Assessment 2: Pressure Injury Prevention and Management Policy Review
VerifiedAdded on 2023/06/07
|23
|4355
|237
Report
AI Summary
This report critically examines the NSW Health Pressure Injury Prevention and Management policy, aiming to identify areas for improvement in the context of enhancing health outcomes for older people. The report begins with an introduction to pressure injuries, their prevalence, and associated complications. It then provides an overview of the current policy, followed by a description of the consultation activities undertaken to update the policy, including identification of gaps, staff, patient and carer meetings, team formation, and construction of a draft policy. A comprehensive literature review supports the recommendations for policy updates, highlighting evidence-based strategies for pressure injury prevention and management. The report also outlines a plan for implementing the updated policy, including an action plan with tasks, resources, timeframes, and outcome measures. The report emphasizes the importance of education and training for healthcare providers to enhance their knowledge and skills in pressure injury prevention, ultimately aiming to improve patient safety and quality of care.

Assessment 2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Contents
Introduction 3
Overview of current policy 4
Consultation Activities 5
Identification of gaps 5
Staff, patient and carer meeting 5
Team formation and consultation 5
Construction of draft of internal policy 6
Expert staff review 6
Final version 6
Literature Review 7
Implementation of the policy 9
Pressure injury audit tools 11
Conclusion 11
References 12
Appendix A Updated Policy 14
1. POLICY STATEMENT 17
2. AIMS 17
3. TARGET AUDIENCE 17
4. RESPONSIBILITIES 18
5. DEFINITIONS 18
Introduction 3
Overview of current policy 4
Consultation Activities 5
Identification of gaps 5
Staff, patient and carer meeting 5
Team formation and consultation 5
Construction of draft of internal policy 6
Expert staff review 6
Final version 6
Literature Review 7
Implementation of the policy 9
Pressure injury audit tools 11
Conclusion 11
References 12
Appendix A Updated Policy 14
1. POLICY STATEMENT 17
2. AIMS 17
3. TARGET AUDIENCE 17
4. RESPONSIBILITIES 18
5. DEFINITIONS 18
6. DOCUMENTATION 18
7. REFERENCES 19
8. REVISION & APPROVAL HISTORY 19
Appendix 2 19
PATIENT ASSESSMENT TOOL 19
7. REFERENCES 19
8. REVISION & APPROVAL HISTORY 19
Appendix 2 19
PATIENT ASSESSMENT TOOL 19
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Introduction
Pressure injury is defined as a confined injury to the skin which may involve the deeper tissue
and is frequently found over a bony prominence due to pressure, shear and/or friction singly
or a combination of these reasons (Australian Wound Management Association, 2014). It is a
common hospital-acquired problem which affects between 9.5 to 17.6% of individuals in
hospital at any given point (Nguyen, Chaboyer, & Whitty, 2015). An estimated 4,313
pressure injuries occurred in patients in public hospitals of Australia in 2015–16. The rate of
hospital-acquired pressure injuries in hospitals of Australia was 9.7 injuries per 10,000
hospitalisations in 2015–16 (Australian Commission on Safety and Quality in Health Care,
2018). Pressure injury is also one of the major comorbidity associated with various illnesses
of old age. Healing of pressure injuries takes longer time which adversely affects the quality
of life of older people by inflicting pain, disturbed sleep, mood disturbance restricting
mobility, and susceptibility to infection (NSW Health; Clinical Excellence Commission,
2014). They also adversely affect rehabilitation, mobility and long-term quality of life
(Clinical Excellence Commission).
Pressure injuries prolong the time in hospitals that influences the older people negatively and
increase the cost of care both due to extension of stay in the health facility and/or more
advanced care needs (National Pressure Ulcer Advisory Panel; European Pressure Ulcer
Advisory Panel (NPUAP & EPUAP), 2009). The treatment cost across all states and severity
in 2012-13 was estimated to be A$983 million per annum. Research has demonstrated
decrease in incidence of pressure injury by some hospitals by taking preventive measures
(Miles, Fulbrook, Nowick, & Franks, 2013). It suggests that the hospital-acquired pressure
injuries can be prevented or reduced by providing patient care that mitigates avoidable
clinical risks to patients.
