Public Health Industry Placement: Diabetes Management in Australia
VerifiedAdded on 2023/03/17
|22
|6830
|72
Report
AI Summary
This report outlines a public health industry placement proposal focusing on the management of Type 2 Diabetes Mellitus in Australia, with a specific emphasis on the collaborative efforts of Torrens University Australia staff. The introduction highlights the global prevalence of diabetes, its associated health burdens, and the need for effective management strategies. The report discusses the issue of T2DM, including genetic predispositions and physiological mechanisms such as insulin resistance and beta-cell dysfunction. A comprehensive needs assessment is conducted, emphasizing the importance of screening, early diagnosis, and quality of life (QoL) assessments. The proposed practice change involves the use of questionnaires, regression models, and risk assessment tools to identify factors affecting QoL and to develop intervention strategies. The project design and implementation plan details a randomized control trial (RCT) study, utilizing the 'Life!' economic assessment tool and evidence-based interventions. A survey will be administered to a large sample of adults with T2DM, and cognitive interviews will be conducted to refine the survey instrument. The program aims to incorporate lifestyle modifications and prevention trials, with the HAPA model of behavioral change used to promote healthy behaviors and improve health outcomes.

RUNNING HEAD: PUBLIC HEALTH INDUSTRY PLACEMENT
PUBLIC HEALTH INDUSTRY PLACEMENT
Name of Student
Name of University
Author note
PUBLIC HEALTH INDUSTRY PLACEMENT
Name of Student
Name of University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PUBLIC HEALTH INDUSTRY PLACEMENT
Practice proposal
1. Introduction/Background
In 2015, about 415 million people, especially the adults of 29 to 79 years were
affected globally by diabetes mellitus and it was that the number will rise to 642 million by
the year of 2040. The Diabetes’s burden of disability is always associated with vast spectrum
of physical symptoms like fatigue, frequent urination, increased thirst and blurred vision
(Lipska, 2016). Complications of diabetes includes cerebral stroke (Poittevin, 2015), heart
failure, retinopathy (Zhang et al., 2017), nephropathy (Gnudi, Coward & Long, 2016)
amputation and diminished cognitive status. Diabetes mellitus is such a dire metabolic
disorder that it restricts activities of daily life and functional independence as well. Over the
last decade diabetes has increased the causation of disability on a widespread basis, globally.
Diabetes is a primary cause of mortality (Zinman et al., 2015) – the rate of whose increase
every year. According to International Diabetes Federation, there had been around 5 million
deaths due to diabetes in 2015.1 6, globally. Other than handling the health burden due to
diabetes, the national governments of different countries and also the international public
health organizations like Organization for Economic Co-operation Development (OECD) and
World Health Organization have concerned themselves about diabetes management. They
have focused on population groups like unprivileged and labors who suffer from diabetes and
connected the factors related to compromised quality of life of people suffering with diabetes.
The factors are financial impacts of the lifestyle disease’s curability costs on individuals and
they also studied how diabetes affected the government framework and how the government
have to have sufficient and enough taxation revenue levied, to provide the healthcare support
and other related services to the geriatric population with Diabetes Mellitus.
Practice proposal
1. Introduction/Background
In 2015, about 415 million people, especially the adults of 29 to 79 years were
affected globally by diabetes mellitus and it was that the number will rise to 642 million by
the year of 2040. The Diabetes’s burden of disability is always associated with vast spectrum
of physical symptoms like fatigue, frequent urination, increased thirst and blurred vision
(Lipska, 2016). Complications of diabetes includes cerebral stroke (Poittevin, 2015), heart
failure, retinopathy (Zhang et al., 2017), nephropathy (Gnudi, Coward & Long, 2016)
amputation and diminished cognitive status. Diabetes mellitus is such a dire metabolic
disorder that it restricts activities of daily life and functional independence as well. Over the
last decade diabetes has increased the causation of disability on a widespread basis, globally.
Diabetes is a primary cause of mortality (Zinman et al., 2015) – the rate of whose increase
every year. According to International Diabetes Federation, there had been around 5 million
deaths due to diabetes in 2015.1 6, globally. Other than handling the health burden due to
diabetes, the national governments of different countries and also the international public
health organizations like Organization for Economic Co-operation Development (OECD) and
World Health Organization have concerned themselves about diabetes management. They
have focused on population groups like unprivileged and labors who suffer from diabetes and
connected the factors related to compromised quality of life of people suffering with diabetes.
The factors are financial impacts of the lifestyle disease’s curability costs on individuals and
they also studied how diabetes affected the government framework and how the government
have to have sufficient and enough taxation revenue levied, to provide the healthcare support
and other related services to the geriatric population with Diabetes Mellitus.
2PUBLIC HEALTH INDUSTRY PLACEMENT
The direct costs of diabetes with regards to healthcare are very substantial and always
rising, with increase in the incidences of T2DM. In case of diabetes type 2, there had been an
increasing incidences of obesity development, more complications associated with the ageing
Fpopulation and the chief factors were identified to be improper diet and sedentary lifestyle.
In Australia alone, diabetes induced a healthcare management cost of $811 million (that is the
year of 2000–2001) to about $1507 million (that is the year of 2008–2009. The increase in
costs was approximately 86% which is even higher than the increase in other healthcare
(required for other diseases) expenditure costs (60%) over this period. In the year of 2008,
almost 43% of the healthcare expenditure that focused on managing diabetes in hospital was
followed by a 24% increase in the expenditure of community medicine (Hessler et al., 2017)
and disability prevention and 33% of the healthcare expenditure (Fayet-Moore et al., 2018)
was contributed to blood glucose controlling medicines. These are direct healthcare costs.
