CNA573 Case Study: Renal Transplant - Acute Allograft Rejection
VerifiedAdded on 2023/06/08
|12
|3128
|491
Case Study
AI Summary
This case study focuses on Mrs. T, a renal transplant recipient who presents with elevated creatinine levels indicative of acute allograft rejection. The paper defines acute allograft rejection, comparing it with chronic allograft nephropathy, and outlines the pathophysiology involving T-lymphocyte infiltration and subsequent cytotoxic effects. Initial management strategies, including immunosuppressive therapy with corticosteroids, calcineurin inhibitors, and mTOR inhibitors, are discussed. Key patient education points, emphasizing the likelihood of rejection, alternative treatment options like dialysis, and the importance of medication adherence and recognizing danger signs, are highlighted. The study also details the nursing care involved in assessing the patient's overall health status, fluid balance, and wound condition, along with post-renal allograft biopsy care to prevent complications such as bleeding and pain. The goal is to improve health outcomes through evidence-based interventions and comprehensive patient education.

Running Head: RENAL TRANSPLANTATION
1
Renal Transplantation
Student’s Name
Institution of Affiliation
Course Name
Date
1
Renal Transplantation
Student’s Name
Institution of Affiliation
Course Name
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
RENAL TRANSPLANTATION 2
Introduction
In medical practice, despite the induction of immunosuppression and the utilization of
highly aggressive immunosuppressive regimens, incidences of acute allograft rejection following
renal transplants are several. These incidences pose significant therapeutic and diagnostic
challenges to health care providers and result in early mortalities and loss of graft. To add on,
acute allograft rejections initiate chronic alloimmune responses and inflammation of the centered
airway which predisposes patients to lung allograft dysfunctions that are chronic and
bronchiolitis obliterans syndrome which is collectively major sources of mortalities and
morbidities following a transplant.
This paper discusses Mrs. T who had received her first renal transplant in 6 weeks’ time
and a recent test revealed that she had a creatinine level of 240mmol/L. Nurses have a role in
assessing patients and instituting evidence-based interventions to improve health outcomes in
clinically unsuspecting patients with acute allograft rejection that have recently undergone a
renal transplant. This can be achieved by nurses having a proper understanding of the definition,
pathophysiology, and management of acute allograft rejection. Only then can nurses convey the
most appropriate health education and develop an effective plan of care for patients with acute
allograft rejection.
Comparison Of Acute Allograft Rejection With Chronic Allograft Nephropathy
Generally, there exist three forms of allograft rejection which are; acute, hyperacute and
chronic. Acute rejection occurs within the initial 6-12 months following transplantation which is
caused primarily by lymphocytes in the thymus (t-cells) (Benzimra, Calligaro & Glanville,
2017). Unless the suppression of the immune system is achieved usually by the use of drugs,
acute allograft rejection tends to occur in nearly all transplants apart from identical twins. Today,
Introduction
In medical practice, despite the induction of immunosuppression and the utilization of
highly aggressive immunosuppressive regimens, incidences of acute allograft rejection following
renal transplants are several. These incidences pose significant therapeutic and diagnostic
challenges to health care providers and result in early mortalities and loss of graft. To add on,
acute allograft rejections initiate chronic alloimmune responses and inflammation of the centered
airway which predisposes patients to lung allograft dysfunctions that are chronic and
bronchiolitis obliterans syndrome which is collectively major sources of mortalities and
morbidities following a transplant.
This paper discusses Mrs. T who had received her first renal transplant in 6 weeks’ time
and a recent test revealed that she had a creatinine level of 240mmol/L. Nurses have a role in
assessing patients and instituting evidence-based interventions to improve health outcomes in
clinically unsuspecting patients with acute allograft rejection that have recently undergone a
renal transplant. This can be achieved by nurses having a proper understanding of the definition,
pathophysiology, and management of acute allograft rejection. Only then can nurses convey the
most appropriate health education and develop an effective plan of care for patients with acute
allograft rejection.
Comparison Of Acute Allograft Rejection With Chronic Allograft Nephropathy
Generally, there exist three forms of allograft rejection which are; acute, hyperacute and
chronic. Acute rejection occurs within the initial 6-12 months following transplantation which is
caused primarily by lymphocytes in the thymus (t-cells) (Benzimra, Calligaro & Glanville,
2017). Unless the suppression of the immune system is achieved usually by the use of drugs,
acute allograft rejection tends to occur in nearly all transplants apart from identical twins. Today,
RENAL TRANSPLANTATION 3
acute allograft rejection is still a prevalent issue in kidney transplantations. Generally, there are
incidences of 38% within the first year following transplants. Despite the fact that when they
occur by themselves they are rarely fatal, the indirect consequences have adverse effects on the
outcomes of transplantation (Moreau et al., 2013). Tissues that are highly vascularized such as
the liver, lungs, and kidneys host the earliest signs. In most cases, it is easy to identify acute
rejection episodes and appropriate treatment offered promptly to prevent the failure of organs.
However, when episodes recur, they lead to chronic allograft rejection/ nephropathy.
On the other hand, chronic allograft neuropathy defines the functional loss of
transplanted tissues through fibrosis. It is a term used to explain long-term morbidities in
recipients who have undergone transplantation and results from several factors including
lymphocytes and antibodies (Fletcher, Nankivell & Alexander, 2013). Chronic allograft
neuropathy also occurs from hypoperfusion, recurrent disease, and ischemia-reperfusion and
infections. However, its diagnosis is often made using a biopsy of a suspected organ with the
heart as the only organ that is exempted (Kloc & Ghobrial, 2014). In pediatric recipients of renal
transplants, chronic allograft neuropathy is the leading cause of the loss of renal allograft. As
outlined by Demetris et.al. (2014), chronic allograft neuropathy has great rates of survival with
improvements in immunosuppression. However, opportunistic infections present challenges.
