HMSV3503 Qualitative Research Study Review: Health and Human Services
VerifiedAdded on 2022/08/26
|11
|10373
|23
Report
AI Summary
This report provides a comprehensive review of a qualitative research study by Broad et al. (2017), focusing on the experiences of young people transitioning from Child and Adolescent Mental Health Services (CAMHS) to Adult Mental Health Services (AMHS). The study, involving 18 articles and 253 unique service-users, utilized thematic synthesis to analyze the perspectives of youth, highlighting the challenges and opportunities associated with this transition. Key findings revealed that youth value preparation, flexible timing, individualized plans, and continuity in care. The analysis underscores the significant cultural shift between CAMHS and AMHS and emphasizes the need for individualized and flexible approaches to transition, incorporating youth perspectives for service improvement. The study also discusses the importance of research in healthcare for evidence-based practice, problem identification, and decision-making capabilities, ultimately improving patient care and outcomes. The report also outlines the key components of the research process and the ethical considerations involved in research.
R E S E A R C H A R T I C L E Open Access
Youth experiences of transition from child
mentalhealth services to adult mental
health services:a qualitative thematic
synthesis
Kathleen L.Broad1
, Vijay K.Sandhu2
, Nadiya Sunderji3,4,5*
and Alice Charach6,7
Abstract
Background:Adolescence and young adulthood is a vulnerable time during which young people experience
development milestones,as well as an increased incidence of mental illness.During this time,youth also transition
between Child and Adolescent Mental Health Services (CAMHS) to Adult Mental Health Services (AMHS).This transition
puts many youth at risk of disengagement from service use;however,our understanding of this transition from
the perspective of youth is limited.This systematic review aims to provide a more comprehensive understanding
of youth experiences of transition from CAMHS to AMHS,through a qualitative thematic synthesis of the extant
literature in this area.
Method:Published and unpublished literature was searched using keywords targeting three subject areas:Transition,
Age and Mental Health.Studies were included if they qualitatively explored the perceptions and experiences of
who received mental health services in both CAMHS and AMHS.There were no limitations on diagnosis or age of
youth.Studies examining youth with chronic physical health conditions were excluded.
Results: Eighteen studies,representing 14 datasets and the experiences of 253 unique service-users were includ
Youth experiences of moving from CAMHS and AMHS are influenced by concurrent life transitions and thei
preferences regarding autonomy and independence.Youth identified preparation,flexible transition timing,
individualized transition plans,and informationalcontinuity as positive factors during transition.Youth also valued
joint working and relationalcontinuity between CAMHS and AMHS.
Conclusions:Youth experience a dramatic culture shift between CAMHS and AMHS,which can be mitigated by
individualized and flexible approaches to transition.Youth have valuable perspectives to guide the intelligent
design of mental health services and their perspectives should be used to inform tools to evaluate and inc
youth perspectives into transitional service improvement.
Trial registration: Clinical Trial or Systematic Review Registry:PROSPERO International Prospective Register of
Systematic Reviews CRD42014013799.
Keywords: Transition to adult care,Transitional programs,Health transition,Continuum of care,Adolescent,Young
adult,Child adolescent psychiatry,Adolescent health services,Mental disorders,Mental health services
* Correspondence:sunderjin@smh.ca
3MentalHealth and Addictions Service,St.Michael’s Hospital,Toronto,ON,
Canada
4Li Ka Shing Knowledge Institute,Toronto,ON,Canada
Fulllist of author information is available at the end of the article
© The Author(s).2017 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,unless otherwise stated.
Broad et al.BMC Psychiatry (2017) 17:380
DOI10.1186/s12888-017-1538-1
Youth experiences of transition from child
mentalhealth services to adult mental
health services:a qualitative thematic
synthesis
Kathleen L.Broad1
, Vijay K.Sandhu2
, Nadiya Sunderji3,4,5*
and Alice Charach6,7
Abstract
Background:Adolescence and young adulthood is a vulnerable time during which young people experience
development milestones,as well as an increased incidence of mental illness.During this time,youth also transition
between Child and Adolescent Mental Health Services (CAMHS) to Adult Mental Health Services (AMHS).This transition
puts many youth at risk of disengagement from service use;however,our understanding of this transition from
the perspective of youth is limited.This systematic review aims to provide a more comprehensive understanding
of youth experiences of transition from CAMHS to AMHS,through a qualitative thematic synthesis of the extant
literature in this area.
Method:Published and unpublished literature was searched using keywords targeting three subject areas:Transition,
Age and Mental Health.Studies were included if they qualitatively explored the perceptions and experiences of
who received mental health services in both CAMHS and AMHS.There were no limitations on diagnosis or age of
youth.Studies examining youth with chronic physical health conditions were excluded.
Results: Eighteen studies,representing 14 datasets and the experiences of 253 unique service-users were includ
Youth experiences of moving from CAMHS and AMHS are influenced by concurrent life transitions and thei
preferences regarding autonomy and independence.Youth identified preparation,flexible transition timing,
individualized transition plans,and informationalcontinuity as positive factors during transition.Youth also valued
joint working and relationalcontinuity between CAMHS and AMHS.
Conclusions:Youth experience a dramatic culture shift between CAMHS and AMHS,which can be mitigated by
individualized and flexible approaches to transition.Youth have valuable perspectives to guide the intelligent
design of mental health services and their perspectives should be used to inform tools to evaluate and inc
youth perspectives into transitional service improvement.
Trial registration: Clinical Trial or Systematic Review Registry:PROSPERO International Prospective Register of
Systematic Reviews CRD42014013799.
Keywords: Transition to adult care,Transitional programs,Health transition,Continuum of care,Adolescent,Young
adult,Child adolescent psychiatry,Adolescent health services,Mental disorders,Mental health services
* Correspondence:sunderjin@smh.ca
3MentalHealth and Addictions Service,St.Michael’s Hospital,Toronto,ON,
Canada
4Li Ka Shing Knowledge Institute,Toronto,ON,Canada
Fulllist of author information is available at the end of the article
© The Author(s).2017 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,unless otherwise stated.
Broad et al.BMC Psychiatry (2017) 17:380
DOI10.1186/s12888-017-1538-1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Background
At least 75% ofmentalhealth problems and illness have
onset in childhood,adolescence,or young adulthood [1].
However,this increased incidence of mental health condi-
tionsin youth correspondsto a weak pointin mental
health care provision [2].The transition from Child and
AdolescentMentalHealth Services (CAMHS)to Adult
Mental Health Services (AMHS) typically occurs between
18 and 21 years according to traditional age boundaries of
service provision organizations,a period that overlaps im-
portant development milestones for emerging adults [3].
This is a vulnerable period [4] during which service users
may disengage from utilizing mentalhealth servicesat
higher rates than other age cohorts [5, 6].
Many factors may contribute to youth disengagement,
including disease-specific ambivalence ordenial[7, 8]
and the potentialfor mentalillness and/or addictions to
interfere with functioning and with acceptance of formal
supports [9,10].It has also been postulated that differ-
ences betweenCAMHS and AMHS servicesmay
contribute to high disengagementrates [11].However,
overallfactors contributing to disengagement,especially
from the perspective of youth remain poorly understood.
Even when youth do receive care in AMHS,only 23%
report finding the service helpful [12].Gaps and subopti-
malcare during this vulnerable time have the potential
for lasting functionalimpairmentand development
derailment[13, 14]. Age-specificoutpatientprograms
have been shown to increasementalhealth service
utilization,compared to standard adultoutpatientpro-
grams[15];however,they lack consistentevidence of
effectiveness [16].Given the vulnerability ofthis period
and the unique needs of transition-aged youth,it is cru-
cialto further understand youth experiences during the
transition from CAMHS to AMHS.
Previoussystematicreviewshaveshown thatyoung
people transitioning to adulthealth services experience
concern over a loss of familiar surroundings and relation-
ships [17] and want providers to be sensitive to their di-
verse needs [18].Personalaccounts from youth [19] and
stakeholders [20, 21] have emphasized the need to directly
involve young adults in the development of mental health
services.Existing literature reviews ofservice transitions
for youth with mental health concerns have identified gaps
in the provision of transitionalcare [22],however,few of
the includedstudiesexaminedthe experiencesand
perspectives ofyouth [23–25].Thus,the youth voice in
mentalhealth planning and service deliveryis under-
represented, and their subjective experiences of transition-
ing from CMHS to AMHS are insufficiently understood.
Our primary aim is to understand and describe the sub-
jective experiences ofyoung people with mentalhealth
problems as they transition from the child and adolescent
services to adult mental health services.This information
will be helpful in planning services to address the needs of
youth transitioning between service systems.
Methods
In this systematic review,we examined youth experi-
ences as they transition from CAMHS to AMHS.The
scope was international,and focusedon qualitative
materialbecausequalitativestudiesenablerich and
open-ended exploration ofsubjective experiences.Such
reviewshave the advantageof providinga greater
breadth and depth ofunderstanding by accessing a lar-
ger number and diversity of service users accounts and a
greaterrangeof methodologiesto elicit and analyze
these accounts [26].This review was designed as a the-
matic synthesis [27],a method thatadapts approaches
from both meta-ethnography and grounded theory and
has been used in severalsystematic reviews examining
people’s perspectives [26,28].Thematic synthesis allows
our analysisto “stay close”to the expressed viewsof
youth in the primary studies and retain particularities,
while also allowing development ofhigher levelthemes
occurringacrossmultiplestudy populationsto offer
both cumulative and novelinterpretations ofthe find-
ings from primary studies as a whole [27].Thus, by being
interpretative and not merely aggregative, this type of syn-
thesis can reduce uncertainty (e.g.in the case of recurrent
themes across studies) and also enhance complexity (e.g.
by highlighting differences and discrepancies) [29].
This review followed the “Enhancing Transparency in
Reporting the Synthesisof QualitativeResearch”
(ENTREQ) guidelines[29] (See Additionalfile 1 for
ENTREQ checklist) and consisted of (1) a systematic lit-
erature search for relevant qualitative and mixed methods
research reports;(2) criticalappraisalof included reports;
and (3) inductive and iterative analysis of included reports.
The protocolfor this thematic synthesis was published a
prioriwith PROSPERO Internationalprospective register
of systematicreviews (availableonline at http://
www.crd.york.ac.uk/prospero/display_record.asp?ID=CRD
42014013799; registration number CRD42014013799).
Search strategy
We searched both published and unpublished (“grey”)
literature.We identified published articles through sys-
tematic searchesof the following electronic databases
for academic journals from inception to October 2014:
MEDLINE, EMBASE, PsycINFO, CINAHL, Social
Services Abstracts,Applied SocialSciences Indexes and
Abstracts (ASSIA);and ofthe following evidence-based
medicine databases:The Cochrane database ofsystem-
atic reviews,EBM Reviews, The Campbell Collaboration,
and Centre for Reviews and Dissemination.A systematic
search strategy was developed with the assistance ofa
Broad et al.BMC Psychiatry (2017) 17:380 Page 2 of 11
At least 75% ofmentalhealth problems and illness have
onset in childhood,adolescence,or young adulthood [1].
However,this increased incidence of mental health condi-
tionsin youth correspondsto a weak pointin mental
health care provision [2].The transition from Child and
AdolescentMentalHealth Services (CAMHS)to Adult
Mental Health Services (AMHS) typically occurs between
18 and 21 years according to traditional age boundaries of
service provision organizations,a period that overlaps im-
portant development milestones for emerging adults [3].
This is a vulnerable period [4] during which service users
may disengage from utilizing mentalhealth servicesat
higher rates than other age cohorts [5, 6].
Many factors may contribute to youth disengagement,
including disease-specific ambivalence ordenial[7, 8]
and the potentialfor mentalillness and/or addictions to
interfere with functioning and with acceptance of formal
supports [9,10].It has also been postulated that differ-
ences betweenCAMHS and AMHS servicesmay
contribute to high disengagementrates [11].However,
overallfactors contributing to disengagement,especially
from the perspective of youth remain poorly understood.
Even when youth do receive care in AMHS,only 23%
report finding the service helpful [12].Gaps and subopti-
malcare during this vulnerable time have the potential
for lasting functionalimpairmentand development
derailment[13, 14]. Age-specificoutpatientprograms
have been shown to increasementalhealth service
utilization,compared to standard adultoutpatientpro-
grams[15];however,they lack consistentevidence of
effectiveness [16].Given the vulnerability ofthis period
and the unique needs of transition-aged youth,it is cru-
cialto further understand youth experiences during the
transition from CAMHS to AMHS.
Previoussystematicreviewshaveshown thatyoung
people transitioning to adulthealth services experience
concern over a loss of familiar surroundings and relation-
ships [17] and want providers to be sensitive to their di-
verse needs [18].Personalaccounts from youth [19] and
stakeholders [20, 21] have emphasized the need to directly
involve young adults in the development of mental health
services.Existing literature reviews ofservice transitions
for youth with mental health concerns have identified gaps
in the provision of transitionalcare [22],however,few of
the includedstudiesexaminedthe experiencesand
perspectives ofyouth [23–25].Thus,the youth voice in
mentalhealth planning and service deliveryis under-
represented, and their subjective experiences of transition-
ing from CMHS to AMHS are insufficiently understood.
Our primary aim is to understand and describe the sub-
jective experiences ofyoung people with mentalhealth
problems as they transition from the child and adolescent
services to adult mental health services.This information
will be helpful in planning services to address the needs of
youth transitioning between service systems.
Methods
In this systematic review,we examined youth experi-
ences as they transition from CAMHS to AMHS.The
scope was international,and focusedon qualitative
materialbecausequalitativestudiesenablerich and
open-ended exploration ofsubjective experiences.Such
reviewshave the advantageof providinga greater
breadth and depth ofunderstanding by accessing a lar-
ger number and diversity of service users accounts and a
greaterrangeof methodologiesto elicit and analyze
these accounts [26].This review was designed as a the-
matic synthesis [27],a method thatadapts approaches
from both meta-ethnography and grounded theory and
has been used in severalsystematic reviews examining
people’s perspectives [26,28].Thematic synthesis allows
our analysisto “stay close”to the expressed viewsof
youth in the primary studies and retain particularities,
while also allowing development ofhigher levelthemes
occurringacrossmultiplestudy populationsto offer
both cumulative and novelinterpretations ofthe find-
ings from primary studies as a whole [27].Thus, by being
interpretative and not merely aggregative, this type of syn-
thesis can reduce uncertainty (e.g.in the case of recurrent
themes across studies) and also enhance complexity (e.g.
by highlighting differences and discrepancies) [29].
This review followed the “Enhancing Transparency in
Reporting the Synthesisof QualitativeResearch”
(ENTREQ) guidelines[29] (See Additionalfile 1 for
ENTREQ checklist) and consisted of (1) a systematic lit-
erature search for relevant qualitative and mixed methods
research reports;(2) criticalappraisalof included reports;
and (3) inductive and iterative analysis of included reports.
The protocolfor this thematic synthesis was published a
prioriwith PROSPERO Internationalprospective register
of systematicreviews (availableonline at http://
www.crd.york.ac.uk/prospero/display_record.asp?ID=CRD
42014013799; registration number CRD42014013799).
Search strategy
We searched both published and unpublished (“grey”)
literature.We identified published articles through sys-
tematic searchesof the following electronic databases
for academic journals from inception to October 2014:
MEDLINE, EMBASE, PsycINFO, CINAHL, Social
Services Abstracts,Applied SocialSciences Indexes and
Abstracts (ASSIA);and ofthe following evidence-based
medicine databases:The Cochrane database ofsystem-
atic reviews,EBM Reviews, The Campbell Collaboration,
and Centre for Reviews and Dissemination.A systematic
search strategy was developed with the assistance ofa
Broad et al.BMC Psychiatry (2017) 17:380 Page 2 of 11
librarian,and peer-reviewed by a second librarian.Key-
words,their truncationsand relevantdatabase-specific
subjectheadings and MeSH terms were used,targeting
three subjectareas:transition,age and mentalhealth.
For an example search strategy see Additional file 2.
We identified additionalpublished literature through
searchesof referencelists of relevantarticles(using
Science Citation Index and hand searching) and forward
citationsof relevantarticles(using ScienceCitation
Index or Google Scholar).We identified unpublished lit-
eraturethrough Googlesearcheswith the samekey-
words, and by contactingexpertsand key authors
identified in the search of published literature.
Inclusion and exclusion criteria
We included studiespublished in English thatused a
qualitative methodology to (1) Describe the perceptions
and experiences of youth utilizing mental health services
and (2) Explore their experiences of receiving services or
care:(a) During the transition from CAMHS to AMHS
setting or (b) In both the CAMHS and AMHS settings.
