the
psychosocialcontextit occursin needsto be accountedfor. But this psychosocialcontextis insufficiently
understood. We examined how Australians’ attitudes to childhood vaccination relate to broader
psychosocialcharacteristicspertaining to two key areas: health and government.
Design:4370Australianswere surveyedand divided into five vaccineattitudegroups.Logisticunivariable
and multivariableregressionanalyseswere used to comparedifferencesin psychosocialcharacteristics
between these groups.
Results:Multivariate analysisshowed that, comparedto groups with positive vaccineattitudes,groups
with negativeattitudeswere more informed,engagedand independenthealth consumers,with greater
adherenceto complementarymedicine,but lower belief in holistic health.Theyhad higher distrust in the
mainstreamhealthcaresystem,higher conspiracistideation, and were more likely to vote for minor
political parties.They were more likely to be male,religious,havechildren,and self-reportbetterhealth.
Conclusions:This researchrevealedHOW profilesof psychosocialcharacteristicsdifferedbetweeneachof
the five attitudes to childhood vaccines.
Practiceimplications:These findings are useful for tailoring communicationsabout vaccination-related
concerns.Theyalso show that more granularclassificationand measurementof vaccineattitudesmay be
useful.
© 2018 Elsevier B.V. All rights reserved.
1. Introduction
Lack of confidencein vaccinationis a concern in Australia [1]
and around the world [2]. Although vaccinationrates in Australia
are high, they are below national targets [3]. Under-vaccinated
people are unevenly distributed, increasing risk of disease
transmission [4,5]. Vaccine-preventabledisease outbreaks and
deaths continue to occur [6]. Confidencein vaccinesis low; in a
2017 study, only 48% of Australian parents reported having no
concernsabout vaccines,while over a fifth believedthat vaccines
causeautism[7]. Other countriesare facingsimilar problems,with
low confidencein many Europeanand North American countries
[8], and vaccine-preventabledeaths continuing to occur despite
good access to vaccination [9–11]. Increasing confidence in
vaccineswill boost vaccineuptake [12–14],but there is a paucity
of effectivestrategiesto do so [15–18].
To help increase confidence, a better understandingof the
relationshipbetween vaccineattitudesand broaderdemographic
and psychosocialattributes within which they exist is needed
[2,15,18].Understandingthe relationship between vaccine atti-
tudes and psychosocial attributes related to healthcare and
governmentis particularlyimportant,becausevaccineconfidence
is linked to beliefs about health [12,17,19,20]and government
[12,21,22],and healthcareand governmentbodies are central to
promoting,delivering and regulatingvaccination.
Existing researchshows that vaccineattitudes exist as part of
psychosocialand demographicattributes[21,23,24].In Australia,
demographicattributeslike socioeconomicstatus(SES)and access
to services [5,7,8,25,26] are linked to vaccine confidence.
Psychosocialfactors related to health, like trust in healthcare
providers,predict vaccineuptake in Australia [27] and elsewhere
[17,28,29].Accessingalternativemedicalpractitionersand greater
relianceon the internetfor health informationare associatedwith
Abbreviations:CAM, complementaryand alternativemedicine; CI, confidence
interval;CMQ, conspiracistmentalityquestionnaire;HCAMQ, holistic complemen-
tary and alternativehealth questionnaire;HCSDS-R, healthcaresystem distrust
scale- revised;HH, holistic health; PSAS,patientself-advocacyscale;RR, risk ratio;
SES,socioeconomicstatus; WHO, World Health Organisation.
* Correspondingauthorat: AustralianResearchCentrein Sex,Health and Society,
La Trobe University,Building NR6, Bundoora,Victoria, 3086, Australia.
E-mail address:t.rozbroj@latrobe.edu.au(T. Rozbroj).
https://doi.org/10.1016/j.pec.2018.08.027
0738-3991/©2018 Elsevier B.V. All rights reserved.
Patient Educationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
Contents lists available at ScienceDirect
Patient Educationand Counseling
j o u r n a lhomep age: w w w . e l s ev i er . c o m / l o c a t e/ p a t e d u c o u
attitudes in Australia
TomasRozbroja,
*, Anthony Lyonsa
, Jayne Luckea,b
aAustralianResearchCentrein Sex,Healthand Society,La TrobeUniversity,Australia
b Schoolof PublicHealth,The Universityof Queensland,Australia
A R T I C L E I N F O
Articlehistory:
Received30 April 2018
Receivedin revised form 13 August 2018
Accepted21 August 2018
Keywords:
Vaccine hesitancy
Vaccine attitude
Vaccine refusal
Vaccine acceptance
Anti-vaccination
Community level
A B S T R A C T
Objective:Distrust in vaccinationis a public health concern.In respondingto vaccinationdistrust, the
psychosocialcontextit occursin needsto be accountedfor. But this psychosocialcontextis insufficiently
understood. We examined how Australians’ attitudes to childhood vaccination relate to broader
psychosocialcharacteristicspertaining to two key areas: health and government.
Design:4370Australianswere surveyedand divided into five vaccineattitudegroups.Logisticunivariable
and multivariableregressionanalyseswere used to comparedifferencesin psychosocialcharacteristics
between these groups.
Results:Multivariate analysisshowed that, comparedto groups with positive vaccineattitudes,groups
with negativeattitudeswere more informed,engagedand independenthealth consumers,with greater
adherenceto complementarymedicine,but lower belief in holistic health.Theyhad higher distrust in the
mainstreamhealthcaresystem,higher conspiracistideation, and were more likely to vote for minor
political parties.They were more likely to be male,religious,havechildren,and self-reportbetterhealth.
Conclusions:This researchrevealedHOW profilesof psychosocialcharacteristicsdifferedbetweeneachof
the five attitudes to childhood vaccines.
Practiceimplications:These findings are useful for tailoring communicationsabout vaccination-related
concerns.Theyalso show that more granularclassificationand measurementof vaccineattitudesmay be
useful.
© 2018 Elsevier B.V. All rights reserved.
1. Introduction
Lack of confidencein vaccinationis a concern in Australia [1]
and around the world [2]. Although vaccinationrates in Australia
are high, they are below national targets [3]. Under-vaccinated
people are unevenly distributed, increasing risk of disease
transmission [4,5]. Vaccine-preventabledisease outbreaks and
deaths continue to occur [6]. Confidencein vaccinesis low; in a
2017 study, only 48% of Australian parents reported having no
concernsabout vaccines,while over a fifth believedthat vaccines
causeautism[7]. Other countriesare facingsimilar problems,with
low confidencein many Europeanand North American countries
[8], and vaccine-preventabledeaths continuing to occur despite
good access to vaccination [9–11]. Increasing confidence in
vaccineswill boost vaccineuptake [12–14],but there is a paucity
of effectivestrategiesto do so [15–18].
To help increase confidence, a better understandingof the
relationshipbetween vaccineattitudesand broaderdemographic
and psychosocialattributes within which they exist is needed
[2,15,18].Understandingthe relationship between vaccine atti-
tudes and psychosocial attributes related to healthcare and
governmentis particularlyimportant,becausevaccineconfidence
is linked to beliefs about health [12,17,19,20]and government
[12,21,22],and healthcareand governmentbodies are central to
promoting,delivering and regulatingvaccination.
Existing researchshows that vaccineattitudes exist as part of
psychosocialand demographicattributes[21,23,24].In Australia,
demographicattributeslike socioeconomicstatus(SES)and access
to services [5,7,8,25,26] are linked to vaccine confidence.
Psychosocialfactors related to health, like trust in healthcare
providers,predict vaccineuptake in Australia [27] and elsewhere
[17,28,29].Accessingalternativemedicalpractitionersand greater
relianceon the internetfor health informationare associatedwith
Abbreviations:CAM, complementaryand alternativemedicine; CI, confidence
interval;CMQ, conspiracistmentalityquestionnaire;HCAMQ, holistic complemen-
tary and alternativehealth questionnaire;HCSDS-R, healthcaresystem distrust
scale- revised;HH, holistic health; PSAS,patientself-advocacyscale;RR, risk ratio;
SES,socioeconomicstatus; WHO, World Health Organisation.
* Correspondingauthorat: AustralianResearchCentrein Sex,Health and Society,
La Trobe University,Building NR6, Bundoora,Victoria, 3086, Australia.
E-mail address:t.rozbroj@latrobe.edu.au(T. Rozbroj).
https://doi.org/10.1016/j.pec.2018.08.027
0738-3991/©2018 Elsevier B.V. All rights reserved.
Patient Educationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
Contents lists available at ScienceDirect
Patient Educationand Counseling
j o u r n a lhomep age: w w w . e l s ev i er . c o m / l o c a t e/ p a t e d u c o u
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

higher distrust in vaccines [7,19,30–33].Psychosocial factors
related to governmentalso predict vaccine confidence.A study
of 24 countries, including Australia, found that antivaccination
attitudes are associatedwith conspiratorialbeliefs and individu-
alist world views [23]. Research from outside the Australian
context has shown that vaccine confidence is associatedwith
trust in government[21,34],culture and values[35,36]and world
views [37].
Important gaps persist in knowledge about how Australians’
attitudes to vaccination relate to psychosocial characteristics
pertaining to healthcare and government.Overseasstudies are
problematic to apply to Australia, because the relationships
between vaccine attitudes and broader attributes are context-
specific [2,38–40]. While it is known that in Australia vaccine
attitudes relate to trust in healthcareproviders, little is known
about how they relate to health decision-making,health educa-
tion, and beliefs about the healthcare system, which may all
influence attitudes. Furthermore, little is known about how
vaccine attitudes in Australia relate to trust in governmentor
political orientations, despite both potentially being important
[21]. Few Australian studies have directly evaluatedhow people
across the spectrum of vaccine attitudes compare in broader
attributes related to either governmentor health, limiting the
extent to which intergroup differencescan be assessed.
The taxonomyand measurementof vaccineattitudes present
further challenges.The prevailing taxonomy,developed by the
World Health Organization (WHO), divides the spectrum of
attitudes into three categories:i) full acceptanceon one end, iii)
full refusal on the other, and ii) vaccine hesitancy in-between
[2,18,41].The hesitancy category is heterogeneous,comprising
those who accept vaccineswith some doubts, those who refuse
almostall vaccines,and all between[2,38].‘Hesitancy’is treatedas
a distinct entity in research [38], measurement [2,42] and
intervention design [18]. But hesitancy is an ambiguous“catch-
all category”, which potentially lumps together contrasting
attributes [43]. A more sensitive measurement of ‘hesitancy’,
which takesaccountof subgroupswithin this broadcategory,may
expose important differences. The prevailing taxonomy also
conflatesbehaviourwith attitude.For example,one point on the
spectrumis “acceptbut unsure”: acceptancereferring to uptake,
level of surenessbeing attitude [2]. But studiesconsistentlyshow
that uptakedoes not correspondto acceptance[7,12,25,27,35,44–
46], so a taxonomy focusing on attitude alone is needed for
researchinto vaccineattitudes.
The aim of this paper was to investigatehow Australianadults’
demographicattributesand psychosocialattributespertaining to
health and government compare among five vaccine attitude
groups, ranging from unwavering support to rejection of all
vaccines.
2. Methods
2.1.Designand sample
We analyseddata collected as part of the Australian Vaccine
Attitudes Survey.The online survey sampled adults (18+)living
acrossAustralia.A conveniencesampleof at least 250 participants
for eachattitudegroup was sought,to enablestatisticalanalysisat
95%CI. Participantswere recruitedbetweenJanuaryand May 2017
by distributinga genericlink to the surveyvia Facebookadverts,e-
newsletters/magazines,and posts on webpagesrelatedto parent-
hood and wellbeing. One Facebookadvert was targetedtowards
people who reject vaccines (approximately 2% of Australians
[7,25]) to boost participation from this group. The survey was
anonymous,and no reminderswere sent to encouragecompletion.
No incentives were offered to encourage participation. Ethics
approval was granted by the La Trobe University Human Ethics
Committee (ref: S16-208). The final sample comprised 4370
respondents.
2.2.Measures
We measured vaccine attitude, demographicattributes, and
psychosocial attributes relating to: i) relationship with the
healthcaresystem,which concernedhow respondentsconsume
health, and ii) relationship with government,which concerned
voting behaviourand trust in government.All study variablesare
listed in Table 2 and explainedin detail below.
2.2.1.Vaccineattitude
Table1 shows the questionused to measurevaccineattitudeas
a categorical variable, and the category labels used. Vaccine
attitude was also measured as a continuous variable, using a
validatedVaccinationScale,which measuresthe extent to which
attitudes are supportive of vaccination[47]. The six-point Likert
scalecomprisesfive items.Scalescorescan rangebetween1 and 6,
with high scores indicating supportive attitudes.This scale was
used to gauge the reliability of the categoricalvaccine attitude
variable.
2.2.2.Demographicprofile
Demographicmeasuresincluded: i) age,codedas 18–29/30–49
/50+; ii) gender,coded as male/female; iii) state or territory in
which participants lived; iv) remotenessof residence,coded as
urban/rural/regional;v) whether respondentshave children; vi)
education,coded as whether university educationwas attained,
vii) income, coded as above/below median weekly personal
income; and viii) perceivedhealth, measuredusing the General
Self-RatedHealth scale: a validated single-item 5-point scale of
Table 1
Vaccineattitude questionwording and categorylabels.
Original Question Outcome variable
category labels
Which of the followingbestdescribesyour attitudeto vaccination?
