Project: Resolve Spinal Fusion Management Problems with New Tech
VerifiedAdded on 2020/02/24
|13
|3456
|176
Project
AI Summary
This project delves into the project management aspects of bone substitutes used in vertebral fusion within spinal surgery. It addresses the limitations of traditional surgical procedures like bone allografts and explores innovative technologies such as bioactive glass to minimize infection risks. The project investigates research questions concerning infection control, new regulations, surgical guidelines, and healing problems. It aims to provide surgeons with new procedures and guidelines to reduce risks associated with spinal fusion, focusing on the benefits of bioactive materials in promoting bone regeneration and reducing complications. The literature review covers various bone graft substitutes, including demineralized bone matrix, ceramic materials, and tissue-engineered scaffolds. The project highlights the significance of bioactive glass in improving bone tissue stability and reducing bacterial growth, ultimately enhancing the efficiency of spinal fusion surgery. The outcomes emphasize the importance of bioactive materials in enhancing the efficiency of spinal fusion surgery and replacing damaged tissue.

Project
Resolve management problem associated with the spinal fusion by providing new techniques and
procedures
9/3/2017
Resolve management problem associated with the spinal fusion by providing new techniques and
procedures
9/3/2017
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Contents
Introduction:..........................................................................................................................................2
Background:..........................................................................................................................................2
Research questions:...............................................................................................................................3
Aims and objectives:.............................................................................................................................3
Literature Review:.................................................................................................................................3
Vertebral Fusion Process:......................................................................................................................6
Significance:..........................................................................................................................................6
Result and outcome:..............................................................................................................................8
Conclusion:............................................................................................................................................9
References:..........................................................................................................................................10
Appendix 1:.........................................................................................................................................12
Introduction:..........................................................................................................................................2
Background:..........................................................................................................................................2
Research questions:...............................................................................................................................3
Aims and objectives:.............................................................................................................................3
Literature Review:.................................................................................................................................3
Vertebral Fusion Process:......................................................................................................................6
Significance:..........................................................................................................................................6
Result and outcome:..............................................................................................................................8
Conclusion:............................................................................................................................................9
References:..........................................................................................................................................10
Appendix 1:.........................................................................................................................................12
Introduction:
This project focuses on the project management aspect of bone substitutes used to promote
vertebral fusion in spinal surgery. The surgical procedures used to correct spinal conditions
such as Adolescence Idiopathic Scoliosis (AIS) generally consist of titanium screws and rods
to confine spine deformation together with the use of bone grafts in order to promote
vertebral fusion. Spine surgery strongly depends on particular fusion technique of bone
allograft. The bone allograft is the surgical procedure which is commonly used for fixing the
bone problems. The bone allograft helps in fixing the bone which is damaged from trauma. It
is the most recommended practice for knee replacement. “There is some limitation in the
bone substitute methodology which is used to cure spine surgery” (Bae, 2017). The surgeons
are looking forward for the innovative technology which can minimise the risks of infection
associated with the bone surgery. The bioactive glass is used for providing structure,
mechanical strength, and architecture to the fractured bone. “It helps in promoting
regeneration of the damaged tissues because the bio active materials are made up of ceramic
and silicon oxide which are naturally present in the human body” (Wang, 2015). The purpose
of this project is to resolve management problems associated with the promotion of the
vertebral fusion for the assessment of bone substitute.
Background:
The traditional surgical procedures which are used for bone grafting are vertebral fusion,
bone allograft, and others. The vertebral fusion focuses on overcoming the problem
associated with the insertion of bone allograft into the allocated disc space. The bone
allograft helps in fixing the bone which is damaged from trauma. It is the most recommended
practice for knee replacement. The other common procedures which are used for bone
grafting are making use of intervertebral cages made of titanium or polymer. The lumbar
fusion is depends on bone morphogenetic protein which is the common substitute of crest
bone grafting surgery. The demand of spinal fusion is continuously increasing from last 10
years. The success of the long term fusion makes use of biological process by using surgical
fixation techniques. The risks which are associated with the spinal fusion are such as cause of
infection due to metallic fixation, difficulty in bone grafting during surgery, and the
dependence on the specific surgical techniques, addition of stress in the patient behaviour,
and others. “The migration of anterior grafting requires the repetition of the spinal surgery”
This project focuses on the project management aspect of bone substitutes used to promote
vertebral fusion in spinal surgery. The surgical procedures used to correct spinal conditions
such as Adolescence Idiopathic Scoliosis (AIS) generally consist of titanium screws and rods
to confine spine deformation together with the use of bone grafts in order to promote
vertebral fusion. Spine surgery strongly depends on particular fusion technique of bone
allograft. The bone allograft is the surgical procedure which is commonly used for fixing the
bone problems. The bone allograft helps in fixing the bone which is damaged from trauma. It
is the most recommended practice for knee replacement. “There is some limitation in the
bone substitute methodology which is used to cure spine surgery” (Bae, 2017). The surgeons
are looking forward for the innovative technology which can minimise the risks of infection
associated with the bone surgery. The bioactive glass is used for providing structure,
mechanical strength, and architecture to the fractured bone. “It helps in promoting
regeneration of the damaged tissues because the bio active materials are made up of ceramic
and silicon oxide which are naturally present in the human body” (Wang, 2015). The purpose
of this project is to resolve management problems associated with the promotion of the
vertebral fusion for the assessment of bone substitute.
Background:
The traditional surgical procedures which are used for bone grafting are vertebral fusion,
bone allograft, and others. The vertebral fusion focuses on overcoming the problem
associated with the insertion of bone allograft into the allocated disc space. The bone
allograft helps in fixing the bone which is damaged from trauma. It is the most recommended
practice for knee replacement. The other common procedures which are used for bone
grafting are making use of intervertebral cages made of titanium or polymer. The lumbar
fusion is depends on bone morphogenetic protein which is the common substitute of crest
bone grafting surgery. The demand of spinal fusion is continuously increasing from last 10
years. The success of the long term fusion makes use of biological process by using surgical
fixation techniques. The risks which are associated with the spinal fusion are such as cause of
infection due to metallic fixation, difficulty in bone grafting during surgery, and the
dependence on the specific surgical techniques, addition of stress in the patient behaviour,
and others. “The migration of anterior grafting requires the repetition of the spinal surgery”
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
(Sheikh, 2017). The PLIF or TLIF methodology should be adopt for placing the anterior
device anteriorly. The posterior approach is the safest approach which is used for carrying
over revision spine fusion surgery.
Research questions:
What the possible steps which should be taken to resolve the problem of infection
occurs in spinal surgery?
What are the new policies and regulations which are used to overcome the issues and
problems occurred in the spinal fusion?
What are the guidelines which should be adopted by the surgeons for providing
medication at the time of spinal surgery?
How to overcome the healing problem in spinal surgery?
What are the steps which should be followed by the surgeons to reduce the risks of
infection in the patient?
Which is the best approach used for providing spinal fusion? Why?
