Quality Management in a Care Setting: Outcomes, CQI, and Belbin
VerifiedAdded on 2022/11/28
|14
|5011
|50
Report
AI Summary
This report delves into the critical aspects of quality management within care settings, emphasizing the achievement of optimal outcomes for service users. It begins by defining outcome-based care, exploring its significance, and analyzing relevant government policies that drive its implementation. The report highlights the benefits of this approach, such as patient-centered care and improved service integration, while also addressing challenges like limited data analytics capabilities and organizational structure issues. Furthermore, it examines the application of the Belbin theory to assess and enhance team performance in continuous quality improvement (CQI) initiatives. The report also discusses the importance of person-centered care and the tools required for CQI in healthcare, providing a comprehensive overview of strategies, structures, and systems that promote the rights and diversity of service users.
Quality Management in a
Care Setting
Care Setting
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION...........................................................................................................................3
MAIN BODY..................................................................................................................................3
Question 1........................................................................................................................................3
Care settings achieving the best possible outcome for users of service in their care..................3
Question 2........................................................................................................................................7
Belbin theory as reference for discussing the performance of the team in Continuous Quality
Improvement (CQI) in the care setting........................................................................................7
Question 3......................................................................................................................................10
Reflection...................................................................................................................................10
CONCLUSION..............................................................................................................................13
REFERENCES..............................................................................................................................14
INTRODUCTION...........................................................................................................................3
MAIN BODY..................................................................................................................................3
Question 1........................................................................................................................................3
Care settings achieving the best possible outcome for users of service in their care..................3
Question 2........................................................................................................................................7
Belbin theory as reference for discussing the performance of the team in Continuous Quality
Improvement (CQI) in the care setting........................................................................................7
Question 3......................................................................................................................................10
Reflection...................................................................................................................................10
CONCLUSION..............................................................................................................................13
REFERENCES..............................................................................................................................14
INTRODUCTION
The essay is about the importance outcomes that need to be achieved by the care setting for the
service users. The outcome based care is explained the importance of the outcome-based
healthcare is described. The importance of outcome-based healthcare for the Soma healthcare is
discussed. The government policies that drive the outcome-based healthcare are discussed. The
benefits of the outcome-based healthcare are discussed. The challenge faced by the healthcare for
adopting the outcome-based healthcare is discussed. The healthcare with the outcome-based
healthcare approach is made person-centered by the teams is discussed. The Belbin theory as the
reference for discussing the team performance in continuous quality improvement in the care
setting is discussed. The tools required for the Continuous Quality Improvement (CQI) in the
healthcare setting are discussed. The reflective model is used for evaluating the strategies,
structures and systems that are used in the health and the social care practices are discussed that
promote the right, responsibility and diversity of the services users.
MAIN BODY
Question 1
Care settings achieving the best possible outcome for users of service in their care
Outcome-based care
The outcome based health care can be explained by the vast variety of spectrum strategies
that are used for transforming the fee-for-services to a value-based care. The healthcare leader
needs to embrace the outcome-based healthcare for surviving in the transition to the value- based
care. The healthcare also has to face many challenges for switching in the value-based approach
in delivering the care services. If the ultimate goal of health care is saving lives of people then
the healthcare should embrace the outcome-based healthcare. The outcome-based healthcare is
the primary beneficiaries to the patient population they are serving. The benefit to the Soma
health cares by adopting the outcome-based healthcare is that it provides the patient-centred
vision that is able to successfully motivate the health care for doing whatever they want to do.
The Soma health care wants to provide its user the best possible services but the FFS model is
3
The essay is about the importance outcomes that need to be achieved by the care setting for the
service users. The outcome based care is explained the importance of the outcome-based
healthcare is described. The importance of outcome-based healthcare for the Soma healthcare is
discussed. The government policies that drive the outcome-based healthcare are discussed. The
benefits of the outcome-based healthcare are discussed. The challenge faced by the healthcare for
adopting the outcome-based healthcare is discussed. The healthcare with the outcome-based
healthcare approach is made person-centered by the teams is discussed. The Belbin theory as the
reference for discussing the team performance in continuous quality improvement in the care
setting is discussed. The tools required for the Continuous Quality Improvement (CQI) in the
healthcare setting are discussed. The reflective model is used for evaluating the strategies,
structures and systems that are used in the health and the social care practices are discussed that
promote the right, responsibility and diversity of the services users.
MAIN BODY
Question 1
Care settings achieving the best possible outcome for users of service in their care
Outcome-based care
The outcome based health care can be explained by the vast variety of spectrum strategies
that are used for transforming the fee-for-services to a value-based care. The healthcare leader
needs to embrace the outcome-based healthcare for surviving in the transition to the value- based
care. The healthcare also has to face many challenges for switching in the value-based approach
in delivering the care services. If the ultimate goal of health care is saving lives of people then
the healthcare should embrace the outcome-based healthcare. The outcome-based healthcare is
the primary beneficiaries to the patient population they are serving. The benefit to the Soma
health cares by adopting the outcome-based healthcare is that it provides the patient-centred
vision that is able to successfully motivate the health care for doing whatever they want to do.
