University of Bedfordshire - Bioscience Research Project Dissertation
VerifiedAdded on 2023/01/11
|27
|7355
|68
Project
AI Summary
This project dissertation investigates the association between Pulmonary Hypertension (PH) and Sickle Cell Anemia (SCA). The study begins with an abstract summarizing the background of both diseases, highlighting the potential for increased mortality when they co-occur. The purpose of the study is to determine if pulmonary hypertension is associated with sickle cell anemia. The methodology involves a literature review of four databases, focusing on studies published within the last 10 years. The findings section presents the results of the literature review, summarizing key studies that explore the prevalence and mechanisms of PH in SCD patients. The dissertation includes an introduction that provides background information on Sickle Cell Anemia and Pulmonary Hypertension, including their pathophysiology and significance. The methodology section details the search strategy, inclusion/exclusion criteria, and ethical considerations. The results are presented in a table, summarizing the findings of the included studies. The study concludes that there is adequate evidence to suggest that both diseases are interrelated.

Project Dissertation 1
Project Dissertation
Title: Is Pulmonary Hypertension associated with Sickle Cell Anaemia?
Student Name:
Student ID:
Degree Program:
Project Dissertation
Title: Is Pulmonary Hypertension associated with Sickle Cell Anaemia?
Student Name:
Student ID:
Degree Program:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Project Dissertation 2
ABSTRACT
Background: Sickle Cell Anaemia is a genetically inherited disorder which may cause extensive
organ damage. In sickle cell patients, Pulmonary Hypertension (PH) can complicate the acute
chest syndrome which is fatal. PH is known to occur in 6-11% of the sickle cell patients
contributing to increased risk of mortality. There is 40% mortality rate depicted in patients of
sickle cell anemia with pulmonary hypertension compared to sickle cell patients without PH .
Therefore, this field requires extensive research to identify their mutual impact.
Purpose of Study: To find out whether pulmonary hypertension is associated with Sickle Cell
Anaemia?
Method: The literature review explored four databases: Pubmed, CINAHL, Cochrane, Allied and
Contemporary medicine Database (AMED). 10 studies reflecting over the association of PH with
Sickle cell Anaemia were consulted.
Findings: Six studies proved the effective role of PH in Sickle Cell Disease (SCD) patients. Two
articles described the potential mechanism involved, and the two articles focused on the types of
PH and their prevalence in Sickle Cell Anaemia patients.
Conclusion: The analysis and evaluation of related articles reflects there are adequate evidences
to suggest that both diseases are interrelated.
Keywords: Sickle Cell Anaemia; Pulmonary Hypertension.
ABSTRACT
Background: Sickle Cell Anaemia is a genetically inherited disorder which may cause extensive
organ damage. In sickle cell patients, Pulmonary Hypertension (PH) can complicate the acute
chest syndrome which is fatal. PH is known to occur in 6-11% of the sickle cell patients
contributing to increased risk of mortality. There is 40% mortality rate depicted in patients of
sickle cell anemia with pulmonary hypertension compared to sickle cell patients without PH .
Therefore, this field requires extensive research to identify their mutual impact.
Purpose of Study: To find out whether pulmonary hypertension is associated with Sickle Cell
Anaemia?
Method: The literature review explored four databases: Pubmed, CINAHL, Cochrane, Allied and
Contemporary medicine Database (AMED). 10 studies reflecting over the association of PH with
Sickle cell Anaemia were consulted.
Findings: Six studies proved the effective role of PH in Sickle Cell Disease (SCD) patients. Two
articles described the potential mechanism involved, and the two articles focused on the types of
PH and their prevalence in Sickle Cell Anaemia patients.
Conclusion: The analysis and evaluation of related articles reflects there are adequate evidences
to suggest that both diseases are interrelated.
Keywords: Sickle Cell Anaemia; Pulmonary Hypertension.
Project Dissertation 3
CHAPTER 1- INTRODUCTION
1.1. Background
Sickle Cell Anemia is a blood disorder mainly occurring due to genetic inheritance of abnormal
protein in the RBCs which makes them distorted and sickle shaped (National Heart, Lung and
Blood Institute, 2018). It is characterized by the substitution of amino acids in beta globin chain
due to presence of homozygous hemoglobin SS (Klings and Farber,2019).
The disease is mostly prevalent in African Americans(National Heart, Lung and Blood Institute,
2018) . It is an autosomal recessive disorder in which the polymerization of Hemoglobin-S
occurs upon deoxygenation. The polymerization increases the sickling and rigidity of red blood
cells. It injures the RBCs and reduces the blood circulation in them. The resulting complications
cause microvascular occlusions leading to injury of several body organs like kidney, lungs,
spleen, liver, central nervous system and severe pain in abdomen, joints, back and chest. The
sickle cell anaemia when associated with pulmonary hypertension, results into elevated risk of
early deaths, elevated WBC count> 15000 cell/mm3, seizures and renal failures (Ataga and
Clinggs, 2014).
Pulmonary Hypertension (PH) refers to a condition of high blood pressure (where resting
Pulmonary artery pressure >25 mmHg) developed within the arteries in the lungs and the heart
(Pulmonary Hypertension Association, 2019). PH may occur due to any illness that obstructs the
normal blood flow in the lungs for sustained periods. For example: collagen vascular disease,
liver cirrhosis, chronic lung disease and thromboembolism. The clinical symptoms and signs
exhibited by the patients of PH are Chronic Dyspnea, Hypoxemia, elevated tricuspid
regurgitation, Syncope, Arrhythmias, Cor Pulmonale and early death.
The sickle cell disease (SCD) patients have enhanced cardiac output due to anaemia. It is
observed that pulmonary vascular resistance and pulmonary pressures are higher in patients of
Sickle cell disease with Pulmonary Hypertension. Their cardiac output is also higher than the
normal range. These patients exhibit high rate of fatigue on exertion.
CHAPTER 1- INTRODUCTION
1.1. Background
Sickle Cell Anemia is a blood disorder mainly occurring due to genetic inheritance of abnormal
protein in the RBCs which makes them distorted and sickle shaped (National Heart, Lung and
Blood Institute, 2018). It is characterized by the substitution of amino acids in beta globin chain
due to presence of homozygous hemoglobin SS (Klings and Farber,2019).
The disease is mostly prevalent in African Americans(National Heart, Lung and Blood Institute,
2018) . It is an autosomal recessive disorder in which the polymerization of Hemoglobin-S
occurs upon deoxygenation. The polymerization increases the sickling and rigidity of red blood
cells. It injures the RBCs and reduces the blood circulation in them. The resulting complications
cause microvascular occlusions leading to injury of several body organs like kidney, lungs,
spleen, liver, central nervous system and severe pain in abdomen, joints, back and chest. The
sickle cell anaemia when associated with pulmonary hypertension, results into elevated risk of
early deaths, elevated WBC count> 15000 cell/mm3, seizures and renal failures (Ataga and
Clinggs, 2014).
Pulmonary Hypertension (PH) refers to a condition of high blood pressure (where resting
Pulmonary artery pressure >25 mmHg) developed within the arteries in the lungs and the heart
(Pulmonary Hypertension Association, 2019). PH may occur due to any illness that obstructs the
normal blood flow in the lungs for sustained periods. For example: collagen vascular disease,
liver cirrhosis, chronic lung disease and thromboembolism. The clinical symptoms and signs
exhibited by the patients of PH are Chronic Dyspnea, Hypoxemia, elevated tricuspid
regurgitation, Syncope, Arrhythmias, Cor Pulmonale and early death.
