Rehabilitation and Community Care: Nursing Care Plan (NSG 3101)
VerifiedAdded on 2022/08/13
|14
|1003
|15
Presentation
AI Summary
This presentation focuses on a nursing care plan for a patient in a rehabilitation setting, likely addressing the needs of a patient with Traumatic Brain Injury (TBI), including challenges like dysphagia and dysphasia. The care plan encompasses various aspects of patient care, including mobility, feeding, and speech. The assignment involves a presentation and a written component, detailing assessment, planning, implementation, and evaluation of nursing interventions. The case study involves a 48-year-old male, Paul, who experienced a TBI. The presentation likely covers aspects of patient assessment, goal setting, intervention strategies, and evaluation of outcomes, considering the patient's physical and cognitive impairments, as well as the involvement of family members in the care process. The provided references support the evidence-based approach to rehabilitation, covering topics such as dysphagia rehabilitation, assessment tools, and the impact of chronic conditions on patient outcomes.
NSG 3101 –
REHABILITATION AND
COMMUNITY CARE
ASSIGNMENT 2 NURSING
CARE PLAN PRESENTATION
Name of the Student
Name of the University
REHABILITATION AND
COMMUNITY CARE
ASSIGNMENT 2 NURSING
CARE PLAN PRESENTATION
Name of the Student
Name of the University
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
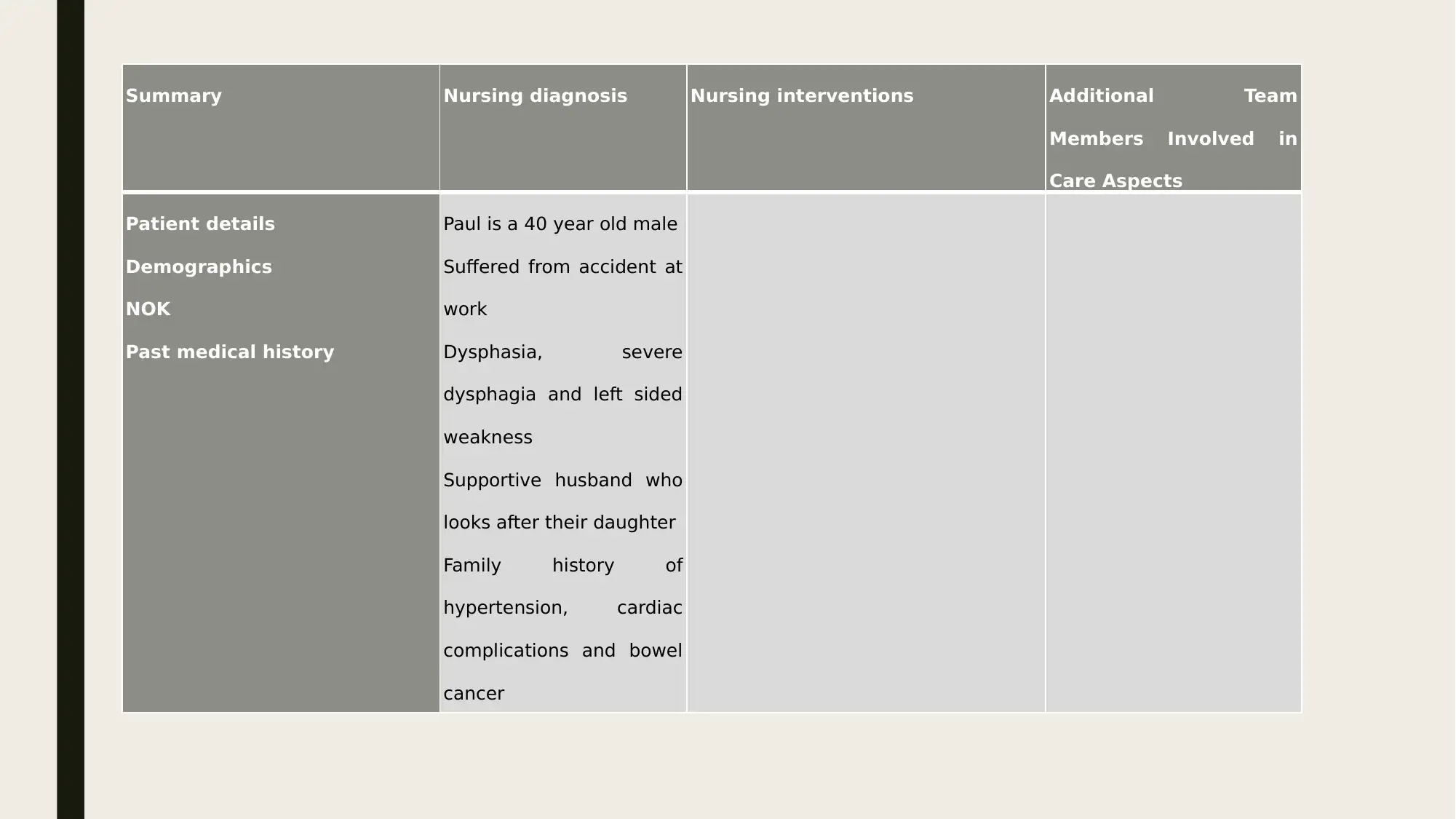
Patient details
Demographics
NOK
Past medical history
Paul is a 40 year old male
Suffered from accident at
work