All recommendedchildhood vaccinesshould be administeredto all eligible children. I have no concernsabout them. All, unconcerned
All recommendedchildhood vaccinesshould be administeredto all eligible children. However,I have some concernsabout them. All, concerned
Most of the recommendedchildhood vaccinesshould be administeredto eligible children, but not in all casesand/or not for all the vaccines
on the schedule.
Most
Some recommendedchildhood vaccinesshould be administeredto eligible children, but not in most casesand/or not for the majority of the
vaccineson the schedule.
Some
None of the recommendedchildhood vaccinesshould be administeredto children. None
2 T. Rozbrojet al. / PatientEducationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
related to governmentalso predict vaccine confidence.A study
of 24 countries, including Australia, found that antivaccination
attitudes are associatedwith conspiratorialbeliefs and individu-
alist world views [23]. Research from outside the Australian
context has shown that vaccine confidence is associatedwith
trust in government[21,34],culture and values[35,36]and world
views [37].
Important gaps persist in knowledge about how Australians’
attitudes to vaccination relate to psychosocial characteristics
pertaining to healthcare and government.Overseasstudies are
problematic to apply to Australia, because the relationships
between vaccine attitudes and broader attributes are context-
specific [2,38–40]. While it is known that in Australia vaccine
attitudes relate to trust in healthcareproviders, little is known
about how they relate to health decision-making,health educa-
tion, and beliefs about the healthcare system, which may all
influence attitudes. Furthermore, little is known about how
vaccine attitudes in Australia relate to trust in governmentor
political orientations, despite both potentially being important
[21]. Few Australian studies have directly evaluatedhow people
across the spectrum of vaccine attitudes compare in broader
attributes related to either governmentor health, limiting the
extent to which intergroup differencescan be assessed.
The taxonomyand measurementof vaccineattitudes present
further challenges.The prevailing taxonomy,developed by the
World Health Organization (WHO), divides the spectrum of
attitudes into three categories:i) full acceptanceon one end, iii)
full refusal on the other, and ii) vaccine hesitancy in-between
[2,18,41].The hesitancy category is heterogeneous,comprising
those who accept vaccineswith some doubts, those who refuse
almostall vaccines,and all between[2,38].‘Hesitancy’is treatedas
a distinct entity in research [38], measurement [2,42] and
intervention design [18]. But hesitancy is an ambiguous“catch-
all category”, which potentially lumps together contrasting
attributes [43]. A more sensitive measurement of ‘hesitancy’,
which takesaccountof subgroupswithin this broadcategory,may
expose important differences. The prevailing taxonomy also
conflatesbehaviourwith attitude.For example,one point on the
spectrumis “acceptbut unsure”: acceptancereferring to uptake,
level of surenessbeing attitude [2]. But studiesconsistentlyshow
that uptakedoes not correspondto acceptance[7,12,25,27,35,44–
46], so a taxonomy focusing on attitude alone is needed for
researchinto vaccineattitudes.
The aim of this paper was to investigatehow Australianadults’
demographicattributesand psychosocialattributespertaining to
health and government compare among five vaccine attitude
groups, ranging from unwavering support to rejection of all
vaccines.
2. Methods
2.1.Designand sample
We analyseddata collected as part of the Australian Vaccine
Attitudes Survey.The online survey sampled adults (18+)living
acrossAustralia.A conveniencesampleof at least 250 participants
for eachattitudegroup was sought,to enablestatisticalanalysisat
95%CI. Participantswere recruitedbetweenJanuaryand May 2017
by distributinga genericlink to the surveyvia Facebookadverts,e-
newsletters/magazines,and posts on webpagesrelatedto parent-
hood and wellbeing. One Facebookadvert was targetedtowards
people who reject vaccines (approximately 2% of Australians
[7,25]) to boost participation from this group. The survey was
anonymous,and no reminderswere sent to encouragecompletion.
No incentives were offered to encourage participation. Ethics
approval was granted by the La Trobe University Human Ethics
Committee (ref: S16-208). The final sample comprised 4370
respondents.
2.2.Measures
We measured vaccine attitude, demographicattributes, and
psychosocial attributes relating to: i) relationship with the
healthcaresystem,which concernedhow respondentsconsume
health, and ii) relationship with government,which concerned
voting behaviourand trust in government.All study variablesare
listed in Table 2 and explainedin detail below.
2.2.1.Vaccineattitude
Table1 shows the questionused to measurevaccineattitudeas
a categorical variable, and the category labels used. Vaccine
attitude was also measured as a continuous variable, using a
validatedVaccinationScale,which measuresthe extent to which
attitudes are supportive of vaccination[47]. The six-point Likert
scalecomprisesfive items.Scalescorescan rangebetween1 and 6,
with high scores indicating supportive attitudes.This scale was
used to gauge the reliability of the categoricalvaccine attitude
variable.
2.2.2.Demographicprofile
Demographicmeasuresincluded: i) age,codedas 18–29/30–49
/50+; ii) gender,coded as male/female; iii) state or territory in
which participants lived; iv) remotenessof residence,coded as
urban/rural/regional;v) whether respondentshave children; vi)
education,coded as whether university educationwas attained,
vii) income, coded as above/below median weekly personal
income; and viii) perceivedhealth, measuredusing the General
Self-RatedHealth scale: a validated single-item 5-point scale of
Table 1
Vaccineattitude questionwording and categorylabels.
Original Question Outcome variable
category labels
Which of the followingbestdescribesyour attitudeto vaccination?
All recommendedchildhood vaccinesshould be administeredto all eligible children. I have no concernsabout them. All, unconcerned
All recommendedchildhood vaccinesshould be administeredto all eligible children. However,I have some concernsabout them. All, concerned
Most of the recommendedchildhood vaccinesshould be administeredto eligible children, but not in all casesand/or not for all the vaccines
on the schedule.
Most
Some recommendedchildhood vaccinesshould be administeredto eligible children, but not in most casesand/or not for the majority of the
vaccineson the schedule.
Some
None of the recommendedchildhood vaccinesshould be administeredto children. None
2 T. Rozbrojet al. / PatientEducationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
self-reportedoverall health. Possiblescoresrangedbetween 1–5,
with 1 indicating “poor health” and 5 indicating “excellent
health” [48].
2.2.3.Relationshipwith healthcaresystem
Relationship with the healthcaresystem was assessedusing
eight measures, covering trust in mainstream and alternative
healthcaresystems,and confidence/involvementin health deci-
sion-making.
Trust in the healthcaresystemwas measuredusing the Revised
Health Care System Distrust Scale (HCSDS-R) [49] on two
dimensions: i) values, comprising five items measuring trust in
the healthcare system’s honesty, motives and equity; and ii)
competence, comprising four items measuring trust in the
competencyof the healthcare system. Answers were provided
on a 5-point Likert scale. Possible score ranges were 5–25 for
values and 4–20 for competence.Higher scores indicate higher
distrust.
Attitudes to alternative medicine were measured using the
Holistic Complementaryand Alternative Health Questionnaire
(HCAMQ) [50] across two dimensions: i) holistic health (HH),
comprisingfive items measuringbelief that health and wellbeing
rely on treating the body holistically; and ii) complementaryand
alternativemedicine(CAM), comprisingsix items measuringbelief
in the scientificvalidity of CAM. Answers were providedon a six-
point Likert scale.Possiblescorerangeswere 5–30 for HH and 6–36
for CAM. Higher scoresindicate greaterbelief in CAM/HH.
Health decision-making was measured using two scales
assessing patient involvement in their health decisions and
confidencein their health decision-makingability. Confidencein
health decision-makingability was measured using the single-
dimensional Decision Self-EfficacyScale [51], which contains 11
items on a five-point Likert scale.Scorescould range between 0-
100.Patientinvolvementin healthdecision-makingwas measured
using the Patient Self-AdvocacyScale(PSAS)[52], which has three
subscales,each comprising four items measured on a 5-point
Likert scale measuringpatients’:i) illness and treatmenteduca-
tion; ii) assertivenessin health decisionmaking; and iii) potential
for non-adherenceto recommendedtreatments.Subscalescores
could range between 1-5. Higher scores indicate greater confi-
dence/involvementin health decision-making.
2.2.4.Relationshipwith government
Relationship with the governmentwas assessedusing three
measures,coveringtrust in government,conspiracistideation and
voter preference.Trust in governmentwas measuredby a single
questiondevelopedby PEW research[53], with possiblescoresof
1-5. High scores indicate high trust. The Conspiracy Mentality
Questionnaire(CMQ) measureddifferencesin the generictenden-
cy for conspiracistideation[54].It containsfive items measuredon
an 11-point scale,with possiblescoresbetween0–10. High scores
indicate high conspiracist ideation. Voter preferencewas mea-
sured by a non-standardisedquestionaskingwhich political party
respondentsvoted for in the last Federalelection,coded as ‘voted
for: major/minor party’.
2.3.Analysis
Descriptivestatisticswere calculatedfor the sample i) overall,
and ii) cross-tabulatedby five vaccine attitudes.Validity of the
categorical vaccine attitude variable was checked using linear
regression,comparingvaccineattitude categorieswith scoreson
the VaccinationScale.Multinomial logistic regressionwas used to
test the extent to which vaccine attitude was predicted by
demographic and psychosocial attributes. The ‘most’ attitude
was assignedthe referencecategory,becausewe were particularly
interested in differences between the three ‘hesitant’ groups.
Univariableregressionswere first conductedfor eachdemographic
and psychosocialvariable.A single multivariable regressionwas
then conducted.Only predictors that were associatedwith the
outcome variable at p < 0.25 in the univariableregressionswere
entered into the multivariable regression.Respondentswho did
not respond on all variablesunder analysis were excludedfrom
multivariableregression,which was conductedwith a sample of
3471.Risk ratios (RR) and 95%confidenceintervals (95%CI) were
calculated,and a Wald test was used to assessthe overall effectof
each predictor variable.Associationsat p < 0.05 were considered
significant.
3. Results
3.1.Preliminaryanalysis
To gaugethe reliability of the five categorymeasureof vaccine
attitude,linear regressionwas usedto comparethe categorieswith
scoreson the VaccinationScale[47].The scalescoressignificantly
differed in the expected direction across the five categories(F
[4,4365]=7319.74,p < 0.001).With the ‘most’categoryas the base,
the coefficients were β =1.69 (p < 0.001) for ‘all unconcerned’,
β =1.27(p < 0.001)for ‘all concerned’,β=-1.83(p < 0.001)for ‘some’,
and β=-2.44(p < 0.001)for ‘none’.This suggeststhat the categorical
outcome variable served as an accurate indicator of vaccine
attitude.
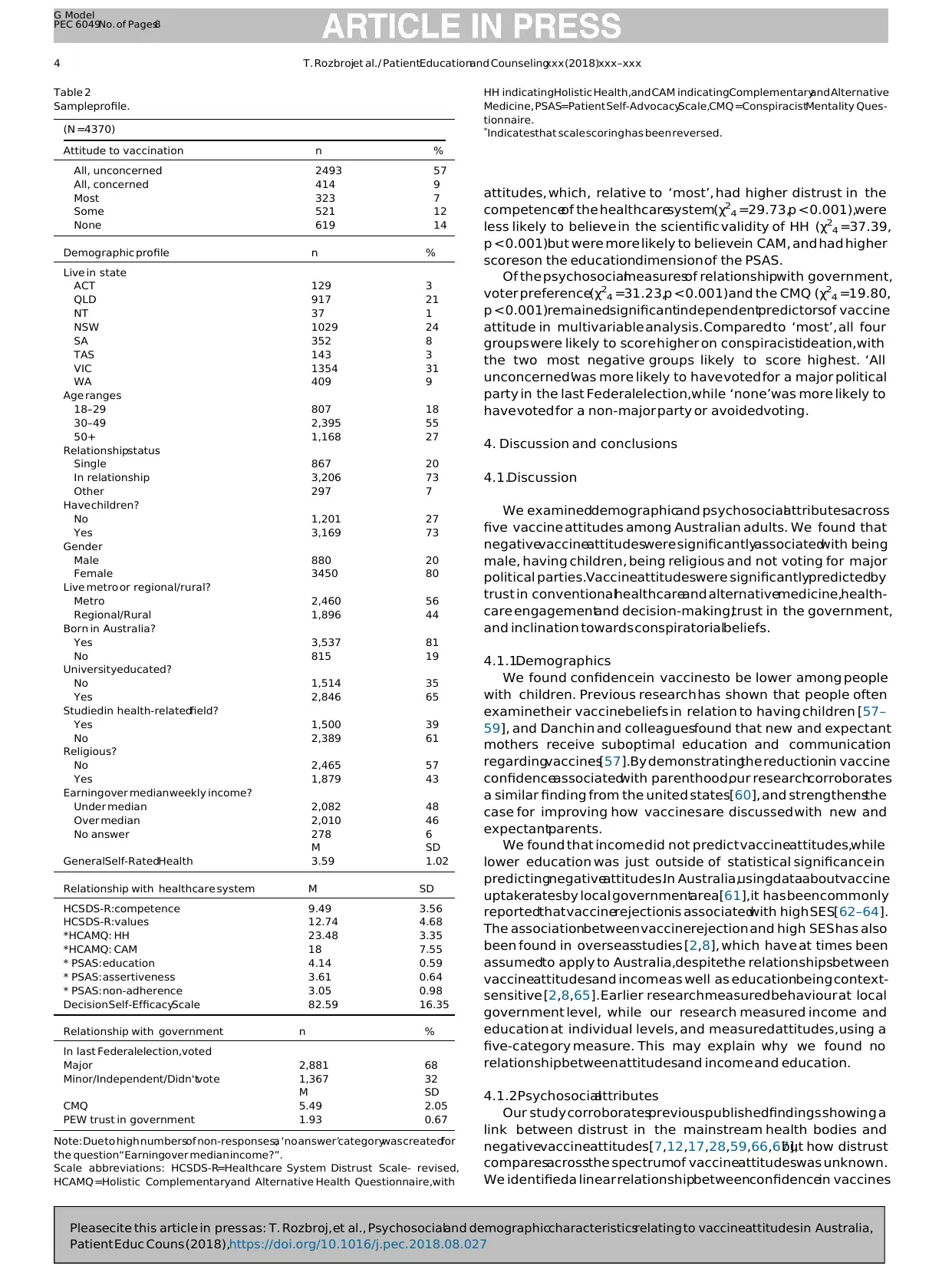
3.2.Sampleprofile
The sampleprofile is displayedin Table2. Typical respondents
were 30–49 yearsold, in a relationship,with children and born in
Australia.Relativeto the Australianpopulation,over-represented
were women (n =80%,comparedto 50.4%in Australiain 2016)[55]
and thosewith a universityeducation(n =65%,comparedto 23.7%
in Australia in 2011) [56]. Among the 4370 respondents,almost
three-fifths supportedvaccineswithout concerns.
