Analyzing Rh System and Transfusion Reactions: A Comprehensive Report
VerifiedAdded on 2023/06/13
|15
|4427
|417
Report
AI Summary
This report examines the significance of the Rhesus (Rh) system in blood transfusion reactions, focusing on the role of Rh antibodies and their impact on hemolytic transfusion reactions. It reviews existing literature to understand the involvement of Rh antigens like D, C/c, and E/e in transfusion reactions, highlighting the importance of pre-transfusion antibody screening. The report also discusses the percentage of antibodies causing transfusion reactions, various techniques for early detection of problems, and potential policies to avoid such reactions. Key findings from cited studies include the prevalence of alloimmunization among different populations, the identification of specific antibodies (e.g., anti-E, anti-c) contributing to reactions, and the need for comprehensive compatibility testing. Ultimately, the report underscores the critical role of healthcare professionals in ensuring accurate patient identification and implementing system-based practices for the early detection and prevention of adverse transfusion events. Desklib provides access to this and other solved assignments to aid students.

Running head: BLOOD TRANSFUSION
Significant and relation between Rhesus system with transfusion reaction in blood bank
Name of the Student
Name of the University
Author Note
Significant and relation between Rhesus system with transfusion reaction in blood bank
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BLOOD TRANSFUSION
Table of Contents
Introduction................................................................................................................................2
Aim of the research....................................................................................................................3
Objective of the research............................................................................................................3
Review of Literature..................................................................................................................3
Significance of Rh system in blood transfusion cases............................................................3
Percentage of antibodies that cause blood transfusion reaction...........................................5
To examine different technique to detect problem early........................................................7
To create a new policy to avoid transfusion reaction............................................................8
Methodology............................................................................................................................10
Time Plan.................................................................................................................................10
Gantt Chart...........................................................................................................................10
References................................................................................................................................12
Table of Contents
Introduction................................................................................................................................2
Aim of the research....................................................................................................................3
Objective of the research............................................................................................................3
Review of Literature..................................................................................................................3
Significance of Rh system in blood transfusion cases............................................................3
Percentage of antibodies that cause blood transfusion reaction...........................................5
To examine different technique to detect problem early........................................................7
To create a new policy to avoid transfusion reaction............................................................8
Methodology............................................................................................................................10
Time Plan.................................................................................................................................10
Gantt Chart...........................................................................................................................10
References................................................................................................................................12
BLOOD TRANSFUSION
Introduction
Provision towards safe blood supply is the main responsibility for every transfusion
facility. Testing for the presence of infectious pathogens along with preventions towards
ABO blood group induced haemolytic transfusion reactions arising out of alloimmunization
is of the prime importance (Makroo, Agrawal & Chowdhry, 2017). However, the adverse
transfusion reaction arising out of the rhesus (Rh) system is gradually gaining immunogenic
significance in transfusion reaction after ABO blood group (Sachan et al., 2015). According
to the reports published by Vamvakas and Blajchman (2009), apart from haemolytic
transfusion reaction,, transfusion reactions is also regarded as a prime thereat towards the
development of transfusion related acute lung injury (TRALI) and transfusion-associated
sepsis. Rh antibody mediated haemolytic transfusion reactions results in extravascular
haemolysis along with delayed haemolytic transfusion reaction. The commonly reported Rh
antigens which are involved in eliciting transfusion reaction include Diego, Kidd and P-
antigens (Sachan et al., 2015). Apart from these anti-C RH antibodies is also gaining
prominence in the domain of haemolytic reaction (Sachan et al., 2015). However, relation
between the Rh antibody and intravascular haemolysis is unclear (Sachan et al., 2015). A
detailed analysis of the relationship between Rh antigen and transfusion reaction will be
important in generating proper action plan for the early detection of the transfusion reaction
and subsequent policy to implement transfusion reaction control measures.
Aim of the research
So the aim of this research is to study the relation and significant of Rh antibodies in blood
transfusion reaction cases.
Introduction
Provision towards safe blood supply is the main responsibility for every transfusion
facility. Testing for the presence of infectious pathogens along with preventions towards
ABO blood group induced haemolytic transfusion reactions arising out of alloimmunization
is of the prime importance (Makroo, Agrawal & Chowdhry, 2017). However, the adverse
transfusion reaction arising out of the rhesus (Rh) system is gradually gaining immunogenic
significance in transfusion reaction after ABO blood group (Sachan et al., 2015). According
to the reports published by Vamvakas and Blajchman (2009), apart from haemolytic
transfusion reaction,, transfusion reactions is also regarded as a prime thereat towards the
development of transfusion related acute lung injury (TRALI) and transfusion-associated
sepsis. Rh antibody mediated haemolytic transfusion reactions results in extravascular
haemolysis along with delayed haemolytic transfusion reaction. The commonly reported Rh
antigens which are involved in eliciting transfusion reaction include Diego, Kidd and P-
antigens (Sachan et al., 2015). Apart from these anti-C RH antibodies is also gaining
prominence in the domain of haemolytic reaction (Sachan et al., 2015). However, relation
between the Rh antibody and intravascular haemolysis is unclear (Sachan et al., 2015). A
detailed analysis of the relationship between Rh antigen and transfusion reaction will be
important in generating proper action plan for the early detection of the transfusion reaction
and subsequent policy to implement transfusion reaction control measures.
