Exploring the Relationship Between PTSD and Dissociative Disorders
VerifiedAdded on 2022/08/16
|5
|1921
|13
Report
AI Summary
This report provides a comprehensive overview of the comorbidity between Posttraumatic Stress Disorder (PTSD) and Dissociative Disorders (DD). It synthesizes findings from numerous studies, highlighting the high risk of suicidal thoughts and other comorbid disorders among individuals suffering from both conditions. The report details the clinical relevance of dissociative symptoms in PTSD and their links to anxiety, depression, and other mental health conditions such as obsessive-compulsive disorder (OCD), borderline personality disorder (BPD), eating disorders (ED), panic disorder (PD), and major depressive disorder (MDD). Several studies are cited to illustrate the prevalence of comorbid personality disorders, particularly BPD, in both D-PTSD and ND-PTSD groups. The report also discusses the high rates of DDs and comorbid DDs among patients with dissociative PTSD and epilepsy. Furthermore, the report examines the relationship between dissociative depression, suicidal attempts, and the impact of ADHD and disruptive behavior disorders. The report concludes by emphasizing the need for further research to break the cycle of dissociative episodes and improve mental health outcomes for individuals affected by these complex conditions. The report uses a wide range of research papers to support the findings.
Many studies suggest that individuals suffering from Posttraumatic Stress Disorder
(PTSD) are at high risk of developing Dissociative Disorder (DD). These people are at higher
risk of developing suicidal thoughts as well as other comorbid disorders. Dissociative
symptoms as identified in PTSD contain high amount of clinical relevance and is linked to
anxiety and depression in obsessive-compulsive disorder (OCD), borderline personality
disorder (BPD), eating disorder (ED), panic disorder (PD), major depressive disorder (MDD),
maladaptive functioning, and quite significantly the history of suicidal thoughts or efforts
(Lyssenko, L., Schmahl, C., Bockhacker, L., Vonderlin, R., Bohus, M., & Kleindienst, N.
(2018); Pick, S., Mellers, J. D. C., & Goldstein, L. H. (2017); Soffer-Dudek, N. (2014);
Yılmaz, E. B. (2019); Bozkurt, H., DuzmanMutluer, T., Kose, C., & Zoroglu, S. (2015). This
study also focuses on factors that may intensify the suicidal thoughts and attempts of a
person.
Another study conducted by Swart, S., Wildschut, M., Draijer, N., Langeland, W., &
Smit, J. H. (2019) suggests that this group primarily had patients with a (comorbid)
personality disorder (88%). BPD was found the most relevant amongst both the ND-PTSD
group and the D-PTSD group (40% and 38%, respectively), followed by personality disorder
(PD-NOS; 64% and 62%, respectively). The use of the depersonalization/derealisation
subscale indicated that more than half of the dissociative PTSD patients (54%) were found to
have met the criteria for DDs. Additionally, 66% did have a comorbid DD (Swart, S.,
Wildschut, M., Draijer, N., Langeland, W., & Smit, J. H., 2019). As much as 67% of the
epileptic patients with Dissociative Symptoms could meet the formal criteria used in the
diagnosis of PTSD (Pick, S., Mellers, J. D. C., & Goldstein, L.H., 2017). Another study by
Swart, S., Wildschut, M., Draijer, N., Langeland, W., & Smith, J. H., (2019) could identify
that 86% of the patients in the Dissociative PTSD (D-PTSD) group had a (comorbid)
personality disorder. In a study of (Lyssenko, L., Schmahl, C., Bockhacker, L., Vonderlin, R.,
(PTSD) are at high risk of developing Dissociative Disorder (DD). These people are at higher
risk of developing suicidal thoughts as well as other comorbid disorders. Dissociative
symptoms as identified in PTSD contain high amount of clinical relevance and is linked to
anxiety and depression in obsessive-compulsive disorder (OCD), borderline personality
disorder (BPD), eating disorder (ED), panic disorder (PD), major depressive disorder (MDD),
maladaptive functioning, and quite significantly the history of suicidal thoughts or efforts
(Lyssenko, L., Schmahl, C., Bockhacker, L., Vonderlin, R., Bohus, M., & Kleindienst, N.