We included allstudies examining young adults who
have utilized mentalhealth services,with no limitations
on diagnosis,age,ethnicity or geographic locale.We ex-
cluded studies examining youth with exclusively chronic
physicalhealth conditions because young people utiliz-
ing mentalhealth services have been much less studied
and may experienceunique challengescompared to
young people with primarily physical disabilities [30].
All titlesand abstractswere reviewed independently
by two research team members(KB and VS) using
DistillerSR,to organize the search,screen titles,and ab-
stracts and extractdata.Any differences were resolved
by consensus amongst the two team members (KB and
VS),and,if necessary,a third team member (NS).Inter--
rateragreementfor inclusion ofstudieswas assessed
using the chance-corrected Kappa statistic.Agreement
for inclusion atthe full textlevelranged from Kappa
scores of 86% to 95%.
Quality assessment
We critically appraised allstudies in duplicate (KB and
VS) using the Critical AppraisalSkills Programme
(CASP) Tool, which provideskey criteriarelevantto
criticallyappraisingqualitativeresearchstudies(e.g.
appropriateness of research design,consideration of eth-
icalissues,rigour ofdata analysis) [31].Any differences
were resolved byconsensusamongstthe two team
members.All studies were included in final analysis.
Data analysis
We conducted an initialcontentanalysis ofindividual
studies,followedby a thematicsynthesisacrossall
studies [27],focusing only on contentrepresenting the
views ofyouth (typically,sections labelled “findings” or
“results”).
Three ofthe authors (KB,VS and NS) independently
read the textof three included studiesand generated
“codes”,and then met over multiple sessions to develop
a consensus ofcodes and their meanings (i.e.a coding
dictionary).We then continued to analyze three more
studiesindependently,meeting regularly to triangulate
perspectives and revise the coding dictionary by adding,
merging,deleting,or modifying codes.Once the codes
were not changing,the remainder ofthe included stud-
ies were coded by the first author (KB).KB then led the
thematic analysis identifying over-arching themes emer-
ging from the results of the studies as a whole and com-
paring and contrastingfindings across studiesand
populations.
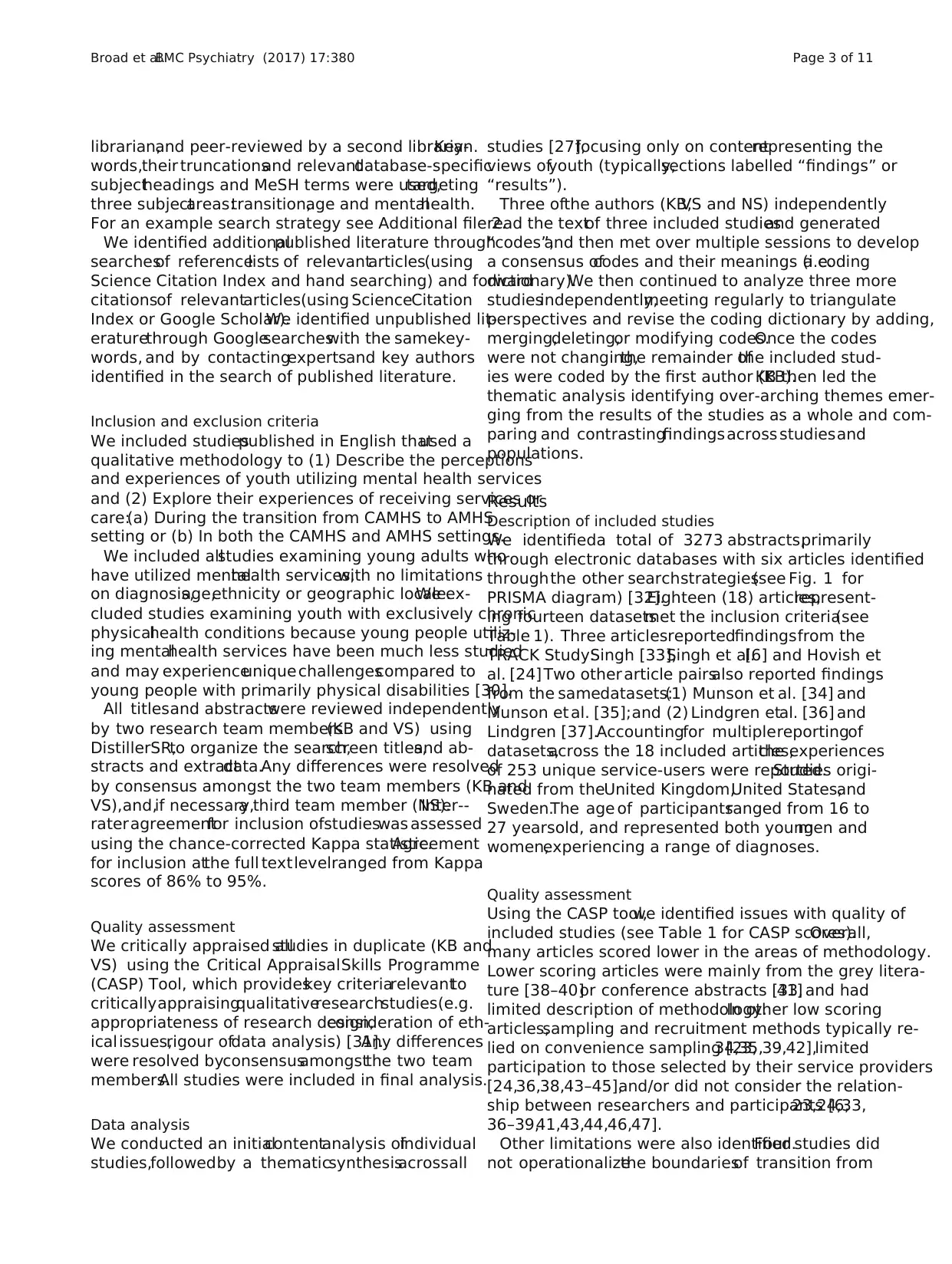
Results
Description of included studies
We identifieda total of 3273 abstracts,primarily
through electronic databases with six articles identified
throughthe other searchstrategies(see Fig. 1 for
PRISMA diagram) [32].Eighteen (18) articles,represent-
ing fourteen datasetsmet the inclusion criteria(see
Table 1). Three articlesreportedfindingsfrom the
TRACK Study:Singh [33],Singh et al.[6] and Hovish et
al. [24] Two other article pairsalso reported findings
from the samedatasets:(1) Munson et al. [34] and
Munson et al. [35];and (2) Lindgren etal. [36] and
Lindgren [37].Accountingfor multiplereportingof
datasets,across the 18 included articles,the experiences
of 253 unique service-users were reported.Studies origi-
nated from theUnited Kingdom,United States,and
Sweden.The age of participantsranged from 16 to
27 yearsold, and represented both youngmen and
women,experiencing a range of diagnoses.
Quality assessment
Using the CASP tool,we identified issues with quality of
included studies (see Table 1 for CASP scores).Overall,
many articles scored lower in the areas of methodology.
Lower scoring articles were mainly from the grey litera-
ture [38–40]or conference abstracts [33,41] and had
limited description of methodology.In other low scoring
articles,sampling and recruitment methods typically re-
lied on convenience sampling [23,34,35,39,42],limited
participation to those selected by their service providers
[24,36,38,43–45],and/or did not consider the relation-
ship between researchers and participants [6,23,24,33,
36–39,41,43,44,46,47].
Other limitations were also identified.Four studies did
not operationalizethe boundariesof transition from
Broad et al.BMC Psychiatry (2017) 17:380 Page 3 of 11
words,their truncationsand relevantdatabase-specific
subjectheadings and MeSH terms were used,targeting
three subjectareas:transition,age and mentalhealth.
For an example search strategy see Additional file 2.
We identified additionalpublished literature through
searchesof referencelists of relevantarticles(using
Science Citation Index and hand searching) and forward
citationsof relevantarticles(using ScienceCitation
Index or Google Scholar).We identified unpublished lit-
eraturethrough Googlesearcheswith the samekey-
words, and by contactingexpertsand key authors
identified in the search of published literature.
Inclusion and exclusion criteria
We included studiespublished in English thatused a
qualitative methodology to (1) Describe the perceptions
and experiences of youth utilizing mental health services
and (2) Explore their experiences of receiving services or
care:(a) During the transition from CAMHS to AMHS
setting or (b) In both the CAMHS and AMHS settings.
We included allstudies examining young adults who
have utilized mentalhealth services,with no limitations
on diagnosis,age,ethnicity or geographic locale.We ex-
cluded studies examining youth with exclusively chronic
physicalhealth conditions because young people utiliz-
ing mentalhealth services have been much less studied
and may experienceunique challengescompared to
young people with primarily physical disabilities [30].
All titlesand abstractswere reviewed independently
by two research team members(KB and VS) using
DistillerSR,to organize the search,screen titles,and ab-
stracts and extractdata.Any differences were resolved
by consensus amongst the two team members (KB and
VS),and,if necessary,a third team member (NS).Inter--
rateragreementfor inclusion ofstudieswas assessed
using the chance-corrected Kappa statistic.Agreement
for inclusion atthe full textlevelranged from Kappa
scores of 86% to 95%.
Quality assessment
We critically appraised allstudies in duplicate (KB and
VS) using the Critical AppraisalSkills Programme
(CASP) Tool, which provideskey criteriarelevantto
criticallyappraisingqualitativeresearchstudies(e.g.
appropriateness of research design,consideration of eth-
icalissues,rigour ofdata analysis) [31].Any differences
were resolved byconsensusamongstthe two team
members.All studies were included in final analysis.
Data analysis
We conducted an initialcontentanalysis ofindividual
studies,followedby a thematicsynthesisacrossall
studies [27],focusing only on contentrepresenting the
views ofyouth (typically,sections labelled “findings” or
“results”).
Three ofthe authors (KB,VS and NS) independently
read the textof three included studiesand generated
“codes”,and then met over multiple sessions to develop
a consensus ofcodes and their meanings (i.e.a coding
dictionary).We then continued to analyze three more
studiesindependently,meeting regularly to triangulate
perspectives and revise the coding dictionary by adding,
merging,deleting,or modifying codes.Once the codes
were not changing,the remainder ofthe included stud-
ies were coded by the first author (KB).KB then led the
thematic analysis identifying over-arching themes emer-
ging from the results of the studies as a whole and com-
paring and contrastingfindings across studiesand
populations.
Results
Description of included studies
We identifieda total of 3273 abstracts,primarily
through electronic databases with six articles identified
throughthe other searchstrategies(see Fig. 1 for
PRISMA diagram) [32].Eighteen (18) articles,represent-
ing fourteen datasetsmet the inclusion criteria(see
Table 1). Three articlesreportedfindingsfrom the
TRACK Study:Singh [33],Singh et al.[6] and Hovish et
al. [24] Two other article pairsalso reported findings
from the samedatasets:(1) Munson et al. [34] and
Munson et al. [35];and (2) Lindgren etal. [36] and
Lindgren [37].Accountingfor multiplereportingof
datasets,across the 18 included articles,the experiences
of 253 unique service-users were reported.Studies origi-
nated from theUnited Kingdom,United States,and
Sweden.The age of participantsranged from 16 to
27 yearsold, and represented both youngmen and
women,experiencing a range of diagnoses.
Quality assessment
Using the CASP tool,we identified issues with quality of
included studies (see Table 1 for CASP scores).Overall,
many articles scored lower in the areas of methodology.
Lower scoring articles were mainly from the grey litera-
ture [38–40]or conference abstracts [33,41] and had
limited description of methodology.In other low scoring
articles,sampling and recruitment methods typically re-
lied on convenience sampling [23,34,35,39,42],limited
participation to those selected by their service providers
[24,36,38,43–45],and/or did not consider the relation-
ship between researchers and participants [6,23,24,33,
36–39,41,43,44,46,47].
Other limitations were also identified.Four studies did
not operationalizethe boundariesof transition from
Broad et al.BMC Psychiatry (2017) 17:380 Page 3 of 11
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CAMHS to AMHS and the timing ofinterviewswith
youth was often unclear [23,38,41,42],making it un-
clear how much exposure youth had to AMHS.Further-
more,in studies that also examined parent,caregiver or
professionalviews,three studieslinked parentaland
youth views together in the discussion of themes [6,24,
44].To keep this thematic analysis in line with views of
youth,only findings indicated as originating from youth
were used in analysis.
Thematic foci
Three thematic fociemerged from the thematic synthe-
sis: (1) Complex Interplayof Multiple Concurrent
Transitions (2)Balancing Autonomy and the Need for
Supports and (3)Factors Impacting Youth Experiences
of Transition.
Complex interplay of multiple concurrent transitions
On the path to becoming an adult,young people experi-
ence multipletransitionsin a varietyof domainsin
addition to the transition from CAMHS to AMHS,such
as change in levelof parentalinvolvement,life events,
and community agency involvement.For some youth,
these transitionswere a majorobstacle forcontinued
mentalhealth service use,such as described by a youth
interviewed by Sakai et al.:
“I didn’t even get no Medicaid when I left foster care.I
had it but,it was never mailed to me.I didn’t even have
an address.” [43],p6.
In contrast,for some,life transitions,such as becom-
ing a parent,were a way for young people to become re-
engagedin mental health servicesas describedin
Munson et al.[35]:
“…and shortly after she was born Ihad talked to the
doctor about postpartum depression… I’m like ‘…I don’t
want to get out ofbed… I don’t want to do nothing’… He
was like ‘Wellyou could be having postpartum depres-
sion,’and that’s when allof my childhood mentalprob-
lems came up,because he had accessed my information
from my old doctor… he’s like ‘Wellyou know you need
to be on this medication…’” [pg 3].
As youth prepared to undergo major life transitions,
some voiced worries about the overlap of these
changes with their mentalhealth care transition.The
interplayof thesetransitionsmadesome feel more
vulnerable,especiallyas they sensed theimpact of
diminishing supports:
“I turn 18 in like 2 weeks,and I want to move out and
live on my own,but it is going to be hard for me because
once Iturn 18,the supports thatI have,some ofthem
are going to disappear.... I am going to have to be able
to dealwith my issues on my own and find other sup-
ports.” [23,p 11].
Fig. 1 PRISMA diagram
Broad et al.BMC Psychiatry (2017) 17:380 Page 4 of 11
youth was often unclear [23,38,41,42],making it un-
clear how much exposure youth had to AMHS.Further-
more,in studies that also examined parent,caregiver or
professionalviews,three studieslinked parentaland
youth views together in the discussion of themes [6,24,
44].To keep this thematic analysis in line with views of
youth,only findings indicated as originating from youth
were used in analysis.
Thematic foci
Three thematic fociemerged from the thematic synthe-
sis: (1) Complex Interplayof Multiple Concurrent
Transitions (2)Balancing Autonomy and the Need for
Supports and (3)Factors Impacting Youth Experiences
of Transition.
Complex interplay of multiple concurrent transitions
On the path to becoming an adult,young people experi-
ence multipletransitionsin a varietyof domainsin
addition to the transition from CAMHS to AMHS,such
as change in levelof parentalinvolvement,life events,
and community agency involvement.For some youth,
these transitionswere a majorobstacle forcontinued
mentalhealth service use,such as described by a youth
interviewed by Sakai et al.:
“I didn’t even get no Medicaid when I left foster care.I
had it but,it was never mailed to me.I didn’t even have
an address.” [43],p6.
In contrast,for some,life transitions,such as becom-
ing a parent,were a way for young people to become re-
engagedin mental health servicesas describedin
Munson et al.[35]:
“…and shortly after she was born Ihad talked to the
doctor about postpartum depression… I’m like ‘…I don’t
want to get out ofbed… I don’t want to do nothing’… He
was like ‘Wellyou could be having postpartum depres-
sion,’and that’s when allof my childhood mentalprob-
lems came up,because he had accessed my information
from my old doctor… he’s like ‘Wellyou know you need
to be on this medication…’” [pg 3].
As youth prepared to undergo major life transitions,
some voiced worries about the overlap of these
changes with their mentalhealth care transition.The
interplayof thesetransitionsmadesome feel more
vulnerable,especiallyas they sensed theimpact of
diminishing supports:
“I turn 18 in like 2 weeks,and I want to move out and
live on my own,but it is going to be hard for me because
once Iturn 18,the supports thatI have,some ofthem
are going to disappear.... I am going to have to be able
to dealwith my issues on my own and find other sup-
ports.” [23,p 11].
