Leadership for Quality and Safety in Healthcare: Assessment 1 Report
VerifiedAdded on 2023/06/07
|10
|2576
|384
Report
AI Summary
This assessment report delves into the critical aspects of leadership in ensuring quality and safety within healthcare settings. It differentiates between patient safety and overall safety in healthcare, emphasizing the importance of risk management and analysis. The report examines safety culture, methods of measurement, and the impact of leadership on fostering a positive safety environment. Furthermore, it discusses the Australian Commission on Safety and Quality in Health Care's National Safety and Quality Health Service Standards (NSQHS), highlighting their role in promoting quality and safe care. The assessment underscores the need for comprehensive leadership strategies, effective risk management, and a strong safety culture to minimize errors and improve patient outcomes. Desklib provides a platform to access this and other solved assignments for students.

Running head: LEADERSHIP FOR QUALITY AND SAFETY IN HEALTH CARE 1
Assessment 1
(Author’s name)
(Institutional Affiliation)
Assessment 1
(Author’s name)
(Institutional Affiliation)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ASSESSMENT 1 2
Assessment 1
Question II Patient Safety, Different between patient safety and safety in health care, risk
management, and risk analysis
Patient safety is all about how hospitals and other healthcare organizations protect their
patients and families from infections, accidents, injuries adverse effects and errors related to
health care delivery. Patient safety is a serious health concern in all medical facilities (WHO,
2017). There is a chance that one person in a million may get harm when traveling by airplane,
but one out of every 300 people get harm when in the hospital(WHO, 2017). Although many
healthcare organizations are good at keeping their patients safe, some hospital has failed.
According to the World Health Organization (WHO) 2018, 18,000 patients die every year due to
medical errors in Australia. In addition to that, about 50,000 patients get disabled due to factors
related to patient safety. In the United States of America (USA) medical errors resulted in as
many as 98,000 deaths each and every year. Other statistics by WHO 2018 report shows that,
patients safety deaths are the fourteenth leading deaths in in health care sectors across the globe
accounting for about 43 million deaths every year of which 42 million of this are due to
medication errors.
There are various reasons that may hinder patients’ safety in our hospitals. First, the
health care systems have become more complicated in the past few decades due to an increase in
the use of new technology, dynamic treatment methods, and procedures plus the rice of new
medicines (Mcfadden, Stock, & Gowen 111, 2015). Other than that, the hospital usually receives
different kind of patients of which some may be aged or present with complicated conditions
(McFadden, Stock, & Gowen 111, 2015). Health care professionals may have difficulties when
making decisions for such patients which in turn can lead to medical errors. In addition, due to
Assessment 1
Question II Patient Safety, Different between patient safety and safety in health care, risk
management, and risk analysis
Patient safety is all about how hospitals and other healthcare organizations protect their
patients and families from infections, accidents, injuries adverse effects and errors related to
health care delivery. Patient safety is a serious health concern in all medical facilities (WHO,
2017). There is a chance that one person in a million may get harm when traveling by airplane,
but one out of every 300 people get harm when in the hospital(WHO, 2017). Although many
healthcare organizations are good at keeping their patients safe, some hospital has failed.
According to the World Health Organization (WHO) 2018, 18,000 patients die every year due to
medical errors in Australia. In addition to that, about 50,000 patients get disabled due to factors
related to patient safety. In the United States of America (USA) medical errors resulted in as
many as 98,000 deaths each and every year. Other statistics by WHO 2018 report shows that,
patients safety deaths are the fourteenth leading deaths in in health care sectors across the globe
accounting for about 43 million deaths every year of which 42 million of this are due to
medication errors.
There are various reasons that may hinder patients’ safety in our hospitals. First, the
health care systems have become more complicated in the past few decades due to an increase in
the use of new technology, dynamic treatment methods, and procedures plus the rice of new
medicines (Mcfadden, Stock, & Gowen 111, 2015). Other than that, the hospital usually receives
different kind of patients of which some may be aged or present with complicated conditions
(McFadden, Stock, & Gowen 111, 2015). Health care professionals may have difficulties when
making decisions for such patients which in turn can lead to medical errors. In addition, due to
ASSESSMENT 1 3
unequal distribution of health workforce affected by social-economic determinants of health
canlead to health workers having a work overload (Mcfadden, Stock, & Gowen 111, 2015).
