Effective Blood Pressure Management Strategies for SAH Patients Review
VerifiedAdded on 2022/10/04
|14
|3274
|443
Literature Review
AI Summary
This literature review focuses on the management of blood pressure in patients with subarachnoid hemorrhage (SAH), a life-threatening stroke caused by bleeding around the brain. The review synthesizes evidence on various techniques, including the use of nimodipine, osmotic diuretics, neurologic monitoring, ventilatory support, and surgical interventions. It explores the rationale behind blood pressure control, the risks associated with elevated intracranial pressure and vasospasm, and the importance of maintaining systolic blood pressure within a specific range to prevent further complications. The review also highlights the search strategy used, encompassing databases like PubMed and CINAHL, and the inclusion and exclusion criteria applied to select relevant articles. The article synthesis section discusses the importance of nimodipine in preventing delayed cerebral ischemia (DCI), the use of hypertensive therapy, and the role of pharmacological and non-pharmacological strategies in managing intracranial pressure. It also covers surgical interventions such as CSF diversion and the use of carbonic anhydrase inhibitors like acetazolamide for blood pressure management. The review concludes by emphasizing the need for individualized blood pressure management and the importance of tailoring autoregulation-based blood pressure targets to improve patient outcomes.

Running head: LITERATURE REVIEW
Blood pressure management of patients with SAH (subarachnoid haemorrhage)
Name of the Student
Name of the University
Author Note
Blood pressure management of patients with SAH (subarachnoid haemorrhage)
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1LITERATURE REVIEW
Executive summary
Subarachnoid haemorrhage (SAH) is an umbrella term that refers to life-threatening kind of
stroke that is generally caused due to bleeding into the region that surrounds the human brain.
SAH can be a direct manifestation of a ruptured aneurysm, or head injury. While several
patients recuperate from the condition, some survive with disability and the rest die. Hence,
the primary aim of treatment is to keep a check on the systolic blood pressure among such
patients. This literature review focused on different blood pressure management techniques
and provided evidence for administration and/or implementation of nimodipine, osmotic
diuretics, neurologic monitoring, ventilatory support, and surgical intervention.
Executive summary
Subarachnoid haemorrhage (SAH) is an umbrella term that refers to life-threatening kind of
stroke that is generally caused due to bleeding into the region that surrounds the human brain.
SAH can be a direct manifestation of a ruptured aneurysm, or head injury. While several
patients recuperate from the condition, some survive with disability and the rest die. Hence,
the primary aim of treatment is to keep a check on the systolic blood pressure among such
patients. This literature review focused on different blood pressure management techniques
and provided evidence for administration and/or implementation of nimodipine, osmotic
diuretics, neurologic monitoring, ventilatory support, and surgical intervention.
2LITERATURE REVIEW
Table of Contents
Introduction................................................................................................................................3
Rationale....................................................................................................................................3
Research question.......................................................................................................................4
Search strategy...........................................................................................................................4
Article synthesis.........................................................................................................................5
Conclusion..................................................................................................................................9
References................................................................................................................................11
Table of Contents
Introduction................................................................................................................................3
Rationale....................................................................................................................................3
Research question.......................................................................................................................4
Search strategy...........................................................................................................................4
Article synthesis.........................................................................................................................5
Conclusion..................................................................................................................................9
References................................................................................................................................11
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3LITERATURE REVIEW
Introduction
Also denoted by SAH, subarachnoid haemorrhage refers to bleeding inside the space
that is present between the pia mater and the arachnoid membrane surrounding the human
brain, also referred to as the subarachnoid space. Some common signs and symptoms of SAH
comprise of vomiting, severe headache of fast onset, fever, reduced level of consciousness,
and sometimes seizures. Some of the most common reasons behind the onset of SAH are
trauma that involve a blow to the human head (Teoh et al. 2019). In addition, traumatic SAH
have been identified to occur at the location of skull fracture and/or intracerebral contusion.