(2018); Pick, S., Mellers, J. D. C., & Goldstein, L. H. (2017); Soffer-Dudek, N. (2014);
Yılmaz, E. B. (2019); Bozkurt, H., DuzmanMutluer, T., Kose, C., & Zoroglu, S. (2015). This
study also focuses on factors that may intensify the suicidal thoughts and attempts of a
person.
Another study conducted by Swart, S., Wildschut, M., Draijer, N., Langeland, W., &
Smit, J. H. (2019) suggests that this group primarily had patients with a (comorbid)
personality disorder (88%). BPD was found the most relevant amongst both the ND-PTSD
group and the D-PTSD group (40% and 38%, respectively), followed by personality disorder
(PD-NOS; 64% and 62%, respectively). The use of the depersonalization/derealisation
subscale indicated that more than half of the dissociative PTSD patients (54%) were found to
have met the criteria for DDs. Additionally, 66% did have a comorbid DD (Swart, S.,
Wildschut, M., Draijer, N., Langeland, W., & Smit, J. H., 2019). As much as 67% of the
epileptic patients with Dissociative Symptoms could meet the formal criteria used in the
diagnosis of PTSD (Pick, S., Mellers, J. D. C., & Goldstein, L.H., 2017). Another study by
Swart, S., Wildschut, M., Draijer, N., Langeland, W., & Smith, J. H., (2019) could identify
that 86% of the patients in the Dissociative PTSD (D-PTSD) group had a (comorbid)
personality disorder. In a study of (Lyssenko, L., Schmahl, C., Bockhacker, L., Vonderlin, R.,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Bohus, M., & Kleindienst, N. (2018) of comorbidities of PTSD, dissociative disorders were
found to have the highest scores for dissociation (mean=35.3) followed by PTSD
(mean=32.6), anxiety disorders (mean=10.2), personality disorders (mean=16.6), affective
disorders (mean=19.4), eating disorders (mean=14.5) and schizophrenia (mean=19.1).
(54%) of people with the Dissociative-PTSD (D-PTSD) were found diagnosed with a
DD (Swart, S., Wildschut, M., Draijer, N., Langeland, W., & Smit, J. H.,2019). BPD had the
third-largest score with a mean score of 27.9 (95% CI=25.3, 30.6). The scoring was done
based on 27 publications and 1,705 individual patients. Considering the descending order, the
scores for other mental disorders were like conversion disorder (mean=25.6), anxiety
disorders (mean=15.2), somatic symptoms disorder (mean=18.8), feeding and eating
disorders (mean=18.6), schizophrenia (mean=17.8), OCD (mean=15.3), depressive disorders
(mean=15.3), substance-related and addictive disorders (gambling disorder, mean=19.9;
alcohol use disorder, mean=19.7; other substance-related disorders, mean=17.7), and bipolar
and related disorders (mean=14.8). The high mean dissociation scores of addictive disorders
were like 19.7 for alcohol use disorder, 17.7 for other substance-related disorders, and 19.9
for gambling disorder. It may be partially related to dissociative disorders, PTSD, and
borderline personality disorder (Lyssenko, L., Schmahl, C., Bockhacker, L., Vonderlin, R.,
Bohus, M., & Kleindienst, N., 2018).
Mood disorders (54%) were being found as the most common of the problems.
ADHD (18%) and disruptive behavior disorders (16%; e.g., conduct disorder, oppositional
defiant disorder) followed this. The majority of participants (90.0%) reported that they take at
a minimum one prescribed medication for treating mood or behavioral health issues
(Woodward, E. C., Viana, A. G., Raines, E. M., Hanna, A. E., &Zvolensky, M. J., 2018). Out
of 7,866 people, those who were found infected from any PTSD comorbidity also had a third
condition. People with a third condition make up around (62.2%) of those who participated in
found to have the highest scores for dissociation (mean=35.3) followed by PTSD
(mean=32.6), anxiety disorders (mean=10.2), personality disorders (mean=16.6), affective
disorders (mean=19.4), eating disorders (mean=14.5) and schizophrenia (mean=19.1).
