Chronic Renal Failure: A Case Study of Melanie Johnson (NURBN2016)
VerifiedAdded on 2022/12/28
|13
|3239
|39
Report
AI Summary
This report presents a comprehensive analysis of a chronic renal failure case study, focusing on a 55-year-old patient named Melanie Johnson. The case study details her symptoms (tiredness, nausea, pruritus), diagnosis of chronic kidney failure, and relevant blood results, including high blood pressure, elevated creatinine, and abnormal GFR. The report delves into the pathophysiology of the condition, exploring causes and complications like uremia, hyperkalemia, and heart failure. It also examines treatment options, specifically hemodialysis, and discusses suitable medications such as Fosrenol and benazepril, along with crucial nursing considerations for each drug. Additionally, the report addresses the patient's low GFR and hemoglobin levels, and highlights the importance of the teach-back method for patient education on fluid restriction and disease management. The report also differentiates between acute and chronic kidney failure, summarizing the key aspects of the case study.

Running head: RENAL FAILURE
RENAL FAILURE
Name of the student:
Name of the university:
Author note
RENAL FAILURE
Name of the student:
Name of the university:
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
RENAL FAILURE
Question 1.1:
The kidneys are defined as bean-shaped organs originate from vertebrates. They are
situated in the retroperitoneal space on the left and right side. The kidneys are 11 centimeters
(4.3 in) in length in adults. They are covered by fibrous connective tissue called renal capsule
(innermost layer) and have two layers of fat which can cushion them and the outermost layer is
renal fascia (Chalmers, 2019). The internal region is separated into three parts such as renal
cortex, medulla and renal pelvis. The nephron is masses of tiny tubules located in the medulla
and receives fluid from the blood vessels situated in the cortex. The erythropoietin is produced
by cortex (Gosling et al., 2016). The bowman capsule is located at the end of nephron of the
cortex which acts as a blood filter. The renal pelvis contains helium, in the concave site where
renal artery, nerves, and vein are enters and ureter leaves. Renal arteries are branched into
abdominal aorta and supply kidney with blood (Chalmers, 2019). The kidney receives blood
from renal arteries and renal veins eliminate blood. It is attached to a ureter that excreted urine to
the bladder which further excrete urines.
Question 1.2:
The case study represents the renal failure of Melanie johnson, a 55 years old lady who
was the mother of 5 kids and lives in a rural Victorian town. Recently she has experienced
increasing tiredness, nausea, and general pruritus. After seeking the help of General practitioner,
she was diagnosed with chronic kidney failure.
Liyanage et al. (2015), define chronic renal failure as a irreversible loss of renal function over
the years which gradually decrease glomerular filtration rate as well creatine level which will
RENAL FAILURE
Question 1.1:
The kidneys are defined as bean-shaped organs originate from vertebrates. They are
situated in the retroperitoneal space on the left and right side. The kidneys are 11 centimeters
(4.3 in) in length in adults. They are covered by fibrous connective tissue called renal capsule
(innermost layer) and have two layers of fat which can cushion them and the outermost layer is
renal fascia (Chalmers, 2019). The internal region is separated into three parts such as renal
cortex, medulla and renal pelvis. The nephron is masses of tiny tubules located in the medulla
and receives fluid from the blood vessels situated in the cortex. The erythropoietin is produced
by cortex (Gosling et al., 2016). The bowman capsule is located at the end of nephron of the
cortex which acts as a blood filter. The renal pelvis contains helium, in the concave site where
renal artery, nerves, and vein are enters and ureter leaves. Renal arteries are branched into
abdominal aorta and supply kidney with blood (Chalmers, 2019). The kidney receives blood
from renal arteries and renal veins eliminate blood. It is attached to a ureter that excreted urine to
the bladder which further excrete urines.
Question 1.2:
The case study represents the renal failure of Melanie johnson, a 55 years old lady who
was the mother of 5 kids and lives in a rural Victorian town. Recently she has experienced
increasing tiredness, nausea, and general pruritus. After seeking the help of General practitioner,
she was diagnosed with chronic kidney failure.
