Sub-Saharan Africa: Challenges and Solutions in Microsurgery Practice
VerifiedAdded on 2022/11/25
|8
|4273
|343
Report
AI Summary
This report, based on a survey of plastic surgeons in East, Central, and Southern Africa, investigates the challenges faced in global reconstructive microsurgery within the sub-Saharan region. The study, which had a 56% response rate, highlights key issues such as inadequate perioperative care due to a shortage of support staff, lack of surgical expertise, insufficient equipment, and public unawareness of the benefits of microsurgery. The research emphasizes the need for enhanced training through a multidisciplinary team approach, increased advocacy, publications, and funding to improve microsurgical practices. The findings underscore the importance of addressing these challenges to advance reconstructive surgery in the region, with a focus on improving outcomes and expanding access to this essential medical technique. The survey results identified Kenya and Uganda as having surgeons performing more than 10 cases annually, with most participants emphasizing the importance of microsurgery in the region.
JPRAS Open 20 (2019) 19–26
Contents lists available at ScienceDirect
JPRAS Open
journal homepage:www.elsevier.com/locate/jpra
Original Article
Challengesin global reconstructivemicrosurgery:
The sub-Saharanafrican surgeons’perspective
Chihena H. Bandaa,b,∗, Pafitanis Georgiosc,
Mitsunaga Narushimaa, Ryohei Ishiuraa, Minami Fujitaa,
Jovic Gorand
a Department of Plastic and Reconstructive Surgery, Graduate School of Medicine, Mie University, Tsu, Japan
b Department of Surgery, Arthur Davison Children’s Hospital, Ndola, Zambia
c Group for Academic Plastic Surgery, The Royal London Hospital, Barts Health NHS Trust, Queen Mary
University of London, London, UK
d Department of Surgery, The University Teaching Hospital, Lusaka, Zambia
a r t i c l e i n f o
Article history:
Received 20 November 2018
Accepted 20 January 2019
Available online 4 February 2019
Keywords:
Microsurgery
Free tissue transfer
Africa
Challenges
Training
Global surgery
a b s t r a c t
Background:Microsurgeryis an essentialelementof plastic surgery
practice.However,it remainsunavailableor rudimentaryin several
developingcountries, especially in sub-SaharanAfrica. This study
presents the local plastic surgeons experience,while focusing on
specific challengesencounteredand methods to improve the sub-
Saharanglobal microsurgerypractice.
Methodology: An online survey was sent to all plastic surgeons
registeredwith the College of SurgeonsEast Central and Southern
Africa and respectivenational plastic surgical societiesin the east
central and southern Africa regional community. A total of 57
questionnaireswere sent. Surgeons’country of practice, years of
experienceand rate of performing microsurgicalprocedureswere
considered.
∗ Corresponding author: Department of Plastic and Reconstructive Surgery, Graduate School of Medicine, Mie University,
2-174 Edobashi, Tsu, Mie Prefecture, 514-8507, JAPAN.
E-mail addresses: 318001c@m.mie-u.ac.jp , chihenab@gmail.com (C.H. Banda).
https://doi.org/10.1016/j.jpra.2019.01.009
2352-5878/© 2019 The Author(s).Published by Elsevier Ltd on behalf of British Association of Plastic,Reconstructive and
Aesthetic Surgeons. This is an open access article under the CC BY license. ( http://creativecommons.org/licenses/by/4.0/ )
Contents lists available at ScienceDirect
JPRAS Open
journal homepage:www.elsevier.com/locate/jpra
Original Article
Challengesin global reconstructivemicrosurgery:
The sub-Saharanafrican surgeons’perspective
Chihena H. Bandaa,b,∗, Pafitanis Georgiosc,
Mitsunaga Narushimaa, Ryohei Ishiuraa, Minami Fujitaa,
Jovic Gorand
a Department of Plastic and Reconstructive Surgery, Graduate School of Medicine, Mie University, Tsu, Japan
b Department of Surgery, Arthur Davison Children’s Hospital, Ndola, Zambia
c Group for Academic Plastic Surgery, The Royal London Hospital, Barts Health NHS Trust, Queen Mary
University of London, London, UK
d Department of Surgery, The University Teaching Hospital, Lusaka, Zambia
a r t i c l e i n f o
Article history:
Received 20 November 2018
Accepted 20 January 2019
Available online 4 February 2019
Keywords:
Microsurgery
Free tissue transfer
Africa
Challenges
Training
Global surgery
a b s t r a c t
Background:Microsurgeryis an essentialelementof plastic surgery
practice.However,it remainsunavailableor rudimentaryin several
developingcountries, especially in sub-SaharanAfrica. This study
presents the local plastic surgeons experience,while focusing on
specific challengesencounteredand methods to improve the sub-
Saharanglobal microsurgerypractice.
Methodology: An online survey was sent to all plastic surgeons
registeredwith the College of SurgeonsEast Central and Southern
Africa and respectivenational plastic surgical societiesin the east
central and southern Africa regional community. A total of 57
questionnaireswere sent. Surgeons’country of practice, years of
experienceand rate of performing microsurgicalprocedureswere
considered.
∗ Corresponding author: Department of Plastic and Reconstructive Surgery, Graduate School of Medicine, Mie University,
2-174 Edobashi, Tsu, Mie Prefecture, 514-8507, JAPAN.
E-mail addresses: 318001c@m.mie-u.ac.jp , chihenab@gmail.com (C.H. Banda).
https://doi.org/10.1016/j.jpra.2019.01.009
2352-5878/© 2019 The Author(s).Published by Elsevier Ltd on behalf of British Association of Plastic,Reconstructive and
Aesthetic Surgeons. This is an open access article under the CC BY license. ( http://creativecommons.org/licenses/by/4.0/ )
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

20 C.H. Banda, P. Georgios and M. Narushima et al. / JPRAS Open 20 (2019) 19–26
Results: The survey responserate was 56%(n = 32). Most partici-
pants believedmicrosurgerywas essentialin the region. The lead-
ing challengewas inadequateperioperativecare,mainly attributed
to shortageof support staff (n = 29, 91%).Others were lack of sur-
gical expertiseand resources.Interestingly,public unawarenessof
the benefitsof microsurgerywas also noted as a critical hindrance.
The foremost suggestionon improvement(n = 19, 59%)was to en-
hance training with a multidisciplinary team-building approach.
Others included increasedadvocacy,publicationsand funding.
Conclusion: The Plastic surgeons’perspectiverecognizesthe needs
of Global ReconstructiveMicrosurgeryin sub-SaharanAfrica. How-
ever, inadequateperioperativecare, insufficient expertise,lack of
equipment and lack of public awarenesswere major hindrances.
Finally, there is a need to improve microsurgery in the region
through advocacy,training and multidisciplinaryteam building.
© 2019The Author(s).Published by Elsevier Ltd on behalf of
British Associationof Plastic,Reconstructiveand Aesthetic
Surgeons.
This is an open accessarticle under the CC BY license.
(http://creativecommons.org/licenses/by/4.0/)
Introduction
Microsurgery is an essential component of modern plastic reconstructivesurgery. The technique
facilitatesfree tissue transfer providing optimal functional and aestheticrecoveryfor a wide range of
complex tissue defects.Although traditionally pioneered by plastic surgeons,microsurgeryhas since
progressedand is increasinglybeing utilized by other specialitiessuch as otolaryngology,orthopaedics
and neurosurgery.With the current refinementsin techniqueand materials,the successrates of free
flaps in developedcountries are as high as 97%–99%.1,2 However,there is a growing gap between de-
veloped and developingcountries,with microsurgerycompletelyunavailableor rudimentary in many
developingcountries,particularly in the east, central and southern Africa (ECSA) region.3
Excluding South Africa, there are scarcely any reports on microsurgical free tissue transfer per-
formed in sub-SaharanAfrica. A few proceduresare occasionallyperformed by surgeonsvisiting from
developed countries with variable results.4–7 Nevertheless,local teams most notably in Kenya and
Uganda have overcomethe numerous challengesand have published their experiencesin a resource-
limited setting not indifferent from those found in other developing countries.3,6 Operations in the
region have largely been electivereconstructiveproceduresmost commonly for head and neck pathol-
ogy, such as cancer,noma and post-burn contracture,with the most frequentlyutilized flaps being the
radial forearm, free fibular and anterolateralthigh flaps.3–6 ,8 Nangole et al. reported using relatively
inexpensivemethods in Kenya including a basic microsurgeryset along with surgical loupes to per-
form free tissue transfers.3 However, such methods have attracted a mixed response of both praise
and criticism from the global community.9
Severalchallengesto performing microsurgeryin the region have been noted from the publications
of individual units and visiting surgeons.These include poor postoperativemonitoring, lack of high-
quality equipment and a lack of surgical skill together resulting in relatively low free flap survival
rates of 76%–89%.3,6,7 However,there is a paucity of literature objectively assessingthese challenges
particularly in countries that do not often practicemicrosurgery.Additionally,the perceivedchallenges
noted from individual unit experiencesdiffer widely. For instance,Citron et al.6 found equivocalflap
survival rates in casesperformed in Ugandabetweenlocal surgeonsand experiencedvisiting surgeons
from developedcountries suggestinglack of surgical skill3 may not be the prime cause of stagnation.