(54%) of people with the Dissociative-PTSD (D-PTSD) were found diagnosed with a
DD (Swart, S., Wildschut, M., Draijer, N., Langeland, W., & Smit, J. H.,2019). BPD had the
third-largest score with a mean score of 27.9 (95% CI=25.3, 30.6). The scoring was done
based on 27 publications and 1,705 individual patients. Considering the descending order, the
scores for other mental disorders were like conversion disorder (mean=25.6), anxiety
disorders (mean=15.2), somatic symptoms disorder (mean=18.8), feeding and eating
disorders (mean=18.6), schizophrenia (mean=17.8), OCD (mean=15.3), depressive disorders
(mean=15.3), substance-related and addictive disorders (gambling disorder, mean=19.9;
alcohol use disorder, mean=19.7; other substance-related disorders, mean=17.7), and bipolar
and related disorders (mean=14.8). The high mean dissociation scores of addictive disorders
were like 19.7 for alcohol use disorder, 17.7 for other substance-related disorders, and 19.9
for gambling disorder. It may be partially related to dissociative disorders, PTSD, and
borderline personality disorder (Lyssenko, L., Schmahl, C., Bockhacker, L., Vonderlin, R.,
Bohus, M., & Kleindienst, N., 2018).
Mood disorders (54%) were being found as the most common of the problems.
ADHD (18%) and disruptive behavior disorders (16%; e.g., conduct disorder, oppositional
defiant disorder) followed this. The majority of participants (90.0%) reported that they take at
a minimum one prescribed medication for treating mood or behavioral health issues
(Woodward, E. C., Viana, A. G., Raines, E. M., Hanna, A. E., &Zvolensky, M. J., 2018). Out
of 7,866 people, those who were found infected from any PTSD comorbidity also had a third
condition. People with a third condition make up around (62.2%) of those who participated in
the study. A majority of these common trimorbidities included depressive disorder, PTSD as
well as another disorder (GAD: 47.2%; AUD: 40.9%; adjustment disorder: 39.4%; and
personality disorder: 21.9%). The list of other common trimorbidities included GAD, PTSD
and another disorder (AUD: 29.8%; adjustment disorder: 29.8%; in addition to the
trimorbidity of PTSD, GAD, and depressive disorder, as listed previously). The list also
included AUD, PTSD and another disorder (adjustment disorder: 24.3%; in addition to
trimorbidities of PTSD, AUD, and depressive disorder or GAD, as listed above) (Walter, K.
H., Levine, J. A., Highfill, M. R. M., Navarro, M., Thomsen, C. J., & Highfill-McRoy, R. M.,
2018).
As discovered by Soffer-Dudek, N (2014), 40% of depressed women also suffered
from “dissociative depression”. Individuals suffering from “dissociative depression” also had
significant depressive symptoms as compared to women diagnosed with non-dissociative
symptoms. There can be many symptoms of dissociative depression-like increased suicidality
attempts or thoughts, self-mutilation, eating disorder symptoms, thoughts of guilt and
worthlessness, reports of childhood trauma, mood swings and feeling of emptiness,
diminished concentration and indecisiveness (Soffer-Dudek, N, 2014). It has to be a case for
an individual diagnosed with PTSD to also have a common comorbidity diagnosis of MDD,
DD or dissociative symptoms and anxiety disorder (AD). In the study of (Soffer-Dudek, N,
2014) of the 2000 patients, 16.8% of the patients were identified to have attempted for
suicide at least once, 1838 patients were found to have suffered from depressive and/or AD,
58% of the patients had once developed the suicidal thoughts while 269 patients were
diagnosed with MDD. Another study states that people diagnosed with MDD 59.2% of those
had developed suicidal thoughts. Additionally, 13.1% of the 480 patients suffered from BPD
and MDD had once attempted suicide (Yilmaz, E. B., 2019). For patients diagnosed with a
psychotic disorder, 30% of them had attempted suicides. As found by Putts, M. R. (2014),
well as another disorder (GAD: 47.2%; AUD: 40.9%; adjustment disorder: 39.4%; and
personality disorder: 21.9%). The list of other common trimorbidities included GAD, PTSD
and another disorder (AUD: 29.8%; adjustment disorder: 29.8%; in addition to the
trimorbidity of PTSD, GAD, and depressive disorder, as listed previously). The list also
included AUD, PTSD and another disorder (adjustment disorder: 24.3%; in addition to
trimorbidities of PTSD, AUD, and depressive disorder or GAD, as listed above) (Walter, K.
