Memo on Roles and Responsibilities for Hospital System Compliance
VerifiedAdded on 2019/09/20
|14
|2941
|428
Report
AI Summary
This report examines the roles and responsibilities of compliance officers within a hospital system, emphasizing adherence to legal and ethical standards. It details the duties of compliance officers, including policy development, training, and reporting. The report explores the Stark Law, which prohibits physician self-referrals, and the Anti-Kickback Statute, which prohibits payments to induce referrals, highlighting their differences and exceptions. It also covers the Corporate Integrity Agreement as an enforcement tool. The analysis includes historical context, penalties for violations, and the rationale behind these regulations, providing a comprehensive overview of compliance requirements in healthcare. The report underscores the importance of compliance in maintaining the integrity of the healthcare system and protecting patients.
Running Head: Memo
MEMo
MEMo
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Memo 1
Memo
To: Chairman
From: Compliance Officers
CC: Board of Director
Date: 19th June 2017
Re: Roles and responsibility for accomplishing for the hospital system.
The following is the roles and responsibilities for accomplishing hospital system.
1. The role of compliance officers, also known as a compliance manager, is to make sure
that the company should conduct its business in full conformity with all laws which
include both national and international and the regulations that relate to the particular
industry, internal standards, and all the accepted business practices.
DUTIES
The duty of compliance officers are as follows:
To link the number of relevant authorities, laboratories, companies as per the description
mention.
To develop, initiate, maintain and revise the policies and procedures for the general
operation of a compliance program as well as its related activities.
To develop and periodically reviews and updates Standards of Conduct to ensure
continuing currency and its relevance in guiding the management and the employees.
Memo
To: Chairman
From: Compliance Officers
CC: Board of Director
Date: 19th June 2017
Re: Roles and responsibility for accomplishing for the hospital system.
The following is the roles and responsibilities for accomplishing hospital system.
1. The role of compliance officers, also known as a compliance manager, is to make sure
that the company should conduct its business in full conformity with all laws which
include both national and international and the regulations that relate to the particular
industry, internal standards, and all the accepted business practices.
DUTIES
The duty of compliance officers are as follows:
To link the number of relevant authorities, laboratories, companies as per the description
mention.
To develop, initiate, maintain and revise the policies and procedures for the general
operation of a compliance program as well as its related activities.
To develop and periodically reviews and updates Standards of Conduct to ensure
continuing currency and its relevance in guiding the management and the employees.
Memo 2
To consult with the corporate attorney that help them to resolve the problems related to
compliance issues.
To act as an independent review as well as the evaluation body by which to ensure that
the compliance issues were being appropriately resolved.
To provide the report on a regular basis so that it will keep in touch with the Corporate
Compliance of the board as well as senior management for the operation and the progress
of the efforts.
To establish and provide direction of the compliance hotline.
To ensure proper reporting of the violation that is authorized by the enforcement
agencies.
To work with the HR Department so that to develop an effective training program for the
new employees in the organizations as well as the ongoing training for rest of the
employees and the manager.
Monitoring compliance program performance and relates it to a continuing basis that will
take an appropriate step to increase its efficiency.
Report to Board of Director
Although the Compliance Officer is an independent officer so it has to report the Board of
Director as it should report the structure that would be in compliance with the purpose of
sentencing guidelines. A report made in 2010 in US where a panel which consists of
representatives from the U.S. tell about that the compliance officer should report to the Board of
Director and not directly to the General officer. At the same time, the conference of the DOJ
To consult with the corporate attorney that help them to resolve the problems related to
compliance issues.
To act as an independent review as well as the evaluation body by which to ensure that
the compliance issues were being appropriately resolved.
To provide the report on a regular basis so that it will keep in touch with the Corporate
Compliance of the board as well as senior management for the operation and the progress
of the efforts.
To establish and provide direction of the compliance hotline.
To ensure proper reporting of the violation that is authorized by the enforcement
agencies.
To work with the HR Department so that to develop an effective training program for the
new employees in the organizations as well as the ongoing training for rest of the
employees and the manager.
Monitoring compliance program performance and relates it to a continuing basis that will
take an appropriate step to increase its efficiency.
Report to Board of Director
Although the Compliance Officer is an independent officer so it has to report the Board of
Director as it should report the structure that would be in compliance with the purpose of
sentencing guidelines. A report made in 2010 in US where a panel which consists of
representatives from the U.S. tell about that the compliance officer should report to the Board of
Director and not directly to the General officer. At the same time, the conference of the DOJ
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Memo 3
Assistant Attorney General Lanny Breuer said that they should directly access the board of
directors, suggesting that it should not directly report to the General compliance as it should
directly report to the board.