The sickle cell disease (SCD) patients have enhanced cardiac output due to anaemia. It is
observed that pulmonary vascular resistance and pulmonary pressures are higher in patients of
Sickle cell disease with Pulmonary Hypertension. Their cardiac output is also higher than the
normal range. These patients exhibit high rate of fatigue on exertion.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Project Dissertation 4
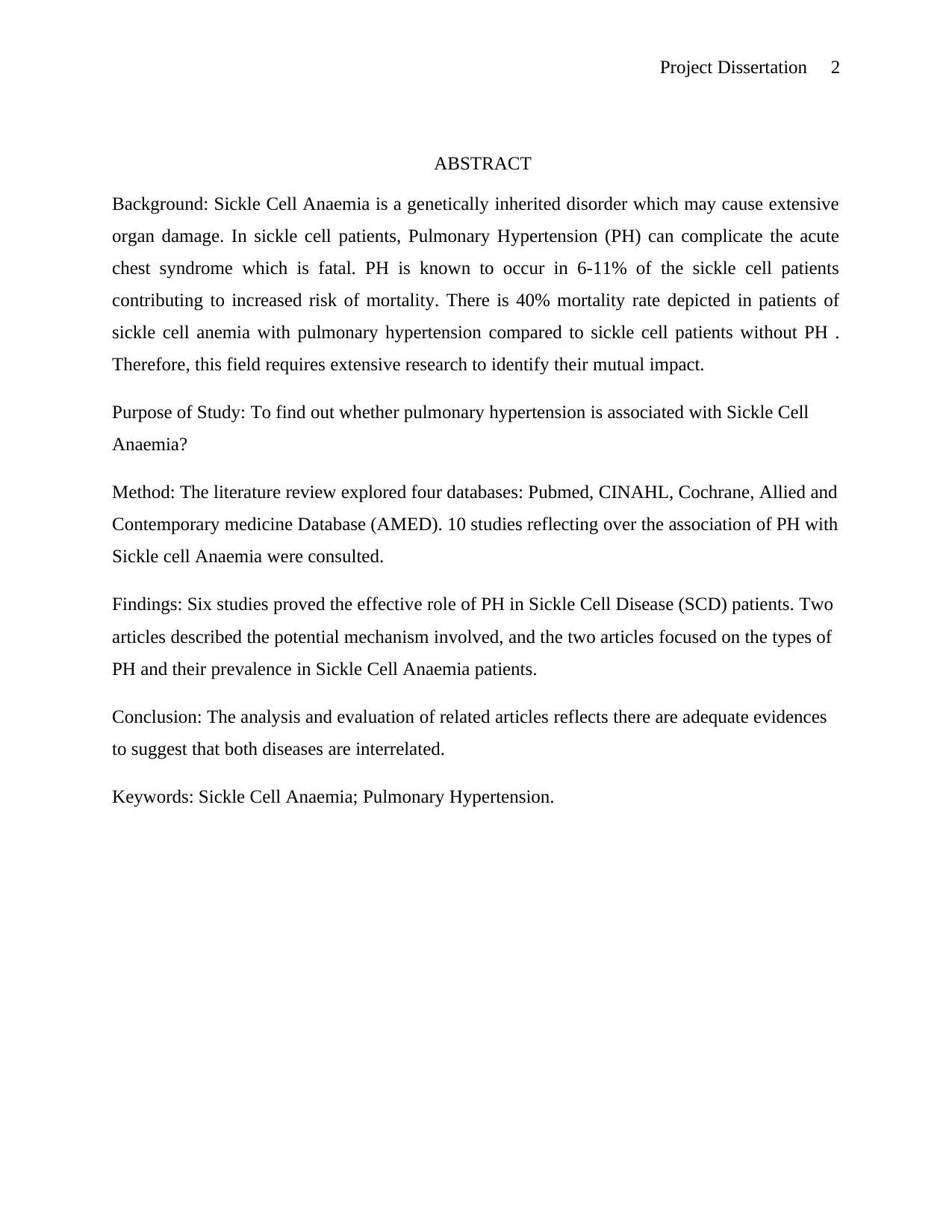
Haemodynamic
Measure
Normal Range Sickle Cell Patients
without PH
Sickle Cell Patients
with PH
Pulmonary Artery
Pressure
7 to 19 19+-45 36+-8
Cardiac Output 4.4 to 8.4 9+-3 8.6+-2
Pulmonary Vascular
Resistance
11-99 83+-46 205+-112
Table 1. Shows Comparison of Pulmonary Hemodynamic in Sickle Cell patients with PH
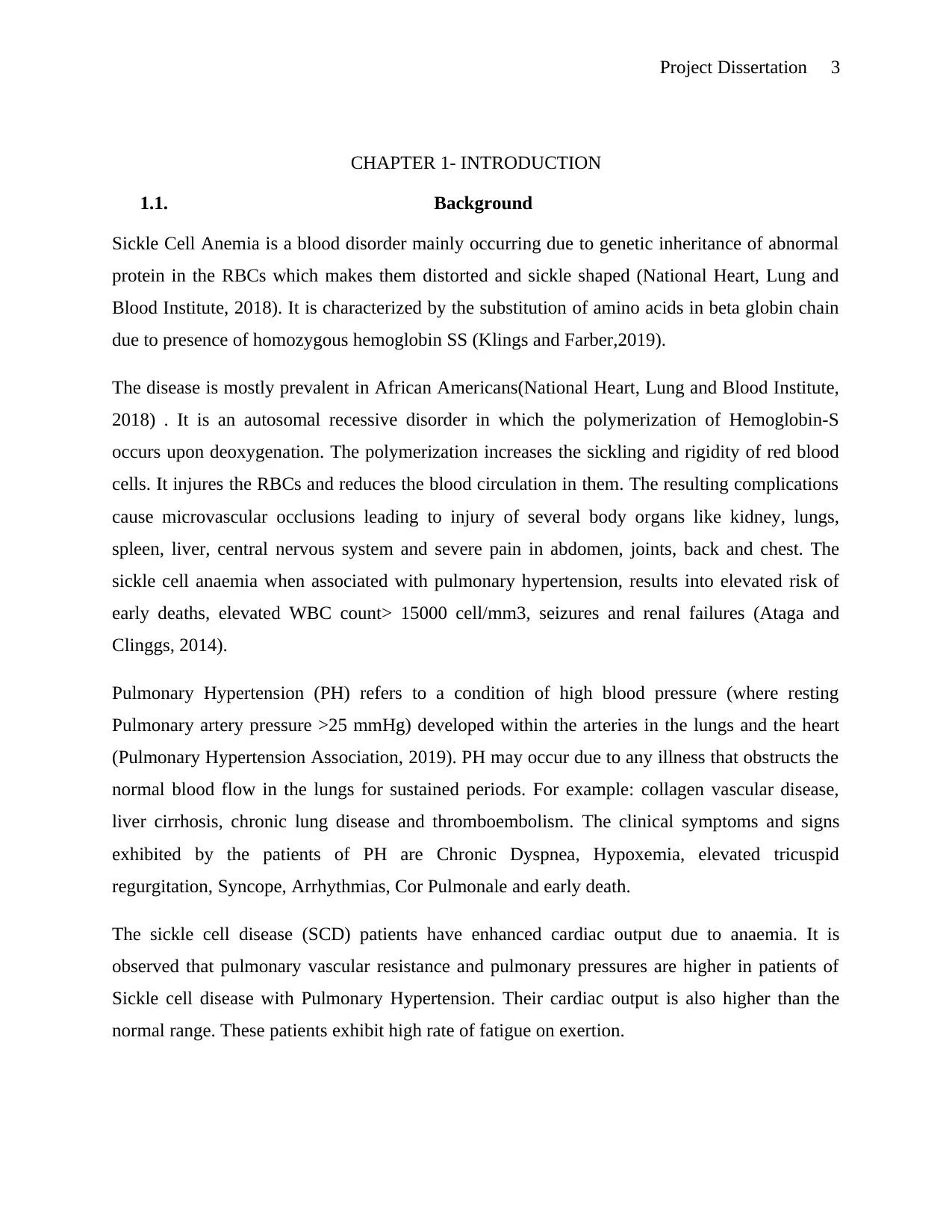
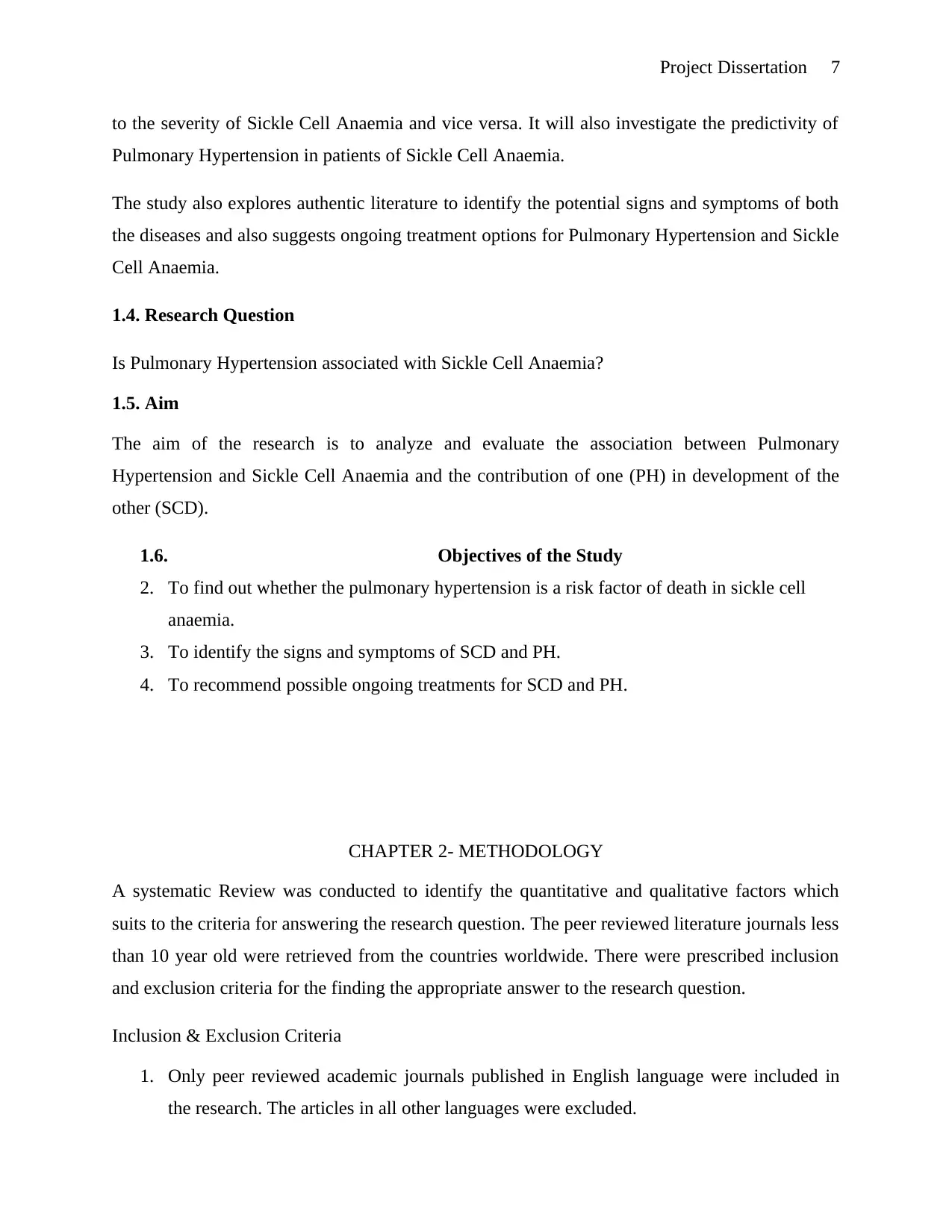
The SCD patients having PH have high mortality rate than the SCD patients without any PH. A
research by Castro colleagues in 2003 evaluated 34 adults who had undergone right heart
catheterization (Clarke, 2019). Initially, 20 of them had Pulmonary Hypertension. After a regular
follow up of 54 months, 11 out of 20 had died while only 3 patients died out of 14 having no
Pulmonary Hypertension (Clarke, 2019). The patients who died had a 10 mm Hg rise in their
mean Arterial pulmonary pressure leading to increase in rate of mortality.
Figure 1. Shows Kaplan Meier Survival in SCD patients with or without PH (Source: Clarke, 2019)
The upper red line in the graph shows the estimate survival of patients having Sickle cell disease,
without any PH. The blue line shows the estimate survival of the patients having Sickle Cell
Anaemia with PH. The time in months exhibited by X axis is the months of follow up post
catheterization of heart.
Haemodynamic
Measure
Normal Range Sickle Cell Patients