Pathophysiology Of Acute Allograft Rejection
Acute allograft rejection is common during the first initial months following
transplantation. However, it may also occur during an allograft’s life. It is mediated by the t-
lymphocytes which are present in the circulation and may infiltrate an allograft via the
endothelium of a vascular tissue. Following infiltration of a graft with lymphocytes, cytotoxic
cells often start to target and kill the cells that function in an allograft (Ingulli, 2013).
acute allograft rejection is still a prevalent issue in kidney transplantations. Generally, there are
incidences of 38% within the first year following transplants. Despite the fact that when they
occur by themselves they are rarely fatal, the indirect consequences have adverse effects on the
outcomes of transplantation (Moreau et al., 2013). Tissues that are highly vascularized such as
the liver, lungs, and kidneys host the earliest signs. In most cases, it is easy to identify acute
rejection episodes and appropriate treatment offered promptly to prevent the failure of organs.
However, when episodes recur, they lead to chronic allograft rejection/ nephropathy.
On the other hand, chronic allograft neuropathy defines the functional loss of
transplanted tissues through fibrosis. It is a term used to explain long-term morbidities in
recipients who have undergone transplantation and results from several factors including
lymphocytes and antibodies (Fletcher, Nankivell & Alexander, 2013). Chronic allograft
neuropathy also occurs from hypoperfusion, recurrent disease, and ischemia-reperfusion and
infections. However, its diagnosis is often made using a biopsy of a suspected organ with the
heart as the only organ that is exempted (Kloc & Ghobrial, 2014). In pediatric recipients of renal
transplants, chronic allograft neuropathy is the leading cause of the loss of renal allograft. As
outlined by Demetris et.al. (2014), chronic allograft neuropathy has great rates of survival with
improvements in immunosuppression. However, opportunistic infections present challenges.
Pathophysiology Of Acute Allograft Rejection
Acute allograft rejection is common during the first initial months following
transplantation. However, it may also occur during an allograft’s life. It is mediated by the t-
lymphocytes which are present in the circulation and may infiltrate an allograft via the
endothelium of a vascular tissue. Following infiltration of a graft with lymphocytes, cytotoxic
cells often start to target and kill the cells that function in an allograft (Ingulli, 2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
RENAL TRANSPLANTATION 4
Simultaneously, the release of lymphocytes locally tends to attract and stimulate the presence of
macrophages to result in damage to tissues through a mechanism that is hypersensitive and
delayed. These series of inflammatory and immunologic events results in nonspecific signs and
symptoms such as lethargy, fever, pain and a tender graft site. Following kidney transplantation,
acute allograft rejection is likely to affect up to 20% of patients in the initial 6 months
(Benzimra, Calligaro & Glanville, 2017). This may be evidenced by the abrupt increase in the
concentration of serum creatinine to levels above 30 beyond the baseline.
Any transplanted organ may be rejected through primary mediation and activation of
alloreactive T cells and cells that present antigens such as dendritic, macrophages and
lymphocytes. Primarily, it should be noted that the infiltration of T cells to allograft results in an
acute allograft rejection that finally triggers cytotoxic and inflammatory effects (Benzimra,
Calligaro & Glanville, 2017). Should there be a failure to maintain immunosuppression;
complex interactions may exist between B cells, T cells, and CD4 cells which may result in
chronic allograft neuropathy and other complications.
Initial Management Of Acute Allograft Rejection
The initial management of an acute allograft rejection aims at improving clinical
outcomes and quality of life by addressing symptoms. Post-op, the overall health status of a
patient should be assessed including fluid status and urine output to check for dehydration.
Preferably, an input-output fluid chart can be used for this assessment with a urinary catheter in
situ (Leblanc et al., 2018). The patients wound should also be assessed daily to check for signs
of poor wound healing and immediately intervene when necessary. The wound should be kept
clean to avoid sepsis that would further result in more complications.
Simultaneously, the release of lymphocytes locally tends to attract and stimulate the presence of
macrophages to result in damage to tissues through a mechanism that is hypersensitive and
delayed. These series of inflammatory and immunologic events results in nonspecific signs and
symptoms such as lethargy, fever, pain and a tender graft site. Following kidney transplantation,
acute allograft rejection is likely to affect up to 20% of patients in the initial 6 months
(Benzimra, Calligaro & Glanville, 2017). This may be evidenced by the abrupt increase in the
concentration of serum creatinine to levels above 30 beyond the baseline.
Any transplanted organ may be rejected through primary mediation and activation of
alloreactive T cells and cells that present antigens such as dendritic, macrophages and
lymphocytes. Primarily, it should be noted that the infiltration of T cells to allograft results in an
acute allograft rejection that finally triggers cytotoxic and inflammatory effects (Benzimra,
Calligaro & Glanville, 2017). Should there be a failure to maintain immunosuppression;
complex interactions may exist between B cells, T cells, and CD4 cells which may result in
chronic allograft neuropathy and other complications.
Initial Management Of Acute Allograft Rejection
The initial management of an acute allograft rejection aims at improving clinical
outcomes and quality of life by addressing symptoms. Post-op, the overall health status of a
patient should be assessed including fluid status and urine output to check for dehydration.
Preferably, an input-output fluid chart can be used for this assessment with a urinary catheter in
situ (Leblanc et al., 2018). The patients wound should also be assessed daily to check for signs
of poor wound healing and immediately intervene when necessary. The wound should be kept
clean to avoid sepsis that would further result in more complications.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
RENAL TRANSPLANTATION 5
Acute rejection is managed by immunosuppressive therapy where a high dose of
corticosteroids can be applied in the short term and repeated severally. While focusing on a triple
therapy, an anti-proliferative agent and calcineurin inhibitor can be added. Some of the well-
known immunosuppressive high-dose corticosteroids include hydrocortisone and prednisolone.
Examples of calcineurin include; ciclosporin and tacrolimus (Leblanc et al., 2018). In patients
who the use of steroids and calcineurin inhibitors is contraindicated, mTOR inhibitors may be
prescribed. They include; everolimus and sirolimus among others. In most common practice,
health care providers initiate treatment with intravenous solumedrol for 3 days.