H., Levine, J. A., Highfill, M. R. M., Navarro, M., Thomsen, C. J., & Highfill-McRoy, R. M.,
2018).
As discovered by Soffer-Dudek, N (2014), 40% of depressed women also suffered
from “dissociative depression”. Individuals suffering from “dissociative depression” also had
significant depressive symptoms as compared to women diagnosed with non-dissociative
symptoms. There can be many symptoms of dissociative depression-like increased suicidality
attempts or thoughts, self-mutilation, eating disorder symptoms, thoughts of guilt and
worthlessness, reports of childhood trauma, mood swings and feeling of emptiness,
diminished concentration and indecisiveness (Soffer-Dudek, N, 2014). It has to be a case for
an individual diagnosed with PTSD to also have a common comorbidity diagnosis of MDD,
DD or dissociative symptoms and anxiety disorder (AD). In the study of (Soffer-Dudek, N,
2014) of the 2000 patients, 16.8% of the patients were identified to have attempted for
suicide at least once, 1838 patients were found to have suffered from depressive and/or AD,
58% of the patients had once developed the suicidal thoughts while 269 patients were
diagnosed with MDD. Another study states that people diagnosed with MDD 59.2% of those
had developed suicidal thoughts. Additionally, 13.1% of the 480 patients suffered from BPD
and MDD had once attempted suicide (Yilmaz, E. B., 2019). For patients diagnosed with a
psychotic disorder, 30% of them had attempted suicides. As found by Putts, M. R. (2014),
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
66% of individuals diagnosed with a recent first episode of psychosis had fulfilled the
standards for PTSD syndrome. In case when the duration of symptoms was not considered,
39% of the individuals met the DSM-5 criteria commonly identified for PTSD. Of individuals
who had a recent onset of psychosis, 32% of these felt the shock of a serious accident. The
percentage rises to 46% in the case when the individuals had multiple psychotic episodes
(Putts, M. R., 2014).
Few studies could identify that ADHD children had comorbid DD. For adolescents or
children with ADHD, some health conditions like hyperactivity and particularly impulsivity
can be the risk factors. In this context, peri-traumatic dissociation was identified as the most
powerful predictor of PTSD as well as related symptoms. This conclusion was drawn using
the reviews of 2647 studies in the context (Yılmaz, E. B., 2019). Adult populations were
found to have high comorbidity as evidenced by 8 studies. The most common of the
psychiatric diagnoses included MDD (100%) followed by PTSD (88%), attention-deficit
hyperactivity disorder (ADHD) (60%) and anxiety disorders (84%). The published work also
revealed higher prevalence rates for anxiety disorders. PTSD was identified to have the
highest prevalence in the studies of Bozkurt, H., DuzmanMutluer, T., Kose, C., &Zoroglu, S.
(2015). Another research done by Psychiatry & clinical neuroscience states that 71% of
children with ADHD also had comorbid DD. In similar studies, 93.9% of the adolescent with
PTSD and DD diagnosed to have MDD, separation anxiety disorder, oppositional defiant
disorder and ADHD.