Pressure injury is defined as a confined injury to the skin which may involve the deeper tissue
and is frequently found over a bony prominence due to pressure, shear and/or friction singly
or a combination of these reasons (Australian Wound Management Association, 2014). It is a
common hospital-acquired problem which affects between 9.5 to 17.6% of individuals in
hospital at any given point (Nguyen, Chaboyer, & Whitty, 2015). An estimated 4,313
pressure injuries occurred in patients in public hospitals of Australia in 2015–16. The rate of
hospital-acquired pressure injuries in hospitals of Australia was 9.7 injuries per 10,000
hospitalisations in 2015–16 (Australian Commission on Safety and Quality in Health Care,
2018). Pressure injury is also one of the major comorbidity associated with various illnesses
of old age. Healing of pressure injuries takes longer time which adversely affects the quality
of life of older people by inflicting pain, disturbed sleep, mood disturbance restricting
mobility, and susceptibility to infection (NSW Health; Clinical Excellence Commission,
2014). They also adversely affect rehabilitation, mobility and long-term quality of life
(Clinical Excellence Commission).
Pressure injuries prolong the time in hospitals that influences the older people negatively and
increase the cost of care both due to extension of stay in the health facility and/or more
advanced care needs (National Pressure Ulcer Advisory Panel; European Pressure Ulcer
Advisory Panel (NPUAP & EPUAP), 2009). The treatment cost across all states and severity
in 2012-13 was estimated to be A$983 million per annum. Research has demonstrated
decrease in incidence of pressure injury by some hospitals by taking preventive measures
(Miles, Fulbrook, Nowick, & Franks, 2013). It suggests that the hospital-acquired pressure
injuries can be prevented or reduced by providing patient care that mitigates avoidable
clinical risks to patients.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
This report is prepared to appraise the pressure injury prevention and management policy to
assess the probable areas of improvement in context with improving health outcomes for
older people. The analysis of the policy will provide the review of policy along with
recommendations to update this policy. The review and recommendations will be supported
by review literature to support the evidence-based practice.
Overview of current policy
The critical review of the NSW Health Pressure injury prevention and management policy
(PD2014_007) (CEC, 2014), will emphasize on the education and awareness of care
providers involved in management of the pressure injury. This policy is publicised on March
24, 2014 and is due to be reviewed on March 24, 2019. This policy is derived from the best
practice guidelines corresponding with Pan Pacific Clinical Practice Guideline for the
Prevention and Management of Pressure Injury 2012 (Australian Wound Management
Association, 2012). The purpose of the policy is to reduce the prevalence of pressure injuries
to NSW Health patients (CEC, 2014). Prevention of hospital acquired pressure injury is a
work in progress. The National Safety and Quality Health Service Standards (NSQHS) are
significant means of improved outcomes provisions for elderly patients (Australian
Commission on Safety and Quality in Health Care, 2012). A recent survey in NSW revealed
that in spite of Standard 8, only 60% of patients went through a detailed risk assessment
involving skin assessment and a reliable tool within 8 hours of presentation to the hospital
( Clinical Excellence Commission, 2017). Prevention and management of pressure injury can
be achieved by acting upon the Prevention and Treatment of Pressure Ulcers: Clinical
Practice Guideline. These provide detailed guidance on the actions needed to prevent
pressure injury. However, for implementation of these Guidelines, an orgnaisational focus on
policies, leadership from management and education is required (Doggett & Buck, 2018).
assess the probable areas of improvement in context with improving health outcomes for
older people. The analysis of the policy will provide the review of policy along with
recommendations to update this policy. The review and recommendations will be supported
by review literature to support the evidence-based practice.
Overview of current policy
The critical review of the NSW Health Pressure injury prevention and management policy
(PD2014_007) (CEC, 2014), will emphasize on the education and awareness of care
providers involved in management of the pressure injury. This policy is publicised on March
24, 2014 and is due to be reviewed on March 24, 2019. This policy is derived from the best
practice guidelines corresponding with Pan Pacific Clinical Practice Guideline for the
Prevention and Management of Pressure Injury 2012 (Australian Wound Management
Association, 2012). The purpose of the policy is to reduce the prevalence of pressure injuries
to NSW Health patients (CEC, 2014). Prevention of hospital acquired pressure injury is a
work in progress. The National Safety and Quality Health Service Standards (NSQHS) are
significant means of improved outcomes provisions for elderly patients (Australian
Commission on Safety and Quality in Health Care, 2012). A recent survey in NSW revealed
that in spite of Standard 8, only 60% of patients went through a detailed risk assessment
involving skin assessment and a reliable tool within 8 hours of presentation to the hospital
( Clinical Excellence Commission, 2017). Prevention and management of pressure injury can
be achieved by acting upon the Prevention and Treatment of Pressure Ulcers: Clinical
Practice Guideline. These provide detailed guidance on the actions needed to prevent
pressure injury. However, for implementation of these Guidelines, an orgnaisational focus on
policies, leadership from management and education is required (Doggett & Buck, 2018).