Dysphasia, severe
dysphagia and left sided
weakness
Supportive husband who
looks after their daughter
Family history of
hypertension, cardiac
complications and bowel
cancer
Members Involved in
Care Aspects
Patient details
Demographics
NOK
Past medical history
Paul is a 40 year old male
Suffered from accident at
work
Dysphasia, severe
dysphagia and left sided
weakness
Supportive husband who
looks after their daughter
Family history of
hypertension, cardiac
complications and bowel
cancer
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
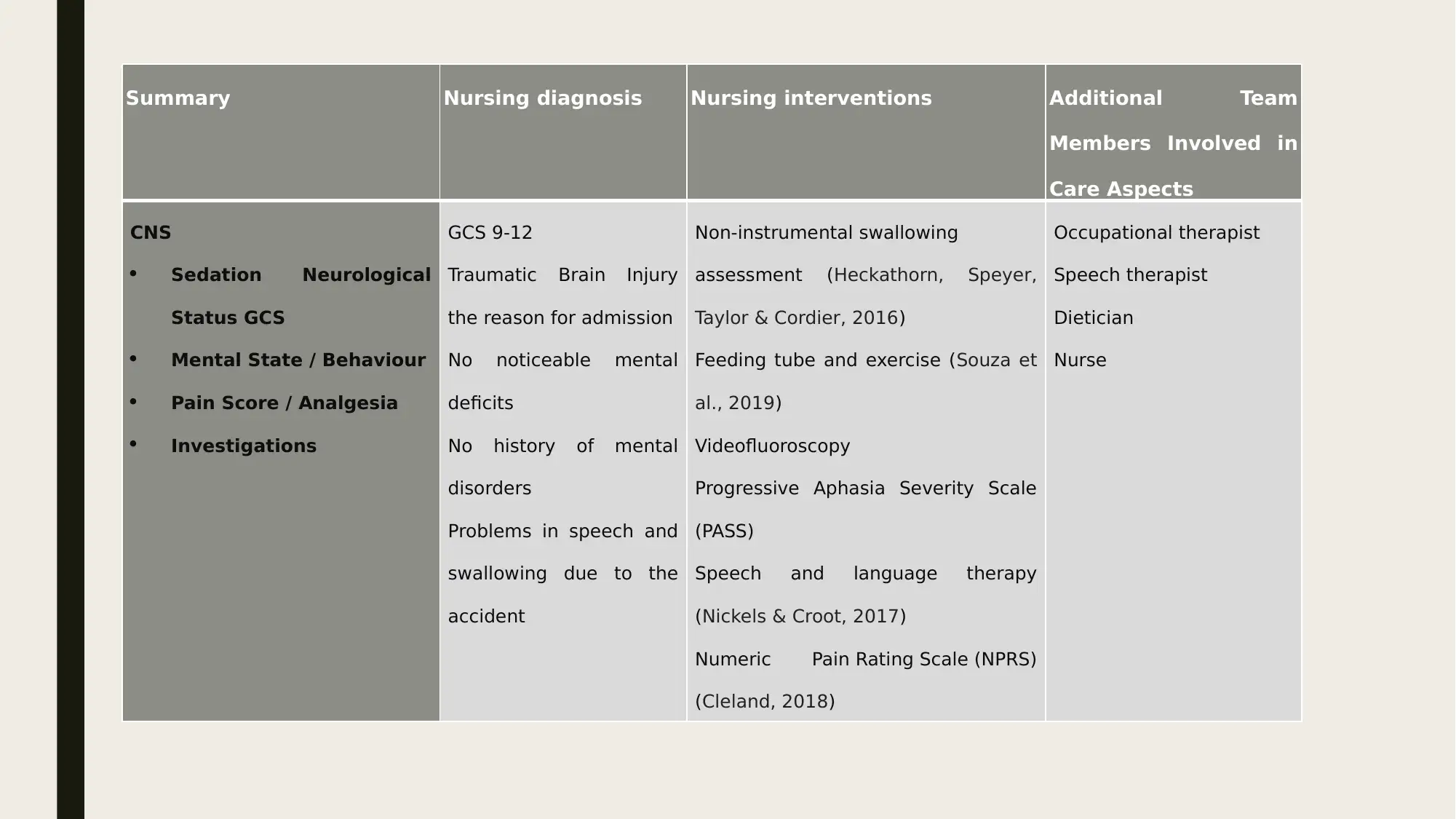
CNS
Sedation Neurological
Status GCS
Mental State / Behaviour
Pain Score / Analgesia
Investigations
GCS 9-12
Traumatic Brain Injury
the reason for admission
No noticeable mental
deficits
No history of mental
disorders
Problems in speech and
swallowing due to the
accident
Non-instrumental swallowing
assessment (Heckathorn, Speyer,
Taylor & Cordier, 2016)
Feeding tube and exercise (Souza et
al., 2019)
Videofluoroscopy
Progressive Aphasia Severity Scale
(PASS)
Speech and language therapy
(Nickels & Croot, 2017)
Numeric Pain Rating Scale (NPRS)
(Cleland, 2018)
Occupational therapist
Speech therapist
Dietician
Nurse
Members Involved in
Care Aspects
CNS
Sedation Neurological
Status GCS
Mental State / Behaviour
Pain Score / Analgesia
Investigations
GCS 9-12
Traumatic Brain Injury
the reason for admission
No noticeable mental
deficits
No history of mental
disorders
Problems in speech and
swallowing due to the
accident
Non-instrumental swallowing
assessment (Heckathorn, Speyer,
Taylor & Cordier, 2016)
