Detailed Analysis of Human Respiratory and Cardiac Systems Report
VerifiedAdded on 2023/01/19
|26
|3751
|23
Report
AI Summary
This report provides a comprehensive overview of the human respiratory and cardiac systems. It begins with an exploration of the respiratory system, detailing the structure and function of key components like the nasal cavity, trachea, bronchi, and alveoli, and explaining the processes of inspiration and expiration. The report then delves into the structure and function of the alveoli, emphasizing the conditions necessary for effective gas exchange. The second part of the report focuses on the circulatory system, describing the components of plasma, the structure and function of red blood cells, and the transport of oxygen and carbon dioxide in the blood. It includes an analysis of the oxygen dissociation curve and the factors influencing gas exchange. The final section examines the structure and function of arteries, veins, and capillaries, and provides a comparison of their features. The report also briefly touches upon the structure of the heart and the cardiac cycle. The report is well-researched and includes citations to support the information provided.

HUMAN RESPIRATORY AND CARDIAC SYSTEMS
Student`s Name
Course Name
Professor`s Name
Institutional Affiliation
6th April, 2019
1
Student`s Name
Course Name
Professor`s Name
Institutional Affiliation
6th April, 2019
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Task 1
1. Nasal Cavity
2. Bronchus
3. Bronchiole
4. Alveolar duct
5. Pharynx
6. Trachea
7. Bronchus
8. Diaphragm
B ) Inspiration
2
1. Nasal Cavity
2. Bronchus
3. Bronchiole
4. Alveolar duct
5. Pharynx
6. Trachea
7. Bronchus
8. Diaphragm
B ) Inspiration
2
Rijnberk and Stokhof (2009, p 63-74) explain the process of inspiration. Respiration
occurs due to the movements of the respiratory muscles, the internal and external
intercostal muscles along with the diaphragm. During inspiration, the diaphragm
contracts, the internal intercostal muscles relax while the external intercostal muscles
contract thereby causing the rib cage to expand and move outward leading to an
increase in the volume of the thoracic cavity. This increase in the volume of the lungs
leads to a decrease in intra-alveolar pressure making it lower than atmospheric
pressure. The pressure accumulated then drives air into the lungs.
Expiration
During expiration, the diaphragm relaxes, the external intercostal muscles relax
whereas the internal intercostal muscles contract. This causes the ribcage to move
inwards and exerting pressure on the lungs. The effect is that the interpulmonary
pressure in the chest cavity rises above the atmospheric pressure, causing air to be
pushed out of the lungs.
3
occurs due to the movements of the respiratory muscles, the internal and external
intercostal muscles along with the diaphragm. During inspiration, the diaphragm
contracts, the internal intercostal muscles relax while the external intercostal muscles
contract thereby causing the rib cage to expand and move outward leading to an
increase in the volume of the thoracic cavity. This increase in the volume of the lungs
leads to a decrease in intra-alveolar pressure making it lower than atmospheric
pressure. The pressure accumulated then drives air into the lungs.
Expiration
During expiration, the diaphragm relaxes, the external intercostal muscles relax
whereas the internal intercostal muscles contract. This causes the ribcage to move
inwards and exerting pressure on the lungs. The effect is that the interpulmonary
pressure in the chest cavity rises above the atmospheric pressure, causing air to be
pushed out of the lungs.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Figure 1: Inspiration and Expiration, Rijnberk, Stokhof(2009)
C
The trachea is a wide hollow tube that connects the larynx and the bronchi of
the lungs. It also allows the passage of air in and out of the lungs during the breathing
process. To perform its functions effectively, the trachea’s structure has certain
adaptations.
The trachea has a thin membranous wall which is made up of C-shaped rings of
cartilage. The rings of cartilage may be between 16 and 20 in number along the whole
4
C
The trachea is a wide hollow tube that connects the larynx and the bronchi of
the lungs. It also allows the passage of air in and out of the lungs during the breathing
process. To perform its functions effectively, the trachea’s structure has certain
adaptations.
The trachea has a thin membranous wall which is made up of C-shaped rings of
cartilage. The rings of cartilage may be between 16 and 20 in number along the whole
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
length of the trachea. These rings of cartilage provide support to the trachea and keep
it open at all times for efficient airflow.