Liyanage et al. (2015), define chronic renal failure as a irreversible loss of renal function over
the years which gradually decrease glomerular filtration rate as well creatine level which will
2
RENAL FAILURE
result in end-stage renal disease. The patient was diagnosed with high blood pressure (190/ 100)
whereas the blood pressure of a healthy individual is 120/80, highlighting is one of the prime
cause of kidney failure. Kidney helps to filter the waste product and extra fluid of the blood
through blood vessels (Hill et al., 2016). However, hypertension cause arteries of the kidneys to
narrow and damage. The damage arteries are not able to deliver enough blood to the kidney
tissues. The patient had palpitation for five years which can a risk of heart condition since
palpitation has resulted in the abnormal sinus rhythm ( changes in the cardiac rate) and heart
failure to the pump the adequate blood which further can induce pressure in the main vein
connected with kidney ( reduced oxygen-rich blood supply) (Xie et al., 2017). Consequently,
renal function declines due to high blood pressure which further reduced glomerular filtration
rate as observed in this case study. The patient had GFR 10ml/min/1.73m2 whereas, for women,
the normal range is 90 to 120mL/min/1.73m2 (Webster et al., 2015). On the other hand, impaired
kidney function is signified by an elevated serum creatinine level since the functional kidney can
clear creatinine from the blood. In this current context, the serum creatinine level was 90 umol/L
whereas, in healthy individuals, the normal range is 45 to 90 mmol/l. when kidney function is
impaired, the kidney failed to eliminate urea from the blood in the form of urine which resulted
in a high level of urea concentration as observed in this case study (Webster et al., 2015). In the
case of a healthy individual, the normal range is 2.5 to 7.1 mmol/l whereas, in the case of the
patient, Serum Urea is 17 mmol/. The impaired kidney simultaneously failed to eliminate
potassium level from the blood as observed in this case study. The blood report highlighted that
Serum Potassium was 5.7 mmol/L whereas, in case of normal individuals, the level is 3.6 to 5.2
mmol/l which further manifested as nausea, tiredness, and pruritus (Young et al., 2015).
RENAL FAILURE
result in end-stage renal disease. The patient was diagnosed with high blood pressure (190/ 100)
whereas the blood pressure of a healthy individual is 120/80, highlighting is one of the prime
cause of kidney failure. Kidney helps to filter the waste product and extra fluid of the blood
through blood vessels (Hill et al., 2016). However, hypertension cause arteries of the kidneys to
narrow and damage. The damage arteries are not able to deliver enough blood to the kidney
tissues. The patient had palpitation for five years which can a risk of heart condition since
palpitation has resulted in the abnormal sinus rhythm ( changes in the cardiac rate) and heart
failure to the pump the adequate blood which further can induce pressure in the main vein
connected with kidney ( reduced oxygen-rich blood supply) (Xie et al., 2017). Consequently,
renal function declines due to high blood pressure which further reduced glomerular filtration
rate as observed in this case study. The patient had GFR 10ml/min/1.73m2 whereas, for women,
the normal range is 90 to 120mL/min/1.73m2 (Webster et al., 2015). On the other hand, impaired
kidney function is signified by an elevated serum creatinine level since the functional kidney can
clear creatinine from the blood. In this current context, the serum creatinine level was 90 umol/L
whereas, in healthy individuals, the normal range is 45 to 90 mmol/l. when kidney function is
impaired, the kidney failed to eliminate urea from the blood in the form of urine which resulted
in a high level of urea concentration as observed in this case study (Webster et al., 2015). In the
case of a healthy individual, the normal range is 2.5 to 7.1 mmol/l whereas, in the case of the
patient, Serum Urea is 17 mmol/. The impaired kidney simultaneously failed to eliminate
potassium level from the blood as observed in this case study. The blood report highlighted that
Serum Potassium was 5.7 mmol/L whereas, in case of normal individuals, the level is 3.6 to 5.2
mmol/l which further manifested as nausea, tiredness, and pruritus (Young et al., 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
RENAL FAILURE
The general complication for these clinical manifestation includes uremia, heart failure,
and hyperkalemia. Uremia can be observed due to the high urea level and hyperkalemia observed
due to the high potassium level. Heart failure can be observed due to hypertension and GRF
(Webster et al., 2015).
The common treatment that can be suggested to the patient involves renal replacement
therapy, transplantation and Vitamin D supplements and treatment of comorbid diseases
(Webster et al., 2015).