To restore kidney function and prevent the loss of grafts, anti-T cell antibodies may be
used and added to the immunosuppressive therapy. Although some are used to prevent rejection,
they are still recommended for the initial treatment of acute allograft rejections. Perfect examples
of specific antibody-based treatments which may be used include; polyclonal anti-T-cell
antibodies and monoclonal anti-CD20 antibodies (Leblanc et al., 2018). In other instances,
similar cases of acute allograft rejection may be managed with blood transfer through photo
immune therapy or photopheresis for the purposes of removing molecules in antibodies which
are specific to a tissue that was transplanted.
Key Education Points about Acute Allograft Rejection for The Patient
Patients who are about to undergo an organ transplant or have already undergone organ
transplant need to be adequately informed of the likelihood of rejection, possible consequences,
and available alternatives. Information of rejection often results in a mixture of complex feelings
such as guilt, depression, failure, and disappointment. With prior information, the intensity of
these feelings may be reduced (Ghadami et. al., 2012). Patients need to also be informed that in
case of rejection, a dialysis is still an option in treating kidney failure which results in lives that
Acute rejection is managed by immunosuppressive therapy where a high dose of
corticosteroids can be applied in the short term and repeated severally. While focusing on a triple
therapy, an anti-proliferative agent and calcineurin inhibitor can be added. Some of the well-
known immunosuppressive high-dose corticosteroids include hydrocortisone and prednisolone.
Examples of calcineurin include; ciclosporin and tacrolimus (Leblanc et al., 2018). In patients
who the use of steroids and calcineurin inhibitors is contraindicated, mTOR inhibitors may be
prescribed. They include; everolimus and sirolimus among others. In most common practice,
health care providers initiate treatment with intravenous solumedrol for 3 days.
To restore kidney function and prevent the loss of grafts, anti-T cell antibodies may be
used and added to the immunosuppressive therapy. Although some are used to prevent rejection,
they are still recommended for the initial treatment of acute allograft rejections. Perfect examples
of specific antibody-based treatments which may be used include; polyclonal anti-T-cell
antibodies and monoclonal anti-CD20 antibodies (Leblanc et al., 2018). In other instances,
similar cases of acute allograft rejection may be managed with blood transfer through photo
immune therapy or photopheresis for the purposes of removing molecules in antibodies which
are specific to a tissue that was transplanted.
Key Education Points about Acute Allograft Rejection for The Patient
Patients who are about to undergo an organ transplant or have already undergone organ
transplant need to be adequately informed of the likelihood of rejection, possible consequences,
and available alternatives. Information of rejection often results in a mixture of complex feelings
such as guilt, depression, failure, and disappointment. With prior information, the intensity of
these feelings may be reduced (Ghadami et. al., 2012). Patients need to also be informed that in
case of rejection, a dialysis is still an option in treating kidney failure which results in lives that
RENAL TRANSPLANTATION 6