This is why the TUA staffs needs to use their volunteering day to engage to the community
service program by collaborating with a non-governmental organization.
While the factors that are associated with the health compromised quality of
(Trikkalinou, Papazafiropoulou & Melidonis, 2017) in people with diabetes and other chronic
diseases, have been addressed in the last decade but on the whole, there are still many lags in
the execution of community medicine and rehabilitation plans targeted towards diabetes
management(Garber et al., 2015). Hence, this study aims is to propose a practice change for a
better community management of diabetes mellitus type 2 (Marso, 2016) in Australia by the
collaborative action of Torrens University Australia staffs.
2. Issue Description (200 words)
There happens to be a strong genetic predisposition of type 2 diabetes mellitus in the
population. Individuals with relatives suffering from T2DM, are in elevated risk of
developing T2DM. A family history of diabetes mellitus is huge concern for the progeny as
The direct costs of diabetes with regards to healthcare are very substantial and always
rising, with increase in the incidences of T2DM. In case of diabetes type 2, there had been an
increasing incidences of obesity development, more complications associated with the ageing
Fpopulation and the chief factors were identified to be improper diet and sedentary lifestyle.
In Australia alone, diabetes induced a healthcare management cost of $811 million (that is the
year of 2000–2001) to about $1507 million (that is the year of 2008–2009. The increase in
costs was approximately 86% which is even higher than the increase in other healthcare
(required for other diseases) expenditure costs (60%) over this period. In the year of 2008,
almost 43% of the healthcare expenditure that focused on managing diabetes in hospital was
followed by a 24% increase in the expenditure of community medicine (Hessler et al., 2017)
and disability prevention and 33% of the healthcare expenditure (Fayet-Moore et al., 2018)
was contributed to blood glucose controlling medicines. These are direct healthcare costs.
This is why the TUA staffs needs to use their volunteering day to engage to the community
service program by collaborating with a non-governmental organization.
While the factors that are associated with the health compromised quality of
(Trikkalinou, Papazafiropoulou & Melidonis, 2017) in people with diabetes and other chronic
diseases, have been addressed in the last decade but on the whole, there are still many lags in
the execution of community medicine and rehabilitation plans targeted towards diabetes
management(Garber et al., 2015). Hence, this study aims is to propose a practice change for a
better community management of diabetes mellitus type 2 (Marso, 2016) in Australia by the
collaborative action of Torrens University Australia staffs.
2. Issue Description (200 words)
There happens to be a strong genetic predisposition of type 2 diabetes mellitus in the
population. Individuals with relatives suffering from T2DM, are in elevated risk of
developing T2DM. A family history of diabetes mellitus is huge concern for the progeny as
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PUBLIC HEALTH INDUSTRY PLACEMENT
well. PPARG,TCF7L2, FTO, NOTCH2, KCNJ11, CDKAL1, WFS1, SLC30A8, HHEX
IGF2BP2 and JAZF1 genes have shown strong associations with the onset and pathogenesis
of T2DM. KCNJ11 that is potassium inwardly rectifying channel, J FMAILY 11 – has been
reported to encode a potassium channel that regulates pro –glucagon’s genetic expression and
glucagon like peptide’s production.
T2DM is classically characterized by the insulin insensitivity (Perry, 2015) which
occurs as a result of a physical insulin resistance, increase blood glucose levels (Nehme et al.,
2016) and decline in insulin production and consequent failure of Beta cells of islets of
Langerhans (Folli et al., 2018). This state leads to diminishing of glucose transport systems
into hepatocytes (Verhave et al., 2016), myocytes (Väremo et al., 2017), adipose cells
(Kusminski, Bickel & Scherer, 2016) breaks down rapidly in a hyper-glycemic state
(Inzucchi et al., 2015). Impaired alpha-cell function (Brereton, 20150 has have been recently
identified to be a contributor of T2DM’s pathophysiology.
There is a feedback loop that interlaces the play between insulin sensitive organs,
tissues and the beta cells. Insulin is released due to β-cell stimulation (Gerber & Rutter, 2017)
that mediate the uptake of amino acids, glucose and also fatty acids by the insulin-sensitive
cells and tissues. The feedback information (that insulin is required) from tissues to islet of
Langerhans, involves a lot of integration between humoral (Farnsworth et al., 2019) and the
brain systems. Insulin resistance if present along with obesity (Miyamoto et al., 2016) - the β-
cell (beta cells of Islet) elevates the insulin secretion to achieve and balance the glucose
tolerance (normal). When β-cells (beta cells) becomes incapable of functioning, the blood
glucose elevates in the plasma.
well. PPARG,TCF7L2, FTO, NOTCH2, KCNJ11, CDKAL1, WFS1, SLC30A8, HHEX
IGF2BP2 and JAZF1 genes have shown strong associations with the onset and pathogenesis
of T2DM. KCNJ11 that is potassium inwardly rectifying channel, J FMAILY 11 – has been
reported to encode a potassium channel that regulates pro –glucagon’s genetic expression and
glucagon like peptide’s production.