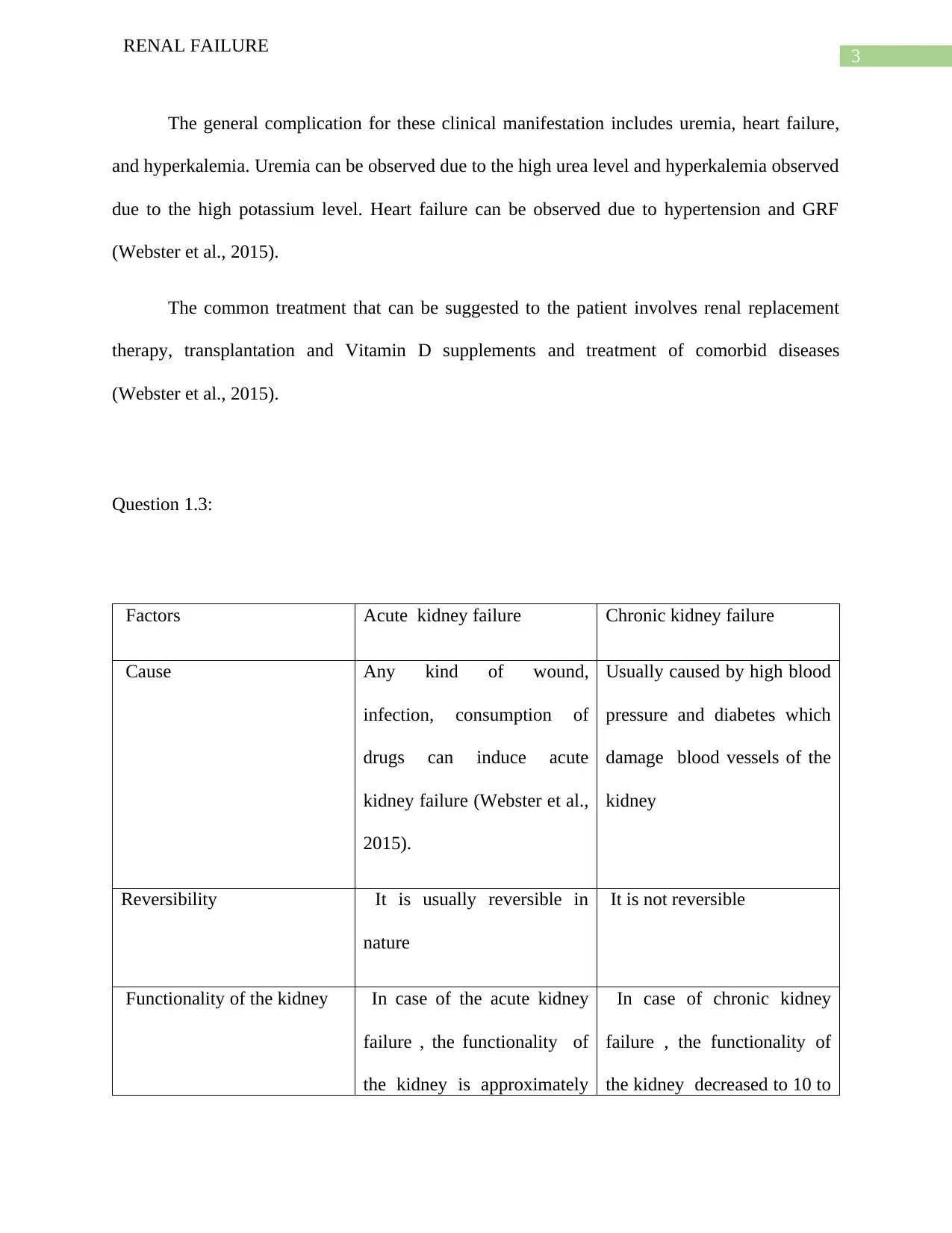
Question 1.3:
Factors Acute kidney failure Chronic kidney failure
Cause Any kind of wound,
infection, consumption of
drugs can induce acute
kidney failure (Webster et al.,
2015).
Usually caused by high blood
pressure and diabetes which
damage blood vessels of the
kidney
Reversibility It is usually reversible in
nature
It is not reversible
Functionality of the kidney In case of the acute kidney
failure , the functionality of
the kidney is approximately
In case of chronic kidney
failure , the functionality of
the kidney decreased to 10 to
RENAL FAILURE
The general complication for these clinical manifestation includes uremia, heart failure,
and hyperkalemia. Uremia can be observed due to the high urea level and hyperkalemia observed
due to the high potassium level. Heart failure can be observed due to hypertension and GRF
(Webster et al., 2015).