3.3.Multivariableanalysis
In the univariableanalyses,all demographicand psychosocial
variables were significantly associatedwith vaccine attitude at
p < 0.001.
In the multivariableanalysis(Table3), significantindependent
demographicfactorsincluded whether respondentshavechildren
(χ24 =28.40,p < 0.001),respondents’gender(χ24 =16.75,p =0.002),
whether they were religious(χ24 =20.09,p =0.001),and their self-
reported health (χ24 =43.82, p < 0.001). Compared to the ‘most’
group,the two ‘all’ groupswere more likely to be childlessand not
religious,while the two most negativegroupswere more likely to
be male and to report being healthier.The ‘none’group was also
more likely to report havingchildrencomparedto the ‘most’group.
Insignificant predictors included respondents’income (p =0.93),
education (p =0.06) and whether they studied a health-related
field (p =0.09).
All psychosocialmeasuresof relationship with the healthcare
systemwere significantindependentfactorsof vaccineattitudein
the multivariableanalysis.Comparedto the ‘most’group,the two
‘all’ groups had significantly higher trust in the values of the
healthcare system (X24 =55.83, p < 0.001), lower education and
non-adherence scores on the PSAS (χ24 =21.12, p < 0.001 and
χ24 =62.86,p < 0.001respectively),and were less likely to believe
in the scientific validity of CAM (χ24 =313.07,p < 0.001).Further-
more, ‘all unconcerned’was associatedwith lower assertiveness
on the PSAS(χ24 =16.79,p =0.002)but higher decisionself-efficacy
(χ24 =47.19,p < 0.001).This comparedto the two least accepting
T. Rozbrojet al./ PatientEducationand Counselingxxx (2018)xxx–xxx 3
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
with 1 indicating “poor health” and 5 indicating “excellent
health” [48].
2.2.3.Relationshipwith healthcaresystem
Relationship with the healthcaresystem was assessedusing
eight measures, covering trust in mainstream and alternative
healthcaresystems,and confidence/involvementin health deci-
sion-making.
Trust in the healthcaresystemwas measuredusing the Revised
Health Care System Distrust Scale (HCSDS-R) [49] on two
dimensions: i) values, comprising five items measuring trust in
the healthcare system’s honesty, motives and equity; and ii)
competence, comprising four items measuring trust in the
competencyof the healthcare system. Answers were provided
on a 5-point Likert scale. Possible score ranges were 5–25 for
values and 4–20 for competence.Higher scores indicate higher
distrust.
Attitudes to alternative medicine were measured using the
Holistic Complementaryand Alternative Health Questionnaire
(HCAMQ) [50] across two dimensions: i) holistic health (HH),
comprisingfive items measuringbelief that health and wellbeing
rely on treating the body holistically; and ii) complementaryand
alternativemedicine(CAM), comprisingsix items measuringbelief
in the scientificvalidity of CAM. Answers were providedon a six-
point Likert scale.Possiblescorerangeswere 5–30 for HH and 6–36
for CAM. Higher scoresindicate greaterbelief in CAM/HH.
Health decision-making was measured using two scales
assessing patient involvement in their health decisions and
confidencein their health decision-makingability. Confidencein
health decision-makingability was measured using the single-
dimensional Decision Self-EfficacyScale [51], which contains 11
items on a five-point Likert scale.Scorescould range between 0-
100.Patientinvolvementin healthdecision-makingwas measured
using the Patient Self-AdvocacyScale(PSAS)[52], which has three
subscales,each comprising four items measured on a 5-point
Likert scale measuringpatients’:i) illness and treatmenteduca-
tion; ii) assertivenessin health decisionmaking; and iii) potential
for non-adherenceto recommendedtreatments.Subscalescores
could range between 1-5. Higher scores indicate greater confi-
dence/involvementin health decision-making.
2.2.4.Relationshipwith government
Relationship with the governmentwas assessedusing three
measures,coveringtrust in government,conspiracistideation and
voter preference.Trust in governmentwas measuredby a single
questiondevelopedby PEW research[53], with possiblescoresof
1-5. High scores indicate high trust. The Conspiracy Mentality
Questionnaire(CMQ) measureddifferencesin the generictenden-
cy for conspiracistideation[54].It containsfive items measuredon
an 11-point scale,with possiblescoresbetween0–10. High scores
indicate high conspiracist ideation. Voter preferencewas mea-
sured by a non-standardisedquestionaskingwhich political party
respondentsvoted for in the last Federalelection,coded as ‘voted
for: major/minor party’.
2.3.Analysis
Descriptivestatisticswere calculatedfor the sample i) overall,
and ii) cross-tabulatedby five vaccine attitudes.Validity of the
categorical vaccine attitude variable was checked using linear
regression,comparingvaccineattitude categorieswith scoreson
the VaccinationScale.Multinomial logistic regressionwas used to
test the extent to which vaccine attitude was predicted by
demographic and psychosocial attributes. The ‘most’ attitude
was assignedthe referencecategory,becausewe were particularly
interested in differences between the three ‘hesitant’ groups.
Univariableregressionswere first conductedfor eachdemographic
and psychosocialvariable.A single multivariable regressionwas
then conducted.Only predictors that were associatedwith the
outcome variable at p < 0.25 in the univariableregressionswere
entered into the multivariable regression.Respondentswho did
not respond on all variablesunder analysis were excludedfrom
multivariableregression,which was conductedwith a sample of
3471.Risk ratios (RR) and 95%confidenceintervals (95%CI) were
calculated,and a Wald test was used to assessthe overall effectof
each predictor variable.Associationsat p < 0.05 were considered
significant.
3. Results
3.1.Preliminaryanalysis
To gaugethe reliability of the five categorymeasureof vaccine
attitude,linear regressionwas usedto comparethe categorieswith
scoreson the VaccinationScale[47].The scalescoressignificantly
differed in the expected direction across the five categories(F
[4,4365]=7319.74,p < 0.001).With the ‘most’categoryas the base,
the coefficients were β =1.69 (p < 0.001) for ‘all unconcerned’,
β =1.27(p < 0.001)for ‘all concerned’,β=-1.83(p < 0.001)for ‘some’,
and β=-2.44(p < 0.001)for ‘none’.This suggeststhat the categorical
outcome variable served as an accurate indicator of vaccine
attitude.
3.2.Sampleprofile
The sampleprofile is displayedin Table2. Typical respondents
were 30–49 yearsold, in a relationship,with children and born in
Australia.Relativeto the Australianpopulation,over-represented
were women (n =80%,comparedto 50.4%in Australiain 2016)[55]
and thosewith a universityeducation(n =65%,comparedto 23.7%
in Australia in 2011) [56]. Among the 4370 respondents,almost
three-fifths supportedvaccineswithout concerns.
3.3.Multivariableanalysis
In the univariableanalyses,all demographicand psychosocial
variables were significantly associatedwith vaccine attitude at
p < 0.001.
In the multivariableanalysis(Table3), significantindependent
demographicfactorsincluded whether respondentshavechildren
(χ24 =28.40,p < 0.001),respondents’gender(χ24 =16.75,p =0.002),
whether they were religious(χ24 =20.09,p =0.001),and their self-
reported health (χ24 =43.82, p < 0.001). Compared to the ‘most’
group,the two ‘all’ groupswere more likely to be childlessand not
religious,while the two most negativegroupswere more likely to
be male and to report being healthier.The ‘none’group was also
more likely to report havingchildrencomparedto the ‘most’group.
Insignificant predictors included respondents’income (p =0.93),
education (p =0.06) and whether they studied a health-related
field (p =0.09).
All psychosocialmeasuresof relationship with the healthcare
systemwere significantindependentfactorsof vaccineattitudein
the multivariableanalysis.Comparedto the ‘most’group,the two
‘all’ groups had significantly higher trust in the values of the
healthcare system (X24 =55.83, p < 0.001), lower education and
non-adherence scores on the PSAS (χ24 =21.12, p < 0.001 and
χ24 =62.86,p < 0.001respectively),and were less likely to believe
in the scientific validity of CAM (χ24 =313.07,p < 0.001).Further-
more, ‘all unconcerned’was associatedwith lower assertiveness
on the PSAS(χ24 =16.79,p =0.002)but higher decisionself-efficacy
(χ24 =47.19,p < 0.001).This comparedto the two least accepting
T. Rozbrojet al./ PatientEducationand Counselingxxx (2018)xxx–xxx 3
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
attitudes, which, relative to ‘most’, had higher distrust in the
competenceof the healthcaresystem(χ24 =29.73,p < 0.001),were
less likely to believe in the scientific validity of HH (χ24 =37.39,
p < 0.001)but were more likely to believein CAM, and had higher
scoreson the educationdimension of the PSAS.
Of the psychosocialmeasuresof relationshipwith government,
voter preference(χ24 =31.23,p < 0.001) and the CMQ (χ24 =19.80,
p < 0.001)remainedsignificantindependentpredictorsof vaccine
attitude in multivariable analysis. Compared to ‘most’, all four
groups were likely to score higher on conspiracistideation, with
the two most negative groups likely to score highest. ‘All
unconcerned’was more likely to have voted for a major political
party in the last Federalelection,while ‘none’was more likely to
have voted for a non-major party or avoidedvoting.
4. Discussion and conclusions
4.1.Discussion
We examineddemographicand psychosocialattributesacross
five vaccine attitudes among Australian adults. We found that
negativevaccineattitudeswere significantlyassociatedwith being
male, having children, being religious and not voting for major
political parties.Vaccineattitudeswere significantlypredictedby
trust in conventionalhealthcareand alternativemedicine,health-
care engagementand decision-making,trust in the government,
and inclination towards conspiratorialbeliefs.
4.1.1.Demographics
We found confidencein vaccinesto be lower among people
with children. Previous research has shown that people often
examinetheir vaccinebeliefs in relation to having children [57–
59], and Danchin and colleaguesfound that new and expectant
mothers receive suboptimal education and communication
regardingvaccines[57].By demonstratingthe reductionin vaccine
confidenceassociatedwith parenthood,our researchcorroborates
a similar finding from the united states[60], and strengthensthe
case for improving how vaccines are discussed with new and
expectantparents.
We found that income did not predict vaccineattitudes,while
lower education was just outside of statistical significance in
predictingnegativeattitudes.In Australia,usingdataaboutvaccine
uptakeratesby local governmentarea[61],it has been commonly
reportedthat vaccinerejectionis associatedwith high SES[62–64].
The associationbetween vaccinerejection and high SES has also
been found in overseasstudies [2,8], which have at times been
assumedto apply to Australia,despitethe relationshipsbetween
vaccineattitudesand income as well as educationbeing context-
sensitive [2,8,65]. Earlier research measured behaviour at local
government level, while our research measured income and
education at individual levels, and measured attitudes, using a
five-category measure. This may explain why we found no
relationship between attitudesand income and education.
4.1.2.Psychosocialattributes
Our study corroboratesprevious publishedfindings showing a
link between distrust in the mainstream health bodies and
negativevaccineattitudes[7,12,17,28,59,66,67],but how distrust
comparesacrossthe spectrumof vaccineattitudeswas unknown.
We identifieda linear relationshipbetweenconfidencein vaccines
Table 2
Sampleprofile.
(N =4370)
Attitude to vaccination n %
All, unconcerned 2493 57
All, concerned 414 9
Most 323 7
Some 521 12
None 619 14
Demographic profile n %
Live in state
ACT 129 3
QLD 917 21
NT 37 1
NSW 1029 24
SA 352 8
TAS 143 3
VIC 1354 31
WA 409 9
Age ranges
18–29 807 18
30–49 2,395 55
50+ 1,168 27
Relationshipstatus
Single 867 20
In relationship 3,206 73
Other 297 7
Have children?
No 1,201 27
Yes 3,169 73
Gender
Male 880 20
Female 3450 80
Live metro or regional/rural?
Metro 2,460 56
Regional/Rural 1,896 44
Born in Australia?
Yes 3,537 81
No 815 19
Universityeducated?
No 1,514 35
Yes 2,846 65
Studied in health-relatedfield?