T2DM is classically characterized by the insulin insensitivity (Perry, 2015) which
occurs as a result of a physical insulin resistance, increase blood glucose levels (Nehme et al.,
2016) and decline in insulin production and consequent failure of Beta cells of islets of
Langerhans (Folli et al., 2018). This state leads to diminishing of glucose transport systems
into hepatocytes (Verhave et al., 2016), myocytes (Väremo et al., 2017), adipose cells
(Kusminski, Bickel & Scherer, 2016) breaks down rapidly in a hyper-glycemic state
(Inzucchi et al., 2015). Impaired alpha-cell function (Brereton, 20150 has have been recently
identified to be a contributor of T2DM’s pathophysiology.
There is a feedback loop that interlaces the play between insulin sensitive organs,
tissues and the beta cells. Insulin is released due to β-cell stimulation (Gerber & Rutter, 2017)
that mediate the uptake of amino acids, glucose and also fatty acids by the insulin-sensitive
cells and tissues. The feedback information (that insulin is required) from tissues to islet of
Langerhans, involves a lot of integration between humoral (Farnsworth et al., 2019) and the
brain systems. Insulin resistance if present along with obesity (Miyamoto et al., 2016) - the β-
cell (beta cells of Islet) elevates the insulin secretion to achieve and balance the glucose
tolerance (normal). When β-cells (beta cells) becomes incapable of functioning, the blood
glucose elevates in the plasma.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PUBLIC HEALTH INDUSTRY PLACEMENT
The TUA staffs will be volunteering for a diabetes control public health program
together with community based organisation.
3. Needs Assessment (750 words)
Tests are must and should be performed imperatively to screen and diagnose Diabetes
Mellitus in the affected population. Public health should be monitored to prevent the
incidences or progression of T2DM in Australian population (Kumar et al., 2018). The tests
that are used for screening diabetes should be incorporated in the health system more often as
there is a high need of diagnosing diabetes as soon as possible so as to prevent its
progressive, life threatening symptoms. Subjects with diabetes mellitus have been reported to
develop micro-vascular complications if the disease goes unchecked for about five years.
Symptoms of later stage diabetes like polydipsia (Aghababaie et al., 2018), polyuria (Thurtell
& Mackie, 2018), polyphagia (Pawar, 2017) and even weight loss (Leung, 2016) are
significant and should be diagnosed with an oral glucose tolerance test (OGTT). This practice
change would strive to make the use of this this glucose tolerance test, mandatory on a
national basis with the help of national framework.
Quality of life is also disturbed in families whose member is suffering from Type 2
diabetes mellitus. Assessment of Qol (Quality of life) is an important tool that the practice
change will use – to analyze the deficiencies in QoL associated with diabetes and a social
intervention in addition to medical intervention will be designed under the proposed public
health plan. Data will first be collected through a mailed self- administered questionnaire.
Regression models along with control variables (adjustable) will be used as the practice
change model – that would study and assess the complication associations and the
comorbidities associated with diabetes-induced QoL. Economic factors, glycemic control and
geriatric health issues will be assessed by the practice change model in order to find the
important correlations with diabetes mellitus. Poor quality of life (PqoL) of patients with
The TUA staffs will be volunteering for a diabetes control public health program
together with community based organisation.
3. Needs Assessment (750 words)
Tests are must and should be performed imperatively to screen and diagnose Diabetes
Mellitus in the affected population. Public health should be monitored to prevent the
incidences or progression of T2DM in Australian population (Kumar et al., 2018). The tests
that are used for screening diabetes should be incorporated in the health system more often as
there is a high need of diagnosing diabetes as soon as possible so as to prevent its
progressive, life threatening symptoms. Subjects with diabetes mellitus have been reported to
develop micro-vascular complications if the disease goes unchecked for about five years.
Symptoms of later stage diabetes like polydipsia (Aghababaie et al., 2018), polyuria (Thurtell
& Mackie, 2018), polyphagia (Pawar, 2017) and even weight loss (Leung, 2016) are
significant and should be diagnosed with an oral glucose tolerance test (OGTT). This practice
change would strive to make the use of this this glucose tolerance test, mandatory on a
national basis with the help of national framework.
Quality of life is also disturbed in families whose member is suffering from Type 2
diabetes mellitus. Assessment of Qol (Quality of life) is an important tool that the practice
change will use – to analyze the deficiencies in QoL associated with diabetes and a social
intervention in addition to medical intervention will be designed under the proposed public
health plan. Data will first be collected through a mailed self- administered questionnaire.
Regression models along with control variables (adjustable) will be used as the practice
change model – that would study and assess the complication associations and the
comorbidities associated with diabetes-induced QoL. Economic factors, glycemic control and
geriatric health issues will be assessed by the practice change model in order to find the
important correlations with diabetes mellitus. Poor quality of life (PqoL) of patients with
5PUBLIC HEALTH INDUSTRY PLACEMENT
mental health associations of diabetes like anxiety, depression and schizophrenia will
assessed by the practice change model as well. Factors like age, gender, diabetes duration,
treatment methods, sampling areas and geography along with socio – demographic factors
will be taken into count. Disease management with self-empowerment and other psychosocial
strategies would be done by the proposed practice change. The chief correlation of mental
health issues with glycemic control will be assessed and the findings will be transferred to
research setting. Mental health care will be used a chief health management tool to improve
the quality of life of people with diabetes.
A Risk assessment tool that based on lifestyle and demographic, other anthropometric
measures will be used by the proposed practise change, with a five year follow up plan.