Fig. 1 PRISMA diagram
Broad et al.BMC Psychiatry (2017) 17:380 Page 4 of 11
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
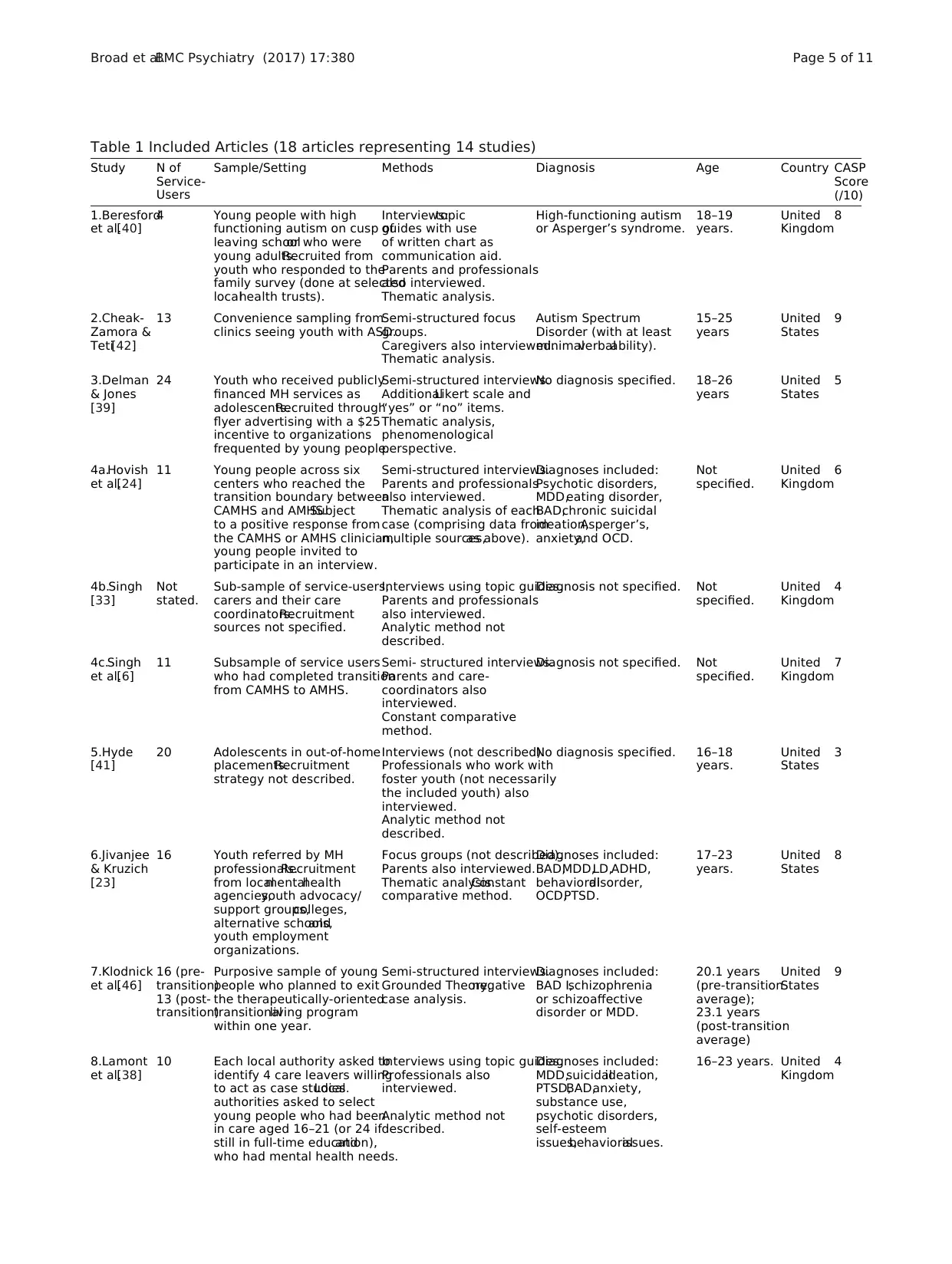
Table 1 Included Articles (18 articles representing 14 studies)
Study N of
Service-
Users
Sample/Setting Methods Diagnosis Age Country CASP
Score
(/10)
1.Beresford
et al.[40]
4 Young people with high
functioning autism on cusp of
leaving schoolor who were
young adults.Recruited from
youth who responded to the
family survey (done at selected
localhealth trusts).
Interviews:topic
guides with use
of written chart as
communication aid.
Parents and professionals
also interviewed.
Thematic analysis.
High-functioning autism
or Asperger’s syndrome.
18–19
years.
United
Kingdom
8
2.Cheak-
Zamora &
Teti[42]
13 Convenience sampling from
clinics seeing youth with ASD.
Semi-structured focus
groups.
Caregivers also interviewed.
Thematic analysis.
Autism Spectrum
Disorder (with at least
minimalverbalability).
15–25
years
United
States
9
3.Delman
& Jones
[39]
24 Youth who received publicly
financed MH services as
adolescents.Recruited through
flyer advertising with a $25
incentive to organizations
frequented by young people.
Semi-structured interviews.
AdditionalLikert scale and
“yes” or “no” items.
Thematic analysis,
phenomenological
perspective.
No diagnosis specified. 18–26
years
United
States
5
4a.Hovish
et al.[24]
11 Young people across six
centers who reached the
transition boundary between
CAMHS and AMHS.Subject
to a positive response from
the CAMHS or AMHS clinician,
young people invited to
participate in an interview.
Semi-structured interviews.
Parents and professionals
also interviewed.
Thematic analysis of each
case (comprising data from
multiple sources,as above).
Diagnoses included:
Psychotic disorders,
MDD,eating disorder,
BAD,chronic suicidal
ideation,Asperger’s,
anxiety,and OCD.
Not
specified.
United
Kingdom
6
4b.Singh
[33]
Not
stated.
Sub-sample of service-users,
carers and their care
coordinators.Recruitment
sources not specified.
Interviews using topic guides.
Parents and professionals
also interviewed.
Analytic method not
described.
Diagnosis not specified. Not
specified.
United
Kingdom
4
4c.Singh
et al.[6]
11 Subsample of service users
who had completed transition
from CAMHS to AMHS.
Semi- structured interviews.
Parents and care-
coordinators also
interviewed.
Constant comparative
method.
Diagnosis not specified. Not
specified.
United
Kingdom
7
5.Hyde
[41]
20 Adolescents in out-of-home
placements.Recruitment
strategy not described.
Interviews (not described).
Professionals who work with
foster youth (not necessarily
the included youth) also
interviewed.
Analytic method not
described.
No diagnosis specified. 16–18
years.
United
States
3
6.Jivanjee
& Kruzich
[23]
16 Youth referred by MH
professionals.Recruitment
from localmentalhealth
agencies,youth advocacy/
support groups,colleges,
alternative schools,and
youth employment
organizations.
Focus groups (not described).
Parents also interviewed.
Thematic analysis.Constant
comparative method.
Diagnoses included:
BAD,MDD,LD,ADHD,
behavioraldisorder,
OCD,PTSD.
17–23
years.
United
States
8
7.Klodnick
et al.[46]
16 (pre-
transition)
13 (post-
transition)
Purposive sample of young
people who planned to exit
the therapeutically-oriented
transitionalliving program
within one year.
Semi-structured interviews.
Grounded Theory,negative
case analysis.
Diagnoses included:
BAD I,schizophrenia
or schizoaffective
disorder or MDD.
20.1 years
(pre-transition
average);
23.1 years
(post-transition
average)
United
States
9
8.Lamont
et al.[38]
10 Each local authority asked to
identify 4 care leavers willing
to act as case studies.Local
authorities asked to select
young people who had been
in care aged 16–21 (or 24 if
still in full-time education),and
who had mental health needs.
Interviews using topic guides.
Professionals also
interviewed.
Analytic method not
described.
Diagnoses included:
MDD,suicidalideation,
PTSD,BAD,anxiety,
substance use,
psychotic disorders,
self-esteem
issues,behavioralissues.
16–23 years. United
Kingdom
4
Broad et al.BMC Psychiatry (2017) 17:380 Page 5 of 11
Study N of
Service-
Users
Sample/Setting Methods Diagnosis Age Country CASP
Score
(/10)
1.Beresford
et al.[40]
4 Young people with high
functioning autism on cusp of
leaving schoolor who were
young adults.Recruited from
youth who responded to the
family survey (done at selected
localhealth trusts).
Interviews:topic
guides with use
of written chart as
communication aid.
Parents and professionals
also interviewed.
Thematic analysis.
High-functioning autism
or Asperger’s syndrome.
18–19
years.
United
Kingdom
8
2.Cheak-
Zamora &
Teti[42]
13 Convenience sampling from
clinics seeing youth with ASD.
Semi-structured focus
groups.
Caregivers also interviewed.
Thematic analysis.
Autism Spectrum
Disorder (with at least
minimalverbalability).
15–25
years
United
States
9
3.Delman
& Jones
[39]
24 Youth who received publicly
financed MH services as
adolescents.Recruited through
flyer advertising with a $25
incentive to organizations
frequented by young people.
Semi-structured interviews.
AdditionalLikert scale and
“yes” or “no” items.
Thematic analysis,
phenomenological
perspective.
No diagnosis specified. 18–26
years
United
States
5
4a.Hovish
et al.[24]
11 Young people across six
centers who reached the
transition boundary between
CAMHS and AMHS.Subject
to a positive response from
the CAMHS or AMHS clinician,
young people invited to
participate in an interview.
Semi-structured interviews.
Parents and professionals
also interviewed.
Thematic analysis of each
case (comprising data from
multiple sources,as above).
Diagnoses included:
Psychotic disorders,
MDD,eating disorder,
BAD,chronic suicidal
ideation,Asperger’s,
anxiety,and OCD.
Not
specified.
United
Kingdom
6
4b.Singh
[33]
Not
stated.
Sub-sample of service-users,
carers and their care
coordinators.Recruitment
sources not specified.
Interviews using topic guides.
Parents and professionals
also interviewed.
Analytic method not
described.
Diagnosis not specified. Not
specified.
United
Kingdom
4
4c.Singh
et al.[6]
11 Subsample of service users
who had completed transition
from CAMHS to AMHS.
Semi- structured interviews.
Parents and care-
coordinators also
interviewed.
Constant comparative
method.
Diagnosis not specified. Not
specified.
United
Kingdom
7
5.Hyde
[41]
20 Adolescents in out-of-home
placements.Recruitment
strategy not described.
Interviews (not described).
Professionals who work with
foster youth (not necessarily
the included youth) also
interviewed.
Analytic method not
described.
No diagnosis specified. 16–18
years.
United
States
3
6.Jivanjee
& Kruzich
[23]
16 Youth referred by MH
professionals.Recruitment
from localmentalhealth
agencies,youth advocacy/
support groups,colleges,
alternative schools,and
youth employment
organizations.
Focus groups (not described).
Parents also interviewed.
Thematic analysis.Constant
comparative method.
Diagnoses included:
BAD,MDD,LD,ADHD,
behavioraldisorder,
OCD,PTSD.
17–23
years.
United
States
8
7.Klodnick
et al.[46]
16 (pre-
transition)
13 (post-
transition)
Purposive sample of young
people who planned to exit
the therapeutically-oriented
transitionalliving program
within one year.
Semi-structured interviews.
Grounded Theory,negative
case analysis.
Diagnoses included:
BAD I,schizophrenia
or schizoaffective
disorder or MDD.
20.1 years
(pre-transition
average);
23.1 years
(post-transition
average)
United
States
9
8.Lamont
et al.[38]
10 Each local authority asked to
identify 4 care leavers willing
to act as case studies.Local
authorities asked to select
young people who had been
in care aged 16–21 (or 24 if
still in full-time education),and
who had mental health needs.
Interviews using topic guides.
Professionals also
interviewed.
Analytic method not
described.
Diagnoses included:
MDD,suicidalideation,
PTSD,BAD,anxiety,
substance use,
psychotic disorders,
self-esteem
issues,behavioralissues.
16–23 years. United
Kingdom
4
Broad et al.BMC Psychiatry (2017) 17:380 Page 5 of 11
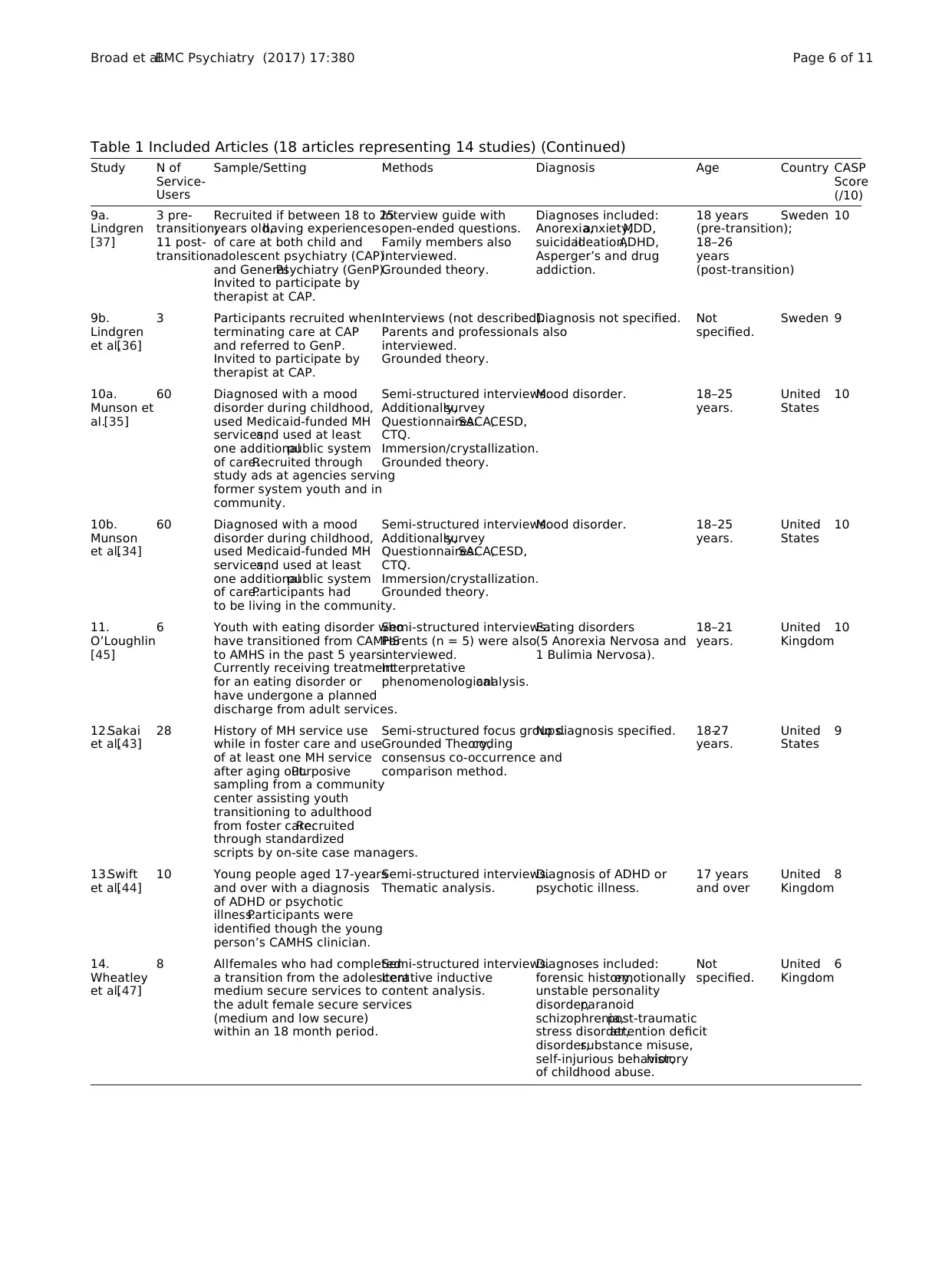
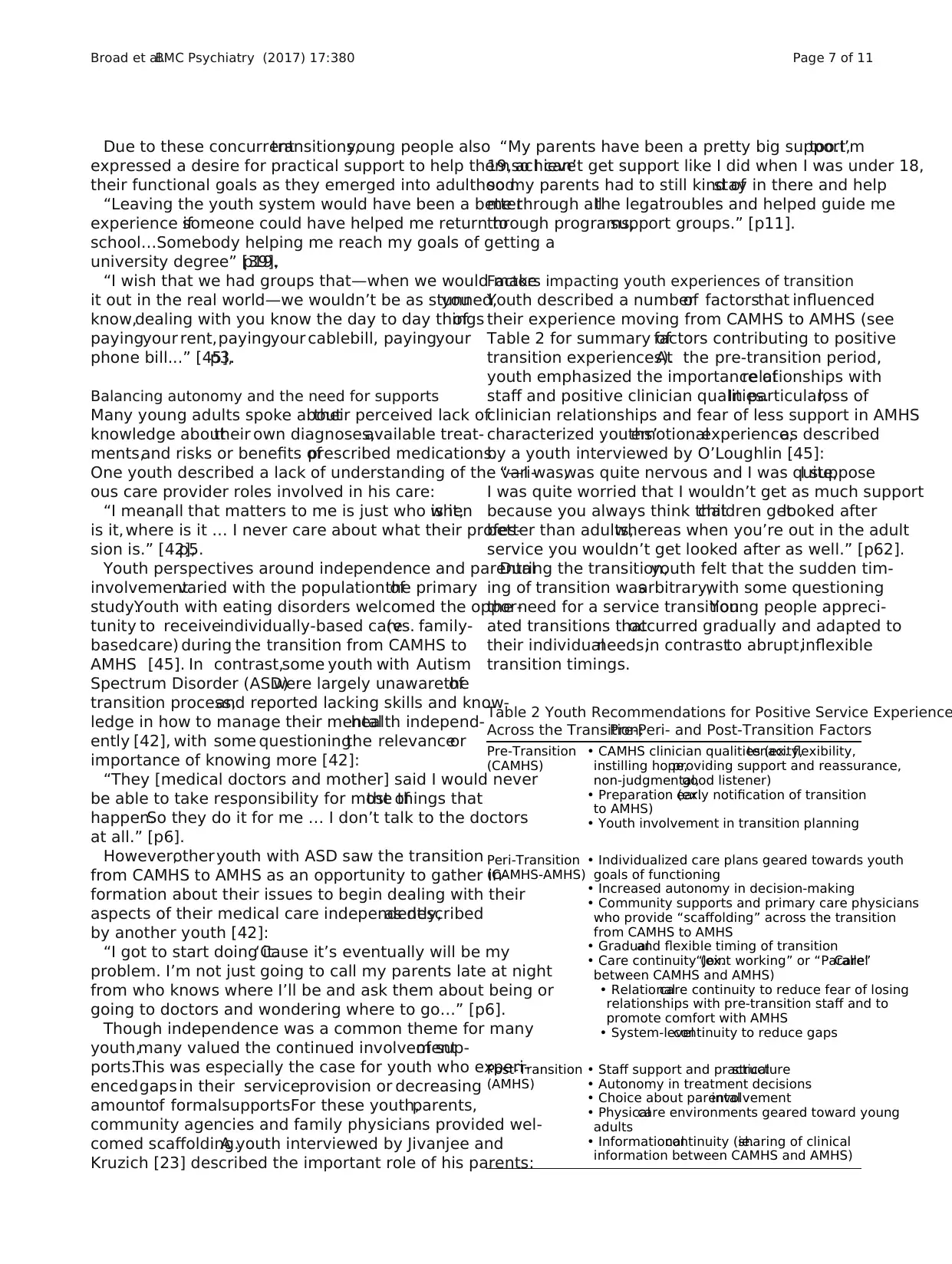
Table 1 Included Articles (18 articles representing 14 studies) (Continued)
Study N of
Service-
Users
Sample/Setting Methods Diagnosis Age Country CASP
Score
(/10)
9a.