Aim of the research
So the aim of this research is to study the relation and significant of Rh antibodies in blood
transfusion reaction cases.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

BLOOD TRANSFUSION
Objective of the research
1- To study the significant of Rh system (D,d,E,e,C,c,Cw) in transfusion reaction cases
2- To determine the percentage of antibodies cause the reaction
3- To examine different technique to detect the problem early
4- To create a new policy to avoid transfusion reaction
Review of Literature
Significance of Rh system in blood transfusion cases
Rh system is classified into Rh-positive or negative based on the presence or absence
of antibodies in the blood. Five main Rh antigens are present on red blood cells for which an
individual can be either positive or negative: D, C/c, and E/e. The significance and need of
including antibody screening during pre-transfusion testing was validated by a study that
emphasised on the role of Rh mediated hemolytic transfusions delaying onset (Sachan et al.,
2015). Findings suggested that Rh antibodies belong to the IgG class of immunoglobulins are
found to exert no action on complement activation. Furthermore, a series of complement
activation gets initiated upon interaction of the antigen and antibody, provided the RBC
antibodies are capable of complement binding (Berséus et al., 2013). Similar findings were
presented by other studies that provided evidence for the role of Rh antigen-antibody reaction
in case of hemolytic transfusions (Tanhehco & Berns, 2012). Evidences further suggest that
acute forms of hemolytic reactions occur upon interaction of the transfused RBCs with the
antibodies that have been performed in the recipients.
Several cases of AHTR were also reported by studies that established its correlation
with multiple alloantibodies, which led to the development of intravascular hemolysis. Other
research articles, also confirmed association between hemolyyic disease of newborns and
Objective of the research
1- To study the significant of Rh system (D,d,E,e,C,c,Cw) in transfusion reaction cases
2- To determine the percentage of antibodies cause the reaction
3- To examine different technique to detect the problem early
4- To create a new policy to avoid transfusion reaction
Review of Literature
Significance of Rh system in blood transfusion cases
Rh system is classified into Rh-positive or negative based on the presence or absence
of antibodies in the blood. Five main Rh antigens are present on red blood cells for which an
individual can be either positive or negative: D, C/c, and E/e. The significance and need of
including antibody screening during pre-transfusion testing was validated by a study that
emphasised on the role of Rh mediated hemolytic transfusions delaying onset (Sachan et al.,
2015). Findings suggested that Rh antibodies belong to the IgG class of immunoglobulins are
found to exert no action on complement activation. Furthermore, a series of complement
activation gets initiated upon interaction of the antigen and antibody, provided the RBC
antibodies are capable of complement binding (Berséus et al., 2013). Similar findings were
presented by other studies that provided evidence for the role of Rh antigen-antibody reaction
in case of hemolytic transfusions (Tanhehco & Berns, 2012). Evidences further suggest that
acute forms of hemolytic reactions occur upon interaction of the transfused RBCs with the
antibodies that have been performed in the recipients.
Several cases of AHTR were also reported by studies that established its correlation
with multiple alloantibodies, which led to the development of intravascular hemolysis. Other
research articles, also confirmed association between hemolyyic disease of newborns and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BLOOD TRANSFUSION
DHTR with Rh antibodies (anti-c) in combination with anti-E (Sachan et al., 2015). Authors
have also established the need of conducting a screening for pre-transfusion antibodies during
compatibility testing. Necessity for conducting transfusion of Kell and Rh matched antibodies
have been confirmed by many articled, with the primary aim of preventing alloantibody
development among individuals requiring multiple transfusions or suffering from a range of
chronic disorders (Makroo, Agrawal & Chowdhry, 2017). Studies suggest that cross-
matching, antibody screening, followed by their identification are the most essential steps that
need to be performed before blood transfusion (Hijji, Parahoo, Hussein & Barr, 2013).
Another study also provided evidence that established the sequence of antigenicity of the Kell
and Rh antigens in the order of D>K>c>E>C>c. Blood transfusion is considered as an
essential component of treating sickle celled patients (Sharma et al., 2013). Furthermore, it
has been confirmed that alteration in Rh alleles in patients suffering from sickle cell anemia
and their donors showed a high prevalence of Rh alloimmunisation. Rates of blood
transfusion have been found indispensible in several regions of sub-Saharan Africa.
Another study showed high prevalence of acute transfusion reactions at a rate of 213
per 1000 transfusions in KATH (Owusu‐Ofori, Owusu‐Ofori & Bates, 2017). Research
studies have also been conducted to elucidate the fact that in order to avoid transfusion
reactions, blood from the donor must always be compatible and matched to that of the
patient. Articles confirm that the blood donated must contain similar Rh antigen D that is
lacking in the body of the patient or the receiver. However, authors have also argued that
donors might still portray incompatibility due to presence of other antigens, which might not
be routinely typed (Chou et al., 2013). Hence, it is essential to cross match the Rh systems
with the aim of ensuring compatibility of the donor RBCs against the recipient’s serum.