without PH
Sickle Cell Patients
with PH
Pulmonary Artery
Pressure
7 to 19 19+-45 36+-8
Cardiac Output 4.4 to 8.4 9+-3 8.6+-2
Pulmonary Vascular
Resistance
11-99 83+-46 205+-112
Table 1. Shows Comparison of Pulmonary Hemodynamic in Sickle Cell patients with PH
The SCD patients having PH have high mortality rate than the SCD patients without any PH. A
research by Castro colleagues in 2003 evaluated 34 adults who had undergone right heart
catheterization (Clarke, 2019). Initially, 20 of them had Pulmonary Hypertension. After a regular
follow up of 54 months, 11 out of 20 had died while only 3 patients died out of 14 having no
Pulmonary Hypertension (Clarke, 2019). The patients who died had a 10 mm Hg rise in their
mean Arterial pulmonary pressure leading to increase in rate of mortality.
Figure 1. Shows Kaplan Meier Survival in SCD patients with or without PH (Source: Clarke, 2019)
The upper red line in the graph shows the estimate survival of patients having Sickle cell disease,
without any PH. The blue line shows the estimate survival of the patients having Sickle Cell
Anaemia with PH. The time in months exhibited by X axis is the months of follow up post
catheterization of heart.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Project Dissertation 5
The prevalence of Pulmonary Hypertension increases in the patients of Sickle Cell Anaemia
with age. The prevalence is nearly 40% in the patients aged 40-49 years, while it is 55-60% in
the patients with age 50 years or more. According to NIH Howard Research published in 2004,
the risk factors for Pulmonary Hypertension in Sickle Cell Anaemia are history of cardiac or
renal diseases, systemic blood pressure, age, degree of hemolysis, cholestasis and iron overload
(Clarke, 2019). Such evidences show that the frequency of PH is increasing in the patients of
Sickle Cell Anaemia.