Risk factors which are associated with T2dM type 2 Diabetes Mellitus are preventable
and it can be done through lifestyle modifications, specifically weight loss and increased
physical activity. The practice change intends to incorporate prevention trials by usage of
lifestyle changes to decrease the risk of diabetes complications. The very role of lifestyle
tools in progression of the T2DM complications among the individuals with a dysfunctional
glucose tolerance – has been found to be very effective by many reports and hence, it
becomes a ‘tool’ of choice for this health project. A randomized control trial study will be
done as well with a research purpose, to transfer the interventional knowledge to further
higher research environments.
Understanding the fact that how interventions will be applied on wider-scale will be
the important step in translation of prevention researches in diabetes into the very population
targeted strategies, spanning from a state to whole nation. The study and public healthcare
plan will also use ‘knowledge’ as a device to increase the effectiveness of healthcare
operations and interventions, the acceptability of these healthcare services by the public or
mental health associations of diabetes like anxiety, depression and schizophrenia will
assessed by the practice change model as well. Factors like age, gender, diabetes duration,
treatment methods, sampling areas and geography along with socio – demographic factors
will be taken into count. Disease management with self-empowerment and other psychosocial
strategies would be done by the proposed practice change. The chief correlation of mental
health issues with glycemic control will be assessed and the findings will be transferred to
research setting. Mental health care will be used a chief health management tool to improve
the quality of life of people with diabetes.
A Risk assessment tool that based on lifestyle and demographic, other anthropometric
measures will be used by the proposed practise change, with a five year follow up plan.
Risk factors which are associated with T2dM type 2 Diabetes Mellitus are preventable
and it can be done through lifestyle modifications, specifically weight loss and increased
physical activity. The practice change intends to incorporate prevention trials by usage of
lifestyle changes to decrease the risk of diabetes complications. The very role of lifestyle
tools in progression of the T2DM complications among the individuals with a dysfunctional
glucose tolerance – has been found to be very effective by many reports and hence, it
becomes a ‘tool’ of choice for this health project. A randomized control trial study will be
done as well with a research purpose, to transfer the interventional knowledge to further
higher research environments.
Understanding the fact that how interventions will be applied on wider-scale will be
the important step in translation of prevention researches in diabetes into the very population
targeted strategies, spanning from a state to whole nation. The study and public healthcare
plan will also use ‘knowledge’ as a device to increase the effectiveness of healthcare
operations and interventions, the acceptability of these healthcare services by the public or
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PUBLIC HEALTH INDUSTRY PLACEMENT
specified population, the uptake of individual responsibilities by the service providers, to
assess the costing and reach of this intended public health service to target groups, practice
policy and health researches. The proposed healthcare program’s fidelity, intensity and
sustainability will be evaluated beforehand.
HAPA model of behavioral change with standardized health educator and participant
manual will be used to note blood pressure, the lipid levels, the blood sugar levels along with
their individual achievable goals and health outcomes. Payments will be made to the
facilitators for returning the data to be used for quality of Life improvement and further
evaluation. HAPA behavior shift theories will be used to stimulate the TUA participants to
forge an intention building, helping them to make their own lifestyle changes which can be
healthy diet, active lifestyle. This would prevent complications like cardiovascular disease
and other neuropathies.
4. Project Design and Implementation Plan (1500 words)
The public health reinforcement program will use the following project design. A
RCT study is also kept as a provision where participants will be randomly allocated to same
intervention and they will receive diabetes specific care for the same duration. Economic
assessment named ‘Life!’ can be used as an assessment tool. And after this, evidence based
interventions will be ‘applied’ to the chosen community. For this design, a PPS analysis
method will be used that demonstrates the alterations bought by the intervention – in weight,
in waist circumference, in systolic pressure, in diastolic pressure as compared to the controls.
The changes will be measured, observed and re analysed to categorise them on the basis of
importance and to develop patient centred healthcare approaches.
Primarily, a survey will be designed that includes a core set of self-administered
therapeutic measures and module specific diabetes treatment regimens. Other specific
specified population, the uptake of individual responsibilities by the service providers, to
assess the costing and reach of this intended public health service to target groups, practice
policy and health researches. The proposed healthcare program’s fidelity, intensity and
sustainability will be evaluated beforehand.
HAPA model of behavioral change with standardized health educator and participant
manual will be used to note blood pressure, the lipid levels, the blood sugar levels along with
their individual achievable goals and health outcomes. Payments will be made to the
facilitators for returning the data to be used for quality of Life improvement and further
evaluation. HAPA behavior shift theories will be used to stimulate the TUA participants to
forge an intention building, helping them to make their own lifestyle changes which can be
healthy diet, active lifestyle. This would prevent complications like cardiovascular disease
and other neuropathies.
4. Project Design and Implementation Plan (1500 words)
The public health reinforcement program will use the following project design. A
RCT study is also kept as a provision where participants will be randomly allocated to same
intervention and they will receive diabetes specific care for the same duration. Economic
assessment named ‘Life!’ can be used as an assessment tool. And after this, evidence based
interventions will be ‘applied’ to the chosen community. For this design, a PPS analysis
method will be used that demonstrates the alterations bought by the intervention – in weight,
in waist circumference, in systolic pressure, in diastolic pressure as compared to the controls.
The changes will be measured, observed and re analysed to categorise them on the basis of
importance and to develop patient centred healthcare approaches.