Lindgren
[37]
3 pre-
transition;
11 post-
transition
Recruited if between 18 to 25
years old,having experiences
of care at both child and
adolescent psychiatry (CAP)
and GeneralPsychiatry (GenP).
Invited to participate by
therapist at CAP.
Interview guide with
open-ended questions.
Family members also
interviewed.
Grounded theory.
Diagnoses included:
Anorexia,anxiety,MDD,
suicidalideation,ADHD,
Asperger’s and drug
addiction.
18 years
(pre-transition);
18–26
years
(post-transition)
Sweden 10
9b.
Lindgren
et al.[36]
3 Participants recruited when
terminating care at CAP
and referred to GenP.
Invited to participate by
therapist at CAP.
Interviews (not described).
Parents and professionals also
interviewed.
Grounded theory.
Diagnosis not specified. Not
specified.
Sweden 9
10a.
Munson et
al.[35]
60 Diagnosed with a mood
disorder during childhood,
used Medicaid-funded MH
services,and used at least
one additionalpublic system
of care.Recruited through
study ads at agencies serving
former system youth and in
community.
Semi-structured interviews.
Additionally,survey
Questionnaires:SACA,CESD,
CTQ.
Immersion/crystallization.
Grounded theory.
Mood disorder. 18–25
years.
United
States
10
10b.
Munson
et al.[34]
60 Diagnosed with a mood
disorder during childhood,
used Medicaid-funded MH
services,and used at least
one additionalpublic system
of care.Participants had
to be living in the community.
Semi-structured interviews.
Additionally,survey
Questionnaires:SACA,CESD,
CTQ.
Immersion/crystallization.
Grounded theory.
Mood disorder. 18–25
years.
United
States
10
11.
O’Loughlin
[45]
6 Youth with eating disorder who
have transitioned from CAMHS
to AMHS in the past 5 years.
Currently receiving treatment
for an eating disorder or
have undergone a planned
discharge from adult services.
Semi-structured interviews.
Parents (n = 5) were also
interviewed.
Interpretative
phenomenologicalanalysis.
Eating disorders
(5 Anorexia Nervosa and
1 Bulimia Nervosa).
18–21
years.
United
Kingdom
10
12.Sakai
et al.[43]
28 History of MH service use
while in foster care and use
of at least one MH service
after aging out.Purposive
sampling from a community
center assisting youth
transitioning to adulthood
from foster care.Recruited
through standardized
scripts by on-site case managers.
Semi-structured focus groups.
Grounded Theory,coding
consensus co-occurrence and
comparison method.
No diagnosis specified. 18–27
years.
United
States
9
13.Swift
et al.[44]
10 Young people aged 17-years
and over with a diagnosis
of ADHD or psychotic
illness.Participants were
identified though the young
person’s CAMHS clinician.
Semi-structured interviews.
Thematic analysis.
Diagnosis of ADHD or
psychotic illness.
17 years
and over
United
Kingdom
8
14.
Wheatley
et al.[47]
8 Allfemales who had completed
a transition from the adolescent
medium secure services to
the adult female secure services
(medium and low secure)
within an 18 month period.
Semi-structured interviews.
Iterative inductive
content analysis.
Diagnoses included:
forensic history,emotionally
unstable personality
disorder,paranoid
schizophrenia,post-traumatic
stress disorder,attention deficit
disorder,substance misuse,
self-injurious behavior,history
of childhood abuse.
Not
specified.
United
Kingdom
6
Broad et al.BMC Psychiatry (2017) 17:380 Page 6 of 11
Study N of
Service-
Users
Sample/Setting Methods Diagnosis Age Country CASP
Score
(/10)
9a.
Lindgren
[37]
3 pre-
transition;
11 post-
transition
Recruited if between 18 to 25
years old,having experiences
of care at both child and
adolescent psychiatry (CAP)
and GeneralPsychiatry (GenP).
Invited to participate by
therapist at CAP.
Interview guide with
open-ended questions.
Family members also
interviewed.
Grounded theory.
Diagnoses included:
Anorexia,anxiety,MDD,
suicidalideation,ADHD,
Asperger’s and drug
addiction.
18 years
(pre-transition);
18–26
years
(post-transition)
Sweden 10
9b.
Lindgren
et al.[36]
3 Participants recruited when
terminating care at CAP
and referred to GenP.
Invited to participate by
therapist at CAP.
Interviews (not described).
Parents and professionals also
interviewed.
Grounded theory.
Diagnosis not specified. Not
specified.
Sweden 9
10a.
Munson et
al.[35]
60 Diagnosed with a mood
disorder during childhood,
used Medicaid-funded MH
services,and used at least
one additionalpublic system
of care.Recruited through
study ads at agencies serving
former system youth and in
community.
Semi-structured interviews.
Additionally,survey
Questionnaires:SACA,CESD,
CTQ.
Immersion/crystallization.
Grounded theory.
Mood disorder. 18–25
years.
United
States
10
10b.
Munson
et al.[34]
60 Diagnosed with a mood
disorder during childhood,
used Medicaid-funded MH
services,and used at least
one additionalpublic system
of care.Participants had
to be living in the community.
Semi-structured interviews.
Additionally,survey
Questionnaires:SACA,CESD,
CTQ.
Immersion/crystallization.
Grounded theory.
Mood disorder. 18–25
years.
United
States
10
11.
O’Loughlin
[45]
6 Youth with eating disorder who
have transitioned from CAMHS
to AMHS in the past 5 years.
Currently receiving treatment
for an eating disorder or
have undergone a planned
discharge from adult services.
Semi-structured interviews.
Parents (n = 5) were also
interviewed.
Interpretative
phenomenologicalanalysis.
Eating disorders
(5 Anorexia Nervosa and
1 Bulimia Nervosa).
18–21
years.
United
Kingdom
10
12.Sakai
et al.[43]
28 History of MH service use
while in foster care and use
of at least one MH service
after aging out.Purposive
sampling from a community
center assisting youth
transitioning to adulthood
from foster care.Recruited
through standardized
scripts by on-site case managers.
Semi-structured focus groups.
Grounded Theory,coding
consensus co-occurrence and
comparison method.
No diagnosis specified. 18–27
years.
United
States
9
13.Swift
et al.[44]
10 Young people aged 17-years
and over with a diagnosis
of ADHD or psychotic
illness.Participants were
identified though the young
person’s CAMHS clinician.
Semi-structured interviews.
Thematic analysis.
Diagnosis of ADHD or
psychotic illness.
17 years
and over
United
Kingdom
8
14.
Wheatley
et al.[47]
8 Allfemales who had completed
a transition from the adolescent
medium secure services to
the adult female secure services
(medium and low secure)
within an 18 month period.
Semi-structured interviews.
Iterative inductive
content analysis.
Diagnoses included:
forensic history,emotionally
unstable personality
disorder,paranoid
schizophrenia,post-traumatic
stress disorder,attention deficit
disorder,substance misuse,
self-injurious behavior,history
of childhood abuse.
Not
specified.
United
Kingdom
6
Broad et al.BMC Psychiatry (2017) 17:380 Page 6 of 11
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Due to these concurrenttransitions,young people also
expressed a desire for practical support to help them achieve
their functional goals as they emerged into adulthood.
“Leaving the youth system would have been a better
experience ifsomeone could have helped me return to
school…Somebody helping me reach my goals of getting a
university degree” [39],p19.
“I wish that we had groups that—when we would make
it out in the real world—we wouldn’t be as stunned,you
know,dealing with you know the day to day thingsof
payingyour rent,payingyour cablebill, payingyour
phone bill...” [45],p3.
Balancing autonomy and the need for supports
Many young adults spoke abouttheir perceived lack of
knowledge abouttheir own diagnoses,available treat-
ments,and risks or benefits ofprescribed medications.
One youth described a lack of understanding of the vari-
ous care provider roles involved in his care:
“I mean,all that matters to me is just who is it,when
is it, where is it … I never care about what their profes-
sion is.” [42],p5.
Youth perspectives around independence and parental
involvementvaried with the population ofthe primary
study.Youth with eating disorders welcomed the oppor-
tunity to receiveindividually-based care(vs. family-
basedcare) during the transition from CAMHS to
AMHS [45]. In contrast,some youth with Autism
Spectrum Disorder (ASD)were largely unaware ofthe
transition process,and reported lacking skills and know-
ledge in how to manage their mentalhealth independ-
ently [42], with some questioningthe relevanceor
importance of knowing more [42]:
“They [medical doctors and mother] said I would never
be able to take responsibility for most ofthe things that
happen.So they do it for me … I don’t talk to the doctors
at all.” [p6].
However,other youth with ASD saw the transition
from CAMHS to AMHS as an opportunity to gather in-
formation about their issues to begin dealing with their
aspects of their medical care independently,as described
by another youth [42]:
“I got to start doing it.‘Cause it’s eventually will be my
problem. I’m not just going to call my parents late at night
from who knows where I’ll be and ask them about being or
going to doctors and wondering where to go…” [p6].
Though independence was a common theme for many
youth,many valued the continued involvementof sup-
ports.This was especially the case for youth who experi-
encedgaps in their serviceprovision or decreasing
amountof formalsupports.For these youth,parents,
community agencies and family physicians provided wel-
comed scaffolding.A youth interviewed by Jivanjee and
Kruzich [23] described the important role of his parents:
“My parents have been a pretty big support,too.I’m
19,so I can’t get support like I did when I was under 18,
so my parents had to still kind ofstay in there and help
me through allthe legaltroubles and helped guide me
through programs,support groups.” [p11].
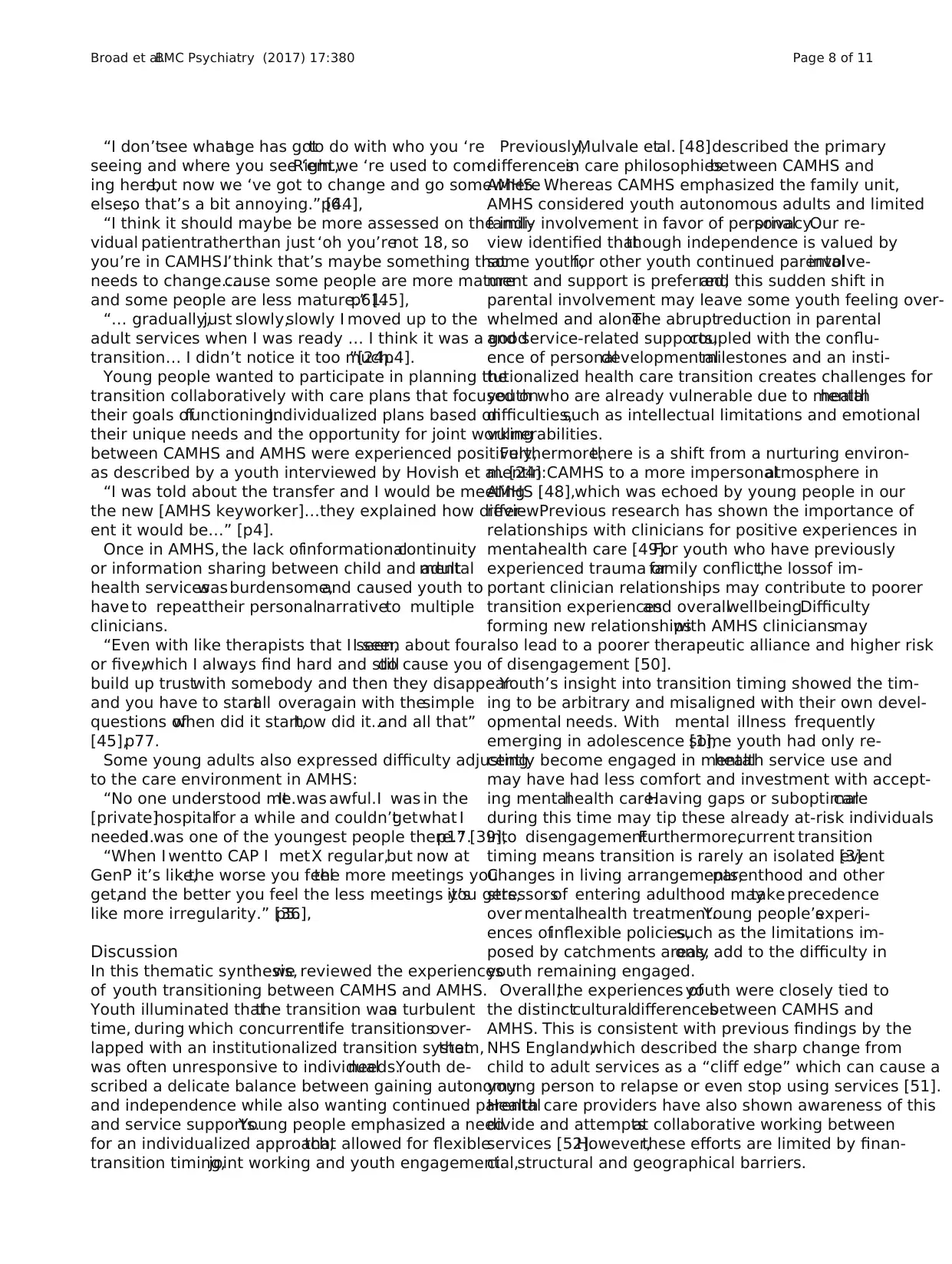
Factors impacting youth experiences of transition
Youth described a numberof factorsthat influenced
their experience moving from CAMHS to AMHS (see
Table 2 for summary offactors contributing to positive
transition experiences).At the pre-transition period,
youth emphasized the importance ofrelationships with
staff and positive clinician qualities.In particular,loss of
clinician relationships and fear of less support in AMHS
characterized youths’emotionalexperience,as described
by a youth interviewed by O’Loughlin [45]:
“—I was,was quite nervous and I was quite,I suppose
I was quite worried that I wouldn’t get as much support
because you always think thatchildren getlooked after
better than adults,whereas when you’re out in the adult
service you wouldn’t get looked after as well.” [p62].