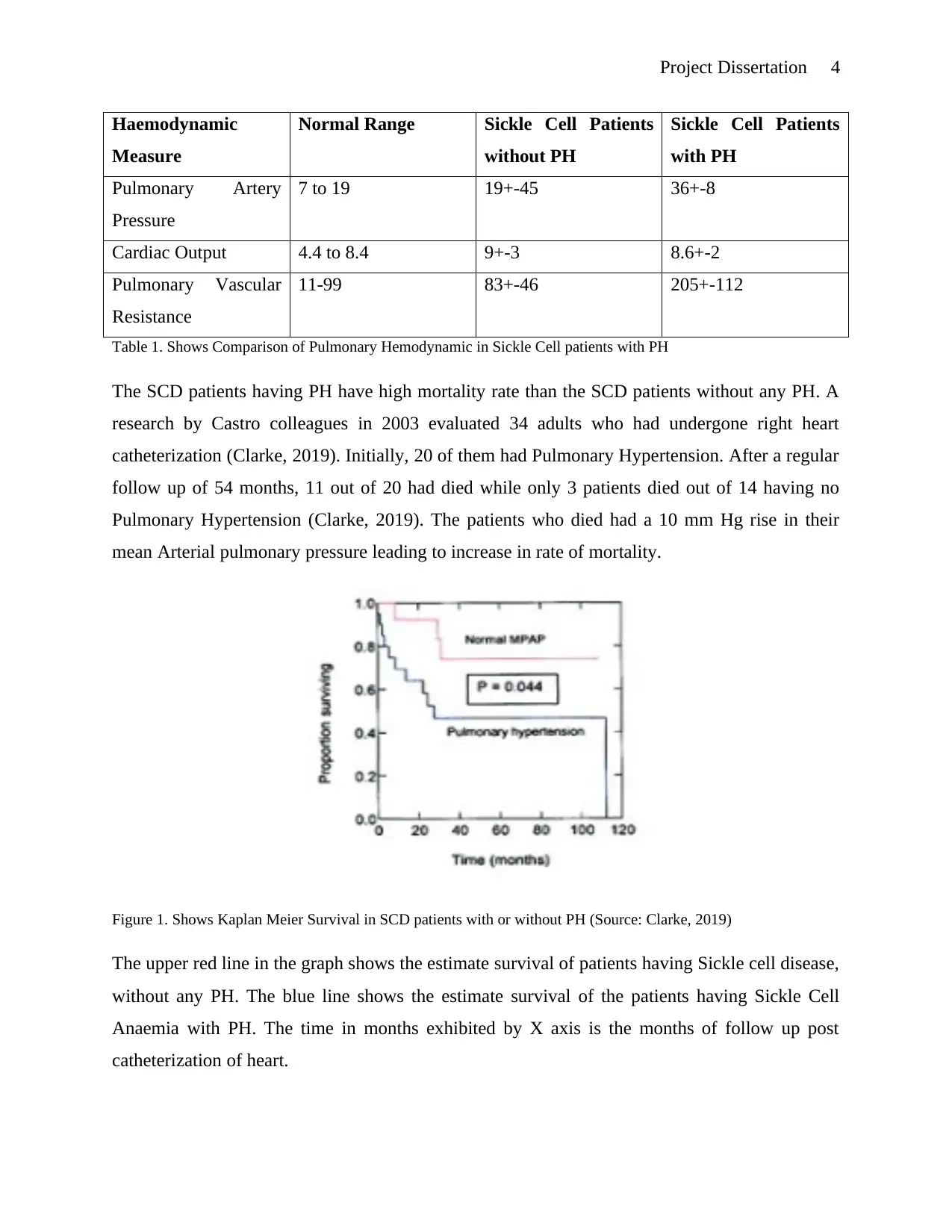
1.2 . Pathophysiology of Pulmonary Hypertension in patients of Sickle Cell Anaemia
Pathogenesis of Pulmonary Hypertension can be elaborated in patients of Sickle Cell Disease in
terms of several mechanisms such as Intravascular Hemolysis resulting into Nitric Oxide (NO)
deficiency, vasculopathy due to intimal thickening and platelet activation, interstitial fibrosis due
to ACS, hypoperfusion of pulmonary blood vessels of the lungs, in-situ thrombosis and recurrent
thromboembolic disease.
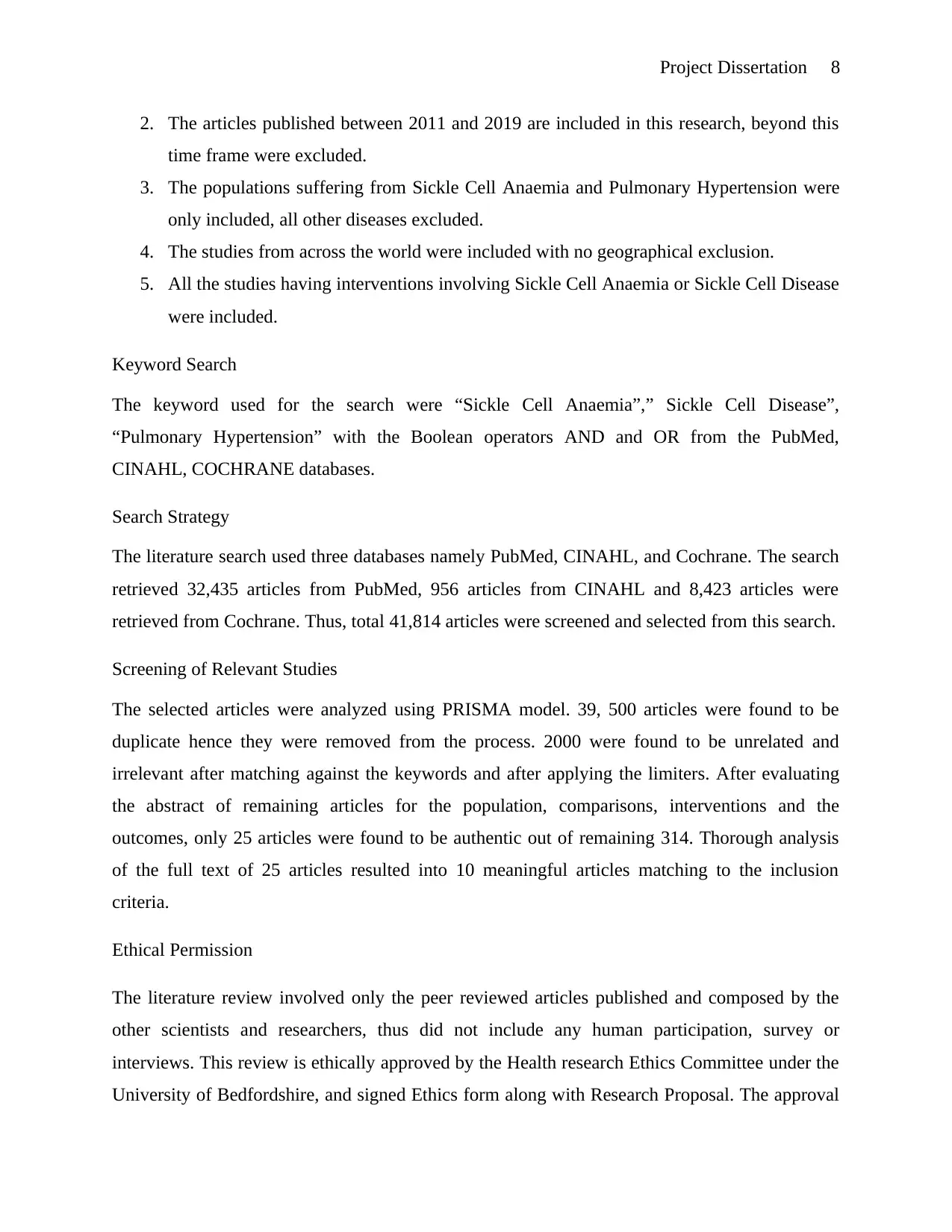
Nitric Oxide is produced by the NO Synthase (NOS) Enzymes which convert Arginine into the
Cittruline, while releasing NO in the process. NO produces cyclic Guanosine 3’5’
monophosphate (cGMP) in myocytes which vasodilates the myocyte wall (Clarke, 2019). In
Sickle Cell Disease, intravascular deficiency of Nitric Oxide leads to vasoconstriction of
pulmonary vessels.