Primarily, a survey will be designed that includes a core set of self-administered
therapeutic measures and module specific diabetes treatment regimens. Other specific
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PUBLIC HEALTH INDUSTRY PLACEMENT
measures and other important items will be included, half way after the survey. Cognitive
interviews (debriefing) will be conducted with 20 selected participants. The survey will be
posted to 15,000 adults (aging between 18 and 70 years) suffering or type 2 diabetes. The
data will be selected randomly using the National Diabetes Services Scheme (NDSS)
database. The online survey version will be advertised on a national platform. Respondents of
all diabetes and genders, ages will be adequately presented in both online and postal survey
samples. The demographics, social settings, family pre- dispositions, income, job related
stress, personal history and overall quality of life will be taken into consideration for the
study and to develop the health management protocols.
Persons who are more than 40 years should be screened and assessed for more often.
The screening is recommended more often as there are certain risk factors for certain
populations like Hispanics, Pacific Islander and Asian Americans. The research design
should collect cues on their BMI (basal metabolic rate) and obesity stages’ relation to the
severity of diabetes, the history of cardiovascular disease, hypertension history, low levels of
HDL cholesterol and also to hypertriglyceridemia. Polycystic ovarian syndrome will be
marked as a special area of care as an associated syndrome. Data cues regarding the physical
inactivity and insulin resistance will be pertinent. Women with gestational diabetes care will
be put under special care as well. The testing would begin first with 45 year and more aged
subjects and patients will be enrolled for a 3 year check-up as well. The tests for diabetes will
be done as well.
The project design also accommodates for Diabetes monitoring of glucose levels.
Fasting Plasma Glucose will be taken as a blood sample after 8 hour fasting. Two-Hour Oral
Glucose Tolerance test will be done to check the plasma glucose level is measured before and
after intake of glucose. DM will be diagnosed if the plasma glucose level is more than11.1
mmol/L in a 2 hour interval. This standard test will be used. Patients will consume a diet with
measures and other important items will be included, half way after the survey. Cognitive
interviews (debriefing) will be conducted with 20 selected participants. The survey will be
posted to 15,000 adults (aging between 18 and 70 years) suffering or type 2 diabetes. The
data will be selected randomly using the National Diabetes Services Scheme (NDSS)
database. The online survey version will be advertised on a national platform. Respondents of
all diabetes and genders, ages will be adequately presented in both online and postal survey
samples. The demographics, social settings, family pre- dispositions, income, job related
stress, personal history and overall quality of life will be taken into consideration for the
study and to develop the health management protocols.
Persons who are more than 40 years should be screened and assessed for more often.
The screening is recommended more often as there are certain risk factors for certain
populations like Hispanics, Pacific Islander and Asian Americans. The research design
should collect cues on their BMI (basal metabolic rate) and obesity stages’ relation to the
severity of diabetes, the history of cardiovascular disease, hypertension history, low levels of
HDL cholesterol and also to hypertriglyceridemia. Polycystic ovarian syndrome will be
marked as a special area of care as an associated syndrome. Data cues regarding the physical
inactivity and insulin resistance will be pertinent. Women with gestational diabetes care will
be put under special care as well. The testing would begin first with 45 year and more aged
subjects and patients will be enrolled for a 3 year check-up as well. The tests for diabetes will
be done as well.
The project design also accommodates for Diabetes monitoring of glucose levels.
Fasting Plasma Glucose will be taken as a blood sample after 8 hour fasting. Two-Hour Oral
Glucose Tolerance test will be done to check the plasma glucose level is measured before and
after intake of glucose. DM will be diagnosed if the plasma glucose level is more than11.1
mmol/L in a 2 hour interval. This standard test will be used. Patients will consume a diet with
8PUBLIC HEALTH INDUSTRY PLACEMENT
150 g carbohydrate per day for about 3 to 5 days, will not intake other medications like
diuretics and thiazides. The research project design will also include Glycated Hemoglobin to
check average blood glucose levels over last two months. Patients whose A1C is greater than
48 mmol/mol will be diagnosed as DM. A1C is a very convenient, standardized rapid test that
shows a less variation in pre-analytic variables. The fact that acute illness cannot affect the
test makes it more reliable.
Ethical implications will be considered. All the participants and diabetic subjects will
be treated with care and respect. A voluntary participation protocol will be used to enrol the
subjects into practise change. The healthcare resources will be distributed equally amongst
the participants and power will be given to participants if they do not want to be part of the
health service. The free will of the participants will be encouraged through and through. No
personal bias from any staff of TAU towards any subject will be entertained. Evidence based
practise protocols with adherence service, public health, nursing, medical and social
guidelines will strictly followed by the practise change practitioners to incorporate a ethical
best practise while treating the diabetic community.
A reference group with concepts, variables and measures well be established and
selection of psychological parameters to measure initial selection after the vital phases of
identification, consultation and cognitive debriefing will be done. Standardised measures
along with the survey-specific items will be distributed in the survey.
As data analysis, the themes like management, empowerment, impact and success
with relevant concepts will be determined and identified. For each one of the concepts -
questionnaire search will be completed. Measures will be considered for a single use if they
are found to appropriate for 18 to 70 year old adults and the findings will be incorporated to
the assessment of generic, chronic specific, diabetes specific population types.