Yes 1,500 39
No 2,389 61
Religious?
No 2,465 57
Yes 1,879 43
Earning over median weekly income?
Under median 2,082 48
Over median 2,010 46
No answer 278 6
M SD
GeneralSelf-RatedHealth 3.59 1.02
Relationship with healthcare system M SD
HCSDS-R:competence 9.49 3.56
HCSDS-R:values 12.74 4.68
*HCAMQ: HH 23.48 3.35
*HCAMQ: CAM 18 7.55
* PSAS: education 4.14 0.59
* PSAS: assertiveness 3.61 0.64
* PSAS: non-adherence 3.05 0.98
Decision Self-EfficacyScale 82.59 16.35
Relationship with government n %
In last Federalelection,voted
Major 2,881 68
Minor/Independent/Didn'tvote 1,367 32
M SD
CMQ 5.49 2.05
PEW trust in government 1.93 0.67
Note: Due to high numbersof non-responses,a ‘no answer’categorywas createdfor
the question“Earningover median income?”.
Scale abbreviations: HCSDS-R=Healthcare System Distrust Scale- revised,
HCAMQ =Holistic Complementaryand Alternative Health Questionnaire,with
HH indicatingHolistic Health,and CAM indicatingComplementaryand Alternative
Medicine, PSAS=Patient Self-AdvocacyScale,CMQ =ConspiracistMentality Ques-
tionnaire.
*
Indicatesthat scale scoring has been reversed.
4 T. Rozbrojet al. / PatientEducationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
competenceof the healthcaresystem(χ24 =29.73,p < 0.001),were
less likely to believe in the scientific validity of HH (χ24 =37.39,
p < 0.001)but were more likely to believein CAM, and had higher
scoreson the educationdimension of the PSAS.
Of the psychosocialmeasuresof relationshipwith government,
voter preference(χ24 =31.23,p < 0.001) and the CMQ (χ24 =19.80,
p < 0.001)remainedsignificantindependentpredictorsof vaccine
attitude in multivariable analysis. Compared to ‘most’, all four
groups were likely to score higher on conspiracistideation, with
the two most negative groups likely to score highest. ‘All
unconcerned’was more likely to have voted for a major political
party in the last Federalelection,while ‘none’was more likely to
have voted for a non-major party or avoidedvoting.
4. Discussion and conclusions
4.1.Discussion
We examineddemographicand psychosocialattributesacross
five vaccine attitudes among Australian adults. We found that
negativevaccineattitudeswere significantlyassociatedwith being
male, having children, being religious and not voting for major
political parties.Vaccineattitudeswere significantlypredictedby
trust in conventionalhealthcareand alternativemedicine,health-
care engagementand decision-making,trust in the government,
and inclination towards conspiratorialbeliefs.
4.1.1.Demographics
We found confidencein vaccinesto be lower among people
with children. Previous research has shown that people often
examinetheir vaccinebeliefs in relation to having children [57–
59], and Danchin and colleaguesfound that new and expectant
mothers receive suboptimal education and communication
regardingvaccines[57].By demonstratingthe reductionin vaccine
confidenceassociatedwith parenthood,our researchcorroborates
a similar finding from the united states[60], and strengthensthe
case for improving how vaccines are discussed with new and
expectantparents.
We found that income did not predict vaccineattitudes,while
lower education was just outside of statistical significance in
predictingnegativeattitudes.In Australia,usingdataaboutvaccine
uptakeratesby local governmentarea[61],it has been commonly
reportedthat vaccinerejectionis associatedwith high SES[62–64].
The associationbetween vaccinerejection and high SES has also
been found in overseasstudies [2,8], which have at times been
assumedto apply to Australia,despitethe relationshipsbetween
vaccineattitudesand income as well as educationbeing context-
sensitive [2,8,65]. Earlier research measured behaviour at local
government level, while our research measured income and
education at individual levels, and measured attitudes, using a
five-category measure. This may explain why we found no
relationship between attitudesand income and education.
4.1.2.Psychosocialattributes
Our study corroboratesprevious publishedfindings showing a
link between distrust in the mainstream health bodies and
negativevaccineattitudes[7,12,17,28,59,66,67],but how distrust
comparesacrossthe spectrumof vaccineattitudeswas unknown.
We identifieda linear relationshipbetweenconfidencein vaccines
Table 2
Sampleprofile.
(N =4370)
Attitude to vaccination n %
All, unconcerned 2493 57
All, concerned 414 9
Most 323 7
Some 521 12
None 619 14
Demographic profile n %
Live in state
ACT 129 3
QLD 917 21
NT 37 1
NSW 1029 24
SA 352 8
TAS 143 3
VIC 1354 31
WA 409 9
Age ranges
18–29 807 18
30–49 2,395 55
50+ 1,168 27
Relationshipstatus
Single 867 20
In relationship 3,206 73
Other 297 7
Have children?
No 1,201 27
Yes 3,169 73
Gender
Male 880 20
Female 3450 80
Live metro or regional/rural?
Metro 2,460 56
Regional/Rural 1,896 44
Born in Australia?
Yes 3,537 81
No 815 19
Universityeducated?
No 1,514 35
Yes 2,846 65
Studied in health-relatedfield?
Yes 1,500 39
No 2,389 61
Religious?
No 2,465 57
Yes 1,879 43
Earning over median weekly income?
Under median 2,082 48
Over median 2,010 46
No answer 278 6
M SD
GeneralSelf-RatedHealth 3.59 1.02
Relationship with healthcare system M SD
HCSDS-R:competence 9.49 3.56
HCSDS-R:values 12.74 4.68
*HCAMQ: HH 23.48 3.35
*HCAMQ: CAM 18 7.55
* PSAS: education 4.14 0.59
* PSAS: assertiveness 3.61 0.64
* PSAS: non-adherence 3.05 0.98
Decision Self-EfficacyScale 82.59 16.35
Relationship with government n %
In last Federalelection,voted
Major 2,881 68
Minor/Independent/Didn'tvote 1,367 32
M SD
CMQ 5.49 2.05
PEW trust in government 1.93 0.67
Note: Due to high numbersof non-responses,a ‘no answer’categorywas createdfor
the question“Earningover median income?”.
Scale abbreviations: HCSDS-R=Healthcare System Distrust Scale- revised,
HCAMQ =Holistic Complementaryand Alternative Health Questionnaire,with
HH indicatingHolistic Health,and CAM indicatingComplementaryand Alternative
Medicine, PSAS=Patient Self-AdvocacyScale,CMQ =ConspiracistMentality Ques-
tionnaire.
*
Indicatesthat scale scoring has been reversed.
4 T. Rozbrojet al. / PatientEducationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
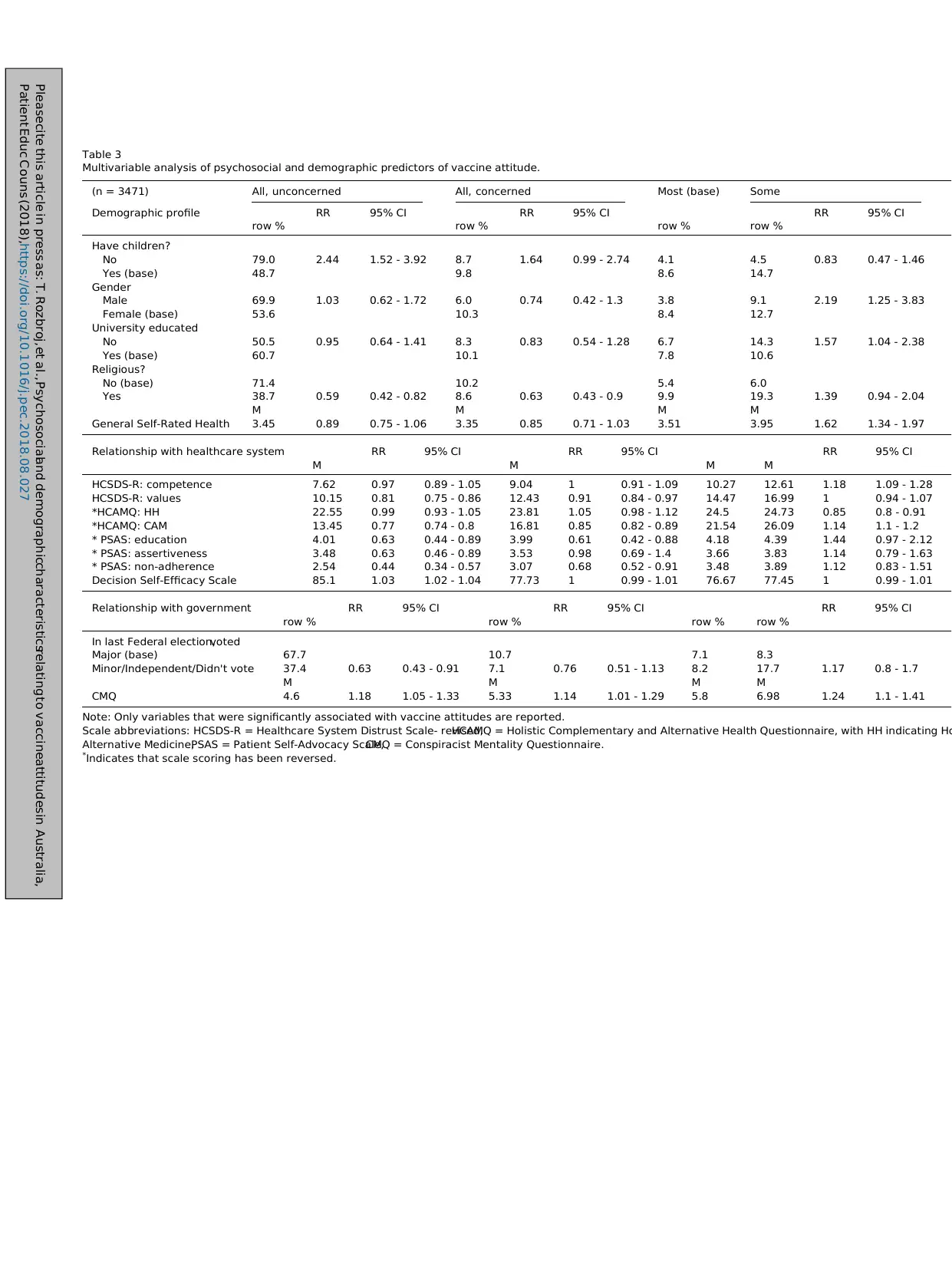
Table 3
Multivariable analysis of psychosocial and demographic predictors of vaccine attitude.
(n = 3471) All, unconcerned All, concerned Most (base) Some
Demographic profile RR 95% CI RR 95% CI RR 95% CI
row % row % row % row %
Have children?
No 79.0 2.44 1.52 - 3.92 8.7 1.64 0.99 - 2.74 4.1 4.5 0.83 0.47 - 1.46
Yes (base) 48.7 9.8 8.6 14.7
Gender
Male 69.9 1.03 0.62 - 1.72 6.0 0.74 0.42 - 1.3 3.8 9.1 2.19 1.25 - 3.83
Female (base) 53.6 10.3 8.4 12.7
University educated
No 50.5 0.95 0.64 - 1.41 8.3 0.83 0.54 - 1.28 6.7 14.3 1.57 1.04 - 2.38
Yes (base) 60.7 10.1 7.8 10.6
Religious?
No (base) 71.4 10.2 5.4 6.0
Yes 38.7 0.59 0.42 - 0.82 8.6 0.63 0.43 - 0.9 9.9 19.3 1.39 0.94 - 2.04
M M M M
General Self-Rated Health 3.45 0.89 0.75 - 1.06 3.35 0.85 0.71 - 1.03 3.51 3.95 1.62 1.34 - 1.97
Relationship with healthcare system RR 95% CI RR 95% CI RR 95% CI
M M M M
HCSDS-R: competence 7.62 0.97 0.89 - 1.05 9.04 1 0.91 - 1.09 10.27 12.61 1.18 1.09 - 1.28
HCSDS-R: values 10.15 0.81 0.75 - 0.86 12.43 0.91 0.84 - 0.97 14.47 16.99 1 0.94 - 1.07
*HCAMQ: HH 22.55 0.99 0.93 - 1.05 23.81 1.05 0.98 - 1.12 24.5 24.73 0.85 0.8 - 0.91
*HCAMQ: CAM 13.45 0.77 0.74 - 0.8 16.81 0.85 0.82 - 0.89 21.54 26.09 1.14 1.1 - 1.2
* PSAS: education 4.01 0.63 0.44 - 0.89 3.99 0.61 0.42 - 0.88 4.18 4.39 1.44 0.97 - 2.12
* PSAS: assertiveness 3.48 0.63 0.46 - 0.89 3.53 0.98 0.69 - 1.4 3.66 3.83 1.14 0.79 - 1.63
* PSAS: non-adherence 2.54 0.44 0.34 - 0.57 3.07 0.68 0.52 - 0.91 3.48 3.89 1.12 0.83 - 1.51
Decision Self-Efficacy Scale 85.1 1.03 1.02 - 1.04 77.73 1 0.99 - 1.01 76.67 77.45 1 0.99 - 1.01
Relationship with government RR 95% CI RR 95% CI RR 95% CI
row % row % row % row %
In last Federal election,voted
Major (base) 67.7 10.7 7.1 8.3
Minor/Independent/Didn't vote 37.4 0.63 0.43 - 0.91 7.1 0.76 0.51 - 1.13 8.2 17.7 1.17 0.8 - 1.7
M M M M
CMQ 4.6 1.18 1.05 - 1.33 5.33 1.14 1.01 - 1.29 5.8 6.98 1.24 1.1 - 1.41
Note: Only variables that were significantly associated with vaccine attitudes are reported.