The Soma health care wants to provide its user the best possible services but the FFS model is
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
interfering in the main goal from being achieved by the healthcare (Krishna, Valleru and Smith,
2019). Instead of saving lives as well as providing the best services to the user the health care is
stuck in managing the inefficiencies and solving problems.
The outcome-based healthcare will be the ideal path for the Soma health care for
restoring the systems of healthcare, the ability to deliver the promised services to the user and the
Soma health care require an attainable and approachable guide for making the switch. Soma
health care can develop the outcome- based healthcare only when they have calculated, have
thoughtful restructuring for meeting the future as well as current needs and also provide with the
on-going framework that drive the continuous improvement.
Government policies in the outcome-based care
The agreement is made by the government for the care services that include increasing
emphasis on the patient outcomes. The agreement did not demand for the radical reform instead
it will demand the healthcare with the well managed and well-resourced process for continuous
improvement and supported by development in the enhanced outcome indicator (Whiteford and
Weissman, 2017). The Ministry of Healthcare of Netherlandsstructured four objectives that are:
putting more insight in the outcomes, making more shared decisions, the funding as well as the
organisation of the care will be focused on the outcomes and the access to up-to-date as well as
relevant outcomes of information.
For delivering the committed services, the government is working closely with the hospital
alliances, advisory groups, and international consortia and with the range of stakeholder for
developing the key metrics along with robust base of knowledge of what is working, what needs
to happen and what is scaled for the outcome-based approaches for streaming in the health care
systems.
The benefits of the outcome-based healthcare
The healthcare having the outcome-based approach in the care services have following
benefits: The services are provided to the patients at the healthcare that are producing meaningful
outcomes. Help in building different relationship with the public as well as the patients for
involving them in maximising the value for more resources. The experience of the services user
and patient is improved by promoting the integration of the services as well as reducing the
fragmentation. More emphasis is placed in prevention with incentives for working in partnership.
Releasing innovative potential in the providers and the clinicians are taking more responsibility
4
2019). Instead of saving lives as well as providing the best services to the user the health care is
stuck in managing the inefficiencies and solving problems.
The outcome-based healthcare will be the ideal path for the Soma health care for
restoring the systems of healthcare, the ability to deliver the promised services to the user and the
Soma health care require an attainable and approachable guide for making the switch. Soma
health care can develop the outcome- based healthcare only when they have calculated, have
thoughtful restructuring for meeting the future as well as current needs and also provide with the
on-going framework that drive the continuous improvement.
Government policies in the outcome-based care
The agreement is made by the government for the care services that include increasing
emphasis on the patient outcomes. The agreement did not demand for the radical reform instead
it will demand the healthcare with the well managed and well-resourced process for continuous
improvement and supported by development in the enhanced outcome indicator (Whiteford and
Weissman, 2017). The Ministry of Healthcare of Netherlandsstructured four objectives that are:
putting more insight in the outcomes, making more shared decisions, the funding as well as the
organisation of the care will be focused on the outcomes and the access to up-to-date as well as
relevant outcomes of information.
For delivering the committed services, the government is working closely with the hospital
alliances, advisory groups, and international consortia and with the range of stakeholder for
developing the key metrics along with robust base of knowledge of what is working, what needs
to happen and what is scaled for the outcome-based approaches for streaming in the health care
systems.
The benefits of the outcome-based healthcare
The healthcare having the outcome-based approach in the care services have following
benefits: The services are provided to the patients at the healthcare that are producing meaningful
outcomes. Help in building different relationship with the public as well as the patients for
involving them in maximising the value for more resources. The experience of the services user
and patient is improved by promoting the integration of the services as well as reducing the
fragmentation. More emphasis is placed in prevention with incentives for working in partnership.
Releasing innovative potential in the providers and the clinicians are taking more responsibility
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
for increasing the value from the existing budget and deliver the outcomes required by the people
(Adida and Bravo, 2019). Facilitate the culture of integration as well as collaboration within the
providers in the health and social care economy. The health care is able to deliver better value,
remove barriers and provide sustainable services for more integrated approach. The healthcare
use contract durations that encourage investment in the prevention, working practices and
improvements in quality for delivering the savings as well as efficiencies for long term. The
duplication and transaction costs across the organisation are reduced. Only the necessary KPIs
are kept while focusing on the outcomes.
Challenges to the outcome-based healthcare
The healthcare in transition to the outcome-based healthcare is facing many difficulties
that are:
Limited analytics capabilities –the healthcare is poor in analytic as well as in healthcare data.
The healthcare needs data and actionable capabilities for succeeding in outcome-based
healthcare. The healthcare need to measure the performance for against the outcomes goals along
with measuring the effectiveness of the improvement in the strategies for the outcomes. The
inabilities of evaluating the performance as well as process along with the lack of analytics are
the barriers for the healthcare systems for moving from the FFS model to the outcome-based
approach.