Feeding tube and exercise (Souza et
al., 2019)
Videofluoroscopy
Progressive Aphasia Severity Scale
(PASS)
Speech and language therapy
(Nickels & Croot, 2017)
Numeric Pain Rating Scale (NPRS)
(Cleland, 2018)
Occupational therapist
Speech therapist
Dietician
Nurse
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
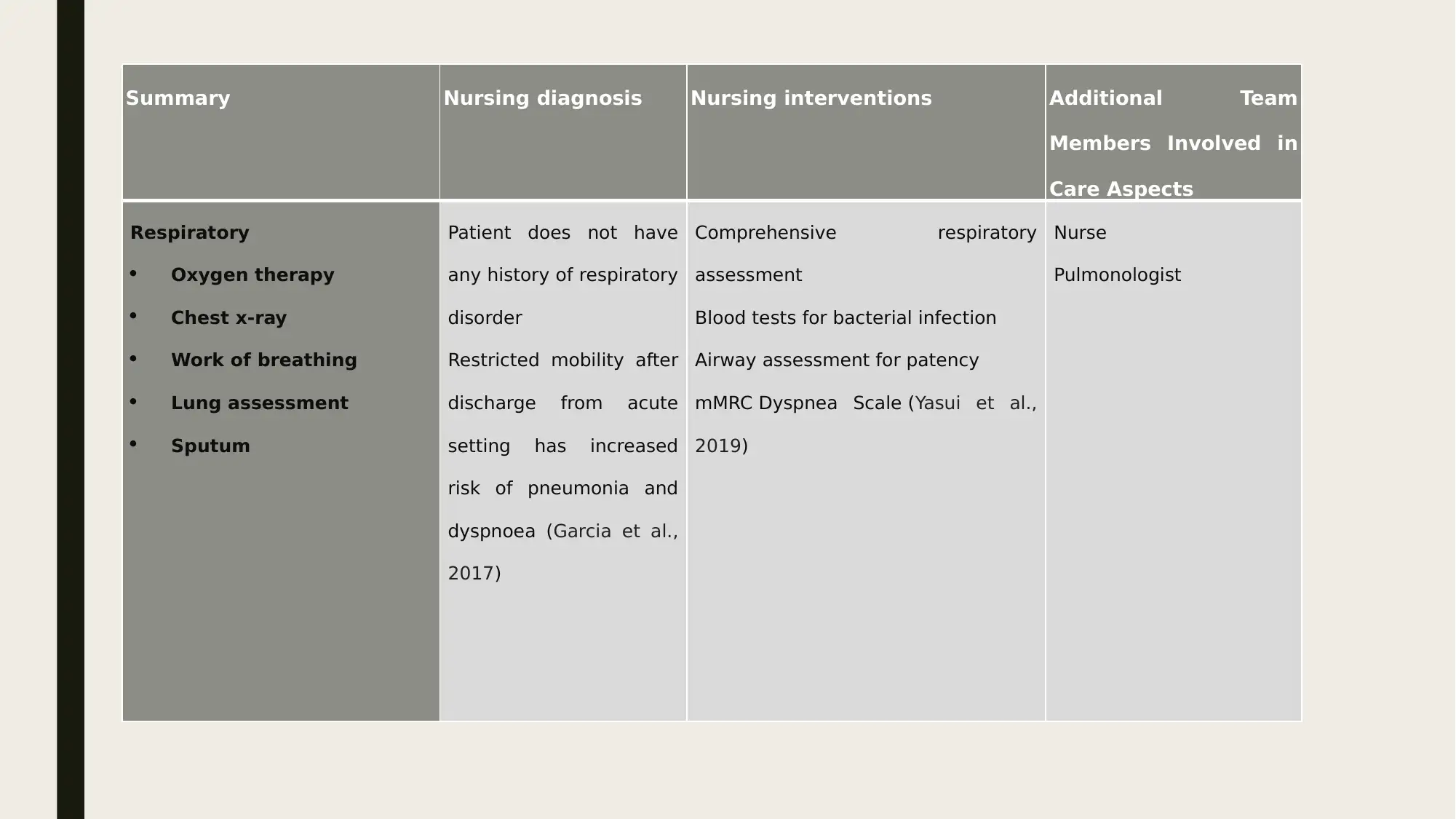
Respiratory
Oxygen therapy
Chest x-ray
Work of breathing
Lung assessment
Sputum
Patient does not have
any history of respiratory
disorder
Restricted mobility after
discharge from acute
setting has increased
risk of pneumonia and
dyspnoea (Garcia et al.,
2017)
Comprehensive respiratory
assessment
Blood tests for bacterial infection
Airway assessment for patency
mMRC Dyspnea Scale (Yasui et al.,
2019)
Nurse
Pulmonologist
Members Involved in
Care Aspects
Respiratory
Oxygen therapy
Chest x-ray
Work of breathing
Lung assessment
Sputum
Patient does not have
any history of respiratory
disorder
Restricted mobility after
discharge from acute
setting has increased
risk of pneumonia and
dyspnoea (Garcia et al.,
2017)
Comprehensive respiratory
assessment
Blood tests for bacterial infection
Airway assessment for patency
mMRC Dyspnea Scale (Yasui et al.,
2019)
Nurse
Pulmonologist
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
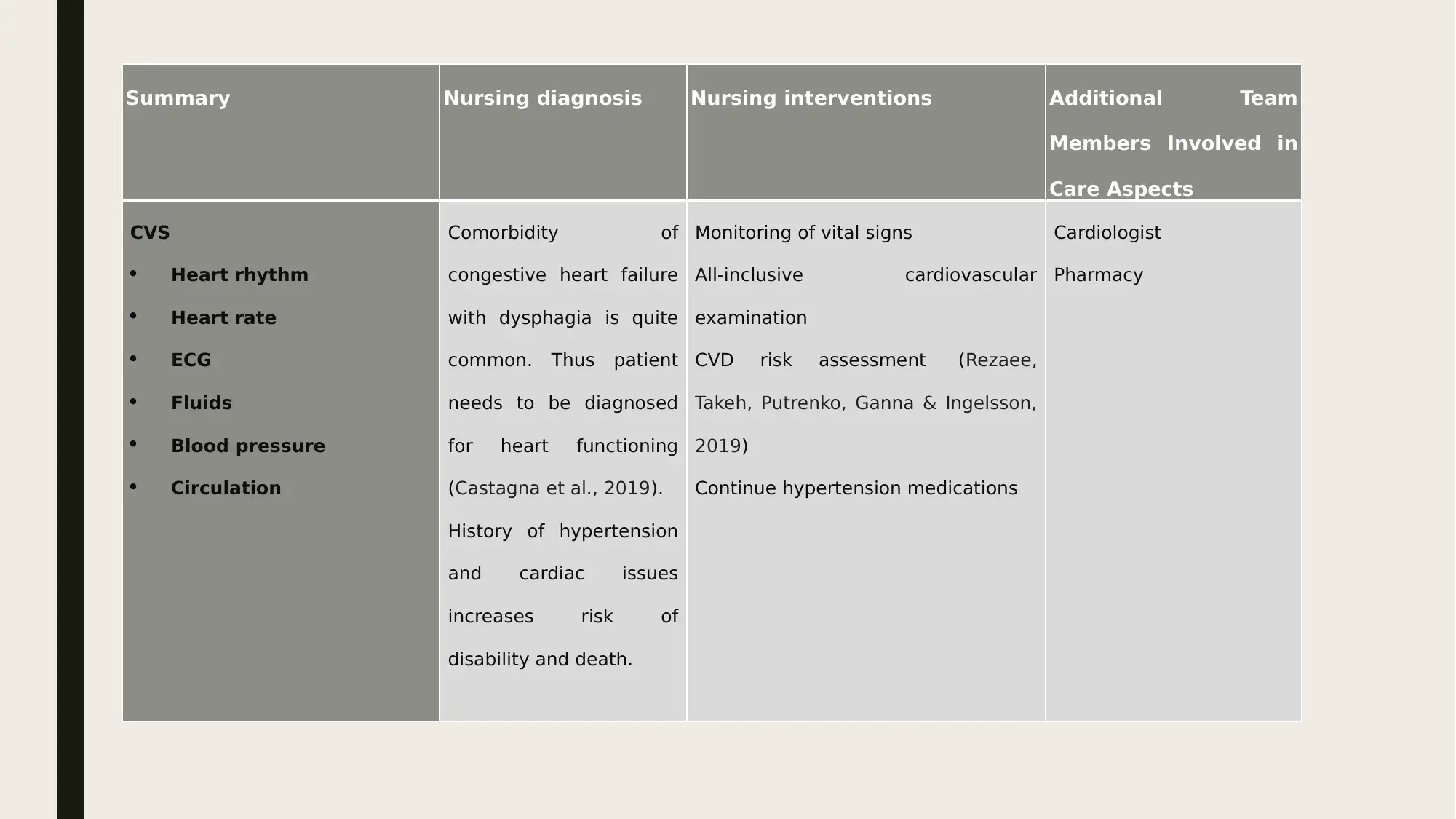
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
CVS
Heart rhythm
Heart rate
ECG
Fluids
Blood pressure
Circulation
Comorbidity of
congestive heart failure
with dysphagia is quite
common. Thus patient
needs to be diagnosed
for heart functioning
(Castagna et al., 2019).