Aims and objectives:
The aim of this project is to resolve the management problem associated with the spinal
fusion by providing new guidelines and procedures to the surgeon to reduce the chance of
risks accompanied with the spinal surgery. The risks associated with the bone grafting are
transmission of the infectious disease, HIV, syphilis, and bacterial sepsis. The objective is to
provide a systematic architecture to handle the management problems associated with the
spinal surgery. The management tools and techniques help in improving the health conditions
of the patient by getting appropriate treatment within a short period of time.
Literature Review:
The complications are reported with the spinal fusion are occurrence of superficial
occurrence, seromas of superficial surgery, hematomas, vascular injuries, neurologic injuries,
pain related with the chronic donor, complication in wound reoperations, bone grafting is not
clearly done, and difficulty in carrying out daily activities. The traditional practices which are
used in the bone grafting are allograft bone, bone morphogenetic proteins, synthetic bone
substitutes, demineralized bone matrix, and cell based matrices. The key drivers which are
used for spinal fusion are categorised as joint reconstruction of spinal fusion, increasing rate
device anteriorly. The posterior approach is the safest approach which is used for carrying
over revision spine fusion surgery.
Research questions:
What the possible steps which should be taken to resolve the problem of infection
occurs in spinal surgery?
What are the new policies and regulations which are used to overcome the issues and
problems occurred in the spinal fusion?
What are the guidelines which should be adopted by the surgeons for providing
medication at the time of spinal surgery?
How to overcome the healing problem in spinal surgery?
What are the steps which should be followed by the surgeons to reduce the risks of
infection in the patient?
Which is the best approach used for providing spinal fusion? Why?
Aims and objectives:
The aim of this project is to resolve the management problem associated with the spinal
fusion by providing new guidelines and procedures to the surgeon to reduce the chance of
risks accompanied with the spinal surgery. The risks associated with the bone grafting are
transmission of the infectious disease, HIV, syphilis, and bacterial sepsis. The objective is to
provide a systematic architecture to handle the management problems associated with the
spinal surgery. The management tools and techniques help in improving the health conditions
of the patient by getting appropriate treatment within a short period of time.
Literature Review:
The complications are reported with the spinal fusion are occurrence of superficial
occurrence, seromas of superficial surgery, hematomas, vascular injuries, neurologic injuries,
pain related with the chronic donor, complication in wound reoperations, bone grafting is not
clearly done, and difficulty in carrying out daily activities. The traditional practices which are
used in the bone grafting are allograft bone, bone morphogenetic proteins, synthetic bone
substitutes, demineralized bone matrix, and cell based matrices. The key drivers which are
used for spinal fusion are categorised as joint reconstruction of spinal fusion, increasing rate
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
of obesity, continued efforts in the innovation of products, creation of comprehensive
platform for orthobiologics, searching materials for orthopaedic community, promoting
osteogenisis, promotion of osteo-inductivity, and improving accessibility of Bone Graft
Substitute (BGS) products. There are various bone graft substitute for spine fusion which are
classified as below:
Use of Demineralised bone matrix: The bone from which bone morphogenetic protein
is extracted is known as demineralised bone. “The process of acid extraction is
performed on allograft bone” (Sherman, 2016). The mineral elements are get lost
from the bone. The surgical repair process is used for bone grafting. The exploration
of the anterior spinal fusion is not generally recommended by the surgeons and
doctors.
Substitute based on ceramic material: The corals are used as a substitute in bone
grafting process. “Ceramic products are biodegradable in nature. It has a limited
compressive strength” (Spivak, 2016). The Ceramic scaffolds are made up of tri-
calcium phosphate. It is the effective technology in surgical repairs in carrying over
the spine fusion.
Concentration of Autologous platelet: The platelets degranulation helps in healing of
the fracture. Ultra concentration of platelet result into autologous growth factors. The
Autologous growth factors are responsible for enhancing the formation of new bone
in lumbar spine fusion.
Spine fusion based on Tissue engineered scaffolds: The applicability of tissue
engineering helps in enhancing the biomaterial scaffolds. The biocompatible materials
are developed which show physical and chemical properties of the associated native
tissues.
Gene Therapy: The hereditary disorders can be improved by performing gene therapy.
The sustainability can be achieved by transferring gene protein in the gene active
target cell. It is the cost effective technique which does not involve culturing of
autogenously cell.
The procedures of bone grafting are shifting from traditional approach to synthetic substitutes
of bone grafting. The bioactive materials are the synthetic silica based material which is used
for bone bonding. The bioactive materials are composed on calcium phosphates,
hydroxyapatite, and tri-calcium phosphates. “The rate of bioactivity is different for different
bioactive materials due to differences in composition” (Forsth, 2016). The reabsorption rate
platform for orthobiologics, searching materials for orthopaedic community, promoting
osteogenisis, promotion of osteo-inductivity, and improving accessibility of Bone Graft
Substitute (BGS) products. There are various bone graft substitute for spine fusion which are
classified as below:
Use of Demineralised bone matrix: The bone from which bone morphogenetic protein
is extracted is known as demineralised bone. “The process of acid extraction is
performed on allograft bone” (Sherman, 2016). The mineral elements are get lost
from the bone. The surgical repair process is used for bone grafting. The exploration
of the anterior spinal fusion is not generally recommended by the surgeons and
doctors.
Substitute based on ceramic material: The corals are used as a substitute in bone
grafting process. “Ceramic products are biodegradable in nature. It has a limited
compressive strength” (Spivak, 2016). The Ceramic scaffolds are made up of tri-
calcium phosphate. It is the effective technology in surgical repairs in carrying over
the spine fusion.
Concentration of Autologous platelet: The platelets degranulation helps in healing of
the fracture. Ultra concentration of platelet result into autologous growth factors. The
Autologous growth factors are responsible for enhancing the formation of new bone
in lumbar spine fusion.
Spine fusion based on Tissue engineered scaffolds: The applicability of tissue
engineering helps in enhancing the biomaterial scaffolds. The biocompatible materials
are developed which show physical and chemical properties of the associated native
tissues.
Gene Therapy: The hereditary disorders can be improved by performing gene therapy.
The sustainability can be achieved by transferring gene protein in the gene active
target cell. It is the cost effective technique which does not involve culturing of
autogenously cell.