The event also occurs among patients who are subjected to cerebral aneurysm that refers to
the presence of weakness at the arterial walls, thus leading to their enlargement. According to
Macdonald and Schweizer (2017) the initial steps that are adopted for assessment of patients
with SAH encompass obtaining detailed medical history and conducting a physical
examination. Furthermore, computed tomography and lumbar puncture are also performed
for SAH diagnosis. This assignment will contain a literature review that will highlight the
strategies that help in effective blood pressure management among SAH patients.
Rationale
Research evidences highlight the fact that surrounded within the firm skull, build-up
of fluid and clotted blood inside the brain results in an increase in blood pressure that
eventually crushes the brain against the cranium and might even bring about shifting or
herniation. Under such circumstances when CSF circulation gets blocked, there occurs
enlargement of the ventricles (hydrocephalus), thus causing lethargy, confusion, and loss of
consciousness (Long et al. 2019). One common complication under such circumstance is
vasospasm that may occur few days after the onset of SAH. Blood by-products generally
result in contraction and subsequent spasm of the walls of the artery, thereby narrowing the
Introduction
Also denoted by SAH, subarachnoid haemorrhage refers to bleeding inside the space
that is present between the pia mater and the arachnoid membrane surrounding the human
brain, also referred to as the subarachnoid space. Some common signs and symptoms of SAH
comprise of vomiting, severe headache of fast onset, fever, reduced level of consciousness,
and sometimes seizures. Some of the most common reasons behind the onset of SAH are
trauma that involve a blow to the human head (Teoh et al. 2019). In addition, traumatic SAH
have been identified to occur at the location of skull fracture and/or intracerebral contusion.
The event also occurs among patients who are subjected to cerebral aneurysm that refers to
the presence of weakness at the arterial walls, thus leading to their enlargement. According to
Macdonald and Schweizer (2017) the initial steps that are adopted for assessment of patients
with SAH encompass obtaining detailed medical history and conducting a physical
examination. Furthermore, computed tomography and lumbar puncture are also performed
for SAH diagnosis. This assignment will contain a literature review that will highlight the
strategies that help in effective blood pressure management among SAH patients.
Rationale
Research evidences highlight the fact that surrounded within the firm skull, build-up
of fluid and clotted blood inside the brain results in an increase in blood pressure that
eventually crushes the brain against the cranium and might even bring about shifting or
herniation. Under such circumstances when CSF circulation gets blocked, there occurs
enlargement of the ventricles (hydrocephalus), thus causing lethargy, confusion, and loss of
consciousness (Long et al. 2019). One common complication under such circumstance is
vasospasm that may occur few days after the onset of SAH. Blood by-products generally
result in contraction and subsequent spasm of the walls of the artery, thereby narrowing the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4LITERATURE REVIEW
arterial lumen, and restricting blood flow to particular regions of the brain. This increase in
blood pressure is therefore associated with the onset of secondary stroke.
Furthermore, as a direct outcome of sympathetic surge, there occurs a sudden upsurge
in blood pressure, which in turn is mediated by ventricle contractility and increase in
vasoconstriction (Bala, Gnanalingham and Gnanalingham 2019). This is also associated with
an upsurge in systemic vascular resistance that creates severe and life-threatening health
consequences. Furthermore, at the time of treating a patient diagnosed with SAH, body
stabilisation remains the first priority, for which the respiratory rate, blood pressure and pulse
are measured at regular intervals. With the aim of preventing further bleeding, it is also
recommended that the systolic blood pressure must be maintained between 140 and 160
mmHg. Thus, high blood pressure is a major risk factor that increases the likelihood of
patients to be affected by SAH, consequently any form of treatment such as, radiologically
mediated interventions or neurosurgery require effective management of blood pressure to
enhance patient health outcomes (Fahmy et al. 2019). However, there is lack of awareness on
the strategies that can be adopted for management of elevated blood pressure amid SAH
patients, which calls for the need of conducting this literature review that will contain a
summary of pertinent articles.