are more happy and productive. Alternatively, patients can be informed that the chances of re-
transplantation are available.
Patients need to be educated on the importance of maintaining a healthy balanced diet
and to maintain contact with social and family support systems to prevent chances of developing
depression following an allograft rejection (Wang et al., 2017). It is also mandatory that the
patient is informed to look for any danger signs such as; reduced urination, fevers, swelling, flu-
like symptoms, weight gain and pain over the site of transplantation and advised to return
immediately to the healthcare provider. Healthcare providers should emphasize on the
importance of keeping to the list of medications that were prescribed upon discharge to prevent
new drug-drug interactions that may prevent the desired health outcomes (García et al., 2016).
To promote a patient’s understanding, this information has to be delivered in simple language
that takes note of cultural competency and aims at attaining effective clinical outcomes.
Demonstrations and brochures may be used to ensure that the patient retains and understands
essential information.
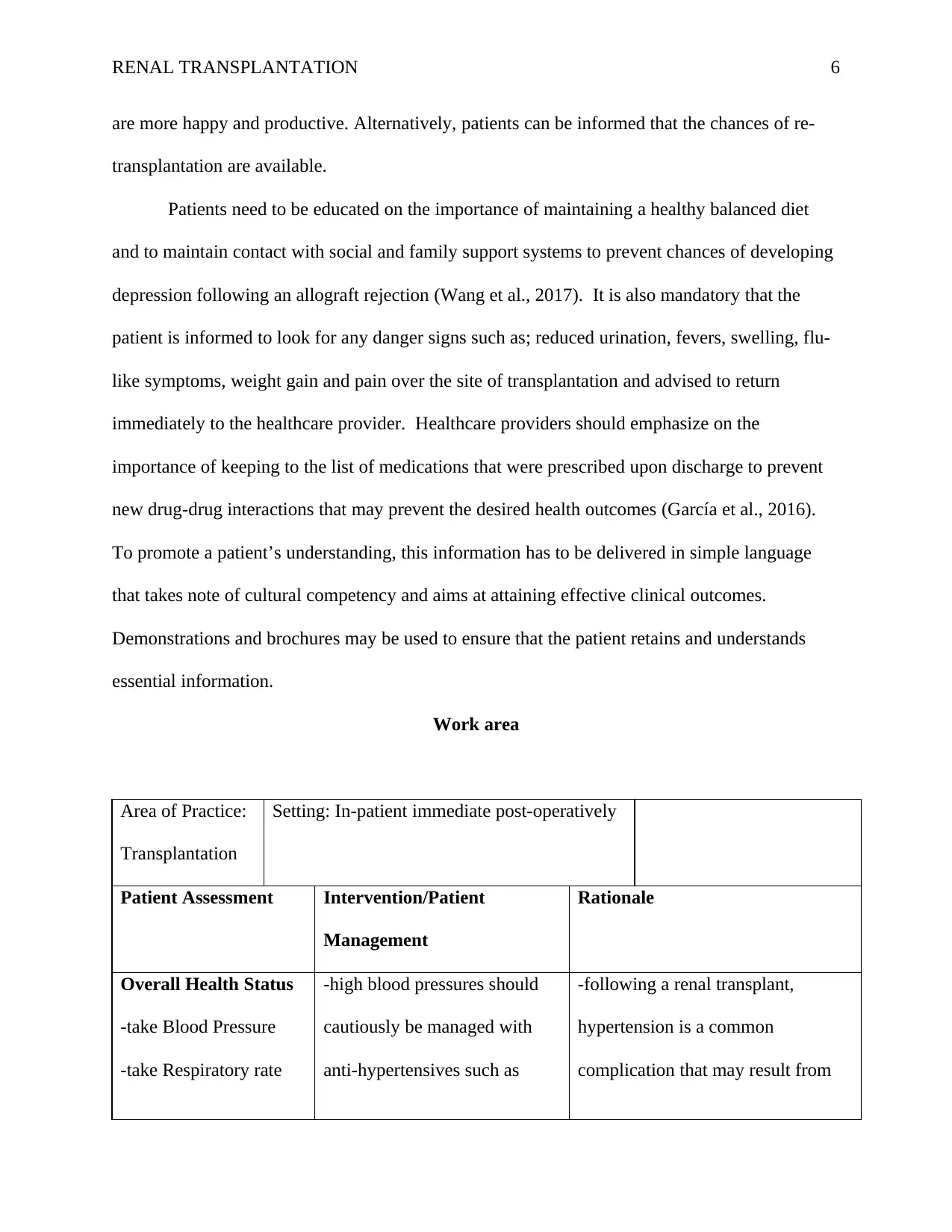
Work area
Area of Practice:
Transplantation
Setting: In-patient immediate post-operatively
Patient Assessment Intervention/Patient
Management
Rationale
Overall Health Status
-take Blood Pressure
-take Respiratory rate
-high blood pressures should
cautiously be managed with
anti-hypertensives such as
-following a renal transplant,
hypertension is a common
complication that may result from
are more happy and productive. Alternatively, patients can be informed that the chances of re-
transplantation are available.
Patients need to be educated on the importance of maintaining a healthy balanced diet
and to maintain contact with social and family support systems to prevent chances of developing
depression following an allograft rejection (Wang et al., 2017). It is also mandatory that the
patient is informed to look for any danger signs such as; reduced urination, fevers, swelling, flu-
like symptoms, weight gain and pain over the site of transplantation and advised to return
immediately to the healthcare provider. Healthcare providers should emphasize on the
importance of keeping to the list of medications that were prescribed upon discharge to prevent
new drug-drug interactions that may prevent the desired health outcomes (García et al., 2016).
To promote a patient’s understanding, this information has to be delivered in simple language
that takes note of cultural competency and aims at attaining effective clinical outcomes.
Demonstrations and brochures may be used to ensure that the patient retains and understands
essential information.
Work area
Area of Practice:
Transplantation
Setting: In-patient immediate post-operatively
Patient Assessment Intervention/Patient
Management
Rationale
Overall Health Status
-take Blood Pressure
-take Respiratory rate
-high blood pressures should
cautiously be managed with
anti-hypertensives such as
-following a renal transplant,
hypertension is a common
complication that may result from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
RENAL TRANSPLANTATION 7
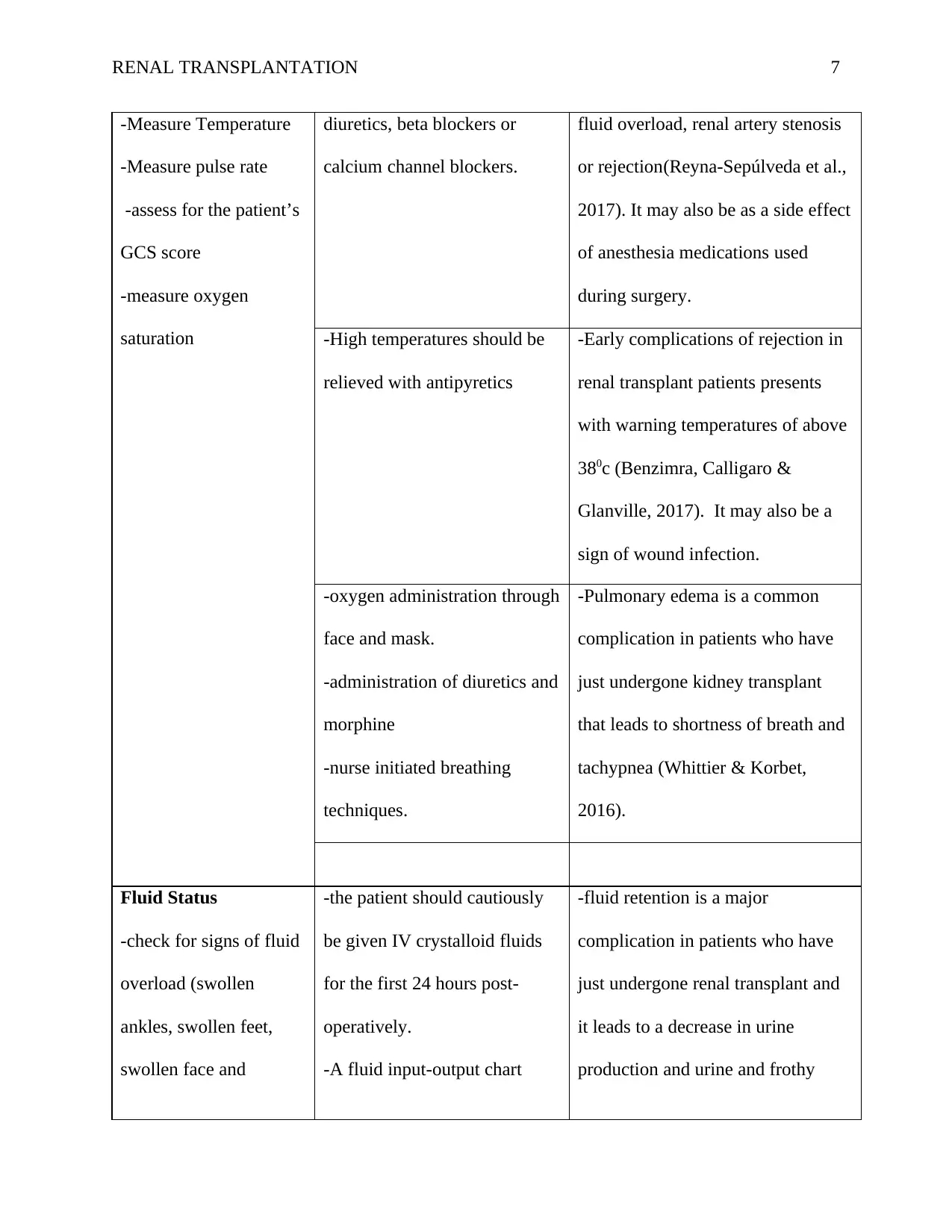
-Measure Temperature
-Measure pulse rate
-assess for the patient’s
GCS score
-measure oxygen
saturation
diuretics, beta blockers or
calcium channel blockers.
