Reflective Approaches in Implementing Person Centred Practice Report
VerifiedAdded on 2023/01/19
|2
|1238
|57
Report
AI Summary
This report delves into person-centred practice within healthcare, comparing the medical and social models and their application. It examines the importance of patient knowledge, beneficence, power dynamics, therapeutic alliances, and self-awareness within the medical model, contrasting it with the social model's focus on removing societal barriers. The report further discusses adopting a person-centred approach, outlining key steps for support workers, including addressing challenging behaviors, promoting self-awareness, respecting patient values, fostering engagement, encouraging shared decision-making, practicing empathy, and implementing holistic care. Challenges faced, such as conflicts and dilemmas, are reviewed, and their impact on consistency in approach is evaluated, emphasizing the need for a cohesive and patient-focused strategy in healthcare delivery.
As reflected above, the medical model pays a significant amount of emphasis of how
knowledge and bonding between patients and care givers must be confined to providing
appropriate treatment for their ailments. This model does not effectively focus upon their
personal needs and strengths, rather just involve them in decision making, without analysis
of their wants (Kitson and Harvey, 2016).
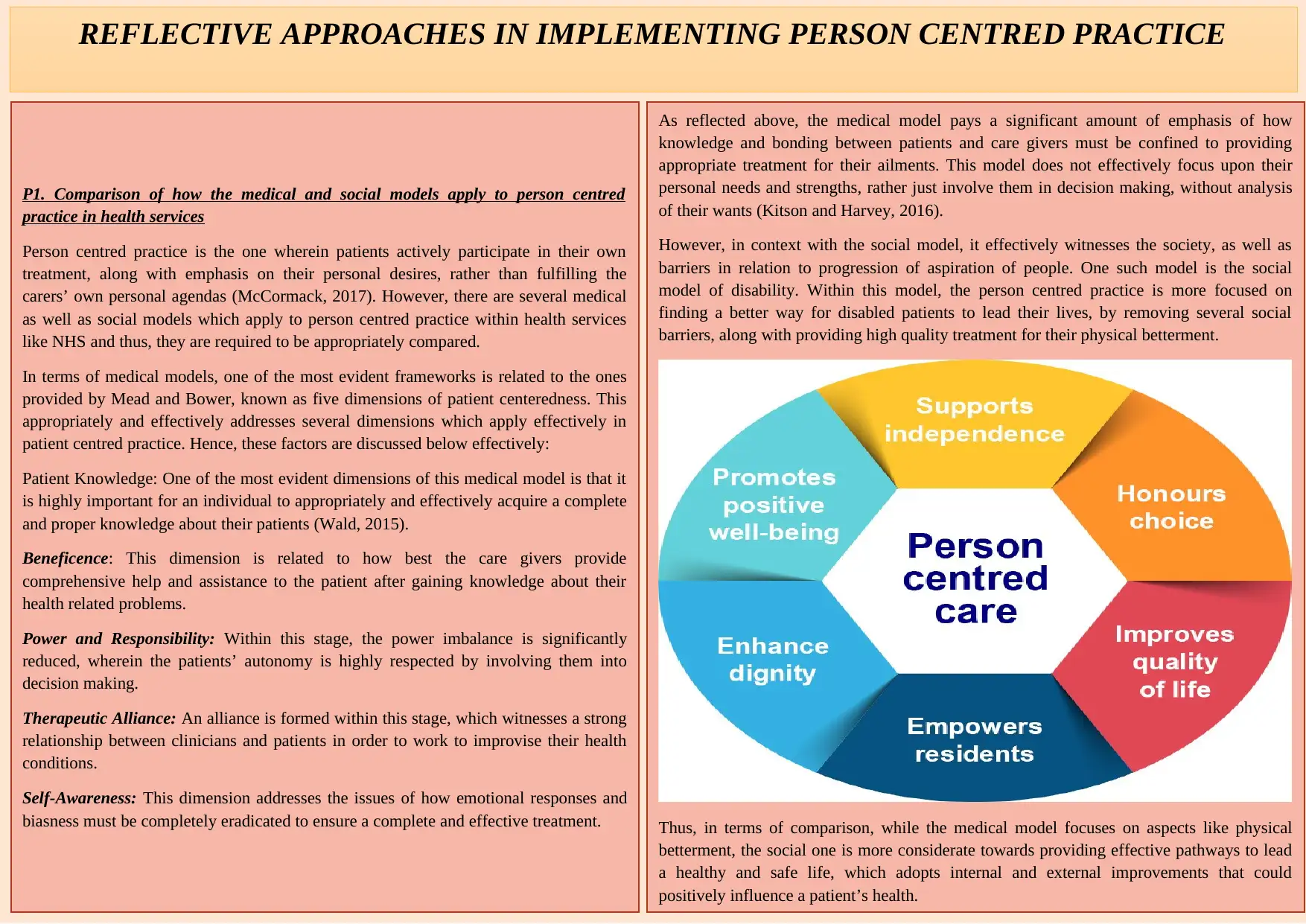
However, in context with the social model, it effectively witnesses the society, as well as
barriers in relation to progression of aspiration of people. One such model is the social
model of disability. Within this model, the person centred practice is more focused on
finding a better way for disabled patients to lead their lives, by removing several social
barriers, along with providing high quality treatment for their physical betterment.
Thus, in terms of comparison, while the medical model focuses on aspects like physical
betterment, the social one is more considerate towards providing effective pathways to lead
a healthy and safe life, which adopts internal and external improvements that could
positively influence a patient’s health.
P1. Comparison of how the medical and social models apply to person centred
practice in health services
Person centred practice is the one wherein patients actively participate in their own
treatment, along with emphasis on their personal desires, rather than fulfilling the
carers’ own personal agendas (McCormack, 2017). However, there are several medical