The common treatment that can be suggested to the patient involves renal replacement
therapy, transplantation and Vitamin D supplements and treatment of comorbid diseases
(Webster et al., 2015).
Question 1.3:
Factors Acute kidney failure Chronic kidney failure
Cause Any kind of wound,
infection, consumption of
drugs can induce acute
kidney failure (Webster et al.,
2015).
Usually caused by high blood
pressure and diabetes which
damage blood vessels of the
kidney
Reversibility It is usually reversible in
nature
It is not reversible
Functionality of the kidney In case of the acute kidney
failure , the functionality of
the kidney is approximately
In case of chronic kidney
failure , the functionality of
the kidney decreased to 10 to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
RENAL FAILURE
50% which can be reversed 15% which cannot be reduced
(Xie et al., 2017)
Peripheral neuropathy Peripheral neuropathy is
absent
Peripheral neuropathy is
present
Renal osteodystrophy It is absent in acute kidney
failure
It is present in acute kidney
failure
Treatment Treated with proper diet,
dialysis exercise and fluid
restrictions (Xie et al., 2017).
It can be cured with the
assistance of hemodialysis
and kidney transplantation
1.4 renal replacement therapy:
Hemodialysis, called simply dialysis, is referred to as a therapy or clinical process of
cleansing the blood of a patient with kidney failure. The case study highlighted that the patient
was experiencing nausea, tiredness, and general pruritus. After seeking the help of General
practitioner, she was diagnosed with chronic kidney failure. She was advised to receive
hemodialysis as a treatment of chronic failure. Fealy et al. (2015), highlighted that it is used in
for extracorporeal removal of waste such as creatinine, urea from the blood when the kidney is
impaired to remove blood urea and blood creatinine. During dialysis, the blood passes through
the dialyzer for the removal of the waste product. The blood enter in the one end of the solution
followed by tiny fibers where simultaneously dialysis solution moves in the opposite on the
RENAL FAILURE
50% which can be reversed 15% which cannot be reduced
(Xie et al., 2017)
Peripheral neuropathy Peripheral neuropathy is
absent
Peripheral neuropathy is
present
Renal osteodystrophy It is absent in acute kidney
failure
It is present in acute kidney
failure
Treatment Treated with proper diet,
dialysis exercise and fluid
restrictions (Xie et al., 2017).
It can be cured with the
assistance of hemodialysis
and kidney transplantation
1.4 renal replacement therapy:
Hemodialysis, called simply dialysis, is referred to as a therapy or clinical process of
cleansing the blood of a patient with kidney failure. The case study highlighted that the patient
was experiencing nausea, tiredness, and general pruritus. After seeking the help of General
practitioner, she was diagnosed with chronic kidney failure. She was advised to receive
hemodialysis as a treatment of chronic failure. Fealy et al. (2015), highlighted that it is used in
for extracorporeal removal of waste such as creatinine, urea from the blood when the kidney is
impaired to remove blood urea and blood creatinine. During dialysis, the blood passes through
the dialyzer for the removal of the waste product. The blood enter in the one end of the solution
followed by tiny fibers where simultaneously dialysis solution moves in the opposite on the
5
RENAL FAILURE
outside of the body (Bellomo et al., 2016). The creatinine and urea moved into the solution and
filtered blood moved into the body. The side effects include too much mineral and low blood
pressure along with muscle cramp.
Question 2.1:
The case study highlighted that the patient had chronic kidney failure where blood test
indicted high blood pressure, potassium level, high serum creatinine, and high urea. In this
context, the two most suitable drugs that can manage this situation would be Fosrenol and
benazepril
Considering forsrenol, it is also called lanthanum prevents the body from absorbing phosphate,
allowing it to be removed from the body. In the case of chronic kidney failure, the high level of
phosphate in the blood hinders the calcium absorption (Chan et al., 2017). Hence, lanthanum
carbonate binds to the phosphate and decreases absorption of phosphate by producing insoluble
lanthanum phosphate complexes which pass through GI tract unabsorbed. In simulated gastric
fluid, it binds to the phosphorus and eliminates it from the body. The common four side effects
of this drug are upset stomach and vomiting, itching and rash in the skin and stomach cramp
(Habbous et al., 2017). As the patient had nausea and feeling of tiredness, the nurses are required
to be exceedingly careful while providing the patient with the drug. The four crucial nursing
consideration would be an assessment of the nursing that assessment of the urine out of the
patient, the assessment of the proper stool output of the patient along with an assessment of diet
and assessment of the skin for any rashes (Habbous et al., 2017). Nurses are required to consider
RENAL FAILURE
outside of the body (Bellomo et al., 2016). The creatinine and urea moved into the solution and
filtered blood moved into the body. The side effects include too much mineral and low blood
pressure along with muscle cramp.