Limited access to the information –the healthcare need to put the data in the hands of the
frontline staff members. The healthcare will be unable to change the working of the care services
if they do not equip the frontline workers with the information that is the data-driven insights that
is needed for getting the improved outcomes at the care services of the patients. The right
information for effectively and proactively managing the patient population is needed to be
accessed from the clinicians for claiming the data form the pharmacy (Borgonovi, Bianchi and
Rivenbark, 2019). The healthcare struggle for making the data useful and accessible, the problem
arises when the data is needed to be aggregate from other entities across the continuum. The
distribution as well as aggregating of data requires technology infrastructure along with
organisation support that the healthcare lack in having all at one place.
Inappropriate organisational structure –the healthcare organisation are not always organised
for the change. The healthcare needs an effective organisational structure for working against the
inherent inertia in the system that is driving the system back to the decades of the same FFS way.
5
(Adida and Bravo, 2019). Facilitate the culture of integration as well as collaboration within the
providers in the health and social care economy. The health care is able to deliver better value,
remove barriers and provide sustainable services for more integrated approach. The healthcare
use contract durations that encourage investment in the prevention, working practices and
improvements in quality for delivering the savings as well as efficiencies for long term. The
duplication and transaction costs across the organisation are reduced. Only the necessary KPIs
are kept while focusing on the outcomes.
Challenges to the outcome-based healthcare
The healthcare in transition to the outcome-based healthcare is facing many difficulties
that are:
Limited analytics capabilities –the healthcare is poor in analytic as well as in healthcare data.
The healthcare needs data and actionable capabilities for succeeding in outcome-based
healthcare. The healthcare need to measure the performance for against the outcomes goals along
with measuring the effectiveness of the improvement in the strategies for the outcomes. The
inabilities of evaluating the performance as well as process along with the lack of analytics are
the barriers for the healthcare systems for moving from the FFS model to the outcome-based
approach.
Limited access to the information –the healthcare need to put the data in the hands of the
frontline staff members. The healthcare will be unable to change the working of the care services
if they do not equip the frontline workers with the information that is the data-driven insights that
is needed for getting the improved outcomes at the care services of the patients. The right
information for effectively and proactively managing the patient population is needed to be
accessed from the clinicians for claiming the data form the pharmacy (Borgonovi, Bianchi and
Rivenbark, 2019). The healthcare struggle for making the data useful and accessible, the problem
arises when the data is needed to be aggregate from other entities across the continuum. The
distribution as well as aggregating of data requires technology infrastructure along with
organisation support that the healthcare lack in having all at one place.
Inappropriate organisational structure –the healthcare organisation are not always organised
for the change. The healthcare needs an effective organisational structure for working against the
inherent inertia in the system that is driving the system back to the decades of the same FFS way.
5
The healthcare leaders need to provide the strategies along with step by step guide for making
the changes in the direction to make the healthcare an outcome-based care without this it is
impossible to gain the outcome-based care in the healthcare.
Person centered care by the teams
The outcome-based care help the care worker in being more reactive and proactive, the
focus of the worker is to restore the health of the patients at the healthcare. The healthcare with
the outcome-based is more reactive towards the approach such as curing the diseases. The
healthcare operates in the reactive mode and the workers continuously ask if the patient is cured
are they doing their treatment properly. The healthcare can reduce the variation for treating
various diseases as well as conditions; this is attained by a process where all the clinicians are
provided with the accurate diagnoses as well as treatment algorithms and the patient outcome are
improved (Brooks, Winship and Kuzel, 2020). The workers strive for overcoming the
inefficiencies and provide quality care for the patients in the outcome-based approach. Along
with focusing on the health of the sick patients the outcome-based approaches also focuses on
the approaches for improving the healthcare system for maintaining healthy population as well as
prevent illness. The proactive aspect of the approach allows the healthcare to ask questions like:
How to maintain the health of the patients?
How to prevent the illness for keeping the individuals out of the healthcare?
How to operate outside the healthcare for community caring?
How to incorporate the business model according to the population health?
Conclusion
The essay is about the care setting achieving the best possible service in the care for
having better outcomes. The outcome-based care is discussed and the government policies
included in the outcome-based care are provided.
Question 2
Belbin theory as reference for discussing the performance of the team in Continuous Quality
Improvement (CQI) in the care setting
6
the changes in the direction to make the healthcare an outcome-based care without this it is
impossible to gain the outcome-based care in the healthcare.
Person centered care by the teams
The outcome-based care help the care worker in being more reactive and proactive, the
focus of the worker is to restore the health of the patients at the healthcare. The healthcare with
the outcome-based is more reactive towards the approach such as curing the diseases. The
healthcare operates in the reactive mode and the workers continuously ask if the patient is cured
are they doing their treatment properly. The healthcare can reduce the variation for treating
various diseases as well as conditions; this is attained by a process where all the clinicians are
provided with the accurate diagnoses as well as treatment algorithms and the patient outcome are
improved (Brooks, Winship and Kuzel, 2020). The workers strive for overcoming the
inefficiencies and provide quality care for the patients in the outcome-based approach. Along
with focusing on the health of the sick patients the outcome-based approaches also focuses on
the approaches for improving the healthcare system for maintaining healthy population as well as
prevent illness. The proactive aspect of the approach allows the healthcare to ask questions like:
How to maintain the health of the patients?