The walls of the trachea are made up of four walls of specialized tissues:
1. The Mucosa: it is the innermost layer and is made up of ciliated pseudostratified
columnar epithelium with numerous goblet cells. Goblet cells produce mucus, a sticky
substance that covers the inner lining of the trachea, used to trap any debris and
particles that may be in inhaled air before the particles reach the lungs. On the surface
of the columnar cells are cilia that work together in a rhythmic movement hence
pushing the mucous along with the trapped debris away from the lungs to the larynx
where it is either swallowed or expelled through coughing.
2. The Submucosa layer: this is a layer just below the mucosa. This layer of tissue
consists of areolar connective tissue containing blood vessels and the nervous tissue.
The collagen, elastic and reticular protein fibers provide support and elasticity to the
tracheal walls (Barclay, 2018). The blood vessels and nerves, on the other hand,
support the other layers of the tracheal wall. For the trachea to be able to adjust its
diameter appropriately, there are longitudinal smooth muscle fibers on the outside
trachea between the rings of cartilage.
3. Hyaline Cartilage: this is a layer surrounding the submucosa, and it forms the
supportive rings of the trachea. It also forms a strong and flexible structure that helps
in maintaining an open airway in the trachea while being resistant to external forces.
4. The Adventitia: this is the outermost layer of the tracheal wall made up of areolar
connective tissue. It anchors the trachea loosely to other surrounding soft tissues
structures.
D)
5
it open at all times for efficient airflow.
The walls of the trachea are made up of four walls of specialized tissues:
1. The Mucosa: it is the innermost layer and is made up of ciliated pseudostratified
columnar epithelium with numerous goblet cells. Goblet cells produce mucus, a sticky
substance that covers the inner lining of the trachea, used to trap any debris and
particles that may be in inhaled air before the particles reach the lungs. On the surface
of the columnar cells are cilia that work together in a rhythmic movement hence
pushing the mucous along with the trapped debris away from the lungs to the larynx
where it is either swallowed or expelled through coughing.
2. The Submucosa layer: this is a layer just below the mucosa. This layer of tissue
consists of areolar connective tissue containing blood vessels and the nervous tissue.
The collagen, elastic and reticular protein fibers provide support and elasticity to the
tracheal walls (Barclay, 2018). The blood vessels and nerves, on the other hand,
support the other layers of the tracheal wall. For the trachea to be able to adjust its
diameter appropriately, there are longitudinal smooth muscle fibers on the outside
trachea between the rings of cartilage.
3. Hyaline Cartilage: this is a layer surrounding the submucosa, and it forms the
supportive rings of the trachea. It also forms a strong and flexible structure that helps
in maintaining an open airway in the trachea while being resistant to external forces.
4. The Adventitia: this is the outermost layer of the tracheal wall made up of areolar
connective tissue. It anchors the trachea loosely to other surrounding soft tissues
structures.
D)
5

Structure and functions of the alveolus
The alveoli are only one cell thick in order to make the path of diffusion of oxygen
between alveoli and blood capillaries shorter.
An alveolar duct is a tube that is made up of connective tissue and smooth muscle and
opens up to a cluster of alveoli. A collection of many individual alveoli is known as
an alveolar sac (Biga et al. 2019).
Alveoli epithelium is composed of two types of cells, type 1 and type 2. Type 1 cells
make up about 95 percent of the surface and constitute mainly the air-blood barrier.
The type 1 cells form an epithelium that is attached to a thin elastic basement
membrane. The membrane is extremely thin and borders the capillary endothelial
membrane. These two epithelial membranes taken together form what is known as a
respiratory membrane, which is about 0.5mm, thick.it is across this membrane that
gaseous exchange occurs (Knudsen and Ochs, 2018).
6
The alveoli are only one cell thick in order to make the path of diffusion of oxygen
between alveoli and blood capillaries shorter.
An alveolar duct is a tube that is made up of connective tissue and smooth muscle and
opens up to a cluster of alveoli. A collection of many individual alveoli is known as
an alveolar sac (Biga et al. 2019).
Alveoli epithelium is composed of two types of cells, type 1 and type 2. Type 1 cells
make up about 95 percent of the surface and constitute mainly the air-blood barrier.