The procedures of bone grafting are shifting from traditional approach to synthetic substitutes
of bone grafting. The bioactive materials are the synthetic silica based material which is used
for bone bonding. The bioactive materials are composed on calcium phosphates,
hydroxyapatite, and tri-calcium phosphates. “The rate of bioactivity is different for different
bioactive materials due to differences in composition” (Forsth, 2016). The reabsorption rate
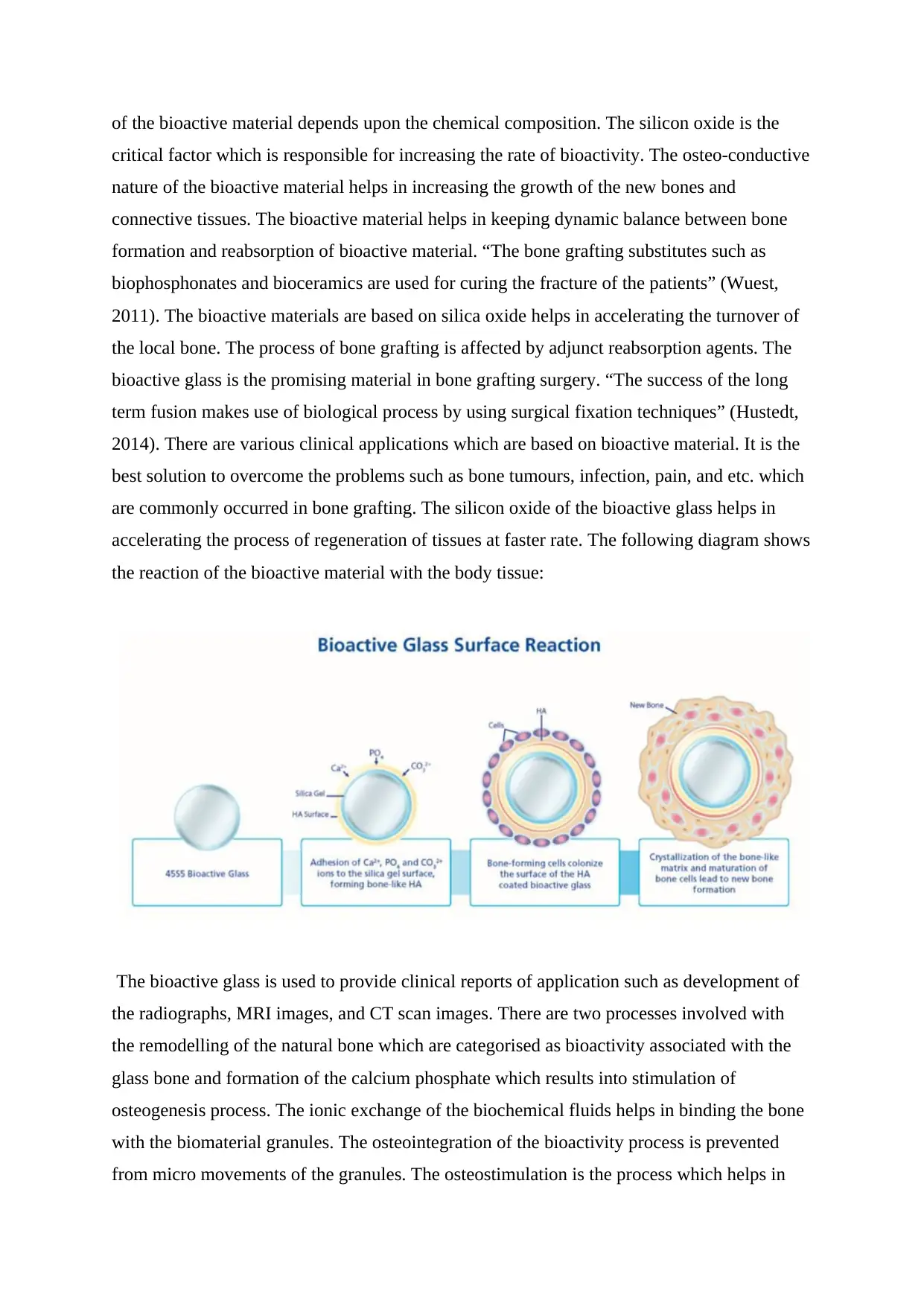
of the bioactive material depends upon the chemical composition. The silicon oxide is the
critical factor which is responsible for increasing the rate of bioactivity. The osteo-conductive
nature of the bioactive material helps in increasing the growth of the new bones and
connective tissues. The bioactive material helps in keeping dynamic balance between bone
formation and reabsorption of bioactive material. “The bone grafting substitutes such as
biophosphonates and bioceramics are used for curing the fracture of the patients” (Wuest,
2011). The bioactive materials are based on silica oxide helps in accelerating the turnover of
the local bone. The process of bone grafting is affected by adjunct reabsorption agents. The
bioactive glass is the promising material in bone grafting surgery. “The success of the long
term fusion makes use of biological process by using surgical fixation techniques” (Hustedt,
2014). There are various clinical applications which are based on bioactive material. It is the
best solution to overcome the problems such as bone tumours, infection, pain, and etc. which
are commonly occurred in bone grafting. The silicon oxide of the bioactive glass helps in
accelerating the process of regeneration of tissues at faster rate. The following diagram shows
the reaction of the bioactive material with the body tissue:
The bioactive glass is used to provide clinical reports of application such as development of
the radiographs, MRI images, and CT scan images. There are two processes involved with
the remodelling of the natural bone which are categorised as bioactivity associated with the
glass bone and formation of the calcium phosphate which results into stimulation of
osteogenesis process. The ionic exchange of the biochemical fluids helps in binding the bone
with the biomaterial granules. The osteointegration of the bioactivity process is prevented
from micro movements of the granules. The osteostimulation is the process which helps in
critical factor which is responsible for increasing the rate of bioactivity. The osteo-conductive
nature of the bioactive material helps in increasing the growth of the new bones and
connective tissues. The bioactive material helps in keeping dynamic balance between bone
formation and reabsorption of bioactive material. “The bone grafting substitutes such as
biophosphonates and bioceramics are used for curing the fracture of the patients” (Wuest,
2011). The bioactive materials are based on silica oxide helps in accelerating the turnover of
the local bone. The process of bone grafting is affected by adjunct reabsorption agents. The
bioactive glass is the promising material in bone grafting surgery. “The success of the long
term fusion makes use of biological process by using surgical fixation techniques” (Hustedt,
2014). There are various clinical applications which are based on bioactive material. It is the
best solution to overcome the problems such as bone tumours, infection, pain, and etc. which
are commonly occurred in bone grafting. The silicon oxide of the bioactive glass helps in
accelerating the process of regeneration of tissues at faster rate. The following diagram shows
the reaction of the bioactive material with the body tissue:
The bioactive glass is used to provide clinical reports of application such as development of
the radiographs, MRI images, and CT scan images. There are two processes involved with
the remodelling of the natural bone which are categorised as bioactivity associated with the
glass bone and formation of the calcium phosphate which results into stimulation of
osteogenesis process. The ionic exchange of the biochemical fluids helps in binding the bone
with the biomaterial granules. The osteointegration of the bioactivity process is prevented
from micro movements of the granules. The osteostimulation is the process which helps in
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
stimulating the differentiation and proliferation of the bone cell. The regeneration of the bone
is promoted by using the glass bone which results into the release of ions. This is the
innovative and safest technology to promote spinal fusion surgery. From the literature review,
we have concluded that there are various clinical situation in which bioactive glass plays an
important role in orthopaedic surgery.