During the transition,youth felt that the sudden tim-
ing of transition wasarbitrary,with some questioning
the need for a service transition.Young people appreci-
ated transitions thatoccurred gradually and adapted to
their individualneeds,in contrastto abrupt,inflexible
transition timings.
Table 2 Youth Recommendations for Positive Service Experience
Across the Transition:Pre-,Peri- and Post-Transition Factors
Pre-Transition
(CAMHS)
• CAMHS clinician qualities (ex.tenacity,flexibility,
instilling hope,providing support and reassurance,
non-judgmental,good listener)
• Preparation (ex.early notification of transition
to AMHS)
• Youth involvement in transition planning
Peri-Transition
(CAMHS-AMHS)
• Individualized care plans geared towards youth
goals of functioning
• Increased autonomy in decision-making
• Community supports and primary care physicians
who provide “scaffolding” across the transition
from CAMHS to AMHS
• Gradualand flexible timing of transition
• Care continuity (ex.“Joint working” or “ParallelCare”
between CAMHS and AMHS)
• Relationalcare continuity to reduce fear of losing
relationships with pre-transition staff and to
promote comfort with AMHS
• System-levelcontinuity to reduce gaps
Post-Transition
(AMHS)
• Staff support and practicalstructure
• Autonomy in treatment decisions
• Choice about parentalinvolvement
• Physicalcare environments geared toward young
adults
• Informationalcontinuity (ie.sharing of clinical
information between CAMHS and AMHS)
Broad et al.BMC Psychiatry (2017) 17:380 Page 7 of 11
expressed a desire for practical support to help them achieve
their functional goals as they emerged into adulthood.
“Leaving the youth system would have been a better
experience ifsomeone could have helped me return to
school…Somebody helping me reach my goals of getting a
university degree” [39],p19.
“I wish that we had groups that—when we would make
it out in the real world—we wouldn’t be as stunned,you
know,dealing with you know the day to day thingsof
payingyour rent,payingyour cablebill, payingyour
phone bill...” [45],p3.
Balancing autonomy and the need for supports
Many young adults spoke abouttheir perceived lack of
knowledge abouttheir own diagnoses,available treat-
ments,and risks or benefits ofprescribed medications.
One youth described a lack of understanding of the vari-
ous care provider roles involved in his care:
“I mean,all that matters to me is just who is it,when
is it, where is it … I never care about what their profes-
sion is.” [42],p5.
Youth perspectives around independence and parental
involvementvaried with the population ofthe primary
study.Youth with eating disorders welcomed the oppor-
tunity to receiveindividually-based care(vs. family-
basedcare) during the transition from CAMHS to
AMHS [45]. In contrast,some youth with Autism
Spectrum Disorder (ASD)were largely unaware ofthe
transition process,and reported lacking skills and know-
ledge in how to manage their mentalhealth independ-
ently [42], with some questioningthe relevanceor
importance of knowing more [42]:
“They [medical doctors and mother] said I would never
be able to take responsibility for most ofthe things that
happen.So they do it for me … I don’t talk to the doctors
at all.” [p6].
However,other youth with ASD saw the transition
from CAMHS to AMHS as an opportunity to gather in-
formation about their issues to begin dealing with their
aspects of their medical care independently,as described
by another youth [42]:
“I got to start doing it.‘Cause it’s eventually will be my
problem. I’m not just going to call my parents late at night
from who knows where I’ll be and ask them about being or
going to doctors and wondering where to go…” [p6].
Though independence was a common theme for many
youth,many valued the continued involvementof sup-
ports.This was especially the case for youth who experi-
encedgaps in their serviceprovision or decreasing
amountof formalsupports.For these youth,parents,
community agencies and family physicians provided wel-
comed scaffolding.A youth interviewed by Jivanjee and
Kruzich [23] described the important role of his parents:
“My parents have been a pretty big support,too.I’m
19,so I can’t get support like I did when I was under 18,
so my parents had to still kind ofstay in there and help
me through allthe legaltroubles and helped guide me
through programs,support groups.” [p11].
Factors impacting youth experiences of transition
Youth described a numberof factorsthat influenced
their experience moving from CAMHS to AMHS (see
Table 2 for summary offactors contributing to positive
transition experiences).At the pre-transition period,
youth emphasized the importance ofrelationships with
staff and positive clinician qualities.In particular,loss of
clinician relationships and fear of less support in AMHS
characterized youths’emotionalexperience,as described
by a youth interviewed by O’Loughlin [45]:
“—I was,was quite nervous and I was quite,I suppose
I was quite worried that I wouldn’t get as much support
because you always think thatchildren getlooked after
better than adults,whereas when you’re out in the adult
service you wouldn’t get looked after as well.” [p62].
During the transition,youth felt that the sudden tim-
ing of transition wasarbitrary,with some questioning
the need for a service transition.Young people appreci-
ated transitions thatoccurred gradually and adapted to
their individualneeds,in contrastto abrupt,inflexible
transition timings.
Table 2 Youth Recommendations for Positive Service Experience
Across the Transition:Pre-,Peri- and Post-Transition Factors
Pre-Transition
(CAMHS)
• CAMHS clinician qualities (ex.tenacity,flexibility,
instilling hope,providing support and reassurance,
non-judgmental,good listener)
• Preparation (ex.early notification of transition
to AMHS)
• Youth involvement in transition planning
Peri-Transition
(CAMHS-AMHS)
• Individualized care plans geared towards youth
goals of functioning
• Increased autonomy in decision-making
• Community supports and primary care physicians
who provide “scaffolding” across the transition
from CAMHS to AMHS
• Gradualand flexible timing of transition
• Care continuity (ex.“Joint working” or “ParallelCare”
between CAMHS and AMHS)
• Relationalcare continuity to reduce fear of losing
relationships with pre-transition staff and to
promote comfort with AMHS
• System-levelcontinuity to reduce gaps
Post-Transition
(AMHS)
• Staff support and practicalstructure
• Autonomy in treatment decisions
• Choice about parentalinvolvement
• Physicalcare environments geared toward young
adults
• Informationalcontinuity (ie.sharing of clinical
information between CAMHS and AMHS)
Broad et al.BMC Psychiatry (2017) 17:380 Page 7 of 11
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
“I don’tsee whatage has gotto do with who you ‘re
seeing and where you see ‘em.Right,we ‘re used to com-
ing here,but now we ‘ve got to change and go somewhere
else,so that’s a bit annoying.” [44],p6.
“I think it should maybe be more assessed on the indi-
vidual patientratherthan just ‘oh you’renot 18, so
you’re in CAMHS.’I think that’s maybe something that
needs to change…...cause some people are more mature
and some people are less mature.” [45],p61.
“… gradually,just slowly,slowly I moved up to the
adult services when I was ready … I think it was a good
transition… I didn’t notice it too much.”[24,p4].
Young people wanted to participate in planning the
transition collaboratively with care plans that focused on
their goals offunctioning.Individualized plans based on
their unique needs and the opportunity for joint working
between CAMHS and AMHS were experienced positively,
as described by a youth interviewed by Hovish et al. [24]:
“I was told about the transfer and I would be meeting
the new [AMHS keyworker]…they explained how differ-
ent it would be…” [p4].
Once in AMHS, the lack ofinformationalcontinuity
or information sharing between child and adultmental
health serviceswasburdensome,and caused youth to
have to repeattheir personalnarrativeto multiple
clinicians.
“Even with like therapists that I seen,I seen about four
or five,which I always find hard and stilldo cause you
build up trustwith somebody and then they disappear
and you have to startall overagain with thesimple
questions ofwhen did it start,how did it...and all that”
[45],p77.
Some young adults also expressed difficulty adjusting
to the care environment in AMHS:
“No one understood me.It was awful.I was in the
[private]hospitalfor a while and couldn’tgetwhat I
needed.I was one of the youngest people there.” [39],p17.
“When I wentto CAP I metX regular,but now at
GenP it’s like,the worse you feelthe more meetings you
get,and the better you feel the less meetings you gets,it’s
like more irregularity.” [36],p5.
Discussion
In this thematic synthesis,we reviewed the experiences
of youth transitioning between CAMHS and AMHS.
Youth illuminated thatthe transition wasa turbulent
time, during which concurrentlife transitionsover-
lapped with an institutionalized transition system,that
was often unresponsive to individualneeds.Youth de-
scribed a delicate balance between gaining autonomy
and independence while also wanting continued parental
and service supports.Young people emphasized a need
for an individualized approach,that allowed for flexible
transition timing,joint working and youth engagement.
Previously,Mulvale etal. [48]described the primary
differencesin care philosophiesbetween CAMHS and
AMHS. Whereas CAMHS emphasized the family unit,
AMHS considered youth autonomous adults and limited
family involvement in favor of personalprivacy.Our re-
view identified thatthough independence is valued by
some youth,for other youth continued parentalinvolve-
ment and support is preferred,and this sudden shift in
parental involvement may leave some youth feeling over-
whelmed and alone.The abruptreduction in parental
and service-related supports,coupled with the conflu-
ence of personaldevelopmentalmilestones and an insti-
tutionalized health care transition creates challenges for
youth who are already vulnerable due to mentalhealth
difficulties,such as intellectual limitations and emotional
vulnerabilities.
Furthermore,there is a shift from a nurturing environ-
mentin CAMHS to a more impersonalatmosphere in
AMHS [48],which was echoed by young people in our
review.Previous research has shown the importance of
relationships with clinicians for positive experiences in
mentalhealth care [49].For youth who have previously
experienced trauma orfamily conflict,the lossof im-
portant clinician relationships may contribute to poorer
transition experiencesand overallwellbeing.Difficulty
forming new relationshipswith AMHS cliniciansmay
also lead to a poorer therapeutic alliance and higher risk
of disengagement [50].
Youth’s insight into transition timing showed the tim-
ing to be arbitrary and misaligned with their own devel-
opmental needs. With mental illness frequently
emerging in adolescence [1],some youth had only re-
cently become engaged in mentalhealth service use and
may have had less comfort and investment with accept-
ing mentalhealth care.Having gaps or suboptimalcare
during this time may tip these already at-risk individuals
into disengagement.Furthermore,current transition
timing means transition is rarely an isolated event[3].
Changes in living arrangements,parenthood and other
stressorsof entering adulthood maytake precedence
over mentalhealth treatment.Young people’sexperi-
ences ofinflexible policies,such as the limitations im-
posed by catchments areas,only add to the difficulty in
youth remaining engaged.
Overall,the experiences ofyouth were closely tied to
the distinctculturaldifferencesbetween CAMHS and
AMHS. This is consistent with previous findings by the
NHS England,which described the sharp change from
child to adult services as a “cliff edge” which can cause a
young person to relapse or even stop using services [51].
Health care providers have also shown awareness of this
divide and attemptsat collaborative working between
services [52].However,these efforts are limited by finan-
cial,structural and geographical barriers.
Broad et al.BMC Psychiatry (2017) 17:380 Page 8 of 11
seeing and where you see ‘em.Right,we ‘re used to com-
ing here,but now we ‘ve got to change and go somewhere
else,so that’s a bit annoying.” [44],p6.
“I think it should maybe be more assessed on the indi-
vidual patientratherthan just ‘oh you’renot 18, so
you’re in CAMHS.’I think that’s maybe something that
needs to change…...cause some people are more mature
and some people are less mature.” [45],p61.
“… gradually,just slowly,slowly I moved up to the
adult services when I was ready … I think it was a good
transition… I didn’t notice it too much.”[24,p4].
Young people wanted to participate in planning the
transition collaboratively with care plans that focused on
their goals offunctioning.Individualized plans based on
their unique needs and the opportunity for joint working
between CAMHS and AMHS were experienced positively,
as described by a youth interviewed by Hovish et al. [24]:
“I was told about the transfer and I would be meeting
the new [AMHS keyworker]…they explained how differ-
ent it would be…” [p4].
Once in AMHS, the lack ofinformationalcontinuity
or information sharing between child and adultmental
health serviceswasburdensome,and caused youth to
have to repeattheir personalnarrativeto multiple
clinicians.
“Even with like therapists that I seen,I seen about four
or five,which I always find hard and stilldo cause you
build up trustwith somebody and then they disappear
and you have to startall overagain with thesimple
questions ofwhen did it start,how did it...and all that”
[45],p77.
Some young adults also expressed difficulty adjusting
to the care environment in AMHS:
“No one understood me.It was awful.I was in the
[private]hospitalfor a while and couldn’tgetwhat I
needed.I was one of the youngest people there.” [39],p17.
“When I wentto CAP I metX regular,but now at
GenP it’s like,the worse you feelthe more meetings you
get,and the better you feel the less meetings you gets,it’s
like more irregularity.” [36],p5.
Discussion
In this thematic synthesis,we reviewed the experiences
of youth transitioning between CAMHS and AMHS.
Youth illuminated thatthe transition wasa turbulent
time, during which concurrentlife transitionsover-
lapped with an institutionalized transition system,that
was often unresponsive to individualneeds.Youth de-
scribed a delicate balance between gaining autonomy
and independence while also wanting continued parental
and service supports.Young people emphasized a need
for an individualized approach,that allowed for flexible
transition timing,joint working and youth engagement.
Previously,Mulvale etal. [48]described the primary
differencesin care philosophiesbetween CAMHS and
AMHS. Whereas CAMHS emphasized the family unit,
AMHS considered youth autonomous adults and limited
family involvement in favor of personalprivacy.Our re-
view identified thatthough independence is valued by
some youth,for other youth continued parentalinvolve-
ment and support is preferred,and this sudden shift in
parental involvement may leave some youth feeling over-
whelmed and alone.The abruptreduction in parental
and service-related supports,coupled with the conflu-
ence of personaldevelopmentalmilestones and an insti-
tutionalized health care transition creates challenges for
youth who are already vulnerable due to mentalhealth
difficulties,such as intellectual limitations and emotional
vulnerabilities.
Furthermore,there is a shift from a nurturing environ-
mentin CAMHS to a more impersonalatmosphere in
AMHS [48],which was echoed by young people in our
review.Previous research has shown the importance of
relationships with clinicians for positive experiences in
mentalhealth care [49].For youth who have previously
experienced trauma orfamily conflict,the lossof im-
portant clinician relationships may contribute to poorer
transition experiencesand overallwellbeing.Difficulty
forming new relationshipswith AMHS cliniciansmay
also lead to a poorer therapeutic alliance and higher risk
of disengagement [50].
Youth’s insight into transition timing showed the tim-
ing to be arbitrary and misaligned with their own devel-
opmental needs. With mental illness frequently
emerging in adolescence [1],some youth had only re-
cently become engaged in mentalhealth service use and
may have had less comfort and investment with accept-
ing mentalhealth care.Having gaps or suboptimalcare
during this time may tip these already at-risk individuals
into disengagement.Furthermore,current transition
timing means transition is rarely an isolated event[3].
Changes in living arrangements,parenthood and other
stressorsof entering adulthood maytake precedence
over mentalhealth treatment.Young people’sexperi-
ences ofinflexible policies,such as the limitations im-
posed by catchments areas,only add to the difficulty in
youth remaining engaged.
Overall,the experiences ofyouth were closely tied to
the distinctculturaldifferencesbetween CAMHS and
AMHS. This is consistent with previous findings by the
NHS England,which described the sharp change from
child to adult services as a “cliff edge” which can cause a
young person to relapse or even stop using services [51].
Health care providers have also shown awareness of this
divide and attemptsat collaborative working between
services [52].However,these efforts are limited by finan-
cial,structural and geographical barriers.