as well as social models which apply to person centred practice within health services
like NHS and thus, they are required to be appropriately compared.
In terms of medical models, one of the most evident frameworks is related to the ones
provided by Mead and Bower, known as five dimensions of patient centeredness. This
appropriately and effectively addresses several dimensions which apply effectively in
patient centred practice. Hence, these factors are discussed below effectively:
Patient Knowledge: One of the most evident dimensions of this medical model is that it
is highly important for an individual to appropriately and effectively acquire a complete
and proper knowledge about their patients (Wald, 2015).
Beneficence: This dimension is related to how best the care givers provide
comprehensive help and assistance to the patient after gaining knowledge about their
health related problems.
Power and Responsibility: Within this stage, the power imbalance is significantly
reduced, wherein the patients’ autonomy is highly respected by involving them into
decision making.
Therapeutic Alliance: An alliance is formed within this stage, which witnesses a strong
relationship between clinicians and patients in order to work to improvise their health
conditions.
Self-Awareness: This dimension addresses the issues of how emotional responses and
biasness must be completely eradicated to ensure a complete and effective treatment.
REFLECTIVE APPROACHES IN IMPLEMENTING PERSON CENTRED PRACTICE
knowledge and bonding between patients and care givers must be confined to providing
appropriate treatment for their ailments. This model does not effectively focus upon their
personal needs and strengths, rather just involve them in decision making, without analysis
of their wants (Kitson and Harvey, 2016).
However, in context with the social model, it effectively witnesses the society, as well as
barriers in relation to progression of aspiration of people. One such model is the social
model of disability. Within this model, the person centred practice is more focused on
finding a better way for disabled patients to lead their lives, by removing several social
barriers, along with providing high quality treatment for their physical betterment.
Thus, in terms of comparison, while the medical model focuses on aspects like physical
betterment, the social one is more considerate towards providing effective pathways to lead
a healthy and safe life, which adopts internal and external improvements that could
positively influence a patient’s health.