Question 2.1:
The case study highlighted that the patient had chronic kidney failure where blood test
indicted high blood pressure, potassium level, high serum creatinine, and high urea. In this
context, the two most suitable drugs that can manage this situation would be Fosrenol and
benazepril
Considering forsrenol, it is also called lanthanum prevents the body from absorbing phosphate,
allowing it to be removed from the body. In the case of chronic kidney failure, the high level of
phosphate in the blood hinders the calcium absorption (Chan et al., 2017). Hence, lanthanum
carbonate binds to the phosphate and decreases absorption of phosphate by producing insoluble
lanthanum phosphate complexes which pass through GI tract unabsorbed. In simulated gastric
fluid, it binds to the phosphorus and eliminates it from the body. The common four side effects
of this drug are upset stomach and vomiting, itching and rash in the skin and stomach cramp
(Habbous et al., 2017). As the patient had nausea and feeling of tiredness, the nurses are required
to be exceedingly careful while providing the patient with the drug. The four crucial nursing
consideration would be an assessment of the nursing that assessment of the urine out of the
patient, the assessment of the proper stool output of the patient along with an assessment of diet
and assessment of the skin for any rashes (Habbous et al., 2017). Nurses are required to consider
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
RENAL FAILURE
these things while administrating the drug to the patient and immediately required to
communicate with the physician during side effects of the drug.
Considering benzapril, it is an angiotensin-converting enzyme (ACE) inhibitor and this
prodrug is hydrolyzed by esterase to its benazeprilat which is used to treat hypertension. It
competes with angiotensin I to bind where it blocks the conversion of angiotensin I into
angiotensin II (Elsebaei & Zhu, 2016). As angiotensin II is a vasoconstrictor, the negative
feedback facilitates vasodilator and reduce the blood pressure along with stimulate baroreceptor
reflex mechanism which further decreases aldosterone secretion. The bioavailability of the oral
dose is 37% and reach peak plasma concentration within 1 hour (Gismondi et al., 2015). The
slow peak reached at a median of 1.5 hours. Hence, it will reduce the blood pressure of the
patient to 120/80 from 190/ 100 which is hypertension. The route of elimination is through urine
output and approximately 11%-12% of benazeprilat excreted through urine in case of healthy
individuals (Elsebaei & Zhu, 2016). While consuming the pharmacological drug, the patient may
experience side effects such as cough, vomiting, dizziness and stomach pain. In this case, the
nurses are required to be exceedingly careful while providing the patient with the drug. The four
nursing considerations nurses are required to consider include assessment of dehydration in the
body and water consumption of the patient, assessment of chest pressure, assessment of dietary
and assessment of stomach pain and pain scale.
Question 2.2:
The patient was diagnosed with chronic kidney failure and the blood result highlighted
that GFR was 10ml/min/1.73m2 and Hb (Haemoglobin) was 95g/L.
RENAL FAILURE
these things while administrating the drug to the patient and immediately required to
communicate with the physician during side effects of the drug.
Considering benzapril, it is an angiotensin-converting enzyme (ACE) inhibitor and this
prodrug is hydrolyzed by esterase to its benazeprilat which is used to treat hypertension. It
competes with angiotensin I to bind where it blocks the conversion of angiotensin I into
angiotensin II (Elsebaei & Zhu, 2016). As angiotensin II is a vasoconstrictor, the negative
feedback facilitates vasodilator and reduce the blood pressure along with stimulate baroreceptor
reflex mechanism which further decreases aldosterone secretion. The bioavailability of the oral
dose is 37% and reach peak plasma concentration within 1 hour (Gismondi et al., 2015). The
slow peak reached at a median of 1.5 hours. Hence, it will reduce the blood pressure of the
patient to 120/80 from 190/ 100 which is hypertension. The route of elimination is through urine
output and approximately 11%-12% of benazeprilat excreted through urine in case of healthy
individuals (Elsebaei & Zhu, 2016). While consuming the pharmacological drug, the patient may
experience side effects such as cough, vomiting, dizziness and stomach pain. In this case, the
nurses are required to be exceedingly careful while providing the patient with the drug. The four
nursing considerations nurses are required to consider include assessment of dehydration in the
body and water consumption of the patient, assessment of chest pressure, assessment of dietary
and assessment of stomach pain and pain scale.