fluid overload, renal artery stenosis
or rejection(Reyna-Sepúlveda et al.,
2017). It may also be as a side effect
of anesthesia medications used
during surgery.
-High temperatures should be
relieved with antipyretics
-Early complications of rejection in
renal transplant patients presents
with warning temperatures of above
380c (Benzimra, Calligaro &
Glanville, 2017). It may also be a
sign of wound infection.
-oxygen administration through
face and mask.
-administration of diuretics and
morphine
-nurse initiated breathing
techniques.
-Pulmonary edema is a common
complication in patients who have
just undergone kidney transplant
that leads to shortness of breath and
tachypnea (Whittier & Korbet,
2016).
Fluid Status
-check for signs of fluid
overload (swollen
ankles, swollen feet,
swollen face and
-the patient should cautiously
be given IV crystalloid fluids
for the first 24 hours post-
operatively.
-A fluid input-output chart
-fluid retention is a major
complication in patients who have
just undergone renal transplant and
it leads to a decrease in urine
production and urine and frothy
-Measure Temperature
-Measure pulse rate
-assess for the patient’s
GCS score
-measure oxygen
saturation
diuretics, beta blockers or
calcium channel blockers.
fluid overload, renal artery stenosis
or rejection(Reyna-Sepúlveda et al.,
2017). It may also be as a side effect
of anesthesia medications used
during surgery.
-High temperatures should be
relieved with antipyretics
-Early complications of rejection in
renal transplant patients presents
with warning temperatures of above
380c (Benzimra, Calligaro &
Glanville, 2017). It may also be a
sign of wound infection.
-oxygen administration through
face and mask.
-administration of diuretics and
morphine
-nurse initiated breathing
techniques.
-Pulmonary edema is a common
complication in patients who have
just undergone kidney transplant
that leads to shortness of breath and
tachypnea (Whittier & Korbet,
2016).
Fluid Status
-check for signs of fluid
overload (swollen
ankles, swollen feet,
swollen face and
-the patient should cautiously
be given IV crystalloid fluids
for the first 24 hours post-
operatively.
-A fluid input-output chart
-fluid retention is a major
complication in patients who have
just undergone renal transplant and
it leads to a decrease in urine
production and urine and frothy
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
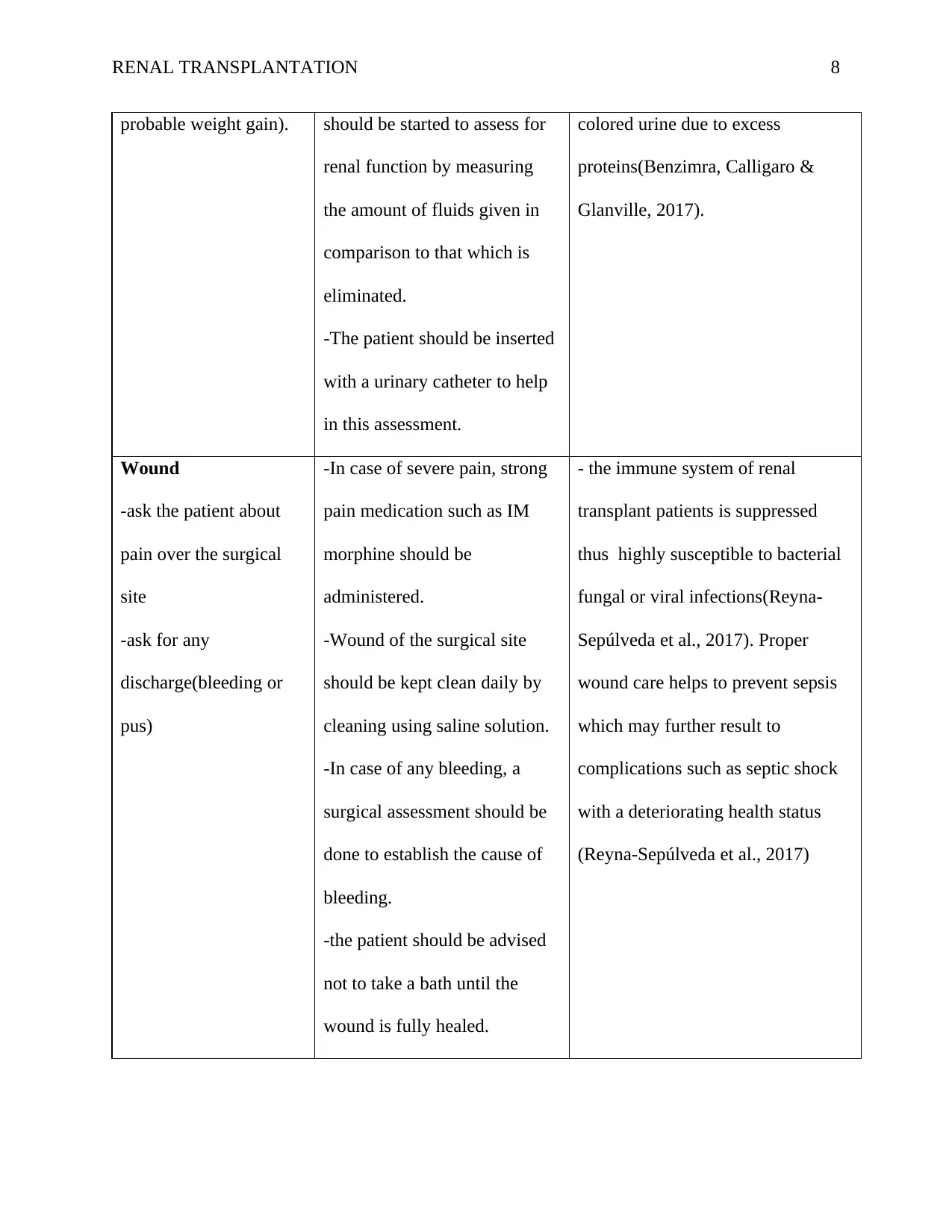
RENAL TRANSPLANTATION 8
probable weight gain). should be started to assess for
renal function by measuring
the amount of fluids given in
comparison to that which is
eliminated.