History of hypertension
and cardiac issues
increases risk of
disability and death.
Monitoring of vital signs
All-inclusive cardiovascular
examination
CVD risk assessment (Rezaee,
Takeh, Putrenko, Ganna & Ingelsson,
2019)
Continue hypertension medications
Cardiologist
Pharmacy
Members Involved in
Care Aspects
CVS
Heart rhythm
Heart rate
ECG
Fluids
Blood pressure
Circulation
Comorbidity of
congestive heart failure
with dysphagia is quite
common. Thus patient
needs to be diagnosed
for heart functioning
(Castagna et al., 2019).
History of hypertension
and cardiac issues
increases risk of
disability and death.
Monitoring of vital signs
All-inclusive cardiovascular
examination
CVD risk assessment (Rezaee,
Takeh, Putrenko, Ganna & Ingelsson,
2019)
Continue hypertension medications
Cardiologist
Pharmacy
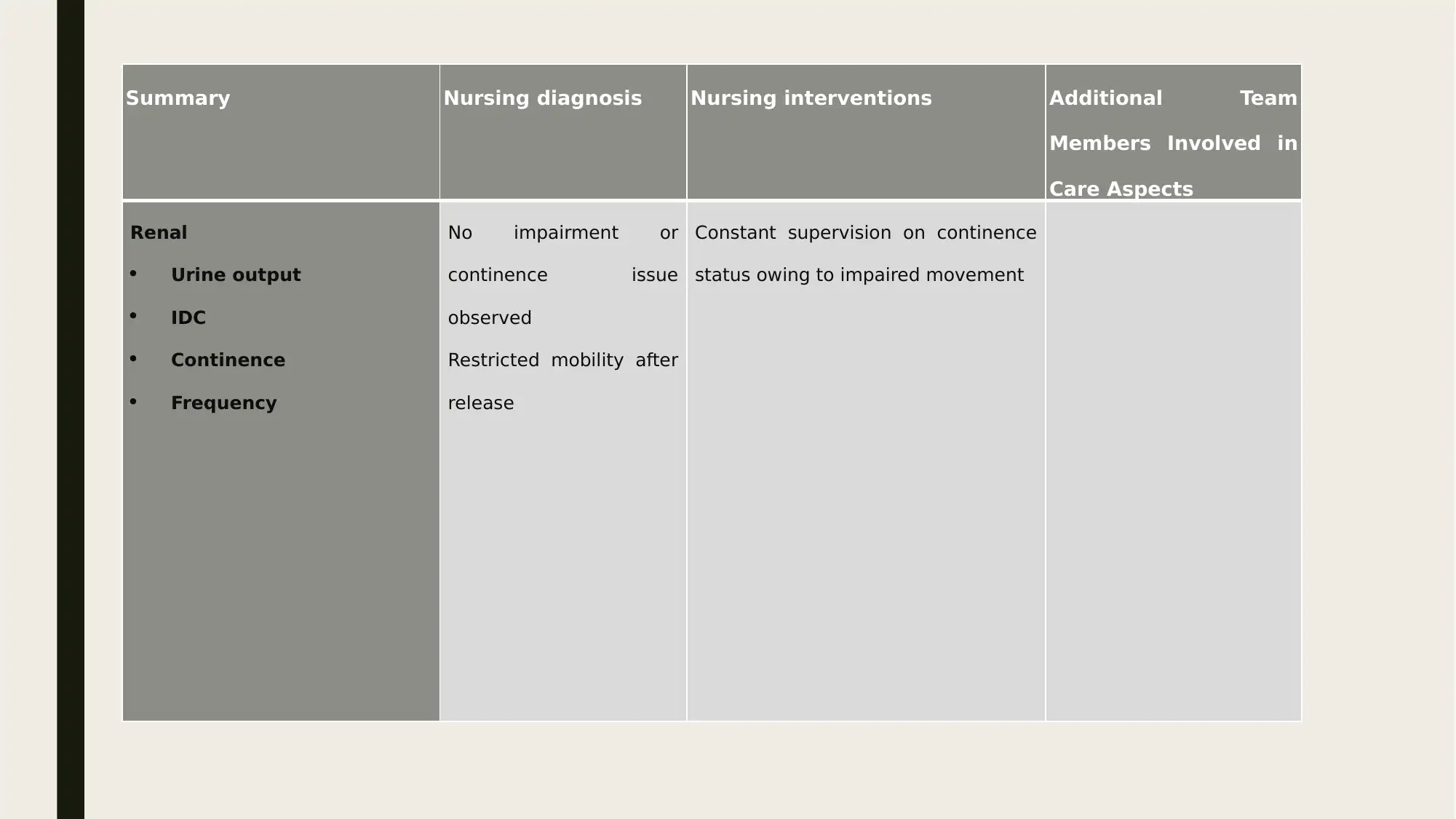
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
Renal
Urine output
IDC
Continence
Frequency
No impairment or
continence issue
observed
Restricted mobility after
release
Constant supervision on continence
status owing to impaired movement
Members Involved in
Care Aspects
Renal
Urine output
IDC
Continence
Frequency
No impairment or
continence issue
observed
Restricted mobility after
release
Constant supervision on continence
status owing to impaired movement
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