Unfortunately, the risk factors with anxiety, depression and PTSD in impatient youth
are still understudied (Woodward, E. C., Viana, A. G., Raines, E. M., Hanna, A. E., &
Zvolensky, M. J., 2018). Many of the participants (64.1%) in the study reported having their
index assault occurred before the age of 18 (Mage of assault = 14.58 years, SD = 9.63). With
regards to the past-month PTSD, only 9 out of the 64 participants could only satisfy the
standards for PTSD syndrome. In case when the duration of symptoms was not considered,
39% of the individuals met the DSM-5 criteria commonly identified for PTSD. Of individuals
who had a recent onset of psychosis, 32% of these felt the shock of a serious accident. The
percentage rises to 46% in the case when the individuals had multiple psychotic episodes
(Putts, M. R., 2014).
Few studies could identify that ADHD children had comorbid DD. For adolescents or
children with ADHD, some health conditions like hyperactivity and particularly impulsivity
can be the risk factors. In this context, peri-traumatic dissociation was identified as the most
powerful predictor of PTSD as well as related symptoms. This conclusion was drawn using
the reviews of 2647 studies in the context (Yılmaz, E. B., 2019). Adult populations were
found to have high comorbidity as evidenced by 8 studies. The most common of the
psychiatric diagnoses included MDD (100%) followed by PTSD (88%), attention-deficit
hyperactivity disorder (ADHD) (60%) and anxiety disorders (84%). The published work also
revealed higher prevalence rates for anxiety disorders. PTSD was identified to have the
highest prevalence in the studies of Bozkurt, H., DuzmanMutluer, T., Kose, C., &Zoroglu, S.
(2015). Another research done by Psychiatry & clinical neuroscience states that 71% of
children with ADHD also had comorbid DD. In similar studies, 93.9% of the adolescent with
PTSD and DD diagnosed to have MDD, separation anxiety disorder, oppositional defiant
disorder and ADHD.
Unfortunately, the risk factors with anxiety, depression and PTSD in impatient youth
are still understudied (Woodward, E. C., Viana, A. G., Raines, E. M., Hanna, A. E., &
Zvolensky, M. J., 2018). Many of the participants (64.1%) in the study reported having their
index assault occurred before the age of 18 (Mage of assault = 14.58 years, SD = 9.63). With
regards to the past-month PTSD, only 9 out of the 64 participants could only satisfy the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
diagnostic criteria (Jones, A. C., Badour, C. L., Brake, C. A., Hood, C. O., & Feldner, M. T.,
2018). Youth (93%) with a psychiatric disorder were found to have the highest prevalence of
trauma exposure. Only 42% of the youth could fulfill the diagnostic criteria set for PTSD
(Woodward, et al., 2018). It also shows that PTSD symptomatology (Suliman et al. 2009)
kind of trauma exposure has the association of other internalizing problems like anxiety
(Pynoos et al. 1999) as well as mood disorders (Goenjian et al. 2011).