-The patient should be inserted
with a urinary catheter to help
in this assessment.
colored urine due to excess
proteins(Benzimra, Calligaro &
Glanville, 2017).
Wound
-ask the patient about
pain over the surgical
site
-ask for any
discharge(bleeding or
pus)
-In case of severe pain, strong
pain medication such as IM
morphine should be
administered.
-Wound of the surgical site
should be kept clean daily by
cleaning using saline solution.
-In case of any bleeding, a
surgical assessment should be
done to establish the cause of
bleeding.
-the patient should be advised
not to take a bath until the
wound is fully healed.
- the immune system of renal
transplant patients is suppressed
thus highly susceptible to bacterial
fungal or viral infections(Reyna-
Sepúlveda et al., 2017). Proper
wound care helps to prevent sepsis
which may further result to
complications such as septic shock
with a deteriorating health status
(Reyna-Sepúlveda et al., 2017)
probable weight gain). should be started to assess for
renal function by measuring
the amount of fluids given in
comparison to that which is
eliminated.
-The patient should be inserted
with a urinary catheter to help
in this assessment.
colored urine due to excess
proteins(Benzimra, Calligaro &
Glanville, 2017).
Wound
-ask the patient about
pain over the surgical
site
-ask for any
discharge(bleeding or
pus)
-In case of severe pain, strong
pain medication such as IM
morphine should be
administered.
-Wound of the surgical site
should be kept clean daily by
cleaning using saline solution.
-In case of any bleeding, a
surgical assessment should be
done to establish the cause of
bleeding.
-the patient should be advised
not to take a bath until the
wound is fully healed.
- the immune system of renal
transplant patients is suppressed
thus highly susceptible to bacterial
fungal or viral infections(Reyna-
Sepúlveda et al., 2017). Proper
wound care helps to prevent sepsis
which may further result to
complications such as septic shock
with a deteriorating health status
(Reyna-Sepúlveda et al., 2017)
RENAL TRANSPLANTATION 9
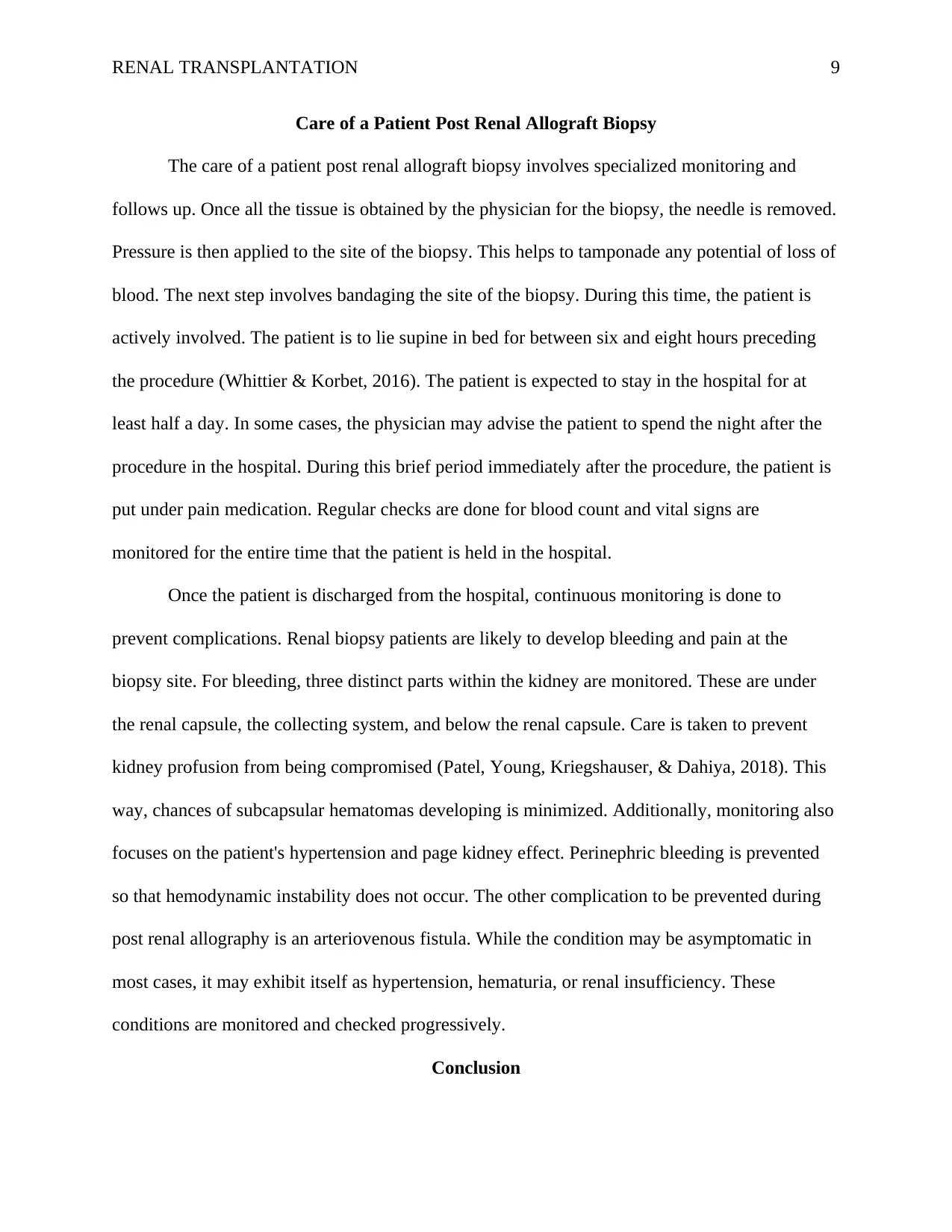
Care of a Patient Post Renal Allograft Biopsy
The care of a patient post renal allograft biopsy involves specialized monitoring and
follows up. Once all the tissue is obtained by the physician for the biopsy, the needle is removed.