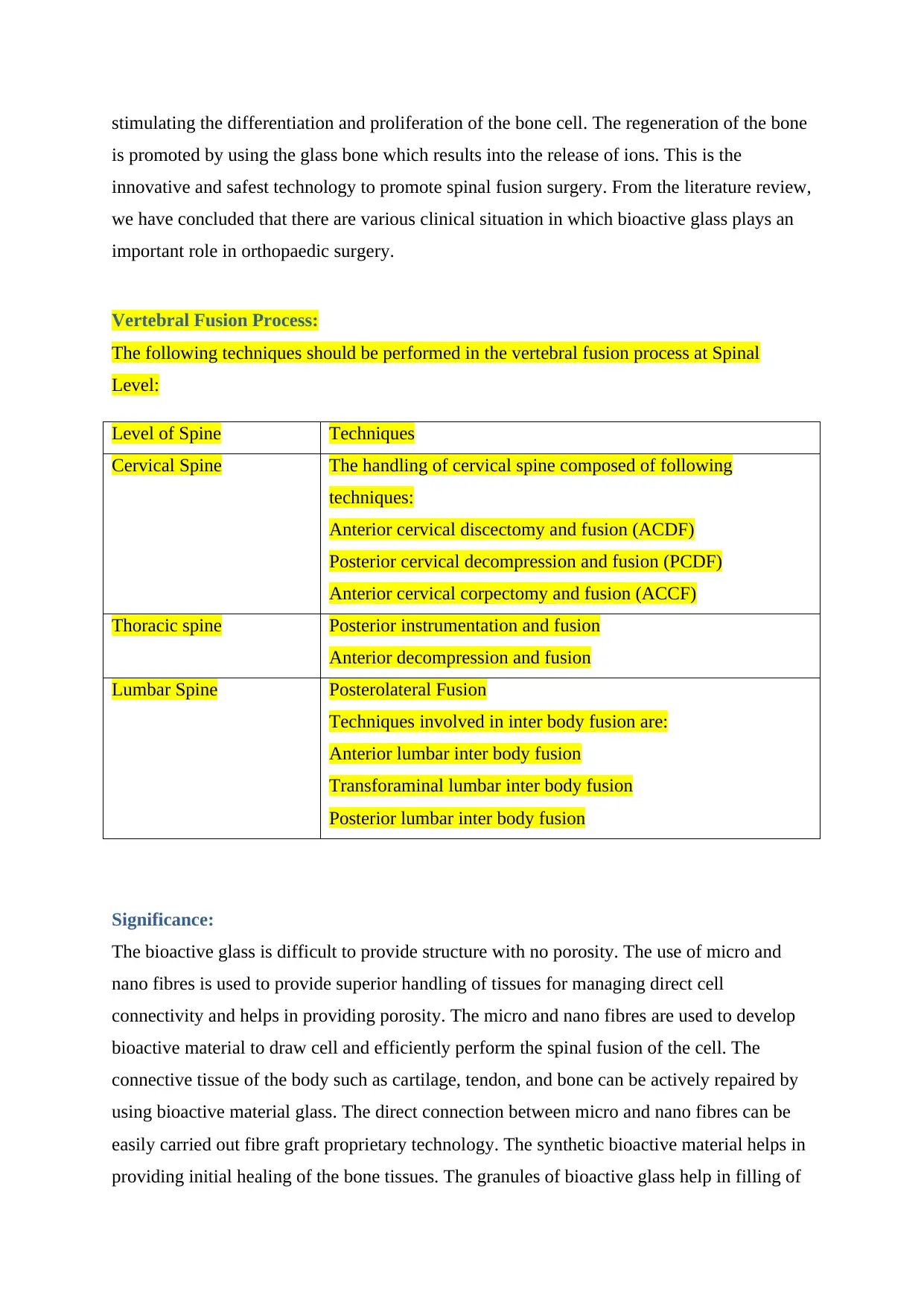
Vertebral Fusion Process:
The following techniques should be performed in the vertebral fusion process at Spinal
Level:
Level of Spine Techniques
Cervical Spine The handling of cervical spine composed of following
techniques:
Anterior cervical discectomy and fusion (ACDF)
Posterior cervical decompression and fusion (PCDF)
Anterior cervical corpectomy and fusion (ACCF)
Thoracic spine Posterior instrumentation and fusion
Anterior decompression and fusion
Lumbar Spine Posterolateral Fusion
Techniques involved in inter body fusion are:
Anterior lumbar inter body fusion
Transforaminal lumbar inter body fusion
Posterior lumbar inter body fusion
Significance:
The bioactive glass is difficult to provide structure with no porosity. The use of micro and
nano fibres is used to provide superior handling of tissues for managing direct cell
connectivity and helps in providing porosity. The micro and nano fibres are used to develop
bioactive material to draw cell and efficiently perform the spinal fusion of the cell. The
connective tissue of the body such as cartilage, tendon, and bone can be actively repaired by
using bioactive material glass. The direct connection between micro and nano fibres can be
easily carried out fibre graft proprietary technology. The synthetic bioactive material helps in
providing initial healing of the bone tissues. The granules of bioactive glass help in filling of
is promoted by using the glass bone which results into the release of ions. This is the
innovative and safest technology to promote spinal fusion surgery. From the literature review,
we have concluded that there are various clinical situation in which bioactive glass plays an
important role in orthopaedic surgery.
