Risk Analysis Report: My Health Record Health System Project
VerifiedAdded on 2022/09/06
|7
|1201
|17
Report
AI Summary
This report provides a comprehensive risk analysis of the My Health Record healthcare system, focusing on potential risks and their impacts. The analysis identifies key risks, including project cost overruns, lack of staff training, data breaches, complex health regulations, violence in hospitals, and the impact of healthcare reforms. Each risk is evaluated for its likelihood, impact, and overall risk level, with corresponding risk treatments and responsible parties outlined to facilitate effective risk management. The report highlights the importance of financial planning, staff training, data security measures, compliance with regulations, violence prevention programs, and quality improvement initiatives to ensure the successful implementation and operation of the My Health Record system. References to relevant literature support the analysis and proposed solutions.

Running head: RISK ANALYSIS
Risk Analysis
Name of the Student:
Name of the University:
Risk Analysis
Name of the Student:
Name of the University:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1RISK ANALYSIS
Risk Analysis
The risk analysis of this paper is focused on My Health Record health system. It is the
national digital health record system for sharing of information with the doctors, hospitals as
well as healthcare providers. The system is provided with secured summary of health related
information and data (Delcea & Ioana-Alexandra, 2016). Following risk analysis table shows
the list of the healthcare risks and its impact on the project success. Risk treatments are also
provided for each project risks so that it can be managed properly.
Risk Analysis
The risk analysis of this paper is focused on My Health Record health system. It is the
national digital health record system for sharing of information with the doctors, hospitals as
well as healthcare providers. The system is provided with secured summary of health related
information and data (Delcea & Ioana-Alexandra, 2016). Following risk analysis table shows
the list of the healthcare risks and its impact on the project success. Risk treatments are also
provided for each project risks so that it can be managed properly.
2RISK ANALYSIS
Risk Impact L C R Risk Treatments Responsibility
and role
Cost for implementing health
system is expensive than its
initial project budget.
Increase in project cost provides impact on
the project completion time, because if the
project cost is increased than it initial
estimated value, then the project should stop
working until funds are collected for
remaining project work (Trein, 2017).
Almost
certain
(5)
Major (4) Extreme
(4)
There should require to collect extra funds
for the healthcare system project, so that
extra project expenses could not cause
problem when addition budget is required.
Financial
Officer-
Responsible to
oversee with
the financial
transactions of
the project
Knowledge and skills level of
the staffs those are taking
account of the system
implementation has lack of
training and support (Alam,
2016).
It provides impact on the healthcare
providers as lack of system knowledge can
lead to training of the staffs who are from
non-technical background. It also impacts
project cost as extra budget is required for
training program (Delcea & Ioana-
Alexandra, 2016).
Possible
(3)
Moderate
(3)
Medium
(2)
There should require to conduct as well as
organize training program so that all the
healthcare staffs should get proper training
on technical fields, therefore they should
handle the system implementation work
efficiently (Fischer & Miller, 2017).
Human
Resource
Manager-
Taking
responsibility
to provide
training to
Risk Impact L C R Risk Treatments Responsibility
and role
Cost for implementing health
system is expensive than its
initial project budget.
Increase in project cost provides impact on
the project completion time, because if the
project cost is increased than it initial
estimated value, then the project should stop
working until funds are collected for
remaining project work (Trein, 2017).
Almost
certain
(5)
Major (4) Extreme
(4)
There should require to collect extra funds
for the healthcare system project, so that
extra project expenses could not cause
problem when addition budget is required.
Financial
Officer-
Responsible to
oversee with
the financial
transactions of
the project
Knowledge and skills level of
the staffs those are taking
account of the system
implementation has lack of
training and support (Alam,
2016).
It provides impact on the healthcare
providers as lack of system knowledge can
lead to training of the staffs who are from
non-technical background. It also impacts
project cost as extra budget is required for
training program (Delcea & Ioana-
Alexandra, 2016).