Question 2.2:
The patient was diagnosed with chronic kidney failure and the blood result highlighted
that GFR was 10ml/min/1.73m2 and Hb (Haemoglobin) was 95g/L.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
RENAL FAILURE
Glomerular are the tiny filters in the kidneys which filter waste products such as
creatinine, urea, and potassium from the blood and eliminate it through the urine. Hence
glomerulus filtration rate is used to estimate the amount of blood passes through the glomeruli in
each minute which further provide the estimation of the functionality of the kidney (Rosansky et
al., 2019). In this current context, the patient had GFR 10ml/min/1.73m2 whereas, for women,
the normal range is 90 to 120mL/min/1.73m2. This result indicates, the patient had impaired
kidney function which failed to eliminate waste from the blood. On the other hand, patient with
chronic kidney failure is unable to make erythropoietin (EPO) which further result in lower
hemoglobin production from the bone marrow and patient experience anemia. In this case, the
patient had Hb was 95g/L (Rosansky et al., 2019).
Question 3.1:
The teach-back method is also called the “show-me" method. It is a communication and
education validation method that is used by healthcare providers for confirming that the provided
information is understood by the patient. The teach-back method is used in health care in order to
improve health literacy in the patient. Dinh et al. (2016) highlighted that there is a persistent gap
in the perception regarding the fact that how many patients need information and how much
providers can communication due to the barriers of the clinical terminology, language, and
communication process. There are six parts of the assignment which is who, what, when, why
and how. The improvement of patient health is depending on these factors (Farris, 2015).
RENAL FAILURE
Glomerular are the tiny filters in the kidneys which filter waste products such as
creatinine, urea, and potassium from the blood and eliminate it through the urine. Hence
glomerulus filtration rate is used to estimate the amount of blood passes through the glomeruli in
each minute which further provide the estimation of the functionality of the kidney (Rosansky et
al., 2019). In this current context, the patient had GFR 10ml/min/1.73m2 whereas, for women,
the normal range is 90 to 120mL/min/1.73m2. This result indicates, the patient had impaired
kidney function which failed to eliminate waste from the blood. On the other hand, patient with
chronic kidney failure is unable to make erythropoietin (EPO) which further result in lower
hemoglobin production from the bone marrow and patient experience anemia. In this case, the
patient had Hb was 95g/L (Rosansky et al., 2019).
Question 3.1:
The teach-back method is also called the “show-me" method. It is a communication and
education validation method that is used by healthcare providers for confirming that the provided
information is understood by the patient. The teach-back method is used in health care in order to
improve health literacy in the patient. Dinh et al. (2016) highlighted that there is a persistent gap
in the perception regarding the fact that how many patients need information and how much
providers can communication due to the barriers of the clinical terminology, language, and
communication process. There are six parts of the assignment which is who, what, when, why
and how. The improvement of patient health is depending on these factors (Farris, 2015).
8
RENAL FAILURE
Question 3.2:
Considering the chronic kidney failure of the patient, the patient is required to manage
her fluid intake which will further improve the prognosis of the disease. In this case, restriction
of fluid intake can improve her situation as excessive fluid cannot be filtered through the
impaired kidney. Hence, health literacy can be given to the patient with the assistance of teach-
back method.
Who:
The health literacy would be provided to Melanie by health care providers such as nurse
with an aim of management of fluid restriction.
What:
Melanie would be engaged in therapeutic communication by a nurse. After gathering
medical history and current status of her health, she would be provided with the information of
fluid restriction such as the need of the for the fluid restrictions. In the case of kidney failure,
patients failed to remove waste product from the blood and it is accumulated in the blood. Hence,
Melanie would be provided with the information that the restriction of fluid consumption will
improve her kidney function since fewer waste products would be accumulated in the blood.