Vertebral Fusion Process:
The following techniques should be performed in the vertebral fusion process at Spinal
Level:
Level of Spine Techniques
Cervical Spine The handling of cervical spine composed of following
techniques:
Anterior cervical discectomy and fusion (ACDF)
Posterior cervical decompression and fusion (PCDF)
Anterior cervical corpectomy and fusion (ACCF)
Thoracic spine Posterior instrumentation and fusion
Anterior decompression and fusion
Lumbar Spine Posterolateral Fusion
Techniques involved in inter body fusion are:
Anterior lumbar inter body fusion
Transforaminal lumbar inter body fusion
Posterior lumbar inter body fusion
Significance:
The bioactive glass is difficult to provide structure with no porosity. The use of micro and
nano fibres is used to provide superior handling of tissues for managing direct cell
connectivity and helps in providing porosity. The micro and nano fibres are used to develop
bioactive material to draw cell and efficiently perform the spinal fusion of the cell. The
connective tissue of the body such as cartilage, tendon, and bone can be actively repaired by
using bioactive material glass. The direct connection between micro and nano fibres can be
easily carried out fibre graft proprietary technology. The synthetic bioactive material helps in
providing initial healing of the bone tissues. The granules of bioactive glass help in filling of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
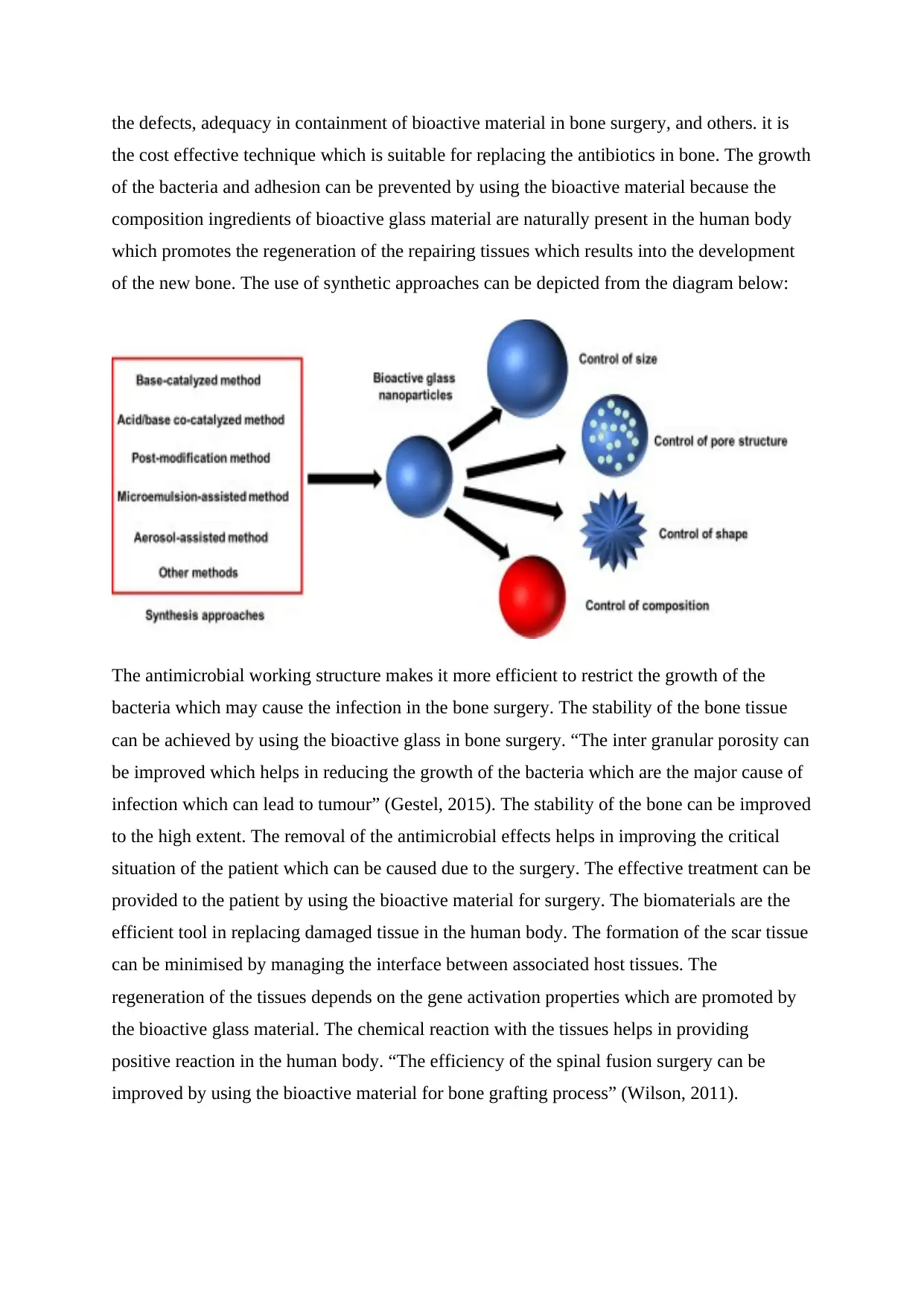
the defects, adequacy in containment of bioactive material in bone surgery, and others. it is
the cost effective technique which is suitable for replacing the antibiotics in bone. The growth
of the bacteria and adhesion can be prevented by using the bioactive material because the
composition ingredients of bioactive glass material are naturally present in the human body
which promotes the regeneration of the repairing tissues which results into the development
of the new bone. The use of synthetic approaches can be depicted from the diagram below:
The antimicrobial working structure makes it more efficient to restrict the growth of the
bacteria which may cause the infection in the bone surgery. The stability of the bone tissue
can be achieved by using the bioactive glass in bone surgery. “The inter granular porosity can
be improved which helps in reducing the growth of the bacteria which are the major cause of
infection which can lead to tumour” (Gestel, 2015). The stability of the bone can be improved
to the high extent. The removal of the antimicrobial effects helps in improving the critical
situation of the patient which can be caused due to the surgery. The effective treatment can be
provided to the patient by using the bioactive material for surgery. The biomaterials are the
efficient tool in replacing damaged tissue in the human body. The formation of the scar tissue
can be minimised by managing the interface between associated host tissues. The
regeneration of the tissues depends on the gene activation properties which are promoted by
the bioactive glass material. The chemical reaction with the tissues helps in providing
positive reaction in the human body. “The efficiency of the spinal fusion surgery can be
improved by using the bioactive material for bone grafting process” (Wilson, 2011).
the cost effective technique which is suitable for replacing the antibiotics in bone. The growth
of the bacteria and adhesion can be prevented by using the bioactive material because the
composition ingredients of bioactive glass material are naturally present in the human body
which promotes the regeneration of the repairing tissues which results into the development
of the new bone. The use of synthetic approaches can be depicted from the diagram below:
The antimicrobial working structure makes it more efficient to restrict the growth of the
bacteria which may cause the infection in the bone surgery. The stability of the bone tissue
can be achieved by using the bioactive glass in bone surgery. “The inter granular porosity can
be improved which helps in reducing the growth of the bacteria which are the major cause of
infection which can lead to tumour” (Gestel, 2015). The stability of the bone can be improved
to the high extent. The removal of the antimicrobial effects helps in improving the critical
situation of the patient which can be caused due to the surgery. The effective treatment can be
provided to the patient by using the bioactive material for surgery. The biomaterials are the
efficient tool in replacing damaged tissue in the human body. The formation of the scar tissue
can be minimised by managing the interface between associated host tissues. The
regeneration of the tissues depends on the gene activation properties which are promoted by
the bioactive glass material. The chemical reaction with the tissues helps in providing
positive reaction in the human body. “The efficiency of the spinal fusion surgery can be
improved by using the bioactive material for bone grafting process” (Wilson, 2011).