Scale abbreviations: HCSDS-R = Healthcare System Distrust Scale- revised,HCAMQ = Holistic Complementary and Alternative Health Questionnaire, with HH indicating Ho
Alternative Medicine,PSAS = Patient Self-Advocacy Scale,CMQ = Conspiracist Mentality Questionnaire.
*
Indicates that scale scoring has been reversed.
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
Multivariable analysis of psychosocial and demographic predictors of vaccine attitude.
(n = 3471) All, unconcerned All, concerned Most (base) Some
Demographic profile RR 95% CI RR 95% CI RR 95% CI
row % row % row % row %
Have children?
No 79.0 2.44 1.52 - 3.92 8.7 1.64 0.99 - 2.74 4.1 4.5 0.83 0.47 - 1.46
Yes (base) 48.7 9.8 8.6 14.7
Gender
Male 69.9 1.03 0.62 - 1.72 6.0 0.74 0.42 - 1.3 3.8 9.1 2.19 1.25 - 3.83
Female (base) 53.6 10.3 8.4 12.7
University educated
No 50.5 0.95 0.64 - 1.41 8.3 0.83 0.54 - 1.28 6.7 14.3 1.57 1.04 - 2.38
Yes (base) 60.7 10.1 7.8 10.6
Religious?
No (base) 71.4 10.2 5.4 6.0
Yes 38.7 0.59 0.42 - 0.82 8.6 0.63 0.43 - 0.9 9.9 19.3 1.39 0.94 - 2.04
M M M M
General Self-Rated Health 3.45 0.89 0.75 - 1.06 3.35 0.85 0.71 - 1.03 3.51 3.95 1.62 1.34 - 1.97
Relationship with healthcare system RR 95% CI RR 95% CI RR 95% CI
M M M M
HCSDS-R: competence 7.62 0.97 0.89 - 1.05 9.04 1 0.91 - 1.09 10.27 12.61 1.18 1.09 - 1.28
HCSDS-R: values 10.15 0.81 0.75 - 0.86 12.43 0.91 0.84 - 0.97 14.47 16.99 1 0.94 - 1.07
*HCAMQ: HH 22.55 0.99 0.93 - 1.05 23.81 1.05 0.98 - 1.12 24.5 24.73 0.85 0.8 - 0.91
*HCAMQ: CAM 13.45 0.77 0.74 - 0.8 16.81 0.85 0.82 - 0.89 21.54 26.09 1.14 1.1 - 1.2
* PSAS: education 4.01 0.63 0.44 - 0.89 3.99 0.61 0.42 - 0.88 4.18 4.39 1.44 0.97 - 2.12
* PSAS: assertiveness 3.48 0.63 0.46 - 0.89 3.53 0.98 0.69 - 1.4 3.66 3.83 1.14 0.79 - 1.63
* PSAS: non-adherence 2.54 0.44 0.34 - 0.57 3.07 0.68 0.52 - 0.91 3.48 3.89 1.12 0.83 - 1.51
Decision Self-Efficacy Scale 85.1 1.03 1.02 - 1.04 77.73 1 0.99 - 1.01 76.67 77.45 1 0.99 - 1.01
Relationship with government RR 95% CI RR 95% CI RR 95% CI
row % row % row % row %
In last Federal election,voted
Major (base) 67.7 10.7 7.1 8.3
Minor/Independent/Didn't vote 37.4 0.63 0.43 - 0.91 7.1 0.76 0.51 - 1.13 8.2 17.7 1.17 0.8 - 1.7
M M M M
CMQ 4.6 1.18 1.05 - 1.33 5.33 1.14 1.01 - 1.29 5.8 6.98 1.24 1.1 - 1.41
Note: Only variables that were significantly associated with vaccine attitudes are reported.
Scale abbreviations: HCSDS-R = Healthcare System Distrust Scale- revised,HCAMQ = Holistic Complementary and Alternative Health Questionnaire, with HH indicating Ho
Alternative Medicine,PSAS = Patient Self-Advocacy Scale,CMQ = Conspiracist Mentality Questionnaire.
*
Indicates that scale scoring has been reversed.
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027

and trust in both the values and competenceof the healthcare
system.Interestingly,even respondentswho believedall vaccines
should be administered,but had concerns,had lower trust in the
valuesof the healthcaresystemthan those without concerns.The
subscale measured level of agreement on items such as “the
healthcare system:. . . lies to make money”, “experimentson
patientswithout them knowing”,and “coversup its mistakes”[49].
The differencein risk ratios betweenthe two ‘all’ groupsshould be
interpreted with caution, as both scores were calculated in
reference to the ‘most’ category.Nevertheless,the increase in
healthcaresystem distrust associatedwith lower confidencein
vaccines is worrying. HCWs are integral to addressingvaccine
concerns[30,31,68],and this role may be encumberedby patients’
distrust in the healthcaresystem.Distrustof both competenceand
values of the healthcare system among people who distrust
vaccines should be accounted for when responding to vaccine
distrust.
To our knowledge,this studywas the first to assessboth HH and
CAM belief across the spectrum of attitudes. Previous research
linked negativeattitudeswith adherenceto alternativemedicine
in general[30,69–71].Theselinks are supportedby our finding that
negativeattitudeswere associatedwith belief in CAM. But we also
found negativeattitudesto be associatedwith rejectionof HH. This
is interesting,becauseusually belief in HH predictsbelief in CAM
[50,72,73].Studiesfrom other topics showed that, in lieu of belief
in HH, CAM was often chosen due to dissatisfaction with
conventional treatment experiences [74–76]. This explanation
would be plausible for our findings,given that negativeattitudes
were also associatedwith lower trust in the competenceof the
healthcaresystem.It may be worth investigatingthis further in
future research to gain insights into why some people begin
distrusting vaccines.
We found that vaccinerejection relatedto broaderdissatisfac-
tion with governance.On the CMQ, which contains no health-
specific questions [54], negativeattitudes were associatedwith
higher scores, suggesting a higher tendency towards general
conspiracistideation. These findings corroborateanother recent
study showing that antivaccination attitudes are linked to
conspiratorialthinking [23]. Negativeattitudes were also linked
to voting for minor political parties, which supports Larson’s
argument that political views play an important role in vaccine
decisions[21].Previousresearchhas shown links betweenvaccine
rejection and conspiracistviews regarding vaccination [77–79].
Our and other findings[21,23]suggestthat vaccinedistrustmay be
linked to broader anti-establishmentbeliefs.
4.1.3.Implicationsfor taxonomyof vaccineattitudes
Substantialresearcheffortsare beinginvestedinto understand-
ing and addressingvaccine‘hesitancy’[2,18,38–43,80].However,
in our data,the ‘hesitant’categorydoesnot capturea distinct set of
demographic or psychosocial attributes. On most predictor
variables,there is a linear pattern between risk ratios across the
five attitudes,with scores often being most similar between ‘all
unconcerned’ and ‘all concerned, and ‘some’ and ‘none’. Our
researchwas designedto respondto a key aim of the WHO: assess
how the hesitantcategoryrelatesto socioculturalprofiles [2,18].In
responding to this aim, we found it would be better to assess
‘hesitancy’using a more granularset of categories,like thosein the
present study, or other alternatives,like the categoriesused by
Leask and colleagues[14].
4.2.Limitations
This researchhad severallimitations.It was not viableto recruit
a representativesample.Sincevaccinationis refusedby only about
2%of the population [7,25],untargetedrecruitmentof this group
would not be feasible.As noted in the results,some demographic
attributeswere over-represented.But overall,a diversesamplewas
achieved.
The cross-sectionaldesign only enabled us to assessassocia-
tions. Understanding the causal interplay between vaccine
attitudes and demographic and psychosocial attributes would
providefurther understandingof how particularattitudesemerge.
Longitudinal design could be considered for future research to
assess directions of causality between attitudes and broader
attributes.
4.3.Practiceimplications
This researchcontributesto understandingvaccineattitudesin
their socio-culturalcontext,which is useful for improving patient
education and communication about vaccines. Our findings
suggestthat vaccinepromotion,which tends to focus on benefits
and safety of vaccines,should also focus on building trust in the
governmentand healthcaresystem.Both healthcaresystem and
governmentwere distrusted by participants who lacked confi-
dence in vaccines,meaning their messagesabout benefits and
safety of vaccines may not persuade people who lack vaccine
confidence.Furthermore,we found that respondentswho distrust
vaccines are highly health-literate, engaged and independent
health consumers,who havelikely encounteredcommonvaccine-
promotion messages.Communicationsresponding to their con-
cerns should be written for a sophisticatedaudience,and respond
to their nuanced concerns in depth. Finally, the variance in
psychosocialprofiles betweeneach of the three subgroupsfalling
under the ‘vaccinehesitancy’categorysuggeststhat communica-
tion should focus on subgroups,rather than target‘hesitancy’as a
whole. Communicationsneed to be sensitiveto the psychosocial
contextwithin which vaccinebeliefsoccur [18],and the hesitancy
categoryappearsto group distinct psychosocialprofiles together.
Similarly,in measuringattitudes,subgroupscomprisinghesitancy
may be more appropriateunits of measurementthan the category
of hesitancy.
4.4.Conclusion
In assessinghow vaccineattitudes relate to psychosocialand
demographic attributes, we found that Australians holding
negative attitudes to vaccines are more likely to distrust the
government,the healthcare system, and to have conspiratorial
beliefs. They are also more likely to report being informed,
independenthealth consumerswith better-than-averagehealth.
These factors may be important to consider in communicating
about vaccines.
Conflicts of interest
None.
References
[1] Departmentof Health, Further StrengtheningNo Jab, No Pay. 2017 01 May
Availablefrom:, (2017). http://www.health.gov.au/internet/ministers/
publishing.nsf/Content/health-mediarel-yr2017-hunt041.htm.
[2] World Health Organisation,Report of the SAGE Working Group on Vaccine
Hesitancy,(2014) Geneva,Switzerland.
[3] Department of Health, AIR - All Children CoverageData [cited 2017 22
November2017];Availablefrom:, (2017). http://www.immunise.health.gov.
au/internet/immunise/publishing.nsf/Content/all-child-cover-data.htm.
[4] H. Brynley,et al.,Annual ImmunisationCoverageReport2015,NationalCentre
for ImmunisationResearchand Surveillanceof VaccinePreventableDiseases:
The Children’sHospital at Westmeadand University of Sydney,2015.
[5] F.H.Beard,et al.,Trendsand patternsin vaccinationobjection,Australia,2002–
2013,Med. J. Aust. 204 (7) (2016)275, doi:http://dx.doi.org/10.5694/
mja15.01226.
6 T. Rozbrojet al. / PatientEducationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
system.Interestingly,even respondentswho believedall vaccines
should be administered,but had concerns,had lower trust in the
valuesof the healthcaresystemthan those without concerns.The
subscale measured level of agreement on items such as “the
healthcare system:. . . lies to make money”, “experimentson
patientswithout them knowing”,and “coversup its mistakes”[49].
The differencein risk ratios betweenthe two ‘all’ groupsshould be
interpreted with caution, as both scores were calculated in
reference to the ‘most’ category.Nevertheless,the increase in
healthcaresystem distrust associatedwith lower confidencein
vaccines is worrying. HCWs are integral to addressingvaccine
concerns[30,31,68],and this role may be encumberedby patients’
distrust in the healthcaresystem.Distrustof both competenceand
values of the healthcare system among people who distrust
vaccines should be accounted for when responding to vaccine
distrust.
To our knowledge,this studywas the first to assessboth HH and
CAM belief across the spectrum of attitudes. Previous research
linked negativeattitudeswith adherenceto alternativemedicine
in general[30,69–71].Theselinks are supportedby our finding that
negativeattitudeswere associatedwith belief in CAM. But we also
found negativeattitudesto be associatedwith rejectionof HH. This
is interesting,becauseusually belief in HH predictsbelief in CAM
[50,72,73].Studiesfrom other topics showed that, in lieu of belief
in HH, CAM was often chosen due to dissatisfaction with
conventional treatment experiences [74–76]. This explanation
would be plausible for our findings,given that negativeattitudes
were also associatedwith lower trust in the competenceof the
healthcaresystem.It may be worth investigatingthis further in
future research to gain insights into why some people begin
distrusting vaccines.
We found that vaccinerejection relatedto broaderdissatisfac-
tion with governance.On the CMQ, which contains no health-
specific questions [54], negativeattitudes were associatedwith
higher scores, suggesting a higher tendency towards general
conspiracistideation. These findings corroborateanother recent
study showing that antivaccination attitudes are linked to
conspiratorialthinking [23]. Negativeattitudes were also linked
to voting for minor political parties, which supports Larson’s
argument that political views play an important role in vaccine
decisions[21].Previousresearchhas shown links betweenvaccine
rejection and conspiracistviews regarding vaccination [77–79].
Our and other findings[21,23]suggestthat vaccinedistrustmay be
linked to broader anti-establishmentbeliefs.