Although several studies have been conducted to elucidate the importance of Rh factor
compatibility before conducting blood transfusions, there is a need to conduct more extensive
DHTR with Rh antibodies (anti-c) in combination with anti-E (Sachan et al., 2015). Authors
have also established the need of conducting a screening for pre-transfusion antibodies during
compatibility testing. Necessity for conducting transfusion of Kell and Rh matched antibodies
have been confirmed by many articled, with the primary aim of preventing alloantibody
development among individuals requiring multiple transfusions or suffering from a range of
chronic disorders (Makroo, Agrawal & Chowdhry, 2017). Studies suggest that cross-
matching, antibody screening, followed by their identification are the most essential steps that
need to be performed before blood transfusion (Hijji, Parahoo, Hussein & Barr, 2013).
Another study also provided evidence that established the sequence of antigenicity of the Kell
and Rh antigens in the order of D>K>c>E>C>c. Blood transfusion is considered as an
essential component of treating sickle celled patients (Sharma et al., 2013). Furthermore, it
has been confirmed that alteration in Rh alleles in patients suffering from sickle cell anemia
and their donors showed a high prevalence of Rh alloimmunisation. Rates of blood
transfusion have been found indispensible in several regions of sub-Saharan Africa.
Another study showed high prevalence of acute transfusion reactions at a rate of 213
per 1000 transfusions in KATH (Owusu‐Ofori, Owusu‐Ofori & Bates, 2017). Research
studies have also been conducted to elucidate the fact that in order to avoid transfusion
reactions, blood from the donor must always be compatible and matched to that of the
patient. Articles confirm that the blood donated must contain similar Rh antigen D that is
lacking in the body of the patient or the receiver. However, authors have also argued that
donors might still portray incompatibility due to presence of other antigens, which might not
be routinely typed (Chou et al., 2013). Hence, it is essential to cross match the Rh systems
with the aim of ensuring compatibility of the donor RBCs against the recipient’s serum.
Although several studies have been conducted to elucidate the importance of Rh factor
compatibility before conducting blood transfusions, there is a need to conduct more extensive
BLOOD TRANSFUSION
literature searches for preventing risks related to sensitization of the receivers and hemolytic
reactions following blood transfusions. Further studies should be conducted to investigate the
concerns about alloimmunisation and future hemolytic reactions.
Percentage of antibodies that cause blood transfusion reaction
Blood transfusion reactions occur when the immune system of the recipient attacks
the red blood cells that were given by the donor during transfusion. A retrospective study that
aimed to determine prevalence of alloimmunisation among the Chinese population identified
83 patients with RBC antibodies. Estimates of the antibody percentages were found to be
approximately 39.3% (anti-E), 13.1% (anti-c), 6.55% (anti-Jka), 38.4% (anti-E), and 7.7%
(anti-Fyb) (Cheng, Lee & Lin, 2012). Another retrospective analysis were conducted to
determine risks of hemolytic transfusion reactions following an emergency and provided
evidences for positive antibody detection in 10.9% of the episodes. Alloantibodies and warm
autoantibodies were found in 6.4% and 2.3% of the cases, respectively (Goodell, Uhl,
Mohammed & Powers, 2010). Results from a prospective analysis that aimed to screen
alloimmunisation after RBC transfusion suggested presence of a high proportion of
individuals with O positive blood group (25%). 13.33% individuals without any history of
blood transfusions were found to produce antibodies. Further estimates suggested presence of
alloimmunisation among patients subjected to more than 10 episodes of blood transfusion
(50%) (Alves et al., 2012).
Similar findings were reported by another study that aimed to determine transfusion
complications that occur in thalassemia patients. The result analysis provided evidence for
19% transfused patients with reported allantibodies. 47% alloimmunised patients were found
to contain multiple antibodies, such as, anti-K, anti-E, anti-C, anti-c, and anti-JKa at
frequencies of 17%, 29%, 12%, 5% and 6%, respectively. Furthermore, rate of
alloimmunisation was found to be maximum at the initiation age of 11-20years, for
literature searches for preventing risks related to sensitization of the receivers and hemolytic
reactions following blood transfusions. Further studies should be conducted to investigate the
concerns about alloimmunisation and future hemolytic reactions.
Percentage of antibodies that cause blood transfusion reaction
Blood transfusion reactions occur when the immune system of the recipient attacks
the red blood cells that were given by the donor during transfusion. A retrospective study that
aimed to determine prevalence of alloimmunisation among the Chinese population identified
83 patients with RBC antibodies. Estimates of the antibody percentages were found to be
approximately 39.3% (anti-E), 13.1% (anti-c), 6.55% (anti-Jka), 38.4% (anti-E), and 7.7%
(anti-Fyb) (Cheng, Lee & Lin, 2012). Another retrospective analysis were conducted to
determine risks of hemolytic transfusion reactions following an emergency and provided
evidences for positive antibody detection in 10.9% of the episodes. Alloantibodies and warm
autoantibodies were found in 6.4% and 2.3% of the cases, respectively (Goodell, Uhl,
Mohammed & Powers, 2010). Results from a prospective analysis that aimed to screen
alloimmunisation after RBC transfusion suggested presence of a high proportion of
individuals with O positive blood group (25%). 13.33% individuals without any history of
blood transfusions were found to produce antibodies. Further estimates suggested presence of
alloimmunisation among patients subjected to more than 10 episodes of blood transfusion
(50%) (Alves et al., 2012).