How to prevent the illness for keeping the individuals out of the healthcare?
How to operate outside the healthcare for community caring?
How to incorporate the business model according to the population health?
Conclusion
The essay is about the care setting achieving the best possible service in the care for
having better outcomes. The outcome-based care is discussed and the government policies
included in the outcome-based care are provided.
Question 2
Belbin theory as reference for discussing the performance of the team in Continuous Quality
Improvement (CQI) in the care setting
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Belbin says that it is important for understanding the individualitsrole in the team; this
will help the individual for developing the strengths; manage the weaknesses as a member of
team and improve the contribution of the individual in the team. The health care leaders can use
the Belbin model for creating more balanced teams. The team can be unbalanced if the members
comprising have similar styles or role in the team. The team will be weak if all the members
have the same weakness. The team having the same strengths then they are able to compete for
the team task as well as the take responsibilities that best suit their styles. Belbin identified the
nine team roles for that are divided in three groups and the team role is associated with the
interpersonal strength as well as the typical behaviour.
Action Oriented Roles
This group consist of shaper (SH), implementer (IMP) and completer-Finisher (CF).
Shaper (SH)–the shaper in the team help in the improvement and they are extroverted as well as
dynamic people who tend to stimulate other in the team for the questing the norms along with
finding the best possible way for solving the problems. The shapers are important for the team as
they find the challenges exciting and push the courage in the team when everyone is feeling like
quitting (Flores-Parra and et.al, 2018). They will continuously help in improving the team at the
care setting by implementing the changes for improving the services.
Implementer (IMP) – the implementers of the team are the one who get the things done. They
help in turning the ideas as well as concepts in the actions and plans that are practically possible.
They are the people who are conservative and disciplined for working systematically towards the
working at the care settings. These people are reliable when job need to be done.
Completer-Finisher (CF)–these are the people who make sure that the work is done completely.
These people ensure that there are no errors or omissions along with it they pay attention on the
smallest details. These people are concerned to the deadlines and make sure that the work is
completed on time by pushing the team.
People Oriented Roles
It is consist of coordinator (CO), team worker (TW) and resource investigator (RI).
Coordinator (CO)–these people take the team leader role and are also known as the chairman.
The objectives for the working are perceived by them along with guiding the members to the
objective. They are excellent at listening and have the capability to recognise the value of all the
team members. They very effectively delegate the tasks.
7
will help the individual for developing the strengths; manage the weaknesses as a member of
team and improve the contribution of the individual in the team. The health care leaders can use
the Belbin model for creating more balanced teams. The team can be unbalanced if the members
comprising have similar styles or role in the team. The team will be weak if all the members
have the same weakness. The team having the same strengths then they are able to compete for
the team task as well as the take responsibilities that best suit their styles. Belbin identified the
nine team roles for that are divided in three groups and the team role is associated with the
interpersonal strength as well as the typical behaviour.
Action Oriented Roles
This group consist of shaper (SH), implementer (IMP) and completer-Finisher (CF).
Shaper (SH)–the shaper in the team help in the improvement and they are extroverted as well as
dynamic people who tend to stimulate other in the team for the questing the norms along with
finding the best possible way for solving the problems. The shapers are important for the team as
they find the challenges exciting and push the courage in the team when everyone is feeling like
quitting (Flores-Parra and et.al, 2018). They will continuously help in improving the team at the
care setting by implementing the changes for improving the services.
Implementer (IMP) – the implementers of the team are the one who get the things done. They
help in turning the ideas as well as concepts in the actions and plans that are practically possible.
They are the people who are conservative and disciplined for working systematically towards the
working at the care settings. These people are reliable when job need to be done.
Completer-Finisher (CF)–these are the people who make sure that the work is done completely.
These people ensure that there are no errors or omissions along with it they pay attention on the
smallest details. These people are concerned to the deadlines and make sure that the work is
completed on time by pushing the team.
People Oriented Roles
It is consist of coordinator (CO), team worker (TW) and resource investigator (RI).
Coordinator (CO)–these people take the team leader role and are also known as the chairman.
The objectives for the working are perceived by them along with guiding the members to the
objective. They are excellent at listening and have the capability to recognise the value of all the
team members. They very effectively delegate the tasks.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Team worker (TW)–the team workers are the ones who provide support to the team and ensure
that the team is working efficiently. They are the negotiator of the team as they are flexible,
perceptive and diplomatic. These people are capable in their own right and are popular but
prioritise the team cohesion along with helping people for getting the work done.
Resource investigator (RI)–these people are innovative as well as the creative people of the
group. These people develop the contact, explore the options that are available and negotiate the
resources for the team. They are enthusiastic team members and are able to identify the work
with the stakeholders for helping the team accomplish the objectives. These people are
extroverted and out-going that means they react to their ideas.