The type 1 cells form an epithelium that is attached to a thin elastic basement
membrane. The membrane is extremely thin and borders the capillary endothelial
membrane. These two epithelial membranes taken together form what is known as a
respiratory membrane, which is about 0.5mm, thick.it is across this membrane that
gaseous exchange occurs (Knudsen and Ochs, 2018).
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Type 2 cells are smaller in size than type 1 and they produce the surfactant that forms
the coating in the inside surface of the alveolus helping to reduce surface tension. It is
the surfactant that is responsible for maintaining the shape of the alveoli every time
you inhale and exhale. Type 2 alveoli cells may also turn into stem cells if need be.
(Hecht, 2018)
There are over 700million alveoli in the lungs to increase and maximise the surface
area for gaseous exchange. Alveoli also have thin and elastic walls that expand during
inhalation thereby increasing the surface area for gaseous exchange. They are
connected to each other by alveolar pores to maintain a steady pressure throughout the
lung.
The alveolar macrophage is a phagocytic cell that moves around the alveolus to
remove debris and pathogens that managed to find their way into the alveolus.
The internal environment of the alveoli is kept warm and moist for optimum gaseous
exchange to take place. Gases can only cross the cell membranes while they are
dissolved in water and therefore the alveolar membranes are always moist. (Eldridge,
2018)
Task 2:
a)
7
the coating in the inside surface of the alveolus helping to reduce surface tension. It is
the surfactant that is responsible for maintaining the shape of the alveoli every time
you inhale and exhale. Type 2 alveoli cells may also turn into stem cells if need be.
(Hecht, 2018)
There are over 700million alveoli in the lungs to increase and maximise the surface
area for gaseous exchange. Alveoli also have thin and elastic walls that expand during
inhalation thereby increasing the surface area for gaseous exchange. They are
connected to each other by alveolar pores to maintain a steady pressure throughout the
lung.
The alveolar macrophage is a phagocytic cell that moves around the alveolus to
remove debris and pathogens that managed to find their way into the alveolus.
The internal environment of the alveoli is kept warm and moist for optimum gaseous
exchange to take place. Gases can only cross the cell membranes while they are
dissolved in water and therefore the alveolar membranes are always moist. (Eldridge,
2018)
Task 2:
a)
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
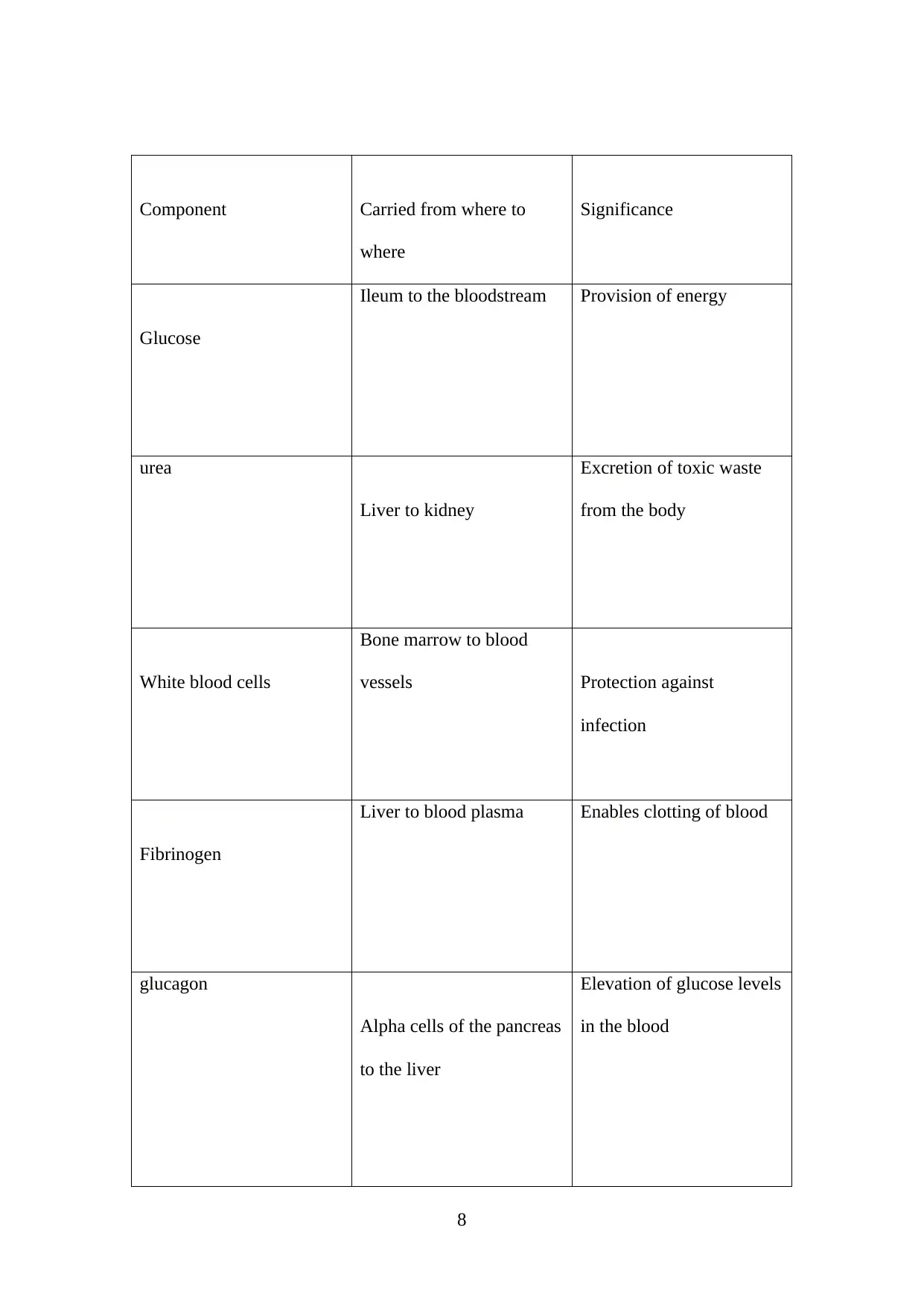
Component Carried from where to
where
Significance
Glucose
Ileum to the bloodstream Provision of energy
urea
Liver to kidney
Excretion of toxic waste
from the body
White blood cells
Bone marrow to blood
vessels Protection against
infection
Fibrinogen