Broad et al.BMC Psychiatry (2017) 17:380 Page 8 of 11
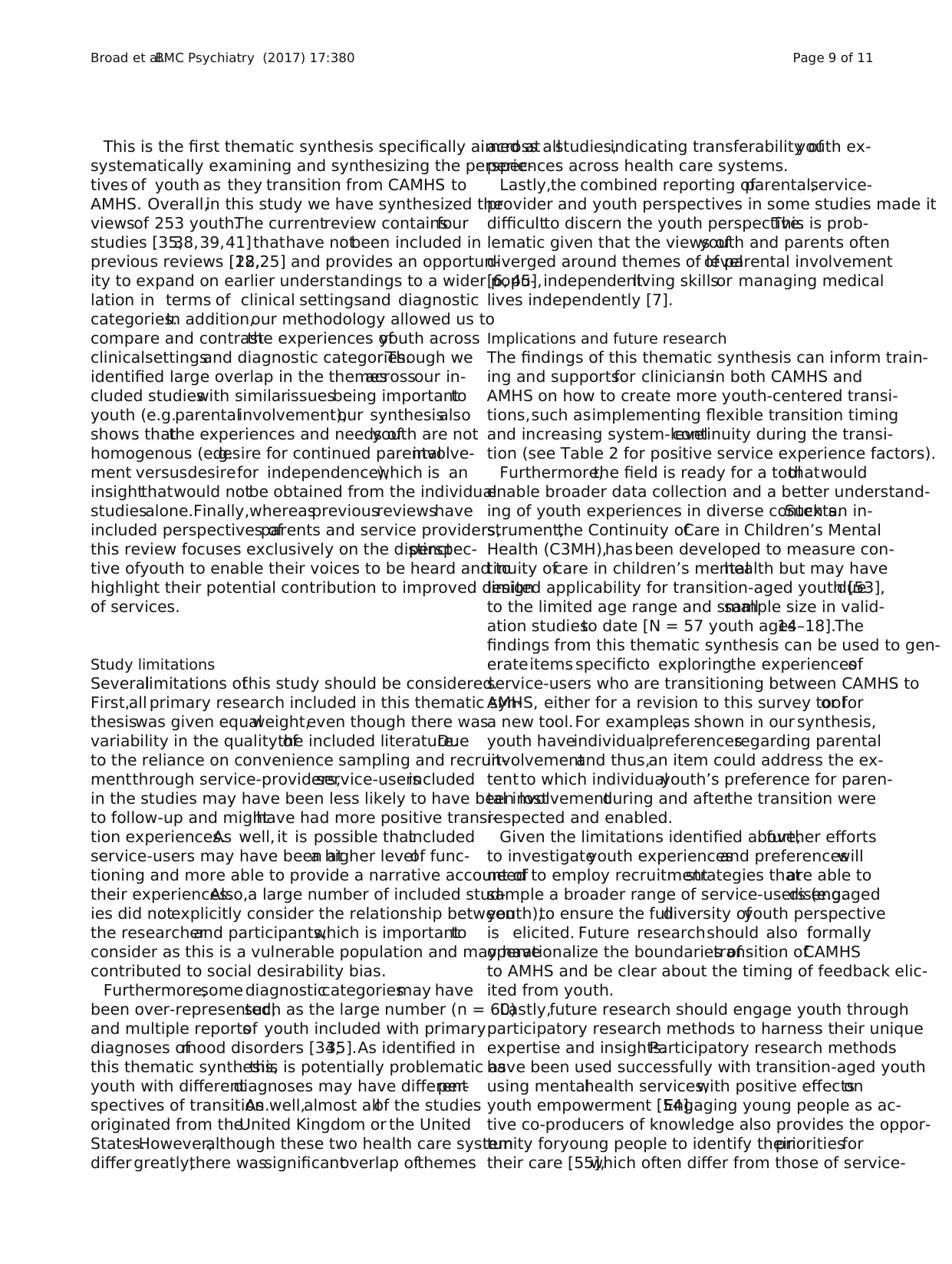
This is the first thematic synthesis specifically aimed at
systematically examining and synthesizing the perspec-
tives of youth as they transition from CAMHS to
AMHS. Overall,in this study we have synthesized the
viewsof 253 youth.The currentreview containsfour
studies [35,38,39,41]thathave notbeen included in
previous reviews [18,22,25] and provides an opportun-
ity to expand on earlier understandings to a wider popu-
lation in terms of clinical settingsand diagnostic
categories.In addition,our methodology allowed us to
compare and contrastthe experiences ofyouth across
clinicalsettingsand diagnostic categories.Though we
identified large overlap in the themesacrossour in-
cluded studieswith similarissuesbeing importantto
youth (e.g.parentalinvolvement),our synthesisalso
shows thatthe experiences and needs ofyouth are not
homogenous (e.g.desire for continued parentalinvolve-
ment versusdesirefor independence),which is an
insightthatwould notbe obtained from the individual
studiesalone.Finally,whereaspreviousreviewshave
included perspectives ofparents and service providers,
this review focuses exclusively on the distinctperspec-
tive ofyouth to enable their voices to be heard and to
highlight their potential contribution to improved design
of services.
Study limitations
Severallimitations ofthis study should be considered.
First,all primary research included in this thematic syn-
thesiswas given equalweight,even though there was
variability in the quality ofthe included literature.Due
to the reliance on convenience sampling and recruit-
mentthrough service-providers,service-usersincluded
in the studies may have been less likely to have been lost
to follow-up and mighthave had more positive transi-
tion experiences.As well, it is possible thatincluded
service-users may have been ata higher levelof func-
tioning and more able to provide a narrative account of
their experiences.Also,a large number of included stud-
ies did notexplicitly consider the relationship between
the researcherand participants,which is importantto
consider as this is a vulnerable population and may have
contributed to social desirability bias.
Furthermore,some diagnosticcategoriesmay have
been over-represented,such as the large number (n = 60)
and multiple reportsof youth included with primary
diagnoses ofmood disorders [34,35].As identified in
this thematic synthesis,this is potentially problematic as
youth with differentdiagnoses may have differentper-
spectives of transition.As well,almost allof the studies
originated from theUnited Kingdom or the United
States.However,although these two health care system
differ greatly,there wassignificantoverlap ofthemes
across allstudies,indicating transferability ofyouth ex-
periences across health care systems.
Lastly,the combined reporting ofparental,service-
provider and youth perspectives in some studies made it
difficultto discern the youth perspective.This is prob-
lematic given that the views ofyouth and parents often
diverged around themes of levelof parental involvement
[6, 45],independentliving skillsor managing medical
lives independently [7].
Implications and future research
The findings of this thematic synthesis can inform train-
ing and supportsfor cliniciansin both CAMHS and
AMHS on how to create more youth-centered transi-
tions,such asimplementing flexible transition timing
and increasing system-levelcontinuity during the transi-
tion (see Table 2 for positive service experience factors).
Furthermore,the field is ready for a toolthatwould
enable broader data collection and a better understand-
ing of youth experiences in diverse contexts.Such an in-
strument,the Continuity ofCare in Children’s Mental
Health (C3MH),has been developed to measure con-
tinuity ofcare in children’s mentalhealth but may have
limited applicability for transition-aged youth [53],due
to the limited age range and smallsample size in valid-
ation studiesto date [N = 57 youth ages14–18].The
findings from this thematic synthesis can be used to gen-
erateitems specificto exploringthe experiencesof
service-users who are transitioning between CAMHS to
AMHS, either for a revision to this survey toolor for
a new tool.For example,as shown in our synthesis,
youth haveindividualpreferencesregarding parental
involvementand thus,an item could address the ex-
tent to which individualyouth’s preference for paren-
tal involvementduring and afterthe transition were
respected and enabled.
Given the limitations identified above,further efforts
to investigateyouth experiencesand preferenceswill
need to employ recruitmentstrategies thatare able to
sample a broader range of service-users (e.g.disengaged
youth),to ensure the fulldiversity ofyouth perspective
is elicited. Future researchshould also formally
operationalize the boundaries oftransition ofCAMHS
to AMHS and be clear about the timing of feedback elic-
ited from youth.
Lastly,future research should engage youth through
participatory research methods to harness their unique
expertise and insights.Participatory research methods
have been used successfully with transition-aged youth
using mentalhealth services,with positive effectson
youth empowerment [54].Engaging young people as ac-
tive co-producers of knowledge also provides the oppor-
tunity foryoung people to identify theirprioritiesfor
their care [55],which often differ from those of service-
Broad et al.BMC Psychiatry (2017) 17:380 Page 9 of 11
systematically examining and synthesizing the perspec-
tives of youth as they transition from CAMHS to
AMHS. Overall,in this study we have synthesized the
viewsof 253 youth.The currentreview containsfour
studies [35,38,39,41]thathave notbeen included in
previous reviews [18,22,25] and provides an opportun-
ity to expand on earlier understandings to a wider popu-
lation in terms of clinical settingsand diagnostic
categories.In addition,our methodology allowed us to
compare and contrastthe experiences ofyouth across
clinicalsettingsand diagnostic categories.Though we
identified large overlap in the themesacrossour in-
cluded studieswith similarissuesbeing importantto
youth (e.g.parentalinvolvement),our synthesisalso
shows thatthe experiences and needs ofyouth are not
homogenous (e.g.desire for continued parentalinvolve-
ment versusdesirefor independence),which is an
insightthatwould notbe obtained from the individual
studiesalone.Finally,whereaspreviousreviewshave
included perspectives ofparents and service providers,
this review focuses exclusively on the distinctperspec-
tive ofyouth to enable their voices to be heard and to
highlight their potential contribution to improved design
of services.
Study limitations
Severallimitations ofthis study should be considered.
First,all primary research included in this thematic syn-
thesiswas given equalweight,even though there was
variability in the quality ofthe included literature.Due
to the reliance on convenience sampling and recruit-
mentthrough service-providers,service-usersincluded
in the studies may have been less likely to have been lost
to follow-up and mighthave had more positive transi-
tion experiences.As well, it is possible thatincluded
service-users may have been ata higher levelof func-
tioning and more able to provide a narrative account of
their experiences.Also,a large number of included stud-
ies did notexplicitly consider the relationship between
the researcherand participants,which is importantto
consider as this is a vulnerable population and may have
contributed to social desirability bias.
Furthermore,some diagnosticcategoriesmay have
been over-represented,such as the large number (n = 60)
and multiple reportsof youth included with primary
diagnoses ofmood disorders [34,35].As identified in
this thematic synthesis,this is potentially problematic as
youth with differentdiagnoses may have differentper-
spectives of transition.As well,almost allof the studies
originated from theUnited Kingdom or the United
States.However,although these two health care system
differ greatly,there wassignificantoverlap ofthemes
across allstudies,indicating transferability ofyouth ex-
periences across health care systems.
Lastly,the combined reporting ofparental,service-
provider and youth perspectives in some studies made it
difficultto discern the youth perspective.This is prob-
lematic given that the views ofyouth and parents often
diverged around themes of levelof parental involvement
[6, 45],independentliving skillsor managing medical
lives independently [7].
Implications and future research
The findings of this thematic synthesis can inform train-
ing and supportsfor cliniciansin both CAMHS and
AMHS on how to create more youth-centered transi-
tions,such asimplementing flexible transition timing
and increasing system-levelcontinuity during the transi-
tion (see Table 2 for positive service experience factors).
Furthermore,the field is ready for a toolthatwould
enable broader data collection and a better understand-
ing of youth experiences in diverse contexts.Such an in-
strument,the Continuity ofCare in Children’s Mental
Health (C3MH),has been developed to measure con-
tinuity ofcare in children’s mentalhealth but may have
limited applicability for transition-aged youth [53],due
to the limited age range and smallsample size in valid-
ation studiesto date [N = 57 youth ages14–18].The
findings from this thematic synthesis can be used to gen-
erateitems specificto exploringthe experiencesof
service-users who are transitioning between CAMHS to
AMHS, either for a revision to this survey toolor for
a new tool.For example,as shown in our synthesis,
youth haveindividualpreferencesregarding parental
involvementand thus,an item could address the ex-
tent to which individualyouth’s preference for paren-
tal involvementduring and afterthe transition were
respected and enabled.
Given the limitations identified above,further efforts
to investigateyouth experiencesand preferenceswill
need to employ recruitmentstrategies thatare able to
sample a broader range of service-users (e.g.disengaged
youth),to ensure the fulldiversity ofyouth perspective
is elicited. Future researchshould also formally
operationalize the boundaries oftransition ofCAMHS
to AMHS and be clear about the timing of feedback elic-
ited from youth.
Lastly,future research should engage youth through
participatory research methods to harness their unique
expertise and insights.Participatory research methods
have been used successfully with transition-aged youth
using mentalhealth services,with positive effectson
youth empowerment [54].Engaging young people as ac-
tive co-producers of knowledge also provides the oppor-
tunity foryoung people to identify theirprioritiesfor
their care [55],which often differ from those of service-
Broad et al.BMC Psychiatry (2017) 17:380 Page 9 of 11
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
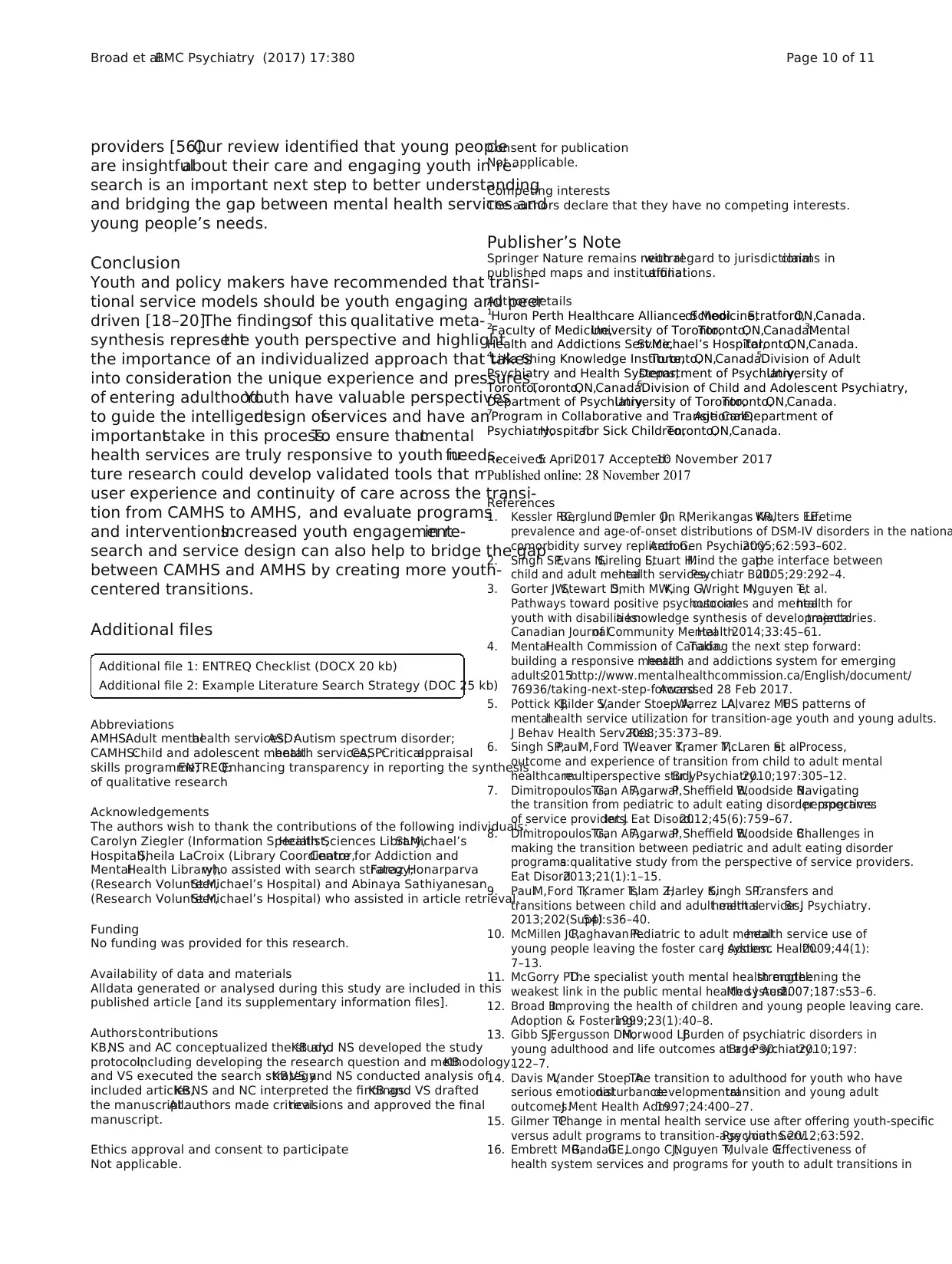
providers [56].Our review identified that young people
are insightfulabout their care and engaging youth in re-
search is an important next step to better understanding
and bridging the gap between mental health services and
young people’s needs.
Conclusion
Youth and policy makers have recommended that transi-
tional service models should be youth engaging and peer
driven [18–20].The findingsof this qualitative meta-
synthesis representthe youth perspective and highlight
the importance of an individualized approach that takes
into consideration the unique experience and pressures
of entering adulthood.Youth have valuable perspectives
to guide the intelligentdesign ofservices and have an
importantstake in this process.To ensure thatmental
health services are truly responsive to youth needs,fu-
ture research could develop validated tools that measure
user experience and continuity of care across the transi-
tion from CAMHS to AMHS, and evaluate programs
and interventions.Increased youth engagementin re-
search and service design can also help to bridge the gap
between CAMHS and AMHS by creating more youth-
centered transitions.