Similar findings were reported by another study that aimed to determine transfusion
complications that occur in thalassemia patients. The result analysis provided evidence for
19% transfused patients with reported allantibodies. 47% alloimmunised patients were found
to contain multiple antibodies, such as, anti-K, anti-E, anti-C, anti-c, and anti-JKa at
frequencies of 17%, 29%, 12%, 5% and 6%, respectively. Furthermore, rate of
alloimmunisation was found to be maximum at the initiation age of 11-20years, for
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BLOOD TRANSFUSION
transfusion therapy (Vichinsky et al., 2014). A particular study was able to determine the
prevalence of the Rh and kell systems and estimated their rates to be 58%, 93.6%, 87%, 98%,
20%, and 3.5% for ‘c’, ‘D’, ‘C’, ‘e’, ‘E’, and ‘K’ antigens respectively (Makroo et al., 2013).
Similar results were demonstrated by another study that determined the prevalence to be
around 58.3%, 91.6%, 84%, 78.5% and 25.6% (Sharma et al., 2013). Studies were also
conducted to ascertain drawing of RBC components predominantly from Caucasian donors
and stated that SCD patients having undergone blood transfusion were found to contain 2%
K, 2% E, 1% C for antibody specificity (Wilkinson et al., 2012).
The major research gap exists in the fact that inadequate literature sources are
available that have investigated the proportion of antibodies that are responsible for the onset
of acute blood transfusion reactions. Good evidence is available for confirming the fact that
blood transfusion is highly variable and often shows a deviation from the evidence-based
guidelines. Owing to the fact that blood transfusions are life saving, it is extremely essential
to identify the percentage and prevalence of the antibodies that significantly contribute to its
associated adverse effects that might be life threatening. Therefore, there is a need to
determine the percentage of allo- and auto-antibodies that lead to the manifestation of acute
hemolytic transfusion reactions, post-transfusion.
To examine different technique to detect problem early
According to Sahu and Hemlata (2014), transfusion reactions are one of the most
common adverse effects associated with the administration of blood products. Adverse
transfusion reaction can lead to extreme discomfort to the patients along with extra burden of
cost to the healthcare system. There, awareness in increasing the clinical efficacy towards
restrictive transfusion thresholds along with early detection of the problem is crucial to
reduce the fatal outcomes (Delaney et al., 2016). Sahu and Hemlata (2014) are of the opinion
that detection of the early symptom is one of the crucial ways to detect the problem early.
transfusion therapy (Vichinsky et al., 2014). A particular study was able to determine the
prevalence of the Rh and kell systems and estimated their rates to be 58%, 93.6%, 87%, 98%,
20%, and 3.5% for ‘c’, ‘D’, ‘C’, ‘e’, ‘E’, and ‘K’ antigens respectively (Makroo et al., 2013).
Similar results were demonstrated by another study that determined the prevalence to be
around 58.3%, 91.6%, 84%, 78.5% and 25.6% (Sharma et al., 2013). Studies were also
conducted to ascertain drawing of RBC components predominantly from Caucasian donors
and stated that SCD patients having undergone blood transfusion were found to contain 2%
K, 2% E, 1% C for antibody specificity (Wilkinson et al., 2012).
The major research gap exists in the fact that inadequate literature sources are
available that have investigated the proportion of antibodies that are responsible for the onset
of acute blood transfusion reactions. Good evidence is available for confirming the fact that
blood transfusion is highly variable and often shows a deviation from the evidence-based
guidelines. Owing to the fact that blood transfusions are life saving, it is extremely essential
to identify the percentage and prevalence of the antibodies that significantly contribute to its
associated adverse effects that might be life threatening. Therefore, there is a need to
determine the percentage of allo- and auto-antibodies that lead to the manifestation of acute
hemolytic transfusion reactions, post-transfusion.