Possible
(3)
Moderate
(3)
Medium
(2)
There should require to conduct as well as
organize training program so that all the
healthcare staffs should get proper training
on technical fields, therefore they should
handle the system implementation work
efficiently (Fischer & Miller, 2017).
Human
Resource
Manager-
Taking
responsibility
to provide
training to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3RISK ANALYSIS
employees on
technical field
Doctors and healthcare
providers are facing issues of
data breaches. The privacy
issues are loss of data, data
tampering and unauthorized
access to the information of
patient.
Data breaches risk provides impact on the
customers as stolen and hacking of
customer’s data cause issue of them when
the third party person should share the data
with others leads to huge risk for the
customers (Fischer & Miller, 2017).
Likely
(4)
Moderate
(3)
High (3) There should require to work with the
software as well as vendor to use proper
firewall as well as protections to secure the
health data.
Security
Officer-
Blocking the
security threats
by enhanced
security
features like
two way
authentication
method
The health regulatory
environment is complex, even it
facilitates at high risk of the
non-compliance. The healthcare
Non-regulatory policies and regulations are
providing impact on the quality level of
healthcare services provided to the patients
(Trein, 2017). The health practices as well
Unlikely
(2)
Moderate
(3)
Medium
(2)
The healthcare providers are complying
with the regulations apply to the non-
healthcare business like Occupational Safety
and Health Administration (Carroll, 2016).
Department of
Health and
Human
Services-
employees on
technical field
Doctors and healthcare
providers are facing issues of
data breaches. The privacy
issues are loss of data, data
tampering and unauthorized
access to the information of
patient.
Data breaches risk provides impact on the
customers as stolen and hacking of
customer’s data cause issue of them when
the third party person should share the data
with others leads to huge risk for the
customers (Fischer & Miller, 2017).
Likely
(4)
Moderate
(3)
High (3) There should require to work with the
software as well as vendor to use proper
firewall as well as protections to secure the
health data.
Security
Officer-
Blocking the
security threats
by enhanced
security
features like
two way
authentication
method
The health regulatory
environment is complex, even it
facilitates at high risk of the
non-compliance. The healthcare
Non-regulatory policies and regulations are
providing impact on the quality level of
healthcare services provided to the patients
(Trein, 2017). The health practices as well
Unlikely
(2)
Moderate
(3)
Medium
(2)
The healthcare providers are complying
with the regulations apply to the non-
healthcare business like Occupational Safety
and Health Administration (Carroll, 2016).
Department of
Health and
Human
Services-
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4RISK ANALYSIS
business as well as healthcare
providers are not aware of laws
as well as regulations applied in
the business (Fischer & Miller,
2017).
as standards are required to apply to the
hospital rules.
Delivering
services plus
policies to
enhance health
The hospitals are placing a
healing, but it has become a
scene of number of incidents in
violent. The incidents are
putting the patients at a high risk
and also the healthcare
professionals, those are targets
of attacks (Trein, 2017).
It should provide impact on the physical
condition of the staffs, therefore can lead to
extra project cost (Delcea & Ioana-
Alexandra, 2016). There is an increase in
project cost due to extra treatment facilitates
required for the physical injuries healthcare
providers.
Unlikely
(2)
Minor (2) Medium
(2)
The healthcare organization should require
to enact of zero tolerance policy, so that
there is no state of violence such as physical
and verbal. Therefore it cannot lead to any
type of physical as well as verbal violence
of the healthcare providers. There should
also require to develop a violence
prevention program to analyze the safety
hazards as well as implement of strategies to
prevent any violent.
Human
Resource
Manager-
Implementation
of zero
tolerance
policy in the
hospitals
The healthcare reform is not It provides impact on both patient’s care as Rare (1) Negligible Low (1) In order to overcome with this quality Department of
business as well as healthcare
providers are not aware of laws
as well as regulations applied in
the business (Fischer & Miller,
2017).
as standards are required to apply to the
hospital rules.
Delivering
services plus
policies to
enhance health
The hospitals are placing a
healing, but it has become a
scene of number of incidents in
violent. The incidents are
putting the patients at a high risk
and also the healthcare
professionals, those are targets
of attacks (Trein, 2017).