Thought Oriented Roles
It consists of the plant (PL), monitor-Evaluator (ME) and specialist (SP).
Plant (PL)–plant in the tem is the innovator of the team who bring new ideas and approaches to
the team. Plants are introverted and have the tendency to work apart from the team. Plants bring
ideas so novel that they are practically impossible sometimes. They can also ignore the provide
parameters and constraints and they are poor at communication.
Monitor-Evaluator (ME)–the ME are best at evaluating as well as analysing the ideas that are
offered by other people (Diab-Bahman, 2021). They are objective along with shrewd and they
are capable for carefully weighing the pros and cons before deciding something. They are critical
thinker and are strategic to their approach.
Specialist (SP) – they have specialised knowledge that is required for completing the job. These
people work for maintaining their status and are very proud of their abilities as well as skills. Thy
have to be the expert in the area of their work and they have committed fully towards their field
of expertise.
All the people have clear roles and responsibilities and this will help the healthcare setting
for being Continuous Quality Improvement (CQI) and the staff of the health care is independent
in their roles after fully getting knowledgeable of their roles, this will help the team to work in
the improvement of the quality continuously for the working of the healthcare. The different
team roles provided by the Belbin model help in providing different roles that are necessary for
the improving the quality. The capabilities, skills and expertise of different team members will
help in improving the quality at the healthcare.
8
that the team is working efficiently. They are the negotiator of the team as they are flexible,
perceptive and diplomatic. These people are capable in their own right and are popular but
prioritise the team cohesion along with helping people for getting the work done.
Resource investigator (RI)–these people are innovative as well as the creative people of the
group. These people develop the contact, explore the options that are available and negotiate the
resources for the team. They are enthusiastic team members and are able to identify the work
with the stakeholders for helping the team accomplish the objectives. These people are
extroverted and out-going that means they react to their ideas.
Thought Oriented Roles
It consists of the plant (PL), monitor-Evaluator (ME) and specialist (SP).
Plant (PL)–plant in the tem is the innovator of the team who bring new ideas and approaches to
the team. Plants are introverted and have the tendency to work apart from the team. Plants bring
ideas so novel that they are practically impossible sometimes. They can also ignore the provide
parameters and constraints and they are poor at communication.
Monitor-Evaluator (ME)–the ME are best at evaluating as well as analysing the ideas that are
offered by other people (Diab-Bahman, 2021). They are objective along with shrewd and they
are capable for carefully weighing the pros and cons before deciding something. They are critical
thinker and are strategic to their approach.
Specialist (SP) – they have specialised knowledge that is required for completing the job. These
people work for maintaining their status and are very proud of their abilities as well as skills. Thy
have to be the expert in the area of their work and they have committed fully towards their field
of expertise.
All the people have clear roles and responsibilities and this will help the healthcare setting
for being Continuous Quality Improvement (CQI) and the staff of the health care is independent
in their roles after fully getting knowledgeable of their roles, this will help the team to work in
the improvement of the quality continuously for the working of the healthcare. The different
team roles provided by the Belbin model help in providing different roles that are necessary for
the improving the quality. The capabilities, skills and expertise of different team members will
help in improving the quality at the healthcare.
8
The Continuous Quality Improvement (CQI)tools that can be used by the healthcare setting
are Fishbone and PDSA.
Fishbone
It is also known as the cause and the effective diagram. The diagram is capable of
brainstorming the possible causes that can help in identifying the main cause of the problem
along with this it help in sorting the ideas into useful categories. The fishbone diagram provides
a visual canvas for looking at the causes as well as the effect. This tool is more structured than
the other tools used for brainstorming the causes of problem. The problem is displayed at the
mouth of the fish (Coccia, 2018). The possible causes that are generating in the problem in the
quality improvement are listed on the smaller bones of the fish under various categories. The
fishbone diagram help in in identify the problem that is obstructing the improvements that is
considered by the directing team to look towards the categories along with thinking for the
alternative causes. The team members also include the care worker those have the personal
knowledge of the process as well as the systems that are involved in the problem that is being
investigated.
PDSA
The PDSA is a tool used for the Continuous Quality Improvement (CQI) and it is a model
having four stages for solving the problem and carry out change.
Stage one is the plan. In this stage the team is recruited having the knowledge of the problem or
have the opportunity for the improvement. The roles, responsibilities, timelines and schedule for
the meeting of the recruited team member are identified. The draft in the aim statement is done
that answer to the three fundamental questions of the aim that are:
What needs to be accomplished?
How to find out that the change is an improvement?
What changes can be made for the improvement?
The current context as well as the process is discussed in this stage. The current process in the
healthcare is brainstormed by asking team members questions. The process can be visually
described by the construction of the swim lane map. It the team runs in the blocks then it can be
found where the process has occurred. More detail need to be gathered for the implementation of
process. The problem is described and the problem statement is written. The causes and the
alternative are identified. The alternatives are developed.
9
are Fishbone and PDSA.