Figure 2. Shows the factors involved in the release and inhibition of NO Radical. (Source: Clarke, 2019)
The prevalence of Pulmonary Hypertension increases in the patients of Sickle Cell Anaemia
with age. The prevalence is nearly 40% in the patients aged 40-49 years, while it is 55-60% in
the patients with age 50 years or more. According to NIH Howard Research published in 2004,
the risk factors for Pulmonary Hypertension in Sickle Cell Anaemia are history of cardiac or
renal diseases, systemic blood pressure, age, degree of hemolysis, cholestasis and iron overload
(Clarke, 2019). Such evidences show that the frequency of PH is increasing in the patients of
Sickle Cell Anaemia.
1.2 . Pathophysiology of Pulmonary Hypertension in patients of Sickle Cell Anaemia
Pathogenesis of Pulmonary Hypertension can be elaborated in patients of Sickle Cell Disease in
terms of several mechanisms such as Intravascular Hemolysis resulting into Nitric Oxide (NO)
deficiency, vasculopathy due to intimal thickening and platelet activation, interstitial fibrosis due
to ACS, hypoperfusion of pulmonary blood vessels of the lungs, in-situ thrombosis and recurrent
thromboembolic disease.
Nitric Oxide is produced by the NO Synthase (NOS) Enzymes which convert Arginine into the
Cittruline, while releasing NO in the process. NO produces cyclic Guanosine 3’5’
monophosphate (cGMP) in myocytes which vasodilates the myocyte wall (Clarke, 2019). In
Sickle Cell Disease, intravascular deficiency of Nitric Oxide leads to vasoconstriction of
pulmonary vessels.
Figure 2. Shows the factors involved in the release and inhibition of NO Radical. (Source: Clarke, 2019)
Project Dissertation 6
Low level of Arginine during the VOC, show depletion of substrates which further reduces the
production of Nitric Oxide (Clarke, 2019). All these factors contribute to the mechanism of
pulmonary hypertension.
Almost half of the patients of SCD having pulmonary hypertension exhibit: (1) a state of NO
deficiency; (2) Chronic pulmonary thrombo-embolism; (3) Microvascular obstruction, low
Oxygen Saturation, and hypoxic response to anaemia (Gordeuk, Castro and Machado, 2016).
The management of patients with SCD and PH is based on anticoagulation for the patients of
thromboembolism; treatment of failure of left ventricle in the patients of post capillary
pulmonary hypertension; oxygen therapy for the patients having low saturation level; and blood
transfusions to elevate the concentration of hemoglobin, to prevent the incidents of vaso-
occlusion and lower down the rate of hemolysis. These patients need to be sent to special centres
and should be treated with the therapies found effective in treating several other PH conditions.
Reports have found such treatments to be successful in several cases (Gordeuk, Castro and
Machado, 2016).
1.3. Significance of the Study
Not all the patients of sickle cell anaemia develop pulmonary hypertension however still the
people who are the patients of SCD are more likely to develop pulmonary hypertension. The
people who have both of these diseases are at high risk of death than the patients having only one
of them. According to Pulmonary Hypertension Studies (2019), about 75% of the SCD patients
develop changes in their lung tissues during death which indicates the presence of Pulmonary
Hypertension. Pulmonary Hypertension occurs in 6-11% of the SCD patients and is identified by
the WHO as having highly variable hemodynamics leading to premature deaths (Hayes, et al.
2014). The risk factors leading to the severity of disease are increasingly a concern for the
pulmonologists, cardiologists, hematologists and internists.
This study will explore the literature review less than 10 year old, to assess the potential
association between the two diseases and factors affecting the involvement of PH in contributing
Low level of Arginine during the VOC, show depletion of substrates which further reduces the
production of Nitric Oxide (Clarke, 2019). All these factors contribute to the mechanism of
pulmonary hypertension.
Almost half of the patients of SCD having pulmonary hypertension exhibit: (1) a state of NO
deficiency; (2) Chronic pulmonary thrombo-embolism; (3) Microvascular obstruction, low
Oxygen Saturation, and hypoxic response to anaemia (Gordeuk, Castro and Machado, 2016).
The management of patients with SCD and PH is based on anticoagulation for the patients of
thromboembolism; treatment of failure of left ventricle in the patients of post capillary
pulmonary hypertension; oxygen therapy for the patients having low saturation level; and blood
transfusions to elevate the concentration of hemoglobin, to prevent the incidents of vaso-
occlusion and lower down the rate of hemolysis. These patients need to be sent to special centres
and should be treated with the therapies found effective in treating several other PH conditions.
Reports have found such treatments to be successful in several cases (Gordeuk, Castro and
Machado, 2016).
1.3. Significance of the Study
Not all the patients of sickle cell anaemia develop pulmonary hypertension however still the
people who are the patients of SCD are more likely to develop pulmonary hypertension. The
people who have both of these diseases are at high risk of death than the patients having only one
of them. According to Pulmonary Hypertension Studies (2019), about 75% of the SCD patients
develop changes in their lung tissues during death which indicates the presence of Pulmonary
Hypertension. Pulmonary Hypertension occurs in 6-11% of the SCD patients and is identified by
the WHO as having highly variable hemodynamics leading to premature deaths (Hayes, et al.
2014). The risk factors leading to the severity of disease are increasingly a concern for the
pulmonologists, cardiologists, hematologists and internists.
This study will explore the literature review less than 10 year old, to assess the potential
association between the two diseases and factors affecting the involvement of PH in contributing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Project Dissertation 7
to the severity of Sickle Cell Anaemia and vice versa. It will also investigate the predictivity of
Pulmonary Hypertension in patients of Sickle Cell Anaemia.
The study also explores authentic literature to identify the potential signs and symptoms of both
the diseases and also suggests ongoing treatment options for Pulmonary Hypertension and Sickle
Cell Anaemia.
1.4. Research Question
Is Pulmonary Hypertension associated with Sickle Cell Anaemia?
1.5. Aim
The aim of the research is to analyze and evaluate the association between Pulmonary
Hypertension and Sickle Cell Anaemia and the contribution of one (PH) in development of the
other (SCD).
1.6. Objectives of the Study
2. To find out whether the pulmonary hypertension is a risk factor of death in sickle cell
anaemia.
3. To identify the signs and symptoms of SCD and PH.
4. To recommend possible ongoing treatments for SCD and PH.
CHAPTER 2- METHODOLOGY
A systematic Review was conducted to identify the quantitative and qualitative factors which
suits to the criteria for answering the research question. The peer reviewed literature journals less
than 10 year old were retrieved from the countries worldwide. There were prescribed inclusion
and exclusion criteria for the finding the appropriate answer to the research question.
Inclusion & Exclusion Criteria
1. Only peer reviewed academic journals published in English language were included in
the research. The articles in all other languages were excluded.
to the severity of Sickle Cell Anaemia and vice versa. It will also investigate the predictivity of
Pulmonary Hypertension in patients of Sickle Cell Anaemia.
The study also explores authentic literature to identify the potential signs and symptoms of both
the diseases and also suggests ongoing treatment options for Pulmonary Hypertension and Sickle
Cell Anaemia.
1.4. Research Question
Is Pulmonary Hypertension associated with Sickle Cell Anaemia?
1.5. Aim
The aim of the research is to analyze and evaluate the association between Pulmonary
Hypertension and Sickle Cell Anaemia and the contribution of one (PH) in development of the
other (SCD).
1.6. Objectives of the Study
2. To find out whether the pulmonary hypertension is a risk factor of death in sickle cell
anaemia.