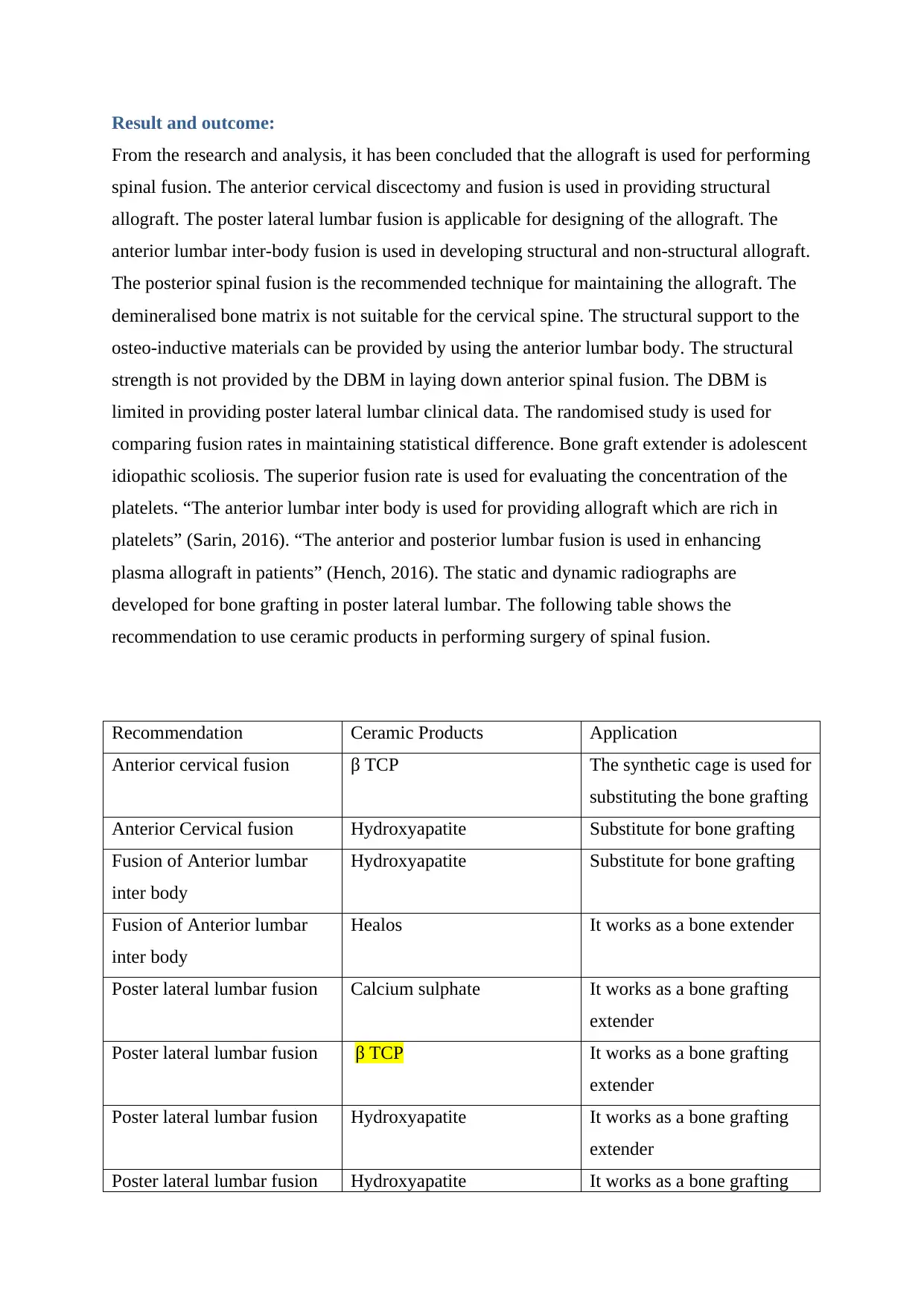
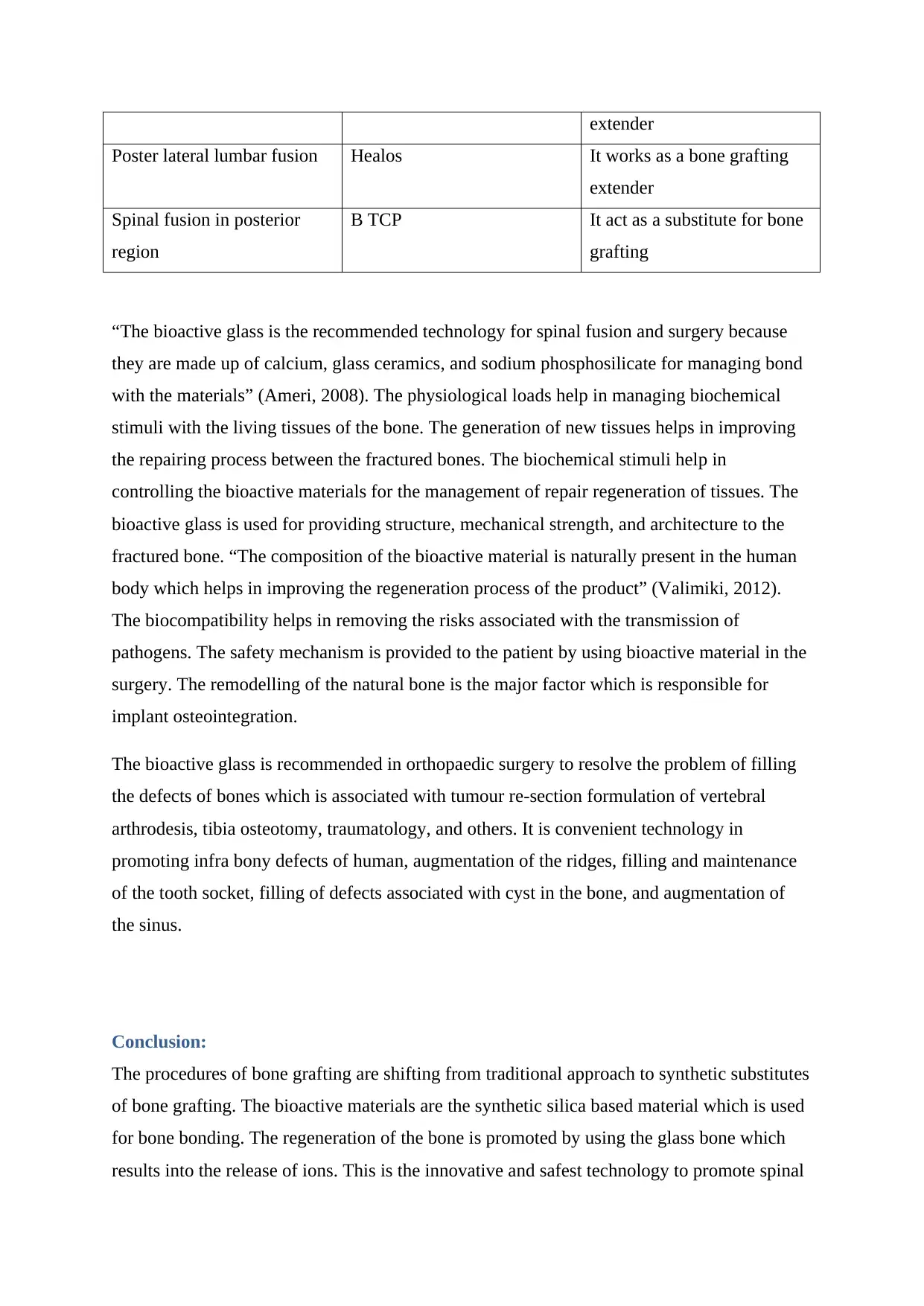
Result and outcome:
From the research and analysis, it has been concluded that the allograft is used for performing
spinal fusion. The anterior cervical discectomy and fusion is used in providing structural
allograft. The poster lateral lumbar fusion is applicable for designing of the allograft. The
anterior lumbar inter-body fusion is used in developing structural and non-structural allograft.