Therefore, this policy should be updated to implement better pressure management practice
by skilled professionals and support evidence based practice.
Consultation Activities
While updating the policy, all the stakeholders were consulted.
Identification of gaps- One of the significant aspect, which is lacking in the
comprehensive care provision to pressure injury elderly patients, is the lack of knowledge
among practitioners. The issue is education and training of the practitioners to prevent or
minimise the development of pressure injuries among older people. This could be
implemented by updating a new policy which enhances evidence based practice
(Volunteering Australia, 2006).
Staff, patient and carer meeting: Regular meetings and debate among the staff members,
patients and carer is essential to provide and receive feedback on the existing policy. It will
offer clarity in information about the existing policy and strategies to prevent pressure
injuries. The question will help to assess the understanding level and knowledge on current
policy and prevention of pressure injury among older people. It will assist in determining the
areas which needs improvement regarding pressure injuries (UOW, n.d.).
Team formation and consultation: A team of health care providers, which must include
medical officer, pharmacist, physiotherapist, and nurses, will be developed. This team will
examine the current pressure injury prevention policy and impact of practitioner’s skill and
knowledge on its pressure injury management. This consultation team assists in exchanging
information for updating the policy (University of Southern Queensland, n.d.).
by skilled professionals and support evidence based practice.
Consultation Activities
While updating the policy, all the stakeholders were consulted.
Identification of gaps- One of the significant aspect, which is lacking in the
comprehensive care provision to pressure injury elderly patients, is the lack of knowledge
among practitioners. The issue is education and training of the practitioners to prevent or
minimise the development of pressure injuries among older people. This could be
implemented by updating a new policy which enhances evidence based practice
(Volunteering Australia, 2006).
Staff, patient and carer meeting: Regular meetings and debate among the staff members,
patients and carer is essential to provide and receive feedback on the existing policy. It will
offer clarity in information about the existing policy and strategies to prevent pressure
injuries. The question will help to assess the understanding level and knowledge on current
policy and prevention of pressure injury among older people. It will assist in determining the
areas which needs improvement regarding pressure injuries (UOW, n.d.).
Team formation and consultation: A team of health care providers, which must include
medical officer, pharmacist, physiotherapist, and nurses, will be developed. This team will
examine the current pressure injury prevention policy and impact of practitioner’s skill and
knowledge on its pressure injury management. This consultation team assists in exchanging
information for updating the policy (University of Southern Queensland, n.d.).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Construction of draft of internal policy: The experts in the team in health facilities will
develop the draft of new internal policy on pressure injury prevention based on the past
policy. In this way, the experts will update the policy on pressure injury prevention and
management. The updated policy will ensure safety and improve the care delivery associated
with pressure injury among older people. Older people will be provided with quality care and
services to maintain safety.
Expert staff review: The leaders, mangers and other experts in the team will review the
policy to ensure that it includes all the factors associated with care providers awareness for
pressure injury prevention practice. Further, the experts will also seek feedback to improve
the quality of care and make sure that the facility has met the goals and objectives for further
positive changes.
Final version: Lastly, the staff members and the expert team will make decision on final
version of pressure injury prevention policy. After decision-making, the updated policy will
be published in the internal system of institution as updated and modified version of pressure
injury prevention policy. Therefore, all the staff members in the health facility will be
informed about the updated policy and instructed to implement it in their practice. To make
the implementation of updated policy more effective the staff member will be given training
and educated. It will increase awareness among the staff to learn the new pressure injury
prevention policy to ensure evidence based practice to reduce the incidence of pressure
injuries.
develop the draft of new internal policy on pressure injury prevention based on the past
policy. In this way, the experts will update the policy on pressure injury prevention and
management. The updated policy will ensure safety and improve the care delivery associated
with pressure injury among older people. Older people will be provided with quality care and
services to maintain safety.