Fishbone
It is also known as the cause and the effective diagram. The diagram is capable of
brainstorming the possible causes that can help in identifying the main cause of the problem
along with this it help in sorting the ideas into useful categories. The fishbone diagram provides
a visual canvas for looking at the causes as well as the effect. This tool is more structured than
the other tools used for brainstorming the causes of problem. The problem is displayed at the
mouth of the fish (Coccia, 2018). The possible causes that are generating in the problem in the
quality improvement are listed on the smaller bones of the fish under various categories. The
fishbone diagram help in in identify the problem that is obstructing the improvements that is
considered by the directing team to look towards the categories along with thinking for the
alternative causes. The team members also include the care worker those have the personal
knowledge of the process as well as the systems that are involved in the problem that is being
investigated.
PDSA
The PDSA is a tool used for the Continuous Quality Improvement (CQI) and it is a model
having four stages for solving the problem and carry out change.
Stage one is the plan. In this stage the team is recruited having the knowledge of the problem or
have the opportunity for the improvement. The roles, responsibilities, timelines and schedule for
the meeting of the recruited team member are identified. The draft in the aim statement is done
that answer to the three fundamental questions of the aim that are:
What needs to be accomplished?
How to find out that the change is an improvement?
What changes can be made for the improvement?
The current context as well as the process is discussed in this stage. The current process in the
healthcare is brainstormed by asking team members questions. The process can be visually
described by the construction of the swim lane map. It the team runs in the blocks then it can be
found where the process has occurred. More detail need to be gathered for the implementation of
process. The problem is described and the problem statement is written. The causes and the
alternative are identified. The alternatives are developed.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
In the stage two the action plans for the improvement of the healthcare setting is
implemented. The data from the implication of the plan is collected for the stage three (Coury
and et.al, 2017). The team need to document the unexpected effects, general observation and
problems. Stage three is of study, the aim statement from the stag one and the data gathered in
the stage two are determine the questions like was the action worth the investment of the
healthcare of not. Stage four is of the act,the standardise improvements need to be used in the
regular basis. It is also required to return to the stage one to re-examine the process. It the team
believes that a different approach can be more successful than the model is to be used from the
stage one again.
Question 3
Reflection
Description- Working in Health and Social Care requires enabled me to understand different
strategies, systems and structure and how role of care provider and care users are included in
this. I also had role in design and implementation of care plan for service users, in which how
they will be provided care considering structure and systems of the organisation and legislation,
policies, outcome benchmarks for care (Sekarwinahyu and et.al., 2019). Care plans for care users
were based on person-centred approach and rights, values, cultures and preferences of services
are considered in developing care plan for them. Structure of the organisation is concerned with
roles and responsibilities are directed. Structure of organisation was designed in a way that
individuals were able to easily participate in their care plan. Systems were also effective and for
the purpose of care, integrated approach was followed in organisation in which according to a
preset plan, care users were given care. Strategies were such that as much possible autonomy of
service users were kept safe and they were encouraged to be independent. My role in designing
and implementation was to assess requirement of care users and on the basis of their requirement
developing a plan that can cater their requirements.
Feelings- During my practice feelings were both good and bad, positive and negative and during
my practice I always constantly considerate about my actions and impact of strategy, structure
and principles for support. Being a care worker it was very important that I consider all these
elements and how they will affect care users. This is because care workers are those who directly
10
implemented. The data from the implication of the plan is collected for the stage three (Coury
and et.al, 2017). The team need to document the unexpected effects, general observation and
problems. Stage three is of study, the aim statement from the stag one and the data gathered in
the stage two are determine the questions like was the action worth the investment of the
healthcare of not. Stage four is of the act,the standardise improvements need to be used in the
regular basis. It is also required to return to the stage one to re-examine the process. It the team
believes that a different approach can be more successful than the model is to be used from the
stage one again.
Question 3
Reflection
Description- Working in Health and Social Care requires enabled me to understand different
strategies, systems and structure and how role of care provider and care users are included in
this. I also had role in design and implementation of care plan for service users, in which how
they will be provided care considering structure and systems of the organisation and legislation,
policies, outcome benchmarks for care (Sekarwinahyu and et.al., 2019). Care plans for care users
were based on person-centred approach and rights, values, cultures and preferences of services
are considered in developing care plan for them. Structure of the organisation is concerned with
roles and responsibilities are directed. Structure of organisation was designed in a way that
individuals were able to easily participate in their care plan. Systems were also effective and for
the purpose of care, integrated approach was followed in organisation in which according to a
preset plan, care users were given care. Strategies were such that as much possible autonomy of
service users were kept safe and they were encouraged to be independent. My role in designing
and implementation was to assess requirement of care users and on the basis of their requirement
developing a plan that can cater their requirements.