When:
The teach-back method would be conducted at the early in the care process where the
patient is required to conduct self-management
RENAL FAILURE
Question 3.2:
Considering the chronic kidney failure of the patient, the patient is required to manage
her fluid intake which will further improve the prognosis of the disease. In this case, restriction
of fluid intake can improve her situation as excessive fluid cannot be filtered through the
impaired kidney. Hence, health literacy can be given to the patient with the assistance of teach-
back method.
Who:
The health literacy would be provided to Melanie by health care providers such as nurse
with an aim of management of fluid restriction.
What:
Melanie would be engaged in therapeutic communication by a nurse. After gathering
medical history and current status of her health, she would be provided with the information of
fluid restriction such as the need of the for the fluid restrictions. In the case of kidney failure,
patients failed to remove waste product from the blood and it is accumulated in the blood. Hence,
Melanie would be provided with the information that the restriction of fluid consumption will
improve her kidney function since fewer waste products would be accumulated in the blood.
When:
The teach-back method would be conducted at the early in the care process where the
patient is required to conduct self-management
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
RENAL FAILURE
Why:
It is important to provide information to the patient as the patient will gather the relevant
information of the medical process and it will improve her adherence to the treatment
How:
The process would be conducted in the hospital where face to face communication would
be done and the explanation would be done with PowerPoint and visual representations.
RENAL FAILURE
Why:
It is important to provide information to the patient as the patient will gather the relevant
information of the medical process and it will improve her adherence to the treatment
How:
The process would be conducted in the hospital where face to face communication would
be done and the explanation would be done with PowerPoint and visual representations.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
RENAL FAILURE
References:
Bellomo, R., Mårtensson, J., Lo, S., Kaukonen, K. M., Cass, A., & Gallagher, M. (2016).
Femoral access and delivery of continuous renal replacement therapy dose. Blood
purification, 41(1-3), 11-17.
Chalmers, C. (2019). Applied anatomy and physiology and the renal disease process. Renal
Nursing: Care and Management of People with Kidney Disease, 21-58.
Chan, S., Au, K., Francis, R. S., Mudge, D. W., Johnson, D. W., & Pillans, P. I. (2017).
Phosphate binders in patients with chronic kidney disease. Australian prescriber, 40(1),
10.
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
Elsebaei, F., & Zhu, Y. (2016). Enhanced elution of angiotensin converting enzyme inhibitors in
ion chromatography: Application to their simultaneous quantitation in formulations and
human plasma. Microchemical Journal, 124, 215-221.
Farris, C. (2015). The teach back method. Home healthcare now, 33(6), 344-345.
Fealy, N., Aitken, L., du Toit, E., & Baldwin, I. (2015). Continuous renal replacement therapy:
current practice in Australian and New Zealand intensive care units. Critical Care and
Resuscitation, 17(2), 83.
Gismondi, R. A., Oigman, W., Bedirian, R., Pozzobon, C. R., Ladeira, M. C. B., & Neves, M. F.
(2015). Comparison of benazepril and losartan on endothelial function and vascular
RENAL FAILURE
References:
Bellomo, R., Mårtensson, J., Lo, S., Kaukonen, K. M., Cass, A., & Gallagher, M. (2016).
Femoral access and delivery of continuous renal replacement therapy dose. Blood
purification, 41(1-3), 11-17.
Chalmers, C. (2019). Applied anatomy and physiology and the renal disease process. Renal
Nursing: Care and Management of People with Kidney Disease, 21-58.
Chan, S., Au, K., Francis, R. S., Mudge, D. W., Johnson, D. W., & Pillans, P. I. (2017).
Phosphate binders in patients with chronic kidney disease. Australian prescriber, 40(1),
10.
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
Elsebaei, F., & Zhu, Y. (2016). Enhanced elution of angiotensin converting enzyme inhibitors in
ion chromatography: Application to their simultaneous quantitation in formulations and
human plasma. Microchemical Journal, 124, 215-221.
Farris, C. (2015). The teach back method. Home healthcare now, 33(6), 344-345.
Fealy, N., Aitken, L., du Toit, E., & Baldwin, I. (2015). Continuous renal replacement therapy:
current practice in Australian and New Zealand intensive care units. Critical Care and
Resuscitation, 17(2), 83.
Gismondi, R. A., Oigman, W., Bedirian, R., Pozzobon, C. R., Ladeira, M. C. B., & Neves, M. F.