Liver to blood plasma Enables clotting of blood
glucagon
Alpha cells of the pancreas
to the liver
Elevation of glucose levels
in the blood
8
where
Significance
Glucose
Ileum to the bloodstream Provision of energy
urea
Liver to kidney
Excretion of toxic waste
from the body
White blood cells
Bone marrow to blood
vessels Protection against
infection
Fibrinogen
Liver to blood plasma Enables clotting of blood
glucagon
Alpha cells of the pancreas
to the liver
Elevation of glucose levels
in the blood
8

Platelets
Bone marrow to the blood
vessels
Coagulation of blood
9
Bone marrow to the blood
vessels
Coagulation of blood
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

1. The biconcave shape of the red bool cells increases the surface area for oxygen
absorption
2. The red blood cells contain haemoglobin-a red protein that combines with oxygen to
form oxyhaemoglobin which is then transported to cells around the body
3. The red blood cells do not have a nucleus to pack more haemoglobin in the cells
b) The graph below shows the amount of oxygen carried by haemoglobin (% saturation)
at different concentrations of oxygen (partial pressure of oxygen ).
10
absorption
2. The red blood cells contain haemoglobin-a red protein that combines with oxygen to
form oxyhaemoglobin which is then transported to cells around the body
3. The red blood cells do not have a nucleus to pack more haemoglobin in the cells
b) The graph below shows the amount of oxygen carried by haemoglobin (% saturation)
at different concentrations of oxygen (partial pressure of oxygen ).
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

The partial pressure of any gas in a gaseous mixture is the equivalent to the amount of
pressure the same gas would exert if it occupied the space alone.
The partial pressure of oxygen is the measurement of oxygen in arterial blood and is
also known as PaO2. It is an indicator of how well oxygen can move from the lungs to
the bloodstream.
The alveolar gas equation is used to calculate alveolar oxygen pressure. The equation
is:
PAO2=(Patm-PH20) FiO2-PaCO2/RQ
This equation is used to calculate the driving force for diffusion of oxygen gases
across alveolar membranes, pulmonary capillary walls and into the arteriolar blood
flow for transportation by erythrocytes. (Leader, 2019)
The oxygen dissociation curve has the distinctive sigmoid shape due to the co-
operative binding of oxygen to the four polypeptide chains. This means that
haemoglobin has greater chances of binding with oxygen when a sub-unit has already
bound oxygen. Haemoglobin has its highest affinity for oxygen when 3 of the 4
polypeptide chains are bound to oxygen. There is a positive feedback effect whereby
loading oxygen accelerates the loading of more oxygen and this accounts for the
rapidly rising midpoint of the sigmoid curve. The graph plateaus when all four
11
pressure the same gas would exert if it occupied the space alone.