Feelings- During my practice feelings were both good and bad, positive and negative and during
my practice I always constantly considerate about my actions and impact of strategy, structure
and principles for support. Being a care worker it was very important that I consider all these
elements and how they will affect care users. This is because care workers are those who directly
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
work with care users and have better understanding of how different factors within organisation
and also factors like policies and regulatory requirements affect care users and make impact of
care quality (Markkanen and et.al., 2020). There was constant stress about adherence to different
rules in relation with care and also about how I will be able to provide effective and qualitative
care without avoiding any of the regulatory requirements. I was also working on assessment of
care needs for the purpose of developing care plan and while doing so I was constantly worried
whether I will be able to rightly and accurately assess requirements of care because it is one of
the most important element of qualitative care that is given to care users. In this it was very
important that principles of support including Empowerment, Safety, Confidentiality, and social
justice and success in doing these in a standard way were a very good feeling for me.
Evaluation- I realised that during my practice there were certain aspects about certain
legislation, and policies and this affected my performance during design and development of
service users care plan. Health and Social Care Act 2008, Social Value Act 2012, legislation
related to mental health and other aspects of health and social care needs to be well considered
before planning and implementation of care plan. Inadequate knowledge about these legislations
and their impact on care service user affected my performance and was also a reason that I was
feeling good. However, I had strong knowledge and understanding of health and social care
practices and because of this I was able to carry out my work efficiently and on time and this
made me feel good and positive (He, Parkinson and Doyle, 2018). I realised that it is important
to possess adequate knowledge of all elements and factors that enable to carry out job effectively
and also affect job and quality of work. Different legislation also needs to be known by me as a
care worker because they enable me to promoting principle for support for health and social care.
I was also able to effective care about rights, values and preferences of care users and was
always considerate about their rights leading to my effective performance.
Analysis- During my practice as care worker I was always conscious about voice of service
users and was considerate about how I can get input and suggestion of those to whom service is
being provided. This is involved in person-centred approach for care and along with this
collecting input is also important for promoting principles of support for working in health and
social care. Experience helps me understand that when input of service users is taken and when
their voice is promoted this helps in achieving better results in relation with services provided to
11
and also factors like policies and regulatory requirements affect care users and make impact of
care quality (Markkanen and et.al., 2020). There was constant stress about adherence to different
rules in relation with care and also about how I will be able to provide effective and qualitative
care without avoiding any of the regulatory requirements. I was also working on assessment of
care needs for the purpose of developing care plan and while doing so I was constantly worried
whether I will be able to rightly and accurately assess requirements of care because it is one of
the most important element of qualitative care that is given to care users. In this it was very
important that principles of support including Empowerment, Safety, Confidentiality, and social
justice and success in doing these in a standard way were a very good feeling for me.
Evaluation- I realised that during my practice there were certain aspects about certain
legislation, and policies and this affected my performance during design and development of
service users care plan. Health and Social Care Act 2008, Social Value Act 2012, legislation
related to mental health and other aspects of health and social care needs to be well considered
before planning and implementation of care plan. Inadequate knowledge about these legislations
and their impact on care service user affected my performance and was also a reason that I was
feeling good. However, I had strong knowledge and understanding of health and social care
practices and because of this I was able to carry out my work efficiently and on time and this
made me feel good and positive (He, Parkinson and Doyle, 2018). I realised that it is important
to possess adequate knowledge of all elements and factors that enable to carry out job effectively
and also affect job and quality of work. Different legislation also needs to be known by me as a
care worker because they enable me to promoting principle for support for health and social care.
I was also able to effective care about rights, values and preferences of care users and was
always considerate about their rights leading to my effective performance.
Analysis- During my practice as care worker I was always conscious about voice of service
users and was considerate about how I can get input and suggestion of those to whom service is
being provided. This is involved in person-centred approach for care and along with this
collecting input is also important for promoting principles of support for working in health and
social care. Experience helps me understand that when input of service users is taken and when
their voice is promoted this helps in achieving better results in relation with services provided to
11
care service users. Promoting voice of care users also unable to understand how effective quality
is being provided to service users. Application of policies such as care quality Commission
health and social care act and control of substances hazardous to health regulations and several
other regulations and legislations are helpful in ensuring that right service is provided to care
service users (Joyce and Jackson, 2021). Strategy, structure and system of organisation where I
was working were also favourable and effective for carrying out care activities in a way that is
according to organisational as well as regulatory standards.
Conclusion- On the basis of above discussion, it can be concluded that working in health and
social care organisation was a very important and effective learning experience. I understood
different aspects of health and social care. During practice I realised that effective knowledge of
regulations and legislations would have enabled to practice more efficiently. However, my
approach of including service users in practice and developing their care plan was effective and
enabled me to effectively carry out practices (Effendi and et.al., 2020). Overall it can be said that
I have all skills required for completing activities in health and social care and I require to
develop knowledge of legislation and rules for improving my practice.