2. The history of Stark law suggests that it was in 1989 when the Stark Law I was enacted
and it was effectively started in 1st January 1992. The fundamental purpose of this law
was to ban the self-referral for the services of clinic laboratory. Also, the Stark law
prohibits the entities for making a claim for the payment in the Medicare program for the
clinical laboratory services which furnished the under that prohibits referral. After that in
1993 Stark Law II was enacted which is the expansion of Stark Law I and it was started
in 1st January 1995. The main purpose of this was to extend the services of additional
health care.
Stark Law is a set of US federal laws which prohibited the physician self-referral, most
importantly for the physician of the Medicare patient to an entity and provide designated
health services (DHS) in case that the physician has a financial relationship with the
entity.
The term "referral" define as the request by a physician for the service for the medical
services and the request for establishment of a plan of care by a physician which involves
the provision related to health services for the other services. The DHS includes the client
laboratory services, physical therapy services, occupational therapy services, services
related to radiology, radiation therapy services, and home care health services as well as
the in and out patient hospital services. It includes the relationship between the
ownership, investment interest, and the arrangements related to compensation.
Assistant Attorney General Lanny Breuer said that they should directly access the board of
directors, suggesting that it should not directly report to the General compliance as it should
directly report to the board.
2. The history of Stark law suggests that it was in 1989 when the Stark Law I was enacted
and it was effectively started in 1st January 1992. The fundamental purpose of this law
was to ban the self-referral for the services of clinic laboratory. Also, the Stark law
prohibits the entities for making a claim for the payment in the Medicare program for the
clinical laboratory services which furnished the under that prohibits referral. After that in