Expert staff review: The leaders, mangers and other experts in the team will review the
policy to ensure that it includes all the factors associated with care providers awareness for
pressure injury prevention practice. Further, the experts will also seek feedback to improve
the quality of care and make sure that the facility has met the goals and objectives for further
positive changes.
Final version: Lastly, the staff members and the expert team will make decision on final
version of pressure injury prevention policy. After decision-making, the updated policy will
be published in the internal system of institution as updated and modified version of pressure
injury prevention policy. Therefore, all the staff members in the health facility will be
informed about the updated policy and instructed to implement it in their practice. To make
the implementation of updated policy more effective the staff member will be given training
and educated. It will increase awareness among the staff to learn the new pressure injury
prevention policy to ensure evidence based practice to reduce the incidence of pressure
injuries.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Literature Review
A systematic review was conducted to identify the evidence based strategies of pressure
injury prevention and management among older people. Databases such as ProQuest and
CINHAL were used through University of Wollongong Library with full text English journal
articles from 2009 to 2018. The key words used to search the articles were ‘pressure injury
prevention’, ‘ pressure injury managment’, ‘pressure ulcer AND elderly people’ ‘knowledge
AND pressure injury’, etc. Out of 26 relevant articles, 7 articles are used to identify the
factors contributing in update of existing policy on pressure injury prevention with respect to
the need of education programs on pressure ulcer prevention for healthcare providers.
A cross sectional study was conducted to assess and compare the quality of life associated
with in elderly patients with pressure ulcers in home care, acute care facility, and long-term
care facility [LTCF]. The study found that the elderly patients with pressure ulcers exhibited
low scores on physical and social functioning and role physical and emotional. This finding
shows a need for an environment which includes health care professionals prepared to
execute strategies for pressure ulcer prevention (Maria, et al., 2015). Another study identifies
the need of a zero-tolerance policy by the primary physician and the nurse regarding pressure
ulcers. The study further suggests ongoing education of the healthcare providers and family
members for effective prevention and management of pressure ulcers (Jaul & Menzel, 2014).
Likewise, another study identified the need of educational program for healthcare providers.
The study suggested that prevention of pressure ulcers in frail older people is a complex task
and highlighted the significance of an organised educational programme that will include
efficient clinical leadership and interprofesssional teamwork (Barry & Nugent, 2015).
A PRIME trial was conducted which included a 15-month pre- and post-intervention study to
examine the efficacy of an unified pressure ulcer management framework including pressure
ulcer risk assessment tools, Australian Wound Management Association (AWMA)
A systematic review was conducted to identify the evidence based strategies of pressure
injury prevention and management among older people. Databases such as ProQuest and
CINHAL were used through University of Wollongong Library with full text English journal
articles from 2009 to 2018. The key words used to search the articles were ‘pressure injury
prevention’, ‘ pressure injury managment’, ‘pressure ulcer AND elderly people’ ‘knowledge
AND pressure injury’, etc. Out of 26 relevant articles, 7 articles are used to identify the
factors contributing in update of existing policy on pressure injury prevention with respect to
the need of education programs on pressure ulcer prevention for healthcare providers.
A cross sectional study was conducted to assess and compare the quality of life associated
with in elderly patients with pressure ulcers in home care, acute care facility, and long-term
care facility [LTCF]. The study found that the elderly patients with pressure ulcers exhibited
low scores on physical and social functioning and role physical and emotional. This finding
shows a need for an environment which includes health care professionals prepared to
execute strategies for pressure ulcer prevention (Maria, et al., 2015). Another study identifies
the need of a zero-tolerance policy by the primary physician and the nurse regarding pressure
ulcers. The study further suggests ongoing education of the healthcare providers and family
members for effective prevention and management of pressure ulcers (Jaul & Menzel, 2014).
Likewise, another study identified the need of educational program for healthcare providers.
The study suggested that prevention of pressure ulcers in frail older people is a complex task
and highlighted the significance of an organised educational programme that will include
efficient clinical leadership and interprofesssional teamwork (Barry & Nugent, 2015).