This highlights the crucial need to further explore the causesof suboptimal results in the region.
Results: The survey responserate was 56%(n = 32). Most partici-
pants believedmicrosurgerywas essentialin the region. The lead-
ing challengewas inadequateperioperativecare,mainly attributed
to shortageof support staff (n = 29, 91%).Others were lack of sur-
gical expertiseand resources.Interestingly,public unawarenessof
the benefitsof microsurgerywas also noted as a critical hindrance.
The foremost suggestionon improvement(n = 19, 59%)was to en-
hance training with a multidisciplinary team-building approach.
Others included increasedadvocacy,publicationsand funding.
Conclusion: The Plastic surgeons’perspectiverecognizesthe needs
of Global ReconstructiveMicrosurgeryin sub-SaharanAfrica. How-
ever, inadequateperioperativecare, insufficient expertise,lack of
equipment and lack of public awarenesswere major hindrances.
Finally, there is a need to improve microsurgery in the region
through advocacy,training and multidisciplinaryteam building.
© 2019The Author(s).Published by Elsevier Ltd on behalf of
British Associationof Plastic,Reconstructiveand Aesthetic
Surgeons.
This is an open accessarticle under the CC BY license.
(http://creativecommons.org/licenses/by/4.0/)
Introduction
Microsurgery is an essential component of modern plastic reconstructivesurgery. The technique
facilitatesfree tissue transfer providing optimal functional and aestheticrecoveryfor a wide range of
complex tissue defects.Although traditionally pioneered by plastic surgeons,microsurgeryhas since
progressedand is increasinglybeing utilized by other specialitiessuch as otolaryngology,orthopaedics
and neurosurgery.With the current refinementsin techniqueand materials,the successrates of free
flaps in developedcountries are as high as 97%–99%.1,2 However,there is a growing gap between de-
veloped and developingcountries,with microsurgerycompletelyunavailableor rudimentary in many
developingcountries,particularly in the east, central and southern Africa (ECSA) region.3
Excluding South Africa, there are scarcely any reports on microsurgical free tissue transfer per-
formed in sub-SaharanAfrica. A few proceduresare occasionallyperformed by surgeonsvisiting from
developed countries with variable results.4–7 Nevertheless,local teams most notably in Kenya and
Uganda have overcomethe numerous challengesand have published their experiencesin a resource-
limited setting not indifferent from those found in other developing countries.3,6 Operations in the
region have largely been electivereconstructiveproceduresmost commonly for head and neck pathol-
ogy, such as cancer,noma and post-burn contracture,with the most frequentlyutilized flaps being the
radial forearm, free fibular and anterolateralthigh flaps.3–6 ,8 Nangole et al. reported using relatively
inexpensivemethods in Kenya including a basic microsurgeryset along with surgical loupes to per-
form free tissue transfers.3 However, such methods have attracted a mixed response of both praise
and criticism from the global community.9
Severalchallengesto performing microsurgeryin the region have been noted from the publications
of individual units and visiting surgeons.These include poor postoperativemonitoring, lack of high-
quality equipment and a lack of surgical skill together resulting in relatively low free flap survival
rates of 76%–89%.3,6,7 However,there is a paucity of literature objectively assessingthese challenges
particularly in countries that do not often practicemicrosurgery.Additionally,the perceivedchallenges
noted from individual unit experiencesdiffer widely. For instance,Citron et al.6 found equivocalflap
survival rates in casesperformed in Ugandabetweenlocal surgeonsand experiencedvisiting surgeons