1993 Stark Law II was enacted which is the expansion of Stark Law I and it was started
in 1st January 1995. The main purpose of this was to extend the services of additional
health care.
Stark Law is a set of US federal laws which prohibited the physician self-referral, most
importantly for the physician of the Medicare patient to an entity and provide designated
health services (DHS) in case that the physician has a financial relationship with the
entity.
The term "referral" define as the request by a physician for the service for the medical
services and the request for establishment of a plan of care by a physician which involves
the provision related to health services for the other services. The DHS includes the client
laboratory services, physical therapy services, occupational therapy services, services
related to radiology, radiation therapy services, and home care health services as well as
the in and out patient hospital services. It includes the relationship between the
ownership, investment interest, and the arrangements related to compensation.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Memo 4
The purpose of the Stark law address that the consulting and the professional relationship
between the doctors, hospitals, and companies.
The Stark law pertain only to the physicians who refers as Medicare patients for a
particular service to the entity by which they have a financial relationship. The list that is
designated health services, as well as the financial relationship, have been addressed by
the statue of the extraordinarily board.
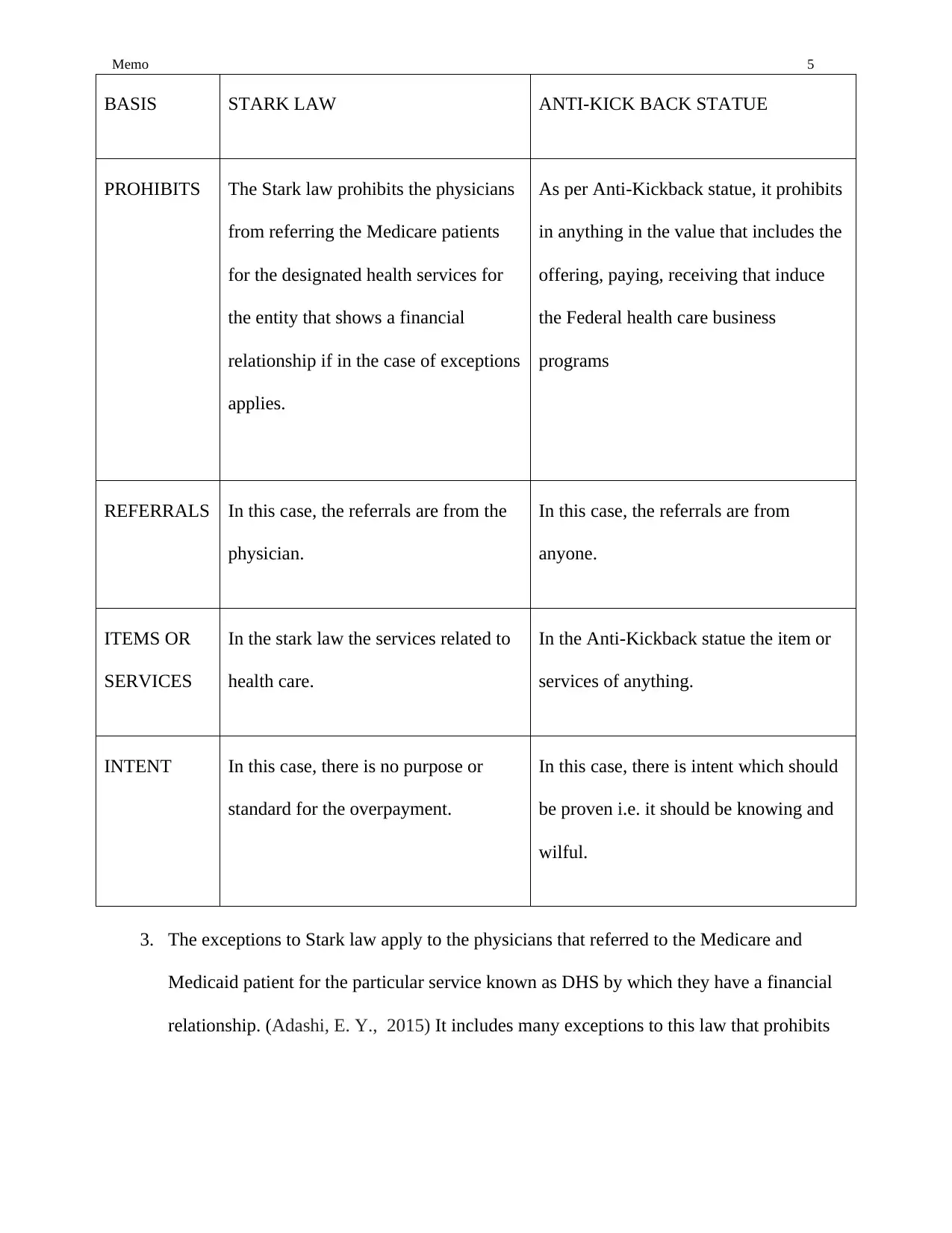
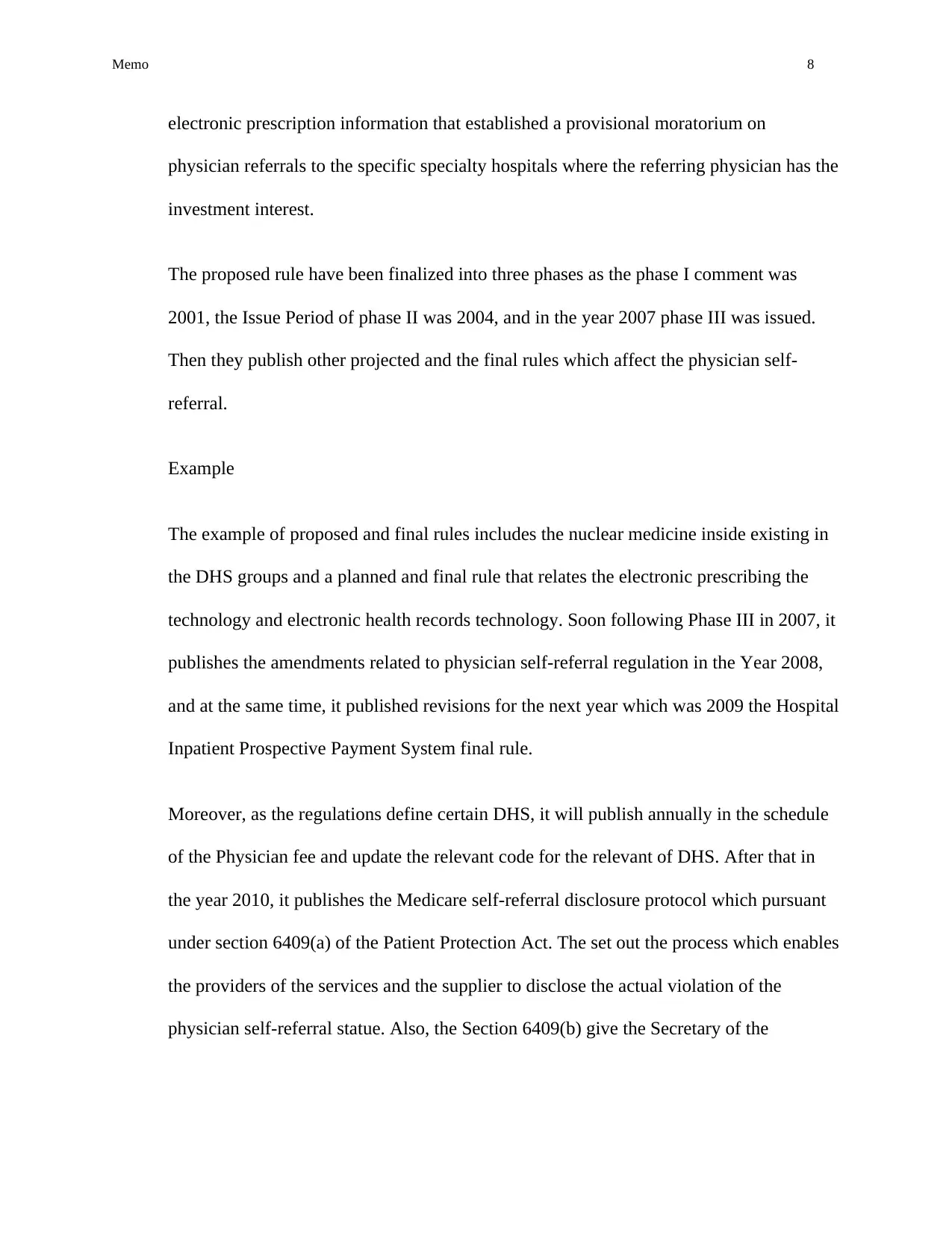
The difference between the Stark law and Anti-kickback statue is given below
The purpose of the Stark law address that the consulting and the professional relationship
between the doctors, hospitals, and companies.
The Stark law pertain only to the physicians who refers as Medicare patients for a
particular service to the entity by which they have a financial relationship. The list that is
designated health services, as well as the financial relationship, have been addressed by
the statue of the extraordinarily board.