3. To identify the signs and symptoms of SCD and PH.
4. To recommend possible ongoing treatments for SCD and PH.
CHAPTER 2- METHODOLOGY
A systematic Review was conducted to identify the quantitative and qualitative factors which
suits to the criteria for answering the research question. The peer reviewed literature journals less
than 10 year old were retrieved from the countries worldwide. There were prescribed inclusion
and exclusion criteria for the finding the appropriate answer to the research question.
Inclusion & Exclusion Criteria
1. Only peer reviewed academic journals published in English language were included in
the research. The articles in all other languages were excluded.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Project Dissertation 8
2. The articles published between 2011 and 2019 are included in this research, beyond this
time frame were excluded.
3. The populations suffering from Sickle Cell Anaemia and Pulmonary Hypertension were
only included, all other diseases excluded.
4. The studies from across the world were included with no geographical exclusion.
5. All the studies having interventions involving Sickle Cell Anaemia or Sickle Cell Disease
were included.
Keyword Search
The keyword used for the search were “Sickle Cell Anaemia”,” Sickle Cell Disease”,
“Pulmonary Hypertension” with the Boolean operators AND and OR from the PubMed,
CINAHL, COCHRANE databases.
Search Strategy
The literature search used three databases namely PubMed, CINAHL, and Cochrane. The search
retrieved 32,435 articles from PubMed, 956 articles from CINAHL and 8,423 articles were
retrieved from Cochrane. Thus, total 41,814 articles were screened and selected from this search.
Screening of Relevant Studies
The selected articles were analyzed using PRISMA model. 39, 500 articles were found to be
duplicate hence they were removed from the process. 2000 were found to be unrelated and
irrelevant after matching against the keywords and after applying the limiters. After evaluating
the abstract of remaining articles for the population, comparisons, interventions and the
outcomes, only 25 articles were found to be authentic out of remaining 314. Thorough analysis
of the full text of 25 articles resulted into 10 meaningful articles matching to the inclusion
criteria.
Ethical Permission
The literature review involved only the peer reviewed articles published and composed by the
other scientists and researchers, thus did not include any human participation, survey or
interviews. This review is ethically approved by the Health research Ethics Committee under the
University of Bedfordshire, and signed Ethics form along with Research Proposal. The approval
2. The articles published between 2011 and 2019 are included in this research, beyond this
time frame were excluded.
3. The populations suffering from Sickle Cell Anaemia and Pulmonary Hypertension were
only included, all other diseases excluded.
4. The studies from across the world were included with no geographical exclusion.
5. All the studies having interventions involving Sickle Cell Anaemia or Sickle Cell Disease
were included.
Keyword Search
The keyword used for the search were “Sickle Cell Anaemia”,” Sickle Cell Disease”,
“Pulmonary Hypertension” with the Boolean operators AND and OR from the PubMed,
CINAHL, COCHRANE databases.
Search Strategy
The literature search used three databases namely PubMed, CINAHL, and Cochrane. The search
retrieved 32,435 articles from PubMed, 956 articles from CINAHL and 8,423 articles were
retrieved from Cochrane. Thus, total 41,814 articles were screened and selected from this search.
Screening of Relevant Studies
The selected articles were analyzed using PRISMA model. 39, 500 articles were found to be
duplicate hence they were removed from the process. 2000 were found to be unrelated and
irrelevant after matching against the keywords and after applying the limiters. After evaluating
the abstract of remaining articles for the population, comparisons, interventions and the
outcomes, only 25 articles were found to be authentic out of remaining 314. Thorough analysis
of the full text of 25 articles resulted into 10 meaningful articles matching to the inclusion
criteria.
Ethical Permission
The literature review involved only the peer reviewed articles published and composed by the
other scientists and researchers, thus did not include any human participation, survey or
interviews. This review is ethically approved by the Health research Ethics Committee under the
University of Bedfordshire, and signed Ethics form along with Research Proposal. The approval
Project Dissertation 9
also ensures that the research should be free from plagiarism, misconduct, falsification or
fabrication of results. It should support research integrity and confidentiality.
The permission was granted to carry out this research through BREO Feedback.
CHAPTER 3- RESULTS
3.1 Summary of Findings
The findings of the literature review will be enlisted in this section in form of a table for effective
presentation of the explored facts.
also ensures that the research should be free from plagiarism, misconduct, falsification or
fabrication of results. It should support research integrity and confidentiality.
The permission was granted to carry out this research through BREO Feedback.
CHAPTER 3- RESULTS
3.1 Summary of Findings
The findings of the literature review will be enlisted in this section in form of a table for effective
presentation of the explored facts.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
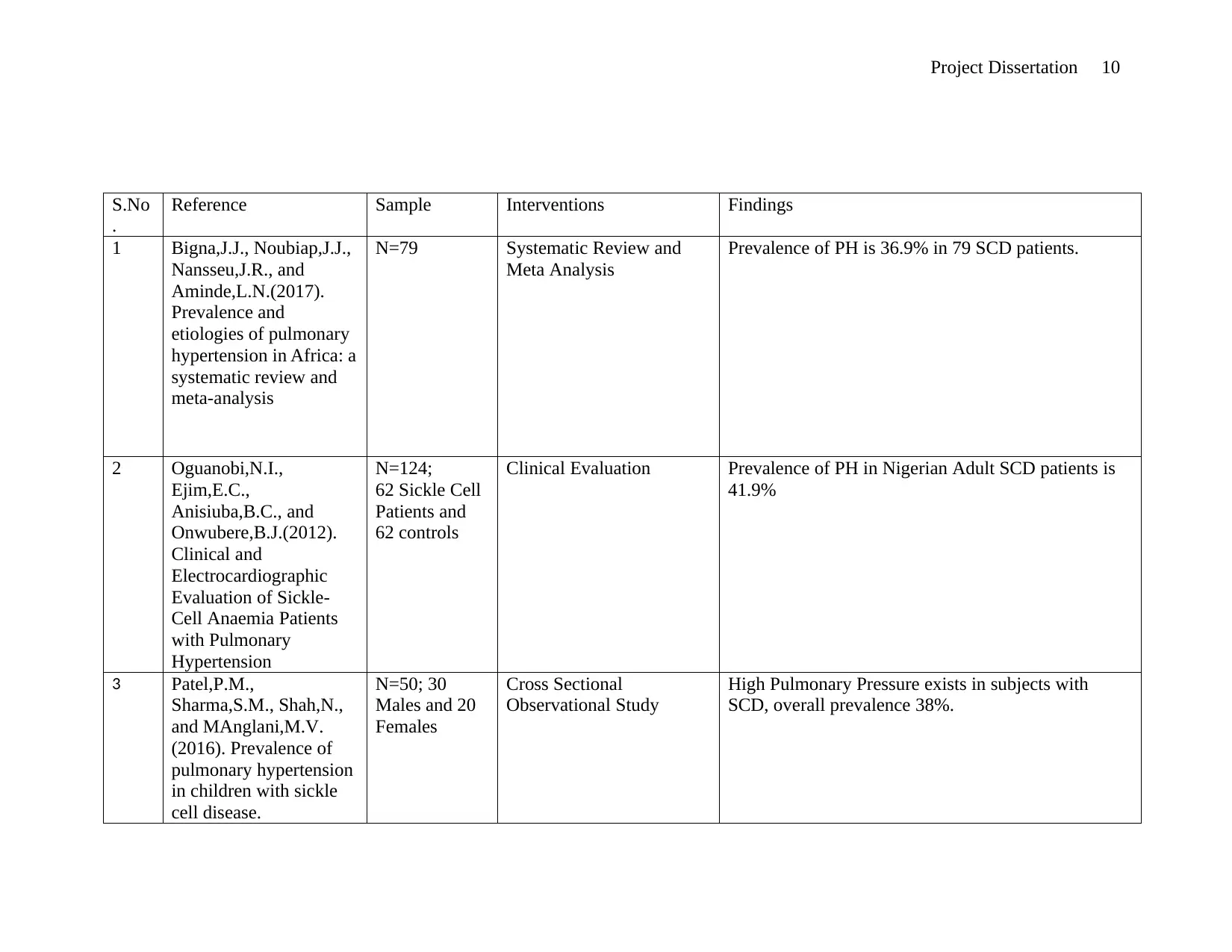
Project Dissertation 10
S.No
.