A PRIME trial was conducted which included a 15-month pre- and post-intervention study to
examine the efficacy of an unified pressure ulcer management framework including pressure
ulcer risk assessment tools, Australian Wound Management Association (AWMA)
guidelines, digital imaging and medical education in decreasing the incidence of pressure
ulcer in residential aged care facilities. The findings of the trial revealed that PRIME system
considerably decreased pressure ulcer incidence risk by 52%. The research concluded that the
combined system is effective in lowering pressure ulcer incidence in the frail elderly
population in residential aged care settings. It must be noted that one of the elements of the
PRIME intervention was Pressure ulcer prevention education programme so; the significance
of education program is established through this study (Santamaria, et al., 2009). A paper
supported this argument by presenting the results of a 5-year pressure ulcer prevention
programme at a Hospital in Australia. The programme consisted of several interventions and
three hospital-wide point prevalence surveys were done for progress evaluation. It revealed
that incidence of hospital-acquired pressure ulcers reduced from 6.6% in 2010 to 6% in 2012
and 2.5% in 2014. The findings exhibited the efficiency of the comprehensive programme of
pressure ulcer prevention which was based on research and education (Santamaria, et al.,
2015).
Nurses play a vital role in the prevention of pressure injuries therefore, a multi-
centered, cross-sectional study was done to evaluate the knowledge and attitude of nurses
towards pressure injury prevention evidence-based guidelines. Paper-based questionnaires
were asked to undergraduate nursing students in seven universities across five states of
Australia. Results revealed a lack of knowledge about prevention strategies to decrease the
amount and duration of pressure/shear, and lower confidence in their ability to prevent
pressure injury. Therefore, the study established the need of implementation of a detailed
approach to enhancing knowledge about pressure injury prevention and management
knowledge among Australian nurses (Usher, et al., 2018). Another study which was used to
examine knowledge of nurses about pressure ulcer management to identify knowledge gaps.
The findings revealed deficits in pressure ulcer knowledge among nurses (Lawrence,
ulcer in residential aged care facilities. The findings of the trial revealed that PRIME system
considerably decreased pressure ulcer incidence risk by 52%. The research concluded that the
combined system is effective in lowering pressure ulcer incidence in the frail elderly
population in residential aged care settings. It must be noted that one of the elements of the
PRIME intervention was Pressure ulcer prevention education programme so; the significance
of education program is established through this study (Santamaria, et al., 2009). A paper
supported this argument by presenting the results of a 5-year pressure ulcer prevention
programme at a Hospital in Australia. The programme consisted of several interventions and
three hospital-wide point prevalence surveys were done for progress evaluation. It revealed
that incidence of hospital-acquired pressure ulcers reduced from 6.6% in 2010 to 6% in 2012
and 2.5% in 2014. The findings exhibited the efficiency of the comprehensive programme of
pressure ulcer prevention which was based on research and education (Santamaria, et al.,
2015).
Nurses play a vital role in the prevention of pressure injuries therefore, a multi-
centered, cross-sectional study was done to evaluate the knowledge and attitude of nurses
towards pressure injury prevention evidence-based guidelines. Paper-based questionnaires
were asked to undergraduate nursing students in seven universities across five states of
Australia. Results revealed a lack of knowledge about prevention strategies to decrease the
amount and duration of pressure/shear, and lower confidence in their ability to prevent
pressure injury. Therefore, the study established the need of implementation of a detailed
approach to enhancing knowledge about pressure injury prevention and management
knowledge among Australian nurses (Usher, et al., 2018). Another study which was used to
examine knowledge of nurses about pressure ulcer management to identify knowledge gaps.
The findings revealed deficits in pressure ulcer knowledge among nurses (Lawrence,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Fulbrook, & Miles, 2015). Therefore, it can be concluded that there is a lack of knowledge
among healthcare providers regarding pressure injury prevention strategies and its guidelines.
So, it is justified to update the Pressure injury prevention and management policy to include
organized education programs in a firmer manner.