Safety in health care is broader than patient safety. It includes the safety of all health care
providers including doctors and nurses. Due to these facts the WHO have developed four major
strategies that may help to minimize errors made during health care in order to promote patient
safety and safety in health care. These include providing a comprehensive leadership strategy
that promotes cooperation of healthcare workers, establishing and developing tools and
guidelines that enhance healthcare workers building capacities, monitoring patients safety
improvements and engaging clients and their families for safer caring(WHO, 2018).
Due to the problems associated with patients safety, hospitals often apply risk
management and analysis strategies to address them (Mcfadden, Stock, & Gowen 111, 2015).
There are various dimensions that are involved in risk management. These include the
organizational resources, structure, procedures, and processes needed to plan, analyze, evaluate
and treat patients risks so as to provide better patients safety (Mcfadden, Stock, & Gowen 111,
2015). Risk management in a clinical setting is normally a process that involves various steps of
risk assessment, judgment and taking the correct actions for risk treatment. (Arfanis, & Smith,
2012). Health care settings are complex and they involve interactions with clinical procedures,
diseases processes, hospital resources including both human and manmade, technologies and
policies (Arfanis, & Smith, 2012). The interactions of those factors can lead to unanticipated
outcomes and harms to patients. Due to those facts a health risk management is needed.
There are various steps that are involved in health risk management. These includes risks
context establishment, identification of available risks, risk analysis, evaluation, and risks
treatment. (Guo, 2015).After risk identification and assessment, a risk analysis is a crucial part of
unequal distribution of health workforce affected by social-economic determinants of health
canlead to health workers having a work overload (Mcfadden, Stock, & Gowen 111, 2015).
Safety in health care is broader than patient safety. It includes the safety of all health care
providers including doctors and nurses. Due to these facts the WHO have developed four major
strategies that may help to minimize errors made during health care in order to promote patient
safety and safety in health care. These include providing a comprehensive leadership strategy
that promotes cooperation of healthcare workers, establishing and developing tools and
guidelines that enhance healthcare workers building capacities, monitoring patients safety
improvements and engaging clients and their families for safer caring(WHO, 2018).
Due to the problems associated with patients safety, hospitals often apply risk