The partial pressure of oxygen is the measurement of oxygen in arterial blood and is
also known as PaO2. It is an indicator of how well oxygen can move from the lungs to
the bloodstream.
The alveolar gas equation is used to calculate alveolar oxygen pressure. The equation
is:
PAO2=(Patm-PH20) FiO2-PaCO2/RQ
This equation is used to calculate the driving force for diffusion of oxygen gases
across alveolar membranes, pulmonary capillary walls and into the arteriolar blood
flow for transportation by erythrocytes. (Leader, 2019)
The oxygen dissociation curve has the distinctive sigmoid shape due to the co-
operative binding of oxygen to the four polypeptide chains. This means that
haemoglobin has greater chances of binding with oxygen when a sub-unit has already
bound oxygen. Haemoglobin has its highest affinity for oxygen when 3 of the 4
polypeptide chains are bound to oxygen. There is a positive feedback effect whereby
loading oxygen accelerates the loading of more oxygen and this accounts for the
rapidly rising midpoint of the sigmoid curve. The graph plateaus when all four
11
polypeptide chains have loaded oxygen and the haemoglobin approaches 100%
saturation.
During exercise, a muscle produces more carbon dioxide while at the same
having a high oxygen affinity. In such a muscle, the partial pressure of carbon dioxide
increases while the partial pressure of oxygen decreases (Boulos and Schmidt, 2017,
p. 140).
Blood in the veins returning to the lungs will have a higher partial pressure of
carbon dioxide and a lower partial pressure of oxygen. The air in the alveoli, on the
other hand, has a higher partial pressure of oxygen and a lower partial pressure of
carbon dioxide. The effect of this will be an increase in the diffusion gradient for both
carbon dioxide and oxygen in the lungs and this will result in a more rapid and greater
amount of gaseous exchange. The high partial pressure of the oxygen in the alveoli
and relatively low partial pressure of oxygen in the blood ensures that haemoglobin is
almost fully saturated with oxygen and this leads to more oxygen being supplied to
the exercising muscles (Sharma and Rawat, 2019).
Arthurs and Sudhakar (2010, p 207-210) posit that transport of Carbon Dioxide in
the blood happens in three forms:
1. Dissolved in solution: Carbon dioxide obeys Henry’s Law that the number of
molecules in solution is proportional to the partial pressure at the liquid surface and it
is 20 times more soluble than oxygen. The partial pressure of Carbon Dioxide in
5.3pKa in arterial blood while it is 6.1pKa in mixed venous blood. Arterial blood will
12
saturation.
During exercise, a muscle produces more carbon dioxide while at the same
having a high oxygen affinity. In such a muscle, the partial pressure of carbon dioxide
increases while the partial pressure of oxygen decreases (Boulos and Schmidt, 2017,
p. 140).
Blood in the veins returning to the lungs will have a higher partial pressure of
carbon dioxide and a lower partial pressure of oxygen. The air in the alveoli, on the
other hand, has a higher partial pressure of oxygen and a lower partial pressure of
carbon dioxide. The effect of this will be an increase in the diffusion gradient for both
carbon dioxide and oxygen in the lungs and this will result in a more rapid and greater
amount of gaseous exchange. The high partial pressure of the oxygen in the alveoli
and relatively low partial pressure of oxygen in the blood ensures that haemoglobin is
almost fully saturated with oxygen and this leads to more oxygen being supplied to
the exercising muscles (Sharma and Rawat, 2019).
Arthurs and Sudhakar (2010, p 207-210) posit that transport of Carbon Dioxide in
the blood happens in three forms:
1. Dissolved in solution: Carbon dioxide obeys Henry’s Law that the number of
molecules in solution is proportional to the partial pressure at the liquid surface and it
is 20 times more soluble than oxygen. The partial pressure of Carbon Dioxide in
5.3pKa in arterial blood while it is 6.1pKa in mixed venous blood. Arterial blood will
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 26
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