150 g carbohydrate per day for about 3 to 5 days, will not intake other medications like
diuretics and thiazides. The research project design will also include Glycated Hemoglobin to
check average blood glucose levels over last two months. Patients whose A1C is greater than
48 mmol/mol will be diagnosed as DM. A1C is a very convenient, standardized rapid test that
shows a less variation in pre-analytic variables. The fact that acute illness cannot affect the
test makes it more reliable.
Ethical implications will be considered. All the participants and diabetic subjects will
be treated with care and respect. A voluntary participation protocol will be used to enrol the
subjects into practise change. The healthcare resources will be distributed equally amongst
the participants and power will be given to participants if they do not want to be part of the
health service. The free will of the participants will be encouraged through and through. No
personal bias from any staff of TAU towards any subject will be entertained. Evidence based
practise protocols with adherence service, public health, nursing, medical and social
guidelines will strictly followed by the practise change practitioners to incorporate a ethical
best practise while treating the diabetic community.
A reference group with concepts, variables and measures well be established and
selection of psychological parameters to measure initial selection after the vital phases of
identification, consultation and cognitive debriefing will be done. Standardised measures
along with the survey-specific items will be distributed in the survey.
As data analysis, the themes like management, empowerment, impact and success
with relevant concepts will be determined and identified. For each one of the concepts -
questionnaire search will be completed. Measures will be considered for a single use if they
are found to appropriate for 18 to 70 year old adults and the findings will be incorporated to
the assessment of generic, chronic specific, diabetes specific population types.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PUBLIC HEALTH INDUSTRY PLACEMENT
For each measurement, information will be collected and then assessed with validity
and reliability and the findings will be applied to diabetes-specific populations.
A Pilot study and also a cognitive debriefing will be done to ensure that the given
survey content is reliable and significant and also be checked for relevance. A suitability of
the study tools for the Australian adults suffering from 2 or 1 type diabetes – has to be
determined.. The patients will be asked to finish the cognitive debriefing and the survey.
Participant data and participants will be collected and selected through diabetes based
advertisements (such as Diabetes Australia-Vic magazines, electronic newsletters and
relevant websites). Potential participants will be contacted by the researchers over email or
telephone as the request for participation will be sent by email, fax or post and a copy of a
plain language written statement will be provided and a consent form will be sent to the
participants to sign which marks and signifies their voluntary support. Participants who are
eligible only if the meet the very inclusion criteria of the research practice change of the
national sample of the survey. Decisions regarding participant recruitment will be made on
basis of the responses to specific screening type of the research questions. This ensures a
sample that is right for the aims addressed by the study phase (that is there should be both
genders - women and men, of both types of diabetes, of different ages and undergoing
various treatments, occupations and educational levels. Also, the subjects are required to be
wilful to be attending the interviews held in their respective areas and the participants should
also be very willing to the practise change research and public healthcare change protocols all
the same.
After the CD session, participants will be posting a copy of survey booklet along with
a letter where they will be informing that they have answered all the necessary questions in
the interviews and also answered the questions in the survey as well. The participants will be
For each measurement, information will be collected and then assessed with validity
and reliability and the findings will be applied to diabetes-specific populations.
A Pilot study and also a cognitive debriefing will be done to ensure that the given
survey content is reliable and significant and also be checked for relevance. A suitability of
the study tools for the Australian adults suffering from 2 or 1 type diabetes – has to be
determined.. The patients will be asked to finish the cognitive debriefing and the survey.
Participant data and participants will be collected and selected through diabetes based
advertisements (such as Diabetes Australia-Vic magazines, electronic newsletters and
relevant websites). Potential participants will be contacted by the researchers over email or
telephone as the request for participation will be sent by email, fax or post and a copy of a
plain language written statement will be provided and a consent form will be sent to the
participants to sign which marks and signifies their voluntary support. Participants who are
eligible only if the meet the very inclusion criteria of the research practice change of the
national sample of the survey. Decisions regarding participant recruitment will be made on
basis of the responses to specific screening type of the research questions. This ensures a
sample that is right for the aims addressed by the study phase (that is there should be both
genders - women and men, of both types of diabetes, of different ages and undergoing
various treatments, occupations and educational levels. Also, the subjects are required to be
wilful to be attending the interviews held in their respective areas and the participants should
also be very willing to the practise change research and public healthcare change protocols all
the same.
After the CD session, participants will be posting a copy of survey booklet along with
a letter where they will be informing that they have answered all the necessary questions in
the interviews and also answered the questions in the survey as well. The participants will be
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10PUBLIC HEALTH INDUSTRY PLACEMENT
asked to follow the survey related instructions, sections or the questions or the response
options as well. During the cognitive debriefing session, the participants will be asked to
write the consent. At every point of the research – the participant would retain his or her
rights and free will. These interviews will be monitored and recorded in a special format (de-
identified). Patient can choose and not choose to answer the CD questions.
Participants will be first asked to answer the survey that they think is relevant to them
in terms of language, readability, culture and even the length. Patients will be asked for a
feedback about the length of the interview and how long or short or time consuming it was.
Participants will be then asked if the number of CD questions in each survey along with the
choosing of a standardised specific set of psychological tools and also study items – were
actually relevant to them.