4.1.3.Implicationsfor taxonomyof vaccineattitudes
Substantialresearcheffortsare beinginvestedinto understand-
ing and addressingvaccine‘hesitancy’[2,18,38–43,80].However,
in our data,the ‘hesitant’categorydoesnot capturea distinct set of
demographic or psychosocial attributes. On most predictor
variables,there is a linear pattern between risk ratios across the
five attitudes,with scores often being most similar between ‘all
unconcerned’ and ‘all concerned, and ‘some’ and ‘none’. Our
researchwas designedto respondto a key aim of the WHO: assess
how the hesitantcategoryrelatesto socioculturalprofiles [2,18].In
responding to this aim, we found it would be better to assess
‘hesitancy’using a more granularset of categories,like thosein the
present study, or other alternatives,like the categoriesused by
Leask and colleagues[14].
4.2.Limitations
This researchhad severallimitations.It was not viableto recruit
a representativesample.Sincevaccinationis refusedby only about
2%of the population [7,25],untargetedrecruitmentof this group
would not be feasible.As noted in the results,some demographic
attributeswere over-represented.But overall,a diversesamplewas
achieved.
The cross-sectionaldesign only enabled us to assessassocia-
tions. Understanding the causal interplay between vaccine
attitudes and demographic and psychosocial attributes would
providefurther understandingof how particularattitudesemerge.
Longitudinal design could be considered for future research to
assess directions of causality between attitudes and broader
attributes.
4.3.Practiceimplications
This researchcontributesto understandingvaccineattitudesin
their socio-culturalcontext,which is useful for improving patient
education and communication about vaccines. Our findings
suggestthat vaccinepromotion,which tends to focus on benefits
and safety of vaccines,should also focus on building trust in the
governmentand healthcaresystem.Both healthcaresystem and
governmentwere distrusted by participants who lacked confi-
dence in vaccines,meaning their messagesabout benefits and
safety of vaccines may not persuade people who lack vaccine
confidence.Furthermore,we found that respondentswho distrust
vaccines are highly health-literate, engaged and independent
health consumers,who havelikely encounteredcommonvaccine-
promotion messages.Communicationsresponding to their con-
cerns should be written for a sophisticatedaudience,and respond
to their nuanced concerns in depth. Finally, the variance in
psychosocialprofiles betweeneach of the three subgroupsfalling
under the ‘vaccinehesitancy’categorysuggeststhat communica-
tion should focus on subgroups,rather than target‘hesitancy’as a
whole. Communicationsneed to be sensitiveto the psychosocial
contextwithin which vaccinebeliefsoccur [18],and the hesitancy
categoryappearsto group distinct psychosocialprofiles together.
Similarly,in measuringattitudes,subgroupscomprisinghesitancy
may be more appropriateunits of measurementthan the category
of hesitancy.
4.4.Conclusion
In assessinghow vaccineattitudes relate to psychosocialand
demographic attributes, we found that Australians holding
negative attitudes to vaccines are more likely to distrust the
government,the healthcare system, and to have conspiratorial
beliefs. They are also more likely to report being informed,
independenthealth consumerswith better-than-averagehealth.
These factors may be important to consider in communicating
about vaccines.
Conflicts of interest
None.
References
[1] Departmentof Health, Further StrengtheningNo Jab, No Pay. 2017 01 May
Availablefrom:, (2017). http://www.health.gov.au/internet/ministers/
publishing.nsf/Content/health-mediarel-yr2017-hunt041.htm.
[2] World Health Organisation,Report of the SAGE Working Group on Vaccine
Hesitancy,(2014) Geneva,Switzerland.
[3] Department of Health, AIR - All Children CoverageData [cited 2017 22
November2017];Availablefrom:, (2017). http://www.immunise.health.gov.
au/internet/immunise/publishing.nsf/Content/all-child-cover-data.htm.
[4] H. Brynley,et al.,Annual ImmunisationCoverageReport2015,NationalCentre
for ImmunisationResearchand Surveillanceof VaccinePreventableDiseases:
The Children’sHospital at Westmeadand University of Sydney,2015.
[5] F.H.Beard,et al.,Trendsand patternsin vaccinationobjection,Australia,2002–
2013,Med. J. Aust. 204 (7) (2016)275, doi:http://dx.doi.org/10.5694/
mja15.01226.
6 T. Rozbrojet al. / PatientEducationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
[6] A. Dey,et al., Summaryof National SurveillanceData on VaccinePreventable
Diseasesin Australia,2008–2011,National Centrefor ImmunisationResearch
and Surveillanceof Vaccine PreventableDiseases:University of Sydney,
2016.
[7] M. Yui Kwan Chow, et al., Parentalattitudes,beliefs,behavioursand concerns
towards childhood vaccinationsin Australia: a national online survey,Aust.
Fam. Phys. 46 (2017)145–151.
[8] H.J. Larson,et al.,The stateof vaccineconfidence2016:globalinsightsthrough
a 67-Countrysurvey,EBioMedicine(2016),doi:http://dx.doi.org/10.1016/j.
ebiom.2016.08.042.
[9] L. Caron-Poulin,et al., Burdenand deathsassociatedwith vaccinepreventable
diseasesin Canada,2010-2014,Online J. Public Health Inform. 9 (1) (2017)
e094, doi:http://dx.doi.org/10.5210/ojphi.v9i1.7676.
[10] Centresfor DiseaseControl and Prevention,Epidemiologyand Preventionof
Vaccine-preventableDiseases:ReportedCasesand DeathsFrom Vaccine
PreventableDiseases,United States[cited 201829th July]; Availablefrom:, (
2018). https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/
appendices/e/reported-cases.pdf.
[11] S. Wicker, H.C. Maltezou, Vaccine-preventablediseasesin Europe: where do
we stand? Expert Rev.Vaccines13 (8) (2014)979–987,doi:http://dx.doi.org/
10.1586/14760584.2014.933077.
[12] O. Yaqub,et al., Attitudes to vaccination:a critical review, Soc. Sci. Med. 112
(2014)1–11,doi:http://dx.doi.org/10.1016/j.socscimed.2014.04.018.
[13] J. Leask, et al., What maintains parental support for vaccination when
challengedby anti-vaccinationmessages?A qualitativestudy,Vaccine24 (49–
50) (2006) 7238–7245,doi:http://dx.doi.org/10.1016/j.vaccine.2006.05.010.
[14] J. Leask,et al., Communicatingwith parentsabout vaccination:a framework
for healthprofessionals,BMC Pediatr.12 (1) (2012)1–11,doi:http://dx.doi.org/
10.1186/1471-2431-12-154.
[15] A. Sadaf, et al., A systematicreview of interventionsfor reducing parental
vaccinerefusaland vaccinehesitancy,Vaccine31 (40) (2013)4293–4304,doi:
http://dx.doi.org/10.1016/j.vaccine.2013.07.013.
[16] E. Dubé, D. Gagnon,N.E. MacDonald,Strategiesintended to addressvaccine
hesitancy:review of published reviews,Vaccine33 (34) (2015) 4191–4203,
doi:http://dx.doi.org/10.1016/j.vaccine.2015.04.041.
[17] C. Jarrett, et al., Strategiesfor addressingvaccine hesitancy– a systematic
review, Vaccine 33 (34) (2015)4180–4190,doi:http://dx.doi.org/10.1016/j.
vaccine.2015.04.040.
[18] World Health Organisation,Strategiesfor AddressingVaccine Hesitancy: a
SystematicReview,(2014) Geneva,Switzerland.
[19] P.R. Ward, et al., Understanding the perceived logic of care by vaccine-
hesitant and vaccine-refusingparents: a qualitativestudy in Australia,PLoS
ONE 12 (10) (2017),doi:http://dx.doi.org/10.1371/journal.pone.0185955
e0185955.
[20] J.C. Bester,Vaccinerefusaland trust: the troublewith coercionand education
and suggestionsfor a cure,J. Bioeth.Inq. 12 (4) (2015)555–559,doi:http://dx.
doi.org/10.1007/s11673-015-9673-1.
[21] H.J. Larson,Politics and Public Trust ShapeVaccineRisk Perceptions,Nat.Hum.
Behav.(2018),doi:http://dx.doi.org/10.1038/s41562-018-0331-6.
[22] G.S. Mesch, K.P. Schwirian, Social and political determinants of vaccine
hesitancy:lessonslearned from the H1N1 pandemicof 2009-2010,Am. J.
Infect. Control 43 (11) (2015)1161–1165,doi:http://dx.doi.org/10.1016/j.
ajic.2015.06.031.
[23] M.J. Hornsey, E.A. Harris, K.S. Fielding, The psychological roots of anti-
vaccinationattitudes:a 24-nationinvestigation,Health Psychol.37 (4) (2018)
307–315,doi:http://dx.doi.org/10.1037/hea0000586.
[24] P. Corben,J. Leask,To closethe childhood immunisationgap,we needa richer
understandingof parents’decision-making,Hum. Vaccin.Immunother.
(2016),doi:http://dx.doi.org/10.1080/21645515.2016.122155300-00.
[25] S. Pemberton, 50% Of Australians Who Oppose Vaccination Get Their
Information From the Internet.2013 23 May [cited 201718 December];
Availablefrom:, (2013). http://www.scienceinpublic.com.au/media-releases/
vaccinationsurvey.
[26] Australian Institute of Family Studies,The Longitudinal Study of Australian
Children Annual StatisticalReport 2015,AIFS, Melbourne, Australia,2016.
[27] J. Costa-Pinto,et al.,ParentalImmunisationNeedsand Attitudes(PINA) Survey
of ParentsAttending GeneralPaediatricClinics in a TertiaryPaediatric
Hospital, and Community Maternal Child Health Centresin Melbourne,
Australia,Royal AustralianCollegeof PhysiciansCongress,RACP: Adelaide
ConventionCentre,2016.
[28] H.J. Larson,Vaccine trust and the limits of information, Science353 (6305)
(2016)1207,doi:http://dx.doi.org/10.1126/science.aah6190.
[29] P. Paterson,et al., Vaccinehesitancyand healthcareproviders,Vaccine34 (52)
(2016)6700–6706,doi:http://dx.doi.org/10.1016/j.vaccine.2016.10.042.
[30] G.L. Freed, et al., Sources and perceived credibility of vaccine-safety
information for parents,Pediatrics127 (Supplement1) (2011)S107,doi:
http://dx.doi.org/10.1542/peds.2010-1722P.
[31] D.J. Opel, et al., The influence of provider communication behaviors on
parentalvaccineacceptanceand visit experience,Am. J. Public Health 105(10)
(2015)1998–2004,doi:http://dx.doi.org/10.2105/ajph.2014.302425.
[32] I.A. Harmsen, et al., Parental information-seekingbehaviour in childhood
vaccinations,BMC Public Health 13 (1) (2013)1–10, doi:http://dx.doi.org/
10.1186/1471-2458-13-1219.
[33] N.J. Berry, et al., When parents won’t vaccinatetheir children: a qualitative
investigationof australianprimary care providers’experiences,BMC Pediatr.
17 (2017)19, doi:http://dx.doi.org/10.1186/s12887-017-0783-2.
[34] C. Lee,et al., Hurdles to herd immunity: Distrust of governmentand vaccine
refusal in the US, 2002-2003,Vaccine34 (34) (2016)3972–3978.http://
10.1016/j.vaccine.2016.06.048.
[35] J.A. Cassell,et al., Is the cultural contextof MMR rejectiona key to an effective
public health discourse?Public Health 120 (9) (2006) 783–794,doi:http://dx.
doi.org/10.1016/j.puhe.2006.03.011.
[36] Mark Navin, Values and Vaccine Refusal: Hard Questions in Ethics,
Epistemology,and Health Care,Taylor & Francis Ltd, Great Britain, 2015,
doi:http://dx.doi.org/10.4324/9781315764078.
[37] J.A. Reich, Neoliberal mothering and vaccine refusal: imagined gated
communitiesand the privilege of choice,Gend. Soc. (2014),doi:http://dx.
doi.org/10.1177/0891243214532711.
[38] E. Dubé,et al.,Vaccinehesitancy:an overview,Hum. Vaccin.Immunother.9 (8)
(2013)1763–1773,doi:http://dx.doi.org/10.4161/hv.24657.
[39] J. Eskola,et al., How to deal with vaccinehesitancy?Vaccine33 (34) (2015)
4215–4217,doi:http://dx.doi.org/10.1016/j.vaccine.2015.04.043.
[40] N.E. MacDonald, Vaccine hesitancy: definition, scope and determinants,
Vaccine 33 (34) (2015)4161–4164,doi:http://dx.doi.org/10.1016/j.
vaccine.2015.04.036.
[41] E. Dubé,et al., Mapping vaccinehesitancy—country-specificcharacteristicsof
a global phenomenon,Vaccine32 (49) (2014)6649–6654,doi:http://dx.doi.
org/10.1016/j.vaccine.2014.09.039.
[42] H.J. Larson,et al., Measuringvaccinehesitancy:the developmentof a survey
tool, Vaccine 33 (34) (2015)4165–4175,doi:http://dx.doi.org/10.1016/j.
vaccine.2015.04.037.
[43] P. Peretti-Watel,et al., Vaccinehesitancy:clarifying a theoreticalframework
for an ambiguousnotion, PLoS Curr. 7 (2015),doi:http://dx.doi.org/10.1371/
currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289.
[44] M.A. Coniglio,et al., Parents’attitudesand behaviourstowardsrecommended
vaccinationsin Sicily,Italy,BMC Public Health 11 (1) (2011)1–6, doi:http://dx.
doi.org/10.1186/1471-2458-11-305.