management and analysis strategies to address them (Mcfadden, Stock, & Gowen 111, 2015).
There are various dimensions that are involved in risk management. These include the
organizational resources, structure, procedures, and processes needed to plan, analyze, evaluate
and treat patients risks so as to provide better patients safety (Mcfadden, Stock, & Gowen 111,
2015). Risk management in a clinical setting is normally a process that involves various steps of
risk assessment, judgment and taking the correct actions for risk treatment. (Arfanis, & Smith,
2012). Health care settings are complex and they involve interactions with clinical procedures,
diseases processes, hospital resources including both human and manmade, technologies and
policies (Arfanis, & Smith, 2012). The interactions of those factors can lead to unanticipated
outcomes and harms to patients. Due to those facts a health risk management is needed.
There are various steps that are involved in health risk management. These includes risks
context establishment, identification of available risks, risk analysis, evaluation, and risks
treatment. (Guo, 2015).After risk identification and assessment, a risk analysis is a crucial part of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ASSESSMENT 1 4
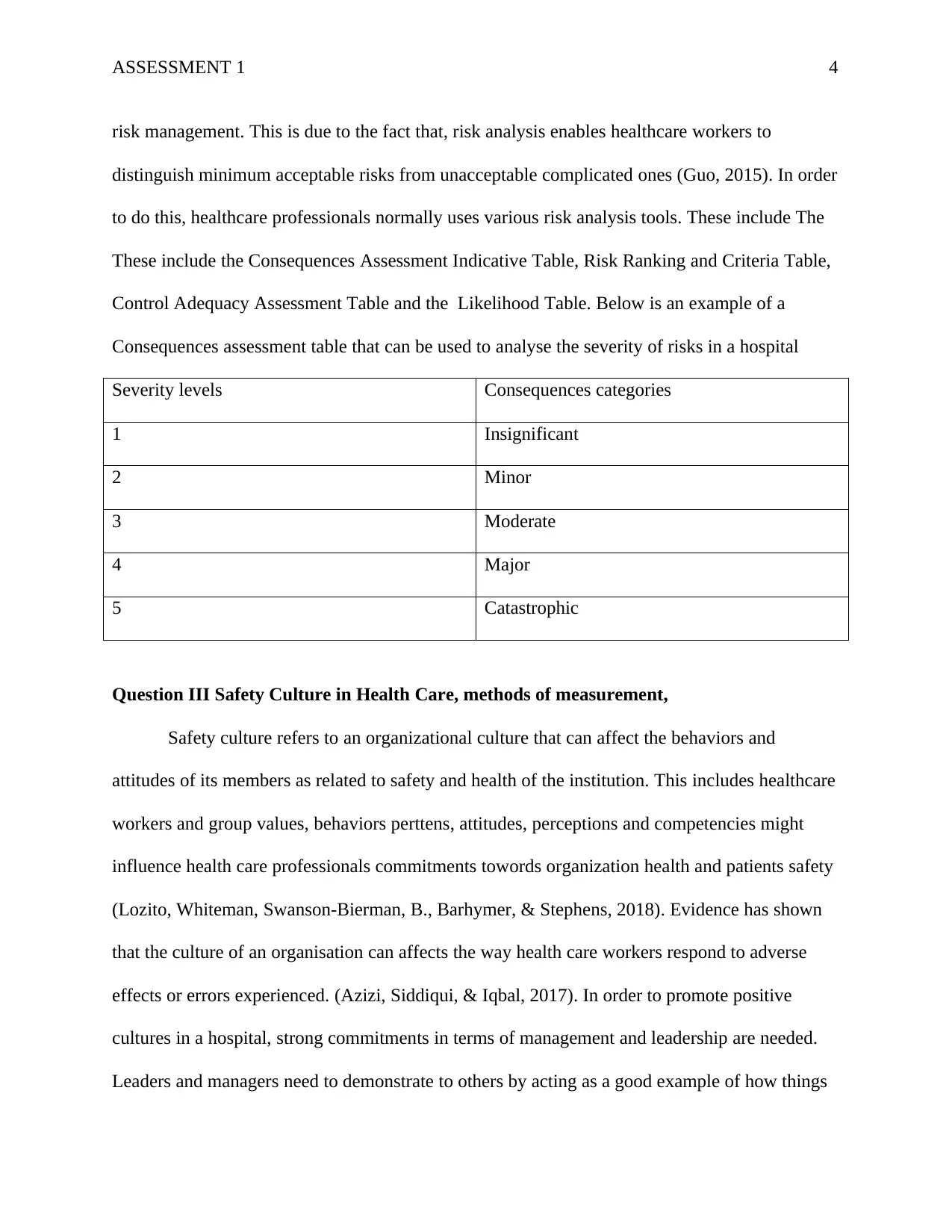
risk management. This is due to the fact that, risk analysis enables healthcare workers to
distinguish minimum acceptable risks from unacceptable complicated ones (Guo, 2015). In order
to do this, healthcare professionals normally uses various risk analysis tools. These include The
These include the Consequences Assessment Indicative Table, Risk Ranking and Criteria Table,
Control Adequacy Assessment Table and the Likelihood Table. Below is an example of a
Consequences assessment table that can be used to analyse the severity of risks in a hospital
Severity levels Consequences categories
1 Insignificant
2 Minor
3 Moderate
4 Major
5 Catastrophic
Question III Safety Culture in Health Care, methods of measurement,
Safety culture refers to an organizational culture that can affect the behaviors and
attitudes of its members as related to safety and health of the institution. This includes healthcare
workers and group values, behaviors perttens, attitudes, perceptions and competencies might
influence health care professionals commitments towords organization health and patients safety
(Lozito, Whiteman, Swanson-Bierman, B., Barhymer, & Stephens, 2018). Evidence has shown
that the culture of an organisation can affects the way health care workers respond to adverse
effects or errors experienced. (Azizi, Siddiqui, & Iqbal, 2017). In order to promote positive
cultures in a hospital, strong commitments in terms of management and leadership are needed.