To examine different technique to detect problem early
According to Sahu and Hemlata (2014), transfusion reactions are one of the most
common adverse effects associated with the administration of blood products. Adverse
transfusion reaction can lead to extreme discomfort to the patients along with extra burden of
cost to the healthcare system. There, awareness in increasing the clinical efficacy towards
restrictive transfusion thresholds along with early detection of the problem is crucial to
reduce the fatal outcomes (Delaney et al., 2016). Sahu and Hemlata (2014) are of the opinion
that detection of the early symptom is one of the crucial ways to detect the problem early.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BLOOD TRANSFUSION
Allergic and anaphylactic transfusion reactions occur within 4 hours of transfusion and are
associated with platelet transfusion. The symptoms caused by the primary mediators
(histamine) are mild including rash, urticaria (hives), pruritus and severe reaction in include
anaphylactic shock (Delaney et al., 2016). Acute haemolytic transfusion reactions are the
common transfusion reactions. Since fever and chills are the few early signs and it is
important to monitor the patients during transfusion and cease the transfusion immediately if
there are any imbalance in the vital signs (Delaney et al., 2016). Early detection and
prevention of delayed haemolytic or delayed serological transfusion reactions are common
phenomenon among the patients with sickle cell anaemia (Delaney et al., 2016). Excretion of
dark urine and jaundice are common symptoms that must be used to monitor the detection of
the transfusion reaction (Delaney et al., 2016). However, the current management of delayed
haemolytic transfusion reaction is controversial because proper mechanism behind the
development of transfusion reaction is unclear because antibodies cannot be detected and lack
of proper corticosteroid treatment in patients with sickle cell anaemia (Yazdanbakhsh, Ware
& Noizat-Pirenne, 2012). Febrile non-haemolytic transfusion reactions have similar early
symptoms like that of the haemolytic transfusion reactions such that monitoring of the fever
or chills are main techniques or approaches that is utilised for the early detection of the
adverse transfusion reaction. However, Delaney et al. (2016) is of the opinion that pre-storage
of leukocyte can help in the prevention of the febrile non-haemolytic reactions. One of the
challenging and most complex blood transfusion reactions is hyper haemolytic transfusion
reaction. According to Delaney et al. (2016), serological analysis of the post-transfusion
samples might not reveal additional red blood cell alloantibodies and direct antiglobulin test
might provide negative results and thus creating confusion. Thus a high index suspicion is
recommended for the early diagnosis of the hyper haemolytic transfusion reaction which
occurs 7 days after the transfusion (Delaney et al., 2016).
Allergic and anaphylactic transfusion reactions occur within 4 hours of transfusion and are
associated with platelet transfusion. The symptoms caused by the primary mediators
(histamine) are mild including rash, urticaria (hives), pruritus and severe reaction in include
anaphylactic shock (Delaney et al., 2016). Acute haemolytic transfusion reactions are the
common transfusion reactions. Since fever and chills are the few early signs and it is
important to monitor the patients during transfusion and cease the transfusion immediately if
there are any imbalance in the vital signs (Delaney et al., 2016). Early detection and
prevention of delayed haemolytic or delayed serological transfusion reactions are common
phenomenon among the patients with sickle cell anaemia (Delaney et al., 2016). Excretion of
dark urine and jaundice are common symptoms that must be used to monitor the detection of
the transfusion reaction (Delaney et al., 2016). However, the current management of delayed
haemolytic transfusion reaction is controversial because proper mechanism behind the
development of transfusion reaction is unclear because antibodies cannot be detected and lack
of proper corticosteroid treatment in patients with sickle cell anaemia (Yazdanbakhsh, Ware
& Noizat-Pirenne, 2012). Febrile non-haemolytic transfusion reactions have similar early
symptoms like that of the haemolytic transfusion reactions such that monitoring of the fever
or chills are main techniques or approaches that is utilised for the early detection of the
adverse transfusion reaction. However, Delaney et al. (2016) is of the opinion that pre-storage
of leukocyte can help in the prevention of the febrile non-haemolytic reactions. One of the
challenging and most complex blood transfusion reactions is hyper haemolytic transfusion
reaction. According to Delaney et al. (2016), serological analysis of the post-transfusion
samples might not reveal additional red blood cell alloantibodies and direct antiglobulin test
might provide negative results and thus creating confusion. Thus a high index suspicion is
recommended for the early diagnosis of the hyper haemolytic transfusion reaction which
occurs 7 days after the transfusion (Delaney et al., 2016).
BLOOD TRANSFUSION
Prevention and early detection relies on systems-based practises along with proper
training of the healthcare professionals in order to ensure accurate patient identification at
crucial steps in sample collection and transfusion process (Figueroa et al., 2006). Further
review of literature will help in the elucidation for the proper system-based practices and
detection methods that is employed for the early detection of the transfusion reactions along
with detailed planning of the effective treatment procurement.
To create a new policy to avoid transfusion reaction
One of the main policy that is utilised to control the blood transfusion reaction include
detailed analysis of the patient’s allergic history before initiation of the blood transfusion
along with proper blood typing (Delaney et al., 2016). In the domain of allergic and
anaphylactic transfusion reaction, Tinegate et al. (2012) is of the opinion that the transfusion
can be resumed with the same unit but at a reduced rate if the symptoms resolved but if the
symptoms reoccur, then the transfusion must be discontinued immediately. Antihistamine
drug along with administration of epinephrine is recommended in order to treat the
anaphylactic transfusion reactions (Delaney et al., 2016). For the juvenile patients suffering
from cerebral palsy multiple intravenous infusions done via allogenic ABO/Rh-indentical
umbilical cord blood cells is considered to be safe and effective procedure in order to prevent
the blood transfusion reaction (Romanov et al., 2015). However, policy framing in order to
implement this procedure is still under way as further trails are require to validate the efficacy
of the results. The study conducted by Owusu‐Ofori, Owusu‐Ofori and Bates (2017) in
Ghana elucidated that there is a significant number of discontinued blood transfusion reaction
cases. They are of the opinion that this incidence suggests that proper guidelines on how to
manage the transfusion reactions would help to preserve the scarcity of the blood stocks.