It should provide impact on the physical
condition of the staffs, therefore can lead to
extra project cost (Delcea & Ioana-
Alexandra, 2016). There is an increase in
project cost due to extra treatment facilitates
required for the physical injuries healthcare
providers.
Unlikely
(2)
Minor (2) Medium
(2)
The healthcare organization should require
to enact of zero tolerance policy, so that
there is no state of violence such as physical
and verbal. Therefore it cannot lead to any
type of physical as well as verbal violence
of the healthcare providers. There should
also require to develop a violence
prevention program to analyze the safety
hazards as well as implement of strategies to
prevent any violent.
Human
Resource
Manager-
Implementation
of zero
tolerance
policy in the
hospitals
The healthcare reform is not It provides impact on both patient’s care as Rare (1) Negligible Low (1) In order to overcome with this quality Department of
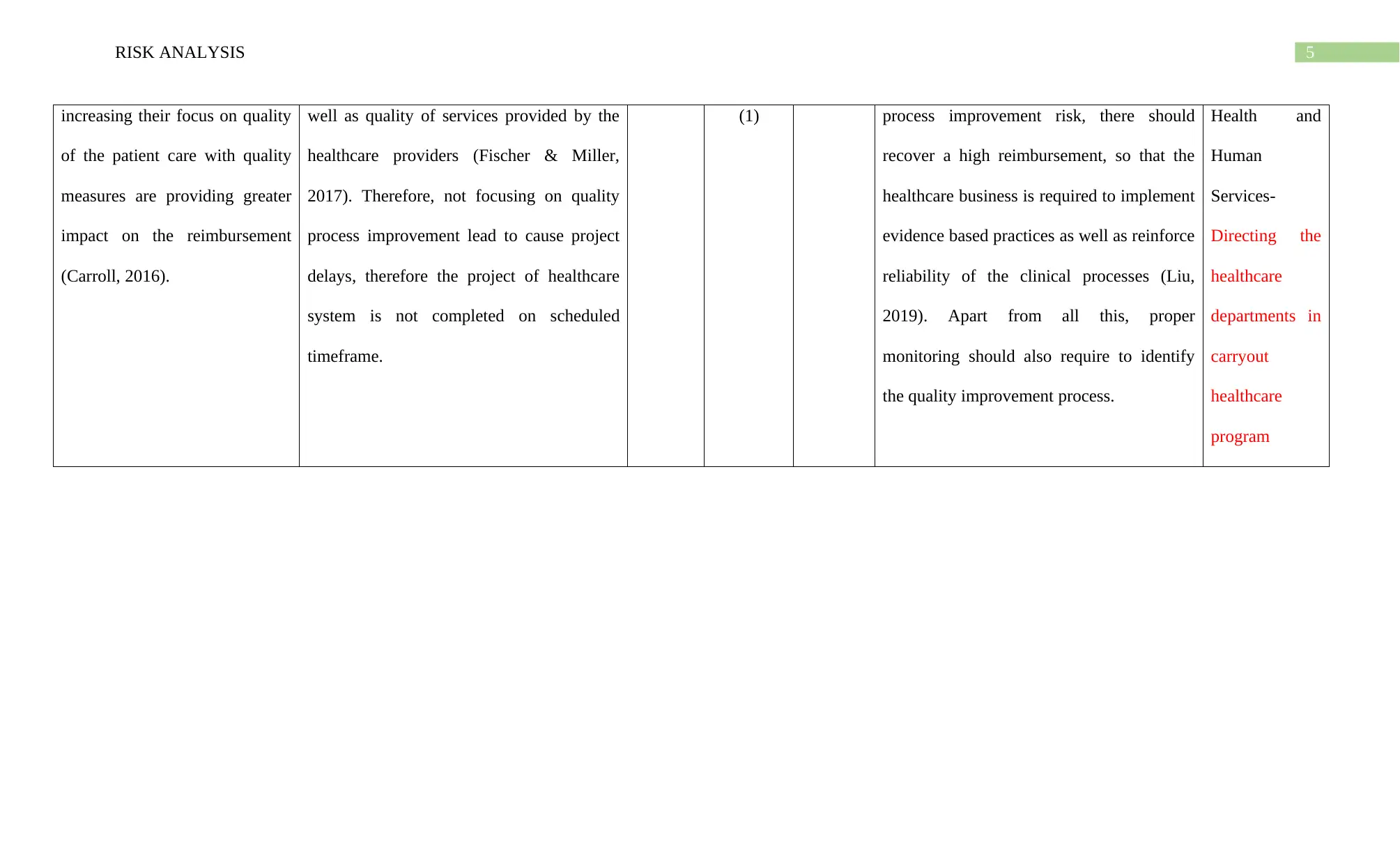
5RISK ANALYSIS
increasing their focus on quality
of the patient care with quality
measures are providing greater
impact on the reimbursement
(Carroll, 2016).