P1. Comparison of how the medical and social models apply to person centred
practice in health services
Person centred practice is the one wherein patients actively participate in their own
treatment, along with emphasis on their personal desires, rather than fulfilling the
carers’ own personal agendas (McCormack, 2017). However, there are several medical
as well as social models which apply to person centred practice within health services
like NHS and thus, they are required to be appropriately compared.
In terms of medical models, one of the most evident frameworks is related to the ones
provided by Mead and Bower, known as five dimensions of patient centeredness. This
appropriately and effectively addresses several dimensions which apply effectively in
patient centred practice. Hence, these factors are discussed below effectively:
Patient Knowledge: One of the most evident dimensions of this medical model is that it
is highly important for an individual to appropriately and effectively acquire a complete
and proper knowledge about their patients (Wald, 2015).
Beneficence: This dimension is related to how best the care givers provide
comprehensive help and assistance to the patient after gaining knowledge about their
health related problems.
Power and Responsibility: Within this stage, the power imbalance is significantly
reduced, wherein the patients’ autonomy is highly respected by involving them into
decision making.
Therapeutic Alliance: An alliance is formed within this stage, which witnesses a strong
relationship between clinicians and patients in order to work to improvise their health
conditions.
Self-Awareness: This dimension addresses the issues of how emotional responses and
biasness must be completely eradicated to ensure a complete and effective treatment.
REFLECTIVE APPROACHES IN IMPLEMENTING PERSON CENTRED PRACTICE
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
As a support worker, in community nurse with children, there have been several
challenges which have been faced by me, which are discussed below:
Challenging Behaviour: One of the major challenges I faced while providing person
centred care to patients has been their constantly challenging behaviour (Mudge, Kayes
and McPherson, 2015). This is because their wants and requirements sometimes
repeatedly change, which makes it quite difficult to support them or provide appropriate
care.
Conflicts: Another challenge which I faced was related to conflicts between values of
others and principles of good practice. Reason for such practice is that the values tend to
be quite dynamic, which sometimes gets challenging to align with principles of good
practice, hence, arising conflicts.
D1. Evaluation of how dilemmas experienced affect consistency in approach
It is highly necessary to ensure consistency within approach while appropriately and
effectively providing person centred care to patients. However, dilemmas tend to refrain
this consistency in care professionals (Cheng and et. al., 2016). In my case, while there
was evident impact of challenging behaviours on my consistency, my performance was
more affected by conflicts within values and principles. The reason for the same is that I
failed to appropriately interpret the changes in values, which broke my consistency in a
P2. Discussion of how to adopt a person centred approach
It is quite important for a care giver, particularly support workers to adopt person
centred approach when planning the delivery of care and support for individuals with
needs. However, there are several steps as well as considerations, which are required to
be appropriately assessed by care givers in order to adopt this practice effectively. All
these variables are presented as under:
Self-Awareness: Self-concept is one of the first stages which must be inculcated within
a professional practitioner in order to adopt person centred care. A prime consideration
which the carer must possess at this stage is the Duty of Care. These are ethical codes of
conduct which reflect adherence to standards of appropriate and reasonable practice.
Patient’s Values and Beliefs: This part of the process is related to effectively acquiring
knowledge related to the beliefs and values within patients. It helps the care givers in
appropriately support them and promote a healthy lifestyle.
Engagement: It is related to engagement of carers with patients, where the latter is
required to appropriately instil trust and transparency, along with appropriately
respecting the rights, choice and privacy of patients. Furthermore, the engagement does
is not confined to patients along, rather their families, friends and communities
associated with them are also included.
Shared Decision Making: This step is related to providing patients with equal
responsibility of taking their own decisions associated with their treatment. Moreover,
professionals are required to empower the patients through an appropriate recognition of
their own requirements for the treatment.
Empathy: One of the major aspects, this step is related to empathising the patient
through an active demonstration of respect, promotion of partnership, along with taking
appropriate feedbacks from the patient (Brooker and et. al., 2016).