[45] A. Kennedy,M. Basket,K. Sheedy,Vaccineattitudes,concerns,and information
sourcesreportedby parentsof young children: results from the 2009
HealthStylessurvey,Pediatrics127 (Supplement1) (2011)92–99, doi:http://
dx.doi.org/10.1542/peds.2010-1722N.
[46] D.J. Opel, et al., The relationship between parent attitudesabout childhood
vaccinessurvey scoresand future child immunization status: a validation
study,JAMA Pediatr.167(11)(2013)1065–1071,doi:http://dx.doi.org/10.1001/
jamapediatrics.2013.2483.
[47] Z. Horne,et al., Counteringantivaccinationattitudes,Proc.Natl. Acad.Sci. U. S.
A. 112 (33) (2015)10321–10324,doi:http://dx.doi.org/10.1073/
pnas.1504019112.
[48] K.B. DeSalvo,et al., Assessingmeasurementproperties of two single-item
generalhealth measures,Qual. Life Res.15 (2) (2006) 191–201,doi:http://dx.
doi.org/10.1007/s11136-005-0887-2.
[49] J.A. Shea,et al., Developmentof a revisedhealth care systemdistrust scale,J.
Gen. Intern. Med. 23 (6) (2008) 727–732,doi:http://dx.doi.org/10.1007/
s11606-008-0575-3.
[50] M.E. Hyland, G.T.Lewith, C. Westoby,Developinga measureof attitudes:the
holistic complementaryand alternativemedicinequestionnaire,Complement.
Ther.Med. 11(1) (2003) 33–38,doi:http://dx.doi.org/10.1016/S0965-2299(02)
00113-9.
[51] M. Dandavino,et al., Developmentand validation of a self-efficacyscale for
clinical decision-makingin generalpaediatrics,Paediatr.Child Health 18 (4)
(2013)184–188,doi:http://dx.doi.org/10.1093/pch/18.4.184.
[52] D.E.Brashers,S.M. Haas,J.L. Neidig,Thepatientself-advocacyscale:measuring
patient involvementin health care decision-makinginteractions,Health
Commun.11 (2) (1999) 97–121,doi:http://dx.doi.org/10.1207/
s15327027hc1102_1.
[53] C. Doherty,et al., Broad Distrust: How Americans View Their Government.
Broad Criticism, but Positive PerformanceRatingsin Many Areas,Pew
ResearchCenter,United States,2012.
[54] M. Bruder, et al., Measuring individual differences in generic beliefs in
conspiracytheories acrosscultures: conspiracymentality questionnaire,
Front. Psychol.4 (2013)225, doi:http://dx.doi.org/10.3389/fpsyg.2013.00225.
[55] A.Bo.Statistics,3235.0- Populationby Age and Sex,Regionsof Australia,2016
[cited 201812 january]; Availablefrom:, (2016). http://www.abs.gov.au/
ausstats/abs@.nsf/mf/3235.0.
[56] AustralianBureauof Statistics,1301.0- YearBook Australia,2012:Educational
Attainment[cited 201812 January];Availablefrom:, (2011). http://www.abs.
gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/1301.02012Main%
20FeaturesEducational%20attainment110.
[57] M.H. Danchin,et al.,Vaccinedecision-makingbeginsin pregnancy:correlation
betweenvaccineconcerns,intentions and maternalvaccinationwith
subsequentchildhood vaccineuptake,Vaccine(2017),doi:http://dx.doi.org/
10.1016/j.vaccine.2017.08.003.
[58] A.L. Benin, et al., Qualitative analysis of mothers’ decision-making about
vaccinesfor infants: the importanceof trust, Pediatrics117(5) (2006) 1532,
doi:http://dx.doi.org/10.1542/peds.2005-1728.
[59] J.M. Glanz,et al., A mixed methodsstudy of parentalvaccinedecisionmaking
and parent-providertrust,Acad.Pediatr.13 (5) (2013)481–488,doi:http://dx.
doi.org/10.1016/j.acap.2013.05.030.
[60] TruvenHealth Analytics,NPR Health Poll: Vaccinations,(2015) United States
of America.
[61] NationalHealth PerformanceAuthority,HealthyCommunities:Immunisation
Ratesfor Children in 2014–15,NHPA, Australia,2016.
T. Rozbrojet al./ PatientEducationand Counselingxxx (2018)xxx–xxx 7
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
Diseasesin Australia,2008–2011,National Centrefor ImmunisationResearch
and Surveillanceof Vaccine PreventableDiseases:University of Sydney,
2016.
[7] M. Yui Kwan Chow, et al., Parentalattitudes,beliefs,behavioursand concerns
towards childhood vaccinationsin Australia: a national online survey,Aust.
Fam. Phys. 46 (2017)145–151.
[8] H.J. Larson,et al.,The stateof vaccineconfidence2016:globalinsightsthrough
a 67-Countrysurvey,EBioMedicine(2016),doi:http://dx.doi.org/10.1016/j.
ebiom.2016.08.042.
[9] L. Caron-Poulin,et al., Burdenand deathsassociatedwith vaccinepreventable
diseasesin Canada,2010-2014,Online J. Public Health Inform. 9 (1) (2017)
e094, doi:http://dx.doi.org/10.5210/ojphi.v9i1.7676.
[10] Centresfor DiseaseControl and Prevention,Epidemiologyand Preventionof
Vaccine-preventableDiseases:ReportedCasesand DeathsFrom Vaccine
PreventableDiseases,United States[cited 201829th July]; Availablefrom:, (
2018). https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/
appendices/e/reported-cases.pdf.
[11] S. Wicker, H.C. Maltezou, Vaccine-preventablediseasesin Europe: where do
we stand? Expert Rev.Vaccines13 (8) (2014)979–987,doi:http://dx.doi.org/
10.1586/14760584.2014.933077.
[12] O. Yaqub,et al., Attitudes to vaccination:a critical review, Soc. Sci. Med. 112
(2014)1–11,doi:http://dx.doi.org/10.1016/j.socscimed.2014.04.018.
[13] J. Leask, et al., What maintains parental support for vaccination when
challengedby anti-vaccinationmessages?A qualitativestudy,Vaccine24 (49–
50) (2006) 7238–7245,doi:http://dx.doi.org/10.1016/j.vaccine.2006.05.010.
[14] J. Leask,et al., Communicatingwith parentsabout vaccination:a framework
for healthprofessionals,BMC Pediatr.12 (1) (2012)1–11,doi:http://dx.doi.org/
10.1186/1471-2431-12-154.
[15] A. Sadaf, et al., A systematicreview of interventionsfor reducing parental
vaccinerefusaland vaccinehesitancy,Vaccine31 (40) (2013)4293–4304,doi:
http://dx.doi.org/10.1016/j.vaccine.2013.07.013.
[16] E. Dubé, D. Gagnon,N.E. MacDonald,Strategiesintended to addressvaccine
hesitancy:review of published reviews,Vaccine33 (34) (2015) 4191–4203,
doi:http://dx.doi.org/10.1016/j.vaccine.2015.04.041.
[17] C. Jarrett, et al., Strategiesfor addressingvaccine hesitancy– a systematic
review, Vaccine 33 (34) (2015)4180–4190,doi:http://dx.doi.org/10.1016/j.
vaccine.2015.04.040.
[18] World Health Organisation,Strategiesfor AddressingVaccine Hesitancy: a
SystematicReview,(2014) Geneva,Switzerland.
[19] P.R. Ward, et al., Understanding the perceived logic of care by vaccine-
hesitant and vaccine-refusingparents: a qualitativestudy in Australia,PLoS
ONE 12 (10) (2017),doi:http://dx.doi.org/10.1371/journal.pone.0185955
e0185955.
[20] J.C. Bester,Vaccinerefusaland trust: the troublewith coercionand education
and suggestionsfor a cure,J. Bioeth.Inq. 12 (4) (2015)555–559,doi:http://dx.
doi.org/10.1007/s11673-015-9673-1.
[21] H.J. Larson,Politics and Public Trust ShapeVaccineRisk Perceptions,Nat.Hum.
Behav.(2018),doi:http://dx.doi.org/10.1038/s41562-018-0331-6.
[22] G.S. Mesch, K.P. Schwirian, Social and political determinants of vaccine
hesitancy:lessonslearned from the H1N1 pandemicof 2009-2010,Am. J.
Infect. Control 43 (11) (2015)1161–1165,doi:http://dx.doi.org/10.1016/j.
ajic.2015.06.031.
[23] M.J. Hornsey, E.A. Harris, K.S. Fielding, The psychological roots of anti-
vaccinationattitudes:a 24-nationinvestigation,Health Psychol.37 (4) (2018)
307–315,doi:http://dx.doi.org/10.1037/hea0000586.
[24] P. Corben,J. Leask,To closethe childhood immunisationgap,we needa richer
understandingof parents’decision-making,Hum. Vaccin.Immunother.
(2016),doi:http://dx.doi.org/10.1080/21645515.2016.122155300-00.
[25] S. Pemberton, 50% Of Australians Who Oppose Vaccination Get Their
Information From the Internet.2013 23 May [cited 201718 December];
Availablefrom:, (2013). http://www.scienceinpublic.com.au/media-releases/
vaccinationsurvey.
[26] Australian Institute of Family Studies,The Longitudinal Study of Australian
Children Annual StatisticalReport 2015,AIFS, Melbourne, Australia,2016.
[27] J. Costa-Pinto,et al.,ParentalImmunisationNeedsand Attitudes(PINA) Survey
of ParentsAttending GeneralPaediatricClinics in a TertiaryPaediatric
Hospital, and Community Maternal Child Health Centresin Melbourne,
Australia,Royal AustralianCollegeof PhysiciansCongress,RACP: Adelaide
ConventionCentre,2016.
[28] H.J. Larson,Vaccine trust and the limits of information, Science353 (6305)
(2016)1207,doi:http://dx.doi.org/10.1126/science.aah6190.
[29] P. Paterson,et al., Vaccinehesitancyand healthcareproviders,Vaccine34 (52)
(2016)6700–6706,doi:http://dx.doi.org/10.1016/j.vaccine.2016.10.042.
[30] G.L. Freed, et al., Sources and perceived credibility of vaccine-safety
information for parents,Pediatrics127 (Supplement1) (2011)S107,doi:
http://dx.doi.org/10.1542/peds.2010-1722P.
[31] D.J. Opel, et al., The influence of provider communication behaviors on
parentalvaccineacceptanceand visit experience,Am. J. Public Health 105(10)
(2015)1998–2004,doi:http://dx.doi.org/10.2105/ajph.2014.302425.
[32] I.A. Harmsen, et al., Parental information-seekingbehaviour in childhood
vaccinations,BMC Public Health 13 (1) (2013)1–10, doi:http://dx.doi.org/
10.1186/1471-2458-13-1219.
[33] N.J. Berry, et al., When parents won’t vaccinatetheir children: a qualitative
investigationof australianprimary care providers’experiences,BMC Pediatr.
17 (2017)19, doi:http://dx.doi.org/10.1186/s12887-017-0783-2.
[34] C. Lee,et al., Hurdles to herd immunity: Distrust of governmentand vaccine
refusal in the US, 2002-2003,Vaccine34 (34) (2016)3972–3978.http://
10.1016/j.vaccine.2016.06.048.
[35] J.A. Cassell,et al., Is the cultural contextof MMR rejectiona key to an effective
public health discourse?Public Health 120 (9) (2006) 783–794,doi:http://dx.
doi.org/10.1016/j.puhe.2006.03.011.
[36] Mark Navin, Values and Vaccine Refusal: Hard Questions in Ethics,
Epistemology,and Health Care,Taylor & Francis Ltd, Great Britain, 2015,
doi:http://dx.doi.org/10.4324/9781315764078.
[37] J.A. Reich, Neoliberal mothering and vaccine refusal: imagined gated
communitiesand the privilege of choice,Gend. Soc. (2014),doi:http://dx.
doi.org/10.1177/0891243214532711.
[38] E. Dubé,et al.,Vaccinehesitancy:an overview,Hum. Vaccin.Immunother.9 (8)
(2013)1763–1773,doi:http://dx.doi.org/10.4161/hv.24657.
[39] J. Eskola,et al., How to deal with vaccinehesitancy?Vaccine33 (34) (2015)
4215–4217,doi:http://dx.doi.org/10.1016/j.vaccine.2015.04.043.
[40] N.E. MacDonald, Vaccine hesitancy: definition, scope and determinants,
Vaccine 33 (34) (2015)4161–4164,doi:http://dx.doi.org/10.1016/j.
vaccine.2015.04.036.
[41] E. Dubé,et al., Mapping vaccinehesitancy—country-specificcharacteristicsof
a global phenomenon,Vaccine32 (49) (2014)6649–6654,doi:http://dx.doi.
org/10.1016/j.vaccine.2014.09.039.
[42] H.J. Larson,et al., Measuringvaccinehesitancy:the developmentof a survey
tool, Vaccine 33 (34) (2015)4165–4175,doi:http://dx.doi.org/10.1016/j.
vaccine.2015.04.037.
[43] P. Peretti-Watel,et al., Vaccinehesitancy:clarifying a theoreticalframework
for an ambiguousnotion, PLoS Curr. 7 (2015),doi:http://dx.doi.org/10.1371/
currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289.
[44] M.A. Coniglio,et al., Parents’attitudesand behaviourstowardsrecommended
vaccinationsin Sicily,Italy,BMC Public Health 11 (1) (2011)1–6, doi:http://dx.
doi.org/10.1186/1471-2458-11-305.