They are also of the opinion that step-by-step implementation of haemovigilance system,
starting with monitoring the negative transfusion reaction is a pragmatic way under resource
Prevention and early detection relies on systems-based practises along with proper
training of the healthcare professionals in order to ensure accurate patient identification at
crucial steps in sample collection and transfusion process (Figueroa et al., 2006). Further
review of literature will help in the elucidation for the proper system-based practices and
detection methods that is employed for the early detection of the transfusion reactions along
with detailed planning of the effective treatment procurement.
To create a new policy to avoid transfusion reaction
One of the main policy that is utilised to control the blood transfusion reaction include
detailed analysis of the patient’s allergic history before initiation of the blood transfusion
along with proper blood typing (Delaney et al., 2016). In the domain of allergic and
anaphylactic transfusion reaction, Tinegate et al. (2012) is of the opinion that the transfusion
can be resumed with the same unit but at a reduced rate if the symptoms resolved but if the
symptoms reoccur, then the transfusion must be discontinued immediately. Antihistamine
drug along with administration of epinephrine is recommended in order to treat the
anaphylactic transfusion reactions (Delaney et al., 2016). For the juvenile patients suffering
from cerebral palsy multiple intravenous infusions done via allogenic ABO/Rh-indentical
umbilical cord blood cells is considered to be safe and effective procedure in order to prevent
the blood transfusion reaction (Romanov et al., 2015). However, policy framing in order to
implement this procedure is still under way as further trails are require to validate the efficacy
of the results. The study conducted by Owusu‐Ofori, Owusu‐Ofori and Bates (2017) in
Ghana elucidated that there is a significant number of discontinued blood transfusion reaction
cases. They are of the opinion that this incidence suggests that proper guidelines on how to
manage the transfusion reactions would help to preserve the scarcity of the blood stocks.
They are also of the opinion that step-by-step implementation of haemovigilance system,
starting with monitoring the negative transfusion reaction is a pragmatic way under resource
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BLOOD TRANSFUSION
limited settings. Overall, Fung et al. (2010) is of the opinion that the health-care organisations
must establish policies that define the vitals sign change that will facilitate quick evaluation
of suspected transfusion reaction. Thus there lies a gap in the domain of proper framing of the
blood transfusion policies which will help to prevent the adverse effects arising out of the
blood transfusion reaction. According to Milkins et al. (2013), any abbreviation of the ABO
group must be assessed in a comprehensive manner. They also further opined that fully
automated systems should be employed in order to reduce the risks associated with the
interpretation and transcription errors. Milkins et al. (2013) also vouched in favour of proper
analysis of the patient’s demographics against the computer-generated record before
validation of the transfusion results this will ensure that the samples are matched and that no
errors are done during the encryption of the data in the laboratory information management
system. Milkins et al. (2013) further opined that indirect antiglobulin test (IAT) cross match
should be used as the default technique when the electronic issue is contra-indicated. IAT
cross match technique should be used only if the patient’s plasma contains allo-antibodies of
the red blood cells. Gender and a unique identification number are proper by Milkins et al.
(2013) as the general identifier for the unknown patient; this will help to track the root cause
of the adverse transfusion reaction.
However, these blood transfusion polices are only related to the pre-transfusion
protocols. A detailed analysis of the governmental policies across the world in relation of
blood transfusion reaction will help to frame concrete transfusion policies which will in turn
provide an effective means to reduce the fatal outcomes of the transfusion reactions.
Methodology
This qualitative research will be conducted based on positivism research philosophy
as this will help the researcher to analyse the topic with logical flow of information. The
limited settings. Overall, Fung et al. (2010) is of the opinion that the health-care organisations
must establish policies that define the vitals sign change that will facilitate quick evaluation
of suspected transfusion reaction. Thus there lies a gap in the domain of proper framing of the
blood transfusion policies which will help to prevent the adverse effects arising out of the
blood transfusion reaction. According to Milkins et al. (2013), any abbreviation of the ABO
group must be assessed in a comprehensive manner. They also further opined that fully
automated systems should be employed in order to reduce the risks associated with the
interpretation and transcription errors. Milkins et al. (2013) also vouched in favour of proper
analysis of the patient’s demographics against the computer-generated record before
validation of the transfusion results this will ensure that the samples are matched and that no
errors are done during the encryption of the data in the laboratory information management
system. Milkins et al. (2013) further opined that indirect antiglobulin test (IAT) cross match
should be used as the default technique when the electronic issue is contra-indicated. IAT
cross match technique should be used only if the patient’s plasma contains allo-antibodies of
the red blood cells. Gender and a unique identification number are proper by Milkins et al.
(2013) as the general identifier for the unknown patient; this will help to track the root cause
of the adverse transfusion reaction.