The difference between the Stark law and Anti-kickback statue is given below
Memo 5
3. The exceptions to Stark law apply to the physicians that referred to the Medicare and
Medicaid patient for the particular service known as DHS by which they have a financial
relationship. (Adashi, E. Y., 2015) It includes many exceptions to this law that prohibits
BASIS STARK LAW ANTI-KICK BACK STATUE
PROHIBITS The Stark law prohibits the physicians
from referring the Medicare patients
for the designated health services for
the entity that shows a financial
relationship if in the case of exceptions
applies.
As per Anti-Kickback statue, it prohibits
in anything in the value that includes the
offering, paying, receiving that induce
the Federal health care business
programs
REFERRALS In this case, the referrals are from the
physician.
In this case, the referrals are from
anyone.
ITEMS OR
SERVICES
In the stark law the services related to
health care.
In the Anti-Kickback statue the item or
services of anything.
INTENT In this case, there is no purpose or
standard for the overpayment.
In this case, there is intent which should
be proven i.e. it should be knowing and
wilful.
3. The exceptions to Stark law apply to the physicians that referred to the Medicare and
Medicaid patient for the particular service known as DHS by which they have a financial
relationship. (Adashi, E. Y., 2015) It includes many exceptions to this law that prohibits
BASIS STARK LAW ANTI-KICK BACK STATUE
PROHIBITS The Stark law prohibits the physicians
from referring the Medicare patients
for the designated health services for
the entity that shows a financial
relationship if in the case of exceptions
applies.
As per Anti-Kickback statue, it prohibits
in anything in the value that includes the
offering, paying, receiving that induce
the Federal health care business
programs
REFERRALS In this case, the referrals are from the
physician.
In this case, the referrals are from
anyone.
ITEMS OR
SERVICES
In the stark law the services related to
health care.
In the Anti-Kickback statue the item or
services of anything.
INTENT In this case, there is no purpose or
standard for the overpayment.