[45] A. Kennedy,M. Basket,K. Sheedy,Vaccineattitudes,concerns,and information
sourcesreportedby parentsof young children: results from the 2009
HealthStylessurvey,Pediatrics127 (Supplement1) (2011)92–99, doi:http://
dx.doi.org/10.1542/peds.2010-1722N.
[46] D.J. Opel, et al., The relationship between parent attitudesabout childhood
vaccinessurvey scoresand future child immunization status: a validation
study,JAMA Pediatr.167(11)(2013)1065–1071,doi:http://dx.doi.org/10.1001/
jamapediatrics.2013.2483.
[47] Z. Horne,et al., Counteringantivaccinationattitudes,Proc.Natl. Acad.Sci. U. S.
A. 112 (33) (2015)10321–10324,doi:http://dx.doi.org/10.1073/
pnas.1504019112.
[48] K.B. DeSalvo,et al., Assessingmeasurementproperties of two single-item
generalhealth measures,Qual. Life Res.15 (2) (2006) 191–201,doi:http://dx.
doi.org/10.1007/s11136-005-0887-2.
[49] J.A. Shea,et al., Developmentof a revisedhealth care systemdistrust scale,J.
Gen. Intern. Med. 23 (6) (2008) 727–732,doi:http://dx.doi.org/10.1007/
s11606-008-0575-3.
[50] M.E. Hyland, G.T.Lewith, C. Westoby,Developinga measureof attitudes:the
holistic complementaryand alternativemedicinequestionnaire,Complement.
Ther.Med. 11(1) (2003) 33–38,doi:http://dx.doi.org/10.1016/S0965-2299(02)
00113-9.
[51] M. Dandavino,et al., Developmentand validation of a self-efficacyscale for
clinical decision-makingin generalpaediatrics,Paediatr.Child Health 18 (4)
(2013)184–188,doi:http://dx.doi.org/10.1093/pch/18.4.184.
[52] D.E.Brashers,S.M. Haas,J.L. Neidig,Thepatientself-advocacyscale:measuring
patient involvementin health care decision-makinginteractions,Health
Commun.11 (2) (1999) 97–121,doi:http://dx.doi.org/10.1207/
s15327027hc1102_1.
[53] C. Doherty,et al., Broad Distrust: How Americans View Their Government.
Broad Criticism, but Positive PerformanceRatingsin Many Areas,Pew
ResearchCenter,United States,2012.
[54] M. Bruder, et al., Measuring individual differences in generic beliefs in
conspiracytheories acrosscultures: conspiracymentality questionnaire,
Front. Psychol.4 (2013)225, doi:http://dx.doi.org/10.3389/fpsyg.2013.00225.
[55] A.Bo.Statistics,3235.0- Populationby Age and Sex,Regionsof Australia,2016
[cited 201812 january]; Availablefrom:, (2016). http://www.abs.gov.au/
ausstats/abs@.nsf/mf/3235.0.
[56] AustralianBureauof Statistics,1301.0- YearBook Australia,2012:Educational
Attainment[cited 201812 January];Availablefrom:, (2011). http://www.abs.
gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/1301.02012Main%
20FeaturesEducational%20attainment110.
[57] M.H. Danchin,et al.,Vaccinedecision-makingbeginsin pregnancy:correlation
betweenvaccineconcerns,intentions and maternalvaccinationwith
subsequentchildhood vaccineuptake,Vaccine(2017),doi:http://dx.doi.org/
10.1016/j.vaccine.2017.08.003.
[58] A.L. Benin, et al., Qualitative analysis of mothers’ decision-making about
vaccinesfor infants: the importanceof trust, Pediatrics117(5) (2006) 1532,
doi:http://dx.doi.org/10.1542/peds.2005-1728.
[59] J.M. Glanz,et al., A mixed methodsstudy of parentalvaccinedecisionmaking
and parent-providertrust,Acad.Pediatr.13 (5) (2013)481–488,doi:http://dx.
doi.org/10.1016/j.acap.2013.05.030.
[60] TruvenHealth Analytics,NPR Health Poll: Vaccinations,(2015) United States
of America.
[61] NationalHealth PerformanceAuthority,HealthyCommunities:Immunisation
Ratesfor Children in 2014–15,NHPA, Australia,2016.
T. Rozbrojet al./ PatientEducationand Counselingxxx (2018)xxx–xxx 7
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
[62] L. Carroll, Rich SuburbsHave Low ImmunisationRates,ResearchShows,The
SydneyMorning Herald, Fairfax Media, 2014.
[63] Marissa Calligeros,Melbourne’santi-vaccinationhot spots: rich suburbshave
low immunisationrates,The Age, Fairfax Media, Melbourne, 2015.
[64] SarahMartin, Child vaccinecampaigntargetswealthy,The Australian,News
Corp Australia,Sydney,2016.
[65] H.J. Larson, et al., Understanding vaccine hesitancy around vaccines and
vaccinationfrom a global perspective:A systematicreview of published
literature,2007–2012,Vaccine32 (19) (2014)2150–2159,doi:http://dx.doi.
org/10.1016/j.vaccine.2014.01.081.
[66] C.R. MacIntyre,D. Salmon,Want to boost vaccination?Don’t punish parents,
build their trust, The Conversation,(2015) Australia.
[67] P. Stefanoff,et al., Trackingparentalattitudeson vaccinationacrossEuropean
countries: the vaccinesafety,attitudes,training and communicationproject
(VACSATC),Vaccine28 (35) (2010)5731–5737,doi:http://dx.doi.org/10.1016/j.
vaccine.2010.06.009.
[68] EuropeanCentrefor DiseasePreventionand Control,Rapid LiteratureReview
on Motivating Hesitant Population Groups in Europe to Vaccinate,(2015)
Stockholm,Sweden.
[69] G.L. Freed,et al., Parentalvaccinesafetyconcernsin 2009, Pediatrics(2010),
doi:http://dx.doi.org/10.1542/peds.2009-1962.
[70] E. Ernst, Rise in popularity of complementaryand alternative medicine:
reasonsand consequencesfor vaccination,Vaccine20 (Supplement1) (2001)
S90–S93,doi:http://dx.doi.org/10.1016/S0264-410X(01)00290-0.
[71] S. Blume,Anti-vaccinationmovementsand their interpretations,Soc.Sci.Med.
62 (3) (2006) 628–642,doi:http://dx.doi.org/10.1016/j.
socscimed.2005.06.020.
[72] M. Siahpush,Why do people favouralternativemedicine?Aust. N. Z. J. Public
Health 23 (3) (1999)266–271,doi:http://dx.doi.org/10.1111/j.1467-842X.1999.
tb01254.x.
[73] J.A. Astin, Why patientsuse alternativemedicine: results of a national study,
JAMA 279 (19) (1998) 1548–1553,doi:http://dx.doi.org/10.1001/
jama.279.19.1548.
[74] A. Furnham,C.Smith,Choosingalternativemedicine:a comparisonof the beliefs
of patientsvisitinga generalpractitioneranda homoeopath,Soc.Sci.Med. 26 (7)
(1988)685–689,doi:http://dx.doi.org/10.1016/0277-9536(88)90060-3.
[75] A. Furnham,R. Bhagrath,A comparisonof health beliefs and behavioursof
clients of orthodoxand complementarymedicine,Br. J. Clin. Psychol.32 (Pt 2)
(1993) 237–246,doi:http://dx.doi.org/10.1111/j.2044-8260.1993.tb01051.x.
[76] C. Vincent,A. Furnham,Why do patientsturn to complementarymedicine?An
empirical study,Br. J. Clin. Psychol.35 (Pt 1) (1996) 37–48, doi:http://dx.doi.
org/10.1111/j.2044-8260.1996.tb01160.x.
[77] G.K. Shapiro, et al., Validation of the vaccine conspiracy beliefs scale,
PapillomavirusRes. (2) (2016)167–172,doi:http://dx.doi.org/10.1016/j.
pvr.2016.09.001.
[78] A. Kata, Anti-vaccineactivists,Web 2.0, and the postmodernparadigm– An
overviewof tacticsand tropesused online by the anti-vaccinationmovement,
Vaccine30 (25) (2012) 3778–3789,doi:http://dx.doi.org/10.1016/j.
vaccine.2011.11.112.
[79] D. Jolley, K.M. Douglas,The effects of anti-vaccine conspiracy theories on
vaccinationintentions,PLoS ONE 9 (2) (2014)e89177,doi:http://dx.doi.org/
10.1371/journal.pone.0089177.
[80] M. Schuster,J. Eskola,P. Duclos,Review of vaccinehesitancy:rationale,remit
and methods,Vaccine 33 (34) (2015)4157–4160,doi:http://dx.doi.org/
10.1016/j.vaccine.2015.04.035.
8 T. Rozbrojet al. / PatientEducationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
SydneyMorning Herald, Fairfax Media, 2014.
[63] Marissa Calligeros,Melbourne’santi-vaccinationhot spots: rich suburbshave
low immunisationrates,The Age, Fairfax Media, Melbourne, 2015.
[64] SarahMartin, Child vaccinecampaigntargetswealthy,The Australian,News
Corp Australia,Sydney,2016.
[65] H.J. Larson, et al., Understanding vaccine hesitancy around vaccines and
vaccinationfrom a global perspective:A systematicreview of published
literature,2007–2012,Vaccine32 (19) (2014)2150–2159,doi:http://dx.doi.
org/10.1016/j.vaccine.2014.01.081.
[66] C.R. MacIntyre,D. Salmon,Want to boost vaccination?Don’t punish parents,
build their trust, The Conversation,(2015) Australia.
[67] P. Stefanoff,et al., Trackingparentalattitudeson vaccinationacrossEuropean
countries: the vaccinesafety,attitudes,training and communicationproject
(VACSATC),Vaccine28 (35) (2010)5731–5737,doi:http://dx.doi.org/10.1016/j.
vaccine.2010.06.009.
[68] EuropeanCentrefor DiseasePreventionand Control,Rapid LiteratureReview
on Motivating Hesitant Population Groups in Europe to Vaccinate,(2015)
Stockholm,Sweden.
[69] G.L. Freed,et al., Parentalvaccinesafetyconcernsin 2009, Pediatrics(2010),
doi:http://dx.doi.org/10.1542/peds.2009-1962.
[70] E. Ernst, Rise in popularity of complementaryand alternative medicine:
reasonsand consequencesfor vaccination,Vaccine20 (Supplement1) (2001)
S90–S93,doi:http://dx.doi.org/10.1016/S0264-410X(01)00290-0.
[71] S. Blume,Anti-vaccinationmovementsand their interpretations,Soc.Sci.Med.
62 (3) (2006) 628–642,doi:http://dx.doi.org/10.1016/j.
socscimed.2005.06.020.
[72] M. Siahpush,Why do people favouralternativemedicine?Aust. N. Z. J. Public
Health 23 (3) (1999)266–271,doi:http://dx.doi.org/10.1111/j.1467-842X.1999.
tb01254.x.
[73] J.A. Astin, Why patientsuse alternativemedicine: results of a national study,
JAMA 279 (19) (1998) 1548–1553,doi:http://dx.doi.org/10.1001/
jama.279.19.1548.
[74] A. Furnham,C.Smith,Choosingalternativemedicine:a comparisonof the beliefs
of patientsvisitinga generalpractitioneranda homoeopath,Soc.Sci.Med. 26 (7)
(1988)685–689,doi:http://dx.doi.org/10.1016/0277-9536(88)90060-3.
[75] A. Furnham,R. Bhagrath,A comparisonof health beliefs and behavioursof
clients of orthodoxand complementarymedicine,Br. J. Clin. Psychol.32 (Pt 2)
(1993) 237–246,doi:http://dx.doi.org/10.1111/j.2044-8260.1993.tb01051.x.
[76] C. Vincent,A. Furnham,Why do patientsturn to complementarymedicine?An
empirical study,Br. J. Clin. Psychol.35 (Pt 1) (1996) 37–48, doi:http://dx.doi.
org/10.1111/j.2044-8260.1996.tb01160.x.
[77] G.K. Shapiro, et al., Validation of the vaccine conspiracy beliefs scale,
PapillomavirusRes. (2) (2016)167–172,doi:http://dx.doi.org/10.1016/j.
pvr.2016.09.001.
[78] A. Kata, Anti-vaccineactivists,Web 2.0, and the postmodernparadigm– An
overviewof tacticsand tropesused online by the anti-vaccinationmovement,
Vaccine30 (25) (2012) 3778–3789,doi:http://dx.doi.org/10.1016/j.
vaccine.2011.11.112.
[79] D. Jolley, K.M. Douglas,The effects of anti-vaccine conspiracy theories on
vaccinationintentions,PLoS ONE 9 (2) (2014)e89177,doi:http://dx.doi.org/
10.1371/journal.pone.0089177.
[80] M. Schuster,J. Eskola,P. Duclos,Review of vaccinehesitancy:rationale,remit
and methods,Vaccine 33 (34) (2015)4157–4160,doi:http://dx.doi.org/
10.1016/j.vaccine.2015.04.035.
8 T. Rozbrojet al. / PatientEducationand Counselingxxx (2018)xxx–xxx
G Model
PEC 6049No. of Pages8
Pleasecite this article in press as: T. Rozbroj, et al., Psychosocialand demographiccharacteristicsrelating to vaccineattitudes in Australia,
Patient Educ Couns (2018),https://doi.org/10.1016/j.pec.2018.08.027
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.