Research question
What strategies can help in effective blood pressure management of patients with
SAH?
Search strategy
Polit and Beck (2014) have often illustrated that identification of search terms and key
phrases forms an essential aspect of literature review, which in turn facilitates the extraction
of relevant scholarly pieces of evidences, in relation to the phenomenon under investigation.
arterial lumen, and restricting blood flow to particular regions of the brain. This increase in
blood pressure is therefore associated with the onset of secondary stroke.
Furthermore, as a direct outcome of sympathetic surge, there occurs a sudden upsurge
in blood pressure, which in turn is mediated by ventricle contractility and increase in
vasoconstriction (Bala, Gnanalingham and Gnanalingham 2019). This is also associated with
an upsurge in systemic vascular resistance that creates severe and life-threatening health
consequences. Furthermore, at the time of treating a patient diagnosed with SAH, body
stabilisation remains the first priority, for which the respiratory rate, blood pressure and pulse
are measured at regular intervals. With the aim of preventing further bleeding, it is also
recommended that the systolic blood pressure must be maintained between 140 and 160
mmHg. Thus, high blood pressure is a major risk factor that increases the likelihood of
patients to be affected by SAH, consequently any form of treatment such as, radiologically
mediated interventions or neurosurgery require effective management of blood pressure to
enhance patient health outcomes (Fahmy et al. 2019). However, there is lack of awareness on
the strategies that can be adopted for management of elevated blood pressure amid SAH
patients, which calls for the need of conducting this literature review that will contain a
summary of pertinent articles.
Research question
What strategies can help in effective blood pressure management of patients with
SAH?
Search strategy
Polit and Beck (2014) have often illustrated that identification of search terms and key
phrases forms an essential aspect of literature review, which in turn facilitates the extraction
of relevant scholarly pieces of evidences, in relation to the phenomenon under investigation.
5LITERATURE REVIEW
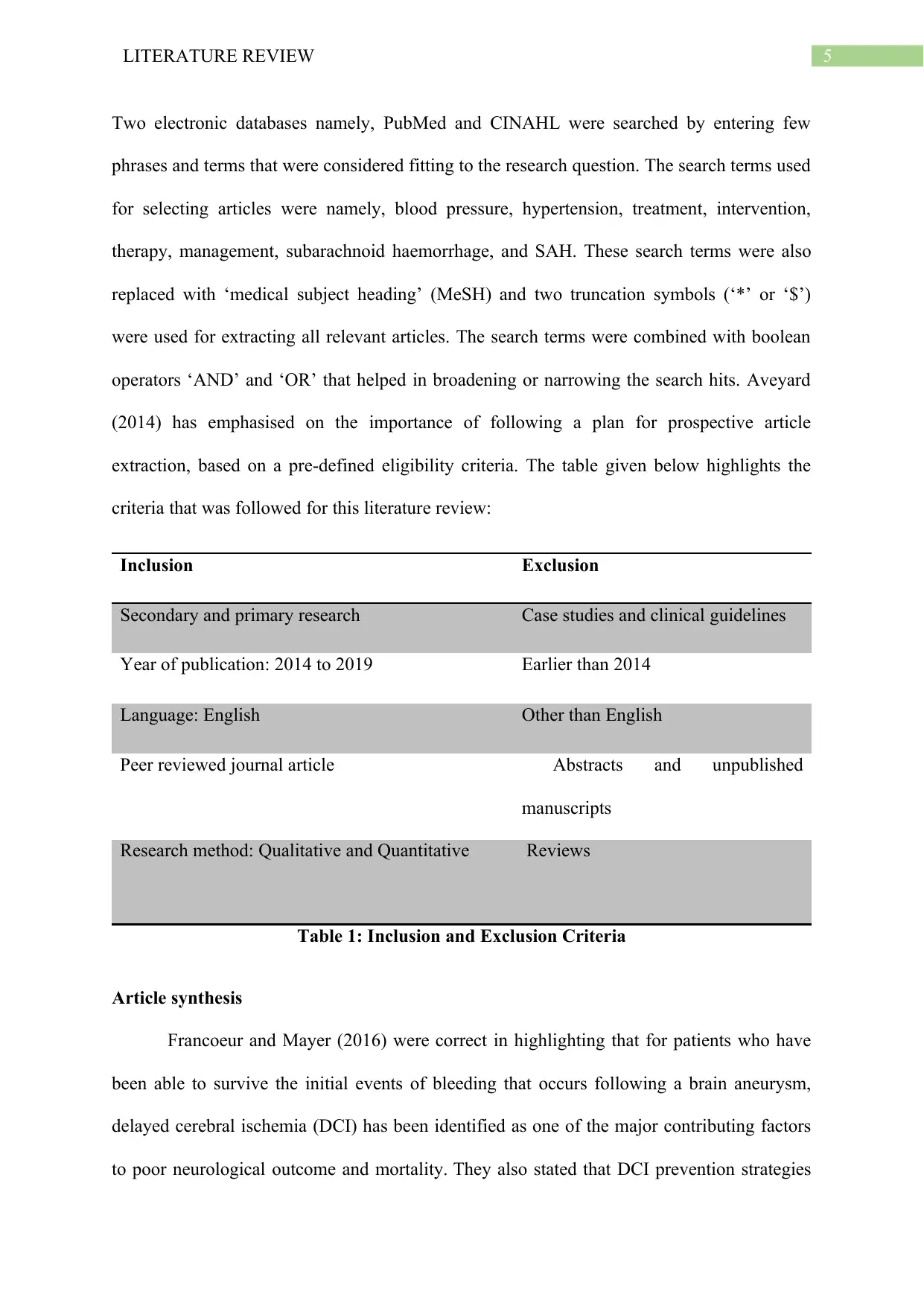
Two electronic databases namely, PubMed and CINAHL were searched by entering few
phrases and terms that were considered fitting to the research question. The search terms used
for selecting articles were namely, blood pressure, hypertension, treatment, intervention,
therapy, management, subarachnoid haemorrhage, and SAH. These search terms were also
replaced with ‘medical subject heading’ (MeSH) and two truncation symbols (‘*’ or ‘$’)
were used for extracting all relevant articles. The search terms were combined with boolean
operators ‘AND’ and ‘OR’ that helped in broadening or narrowing the search hits. Aveyard