from developedcountries suggestinglack of surgical skill3 may not be the prime cause of stagnation.
This highlights the crucial need to further explore the causesof suboptimal results in the region.
C.H. Banda, P. Georgios and M. Narushima et al. / JPRAS Open 20 (2019) 19–26 21
On the positive side, the number of plastic surgeonsin the ECSA region is rapidly growing, largely
due to efforts in regional cooperation of surgical training fostered by the College of SurgeonsEast
Central and Southern Africa (COSECSA)and its partners.10,11 Consideringthis, coupled with the posi-
tive economic growth seen over the last decade,12,13 microsurgeryis poised to play a greater part in
reconstructivesurgery in this region in the years to come.
The aim of this study was to assessthe opinions of local plastic surgeonson the challengesfaced
practising microsurgeryin the ECSA region and how to improve the service.
Methodology
An anonymous survey (5-point Likert-style) was sent to all plastic surgeons registered with
COSECSA.Additional invitations were sent to all plastic surgeonsregisteredwith respectivenational
plastic surgeryassociations/societiesto ensuresurgeonsnot part of the regional collegewere also con-
tacted.The countries forming the ECSA region included in this survey were; Burundi, Ethiopia, Kenya,
Malawi, Mozambique,Namibia, Rwanda,South Sudan,Tanzania,Uganda,Zambia and Zimbabwe.Sur-
geons from Namibia were contacted individually, as the country only recently joined the regional
body. A total of 57 surgeonswere invited. Plastic surgeonsresident and practising in the region (in-
cluding academic and administrativepositions) as of July 1, 2018, were included in this study. All
surgeonswithout permanentresidencyin the region, such as visiting surgeons,charity missions and
COSECSAoverseasfellows, were excluded.Email reminders were sent after 2 weeks and 4 weeks to
encourageparticipation.
Data were collected for country of clinical practice,years of experience,number of microsurgery
procedures performed over the last 5 years, opinions on the challengesof microsurgery and sug-
gestions for improvement. The survey was delivered through an online platform, Google Forms
(https://goo.gl/forms/nKnhD1MzFNN1Gxgh1). Respondentswere grouped into two groups by country
of practice: countries with surgeonsreporting > 10 microsurgicalproceduresannually were assigned
to study Group A and the rest to Group B.
All survey questionswere digitalisedand analysedusing IBM SPSSStatistics25 (IBM Corp. Released
2017.IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp). Data were analysed
depending on country group and surgeons’years of experienceusing two-tailed Mann–Whitney U
and Kruskal–Wallis tests,respectively.Statisticalsignificancewas defined as P < 0.05.
Results
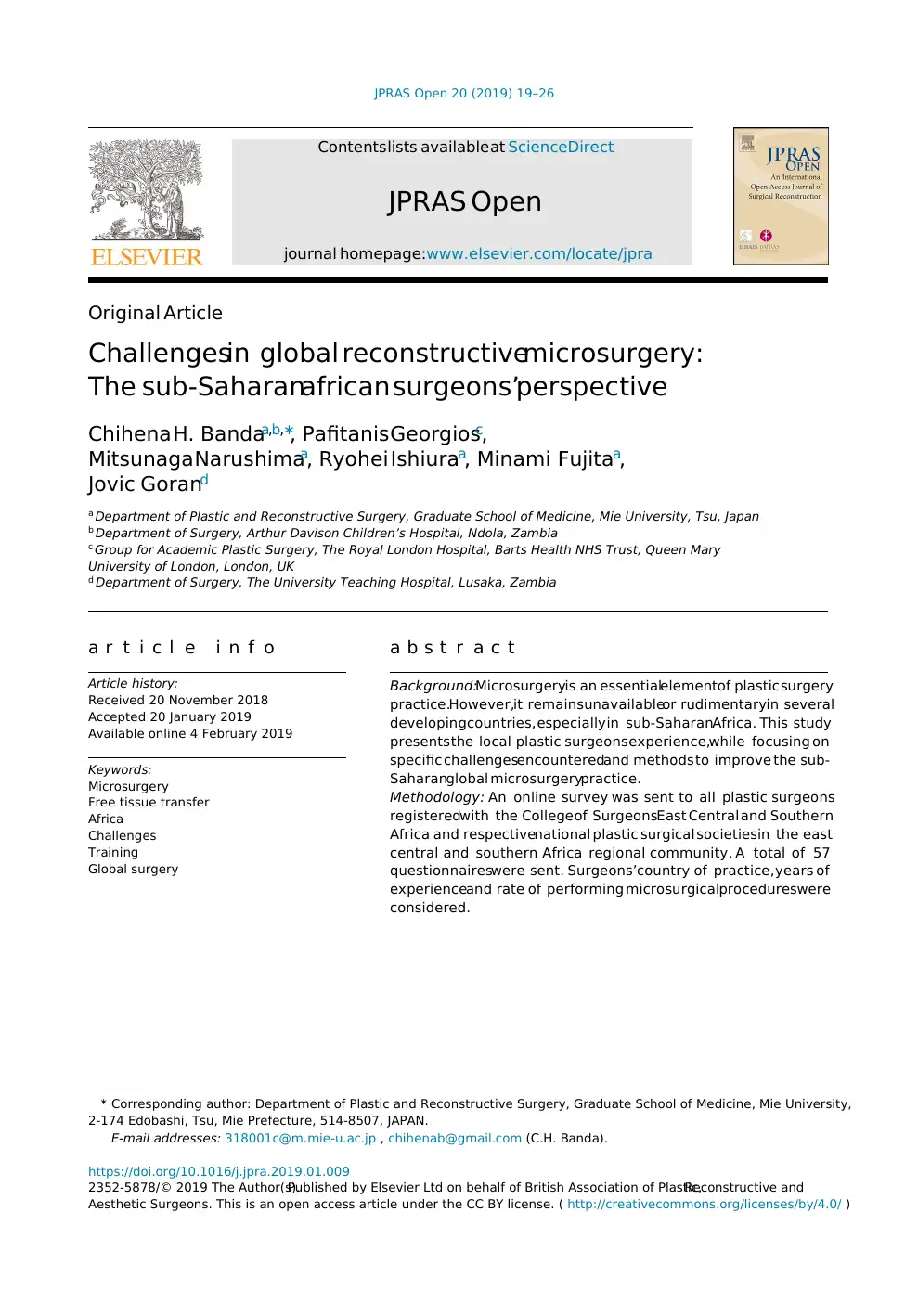
The survey responserate was 56%,with 32 of the regions 57 surgeonscompleting the survey.All
countries in the region were representedexcept for Burundi and South Sudan, which did not have
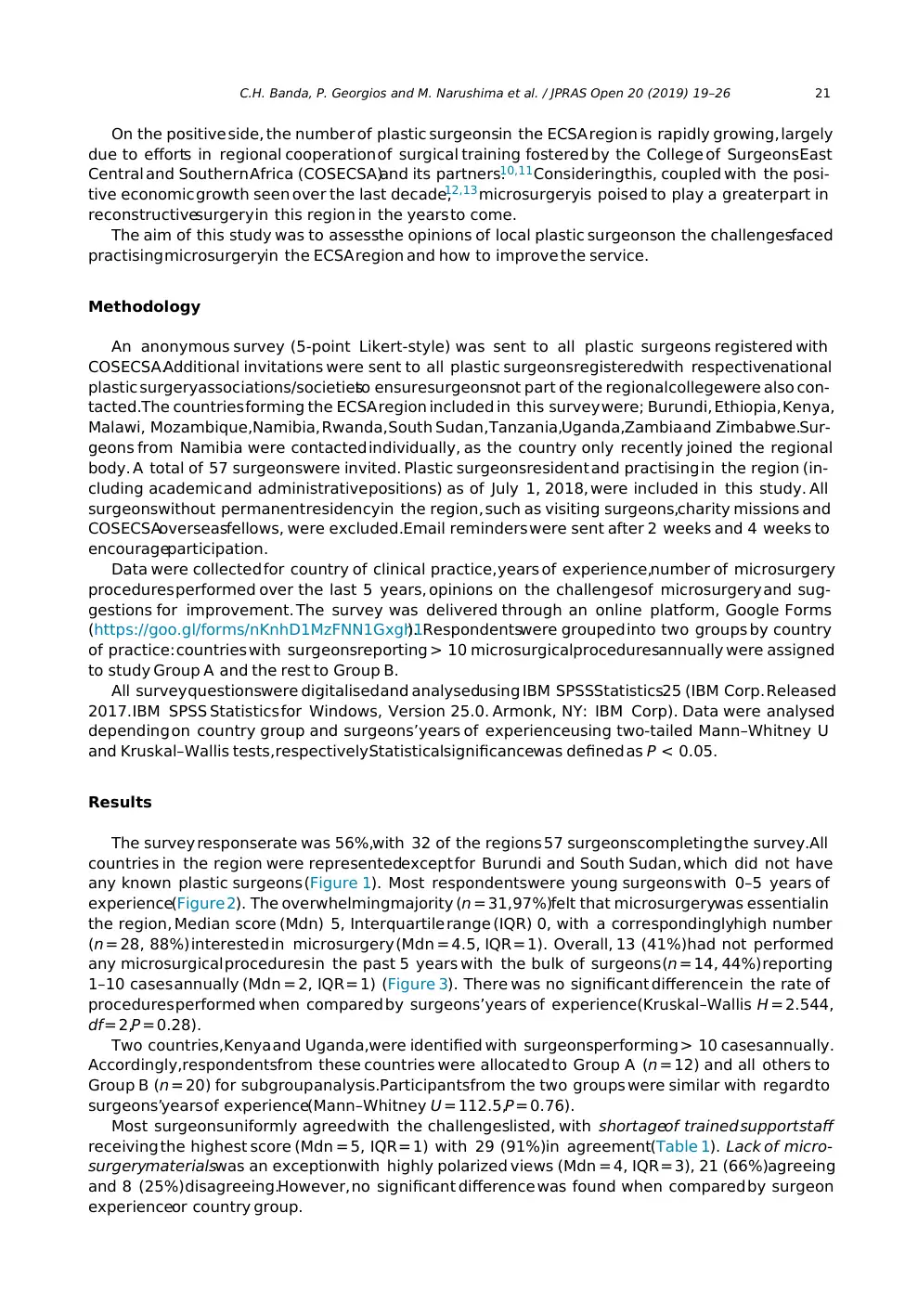
any known plastic surgeons (Figure 1). Most respondentswere young surgeons with 0–5 years of
experience(Figure 2). The overwhelmingmajority (n = 31,97%)felt that microsurgerywas essentialin
the region, Median score (Mdn) 5, Interquartile range (IQR) 0, with a correspondinglyhigh number
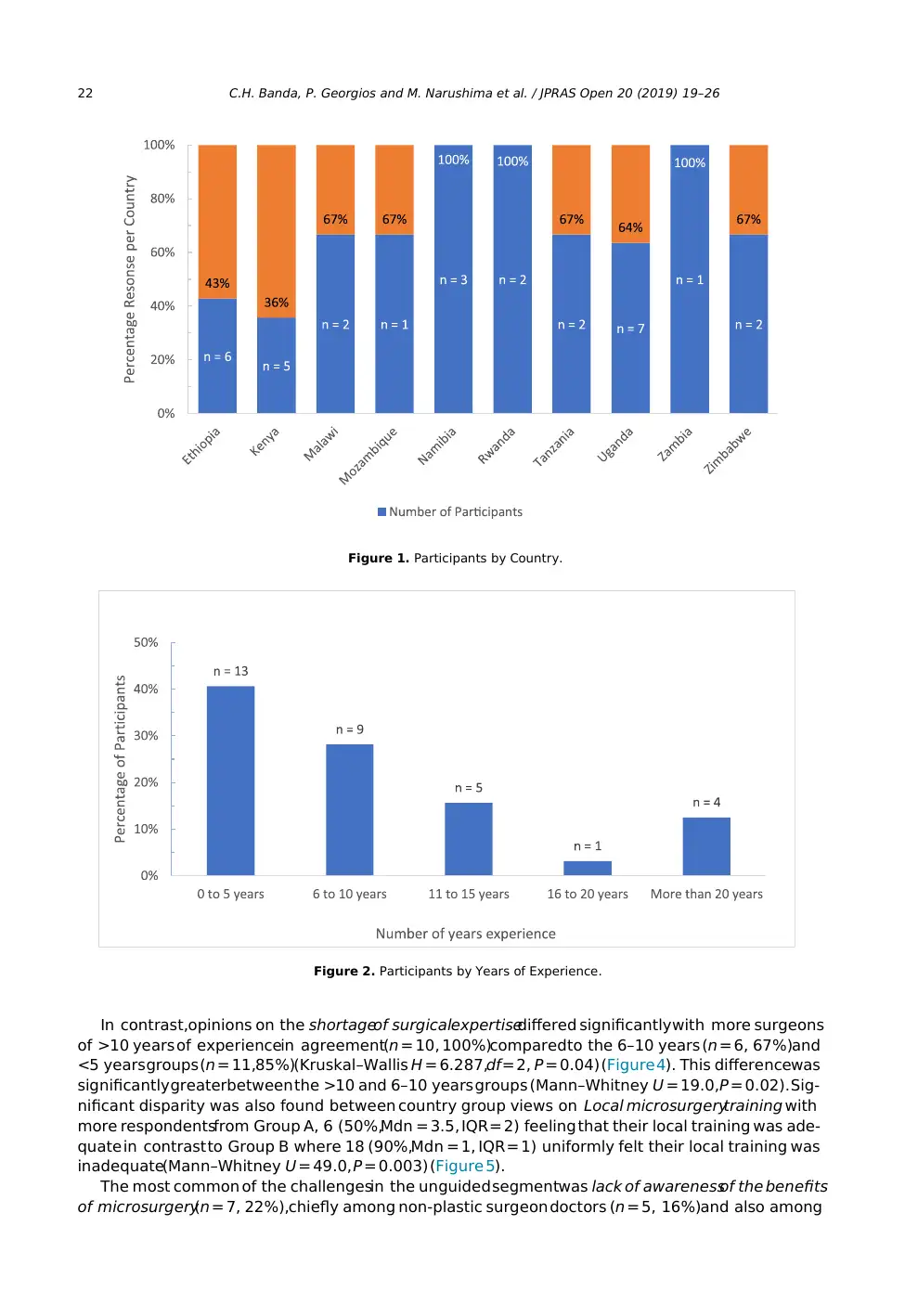
(n = 28, 88%) interested in microsurgery (Mdn = 4.5, IQR = 1). Overall, 13 (41%)had not performed
any microsurgical proceduresin the past 5 years with the bulk of surgeons (n = 14, 44%) reporting
1–10 cases annually (Mdn = 2, IQR = 1) (Figure 3). There was no significant difference in the rate of
procedures performed when compared by surgeons’years of experience(Kruskal–Wallis H = 2.544,
df = 2,P = 0.28).