In this case, there is intent which should
be proven i.e. it should be knowing and
wilful.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Memo 6
in the Stark II Regs which based on the facts of specific analysis as well as the
application of the certain terms which as follows:
a. Physical services: It includes the services that are furnished which are personally by
another physician who is the member of referred physician group.
b. In-office Ancillary Services: These are furnished by the referring the physician who is
the member of the same physical group.
c. Organization services: These services are furnished if the organization is providing
services to the health plans which are a contract to HCFA that provide services to
medical beneficiaries.
d. Services related to client laboratories: These are exempted from the Stark law
probation as in case if the charges for DHS that include at ASC Rate (Ambulatory
surgical Center).
Also, there are other exceptions which include the financial relationship are as follows:
Payment of office space and equipment.
Real employment relationships.
Recruitment of the Physician.
The arrangement of the personal services.
Compensation agreement in stark law suggests that it prohibited from referring the
Medicare Beneficiaries to the entity for the selected health services in the case of
financial relationship of the physician with the entity. The law prohibits the entity from
the presenting the claims to the Medicare that prohibited the referral of DHS. The
in the Stark II Regs which based on the facts of specific analysis as well as the
application of the certain terms which as follows:
a. Physical services: It includes the services that are furnished which are personally by
another physician who is the member of referred physician group.
b. In-office Ancillary Services: These are furnished by the referring the physician who is
the member of the same physical group.
c. Organization services: These services are furnished if the organization is providing
services to the health plans which are a contract to HCFA that provide services to
medical beneficiaries.
d. Services related to client laboratories: These are exempted from the Stark law
probation as in case if the charges for DHS that include at ASC Rate (Ambulatory
surgical Center).
Also, there are other exceptions which include the financial relationship are as follows:
Payment of office space and equipment.
Real employment relationships.
Recruitment of the Physician.
The arrangement of the personal services.
Compensation agreement in stark law suggests that it prohibited from referring the
Medicare Beneficiaries to the entity for the selected health services in the case of
financial relationship of the physician with the entity. The law prohibits the entity from
the presenting the claims to the Medicare that prohibited the referral of DHS. The
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Memo 7
physicians have the financial relationship with the entity only when the person has the
ownership interest in the entity or the direct compensation agreement with the individual.
Then a physician, as well as the entity, were held strictly liable under the Stark and in
case if there is a prohibited referral for the DHS is made a claim is presented to the
Medicare, irrespective of the intent, and this can be further ordered for paying the
financial penalty as well as for damages.
Rationale of Stark Law
The rationale of the Stark law is that the physicians should perform as per the best
interest of the patient and not for the financial interest of surgeons and these financial
arrangements could encourage the extreme use of the services that drives up the cost of
the health care. (Sloss, D. L. 2013)
4. The section of Social Security Act of 1877 which commonly known as physician self-
referral law also refers to the Stark law. When enacted was passed in 1989 of the social
security act 1877 it applies only to the physician referrals for the services of the clinical
laboratory. In the year 1993 and 1994, the Congress expanded the ban to additional DHS
that applies certain aspects of the physician's self-referral law to the Medicaid program.
Then, in the year 1997, the Congress adds a provision which permits the Secretary to
issue the written advisory opinion which concerns that whether a referral relating to DHS
is prohibited under the section of 1877 of the social security act. After that in the year
2003, the Congress authorized the Secretary to spread an exception to the physician self-
referral prohibitions for the certain arrangements where they receive the non-monetary
remuneration which is necessary and which can be used solely to accept and transmit the
physicians have the financial relationship with the entity only when the person has the
ownership interest in the entity or the direct compensation agreement with the individual.
Then a physician, as well as the entity, were held strictly liable under the Stark and in
case if there is a prohibited referral for the DHS is made a claim is presented to the
Medicare, irrespective of the intent, and this can be further ordered for paying the
financial penalty as well as for damages.
Rationale of Stark Law
The rationale of the Stark law is that the physicians should perform as per the best
interest of the patient and not for the financial interest of surgeons and these financial
arrangements could encourage the extreme use of the services that drives up the cost of
the health care. (Sloss, D. L. 2013)
4. The section of Social Security Act of 1877 which commonly known as physician self-
referral law also refers to the Stark law. When enacted was passed in 1989 of the social
security act 1877 it applies only to the physician referrals for the services of the clinical
laboratory. In the year 1993 and 1994, the Congress expanded the ban to additional DHS
that applies certain aspects of the physician's self-referral law to the Medicaid program.