Leaders and managers need to demonstrate to others by acting as a good example of how things
risk management. This is due to the fact that, risk analysis enables healthcare workers to
distinguish minimum acceptable risks from unacceptable complicated ones (Guo, 2015). In order
to do this, healthcare professionals normally uses various risk analysis tools. These include The
These include the Consequences Assessment Indicative Table, Risk Ranking and Criteria Table,
Control Adequacy Assessment Table and the Likelihood Table. Below is an example of a
Consequences assessment table that can be used to analyse the severity of risks in a hospital
Severity levels Consequences categories
1 Insignificant
2 Minor
3 Moderate
4 Major
5 Catastrophic
Question III Safety Culture in Health Care, methods of measurement,
Safety culture refers to an organizational culture that can affect the behaviors and
attitudes of its members as related to safety and health of the institution. This includes healthcare
workers and group values, behaviors perttens, attitudes, perceptions and competencies might
influence health care professionals commitments towords organization health and patients safety
(Lozito, Whiteman, Swanson-Bierman, B., Barhymer, & Stephens, 2018). Evidence has shown
that the culture of an organisation can affects the way health care workers respond to adverse
effects or errors experienced. (Azizi, Siddiqui, & Iqbal, 2017). In order to promote positive
cultures in a hospital, strong commitments in terms of management and leadership are needed.
Leaders and managers need to demonstrate to others by acting as a good example of how things
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ASSESSMENT 1 5
need to be done (Nacioglu, 2016). The key management roles is to demonstrate commitments
and act accordingly in order to influence the attitudes and behaviours of other health care
professionals Safety culture is influenced by various safety culture domains which include
supervisions, safety systems, management jobs satisfaction, , management perceptions, risks
available, working conditions, commitments of the organization in policy implementation and
the overall values and beliefs of workers(Halligan, & Zecevic, (2011).
The key factors that can lead to poor safety culture in any given health organization are
poor management and leadership qualities (Mcfadden., Stock, & Gowen 111,2015). Managers
and supervisers who do not portray good leadership skills in hospitals end up promoting poor
safety culture. (Daly, Jackson, Mannix, Davidson, & Hutchinson, 2014). A health organization
can measure its safety culture in different ways. First is by identifying the level of commitment
its workers have (McSherry, & Pearce, 2016). Commented workers respond quickly to an
emergency, treat patients with respect and dignity and are always aware of all standard
procedures in the hospital. Secondly, safety culture can be measured by evaluating the outcomes
(Halligan, & Zecevic, 2011). Positive outcomes indicate all health workers are collaborating in
health care delivery and understand how the organization system works (Mcfadden., Stock, &
Gowen 111,2015). On the other hand, Poor safety culture always affects patients’ care and health
workers in various ways. These include poor patients support, staffs intimidations, late responses
to adverse effects thus increasing patients disabilities and poor continuous education for
healthcare workers.
Question V Australian Commission on Safety and Quality in Health Care (2012) National
Safety and Quality Health Service Standards
need to be done (Nacioglu, 2016). The key management roles is to demonstrate commitments
and act accordingly in order to influence the attitudes and behaviours of other health care
professionals Safety culture is influenced by various safety culture domains which include
supervisions, safety systems, management jobs satisfaction, , management perceptions, risks
available, working conditions, commitments of the organization in policy implementation and
the overall values and beliefs of workers(Halligan, & Zecevic, (2011).
The key factors that can lead to poor safety culture in any given health organization are
poor management and leadership qualities (Mcfadden., Stock, & Gowen 111,2015). Managers
and supervisers who do not portray good leadership skills in hospitals end up promoting poor
safety culture. (Daly, Jackson, Mannix, Davidson, & Hutchinson, 2014). A health organization
can measure its safety culture in different ways. First is by identifying the level of commitment
its workers have (McSherry, & Pearce, 2016). Commented workers respond quickly to an
emergency, treat patients with respect and dignity and are always aware of all standard
procedures in the hospital. Secondly, safety culture can be measured by evaluating the outcomes
(Halligan, & Zecevic, 2011). Positive outcomes indicate all health workers are collaborating in
health care delivery and understand how the organization system works (Mcfadden., Stock, &
Gowen 111,2015). On the other hand, Poor safety culture always affects patients’ care and health
workers in various ways. These include poor patients support, staffs intimidations, late responses
to adverse effects thus increasing patients disabilities and poor continuous education for
healthcare workers.
Question V Australian Commission on Safety and Quality in Health Care (2012) National
Safety and Quality Health Service Standards
ASSESSMENT 1 6
The ten National Safety and Quality Health Services Standards (NSQHS) were developed
by the Australian Commission for Safety and Quality Health Care (ACSQHC) in the year 2012
for the purpose of protecting individuals and their families from health services related harms.