5. Gantt Chart and Budget
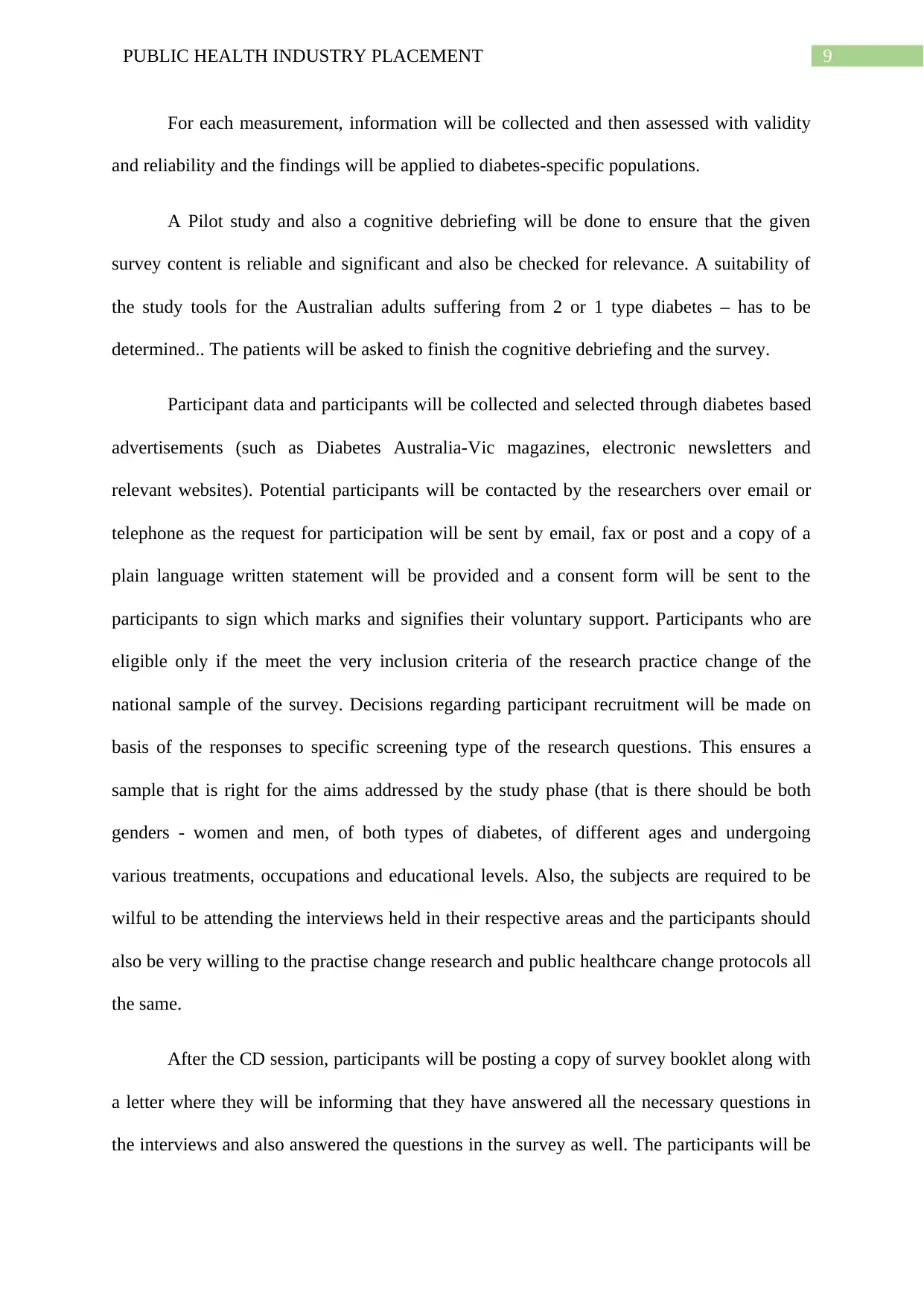
Week 1-4 Week 5-9 Week 10-15 Week 16-26 Week 26-29 Week 30
Topic selection
Structuring the
Proposal
Research about
Literature review
Collection of
samples
Experiments
asked to follow the survey related instructions, sections or the questions or the response
options as well. During the cognitive debriefing session, the participants will be asked to
write the consent. At every point of the research – the participant would retain his or her
rights and free will. These interviews will be monitored and recorded in a special format (de-
identified). Patient can choose and not choose to answer the CD questions.
Participants will be first asked to answer the survey that they think is relevant to them
in terms of language, readability, culture and even the length. Patients will be asked for a
feedback about the length of the interview and how long or short or time consuming it was.
Participants will be then asked if the number of CD questions in each survey along with the
choosing of a standardised specific set of psychological tools and also study items – were
actually relevant to them.