Two countries,Kenya and Uganda,were identified with surgeonsperforming > 10 casesannually.
Accordingly,respondentsfrom these countries were allocated to Group A (n = 12) and all others to
Group B (n = 20) for subgroup analysis.Participantsfrom the two groups were similar with regard to
surgeons’years of experience(Mann–Whitney U = 112.5,P = 0.76).
Most surgeonsuniformly agreed with the challengeslisted, with shortageof trained support staff
receiving the highest score (Mdn = 5, IQR = 1) with 29 (91%)in agreement(Table 1). Lack of micro-
surgerymaterialswas an exceptionwith highly polarized views (Mdn = 4, IQR = 3), 21 (66%)agreeing
and 8 (25%)disagreeing.However, no significant difference was found when compared by surgeon
experienceor country group.
On the positive side, the number of plastic surgeonsin the ECSA region is rapidly growing, largely
due to efforts in regional cooperation of surgical training fostered by the College of SurgeonsEast
Central and Southern Africa (COSECSA)and its partners.10,11 Consideringthis, coupled with the posi-
tive economic growth seen over the last decade,12,13 microsurgeryis poised to play a greater part in
reconstructivesurgery in this region in the years to come.
The aim of this study was to assessthe opinions of local plastic surgeonson the challengesfaced
practising microsurgeryin the ECSA region and how to improve the service.
Methodology
An anonymous survey (5-point Likert-style) was sent to all plastic surgeons registered with
COSECSA.Additional invitations were sent to all plastic surgeonsregisteredwith respectivenational
plastic surgeryassociations/societiesto ensuresurgeonsnot part of the regional collegewere also con-
tacted.The countries forming the ECSA region included in this survey were; Burundi, Ethiopia, Kenya,
Malawi, Mozambique,Namibia, Rwanda,South Sudan,Tanzania,Uganda,Zambia and Zimbabwe.Sur-
geons from Namibia were contacted individually, as the country only recently joined the regional
body. A total of 57 surgeonswere invited. Plastic surgeonsresident and practising in the region (in-
cluding academic and administrativepositions) as of July 1, 2018, were included in this study. All
surgeonswithout permanentresidencyin the region, such as visiting surgeons,charity missions and
COSECSAoverseasfellows, were excluded.Email reminders were sent after 2 weeks and 4 weeks to
encourageparticipation.
Data were collected for country of clinical practice,years of experience,number of microsurgery
procedures performed over the last 5 years, opinions on the challengesof microsurgery and sug-
gestions for improvement. The survey was delivered through an online platform, Google Forms
(https://goo.gl/forms/nKnhD1MzFNN1Gxgh1). Respondentswere grouped into two groups by country
of practice: countries with surgeonsreporting > 10 microsurgicalproceduresannually were assigned
to study Group A and the rest to Group B.
All survey questionswere digitalisedand analysedusing IBM SPSSStatistics25 (IBM Corp. Released
2017.IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp). Data were analysed
depending on country group and surgeons’years of experienceusing two-tailed Mann–Whitney U
and Kruskal–Wallis tests,respectively.Statisticalsignificancewas defined as P < 0.05.
Results
The survey responserate was 56%,with 32 of the regions 57 surgeonscompleting the survey.All
countries in the region were representedexcept for Burundi and South Sudan, which did not have
any known plastic surgeons (Figure 1). Most respondentswere young surgeons with 0–5 years of
experience(Figure 2). The overwhelmingmajority (n = 31,97%)felt that microsurgerywas essentialin
the region, Median score (Mdn) 5, Interquartile range (IQR) 0, with a correspondinglyhigh number
(n = 28, 88%) interested in microsurgery (Mdn = 4.5, IQR = 1). Overall, 13 (41%)had not performed
any microsurgical proceduresin the past 5 years with the bulk of surgeons (n = 14, 44%) reporting
1–10 cases annually (Mdn = 2, IQR = 1) (Figure 3). There was no significant difference in the rate of
procedures performed when compared by surgeons’years of experience(Kruskal–Wallis H = 2.544,
df = 2,P = 0.28).
Two countries,Kenya and Uganda,were identified with surgeonsperforming > 10 casesannually.
Accordingly,respondentsfrom these countries were allocated to Group A (n = 12) and all others to
Group B (n = 20) for subgroup analysis.Participantsfrom the two groups were similar with regard to
surgeons’years of experience(Mann–Whitney U = 112.5,P = 0.76).
Most surgeonsuniformly agreed with the challengeslisted, with shortageof trained support staff
receiving the highest score (Mdn = 5, IQR = 1) with 29 (91%)in agreement(Table 1). Lack of micro-