The standards were developed to enable health service organizations to deliver quality and safe
care (ACSQHC, 2012). All standards were consistent with the current evidence-based practice
and were indented to enhance deliverance of best outcomes across the country. The first two
standards were established to promote the effective use of the other eight standards. These
include Governance for Safety and Quality in Health Service Organization and Partnering with
Consumers (ACSQHC, 2012). The first standard was developed to guide healthcare
organizations in adopting a plan, policy or program that provides information about individuals,
caregivers and the community (ACSQHC, 2012). The organizations were then supposed to
actively involve the consumers by presenting their plan to them in order to understand their
decisions or proposed plans (ACSQHC, 2012). The standards have been reduced from ten to
eight in number in the second edition developed in 2017. Although the second edition has eight
standards, the concepts are similar to the original version (Safety and Quality, 2018). However,
the second versions highlight the improvement that has been made and gaps that still to be
implemented which will later be evaluated in the year 2019 (ACSQHC, 2017). Both editions
must be approved and accredited by Ministry of Health, International Society for Quality in
Health Care and the Joint Accreditation Scheme of Australia for quality and legal purposes
(Safety and Quality, 2018).
Through the use of Standards, health care institutions have been able to set
responsibilities and relationships between the available workforce, executive and other
stakeholders including patients and their families (ACSQHC, 2017). This includes incorporating
The ten National Safety and Quality Health Services Standards (NSQHS) were developed
by the Australian Commission for Safety and Quality Health Care (ACSQHC) in the year 2012
for the purpose of protecting individuals and their families from health services related harms.
The standards were developed to enable health service organizations to deliver quality and safe
care (ACSQHC, 2012). All standards were consistent with the current evidence-based practice
and were indented to enhance deliverance of best outcomes across the country. The first two
standards were established to promote the effective use of the other eight standards. These
include Governance for Safety and Quality in Health Service Organization and Partnering with
Consumers (ACSQHC, 2012). The first standard was developed to guide healthcare
organizations in adopting a plan, policy or program that provides information about individuals,
caregivers and the community (ACSQHC, 2012). The organizations were then supposed to
actively involve the consumers by presenting their plan to them in order to understand their
decisions or proposed plans (ACSQHC, 2012). The standards have been reduced from ten to
eight in number in the second edition developed in 2017. Although the second edition has eight
standards, the concepts are similar to the original version (Safety and Quality, 2018). However,
the second versions highlight the improvement that has been made and gaps that still to be
implemented which will later be evaluated in the year 2019 (ACSQHC, 2017). Both editions
must be approved and accredited by Ministry of Health, International Society for Quality in
Health Care and the Joint Accreditation Scheme of Australia for quality and legal purposes
(Safety and Quality, 2018).
Through the use of Standards, health care institutions have been able to set
responsibilities and relationships between the available workforce, executive and other
stakeholders including patients and their families (ACSQHC, 2017). This includes incorporating
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

ASSESSMENT 1 7
a set of customs, laws, processes, and conventions that guides hor hospitals are administered and
directed. Over the time, health care organizations have been able to provide a specific structure
by using objectives that are achievable (Safety and Quality, 2018). The standards have also
increased individuals health literacy (Australian Commission on Safety and Quality in Health
Care, 2013). This is due to the fact there has been an elaborate process of how people can obtain
and understand useful health care information concerning various treatment methods, health
system and other health-related concerns (Safety and Quality, 2018). This, in turn, has enabled
patients seeking healthcare to be able to make decisions concerning their health care. In
addition, the standards have promoted an effective care that is based on a partnership with
consumers. Patients have benefited from high-quality care and good hospital experiences that
recognise their dignity and respect (ACSQHC, 2017). More services that are appropriate and
accessible for consumers have been established due to the current involvement of individuals and
communities in health services planning, monitoring and evaluation (ACSQHC, 2017). For
instance, there has been evidence of improved clinical outcomes with minimal readmissions, the
nosocomial infections have drastically decreased, there has been an increase in health promotion
and preventive strategies, improved adherence to treatments and increased health workforce.