Pressure is then applied to the site of the biopsy. This helps to tamponade any potential of loss of
blood. The next step involves bandaging the site of the biopsy. During this time, the patient is
actively involved. The patient is to lie supine in bed for between six and eight hours preceding
the procedure (Whittier & Korbet, 2016). The patient is expected to stay in the hospital for at
least half a day. In some cases, the physician may advise the patient to spend the night after the
procedure in the hospital. During this brief period immediately after the procedure, the patient is
put under pain medication. Regular checks are done for blood count and vital signs are
monitored for the entire time that the patient is held in the hospital.
Once the patient is discharged from the hospital, continuous monitoring is done to
prevent complications. Renal biopsy patients are likely to develop bleeding and pain at the
biopsy site. For bleeding, three distinct parts within the kidney are monitored. These are under
the renal capsule, the collecting system, and below the renal capsule. Care is taken to prevent
kidney profusion from being compromised (Patel, Young, Kriegshauser, & Dahiya, 2018). This
way, chances of subcapsular hematomas developing is minimized. Additionally, monitoring also
focuses on the patient's hypertension and page kidney effect. Perinephric bleeding is prevented
so that hemodynamic instability does not occur. The other complication to be prevented during
post renal allography is an arteriovenous fistula. While the condition may be asymptomatic in
most cases, it may exhibit itself as hypertension, hematuria, or renal insufficiency. These
conditions are monitored and checked progressively.
Conclusion
Care of a Patient Post Renal Allograft Biopsy
The care of a patient post renal allograft biopsy involves specialized monitoring and
follows up. Once all the tissue is obtained by the physician for the biopsy, the needle is removed.
Pressure is then applied to the site of the biopsy. This helps to tamponade any potential of loss of
blood. The next step involves bandaging the site of the biopsy. During this time, the patient is
actively involved. The patient is to lie supine in bed for between six and eight hours preceding
the procedure (Whittier & Korbet, 2016). The patient is expected to stay in the hospital for at
least half a day. In some cases, the physician may advise the patient to spend the night after the
procedure in the hospital. During this brief period immediately after the procedure, the patient is
put under pain medication. Regular checks are done for blood count and vital signs are
monitored for the entire time that the patient is held in the hospital.
Once the patient is discharged from the hospital, continuous monitoring is done to
prevent complications. Renal biopsy patients are likely to develop bleeding and pain at the
biopsy site. For bleeding, three distinct parts within the kidney are monitored. These are under
the renal capsule, the collecting system, and below the renal capsule. Care is taken to prevent
kidney profusion from being compromised (Patel, Young, Kriegshauser, & Dahiya, 2018). This
way, chances of subcapsular hematomas developing is minimized. Additionally, monitoring also
focuses on the patient's hypertension and page kidney effect. Perinephric bleeding is prevented
so that hemodynamic instability does not occur. The other complication to be prevented during
post renal allography is an arteriovenous fistula. While the condition may be asymptomatic in
most cases, it may exhibit itself as hypertension, hematuria, or renal insufficiency. These
conditions are monitored and checked progressively.
Conclusion
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

RENAL TRANSPLANTATION 10
Acute allograft rejection is a critical and life-threatening complication that arises from
organ transplantation that affects thousands of patients who opt for an organ transplant. Nurses
have the role of performing clinical assessments and instituting evidence-based interventions in
clinically unsuspecting patients with acute allograft rejection. However, a proper understanding
of the definition, pathophysiology and initial management of acute allograft rejection can support
the ability of nurses to provide prioritized clinical care, patient health education and follow-up
care in health settings. Following the diagnosis of an acute allograft rejection, nurses should
assess a patient's overall health status, fluid status, urine output, and the wound. Health education
should be provided in simple English language and should include information on nutrition and
diet, medications, physical exercise, wound care, the social support system, danger signs, and
currently available alternatives.
References
Benzimra, M., Calligaro, G. L., & Glanville, A. R. (2017). Acute rejection. Journal of Thoracic
Disease, 9(12), 5440–5457.
Demetris, A. J., Murase, N., Starzl, T. ., & Fung, J. J. (2014). Pathology of Chronic Rejection:
Acute allograft rejection is a critical and life-threatening complication that arises from
organ transplantation that affects thousands of patients who opt for an organ transplant. Nurses
have the role of performing clinical assessments and instituting evidence-based interventions in
clinically unsuspecting patients with acute allograft rejection. However, a proper understanding
of the definition, pathophysiology and initial management of acute allograft rejection can support
the ability of nurses to provide prioritized clinical care, patient health education and follow-up
care in health settings. Following the diagnosis of an acute allograft rejection, nurses should
assess a patient's overall health status, fluid status, urine output, and the wound. Health education
should be provided in simple English language and should include information on nutrition and
diet, medications, physical exercise, wound care, the social support system, danger signs, and
currently available alternatives.