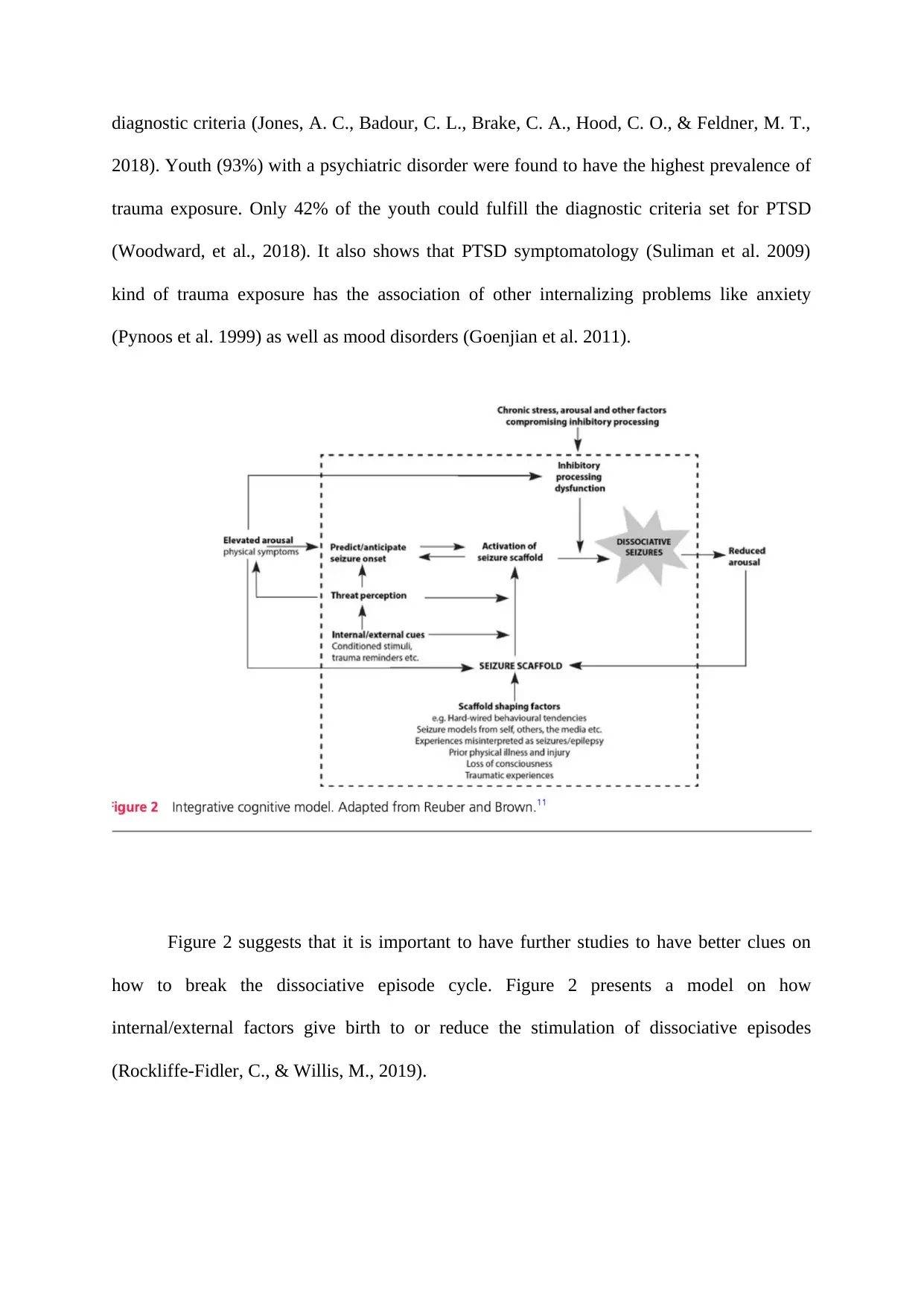
Figure 2 suggests that it is important to have further studies to have better clues on
how to break the dissociative episode cycle. Figure 2 presents a model on how
internal/external factors give birth to or reduce the stimulation of dissociative episodes
(Rockliffe-Fidler, C., & Willis, M., 2019).
2018). Youth (93%) with a psychiatric disorder were found to have the highest prevalence of
trauma exposure. Only 42% of the youth could fulfill the diagnostic criteria set for PTSD
(Woodward, et al., 2018). It also shows that PTSD symptomatology (Suliman et al. 2009)
kind of trauma exposure has the association of other internalizing problems like anxiety
(Pynoos et al. 1999) as well as mood disorders (Goenjian et al. 2011).
Figure 2 suggests that it is important to have further studies to have better clues on
how to break the dissociative episode cycle. Figure 2 presents a model on how
internal/external factors give birth to or reduce the stimulation of dissociative episodes
(Rockliffe-Fidler, C., & Willis, M., 2019).
1 out of 5
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.