a set of customs, laws, processes, and conventions that guides hor hospitals are administered and
directed. Over the time, health care organizations have been able to provide a specific structure
by using objectives that are achievable (Safety and Quality, 2018). The standards have also
increased individuals health literacy (Australian Commission on Safety and Quality in Health
Care, 2013). This is due to the fact there has been an elaborate process of how people can obtain
and understand useful health care information concerning various treatment methods, health
system and other health-related concerns (Safety and Quality, 2018). This, in turn, has enabled
patients seeking healthcare to be able to make decisions concerning their health care. In
addition, the standards have promoted an effective care that is based on a partnership with
consumers. Patients have benefited from high-quality care and good hospital experiences that
recognise their dignity and respect (ACSQHC, 2017). More services that are appropriate and
accessible for consumers have been established due to the current involvement of individuals and
communities in health services planning, monitoring and evaluation (ACSQHC, 2017). For
instance, there has been evidence of improved clinical outcomes with minimal readmissions, the
nosocomial infections have drastically decreased, there has been an increase in health promotion
and preventive strategies, improved adherence to treatments and increased health workforce.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ASSESSMENT 1 8
References
Allen, S., Chiarella, M., & Homer, C. S. E. (2010). Lessons learned from measuring safety
culture: An Australian case study. Midwifery, 26, 497–503.
doi:10.1016/j.midw.2010.07.002
Arfanis, K., & Smith, A. (2012). Informal risk assessment strategies in health care staff:
An unrecognized source of resilience? Journal of Evaluation in Clinical Practice, 18,
1140- 1146. doi:10.1111/j.1365-2753.2011.01759.x
Australian Commission on Safety and Quality in Health Care (ACSQHC). (2012). The national
safety and quality health service standards. Sydney: ACSQHC. Retrieved from
https://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-Standards-
Sept-2012.pdf
Australian Commission on Safety and Quality in Health Care. (2013). The National Safety and
Quality Health Service Standards in 2013: Transforming the safety and quality of health
care. Sydney: ACSQHC. Retrieved from https://www.safetyandquality.gov.au/wp-
content/uploads/2014/10/NSQHSS-in-2013-Transforming-the-safety-and-quality-of-
health-care.pdf
Australian Commission on Safety and Quality in Health Care (ACSQHC). (2017). National
Safety and Quality Health Service Standards Second edition. Retrieved from
https://www.safetyandquality.gov.au/wp-content/uploads/2017/12/National-Safety-and-
Quality-Health-Service-Standards-second-edition.pdf
Azizi, S., Siddiqui, F., & Iqbal, I. (2017). Changing health care culture: A prerequisite to
References
Allen, S., Chiarella, M., & Homer, C. S. E. (2010). Lessons learned from measuring safety
culture: An Australian case study. Midwifery, 26, 497–503.
doi:10.1016/j.midw.2010.07.002
Arfanis, K., & Smith, A. (2012). Informal risk assessment strategies in health care staff:
An unrecognized source of resilience? Journal of Evaluation in Clinical Practice, 18,
1140- 1146. doi:10.1111/j.1365-2753.2011.01759.x
Australian Commission on Safety and Quality in Health Care (ACSQHC). (2012). The national
safety and quality health service standards. Sydney: ACSQHC. Retrieved from
https://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-Standards-
Sept-2012.pdf
Australian Commission on Safety and Quality in Health Care. (2013). The National Safety and
Quality Health Service Standards in 2013: Transforming the safety and quality of health
care. Sydney: ACSQHC. Retrieved from https://www.safetyandquality.gov.au/wp-
content/uploads/2014/10/NSQHSS-in-2013-Transforming-the-safety-and-quality-of-
health-care.pdf
Australian Commission on Safety and Quality in Health Care (ACSQHC). (2017). National
Safety and Quality Health Service Standards Second edition. Retrieved from
https://www.safetyandquality.gov.au/wp-content/uploads/2017/12/National-Safety-and-
Quality-Health-Service-Standards-second-edition.pdf
Azizi, S., Siddiqui, F., & Iqbal, I. (2017). Changing health care culture: A prerequisite to
ASSESSMENT 1 9
improving patient safety. Therapeutics and Clinical Risk Management, 13, 623–624.
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5428755/
doi: 10.2147/TCRM.S138896
Daly, J., Jackson, D., Mannix, J., Davidson, P.M., & Hutchinson, M. (2014). The importance of
clinical leadership in the hospital setting. Journal of Healthcare Leadership, 6, 75-83.
http://epubs.scu.edu.au/cgi/viewcontent.cgi?article=2954&context=hahs_pubs
Halligan, M., & Zecevic, A. (2011). Safety culture in healthcare: A review of concepts,
dimensions, measures, and progress. BMJ Quality and Safety, 20, 338-343.