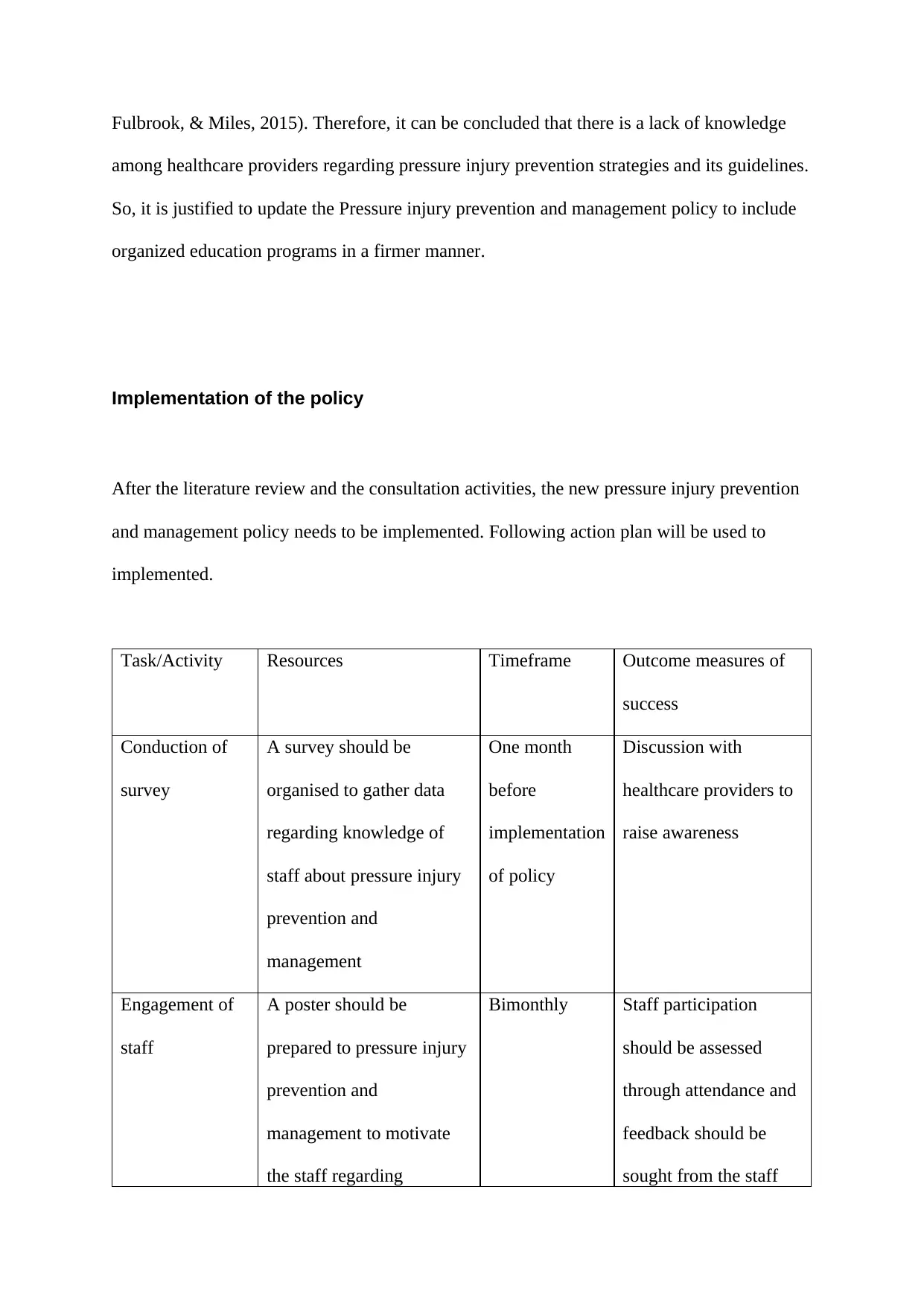
Implementation of the policy
After the literature review and the consultation activities, the new pressure injury prevention
and management policy needs to be implemented. Following action plan will be used to
implemented.
Task/Activity Resources Timeframe Outcome measures of
success
Conduction of
survey
A survey should be
organised to gather data
regarding knowledge of
staff about pressure injury
prevention and
management
One month
before
implementation
of policy
Discussion with
healthcare providers to
raise awareness
Engagement of
staff
A poster should be
prepared to pressure injury
prevention and
management to motivate
the staff regarding
Bimonthly Staff participation
should be assessed
through attendance and
feedback should be
sought from the staff
among healthcare providers regarding pressure injury prevention strategies and its guidelines.
So, it is justified to update the Pressure injury prevention and management policy to include
organized education programs in a firmer manner.
Implementation of the policy
After the literature review and the consultation activities, the new pressure injury prevention
and management policy needs to be implemented. Following action plan will be used to
implemented.