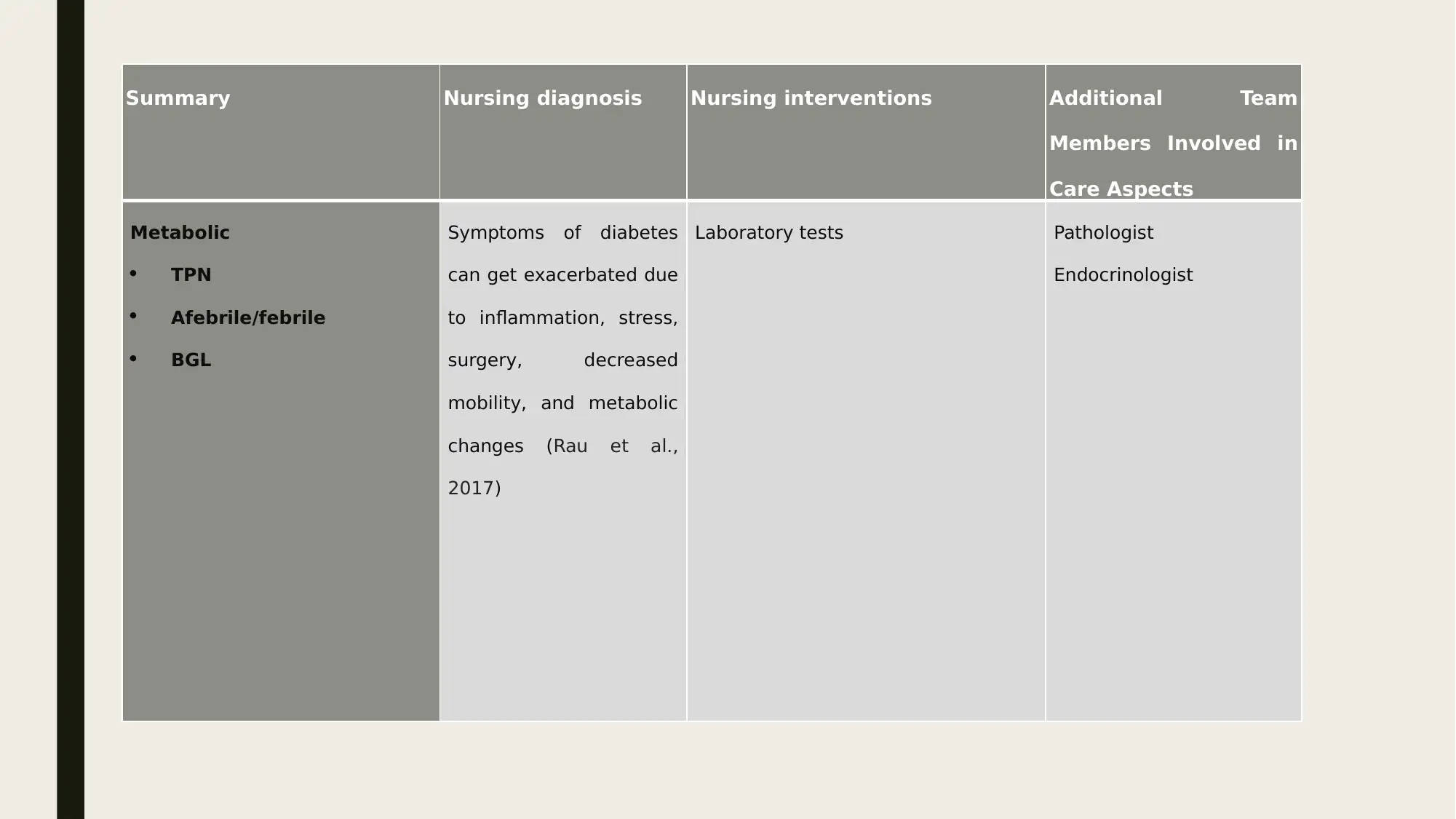
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
Metabolic
TPN
Afebrile/febrile
BGL
Symptoms of diabetes
can get exacerbated due
to inflammation, stress,
surgery, decreased
mobility, and metabolic
changes (Rau et al.,
2017)
Laboratory tests Pathologist
Endocrinologist
Members Involved in
Care Aspects
Metabolic
TPN
Afebrile/febrile
BGL
Symptoms of diabetes
can get exacerbated due
to inflammation, stress,
surgery, decreased
mobility, and metabolic
changes (Rau et al.,
2017)
Laboratory tests Pathologist
Endocrinologist
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
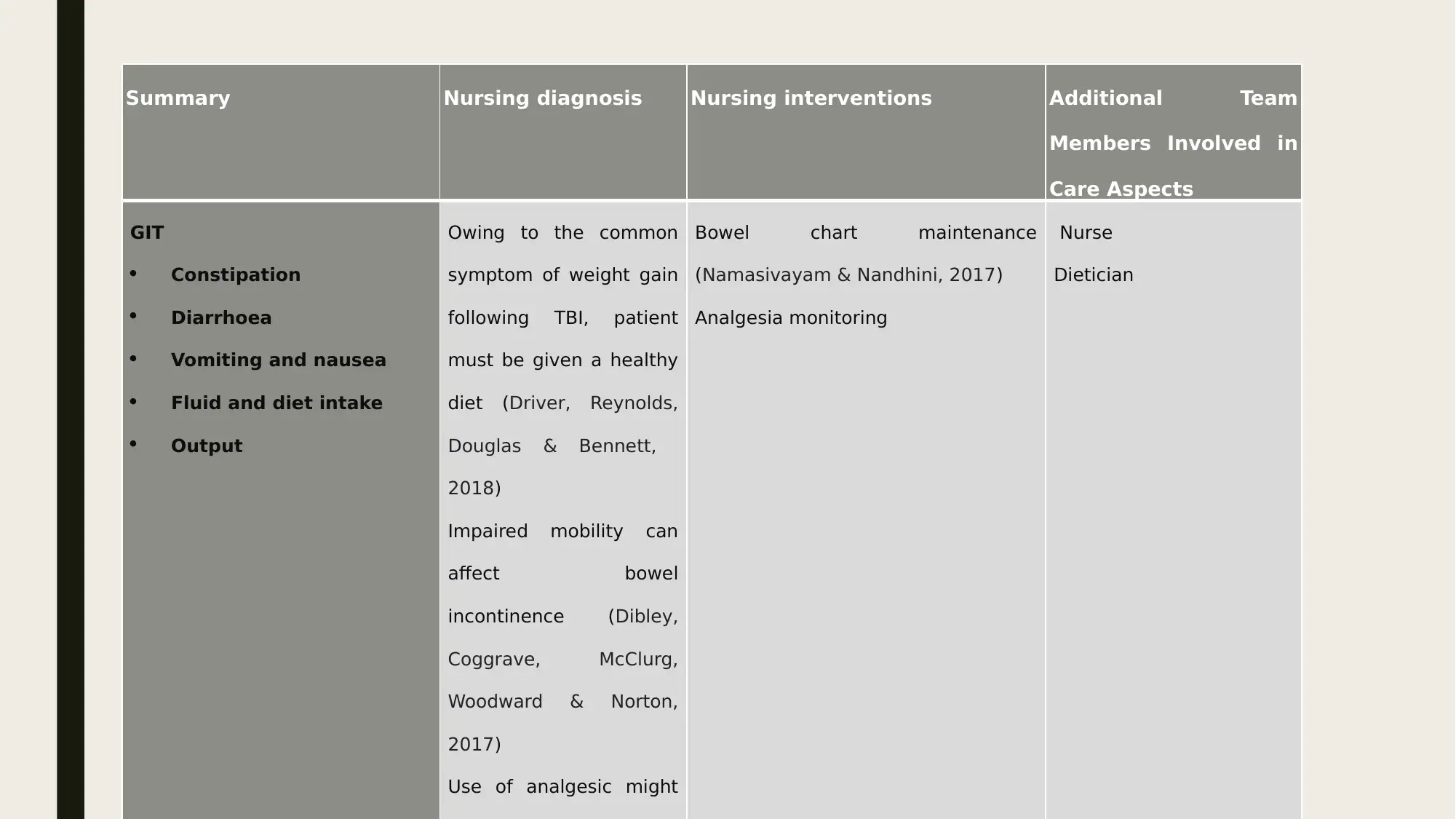
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
GIT
Constipation
Diarrhoea
Vomiting and nausea
Fluid and diet intake
Output
Owing to the common
symptom of weight gain
following TBI, patient
must be given a healthy
diet (Driver, Reynolds,
Douglas & Bennett,
2018)
Impaired mobility can
affect bowel
incontinence (Dibley,
Coggrave, McClurg,
Woodward & Norton,
2017)
Use of analgesic might
Bowel chart maintenance
(Namasivayam & Nandhini, 2017)
Analgesia monitoring
Nurse
Dietician
Members Involved in
Care Aspects
GIT
Constipation
Diarrhoea
Vomiting and nausea
Fluid and diet intake
Output
Owing to the common
symptom of weight gain
following TBI, patient