Additional files
Additional file 1: ENTREQ Checklist (DOCX 20 kb)
Additional file 2: Example Literature Search Strategy (DOC 25 kb)
Abbreviations
AMHS:Adult mentalhealth services;ASD:Autism spectrum disorder;
CAMHS:Child and adolescent mentalhealth services;CASP:Criticalappraisal
skills programme;ENTREQ:Enhancing transparency in reporting the synthesis
of qualitative research
Acknowledgements
The authors wish to thank the contributions of the following individuals:
Carolyn Ziegler (Information Specialist,Health Sciences Library,St.Michael’s
Hospital),Sheila LaCroix (Library Coordinator,Centre for Addiction and
MentalHealth Library),who assisted with search strategy;Faraz Honarparva
(Research Volunteer,St.Michael’s Hospital) and Abinaya Sathiyanesan
(Research Volunteer,St.Michael’s Hospital) who assisted in article retrieval.
Funding
No funding was provided for this research.
Availability of data and materials
Alldata generated or analysed during this study are included in this
published article [and its supplementary information files].
Authors’contributions
KB,NS and AC conceptualized the study.KB and NS developed the study
protocol,including developing the research question and methodology.KB
and VS executed the search strategy.KB,VS and NS conducted analysis of
included articles.KB,NS and NC interpreted the findings.KB and VS drafted
the manuscript.Allauthors made criticalrevisions and approved the final
manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutralwith regard to jurisdictionalclaims in
published maps and institutionalaffiliations.
Author details
1Huron Perth Healthcare Alliance Schoolof Medicine,Stratford,ON,Canada.
2Faculty of Medicine,University of Toronto,Toronto,ON,Canada.3Mental
Health and Addictions Service,St.Michael’s Hospital,Toronto,ON,Canada.
4Li Ka Shing Knowledge Institute,Toronto,ON,Canada.5Division of Adult
Psychiatry and Health Systems,Department of Psychiatry,University of
Toronto,Toronto,ON,Canada.6Division of Child and Adolescent Psychiatry,
Department of Psychiatry,University of Toronto,Toronto,ON,Canada.
7Program in Collaborative and TransitionalAge Care,Department of
Psychiatry,Hospitalfor Sick Children,Toronto,ON,Canada.
Received:5 April2017 Accepted:10 November 2017
References
1. Kessler RC,Berglund P,Demler O,Jin R,Merikangas KR,Walters EE.Lifetime
prevalence and age-of-onset distributions of DSM-IV disorders in the nationa
comorbidity survey replication.Arch Gen Psychiatry.2005;62:593–602.
2. Singh SP,Evans N,Sireling L,Stuart H.Mind the gap:the interface between
child and adult mentalhealth services.Psychiatr Bull.2005;29:292–4.
3. Gorter JW,Stewart D,Smith MW,King G,Wright M,Nguyen T,et al.
Pathways toward positive psychosocialoutcomes and mentalhealth for
youth with disabilities:a knowledge synthesis of developmentaltrajectories.
Canadian Journalof Community MentalHealth.2014;33:45–61.
4. MentalHealth Commission of Canada.Taking the next step forward:
building a responsive mentalhealth and addictions system for emerging
adults.2015.http://www.mentalhealthcommission.ca/English/document/
76936/taking-next-step-forward.Accessed 28 Feb 2017.
5. Pottick KJ,Bilder S,Vander Stoep A,Warrez LA,Alvarez MF.US patterns of
mentalhealth service utilization for transition-age youth and young adults.
J Behav Health Serv Res.2008;35:373–89.
6. Singh SP,PaulM,Ford T,Weaver T,Kramer T,McLaren S,et al.Process,
outcome and experience of transition from child to adult mental
healthcare:multiperspective study.Br J Psychiatry.2010;197:305–12.
7. Dimitropoulos G,Tran AF,AgarwalP,Sheffield B,Woodside B.Navigating
the transition from pediatric to adult eating disorder programs:perspectives
of service providers.Int J Eat Disord.2012;45(6):759–67.
8. Dimitropoulos G,Tran AF,AgarwalP,Sheffield B,Woodside B.Challenges in
making the transition between pediatric and adult eating disorder
programs:a qualitative study from the perspective of service providers.
Eat Disord.2013;21(1):1–15.
9. PaulM,Ford T,Kramer T,Islam Z,Harley K,Singh SP.Transfers and
transitions between child and adult mentalhealth services.Br J Psychiatry.
2013;202(Suppl54):s36–40.
10. McMillen JC,Raghavan R.Pediatric to adult mentalhealth service use of
young people leaving the foster care system.J Adolesc Health.2009;44(1):
7–13.
11. McGorry PD.The specialist youth mental health model:strengthening the
weakest link in the public mental health system.Med J Aust.2007;187:s53–6.
12. Broad B.Improving the health of children and young people leaving care.
Adoption & Fostering.1999;23(1):40–8.
13. Gibb SJ,Fergusson DM,Horwood LJ.Burden of psychiatric disorders in
young adulthood and life outcomes at age 30.Br J Psychiatry.2010;197:
122–7.
14. Davis M,Vander Stoep A.The transition to adulthood for youth who have
serious emotionaldisturbance:developmentaltransition and young adult
outcomes.J Ment Health Adm.1997;24:400–27.
15. Gilmer TP.Change in mental health service use after offering youth-specific
versus adult programs to transition-age youths.Psychiatr Serv.2012;63:592.
16. Embrett MG,RandallGE,Longo CJ,Nguyen T,Mulvale G.Effectiveness of
health system services and programs for youth to adult transitions in
Broad et al.BMC Psychiatry (2017) 17:380 Page 10 of 11
are insightfulabout their care and engaging youth in re-
search is an important next step to better understanding
and bridging the gap between mental health services and
young people’s needs.
Conclusion
Youth and policy makers have recommended that transi-
tional service models should be youth engaging and peer
driven [18–20].The findingsof this qualitative meta-
synthesis representthe youth perspective and highlight
the importance of an individualized approach that takes
into consideration the unique experience and pressures
of entering adulthood.Youth have valuable perspectives
to guide the intelligentdesign ofservices and have an
importantstake in this process.To ensure thatmental
health services are truly responsive to youth needs,fu-
ture research could develop validated tools that measure
user experience and continuity of care across the transi-
tion from CAMHS to AMHS, and evaluate programs
and interventions.Increased youth engagementin re-
search and service design can also help to bridge the gap
between CAMHS and AMHS by creating more youth-
centered transitions.
Additional files
Additional file 1: ENTREQ Checklist (DOCX 20 kb)
Additional file 2: Example Literature Search Strategy (DOC 25 kb)
Abbreviations
AMHS:Adult mentalhealth services;ASD:Autism spectrum disorder;
CAMHS:Child and adolescent mentalhealth services;CASP:Criticalappraisal
skills programme;ENTREQ:Enhancing transparency in reporting the synthesis
of qualitative research
Acknowledgements
The authors wish to thank the contributions of the following individuals:
Carolyn Ziegler (Information Specialist,Health Sciences Library,St.Michael’s
Hospital),Sheila LaCroix (Library Coordinator,Centre for Addiction and
MentalHealth Library),who assisted with search strategy;Faraz Honarparva
(Research Volunteer,St.Michael’s Hospital) and Abinaya Sathiyanesan
(Research Volunteer,St.Michael’s Hospital) who assisted in article retrieval.
Funding
No funding was provided for this research.
Availability of data and materials
Alldata generated or analysed during this study are included in this
published article [and its supplementary information files].
Authors’contributions
KB,NS and AC conceptualized the study.KB and NS developed the study
protocol,including developing the research question and methodology.KB
and VS executed the search strategy.KB,VS and NS conducted analysis of
included articles.KB,NS and NC interpreted the findings.KB and VS drafted
the manuscript.Allauthors made criticalrevisions and approved the final
manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutralwith regard to jurisdictionalclaims in
published maps and institutionalaffiliations.
Author details
1Huron Perth Healthcare Alliance Schoolof Medicine,Stratford,ON,Canada.
2Faculty of Medicine,University of Toronto,Toronto,ON,Canada.3Mental
Health and Addictions Service,St.Michael’s Hospital,Toronto,ON,Canada.
4Li Ka Shing Knowledge Institute,Toronto,ON,Canada.5Division of Adult
Psychiatry and Health Systems,Department of Psychiatry,University of
Toronto,Toronto,ON,Canada.6Division of Child and Adolescent Psychiatry,
Department of Psychiatry,University of Toronto,Toronto,ON,Canada.
7Program in Collaborative and TransitionalAge Care,Department of
Psychiatry,Hospitalfor Sick Children,Toronto,ON,Canada.
Received:5 April2017 Accepted:10 November 2017
References
1. Kessler RC,Berglund P,Demler O,Jin R,Merikangas KR,Walters EE.Lifetime
prevalence and age-of-onset distributions of DSM-IV disorders in the nationa
comorbidity survey replication.Arch Gen Psychiatry.2005;62:593–602.
2. Singh SP,Evans N,Sireling L,Stuart H.Mind the gap:the interface between
child and adult mentalhealth services.Psychiatr Bull.2005;29:292–4.
3. Gorter JW,Stewart D,Smith MW,King G,Wright M,Nguyen T,et al.
Pathways toward positive psychosocialoutcomes and mentalhealth for
youth with disabilities:a knowledge synthesis of developmentaltrajectories.
Canadian Journalof Community MentalHealth.2014;33:45–61.
4. MentalHealth Commission of Canada.Taking the next step forward:
building a responsive mentalhealth and addictions system for emerging
adults.2015.http://www.mentalhealthcommission.ca/English/document/
76936/taking-next-step-forward.Accessed 28 Feb 2017.
5. Pottick KJ,Bilder S,Vander Stoep A,Warrez LA,Alvarez MF.US patterns of
mentalhealth service utilization for transition-age youth and young adults.
J Behav Health Serv Res.2008;35:373–89.
6. Singh SP,PaulM,Ford T,Weaver T,Kramer T,McLaren S,et al.Process,
outcome and experience of transition from child to adult mental
healthcare:multiperspective study.Br J Psychiatry.2010;197:305–12.
7. Dimitropoulos G,Tran AF,AgarwalP,Sheffield B,Woodside B.Navigating
the transition from pediatric to adult eating disorder programs:perspectives
of service providers.Int J Eat Disord.2012;45(6):759–67.
8. Dimitropoulos G,Tran AF,AgarwalP,Sheffield B,Woodside B.Challenges in
making the transition between pediatric and adult eating disorder
programs:a qualitative study from the perspective of service providers.
Eat Disord.2013;21(1):1–15.
9. PaulM,Ford T,Kramer T,Islam Z,Harley K,Singh SP.Transfers and
transitions between child and adult mentalhealth services.Br J Psychiatry.
2013;202(Suppl54):s36–40.
10. McMillen JC,Raghavan R.Pediatric to adult mentalhealth service use of
young people leaving the foster care system.J Adolesc Health.2009;44(1):
7–13.
11. McGorry PD.The specialist youth mental health model:strengthening the
weakest link in the public mental health system.Med J Aust.2007;187:s53–6.
12. Broad B.Improving the health of children and young people leaving care.
Adoption & Fostering.1999;23(1):40–8.
13. Gibb SJ,Fergusson DM,Horwood LJ.Burden of psychiatric disorders in
young adulthood and life outcomes at age 30.Br J Psychiatry.2010;197:
122–7.
14. Davis M,Vander Stoep A.The transition to adulthood for youth who have
serious emotionaldisturbance:developmentaltransition and young adult
outcomes.J Ment Health Adm.1997;24:400–27.
15. Gilmer TP.Change in mental health service use after offering youth-specific
versus adult programs to transition-age youths.Psychiatr Serv.2012;63:592.
16. Embrett MG,RandallGE,Longo CJ,Nguyen T,Mulvale G.Effectiveness of
health system services and programs for youth to adult transitions in
Broad et al.BMC Psychiatry (2017) 17:380 Page 10 of 11
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
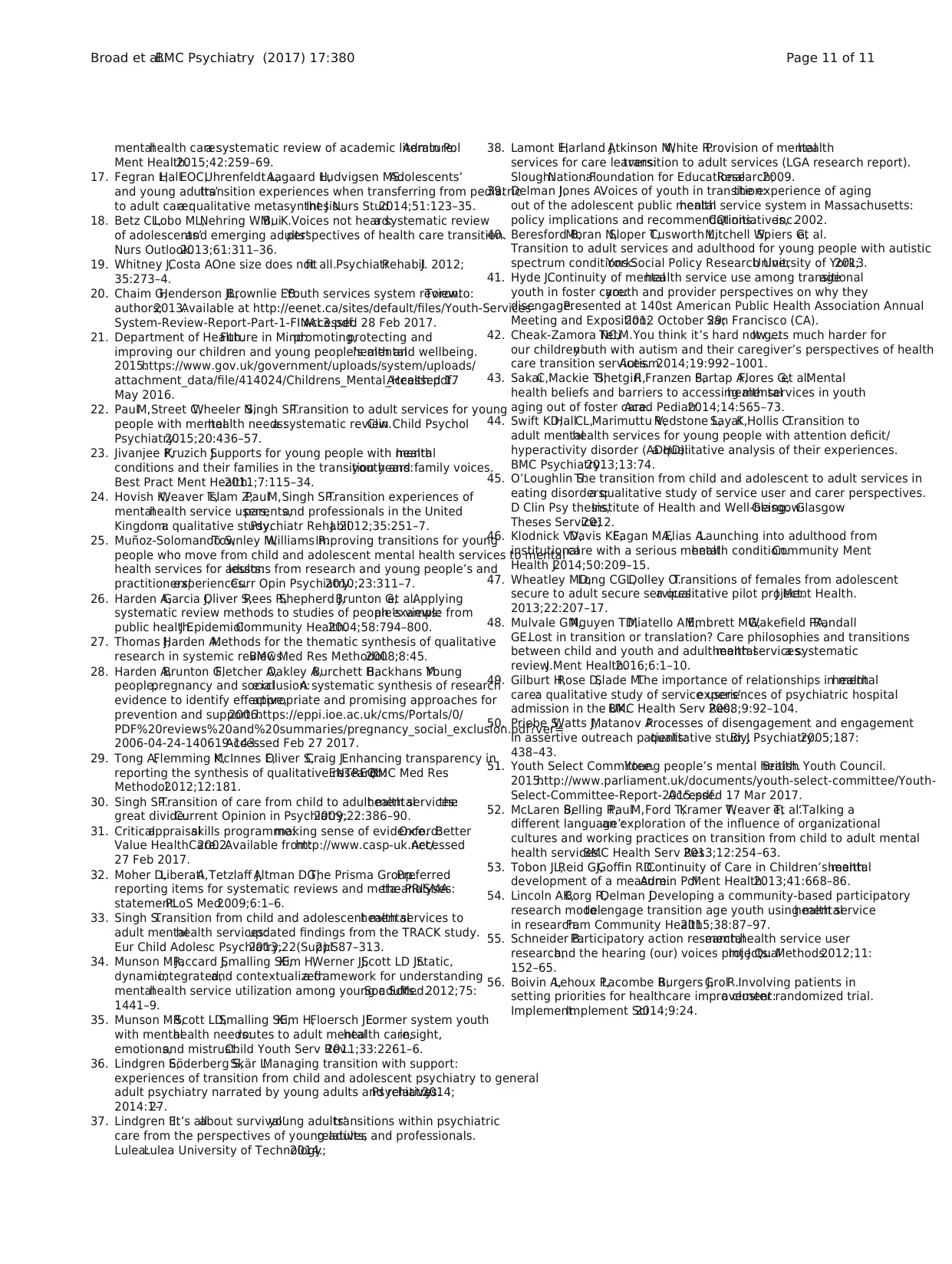
mentalhealth care:a systematic review of academic literature.Admin Pol
Ment Health.2015;42:259–69.
17. Fegran L,HallEOC,Uhrenfeldt L,Aagaard H,Ludvigsen MS.Adolescents’
and young adults’transition experiences when transferring from pediatric
to adult care:a qualitative metasynthesis.Int J Nurs Stud.2014;51:123–35.
18. Betz CL,Lobo ML,Nehring WM,BuiK.Voices not heard:a systematic review
of adolescents’and emerging adults’perspectives of health care transition.
Nurs Outlook.2013;61:311–36.
19. Whitney J,Costa A.One size does notfit all.PsychiatrRehabilJ. 2012;
35:273–4.
20. Chaim G,Henderson JL,Brownlie EB.Youth services system review.Toronto:
authors;2013.Available at http://eenet.ca/sites/default/files/Youth-Services-
System-Review-Report-Part-1-FINAL3.pdf.Accessed 28 Feb 2017.