Task/Activity Resources Timeframe Outcome measures of
success
Conduction of
survey
A survey should be
organised to gather data
regarding knowledge of
staff about pressure injury
prevention and
management
One month
before
implementation
of policy
Discussion with
healthcare providers to
raise awareness
Engagement of
staff
A poster should be
prepared to pressure injury
prevention and
management to motivate
the staff regarding
Bimonthly Staff participation
should be assessed
through attendance and
feedback should be
sought from the staff
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
implementation of policy
in their practice
members
Provision of
training and
education
The training program and
education sessions will
assist in upgrading the
existing knowledge and
raising awareness
regarding pressure injury
prevention and
management among older
people
Monthly A questionnaire can be
prepared to evaluate
knowledge level of
knowledge among
nurses regarding new
policy adherence.
Conduction of
meeting
Meeting should be
organised for the
multidisciplinary team
members to deliberate
regarding the updated
policy and its impact on
the health outcomes of the
older people.
Biweekly Analysis should be
done to assess the
reduction in prevalence
of pressure injuries
among older people and
active participation in
prevention and
management.
Data collection Data should be collected
about incidence of pressure
injuries in older people
Once in a
month
Decrease in the number
of pressure injuries
Post-survey
conduction
A post-implementation
survey should be
conducted to evaluate the
After one
month of
implementation
Assessment of
improvement of
knowledge level on
in their practice
members
Provision of
training and
education
The training program and
education sessions will
assist in upgrading the
existing knowledge and
raising awareness
regarding pressure injury
prevention and
management among older
people
Monthly A questionnaire can be
prepared to evaluate
knowledge level of
knowledge among
nurses regarding new
policy adherence.
Conduction of
meeting
Meeting should be
organised for the
multidisciplinary team
members to deliberate
regarding the updated
policy and its impact on
the health outcomes of the
older people.
Biweekly Analysis should be
done to assess the
reduction in prevalence
of pressure injuries
among older people and
active participation in
prevention and
management.
Data collection Data should be collected
about incidence of pressure
injuries in older people
Once in a
month
Decrease in the number
of pressure injuries
Post-survey
conduction
A post-implementation
survey should be
conducted to evaluate the
After one
month of
implementation
Assessment of
improvement of
knowledge level on
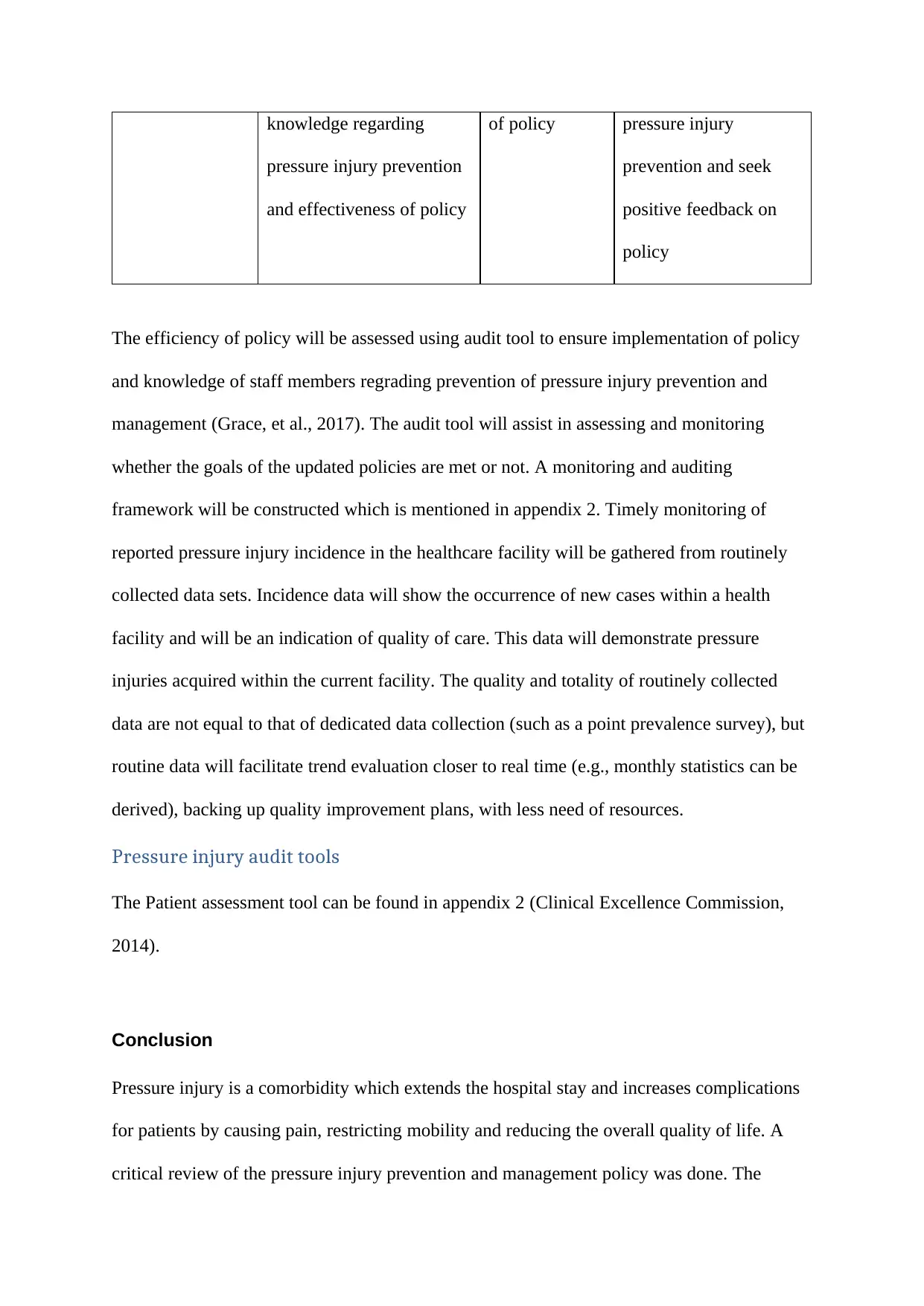
knowledge regarding
pressure injury prevention
and effectiveness of policy
of policy pressure injury
prevention and seek
positive feedback on
policy
The efficiency of policy will be assessed using audit tool to ensure implementation of policy
and knowledge of staff members regrading prevention of pressure injury prevention and