However, these blood transfusion polices are only related to the pre-transfusion
protocols. A detailed analysis of the governmental policies across the world in relation of
blood transfusion reaction will help to frame concrete transfusion policies which will in turn
provide an effective means to reduce the fatal outcomes of the transfusion reactions.
Methodology
This qualitative research will be conducted based on positivism research philosophy
as this will help the researcher to analyse the topic with logical flow of information. The
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
BLOOD TRANSFUSION
research design which will be used by researcher include descriptive approach as this will
help the research to analyse various approaches in a descriptive manner. Research strategy
that will be suitable for this research is secondary and this will aid qualitative data analysis
(Parahoo et al., 2014). The sampling or the collection of sample in this research generally
deals with search of the literary articles. The search of the articles will mostly be based on the
broad key-word search of the articles in the electronic data base include PubMed, Medline
and Crochane. The main keywords which will be used for the search of the literary articles
include “blood transfusion”, “transfusion reaction”, “transfusion reaction” AND “ABO blood
group”, “transfusion reaction” AND adverse events”. The main inclusion criteria that will be
selected for the study include, literary articles published within last 10 years (2008 to 2018)
and in English language. The main exclusion criteria that will be selected for the study
include the articles focused on the plasma derivatives.
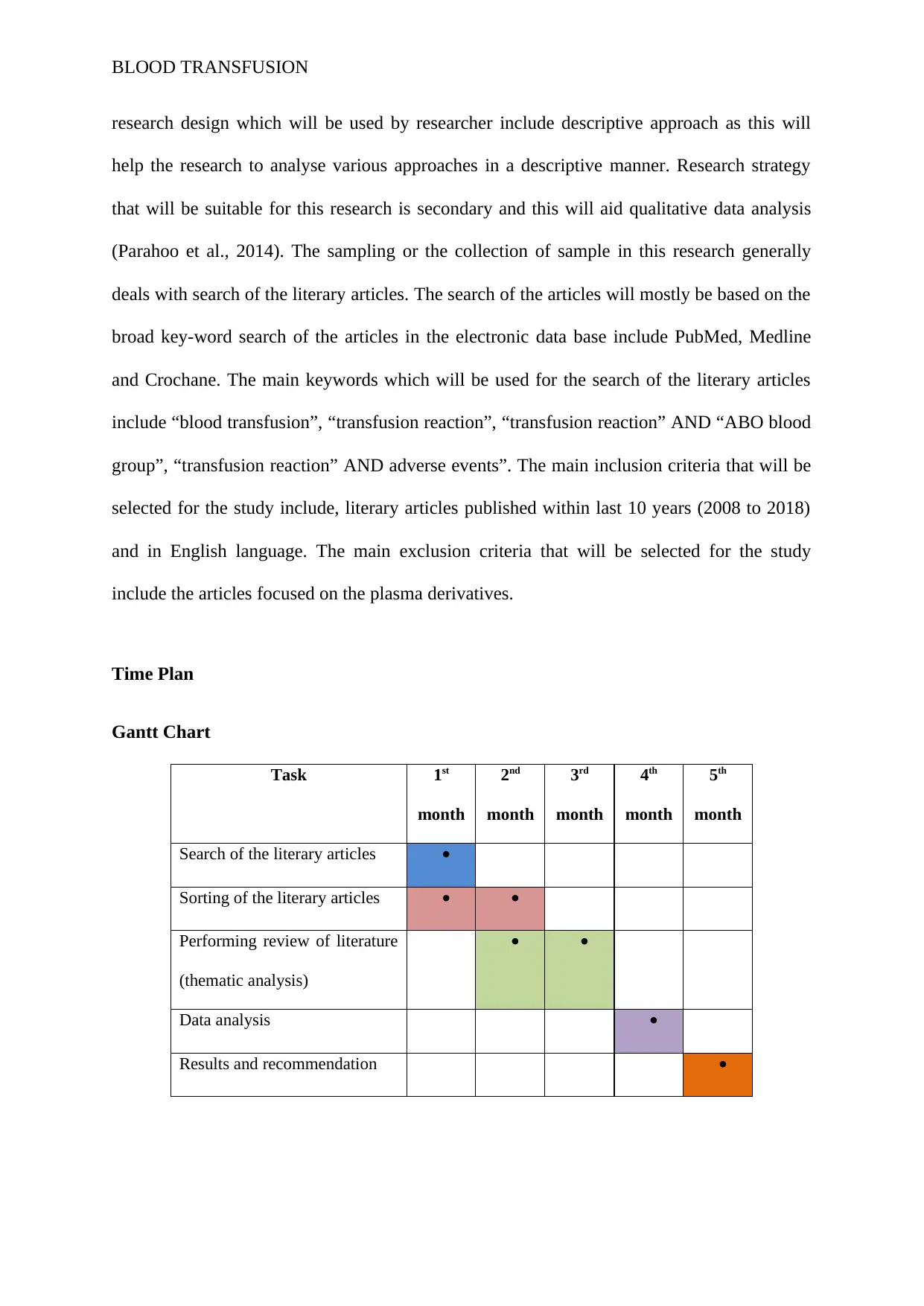
Time Plan
Gantt Chart
Task 1st
month
2nd
month
3rd
month
4th
month
5th
month
Search of the literary articles
Sorting of the literary articles
Performing review of literature
(thematic analysis)
Data analysis
Results and recommendation
research design which will be used by researcher include descriptive approach as this will
help the research to analyse various approaches in a descriptive manner. Research strategy
that will be suitable for this research is secondary and this will aid qualitative data analysis
(Parahoo et al., 2014). The sampling or the collection of sample in this research generally
deals with search of the literary articles. The search of the articles will mostly be based on the
broad key-word search of the articles in the electronic data base include PubMed, Medline
and Crochane. The main keywords which will be used for the search of the literary articles
include “blood transfusion”, “transfusion reaction”, “transfusion reaction” AND “ABO blood
group”, “transfusion reaction” AND adverse events”. The main inclusion criteria that will be
selected for the study include, literary articles published within last 10 years (2008 to 2018)
and in English language. The main exclusion criteria that will be selected for the study
include the articles focused on the plasma derivatives.