Then, in the year 1997, the Congress adds a provision which permits the Secretary to
issue the written advisory opinion which concerns that whether a referral relating to DHS
is prohibited under the section of 1877 of the social security act. After that in the year
2003, the Congress authorized the Secretary to spread an exception to the physician self-
referral prohibitions for the certain arrangements where they receive the non-monetary
remuneration which is necessary and which can be used solely to accept and transmit the
Memo 8
electronic prescription information that established a provisional moratorium on
physician referrals to the specific specialty hospitals where the referring physician has the
investment interest.
The proposed rule have been finalized into three phases as the phase I comment was
2001, the Issue Period of phase II was 2004, and in the year 2007 phase III was issued.
Then they publish other projected and the final rules which affect the physician self-
referral.
Example
The example of proposed and final rules includes the nuclear medicine inside existing in
the DHS groups and a planned and final rule that relates the electronic prescribing the
technology and electronic health records technology. Soon following Phase III in 2007, it
publishes the amendments related to physician self-referral regulation in the Year 2008,
and at the same time, it published revisions for the next year which was 2009 the Hospital
Inpatient Prospective Payment System final rule.
Moreover, as the regulations define certain DHS, it will publish annually in the schedule
of the Physician fee and update the relevant code for the relevant of DHS. After that in
the year 2010, it publishes the Medicare self-referral disclosure protocol which pursuant
under section 6409(a) of the Patient Protection Act. The set out the process which enables
the providers of the services and the supplier to disclose the actual violation of the
physician self-referral statue. Also, the Section 6409(b) give the Secretary of the
electronic prescription information that established a provisional moratorium on
physician referrals to the specific specialty hospitals where the referring physician has the
investment interest.
The proposed rule have been finalized into three phases as the phase I comment was
2001, the Issue Period of phase II was 2004, and in the year 2007 phase III was issued.
Then they publish other projected and the final rules which affect the physician self-
referral.
Example
The example of proposed and final rules includes the nuclear medicine inside existing in
the DHS groups and a planned and final rule that relates the electronic prescribing the
technology and electronic health records technology. Soon following Phase III in 2007, it
publishes the amendments related to physician self-referral regulation in the Year 2008,
and at the same time, it published revisions for the next year which was 2009 the Hospital
Inpatient Prospective Payment System final rule.
Moreover, as the regulations define certain DHS, it will publish annually in the schedule
of the Physician fee and update the relevant code for the relevant of DHS. After that in
the year 2010, it publishes the Medicare self-referral disclosure protocol which pursuant
under section 6409(a) of the Patient Protection Act. The set out the process which enables
the providers of the services and the supplier to disclose the actual violation of the
physician self-referral statue. Also, the Section 6409(b) give the Secretary of the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Memo 9
authority to decline the amount which is due and the violation of the social security act
1977.
Corporate Integrity Agreement is defined as an enforcement tool which is used by the
officer of General Inspector of the Department of Health and Human Services
5. Inspector General in the Department of Health and Human Services which improve the
quality of health care and to promote the compliance of health care regulations.
The one violation of the Anti-kickback statue is a general prohibition that it prohibits to
the significant and wilful solicitation, proposal, and payment of several remunerations
either directly or indirectly, or in the form of cash or in kind:
(1) To refer an individual for the services that are covered under federal health care program
or,
(2) To recommend the purchase, rent, or order the goods or services under the federal health
care program. It can be broken into different forms:
1. There should be no remuneration in the form of cash or kind.
2. It may be solicited, accepted or received either by directly or indirectly.
3. Knowingly and willfully
4. The payment has been made in full or some part of the benefit of federal health care
program which includes Medicare and Medicaid. (Centers for Medicare and Medicaid
Services. 2013).
authority to decline the amount which is due and the violation of the social security act
1977.
Corporate Integrity Agreement is defined as an enforcement tool which is used by the
officer of General Inspector of the Department of Health and Human Services
5. Inspector General in the Department of Health and Human Services which improve the
quality of health care and to promote the compliance of health care regulations.
The one violation of the Anti-kickback statue is a general prohibition that it prohibits to
the significant and wilful solicitation, proposal, and payment of several remunerations
either directly or indirectly, or in the form of cash or in kind:
(1) To refer an individual for the services that are covered under federal health care program
or,
(2) To recommend the purchase, rent, or order the goods or services under the federal health
care program. It can be broken into different forms:
1. There should be no remuneration in the form of cash or kind.
2. It may be solicited, accepted or received either by directly or indirectly.
3. Knowingly and willfully
4. The payment has been made in full or some part of the benefit of federal health care
program which includes Medicare and Medicaid. (Centers for Medicare and Medicaid
Services. 2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Memo 10
Penalties
For the violation of Anti-kickback law is a punishable as well as criminal offense and it
will be punished up to the imprisonment of five years and/or a fine of $25,000. Violation
of the law is a felony, punishable by up to five years imprisonment and/or $25,000 fine.