management (Grace, et al., 2017). The audit tool will assist in assessing and monitoring
whether the goals of the updated policies are met or not. A monitoring and auditing
framework will be constructed which is mentioned in appendix 2. Timely monitoring of
reported pressure injury incidence in the healthcare facility will be gathered from routinely
collected data sets. Incidence data will show the occurrence of new cases within a health
facility and will be an indication of quality of care. This data will demonstrate pressure
injuries acquired within the current facility. The quality and totality of routinely collected
data are not equal to that of dedicated data collection (such as a point prevalence survey), but
routine data will facilitate trend evaluation closer to real time (e.g., monthly statistics can be
derived), backing up quality improvement plans, with less need of resources.
Pressure injury audit tools
The Patient assessment tool can be found in appendix 2 (Clinical Excellence Commission,
2014).
Conclusion
Pressure injury is a comorbidity which extends the hospital stay and increases complications
for patients by causing pain, restricting mobility and reducing the overall quality of life. A
critical review of the pressure injury prevention and management policy was done. The
pressure injury prevention
and effectiveness of policy
of policy pressure injury
prevention and seek
positive feedback on
policy
The efficiency of policy will be assessed using audit tool to ensure implementation of policy
and knowledge of staff members regrading prevention of pressure injury prevention and
management (Grace, et al., 2017). The audit tool will assist in assessing and monitoring
whether the goals of the updated policies are met or not. A monitoring and auditing
framework will be constructed which is mentioned in appendix 2. Timely monitoring of
reported pressure injury incidence in the healthcare facility will be gathered from routinely
collected data sets. Incidence data will show the occurrence of new cases within a health
facility and will be an indication of quality of care. This data will demonstrate pressure
injuries acquired within the current facility. The quality and totality of routinely collected
data are not equal to that of dedicated data collection (such as a point prevalence survey), but
routine data will facilitate trend evaluation closer to real time (e.g., monthly statistics can be
derived), backing up quality improvement plans, with less need of resources.
Pressure injury audit tools
The Patient assessment tool can be found in appendix 2 (Clinical Excellence Commission,
2014).
Conclusion
Pressure injury is a comorbidity which extends the hospital stay and increases complications
for patients by causing pain, restricting mobility and reducing the overall quality of life. A
critical review of the pressure injury prevention and management policy was done. The
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 23
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