(2015). Comparison of benazepril and losartan on endothelial function and vascular
11
RENAL FAILURE
stiffness in patients with Type 2 diabetes mellitus and hypertension: A randomized
controlled trial. Journal of the Renin-Angiotensin-Aldosterone System, 16(4), 967-974.
Gosling, J. A., Harris, P. F., Humpherson, J. R., Whitmore, I., & Willan, P. L. (2016). Human
Anatomy, Color Atlas and Textbook E-Book. Elsevier Health Sciences.
Habbous, S., Przech, S., Acedillo, R., Sarma, S., Garg, A. X., & Martin, J. (2017). The efficacy
and safety of sevelamer and lanthanum versus calcium-containing and iron-based binders
in treating hyperphosphatemia in patients with chronic kidney disease: a systematic
review and meta-analysis. Nephrology Dialysis Transplantation, 32(1), 111-125.
Hill, N. R., Fatoba, S. T., Oke, J. L., Hirst, J. A., O’Callaghan, C. A., Lasserson, D. S., &
Hobbs, F. R. (2016). Global prevalence of chronic kidney disease–a systematic review
and meta-analysis. PloS one, 11(7), e0158765.
Liyanage, T., Ninomiya, T., Jha, V., Neal, B., Patrice, H. M., Okpechi, I., ... & Rodgers, A.
(2015). Worldwide access to treatment for end-stage kidney disease: a systematic
review. The Lancet, 385(9981), 1975-1982.
Rosansky, S. J., Thamer, M., Caskey, F., Couchoud, C., McDonald, S. P., & Moist, L. (2019). A
comparison of predialysis estimated glomerular filtration rate in the US, Canada, France,
Australia, and the UK between 2005 and 2015. Kidney international, 95(5), 1273.
Webster, A. C., Nagler, E. V., Morton, R. L., & Masson, P. (2017). Chronic kidney disease. The
lancet, 389(10075), 1238-1252.
Xie, X., Atkins, E., Lv, J., Bennett, A., Neal, B., Ninomiya, T., ... & Chalmers, J. (2016). Effects
of intensive blood pressure lowering on cardiovascular and renal outcomes: updated
systematic review and meta-analysis. The Lancet, 387(10017), 435-443.
RENAL FAILURE
stiffness in patients with Type 2 diabetes mellitus and hypertension: A randomized
controlled trial. Journal of the Renin-Angiotensin-Aldosterone System, 16(4), 967-974.
Gosling, J. A., Harris, P. F., Humpherson, J. R., Whitmore, I., & Willan, P. L. (2016). Human
Anatomy, Color Atlas and Textbook E-Book. Elsevier Health Sciences.
Habbous, S., Przech, S., Acedillo, R., Sarma, S., Garg, A. X., & Martin, J. (2017). The efficacy
and safety of sevelamer and lanthanum versus calcium-containing and iron-based binders
in treating hyperphosphatemia in patients with chronic kidney disease: a systematic
review and meta-analysis. Nephrology Dialysis Transplantation, 32(1), 111-125.
Hill, N. R., Fatoba, S. T., Oke, J. L., Hirst, J. A., O’Callaghan, C. A., Lasserson, D. S., &
Hobbs, F. R. (2016). Global prevalence of chronic kidney disease–a systematic review
and meta-analysis. PloS one, 11(7), e0158765.
Liyanage, T., Ninomiya, T., Jha, V., Neal, B., Patrice, H. M., Okpechi, I., ... & Rodgers, A.
(2015). Worldwide access to treatment for end-stage kidney disease: a systematic
review. The Lancet, 385(9981), 1975-1982.
Rosansky, S. J., Thamer, M., Caskey, F., Couchoud, C., McDonald, S. P., & Moist, L. (2019). A
comparison of predialysis estimated glomerular filtration rate in the US, Canada, France,
Australia, and the UK between 2005 and 2015. Kidney international, 95(5), 1273.
Webster, A. C., Nagler, E. V., Morton, R. L., & Masson, P. (2017). Chronic kidney disease. The
lancet, 389(10075), 1238-1252.
Xie, X., Atkins, E., Lv, J., Bennett, A., Neal, B., Ninomiya, T., ... & Chalmers, J. (2016). Effects
of intensive blood pressure lowering on cardiovascular and renal outcomes: updated
systematic review and meta-analysis. The Lancet, 387(10017), 435-443.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