must be given a healthy
diet (Driver, Reynolds,
Douglas & Bennett,
2018)
Impaired mobility can
affect bowel
incontinence (Dibley,
Coggrave, McClurg,
Woodward & Norton,
2017)
Use of analgesic might
Bowel chart maintenance
(Namasivayam & Nandhini, 2017)
Analgesia monitoring
Nurse
Dietician
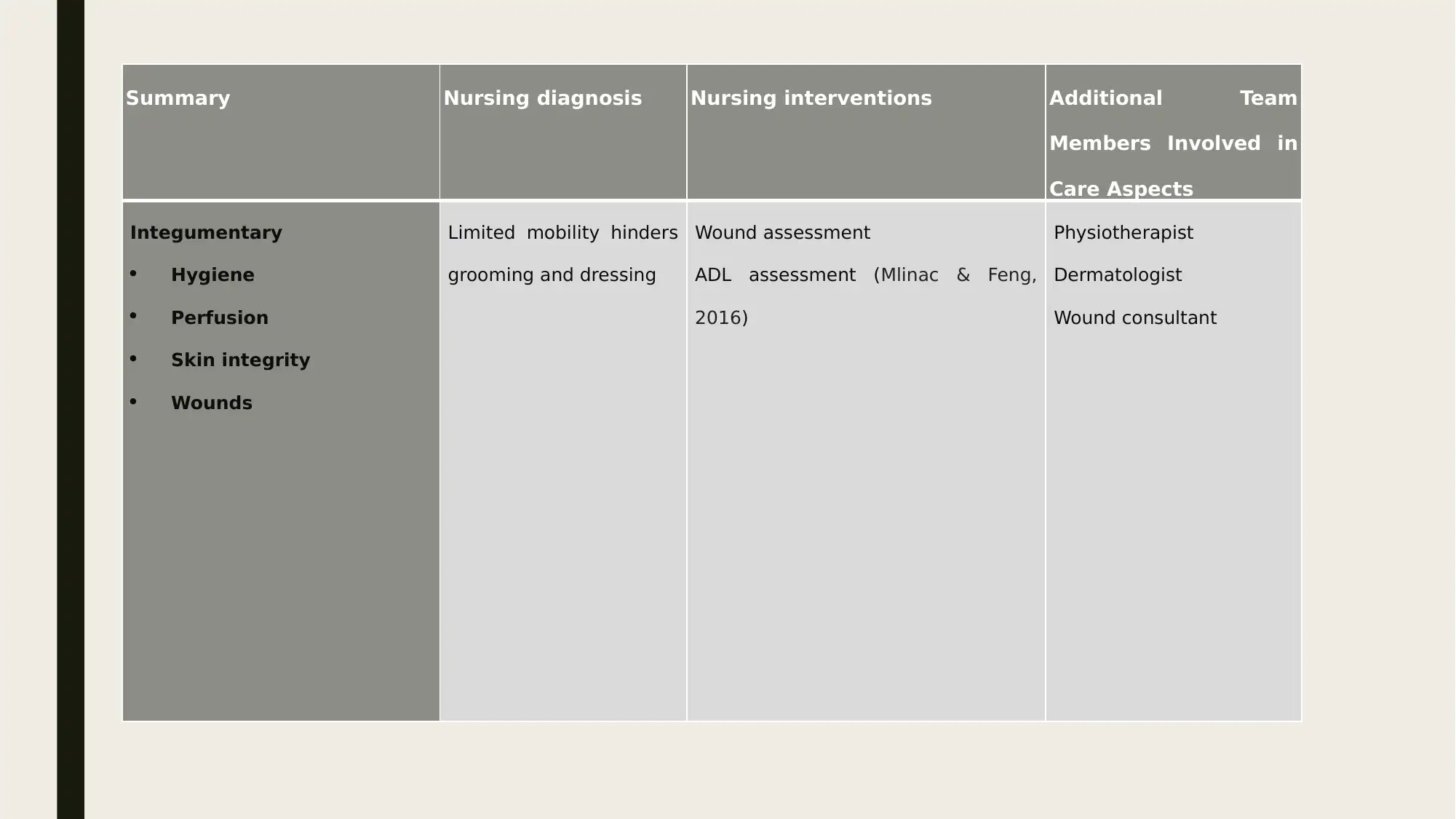
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
Integumentary
Hygiene
Perfusion
Skin integrity
Wounds
Limited mobility hinders
grooming and dressing
Wound assessment
ADL assessment (Mlinac & Feng,
2016)
Physiotherapist
Dermatologist
Wound consultant
Members Involved in
Care Aspects
Integumentary
Hygiene
Perfusion
Skin integrity
Wounds
Limited mobility hinders
grooming and dressing
Wound assessment
ADL assessment (Mlinac & Feng,
2016)
Physiotherapist
Dermatologist
Wound consultant
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
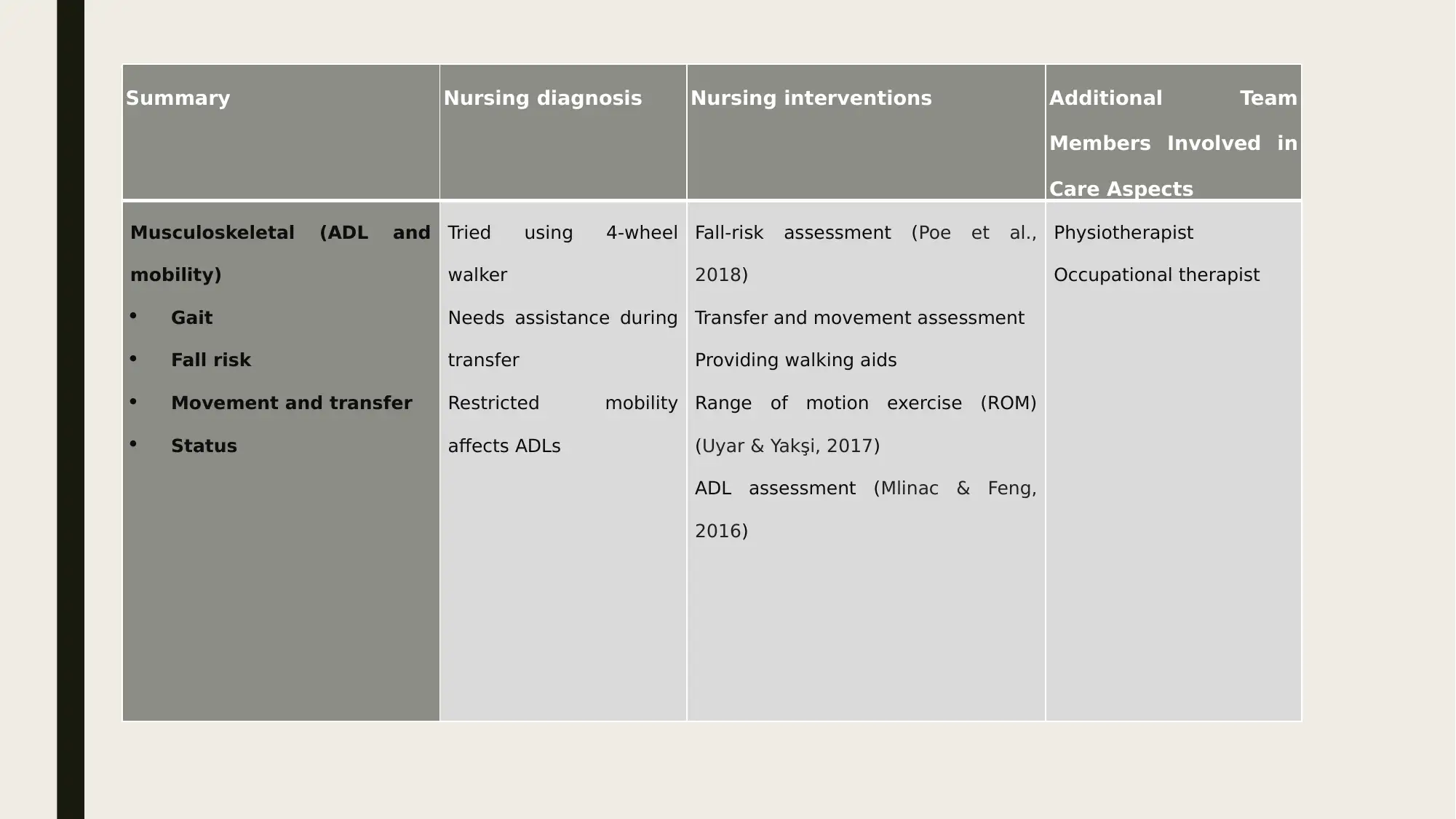
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
Musculoskeletal (ADL and
mobility)
Gait
Fall risk
Movement and transfer
Status
Tried using 4-wheel
walker
Needs assistance during
transfer
Restricted mobility
affects ADLs
Fall-risk assessment (Poe et al.,
2018)
Transfer and movement assessment
Providing walking aids
Range of motion exercise (ROM)
(Uyar & Yakşi, 2017)
ADL assessment (Mlinac & Feng,
2016)
Physiotherapist
Occupational therapist