(2014) has emphasised on the importance of following a plan for prospective article
extraction, based on a pre-defined eligibility criteria. The table given below highlights the
criteria that was followed for this literature review:
Inclusion Exclusion
Secondary and primary research Case studies and clinical guidelines
Year of publication: 2014 to 2019 Earlier than 2014
Language: English Other than English
Peer reviewed journal article Abstracts and unpublished
manuscripts
Research method: Qualitative and Quantitative Reviews
Table 1: Inclusion and Exclusion Criteria
Article synthesis
Francoeur and Mayer (2016) were correct in highlighting that for patients who have
been able to survive the initial events of bleeding that occurs following a brain aneurysm,
delayed cerebral ischemia (DCI) has been identified as one of the major contributing factors
to poor neurological outcome and mortality. They also stated that DCI prevention strategies
Two electronic databases namely, PubMed and CINAHL were searched by entering few
phrases and terms that were considered fitting to the research question. The search terms used
for selecting articles were namely, blood pressure, hypertension, treatment, intervention,
therapy, management, subarachnoid haemorrhage, and SAH. These search terms were also
replaced with ‘medical subject heading’ (MeSH) and two truncation symbols (‘*’ or ‘$’)
were used for extracting all relevant articles. The search terms were combined with boolean
operators ‘AND’ and ‘OR’ that helped in broadening or narrowing the search hits. Aveyard
(2014) has emphasised on the importance of following a plan for prospective article
extraction, based on a pre-defined eligibility criteria. The table given below highlights the
criteria that was followed for this literature review:
Inclusion Exclusion
Secondary and primary research Case studies and clinical guidelines
Year of publication: 2014 to 2019 Earlier than 2014
Language: English Other than English
Peer reviewed journal article Abstracts and unpublished
manuscripts
Research method: Qualitative and Quantitative Reviews
Table 1: Inclusion and Exclusion Criteria
Article synthesis
Francoeur and Mayer (2016) were correct in highlighting that for patients who have
been able to survive the initial events of bleeding that occurs following a brain aneurysm,
delayed cerebral ischemia (DCI) has been identified as one of the major contributing factors
to poor neurological outcome and mortality. They also stated that DCI prevention strategies
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6LITERATURE REVIEW
predominantly rely on administration of nimodipine, besides blood volume and cardiac
performance optimisation. The researchers illustrated that initially systolic target fluctuating
between 160 and 180 mmHg is carefully chosen, depending on the baseline blood pressure of
the patient. This is followed by administration of vasopressors to increase blood pressure,