Time Plan
Gantt Chart
Task 1st
month
2nd
month
3rd
month
4th
month
5th
month
Search of the literary articles
Sorting of the literary articles
Performing review of literature
(thematic analysis)
Data analysis
Results and recommendation
BLOOD TRANSFUSION
References
Alves, V. M., Martins, P. R. J., Soares, S., Araújo, G., Schmidt, L. C., Costa, S. S. D. M., ...
& Moraes-Souza, H. (2012). Alloimmunization screening after transfusion of red
blood cells in a prospective study. Revista brasileira de hematologia e
hemoterapia, 34(3), 206-211.
Berséus, O., Boman, K., Nessen, S. C., & Westerberg, L. A. (2013). Risks of hemolysis due
to anti‐A and anti‐B caused by the transfusion of blood or blood components
containing ABO‐incompatible plasma. Transfusion, 53(S1), 114S-123S.
Cheng, C. K., Lee, C. K., & Lin, C. K. (2012). Clinically significant red blood cell antibodies
in chronically transfused patients: a survey of Chinese thalassemia major patients and
literature review. Transfusion, 52(10), 2220-2224.
Chou, S. T., Jackson, T., Vege, S., Smith-Whitley, K., Friedman, D. F., & Westhoff, C. M.
(2013). High prevalence of red blood cell alloimmunization in sickle cell disease
despite transfusion from Rh-matched minority donors. Blood, 122(6), 1062-1071.
Delaney, M., Wendel, S., Bercovitz, R. S., Cid, J., Cohn, C., Dunbar, N. M., ... & Van De
Watering, L. (2016). Transfusion reactions: prevention, diagnosis, and treatment. The
Lancet, 388(10061), 2825-2836.
Figueroa, P. I., Ziman, A., Wheeler, C., Gornbein, J., Monson, M., & Calhoun, L. (2006).
Nearly two decades using the check-type to prevent ABO-incompatible transfusions:
one institution’s experience. American journal of clinical pathology, 126(3), 422-426.
Fung M, Grossman BJ, Hillyer CD & Westhoff CM. (2014). Technical Manual, 18th edn.
Glen Burnie, MD: AABB Press.
References
Alves, V. M., Martins, P. R. J., Soares, S., Araújo, G., Schmidt, L. C., Costa, S. S. D. M., ...
& Moraes-Souza, H. (2012). Alloimmunization screening after transfusion of red
blood cells in a prospective study. Revista brasileira de hematologia e
hemoterapia, 34(3), 206-211.
Berséus, O., Boman, K., Nessen, S. C., & Westerberg, L. A. (2013). Risks of hemolysis due
to anti‐A and anti‐B caused by the transfusion of blood or blood components
containing ABO‐incompatible plasma. Transfusion, 53(S1), 114S-123S.
Cheng, C. K., Lee, C. K., & Lin, C. K. (2012). Clinically significant red blood cell antibodies
in chronically transfused patients: a survey of Chinese thalassemia major patients and
literature review. Transfusion, 52(10), 2220-2224.
Chou, S. T., Jackson, T., Vege, S., Smith-Whitley, K., Friedman, D. F., & Westhoff, C. M.
(2013). High prevalence of red blood cell alloimmunization in sickle cell disease
despite transfusion from Rh-matched minority donors. Blood, 122(6), 1062-1071.
Delaney, M., Wendel, S., Bercovitz, R. S., Cid, J., Cohn, C., Dunbar, N. M., ... & Van De
Watering, L. (2016). Transfusion reactions: prevention, diagnosis, and treatment. The
Lancet, 388(10061), 2825-2836.
Figueroa, P. I., Ziman, A., Wheeler, C., Gornbein, J., Monson, M., & Calhoun, L. (2006).
Nearly two decades using the check-type to prevent ABO-incompatible transfusions:
one institution’s experience. American journal of clinical pathology, 126(3), 422-426.
Fung M, Grossman BJ, Hillyer CD & Westhoff CM. (2014). Technical Manual, 18th edn.
Glen Burnie, MD: AABB Press.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