doi:10.1136/bmjqs.2010.0409
Li, Guo. (2015). Implementation of a risk management plan in a hospital
operating room. International Journal of Nursing Sciences, 2(34), 348-
354. Retrieved from
http://www.elsevier.com/journals/internationaljournal-of-nursing-sciences/2352-0132
Lozito, M., Whiteman, K., Swanson-Bierman, B., Barhymer, M., & Stephens, K. (2018). Good
catch campaign: Improving perioperative culture of safety. Quality Improvement, 10(6)
705-714. Retrieved from http://doi.org/10.1002/aorn.12148
Mcfadden,K. L., Stock, G. N., & Gowen 111, C. R. (2015). Leadership, safety climate, and
continuous quality improvement: Impact on process quality and patient safety. Health
CareManagement Review, 40(1), 2434.https://doi.org/10.1097/HMR.0000000000000006
McSherry, R., & Pearce, P. (2016). What are the effective ways to translate clinical leadership
into healthcare quality improvement? Journal of Healthcare Leadership. 8, 11-17.
doi: 10.2147/JHL.S46170
improving patient safety. Therapeutics and Clinical Risk Management, 13, 623–624.
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5428755/
doi: 10.2147/TCRM.S138896
Daly, J., Jackson, D., Mannix, J., Davidson, P.M., & Hutchinson, M. (2014). The importance of
clinical leadership in the hospital setting. Journal of Healthcare Leadership, 6, 75-83.
http://epubs.scu.edu.au/cgi/viewcontent.cgi?article=2954&context=hahs_pubs
Halligan, M., & Zecevic, A. (2011). Safety culture in healthcare: A review of concepts,
dimensions, measures, and progress. BMJ Quality and Safety, 20, 338-343.
doi:10.1136/bmjqs.2010.0409
Li, Guo. (2015). Implementation of a risk management plan in a hospital
operating room. International Journal of Nursing Sciences, 2(34), 348-
354. Retrieved from
http://www.elsevier.com/journals/internationaljournal-of-nursing-sciences/2352-0132
Lozito, M., Whiteman, K., Swanson-Bierman, B., Barhymer, M., & Stephens, K. (2018). Good
catch campaign: Improving perioperative culture of safety. Quality Improvement, 10(6)
705-714. Retrieved from http://doi.org/10.1002/aorn.12148
Mcfadden,K. L., Stock, G. N., & Gowen 111, C. R. (2015). Leadership, safety climate, and
continuous quality improvement: Impact on process quality and patient safety. Health
CareManagement Review, 40(1), 2434.https://doi.org/10.1097/HMR.0000000000000006
McSherry, R., & Pearce, P. (2016). What are the effective ways to translate clinical leadership
into healthcare quality improvement? Journal of Healthcare Leadership. 8, 11-17.
doi: 10.2147/JHL.S46170
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ASSESSMENT 1
10
Nacioglu, A. (2016). As a critical behavior to improve quality and patient safety in healthcare:
Speaking p! Safety in Health, 2(10), 1-25. Retrieved from
https://doi.org/10.1186/s40886-016-0021-x
Safety and Quality. (2018). Accreditation and the NSQHS Standards. Retrieved from
https://www.safetyandquality.gov.au/our-work/assessment-to-the-nsqhs-standards/
World Health Organization (WHO), (2018). 10 facts on patient safety. Retrieved from
http://www.who.int/features/factfiles/patient_safety/en/
World Health Organization (WHO) (2017) Patient Safety Making health care safer.
Retrieved from http://apps.who.int/iris/bitstream/handle/10665/255507/WHO-HIS-SDS-
2017.11-eng.pdf;jsessionid=C4B5BBC298C208D9774B59BE330D3115?sequence=1
10
Nacioglu, A. (2016). As a critical behavior to improve quality and patient safety in healthcare:
Speaking p! Safety in Health, 2(10), 1-25. Retrieved from
https://doi.org/10.1186/s40886-016-0021-x
Safety and Quality. (2018). Accreditation and the NSQHS Standards. Retrieved from
https://www.safetyandquality.gov.au/our-work/assessment-to-the-nsqhs-standards/
World Health Organization (WHO), (2018). 10 facts on patient safety. Retrieved from
http://www.who.int/features/factfiles/patient_safety/en/
World Health Organization (WHO) (2017) Patient Safety Making health care safer.
Retrieved from http://apps.who.int/iris/bitstream/handle/10665/255507/WHO-HIS-SDS-
2017.11-eng.pdf;jsessionid=C4B5BBC298C208D9774B59BE330D3115?sequence=1
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