21. Department of Health.Future in Mind:promoting,protecting and
improving our children and young people’s mentalhealth and wellbeing.
2015.https://www.gov.uk/government/uploads/system/uploads/
attachment_data/file/414024/Childrens_Mental_Health.pdf.Accessed 17
May 2016.
22. PaulM,Street C,Wheeler N,Singh SP.Transition to adult services for young
people with mentalhealth needs:a systematic review.Clin Child Psychol
Psychiatry.2015;20:436–57.
23. Jivanjee P,Kruzich J.Supports for young people with mentalhealth
conditions and their families in the transition years:youth and family voices.
Best Pract Ment Health.2011;7:115–34.
24. Hovish K,Weaver T,Islam Z,PaulM,Singh SP.Transition experiences of
mentalhealth service users,parents,and professionals in the United
Kingdom:a qualitative study.Psychiatr RehabilJ. 2012;35:251–7.
25. Muñoz-Solomando S,Townley M,Williams R.Improving transitions for young
people who move from child and adolescent mental health services to mental
health services for adults:lessons from research and young people’s and
practitioners’experiences.Curr Opin Psychiatry.2010;23:311–7.
26. Harden A,Garcia J,Oliver S,Rees R,Shepherd J,Brunton G,et al.Applying
systematic review methods to studies of people’s views:an example from
public health.J EpidemiolCommunity Health.2004;58:794–800.
27. Thomas J,Harden A.Methods for the thematic synthesis of qualitative
research in systemic reviews.BMC Med Res Methodol.2008;8:45.
28. Harden A,Brunton G,Fletcher A,Oakley A,Burchett H,Backhans M.Young
people,pregnancy and socialexclusion:A systematic synthesis of research
evidence to identify effective,appropriate and promising approaches for
prevention and support.2006.https://eppi.ioe.ac.uk/cms/Portals/0/
PDF%20reviews%20and%20summaries/pregnancy_social_exclusion.pdf?ver=
2006-04-24-140619-143.Accessed Feb 27 2017.
29. Tong A,Flemming K,McInnes E,Oliver S,Craig J.Enhancing transparency in
reporting the synthesis of qualitative research:ENTREQ.BMC Med Res
Methodol.2012;12:181.
30. Singh SP.Transition of care from child to adult mentalhealth services:the
great divide.Current Opinion in Psychiatry.2009;22:386–90.
31. Criticalappraisalskills programme:making sense of evidence.Oxford:Better
Value HealthCare.2002.Available from:http://www.casp-uk.net/.Accessed
27 Feb 2017.
32. Moher D,LiberatiA,Tetzlaff J,Altman DG,The Prisma Group.Preferred
reporting items for systematic reviews and meta-analyses:the PRISMA
statement.PLoS Med.2009;6:1–6.
33. Singh S.Transition from child and adolescent mentalhealth services to
adult mentalhealth services:updated findings from the TRACK study.
Eur Child Adolesc Psychiatry.2013;22(Suppl2):S87–313.
34. Munson MR,Jaccard J,Smalling SE,Kim H,Werner JJ,Scott LD Jr.Static,
dynamic,integrated,and contextualized:a framework for understanding
mentalhealth service utilization among young adults.Soc SciMed.2012;75:
1441–9.
35. Munson MR,Scott LD,Smalling SE,Kim H,Floersch JE.Former system youth
with mentalhealth needs:routes to adult mentalhealth care,insight,
emotions,and mistrust.Child Youth Serv Rev.2011;33:2261–6.
36. Lindgren E,Söderberg S,Skär L.Managing transition with support:
experiences of transition from child and adolescent psychiatry to general
adult psychiatry narrated by young adults and relatives.Psychiatry.2014;
2014:1–27.
37. Lindgren E.‘It’s allabout survival’young adults’transitions within psychiatric
care from the perspectives of young adults,relatives and professionals.
Lulea:Lulea University of Technology;2014.
38. Lamont E,Harland J,Atkinson M,White R.Provision of mentalhealth
services for care leavers:transition to adult services (LGA research report).
Slough:NationalFoundation for EducationalResearch;2009.
39. Delman J,Jones A.Voices of youth in transition:the experience of aging
out of the adolescent public mentalhealth service system in Massachusetts:
policy implications and recommendations.CQIinitiatives,inc.2002.
40. Beresford B,Moran N,Sloper T,Cusworth L,Mitchell W,Spiers G,et al.
Transition to adult services and adulthood for young people with autistic
spectrum conditions.York:Social Policy Research Unit,University of York;2013.
41. Hyde J.Continuity of mentalhealth service use among transitionalage
youth in foster care:youth and provider perspectives on why they
disengage.Presented at 140st American Public Health Association Annual
Meeting and Exposition;2012 October 29;San Francisco (CA).
42. Cheak-Zamora NC,TetiM.You think it’s hard now ...It gets much harder for
our children’:youth with autism and their caregiver’s perspectives of health
care transition services.Autism.2014;19:992–1001.
43. SakaiC,Mackie TI,ShetgiriR,Franzen S,Partap A,Flores G,et al.Mental
health beliefs and barriers to accessing mentalhealth services in youth
aging out of foster care.Acad Pediatr.2014;14:565–73.
44. Swift KD,HallCL,Marimuttu V,Redstone L,SayalK,Hollis C.Transition to
adult mentalhealth services for young people with attention deficit/
hyperactivity disorder (ADHD):a qualitative analysis of their experiences.
BMC Psychiatry.2013;13:74.
45. O’Loughlin S.The transition from child and adolescent to adult services in
eating disorders:a qualitative study of service user and carer perspectives.
D Clin Psy thesis,Institute of Health and Well-being.Glasgow:Glasgow
Theses Service;2012.
46. Klodnick VV,Davis KE,Fagan MA,Elias A.Launching into adulthood from
institutionalcare with a serious mentalhealth condition.Community Ment
Health J.2014;50:209–15.
47. Wheatley MD,Long CGL,Dolley O.Transitions of females from adolescent
secure to adult secure services:a qualitative pilot project.J Ment Health.
2013;22:207–17.
48. Mulvale GM,Nguyen TD,Miatello AM,Embrett MG,Wakefield PA,Randall
GE.Lost in transition or translation? Care philosophies and transitions
between child and youth and adult mentalhealth services:a systematic
review.J Ment Health.2016;6:1–10.
49. Gilburt H,Rose D,Slade M.The importance of relationships in mentalhealth
care:a qualitative study of service users’experiences of psychiatric hospital
admission in the UK.BMC Health Serv Res.2008;9:92–104.
50. Priebe S,Watts J,Matanov A.Processes of disengagement and engagement
in assertive outreach patients:qualitative study.Br J Psychiatry.2005;187:
438–43.
51. Youth Select Committee.Young people’s mental health.British Youth Council.
2015.http://www.parliament.uk/documents/youth-select-committee/Youth-
Select-Committee-Report-2015.pdf.Accessed 17 Mar 2017.
52. McLaren S,Belling R,PaulM,Ford T,Kramer T,Weaver T,et al.‘Talking a
different language’:an exploration of the influence of organizational
cultures and working practices on transition from child to adult mental
health services.BMC Health Serv Res.2013;12:254–63.
53. Tobon JL,Reid GJ,Goffin RD.Continuity of Care in Children’s mentalhealth:
development of a measure.Admin PolMent Health.2013;41:668–86.
54. Lincoln AK,Borg R,Delman J.Developing a community-based participatory
research modelto engage transition age youth using mentalhealth service
in research.Fam Community Health.2015;38:87–97.
55. Schneider B.Participatory action research,mentalhealth service user
research,and the hearing (our) voices projects.Int J QualMethods.2012;11:
152–65.
56. Boivin A,Lehoux P,Lacombe R,Burgers J,GrolR.Involving patients in
setting priorities for healthcare improvement:a cluster randomized trial.
Implement.Implement Sci2014;9:24.
Broad et al.BMC Psychiatry (2017) 17:380 Page 11 of 11
Ment Health.2015;42:259–69.
17. Fegran L,HallEOC,Uhrenfeldt L,Aagaard H,Ludvigsen MS.Adolescents’
and young adults’transition experiences when transferring from pediatric
to adult care:a qualitative metasynthesis.Int J Nurs Stud.2014;51:123–35.
18. Betz CL,Lobo ML,Nehring WM,BuiK.Voices not heard:a systematic review
of adolescents’and emerging adults’perspectives of health care transition.
Nurs Outlook.2013;61:311–36.
19. Whitney J,Costa A.One size does notfit all.PsychiatrRehabilJ. 2012;
35:273–4.
20. Chaim G,Henderson JL,Brownlie EB.Youth services system review.Toronto:
authors;2013.Available at http://eenet.ca/sites/default/files/Youth-Services-
System-Review-Report-Part-1-FINAL3.pdf.Accessed 28 Feb 2017.
21. Department of Health.Future in Mind:promoting,protecting and
improving our children and young people’s mentalhealth and wellbeing.
2015.https://www.gov.uk/government/uploads/system/uploads/
attachment_data/file/414024/Childrens_Mental_Health.pdf.Accessed 17
May 2016.
22. PaulM,Street C,Wheeler N,Singh SP.Transition to adult services for young
people with mentalhealth needs:a systematic review.Clin Child Psychol
Psychiatry.2015;20:436–57.
23. Jivanjee P,Kruzich J.Supports for young people with mentalhealth
conditions and their families in the transition years:youth and family voices.
Best Pract Ment Health.2011;7:115–34.
24. Hovish K,Weaver T,Islam Z,PaulM,Singh SP.Transition experiences of
mentalhealth service users,parents,and professionals in the United
Kingdom:a qualitative study.Psychiatr RehabilJ. 2012;35:251–7.
25. Muñoz-Solomando S,Townley M,Williams R.Improving transitions for young
people who move from child and adolescent mental health services to mental
health services for adults:lessons from research and young people’s and
practitioners’experiences.Curr Opin Psychiatry.2010;23:311–7.
26. Harden A,Garcia J,Oliver S,Rees R,Shepherd J,Brunton G,et al.Applying
systematic review methods to studies of people’s views:an example from
public health.J EpidemiolCommunity Health.2004;58:794–800.
27. Thomas J,Harden A.Methods for the thematic synthesis of qualitative
research in systemic reviews.BMC Med Res Methodol.2008;8:45.
28. Harden A,Brunton G,Fletcher A,Oakley A,Burchett H,Backhans M.Young
people,pregnancy and socialexclusion:A systematic synthesis of research
evidence to identify effective,appropriate and promising approaches for
prevention and support.2006.https://eppi.ioe.ac.uk/cms/Portals/0/
PDF%20reviews%20and%20summaries/pregnancy_social_exclusion.pdf?ver=
2006-04-24-140619-143.Accessed Feb 27 2017.
29. Tong A,Flemming K,McInnes E,Oliver S,Craig J.Enhancing transparency in
reporting the synthesis of qualitative research:ENTREQ.BMC Med Res
Methodol.2012;12:181.
30. Singh SP.Transition of care from child to adult mentalhealth services:the
great divide.Current Opinion in Psychiatry.2009;22:386–90.
31. Criticalappraisalskills programme:making sense of evidence.Oxford:Better
Value HealthCare.2002.Available from:http://www.casp-uk.net/.Accessed
27 Feb 2017.
32. Moher D,LiberatiA,Tetzlaff J,Altman DG,The Prisma Group.Preferred
reporting items for systematic reviews and meta-analyses:the PRISMA
statement.PLoS Med.2009;6:1–6.
33. Singh S.Transition from child and adolescent mentalhealth services to
adult mentalhealth services:updated findings from the TRACK study.
Eur Child Adolesc Psychiatry.2013;22(Suppl2):S87–313.
34. Munson MR,Jaccard J,Smalling SE,Kim H,Werner JJ,Scott LD Jr.Static,
dynamic,integrated,and contextualized:a framework for understanding
mentalhealth service utilization among young adults.Soc SciMed.2012;75:
1441–9.
35. Munson MR,Scott LD,Smalling SE,Kim H,Floersch JE.Former system youth
with mentalhealth needs:routes to adult mentalhealth care,insight,
emotions,and mistrust.Child Youth Serv Rev.2011;33:2261–6.
36. Lindgren E,Söderberg S,Skär L.Managing transition with support:
experiences of transition from child and adolescent psychiatry to general
adult psychiatry narrated by young adults and relatives.Psychiatry.2014;
2014:1–27.
37. Lindgren E.‘It’s allabout survival’young adults’transitions within psychiatric
care from the perspectives of young adults,relatives and professionals.
Lulea:Lulea University of Technology;2014.
38. Lamont E,Harland J,Atkinson M,White R.Provision of mentalhealth
services for care leavers:transition to adult services (LGA research report).
Slough:NationalFoundation for EducationalResearch;2009.
39. Delman J,Jones A.Voices of youth in transition:the experience of aging
out of the adolescent public mentalhealth service system in Massachusetts:
policy implications and recommendations.CQIinitiatives,inc.2002.
40. Beresford B,Moran N,Sloper T,Cusworth L,Mitchell W,Spiers G,et al.
Transition to adult services and adulthood for young people with autistic
spectrum conditions.York:Social Policy Research Unit,University of York;2013.
41. Hyde J.Continuity of mentalhealth service use among transitionalage
youth in foster care:youth and provider perspectives on why they
disengage.Presented at 140st American Public Health Association Annual
Meeting and Exposition;2012 October 29;San Francisco (CA).
42. Cheak-Zamora NC,TetiM.You think it’s hard now ...It gets much harder for
our children’:youth with autism and their caregiver’s perspectives of health
care transition services.Autism.2014;19:992–1001.
43. SakaiC,Mackie TI,ShetgiriR,Franzen S,Partap A,Flores G,et al.Mental
health beliefs and barriers to accessing mentalhealth services in youth
aging out of foster care.Acad Pediatr.2014;14:565–73.
44. Swift KD,HallCL,Marimuttu V,Redstone L,SayalK,Hollis C.Transition to
adult mentalhealth services for young people with attention deficit/
hyperactivity disorder (ADHD):a qualitative analysis of their experiences.
BMC Psychiatry.2013;13:74.
45. O’Loughlin S.The transition from child and adolescent to adult services in
eating disorders:a qualitative study of service user and carer perspectives.
D Clin Psy thesis,Institute of Health and Well-being.Glasgow:Glasgow
Theses Service;2012.
46. Klodnick VV,Davis KE,Fagan MA,Elias A.Launching into adulthood from
institutionalcare with a serious mentalhealth condition.Community Ment
Health J.2014;50:209–15.
47. Wheatley MD,Long CGL,Dolley O.Transitions of females from adolescent
secure to adult secure services:a qualitative pilot project.J Ment Health.
2013;22:207–17.
48. Mulvale GM,Nguyen TD,Miatello AM,Embrett MG,Wakefield PA,Randall
GE.Lost in transition or translation? Care philosophies and transitions
between child and youth and adult mentalhealth services:a systematic
review.J Ment Health.2016;6:1–10.
49. Gilburt H,Rose D,Slade M.The importance of relationships in mentalhealth
care:a qualitative study of service users’experiences of psychiatric hospital
admission in the UK.BMC Health Serv Res.2008;9:92–104.
50. Priebe S,Watts J,Matanov A.Processes of disengagement and engagement
in assertive outreach patients:qualitative study.Br J Psychiatry.2005;187:
438–43.
51. Youth Select Committee.Young people’s mental health.British Youth Council.
2015.http://www.parliament.uk/documents/youth-select-committee/Youth-
Select-Committee-Report-2015.pdf.Accessed 17 Mar 2017.
52. McLaren S,Belling R,PaulM,Ford T,Kramer T,Weaver T,et al.‘Talking a
different language’:an exploration of the influence of organizational
cultures and working practices on transition from child to adult mental
health services.BMC Health Serv Res.2013;12:254–63.
53. Tobon JL,Reid GJ,Goffin RD.Continuity of Care in Children’s mentalhealth:
development of a measure.Admin PolMent Health.2013;41:668–86.
54. Lincoln AK,Borg R,Delman J.Developing a community-based participatory
research modelto engage transition age youth using mentalhealth service
in research.Fam Community Health.2015;38:87–97.
55. Schneider B.Participatory action research,mentalhealth service user
research,and the hearing (our) voices projects.Int J QualMethods.2012;11:
152–65.
56. Boivin A,Lehoux P,Lacombe R,Burgers J,GrolR.Involving patients in
setting priorities for healthcare improvement:a cluster randomized trial.
Implement.Implement Sci2014;9:24.
Broad et al.BMC Psychiatry (2017) 17:380 Page 11 of 11
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