well as quality of services provided by the
healthcare providers (Fischer & Miller,
2017). Therefore, not focusing on quality
process improvement lead to cause project
delays, therefore the project of healthcare
system is not completed on scheduled
timeframe.
(1) process improvement risk, there should
recover a high reimbursement, so that the
healthcare business is required to implement
evidence based practices as well as reinforce
reliability of the clinical processes (Liu,
2019). Apart from all this, proper
monitoring should also require to identify
the quality improvement process.
Health and
Human
Services-
Directing the
healthcare
departments in
carryout
healthcare
program
increasing their focus on quality
of the patient care with quality
measures are providing greater
impact on the reimbursement
(Carroll, 2016).
well as quality of services provided by the
healthcare providers (Fischer & Miller,
2017). Therefore, not focusing on quality
process improvement lead to cause project
delays, therefore the project of healthcare
system is not completed on scheduled
timeframe.
(1) process improvement risk, there should
recover a high reimbursement, so that the
healthcare business is required to implement
evidence based practices as well as reinforce
reliability of the clinical processes (Liu,
2019). Apart from all this, proper
monitoring should also require to identify
the quality improvement process.
Health and
Human
Services-
Directing the
healthcare
departments in
carryout
healthcare
program
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6RISK ANALYSIS
References
Alam, A. Y. (2016). Steps in the process of risk management in healthcare. J Epid Prev
Med, 2(2), 118.
Carroll, R. (2016). Identifying risks in the realm of enterprise risk management. Journal of
Healthcare Risk Management, 35(3), 24-30.
Delcea, C., & Ioana-Alexandra, B. (2016). Fostering risk management in healthcare units
using grey systems theory. Grey Systems: Theory and Application.
Fischer, F., & Miller, G. J. (Eds.). (2017). Handbook of public policy analysis: theory,
politics, and methods. Routledge.
Liu, H. C. (2019). Healthcare risk management from a proactive perspective. In Improved
FMEA methods for proactive healthcare risk analysis (pp. 3-13). Springer, Singapore.
Trein, P. (2017). Coevolution of policy sectors: A comparative analysis of healthcare and
public health. Public Administration, 95(3), 744-758.
References
Alam, A. Y. (2016). Steps in the process of risk management in healthcare. J Epid Prev
Med, 2(2), 118.
Carroll, R. (2016). Identifying risks in the realm of enterprise risk management. Journal of
Healthcare Risk Management, 35(3), 24-30.
Delcea, C., & Ioana-Alexandra, B. (2016). Fostering risk management in healthcare units
using grey systems theory. Grey Systems: Theory and Application.
Fischer, F., & Miller, G. J. (Eds.). (2017). Handbook of public policy analysis: theory,
politics, and methods. Routledge.
Liu, H. C. (2019). Healthcare risk management from a proactive perspective. In Improved
FMEA methods for proactive healthcare risk analysis (pp. 3-13). Springer, Singapore.
Trein, P. (2017). Coevolution of policy sectors: A comparative analysis of healthcare and
public health. Public Administration, 95(3), 744-758.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