5. Gantt Chart and Budget
Week 1-4 Week 5-9 Week 10-15 Week 16-26 Week 26-29 Week 30
Topic selection
Structuring the
Proposal
Research about
Literature review
Collection of
samples
Experiments
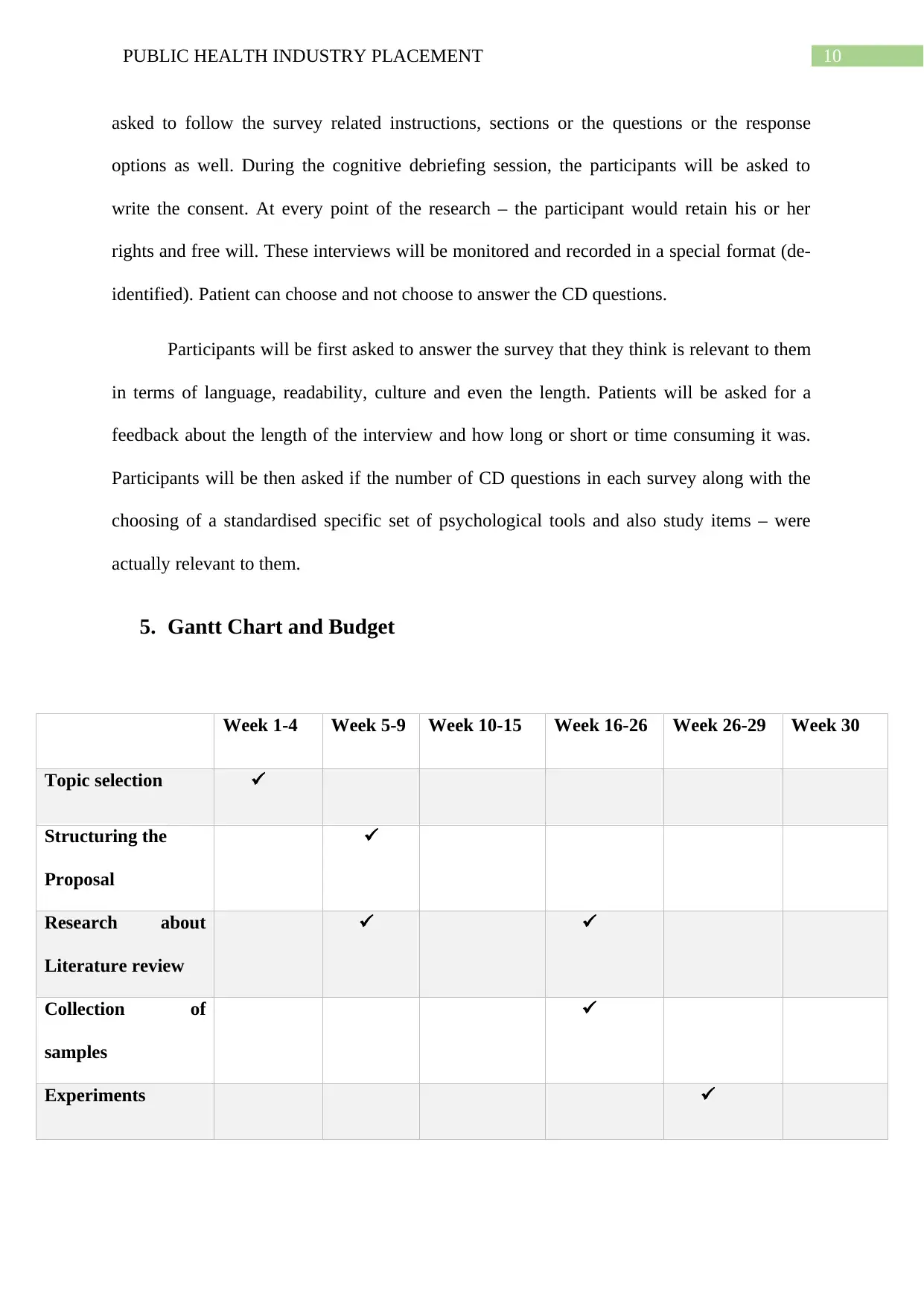
11PUBLIC HEALTH INDUSTRY PLACEMENT
Analysis of results
Submission of final
work
6. Evaluation Criteria (750 words)
Hard copy along with online survey versions will be developed. A clinical research
terminology will be used and then all the hard copied survey booklets that is in a closed
format will be put to a data entry system (automated). The whole research survey will be
designed using a web developer based application.
The postal survey booklets specific to diabetic studies and diabetic characteristics
with symptoms will be packaged in an envelope (reply envelope), and a plain or simplistic
language statement along with consent file, language and contact form will be sent. The
language form will include all the major global languages.
Approximately about six weeks will be allocated for the data collection procedure
(that is through postal survey’s distribution and completion).
Postal survey will be given to a very randomly selected sample of apt registrants who
are under the scheme of National Diabetes Services. The scheme already has 1 million
citizens of Australia affected by diabetes (for example T2DM, T1DM, gestational) under its
policy and service. These applicants will be considered for the selection only if they meet the
study’s inclusion criteria: like surviving with T1DM/T1DM diabetes and should be in the age
group of eighteen to seventy years and they should have a minimal functional independence
so as to participle. In order words, they should be paralysed or bed ridden.
Analysis of results
Submission of final
work
6. Evaluation Criteria (750 words)
Hard copy along with online survey versions will be developed. A clinical research
terminology will be used and then all the hard copied survey booklets that is in a closed
format will be put to a data entry system (automated). The whole research survey will be
designed using a web developer based application.
The postal survey booklets specific to diabetic studies and diabetic characteristics
with symptoms will be packaged in an envelope (reply envelope), and a plain or simplistic
language statement along with consent file, language and contact form will be sent. The
language form will include all the major global languages.
Approximately about six weeks will be allocated for the data collection procedure
(that is through postal survey’s distribution and completion).
Postal survey will be given to a very randomly selected sample of apt registrants who
are under the scheme of National Diabetes Services. The scheme already has 1 million
citizens of Australia affected by diabetes (for example T2DM, T1DM, gestational) under its
policy and service. These applicants will be considered for the selection only if they meet the
study’s inclusion criteria: like surviving with T1DM/T1DM diabetes and should be in the age
group of eighteen to seventy years and they should have a minimal functional independence
so as to participle. In order words, they should be paralysed or bed ridden.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 22
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