The posterior spinal fusion is the recommended technique for maintaining the allograft. The
demineralised bone matrix is not suitable for the cervical spine. The structural support to the
osteo-inductive materials can be provided by using the anterior lumbar body. The structural
strength is not provided by the DBM in laying down anterior spinal fusion. The DBM is
limited in providing poster lateral lumbar clinical data. The randomised study is used for
comparing fusion rates in maintaining statistical difference. Bone graft extender is adolescent
idiopathic scoliosis. The superior fusion rate is used for evaluating the concentration of the
platelets. “The anterior lumbar inter body is used for providing allograft which are rich in
platelets” (Sarin, 2016). “The anterior and posterior lumbar fusion is used in enhancing
plasma allograft in patients” (Hench, 2016). The static and dynamic radiographs are
developed for bone grafting in poster lateral lumbar. The following table shows the
recommendation to use ceramic products in performing surgery of spinal fusion.
Recommendation Ceramic Products Application
Anterior cervical fusion β TCP The synthetic cage is used for
substituting the bone grafting
Anterior Cervical fusion Hydroxyapatite Substitute for bone grafting
Fusion of Anterior lumbar
inter body
Hydroxyapatite Substitute for bone grafting
Fusion of Anterior lumbar
inter body
Healos It works as a bone extender
Poster lateral lumbar fusion Calcium sulphate It works as a bone grafting
extender
Poster lateral lumbar fusion β TCP It works as a bone grafting
extender
Poster lateral lumbar fusion Hydroxyapatite It works as a bone grafting
extender
Poster lateral lumbar fusion Hydroxyapatite It works as a bone grafting
From the research and analysis, it has been concluded that the allograft is used for performing
spinal fusion. The anterior cervical discectomy and fusion is used in providing structural
allograft. The poster lateral lumbar fusion is applicable for designing of the allograft. The
anterior lumbar inter-body fusion is used in developing structural and non-structural allograft.
The posterior spinal fusion is the recommended technique for maintaining the allograft. The
demineralised bone matrix is not suitable for the cervical spine. The structural support to the
osteo-inductive materials can be provided by using the anterior lumbar body. The structural
strength is not provided by the DBM in laying down anterior spinal fusion. The DBM is
limited in providing poster lateral lumbar clinical data. The randomised study is used for
comparing fusion rates in maintaining statistical difference. Bone graft extender is adolescent
idiopathic scoliosis. The superior fusion rate is used for evaluating the concentration of the
platelets. “The anterior lumbar inter body is used for providing allograft which are rich in
platelets” (Sarin, 2016). “The anterior and posterior lumbar fusion is used in enhancing
plasma allograft in patients” (Hench, 2016). The static and dynamic radiographs are
developed for bone grafting in poster lateral lumbar. The following table shows the
recommendation to use ceramic products in performing surgery of spinal fusion.
Recommendation Ceramic Products Application
Anterior cervical fusion β TCP The synthetic cage is used for
substituting the bone grafting
Anterior Cervical fusion Hydroxyapatite Substitute for bone grafting
Fusion of Anterior lumbar
inter body
Hydroxyapatite Substitute for bone grafting
Fusion of Anterior lumbar
inter body
Healos It works as a bone extender
Poster lateral lumbar fusion Calcium sulphate It works as a bone grafting
extender
Poster lateral lumbar fusion β TCP It works as a bone grafting
extender
Poster lateral lumbar fusion Hydroxyapatite It works as a bone grafting
extender
Poster lateral lumbar fusion Hydroxyapatite It works as a bone grafting
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
extender
Poster lateral lumbar fusion Healos It works as a bone grafting
extender
Spinal fusion in posterior
region
Β TCP It act as a substitute for bone
grafting
“The bioactive glass is the recommended technology for spinal fusion and surgery because
they are made up of calcium, glass ceramics, and sodium phosphosilicate for managing bond
with the materials” (Ameri, 2008). The physiological loads help in managing biochemical
stimuli with the living tissues of the bone. The generation of new tissues helps in improving
the repairing process between the fractured bones. The biochemical stimuli help in
controlling the bioactive materials for the management of repair regeneration of tissues. The
bioactive glass is used for providing structure, mechanical strength, and architecture to the
fractured bone. “The composition of the bioactive material is naturally present in the human
body which helps in improving the regeneration process of the product” (Valimiki, 2012).
The biocompatibility helps in removing the risks associated with the transmission of
pathogens. The safety mechanism is provided to the patient by using bioactive material in the
surgery. The remodelling of the natural bone is the major factor which is responsible for
implant osteointegration.
The bioactive glass is recommended in orthopaedic surgery to resolve the problem of filling
the defects of bones which is associated with tumour re-section formulation of vertebral
arthrodesis, tibia osteotomy, traumatology, and others. It is convenient technology in
promoting infra bony defects of human, augmentation of the ridges, filling and maintenance
of the tooth socket, filling of defects associated with cyst in the bone, and augmentation of
the sinus.
Conclusion:
The procedures of bone grafting are shifting from traditional approach to synthetic substitutes
of bone grafting. The bioactive materials are the synthetic silica based material which is used
for bone bonding. The regeneration of the bone is promoted by using the glass bone which
results into the release of ions. This is the innovative and safest technology to promote spinal
Poster lateral lumbar fusion Healos It works as a bone grafting
extender
Spinal fusion in posterior
region
Β TCP It act as a substitute for bone
grafting
“The bioactive glass is the recommended technology for spinal fusion and surgery because
they are made up of calcium, glass ceramics, and sodium phosphosilicate for managing bond
with the materials” (Ameri, 2008). The physiological loads help in managing biochemical
stimuli with the living tissues of the bone. The generation of new tissues helps in improving
the repairing process between the fractured bones. The biochemical stimuli help in
controlling the bioactive materials for the management of repair regeneration of tissues. The
bioactive glass is used for providing structure, mechanical strength, and architecture to the
fractured bone. “The composition of the bioactive material is naturally present in the human
body which helps in improving the regeneration process of the product” (Valimiki, 2012).
The biocompatibility helps in removing the risks associated with the transmission of
pathogens. The safety mechanism is provided to the patient by using bioactive material in the
surgery. The remodelling of the natural bone is the major factor which is responsible for
implant osteointegration.