Reference Sample Interventions Findings
1 Bigna,J.J., Noubiap,J.J.,
Nansseu,J.R., and
Aminde,L.N.(2017).
Prevalence and
etiologies of pulmonary
hypertension in Africa: a
systematic review and
meta-analysis
N=79 Systematic Review and
Meta Analysis
Prevalence of PH is 36.9% in 79 SCD patients.
2 Oguanobi,N.I.,
Ejim,E.C.,
Anisiuba,B.C., and
Onwubere,B.J.(2012).
Clinical and
Electrocardiographic
Evaluation of Sickle-
Cell Anaemia Patients
with Pulmonary
Hypertension
N=124;
62 Sickle Cell
Patients and
62 controls
Clinical Evaluation Prevalence of PH in Nigerian Adult SCD patients is
41.9%
3 Patel,P.M.,
Sharma,S.M., Shah,N.,
and MAnglani,M.V.
(2016). Prevalence of
pulmonary hypertension
in children with sickle
cell disease.
N=50; 30
Males and 20
Females
Cross Sectional
Observational Study
High Pulmonary Pressure exists in subjects with
SCD, overall prevalence 38%.
S.No
.
Reference Sample Interventions Findings
1 Bigna,J.J., Noubiap,J.J.,
Nansseu,J.R., and
Aminde,L.N.(2017).
Prevalence and
etiologies of pulmonary
hypertension in Africa: a
systematic review and
meta-analysis
N=79 Systematic Review and
Meta Analysis
Prevalence of PH is 36.9% in 79 SCD patients.
2 Oguanobi,N.I.,
Ejim,E.C.,
Anisiuba,B.C., and
Onwubere,B.J.(2012).
Clinical and
Electrocardiographic
Evaluation of Sickle-
Cell Anaemia Patients
with Pulmonary
Hypertension
N=124;
62 Sickle Cell
Patients and
62 controls
Clinical Evaluation Prevalence of PH in Nigerian Adult SCD patients is
41.9%
3 Patel,P.M.,
Sharma,S.M., Shah,N.,
and MAnglani,M.V.
(2016). Prevalence of
pulmonary hypertension
in children with sickle
cell disease.
N=50; 30
Males and 20
Females
Cross Sectional
Observational Study
High Pulmonary Pressure exists in subjects with
SCD, overall prevalence 38%.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
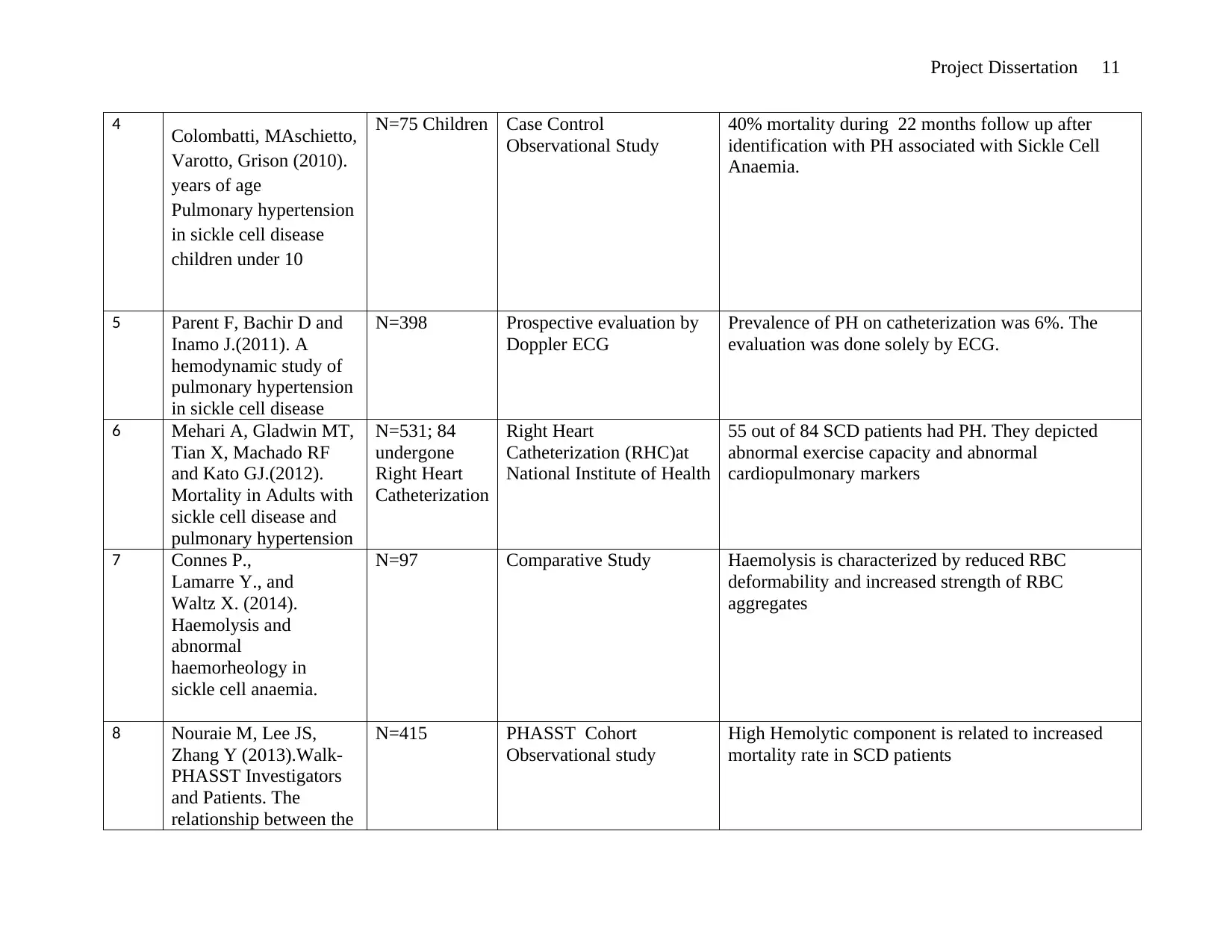
Project Dissertation 11
4 Colombatti, MAschietto,
Varotto, Grison (2010).
years of age
Pulmonary hypertension
in sickle cell disease
children under 10
N=75 Children Case Control
Observational Study
40% mortality during 22 months follow up after
identification with PH associated with Sickle Cell
Anaemia.
5 Parent F, Bachir D and
Inamo J.(2011). A
hemodynamic study of
pulmonary hypertension
in sickle cell disease
N=398 Prospective evaluation by
Doppler ECG
Prevalence of PH on catheterization was 6%. The
evaluation was done solely by ECG.
6 Mehari A, Gladwin MT,
Tian X, Machado RF
and Kato GJ.(2012).
Mortality in Adults with
sickle cell disease and
pulmonary hypertension
N=531; 84
undergone
Right Heart
Catheterization
Right Heart
Catheterization (RHC)at
National Institute of Health
55 out of 84 SCD patients had PH. They depicted
abnormal exercise capacity and abnormal
cardiopulmonary markers
7 Connes P.,
Lamarre Y., and
Waltz X. (2014).