References
Benzimra, M., Calligaro, G. L., & Glanville, A. R. (2017). Acute rejection. Journal of Thoracic
Disease, 9(12), 5440–5457.
Demetris, A. J., Murase, N., Starzl, T. ., & Fung, J. J. (2014). Pathology of Chronic Rejection:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
RENAL TRANSPLANTATION 11
An Overview of Common Findings and Observations About Pathogenic Mechanisms and
Possible Prevention. Graft (Georgetown, Tex.), 1(2), 52–59.
Fletcher, J. T., Nankivell, B. J., & Alexander, S. I. (2013). Chronic allograft
neuropathy. Pediatric Nephrology (Berlin, Germany), 24(8), 1465–1471.
García, P., Huerfano, M., Rodríguez, M., Caicedo, A., Berrío, F., & Gonzalez, C. (2016). Acute
Rejection in Renal Transplant Patients of a Hospital in Bogota, Colombia. International
Journal of Organ Transplantation Medicine, 7(3), 161–166.
Ghadami, A., Memarian, R., Mohamadi, E., & Abdoli, S. (2012). Patients’ experiences from
Their received education about the process of kidney transplant: A qualitative
study. Iranian Journal of Nursing and Midwifery Research, 17(2 Suppl1), S157–S164.
Ingulli, E. (2013). Mechanism of cellular rejection in transplantation. Pediatric Nephrology
(Berlin, Germany), 25(1), 61–74.
Kloc, M., & Ghobrial, R. M. (2014). Chronic allograft rejection: A significant hurdle to
transplant success. Burns & Trauma, 2(1), 3–10.
Leblanc, J., Subrt, P., Paré, M., Hartell, D., Sénécal, L., Blydt-Hansen, T., & Cardinal, H. (2018).
Practice Patterns in the Treatment and Monitoring of Acute T Cell-Mediated Kidney
Graft Rejection in Canada. Canadian Journal of Kidney Health and Disease, 5.
Moreau, A., Varey, E., Anegon, I., & Cuturi, M.-C. (2013). Effector Mechanisms of
Rejection. Cold Spring Harbor Perspectives in Medicine, 3(11), a015461.
Patel, M. D., Young, S. W., Kriegshauser, J. S., & Dahiya, N. (2018). Ultrasound-guided renal
transplant biopsy: practical and pragmatic considerations. Abdominal Radiology, 1-7.
Reyna-Sepúlveda, F., Ponce-Escobedo, A., Guevara-Charles, A., Escobedo-Villarreal, M., Pérez-
An Overview of Common Findings and Observations About Pathogenic Mechanisms and
Possible Prevention. Graft (Georgetown, Tex.), 1(2), 52–59.
Fletcher, J. T., Nankivell, B. J., & Alexander, S. I. (2013). Chronic allograft
neuropathy. Pediatric Nephrology (Berlin, Germany), 24(8), 1465–1471.
García, P., Huerfano, M., Rodríguez, M., Caicedo, A., Berrío, F., & Gonzalez, C. (2016). Acute
Rejection in Renal Transplant Patients of a Hospital in Bogota, Colombia. International
Journal of Organ Transplantation Medicine, 7(3), 161–166.
Ghadami, A., Memarian, R., Mohamadi, E., & Abdoli, S. (2012). Patients’ experiences from
Their received education about the process of kidney transplant: A qualitative
study. Iranian Journal of Nursing and Midwifery Research, 17(2 Suppl1), S157–S164.
Ingulli, E. (2013). Mechanism of cellular rejection in transplantation. Pediatric Nephrology
(Berlin, Germany), 25(1), 61–74.
Kloc, M., & Ghobrial, R. M. (2014). Chronic allograft rejection: A significant hurdle to
transplant success. Burns & Trauma, 2(1), 3–10.
Leblanc, J., Subrt, P., Paré, M., Hartell, D., Sénécal, L., Blydt-Hansen, T., & Cardinal, H. (2018).
Practice Patterns in the Treatment and Monitoring of Acute T Cell-Mediated Kidney
Graft Rejection in Canada. Canadian Journal of Kidney Health and Disease, 5.
Moreau, A., Varey, E., Anegon, I., & Cuturi, M.-C. (2013). Effector Mechanisms of
Rejection. Cold Spring Harbor Perspectives in Medicine, 3(11), a015461.
Patel, M. D., Young, S. W., Kriegshauser, J. S., & Dahiya, N. (2018). Ultrasound-guided renal
transplant biopsy: practical and pragmatic considerations. Abdominal Radiology, 1-7.
Reyna-Sepúlveda, F., Ponce-Escobedo, A., Guevara-Charles, A., Escobedo-Villarreal, M., Pérez-
RENAL TRANSPLANTATION 12
Rodríguez, E., Muñoz-Maldonado, G., & Hernández-Guedea, M. (2017). Outcomes and Surgical
Complications in Kidney Transplantation. International Journal of Organ
Transplantation Medicine, 8(2), 78–84.
Wang, W., van Lint, C. L., Brinkman, W.-P., Rövekamp, T. J. M., van Dijk, S., van der Boog, P.
J. M., & Neerincx, M. A. (2017). Renal transplant patient acceptance of a self-
management support system. BMC Medical Informatics and Decision Making, 17, 58.
Whittier, W. L., & Korbet, S. M. (2016). Indications for and complications of renal
biopsy. UpToDate, Waltham, MA.
Rodríguez, E., Muñoz-Maldonado, G., & Hernández-Guedea, M. (2017). Outcomes and Surgical
Complications in Kidney Transplantation. International Journal of Organ
Transplantation Medicine, 8(2), 78–84.
Wang, W., van Lint, C. L., Brinkman, W.-P., Rövekamp, T. J. M., van Dijk, S., van der Boog, P.
J. M., & Neerincx, M. A. (2017). Renal transplant patient acceptance of a self-
management support system. BMC Medical Informatics and Decision Making, 17, 58.
Whittier, W. L., & Korbet, S. M. (2016). Indications for and complications of renal
biopsy. UpToDate, Waltham, MA.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.