Holistic Care: The last step of the process while planning delivery of care and
supporting individuals is to implement a holistic approach in context of enhancing the
overall care provided to patients. For this, the carer must adopt professional approaches
to care, which includes effective compassion, competence, appropriate channels of
communication, transparency and effective commitment.
M1. Reviewing of challenges with applying person centred care
While providing effective person centred care to patients, there are several challenges
which could be faced by a care giver within their organisational settings.
Gabrielsson, S., Sävenstedt, S. and Zingmark, K., 2015. Person‐centred care: clarifying the
concept in the context of inpatient psychiatry. Scandinavian journal of caring sciences.
29(3). pp.555-562.
Parker, J., 2017. Social work practice: Assessment, planning, intervention and review.
Learning Matters.
References
challenges which have been faced by me, which are discussed below:
Challenging Behaviour: One of the major challenges I faced while providing person
centred care to patients has been their constantly challenging behaviour (Mudge, Kayes
and McPherson, 2015). This is because their wants and requirements sometimes
repeatedly change, which makes it quite difficult to support them or provide appropriate
care.
Conflicts: Another challenge which I faced was related to conflicts between values of
others and principles of good practice. Reason for such practice is that the values tend to
be quite dynamic, which sometimes gets challenging to align with principles of good
practice, hence, arising conflicts.
D1. Evaluation of how dilemmas experienced affect consistency in approach
It is highly necessary to ensure consistency within approach while appropriately and
effectively providing person centred care to patients. However, dilemmas tend to refrain
this consistency in care professionals (Cheng and et. al., 2016). In my case, while there
was evident impact of challenging behaviours on my consistency, my performance was
more affected by conflicts within values and principles. The reason for the same is that I
failed to appropriately interpret the changes in values, which broke my consistency in a
P2. Discussion of how to adopt a person centred approach
It is quite important for a care giver, particularly support workers to adopt person
centred approach when planning the delivery of care and support for individuals with
needs. However, there are several steps as well as considerations, which are required to
be appropriately assessed by care givers in order to adopt this practice effectively. All
these variables are presented as under:
Self-Awareness: Self-concept is one of the first stages which must be inculcated within
a professional practitioner in order to adopt person centred care. A prime consideration
which the carer must possess at this stage is the Duty of Care. These are ethical codes of
conduct which reflect adherence to standards of appropriate and reasonable practice.
Patient’s Values and Beliefs: This part of the process is related to effectively acquiring
knowledge related to the beliefs and values within patients. It helps the care givers in
appropriately support them and promote a healthy lifestyle.
Engagement: It is related to engagement of carers with patients, where the latter is
required to appropriately instil trust and transparency, along with appropriately
respecting the rights, choice and privacy of patients. Furthermore, the engagement does
is not confined to patients along, rather their families, friends and communities
associated with them are also included.
Shared Decision Making: This step is related to providing patients with equal
responsibility of taking their own decisions associated with their treatment. Moreover,
professionals are required to empower the patients through an appropriate recognition of
their own requirements for the treatment.
Empathy: One of the major aspects, this step is related to empathising the patient
through an active demonstration of respect, promotion of partnership, along with taking
appropriate feedbacks from the patient (Brooker and et. al., 2016).
Holistic Care: The last step of the process while planning delivery of care and
supporting individuals is to implement a holistic approach in context of enhancing the
overall care provided to patients. For this, the carer must adopt professional approaches
to care, which includes effective compassion, competence, appropriate channels of
communication, transparency and effective commitment.
M1. Reviewing of challenges with applying person centred care
While providing effective person centred care to patients, there are several challenges
which could be faced by a care giver within their organisational settings.
Gabrielsson, S., Sävenstedt, S. and Zingmark, K., 2015. Person‐centred care: clarifying the
concept in the context of inpatient psychiatry. Scandinavian journal of caring sciences.
29(3). pp.555-562.
Parker, J., 2017. Social work practice: Assessment, planning, intervention and review.
Learning Matters.
References
1 out of 2
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