surgerymaterialswas an exceptionwith highly polarized views (Mdn = 4, IQR = 3), 21 (66%)agreeing
and 8 (25%)disagreeing.However, no significant difference was found when compared by surgeon
experienceor country group.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
22 C.H. Banda, P. Georgios and M. Narushima et al. / JPRAS Open 20 (2019) 19–26
Figure 1. Participants by Country.
Figure 2. Participants by Years of Experience.
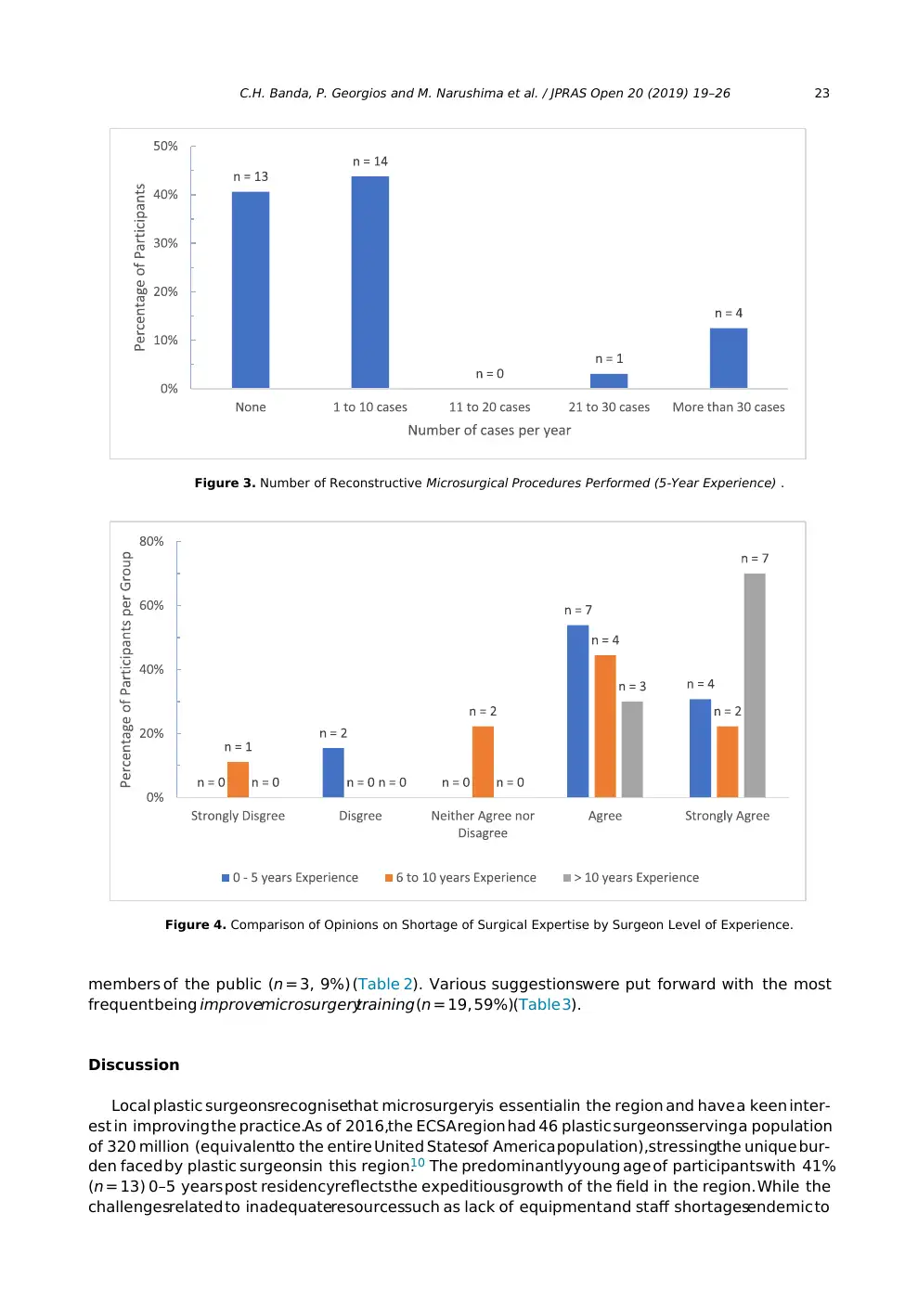
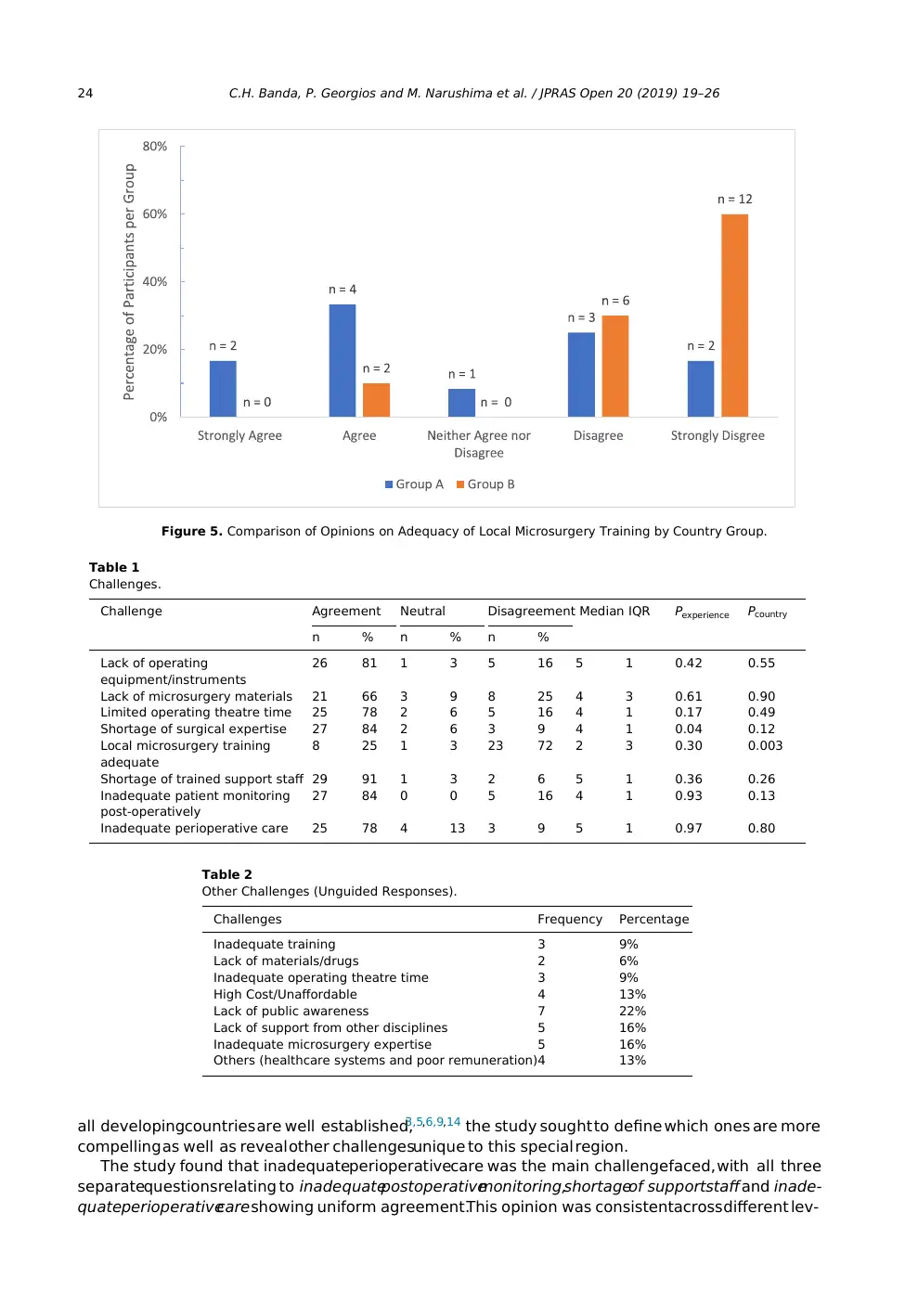
In contrast,opinions on the shortageof surgicalexpertisediffered significantly with more surgeons
of >10 years of experiencein agreement(n = 10, 100%)comparedto the 6–10 years (n = 6, 67%)and
<5 years groups (n = 11,85%)(Kruskal–Wallis H = 6.287,df = 2, P = 0.04) (Figure 4). This differencewas
significantly greaterbetween the >10 and 6–10 years groups (Mann–Whitney U = 19.0,P = 0.02). Sig-
nificant disparity was also found between country group views on Local microsurgerytraining with
more respondentsfrom Group A, 6 (50%,Mdn = 3.5, IQR = 2) feeling that their local training was ade-
quate in contrast to Group B where 18 (90%,Mdn = 1, IQR = 1) uniformly felt their local training was
inadequate(Mann–Whitney U = 49.0, P = 0.003) (Figure 5).
The most common of the challengesin the unguided segmentwas lack of awarenessof the benefits
of microsurgery(n = 7, 22%),chiefly among non-plastic surgeon doctors (n = 5, 16%)and also among
Figure 1. Participants by Country.
Figure 2. Participants by Years of Experience.
In contrast,opinions on the shortageof surgicalexpertisediffered significantly with more surgeons
of >10 years of experiencein agreement(n = 10, 100%)comparedto the 6–10 years (n = 6, 67%)and
<5 years groups (n = 11,85%)(Kruskal–Wallis H = 6.287,df = 2, P = 0.04) (Figure 4). This differencewas
significantly greaterbetween the >10 and 6–10 years groups (Mann–Whitney U = 19.0,P = 0.02). Sig-
nificant disparity was also found between country group views on Local microsurgerytraining with
more respondentsfrom Group A, 6 (50%,Mdn = 3.5, IQR = 2) feeling that their local training was ade-
quate in contrast to Group B where 18 (90%,Mdn = 1, IQR = 1) uniformly felt their local training was
inadequate(Mann–Whitney U = 49.0, P = 0.003) (Figure 5).
The most common of the challengesin the unguided segmentwas lack of awarenessof the benefits
of microsurgery(n = 7, 22%),chiefly among non-plastic surgeon doctors (n = 5, 16%)and also among
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
C.H. Banda, P. Georgios and M. Narushima et al. / JPRAS Open 20 (2019) 19–26 23
Figure 3. Number of Reconstructive Microsurgical Procedures Performed (5-Year Experience) .
Figure 4. Comparison of Opinions on Shortage of Surgical Expertise by Surgeon Level of Experience.
members of the public (n = 3, 9%) (Table 2). Various suggestionswere put forward with the most
frequent being improvemicrosurgerytraining (n = 19, 59%)(Table 3).
Discussion
Local plastic surgeonsrecognisethat microsurgeryis essentialin the region and have a keen inter-
est in improving the practice.As of 2016,the ECSA region had 46 plastic surgeonsserving a population
of 320 million (equivalentto the entire United Statesof America population),stressingthe unique bur-
den faced by plastic surgeonsin this region.10 The predominantlyyoung age of participantswith 41%
(n = 13) 0–5 years post residencyreflects the expeditiousgrowth of the field in the region. While the
challengesrelated to inadequateresourcessuch as lack of equipment and staff shortagesendemic to
Figure 3. Number of Reconstructive Microsurgical Procedures Performed (5-Year Experience) .
Figure 4. Comparison of Opinions on Shortage of Surgical Expertise by Surgeon Level of Experience.
members of the public (n = 3, 9%) (Table 2). Various suggestionswere put forward with the most
frequent being improvemicrosurgerytraining (n = 19, 59%)(Table 3).
Discussion
Local plastic surgeonsrecognisethat microsurgeryis essentialin the region and have a keen inter-
est in improving the practice.As of 2016,the ECSA region had 46 plastic surgeonsserving a population
of 320 million (equivalentto the entire United Statesof America population),stressingthe unique bur-
den faced by plastic surgeonsin this region.10 The predominantlyyoung age of participantswith 41%
(n = 13) 0–5 years post residencyreflects the expeditiousgrowth of the field in the region. While the
challengesrelated to inadequateresourcessuch as lack of equipment and staff shortagesendemic to
24 C.H. Banda, P. Georgios and M. Narushima et al. / JPRAS Open 20 (2019) 19–26
Figure 5. Comparison of Opinions on Adequacy of Local Microsurgery Training by Country Group.