The bioactive glass is recommended in orthopaedic surgery to resolve the problem of filling
the defects of bones which is associated with tumour re-section formulation of vertebral
arthrodesis, tibia osteotomy, traumatology, and others. It is convenient technology in
promoting infra bony defects of human, augmentation of the ridges, filling and maintenance
of the tooth socket, filling of defects associated with cyst in the bone, and augmentation of
the sinus.
Conclusion:
The procedures of bone grafting are shifting from traditional approach to synthetic substitutes
of bone grafting. The bioactive materials are the synthetic silica based material which is used
for bone bonding. The regeneration of the bone is promoted by using the glass bone which
results into the release of ions. This is the innovative and safest technology to promote spinal
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
fusion surgery. The purpose of this project is to resolve management problems associated
with the promotion of the vertebral fusion for the assessment of bone substitute. The
generation of new tissues helps in improving the repairing process between the fractured
bones. The bioactive glass is used for providing structure, mechanical strength, and
architecture to the fractured bone. The biomaterials are the efficient tool in replacing
damaged tissue in the human body. The formation of the scar tissue can be minimised by
managing the interface between associated host tissues. The healing of the fracture can be
effectively done due to the formation of new tissues and regeneration of the damaged tissue.
The silicon oxide of the bioactive glass helps in accelerating the process of regeneration of
tissues at faster rate. The research is going in the field of bioactive material to promote the
use of it in surgery so as to provide mechanism to the patients and helps in overcoming the
problem of infection. The bioactive material is the most promising technique which will be
used in near future for bone grafting.
References:
Ameri, E. (2008). Bioactive glass versus Autogenous Iliac crest bone in Adolescent
idiopathic Scoliosis surgery. Retrieved from
http://www.extera.com.br/osc/download/putty.pdf
Bae, H. (2017). Bioactive bone graft substitutes for spinal fusion. Retrieved from
http://www.sst7.org/media/BruceTuckman_Team_Development_Model.pdf
Forsth, P. (2016). A randomized controlled trial of fusion surgery for Lumbar spinal
stenosis. Retrieved from
http://www.nejm.org/doi/full/10.1056/NEJMoa1513721#t=article
Gestel, N. (2015). Clinical application of bioactive glass in bone healing and osteomeletic
treatment. Retrieved from https://www.hindawi.com/journals/bmri/2015/684826/
Hench, L. (2016). Bioactive glass bone grafts: History and clinical application. Retrieved
from https://link.springer.com/referenceworkentry/10.1007/978-3-319-12460-5_5
with the promotion of the vertebral fusion for the assessment of bone substitute. The
generation of new tissues helps in improving the repairing process between the fractured
bones. The bioactive glass is used for providing structure, mechanical strength, and
architecture to the fractured bone. The biomaterials are the efficient tool in replacing
damaged tissue in the human body. The formation of the scar tissue can be minimised by
managing the interface between associated host tissues. The healing of the fracture can be
effectively done due to the formation of new tissues and regeneration of the damaged tissue.
The silicon oxide of the bioactive glass helps in accelerating the process of regeneration of
tissues at faster rate. The research is going in the field of bioactive material to promote the
use of it in surgery so as to provide mechanism to the patients and helps in overcoming the
problem of infection. The bioactive material is the most promising technique which will be
used in near future for bone grafting.
References:
Ameri, E. (2008). Bioactive glass versus Autogenous Iliac crest bone in Adolescent
idiopathic Scoliosis surgery. Retrieved from
http://www.extera.com.br/osc/download/putty.pdf
Bae, H. (2017). Bioactive bone graft substitutes for spinal fusion. Retrieved from
http://www.sst7.org/media/BruceTuckman_Team_Development_Model.pdf
Forsth, P. (2016). A randomized controlled trial of fusion surgery for Lumbar spinal
stenosis. Retrieved from
http://www.nejm.org/doi/full/10.1056/NEJMoa1513721#t=article
Gestel, N. (2015). Clinical application of bioactive glass in bone healing and osteomeletic
treatment. Retrieved from https://www.hindawi.com/journals/bmri/2015/684826/
Hench, L. (2016). Bioactive glass bone grafts: History and clinical application. Retrieved
from https://link.springer.com/referenceworkentry/10.1007/978-3-319-12460-5_5
Hustedt, J. (2014). The controversy surrounding bone morphogenetic proteins in the spine: A
review of current research. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4257039/
Sarin, S. (2016). Bioactive glass: A potential next generation biomaterial. Retrieved from
http://www.srmjrds.in/article.asp?issn=0976-
433X;year=2016;volume=7;issue=1;spage=27;epage=32;aulast=Sarin
Sheikh, Z. (2017). Natural graft tissues and synthetic biomaterials for periodontal and
alveolar bone reconstructive application: A review. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5460509/
Sherman, J. (2016). Spinal fusion risks and complication. Retrieved from https://www.spine-
health.com/treatment/spinal-fusion/spine-fusion-risks-and-complications
Spivak, J. (2016). Evaluating the potential risks and consequences of spinal fusion. Retrieved
from https://www.spine-health.com/treatment/spinal-fusion/spine-fusion-risks-and-
complications
Valimiki, V. (2012). Molecular basis for action of bioactive glass as a bone substitute.
Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16821652
Wang, C. (2015). Bone grafts and substitutes- Global analysis and market forecasts.
Retrieved from https://www.marketresearch.com/product/sample-8021855.pdf
Wilson, C. (2011). Synthetic and bioactive bone graft substitute. Retrieved from
http://www.noraker.com/glassbone/en/
Wuest, W. (2011). Policy statement on Lumbar spinal fusion surgery. Retrieved from
http://www.isass.org/pdf/2011-07-15_policy_statement_lumbar_surgery.pdf
review of current research. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4257039/
Sarin, S. (2016). Bioactive glass: A potential next generation biomaterial. Retrieved from
http://www.srmjrds.in/article.asp?issn=0976-
433X;year=2016;volume=7;issue=1;spage=27;epage=32;aulast=Sarin
Sheikh, Z. (2017). Natural graft tissues and synthetic biomaterials for periodontal and
alveolar bone reconstructive application: A review. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5460509/
Sherman, J. (2016). Spinal fusion risks and complication. Retrieved from https://www.spine-
health.com/treatment/spinal-fusion/spine-fusion-risks-and-complications
Spivak, J. (2016). Evaluating the potential risks and consequences of spinal fusion. Retrieved
from https://www.spine-health.com/treatment/spinal-fusion/spine-fusion-risks-and-
complications
Valimiki, V. (2012). Molecular basis for action of bioactive glass as a bone substitute.
Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16821652
Wang, C. (2015). Bone grafts and substitutes- Global analysis and market forecasts.
Retrieved from https://www.marketresearch.com/product/sample-8021855.pdf
Wilson, C. (2011). Synthetic and bioactive bone graft substitute. Retrieved from
http://www.noraker.com/glassbone/en/
Wuest, W. (2011). Policy statement on Lumbar spinal fusion surgery. Retrieved from
http://www.isass.org/pdf/2011-07-15_policy_statement_lumbar_surgery.pdf
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


