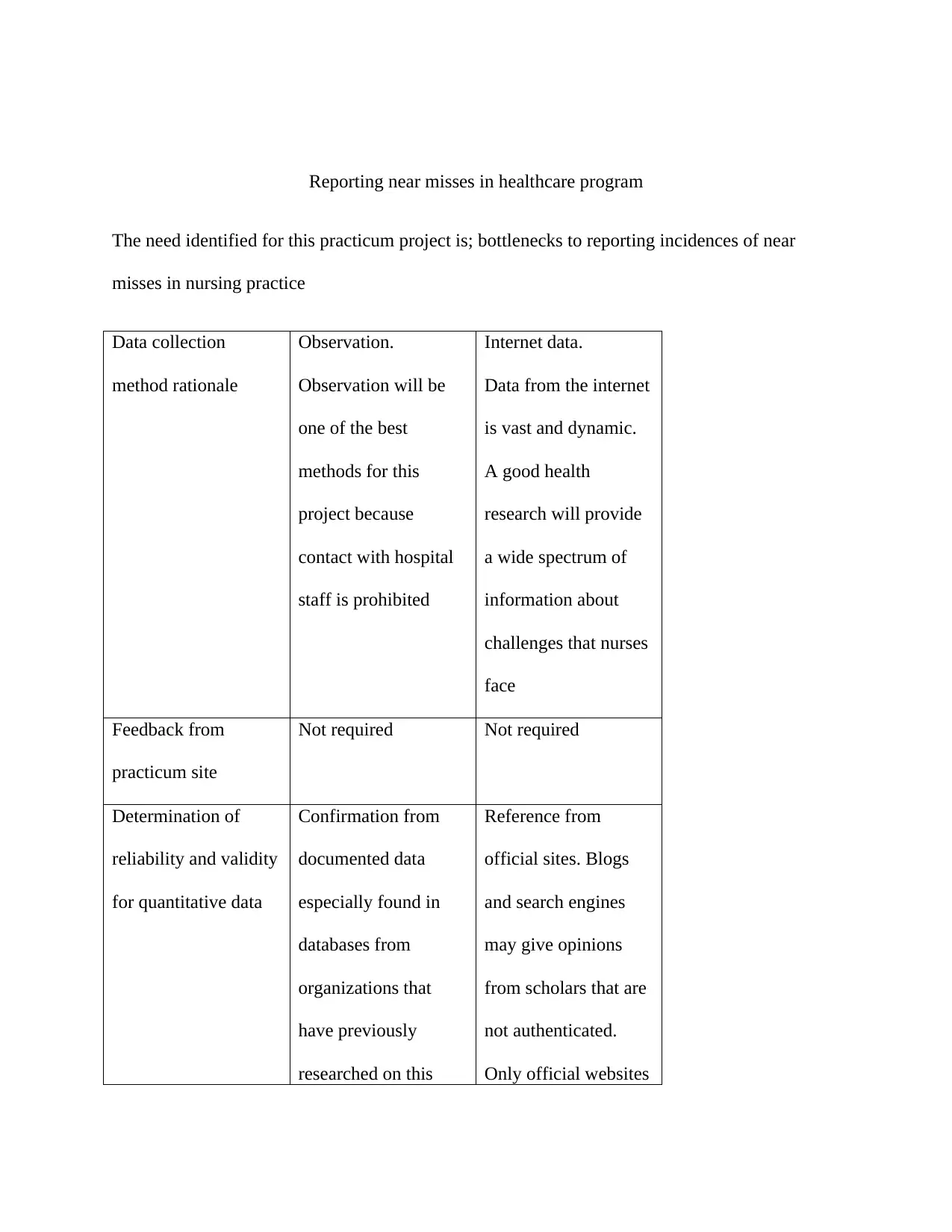
Healthcare Program Project: Reporting Near Misses Analysis
VerifiedAdded on 2020/03/16
|5
|1024
|260
Project
AI Summary
This project addresses the critical need for reporting near misses in nursing practice, highlighting bottlenecks and potential solutions. The methodology involves data collection through observation and internet research, with a focus on secondary data due to restrictions on direct hospital staff contact. The project assesses the return on investment (ROI) of improving patient care and nurse satisfaction, emphasizing the use of secondary data for cost-effectiveness. The findings suggest that the project has a positive ROI, focusing on qualitative gains and motivation for nurses. The project aims to improve patient care through feedback mechanisms, including direct communication with nurses and public dissemination via print media, which will facilitate discussions on healthcare policy decisions. The report references several studies supporting its claims and methodologies.
1 out of 5





![[object Object]](/_next/static/media/star-bottom.7253800d.svg)