Members Involved in
Care Aspects
Musculoskeletal (ADL and
mobility)
Gait
Fall risk
Movement and transfer
Status
Tried using 4-wheel
walker
Needs assistance during
transfer
Restricted mobility
affects ADLs
Fall-risk assessment (Poe et al.,
2018)
Transfer and movement assessment
Providing walking aids
Range of motion exercise (ROM)
(Uyar & Yakşi, 2017)
ADL assessment (Mlinac & Feng,
2016)
Physiotherapist
Occupational therapist
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
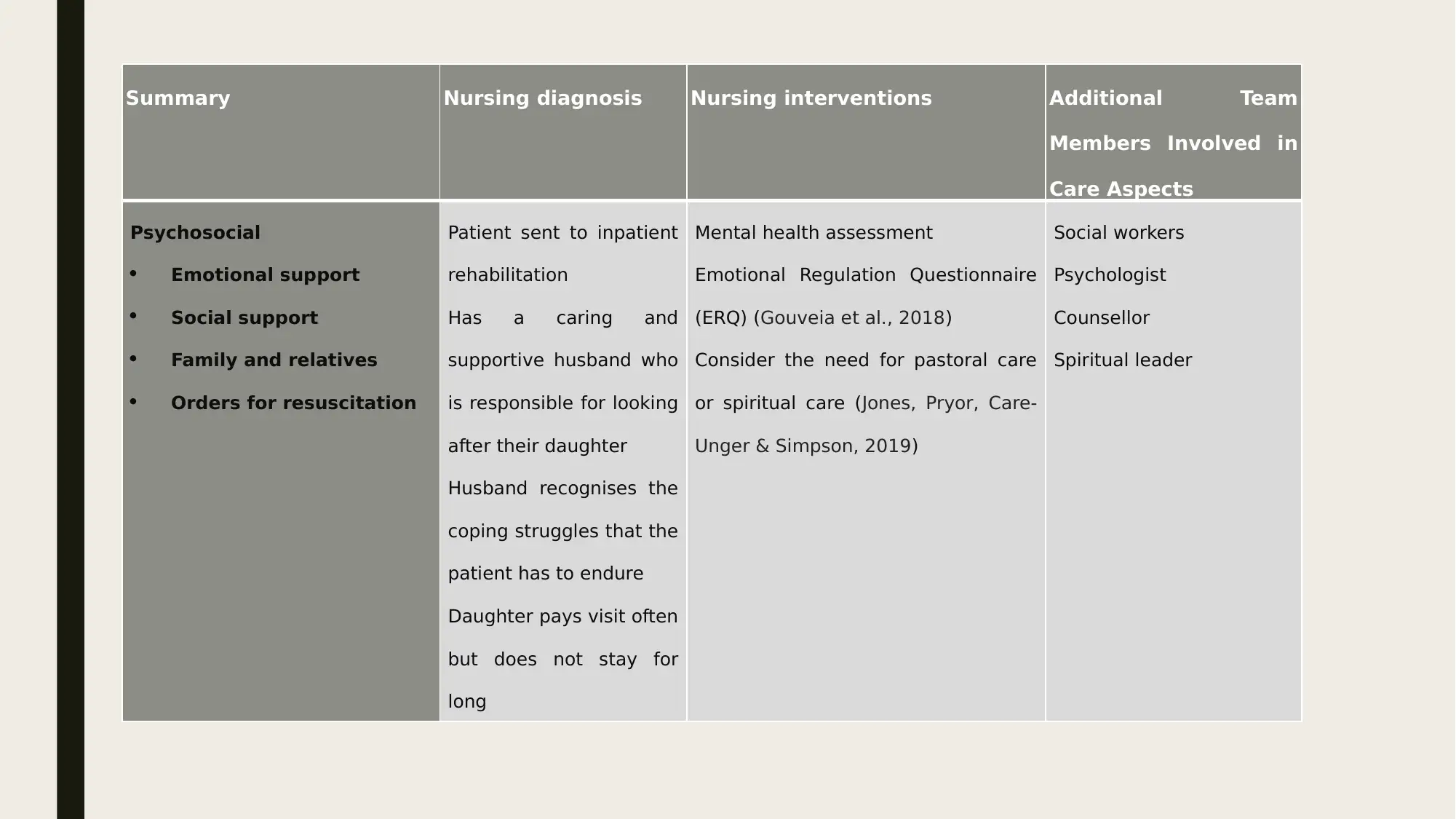
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
Psychosocial
Emotional support
Social support
Family and relatives
Orders for resuscitation
Patient sent to inpatient
rehabilitation
Has a caring and
supportive husband who
is responsible for looking
after their daughter
Husband recognises the
coping struggles that the
patient has to endure
Daughter pays visit often
but does not stay for
long
Mental health assessment
Emotional Regulation Questionnaire
(ERQ) (Gouveia et al., 2018)
Consider the need for pastoral care
or spiritual care (Jones, Pryor, Care-
Unger & Simpson, 2019)
Social workers
Psychologist
Counsellor
Spiritual leader
Members Involved in
Care Aspects
Psychosocial
Emotional support
Social support
Family and relatives
Orders for resuscitation
Patient sent to inpatient
rehabilitation
Has a caring and