Also, the violation may result in eliminating the federal health care programs which
include both the Medicare and Medicaid as well as parallel loss of the State licensure,
eliminate from the participation in managing the health care contracts.
6. Board of the director is liable for Stark and/or Anti-Trust Violation as a corporate
obligation to the public which may violate the law, and they were liable for it. Although
the board of directors is the governing body of the various types which includes
association which is responsible for an ultimate direction of the management of affairs in
the organization. It is responsible for making the policy, while the employees are
responsible for the execution of day-to-day management that help them to implement the
policy that the board has made. Also, there is a crucial legal responsibility for the actions
of the association and with the rest of the board.
The board acts legally only when there is a majority of the vote as well as when it is duly
constituted and proper conduction of the meeting. The board may delegate the authority
on behalf of itself to the others, which includes the committees but in some other cases, it
is still responsible for taking any action by the committee to whom it delegates the
authority.
The member of the board has no authority by virtue of being the member of the board in
the case of an individual. Though, the board may give additional responsibility to the
Penalties
For the violation of Anti-kickback law is a punishable as well as criminal offense and it
will be punished up to the imprisonment of five years and/or a fine of $25,000. Violation
of the law is a felony, punishable by up to five years imprisonment and/or $25,000 fine.
Also, the violation may result in eliminating the federal health care programs which
include both the Medicare and Medicaid as well as parallel loss of the State licensure,
eliminate from the participation in managing the health care contracts.
6. Board of the director is liable for Stark and/or Anti-Trust Violation as a corporate
obligation to the public which may violate the law, and they were liable for it. Although
the board of directors is the governing body of the various types which includes
association which is responsible for an ultimate direction of the management of affairs in
the organization. It is responsible for making the policy, while the employees are
responsible for the execution of day-to-day management that help them to implement the
policy that the board has made. Also, there is a crucial legal responsibility for the actions
of the association and with the rest of the board.
The board acts legally only when there is a majority of the vote as well as when it is duly
constituted and proper conduction of the meeting. The board may delegate the authority
on behalf of itself to the others, which includes the committees but in some other cases, it
is still responsible for taking any action by the committee to whom it delegates the
authority.
The member of the board has no authority by virtue of being the member of the board in
the case of an individual. Though, the board may give additional responsibility to the
Memo 11
board members, as it appoints the members of the committee. In such a way the board has
only the authority to the specifically delegated to the laws or the board, as it can be
general or in the abroad.
7. The list of sources for the future use which includes:
CFR Section
Centers for Medicare and Medicaid Services. (2013). CMS Manual System. Pub 100-07
State Operations Provider Certification. Appendix A. 42 CFR. Section 482.52. Revised
hospital anesthesia services interpretive guidelines, 14 Jan 2011.
Law related article
Lake, M. (2014). Organizing hypocrisy: providing legal accountability for human rights
violations in areas of limited statehood. International Studies Quarterly, 58(3), 515-526.
Links to federal website
Anthopoulos, L., Reddick, C. G., Giannakidou, I., & Mavridis, N. (2016). Why e-
government projects fail? An analysis of the Healthcare. gov website. Government
Information Quarterly, 33(1), 161-173.
Stakeholder Association for the hospitals
board members, as it appoints the members of the committee. In such a way the board has
only the authority to the specifically delegated to the laws or the board, as it can be
general or in the abroad.
7. The list of sources for the future use which includes:
CFR Section
Centers for Medicare and Medicaid Services. (2013). CMS Manual System. Pub 100-07
State Operations Provider Certification. Appendix A. 42 CFR. Section 482.52. Revised
hospital anesthesia services interpretive guidelines, 14 Jan 2011.
Law related article
Lake, M. (2014). Organizing hypocrisy: providing legal accountability for human rights
violations in areas of limited statehood. International Studies Quarterly, 58(3), 515-526.
Links to federal website
Anthopoulos, L., Reddick, C. G., Giannakidou, I., & Mavridis, N. (2016). Why e-
government projects fail? An analysis of the Healthcare. gov website. Government
Information Quarterly, 33(1), 161-173.
Stakeholder Association for the hospitals
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