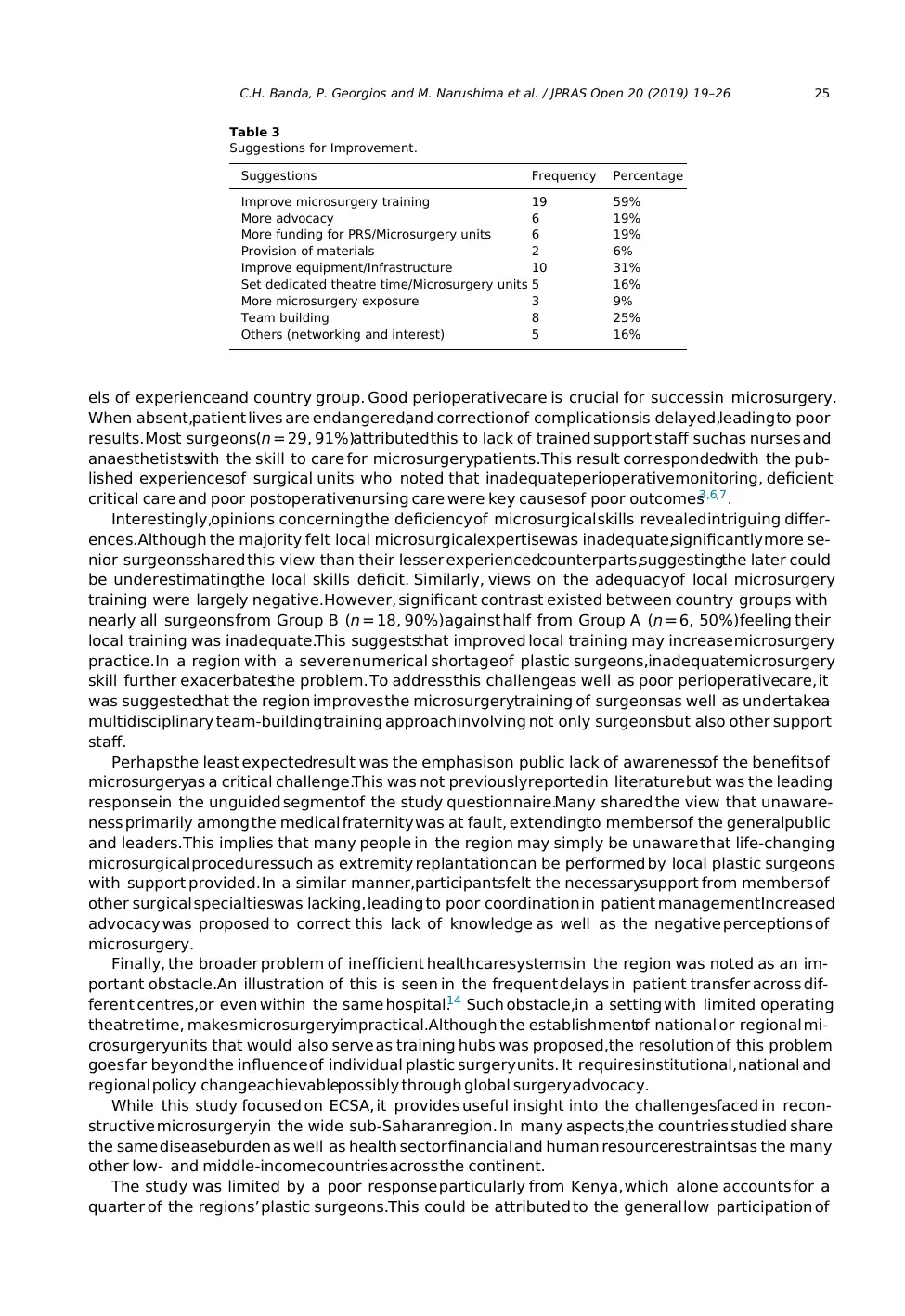
Table 1
Challenges.
Challenge Agreement Neutral Disagreement Median IQR Pexperience Pcountry
n % n % n %
Lack of operating
equipment/instruments
26 81 1 3 5 16 5 1 0.42 0.55
Lack of microsurgery materials 21 66 3 9 8 25 4 3 0.61 0.90
Limited operating theatre time 25 78 2 6 5 16 4 1 0.17 0.49
Shortage of surgical expertise 27 84 2 6 3 9 4 1 0.04 0.12
Local microsurgery training
adequate
8 25 1 3 23 72 2 3 0.30 0.003
Shortage of trained support staff 29 91 1 3 2 6 5 1 0.36 0.26
Inadequate patient monitoring
post-operatively
27 84 0 0 5 16 4 1 0.93 0.13
Inadequate perioperative care 25 78 4 13 3 9 5 1 0.97 0.80
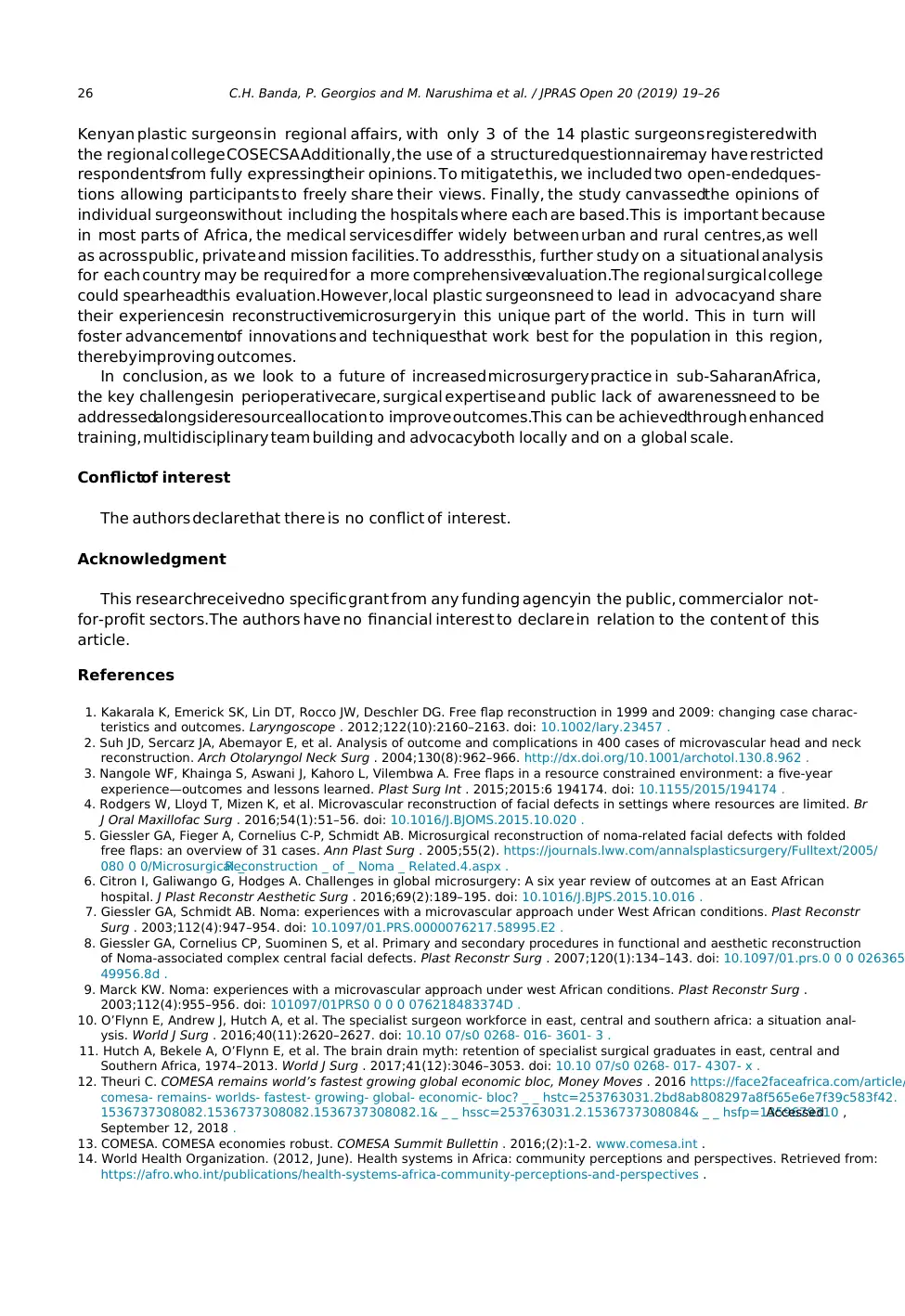
Table 2
Other Challenges (Unguided Responses).
Challenges Frequency Percentage
Inadequate training 3 9%
Lack of materials/drugs 2 6%
Inadequate operating theatre time 3 9%
High Cost/Unaffordable 4 13%
Lack of public awareness 7 22%
Lack of support from other disciplines 5 16%
Inadequate microsurgery expertise 5 16%
Others (healthcare systems and poor remuneration)4 13%
all developingcountries are well established,3,5,6,9,14 the study sought to define which ones are more
compelling as well as reveal other challengesunique to this special region.
The study found that inadequateperioperativecare was the main challengefaced, with all three
separatequestionsrelating to inadequatepostoperativemonitoring,shortageof supportstaffand inade-
quateperioperativecare showing uniform agreement.This opinion was consistentacross different lev-
Figure 5. Comparison of Opinions on Adequacy of Local Microsurgery Training by Country Group.
Table 1
Challenges.
Challenge Agreement Neutral Disagreement Median IQR Pexperience Pcountry
n % n % n %
Lack of operating
equipment/instruments
26 81 1 3 5 16 5 1 0.42 0.55
Lack of microsurgery materials 21 66 3 9 8 25 4 3 0.61 0.90
Limited operating theatre time 25 78 2 6 5 16 4 1 0.17 0.49
Shortage of surgical expertise 27 84 2 6 3 9 4 1 0.04 0.12
Local microsurgery training
adequate
8 25 1 3 23 72 2 3 0.30 0.003
Shortage of trained support staff 29 91 1 3 2 6 5 1 0.36 0.26
Inadequate patient monitoring
post-operatively
27 84 0 0 5 16 4 1 0.93 0.13
Inadequate perioperative care 25 78 4 13 3 9 5 1 0.97 0.80
Table 2
Other Challenges (Unguided Responses).