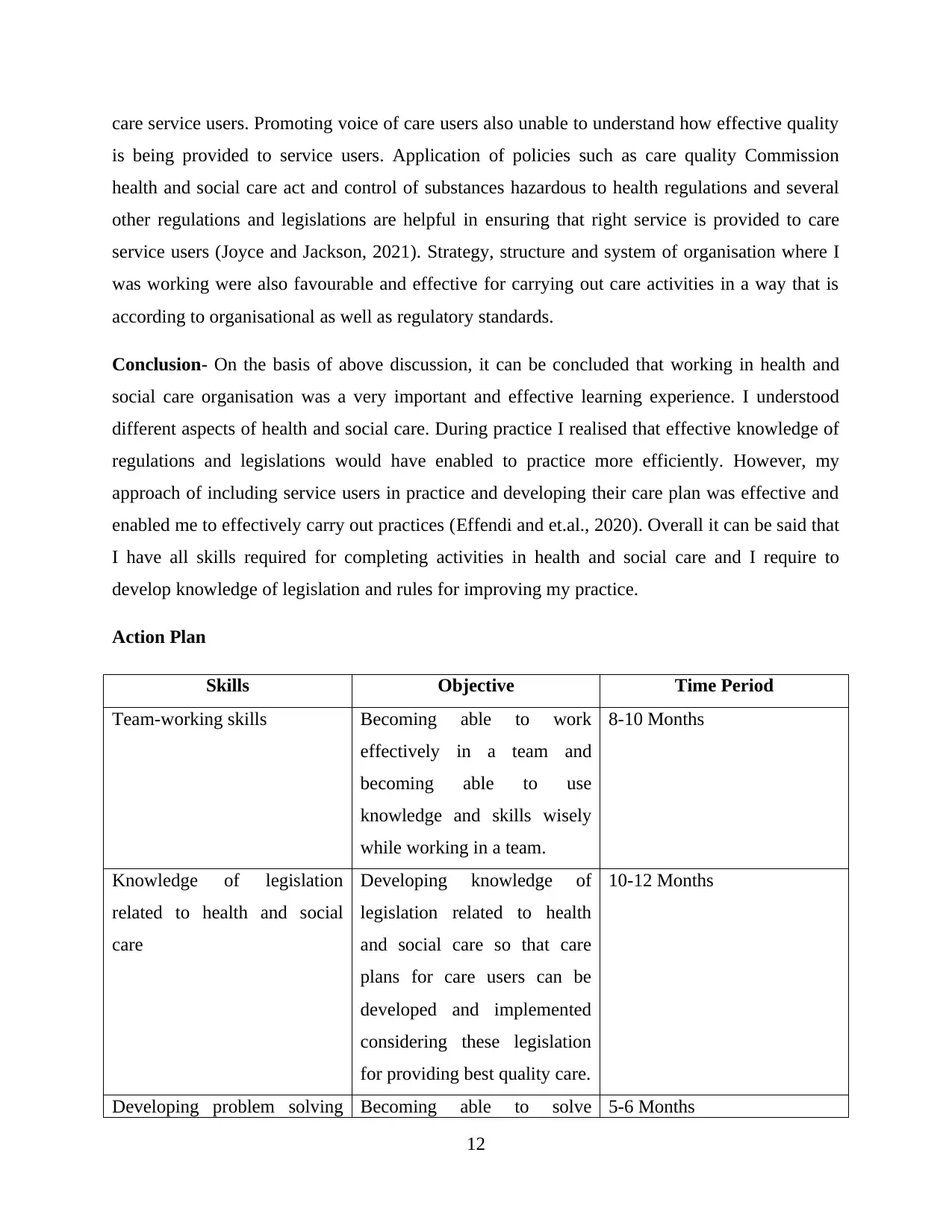
Action Plan
Skills Objective Time Period
Team-working skills Becoming able to work
effectively in a team and
becoming able to use
knowledge and skills wisely
while working in a team.
8-10 Months
Knowledge of legislation
related to health and social
care
Developing knowledge of
legislation related to health
and social care so that care
plans for care users can be
developed and implemented
considering these legislation
for providing best quality care.
10-12 Months
Developing problem solving Becoming able to solve 5-6 Months
12
is being provided to service users. Application of policies such as care quality Commission
health and social care act and control of substances hazardous to health regulations and several
other regulations and legislations are helpful in ensuring that right service is provided to care
service users (Joyce and Jackson, 2021). Strategy, structure and system of organisation where I
was working were also favourable and effective for carrying out care activities in a way that is
according to organisational as well as regulatory standards.
Conclusion- On the basis of above discussion, it can be concluded that working in health and
social care organisation was a very important and effective learning experience. I understood
different aspects of health and social care. During practice I realised that effective knowledge of
regulations and legislations would have enabled to practice more efficiently. However, my
approach of including service users in practice and developing their care plan was effective and
enabled me to effectively carry out practices (Effendi and et.al., 2020). Overall it can be said that
I have all skills required for completing activities in health and social care and I require to
develop knowledge of legislation and rules for improving my practice.
Action Plan
Skills Objective Time Period
Team-working skills Becoming able to work
effectively in a team and
becoming able to use
knowledge and skills wisely
while working in a team.
8-10 Months
Knowledge of legislation
related to health and social
care
Developing knowledge of
legislation related to health
and social care so that care
plans for care users can be
developed and implemented
considering these legislation
for providing best quality care.
10-12 Months
Developing problem solving Becoming able to solve 5-6 Months
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