Haemolysis and
abnormal
haemorheology in
sickle cell anaemia.
N=97 Comparative Study Haemolysis is characterized by reduced RBC
deformability and increased strength of RBC
aggregates
8 Nouraie M, Lee JS,
Zhang Y (2013).Walk-
PHASST Investigators
and Patients. The
relationship between the
N=415 PHASST Cohort
Observational study
High Hemolytic component is related to increased
mortality rate in SCD patients
4 Colombatti, MAschietto,
Varotto, Grison (2010).
years of age
Pulmonary hypertension
in sickle cell disease
children under 10
N=75 Children Case Control
Observational Study
40% mortality during 22 months follow up after
identification with PH associated with Sickle Cell
Anaemia.
5 Parent F, Bachir D and
Inamo J.(2011). A
hemodynamic study of
pulmonary hypertension
in sickle cell disease
N=398 Prospective evaluation by
Doppler ECG
Prevalence of PH on catheterization was 6%. The
evaluation was done solely by ECG.
6 Mehari A, Gladwin MT,
Tian X, Machado RF
and Kato GJ.(2012).
Mortality in Adults with
sickle cell disease and
pulmonary hypertension
N=531; 84
undergone
Right Heart
Catheterization
Right Heart
Catheterization (RHC)at
National Institute of Health
55 out of 84 SCD patients had PH. They depicted
abnormal exercise capacity and abnormal
cardiopulmonary markers
7 Connes P.,
Lamarre Y., and
Waltz X. (2014).
Haemolysis and
abnormal
haemorheology in
sickle cell anaemia.
N=97 Comparative Study Haemolysis is characterized by reduced RBC
deformability and increased strength of RBC
aggregates
8 Nouraie M, Lee JS,
Zhang Y (2013).Walk-
PHASST Investigators
and Patients. The
relationship between the
N=415 PHASST Cohort
Observational study
High Hemolytic component is related to increased
mortality rate in SCD patients
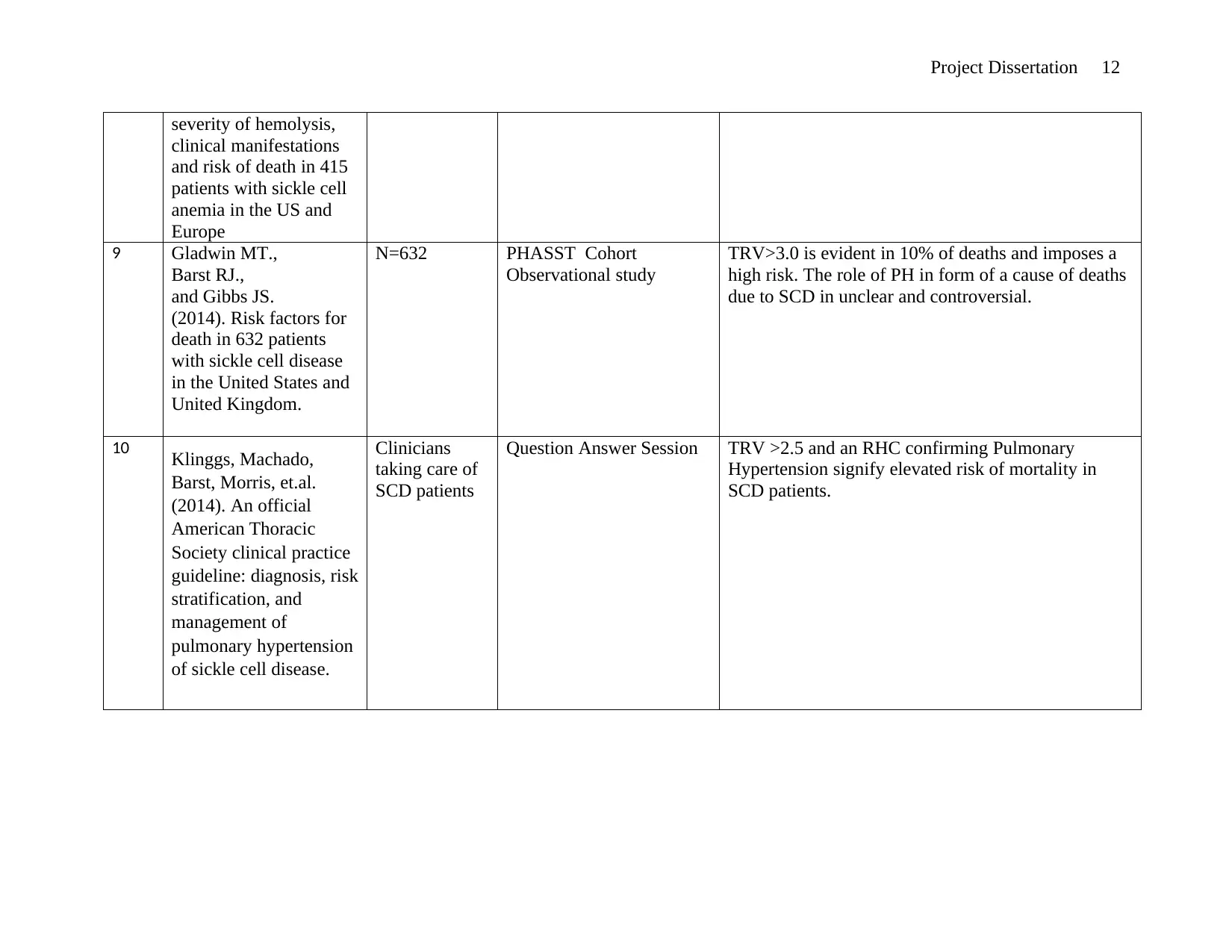
Project Dissertation 12
severity of hemolysis,
clinical manifestations
and risk of death in 415
patients with sickle cell
anemia in the US and
Europe
9 Gladwin MT.,
Barst RJ.,
and Gibbs JS.
(2014). Risk factors for
death in 632 patients
with sickle cell disease
in the United States and
United Kingdom.
N=632 PHASST Cohort
Observational study
TRV>3.0 is evident in 10% of deaths and imposes a
high risk. The role of PH in form of a cause of deaths
due to SCD in unclear and controversial.
10 Klinggs, Machado,
Barst, Morris, et.al.
(2014). An official
American Thoracic
Society clinical practice
guideline: diagnosis, risk
stratification, and
management of
pulmonary hypertension
of sickle cell disease.
Clinicians
taking care of
SCD patients
Question Answer Session TRV >2.5 and an RHC confirming Pulmonary
Hypertension signify elevated risk of mortality in
SCD patients.
severity of hemolysis,
clinical manifestations
and risk of death in 415
patients with sickle cell
anemia in the US and
Europe
9 Gladwin MT.,
Barst RJ.,
and Gibbs JS.
(2014). Risk factors for
death in 632 patients
with sickle cell disease
in the United States and
United Kingdom.
N=632 PHASST Cohort
Observational study
TRV>3.0 is evident in 10% of deaths and imposes a
high risk. The role of PH in form of a cause of deaths
due to SCD in unclear and controversial.
10 Klinggs, Machado,
Barst, Morris, et.al.
(2014). An official
American Thoracic
Society clinical practice
guideline: diagnosis, risk
stratification, and
management of
pulmonary hypertension
of sickle cell disease.
Clinicians
taking care of
SCD patients
Question Answer Session TRV >2.5 and an RHC confirming Pulmonary
Hypertension signify elevated risk of mortality in
SCD patients.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 27
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