Challenges Frequency Percentage
Inadequate training 3 9%
Lack of materials/drugs 2 6%
Inadequate operating theatre time 3 9%
High Cost/Unaffordable 4 13%
Lack of public awareness 7 22%
Lack of support from other disciplines 5 16%
Inadequate microsurgery expertise 5 16%
Others (healthcare systems and poor remuneration)4 13%
all developingcountries are well established,3,5,6,9,14 the study sought to define which ones are more
compelling as well as reveal other challengesunique to this special region.
The study found that inadequateperioperativecare was the main challengefaced, with all three
separatequestionsrelating to inadequatepostoperativemonitoring,shortageof supportstaffand inade-
quateperioperativecare showing uniform agreement.This opinion was consistentacross different lev-
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
C.H. Banda, P. Georgios and M. Narushima et al. / JPRAS Open 20 (2019) 19–26 25
Table 3
Suggestions for Improvement.
Suggestions Frequency Percentage
Improve microsurgery training 19 59%
More advocacy 6 19%
More funding for PRS/Microsurgery units 6 19%
Provision of materials 2 6%
Improve equipment/Infrastructure 10 31%
Set dedicated theatre time/Microsurgery units 5 16%
More microsurgery exposure 3 9%
Team building 8 25%
Others (networking and interest) 5 16%
els of experienceand country group. Good perioperativecare is crucial for successin microsurgery.
When absent,patient lives are endangered,and correction of complicationsis delayed,leading to poor
results. Most surgeons(n = 29, 91%)attributed this to lack of trained support staff such as nurses and
anaesthetistswith the skill to care for microsurgerypatients.This result correspondedwith the pub-
lished experiencesof surgical units who noted that inadequateperioperativemonitoring, deficient
critical care and poor postoperativenursing care were key causesof poor outcomes3,6,7.
Interestingly,opinions concerning the deficiency of microsurgical skills revealedintriguing differ-
ences.Although the majority felt local microsurgicalexpertisewas inadequate,significantly more se-
nior surgeonsshared this view than their lesser experiencedcounterparts,suggestingthe later could
be underestimatingthe local skills deficit. Similarly, views on the adequacyof local microsurgery
training were largely negative.However, significant contrast existed between country groups with
nearly all surgeons from Group B (n = 18, 90%)against half from Group A (n = 6, 50%)feeling their
local training was inadequate.This suggeststhat improved local training may increase microsurgery
practice. In a region with a severe numerical shortage of plastic surgeons,inadequatemicrosurgery
skill further exacerbatesthe problem. To addressthis challengeas well as poor perioperativecare, it
was suggestedthat the region improves the microsurgerytraining of surgeonsas well as undertakea
multidisciplinary team-building training approachinvolving not only surgeonsbut also other support
staff.
Perhaps the least expectedresult was the emphasison public lack of awarenessof the benefits of
microsurgeryas a critical challenge.This was not previouslyreported in literature but was the leading
responsein the unguided segmentof the study questionnaire.Many shared the view that unaware-
ness primarily among the medical fraternity was at fault, extendingto membersof the generalpublic
and leaders.This implies that many people in the region may simply be unaware that life-changing
microsurgical proceduressuch as extremity replantation can be performed by local plastic surgeons
with support provided. In a similar manner,participantsfelt the necessarysupport from members of
other surgical specialtieswas lacking, leading to poor coordination in patient management.Increased
advocacy was proposed to correct this lack of knowledge as well as the negative perceptions of
microsurgery.
Finally, the broader problem of inefficient healthcaresystemsin the region was noted as an im-
portant obstacle.An illustration of this is seen in the frequent delays in patient transfer across dif-
ferent centres,or even within the same hospital.14 Such obstacle,in a setting with limited operating
theatre time, makes microsurgeryimpractical.Although the establishmentof national or regional mi-
crosurgeryunits that would also serve as training hubs was proposed,the resolution of this problem
goes far beyond the influence of individual plastic surgery units. It requires institutional, national and
regional policy changeachievablepossibly through global surgery advocacy.
While this study focused on ECSA, it provides useful insight into the challengesfaced in recon-
structive microsurgeryin the wide sub-Saharanregion. In many aspects,the countries studied share
the same diseaseburden as well as health sector financial and human resourcerestraintsas the many
other low- and middle-income countries across the continent.
The study was limited by a poor response particularly from Kenya, which alone accounts for a
quarter of the regions’ plastic surgeons.This could be attributed to the general low participation of
Table 3
Suggestions for Improvement.
Suggestions Frequency Percentage
Improve microsurgery training 19 59%
More advocacy 6 19%
More funding for PRS/Microsurgery units 6 19%
Provision of materials 2 6%
Improve equipment/Infrastructure 10 31%
Set dedicated theatre time/Microsurgery units 5 16%
More microsurgery exposure 3 9%
Team building 8 25%
Others (networking and interest) 5 16%
els of experienceand country group. Good perioperativecare is crucial for successin microsurgery.
When absent,patient lives are endangered,and correction of complicationsis delayed,leading to poor
results. Most surgeons(n = 29, 91%)attributed this to lack of trained support staff such as nurses and
anaesthetistswith the skill to care for microsurgerypatients.This result correspondedwith the pub-
lished experiencesof surgical units who noted that inadequateperioperativemonitoring, deficient
critical care and poor postoperativenursing care were key causesof poor outcomes3,6,7.
Interestingly,opinions concerning the deficiency of microsurgical skills revealedintriguing differ-
ences.Although the majority felt local microsurgicalexpertisewas inadequate,significantly more se-
nior surgeonsshared this view than their lesser experiencedcounterparts,suggestingthe later could
be underestimatingthe local skills deficit. Similarly, views on the adequacyof local microsurgery
training were largely negative.However, significant contrast existed between country groups with
nearly all surgeons from Group B (n = 18, 90%)against half from Group A (n = 6, 50%)feeling their
local training was inadequate.This suggeststhat improved local training may increase microsurgery
practice. In a region with a severe numerical shortage of plastic surgeons,inadequatemicrosurgery
skill further exacerbatesthe problem. To addressthis challengeas well as poor perioperativecare, it
was suggestedthat the region improves the microsurgerytraining of surgeonsas well as undertakea
multidisciplinary team-building training approachinvolving not only surgeonsbut also other support
staff.
Perhaps the least expectedresult was the emphasison public lack of awarenessof the benefits of
microsurgeryas a critical challenge.This was not previouslyreported in literature but was the leading
responsein the unguided segmentof the study questionnaire.Many shared the view that unaware-
ness primarily among the medical fraternity was at fault, extendingto membersof the generalpublic
and leaders.This implies that many people in the region may simply be unaware that life-changing
microsurgical proceduressuch as extremity replantation can be performed by local plastic surgeons
with support provided. In a similar manner,participantsfelt the necessarysupport from members of
other surgical specialtieswas lacking, leading to poor coordination in patient management.Increased
advocacy was proposed to correct this lack of knowledge as well as the negative perceptions of
microsurgery.
Finally, the broader problem of inefficient healthcaresystemsin the region was noted as an im-
portant obstacle.An illustration of this is seen in the frequent delays in patient transfer across dif-
ferent centres,or even within the same hospital.14 Such obstacle,in a setting with limited operating
theatre time, makes microsurgeryimpractical.Although the establishmentof national or regional mi-
crosurgeryunits that would also serve as training hubs was proposed,the resolution of this problem
goes far beyond the influence of individual plastic surgery units. It requires institutional, national and
regional policy changeachievablepossibly through global surgery advocacy.
While this study focused on ECSA, it provides useful insight into the challengesfaced in recon-
structive microsurgeryin the wide sub-Saharanregion. In many aspects,the countries studied share
the same diseaseburden as well as health sector financial and human resourcerestraintsas the many
other low- and middle-income countries across the continent.
The study was limited by a poor response particularly from Kenya, which alone accounts for a
quarter of the regions’ plastic surgeons.This could be attributed to the general low participation of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
26 C.H. Banda, P. Georgios and M. Narushima et al. / JPRAS Open 20 (2019) 19–26
Kenyan plastic surgeons in regional affairs, with only 3 of the 14 plastic surgeons registered with
the regional college COSECSA.Additionally, the use of a structured questionnairemay have restricted
respondentsfrom fully expressingtheir opinions. To mitigate this, we included two open-endedques-
tions allowing participants to freely share their views. Finally, the study canvassedthe opinions of
individual surgeonswithout including the hospitals where each are based.This is important because
in most parts of Africa, the medical services differ widely between urban and rural centres,as well
as across public, private and mission facilities. To addressthis, further study on a situational analysis
for each country may be required for a more comprehensiveevaluation.The regional surgical college
could spearheadthis evaluation.However,local plastic surgeonsneed to lead in advocacyand share
their experiencesin reconstructivemicrosurgery in this unique part of the world. This in turn will
foster advancementof innovations and techniquesthat work best for the population in this region,
therebyimproving outcomes.
In conclusion, as we look to a future of increased microsurgery practice in sub-SaharanAfrica,
the key challengesin perioperativecare, surgical expertise and public lack of awarenessneed to be
addressedalongsideresourceallocation to improve outcomes.This can be achievedthrough enhanced
training, multidisciplinary team building and advocacyboth locally and on a global scale.
Conflictof interest
The authors declarethat there is no conflict of interest.