supportive husband who
is responsible for looking
after their daughter
Husband recognises the
coping struggles that the
patient has to endure
Daughter pays visit often
but does not stay for
long
Mental health assessment
Emotional Regulation Questionnaire
(ERQ) (Gouveia et al., 2018)
Consider the need for pastoral care
or spiritual care (Jones, Pryor, Care-
Unger & Simpson, 2019)
Social workers
Psychologist
Counsellor
Spiritual leader
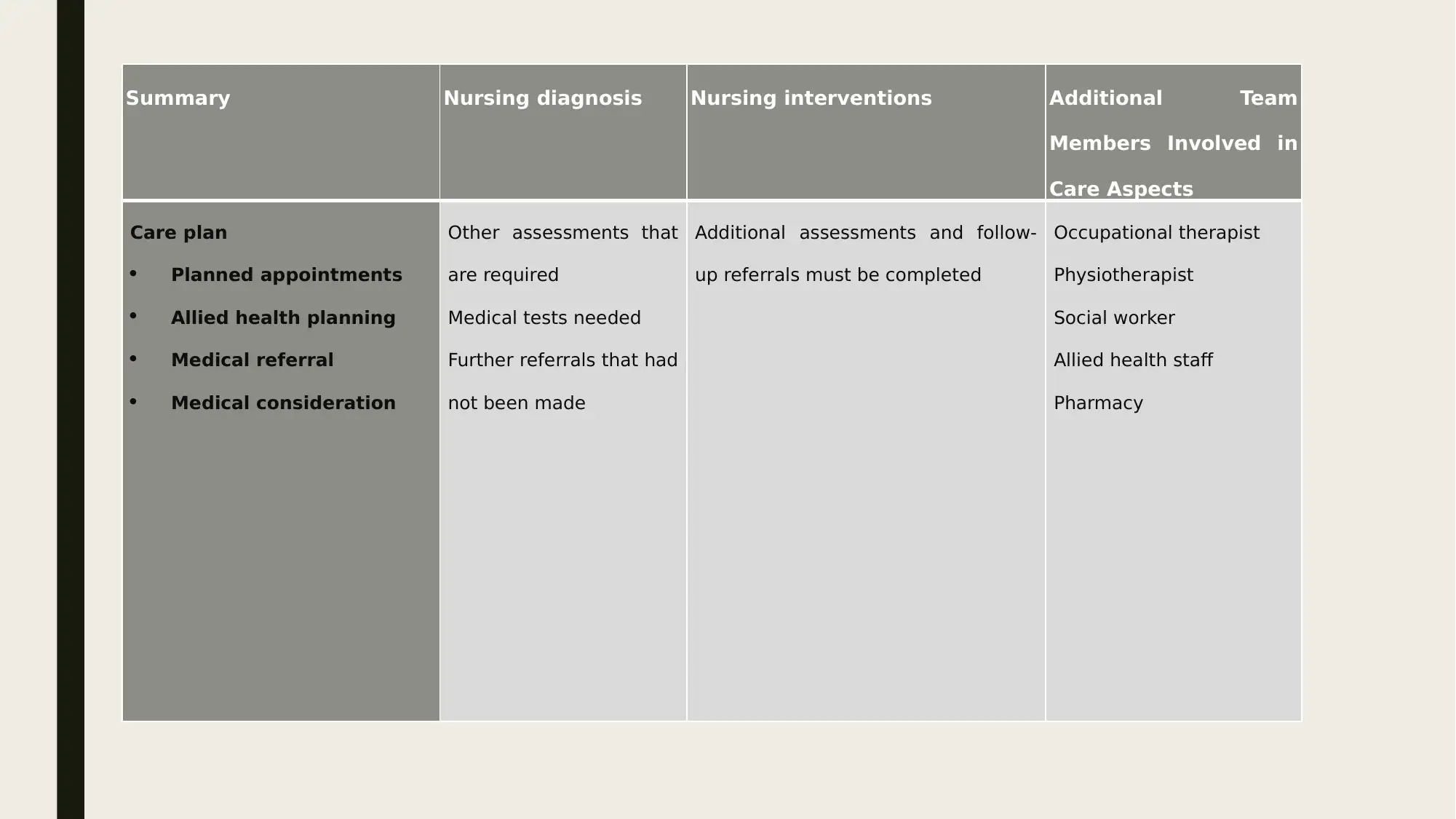
Summary Nursing diagnosis Nursing interventions Additional Team
Members Involved in
Care Aspects
Care plan
Planned appointments
Allied health planning
Medical referral
Medical consideration
Other assessments that
are required
Medical tests needed
Further referrals that had
not been made
Additional assessments and follow-
up referrals must be completed
Occupational therapist
Physiotherapist
Social worker
Allied health staff
Pharmacy
Members Involved in
Care Aspects
Care plan
Planned appointments
Allied health planning
Medical referral
Medical consideration
Other assessments that
are required
Medical tests needed
Further referrals that had
not been made
Additional assessments and follow-
up referrals must be completed
Occupational therapist
Physiotherapist
Social worker
Allied health staff
Pharmacy
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