Acknowledgment
This researchreceivedno specific grant from any funding agencyin the public, commercialor not-
for-profit sectors.The authors have no financial interest to declare in relation to the content of this
article.
References
1. Kakarala K, Emerick SK, Lin DT, Rocco JW, Deschler DG. Free flap reconstruction in 1999 and 2009: changing case charac-
teristics and outcomes. Laryngoscope . 2012;122(10):2160–2163. doi: 10.1002/lary.23457 .
2. Suh JD, Sercarz JA, Abemayor E, et al. Analysis of outcome and complications in 400 cases of microvascular head and neck
reconstruction. Arch Otolaryngol Neck Surg . 2004;130(8):962–966. http://dx.doi.org/10.1001/archotol.130.8.962 .
3. Nangole WF, Khainga S, Aswani J, Kahoro L, Vilembwa A. Free flaps in a resource constrained environment: a five-year
experience—outcomes and lessons learned. Plast Surg Int . 2015;2015:6 194174. doi: 10.1155/2015/194174 .
4. Rodgers W, Lloyd T, Mizen K, et al. Microvascular reconstruction of facial defects in settings where resources are limited. Br
J Oral Maxillofac Surg . 2016;54(1):51–56. doi: 10.1016/J.BJOMS.2015.10.020 .
5. Giessler GA, Fieger A, Cornelius C-P, Schmidt AB. Microsurgical reconstruction of noma-related facial defects with folded
free flaps: an overview of 31 cases. Ann Plast Surg . 2005;55(2). https://journals.lww.com/annalsplasticsurgery/Fulltext/2005/
080 0 0/Microsurgical _Reconstruction _ of _ Noma _ Related.4.aspx .
6. Citron I, Galiwango G, Hodges A. Challenges in global microsurgery: A six year review of outcomes at an East African
hospital. J Plast Reconstr Aesthetic Surg . 2016;69(2):189–195. doi: 10.1016/J.BJPS.2015.10.016 .
7. Giessler GA, Schmidt AB. Noma: experiences with a microvascular approach under West African conditions. Plast Reconstr
Surg . 2003;112(4):947–954. doi: 10.1097/01.PRS.0000076217.58995.E2 .
8. Giessler GA, Cornelius CP, Suominen S, et al. Primary and secondary procedures in functional and aesthetic reconstruction
of Noma-associated complex central facial defects. Plast Reconstr Surg . 2007;120(1):134–143. doi: 10.1097/01.prs.0 0 0 026365
49956.8d .
9. Marck KW. Noma: experiences with a microvascular approach under west African conditions. Plast Reconstr Surg .
2003;112(4):955–956. doi: 101097/01PRS0 0 0 0 076218483374D .
10. O’Flynn E, Andrew J, Hutch A, et al. The specialist surgeon workforce in east, central and southern africa: a situation anal-
ysis. World J Surg . 2016;40(11):2620–2627. doi: 10.10 07/s0 0268- 016- 3601- 3 .
11. Hutch A, Bekele A, O’Flynn E, et al. The brain drain myth: retention of specialist surgical graduates in east, central and
Southern Africa, 1974–2013. World J Surg . 2017;41(12):3046–3053. doi: 10.10 07/s0 0268- 017- 4307- x .
12. Theuri C. COMESA remains world’s fastest growing global economic bloc, Money Moves . 2016 https://face2faceafrica.com/article/
comesa- remains- worlds- fastest- growing- global- economic- bloc? _ _ hstc=253763031.2bd8ab808297a8f565e6e7f39c583f42.
1536737308082.1536737308082.1536737308082.1& _ _ hssc=253763031.2.1536737308084& _ _ hsfp=1359679310 ,Accessed
September 12, 2018 .
13. COMESA. COMESA economies robust. COMESA Summit Bullettin . 2016;(2):1-2. www.comesa.int .
14. World Health Organization. (2012, June). Health systems in Africa: community perceptions and perspectives. Retrieved from:
https://afro.who.int/publications/health-systems-africa-community-perceptions-and-perspectives .
Kenyan plastic surgeons in regional affairs, with only 3 of the 14 plastic surgeons registered with
the regional college COSECSA.Additionally, the use of a structured questionnairemay have restricted
respondentsfrom fully expressingtheir opinions. To mitigate this, we included two open-endedques-
tions allowing participants to freely share their views. Finally, the study canvassedthe opinions of
individual surgeonswithout including the hospitals where each are based.This is important because
in most parts of Africa, the medical services differ widely between urban and rural centres,as well
as across public, private and mission facilities. To addressthis, further study on a situational analysis
for each country may be required for a more comprehensiveevaluation.The regional surgical college
could spearheadthis evaluation.However,local plastic surgeonsneed to lead in advocacyand share
their experiencesin reconstructivemicrosurgery in this unique part of the world. This in turn will
foster advancementof innovations and techniquesthat work best for the population in this region,
therebyimproving outcomes.
In conclusion, as we look to a future of increased microsurgery practice in sub-SaharanAfrica,
the key challengesin perioperativecare, surgical expertise and public lack of awarenessneed to be
addressedalongsideresourceallocation to improve outcomes.This can be achievedthrough enhanced
training, multidisciplinary team building and advocacyboth locally and on a global scale.
Conflictof interest
The authors declarethat there is no conflict of interest.
Acknowledgment
This researchreceivedno specific grant from any funding agencyin the public, commercialor not-
for-profit sectors.The authors have no financial interest to declare in relation to the content of this
article.
References
1. Kakarala K, Emerick SK, Lin DT, Rocco JW, Deschler DG. Free flap reconstruction in 1999 and 2009: changing case charac-
teristics and outcomes. Laryngoscope . 2012;122(10):2160–2163. doi: 10.1002/lary.23457 .
2. Suh JD, Sercarz JA, Abemayor E, et al. Analysis of outcome and complications in 400 cases of microvascular head and neck
reconstruction. Arch Otolaryngol Neck Surg . 2004;130(8):962–966. http://dx.doi.org/10.1001/archotol.130.8.962 .
3. Nangole WF, Khainga S, Aswani J, Kahoro L, Vilembwa A. Free flaps in a resource constrained environment: a five-year
experience—outcomes and lessons learned. Plast Surg Int . 2015;2015:6 194174. doi: 10.1155/2015/194174 .
4. Rodgers W, Lloyd T, Mizen K, et al. Microvascular reconstruction of facial defects in settings where resources are limited. Br
J Oral Maxillofac Surg . 2016;54(1):51–56. doi: 10.1016/J.BJOMS.2015.10.020 .
5. Giessler GA, Fieger A, Cornelius C-P, Schmidt AB. Microsurgical reconstruction of noma-related facial defects with folded
free flaps: an overview of 31 cases. Ann Plast Surg . 2005;55(2). https://journals.lww.com/annalsplasticsurgery/Fulltext/2005/
080 0 0/Microsurgical _Reconstruction _ of _ Noma _ Related.4.aspx .
6. Citron I, Galiwango G, Hodges A. Challenges in global microsurgery: A six year review of outcomes at an East African
hospital. J Plast Reconstr Aesthetic Surg . 2016;69(2):189–195. doi: 10.1016/J.BJPS.2015.10.016 .
7. Giessler GA, Schmidt AB. Noma: experiences with a microvascular approach under West African conditions. Plast Reconstr
Surg . 2003;112(4):947–954. doi: 10.1097/01.PRS.0000076217.58995.E2 .
8. Giessler GA, Cornelius CP, Suominen S, et al. Primary and secondary procedures in functional and aesthetic reconstruction
of Noma-associated complex central facial defects. Plast Reconstr Surg . 2007;120(1):134–143. doi: 10.1097/01.prs.0 0 0 026365
49956.8d .
9. Marck KW. Noma: experiences with a microvascular approach under west African conditions. Plast Reconstr Surg .
2003;112(4):955–956. doi: 101097/01PRS0 0 0 0 076218483374D .
10. O’Flynn E, Andrew J, Hutch A, et al. The specialist surgeon workforce in east, central and southern africa: a situation anal-
ysis. World J Surg . 2016;40(11):2620–2627. doi: 10.10 07/s0 0268- 016- 3601- 3 .
11. Hutch A, Bekele A, O’Flynn E, et al. The brain drain myth: retention of specialist surgical graduates in east, central and
Southern Africa, 1974–2013. World J Surg . 2017;41(12):3046–3053. doi: 10.10 07/s0 0268- 017- 4307- x .
12. Theuri C. COMESA remains world’s fastest growing global economic bloc, Money Moves . 2016 https://face2faceafrica.com/article/
comesa- remains- worlds- fastest- growing- global- economic- bloc? _ _ hstc=253763031.2bd8ab808297a8f565e6e7f39c583f42.
1536737308082.1536737308082.1536737308082.1& _ _ hssc=253763031.2.1536737308084& _ _ hsfp=1359679310 ,Accessed
September 12, 2018 .
13. COMESA. COMESA economies robust. COMESA Summit Bullettin . 2016;(2):1-2. www.comesa.int .
14. World Health Organization. (2012, June). Health systems in Africa: community perceptions and perspectives. Retrieved from:
https://afro.who.int/publications/health-systems-africa-community-perceptions-and-perspectives .
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.