which has been acknowledged as the first-line treatment for DCI. Under most circumstances,
the patient is subjected to a normal saline bolus (15 ml/kg over a duration of 1 hour) which
gradually increases the cerebral blood flow (CBF). Furthermore dopamine, norepinephrine,
and phenylephrine-mediated hypertension also bring about significant improvements in
cerebral oxygenation and CBF, thus preventing neurological deficit in around 70% patients.
However, it has been argued by Suwatcharangkoon et al. (2019) failure of the patients
to show response towards induced hypertension therapy for symptomatic vasospasm
intimidates their long-term health outcomes. The researchers performed a retrospective
analysis among1520 SAH patients, and found that 21% patients were subjected to
hypertensive therapy. This mode of treatment was administered with the sole objective of
lowering elevated blood pressure, thus protecting the internal organs like the heart and the
brain from further damage. The patients subjected to this therapy were administered 60 mg of
oral nimodipine, after an interval of four hours, unless the systolic blood pressure was less
than 140 mm Hg. The therapy also comprised of 0.9% normal saline administration at a rate
of 1 mL/kg/hour, in addition to 5% 250 ml albumin solution. This treatment modality was
correct for reducing hypertension among the SAH patients since it has previously proved
effective in reducing hypertension. However, the researchers found that failure of the
treatment could be accredited to an increased susceptibility of severe disability or death
among the patients, aneurysm coiling (43% versus 20%; P=0.004), admission troponin I level
>0.3 μg/L (64% versus 28%; P=0.001), and association of >1 symptomatic vascular territory
predominantly rely on administration of nimodipine, besides blood volume and cardiac
performance optimisation. The researchers illustrated that initially systolic target fluctuating
between 160 and 180 mmHg is carefully chosen, depending on the baseline blood pressure of
the patient. This is followed by administration of vasopressors to increase blood pressure,
which has been acknowledged as the first-line treatment for DCI. Under most circumstances,
the patient is subjected to a normal saline bolus (15 ml/kg over a duration of 1 hour) which
gradually increases the cerebral blood flow (CBF). Furthermore dopamine, norepinephrine,
and phenylephrine-mediated hypertension also bring about significant improvements in
cerebral oxygenation and CBF, thus preventing neurological deficit in around 70% patients.
However, it has been argued by Suwatcharangkoon et al. (2019) failure of the patients
to show response towards induced hypertension therapy for symptomatic vasospasm
intimidates their long-term health outcomes. The researchers performed a retrospective
analysis among1520 SAH patients, and found that 21% patients were subjected to
hypertensive therapy. This mode of treatment was administered with the sole objective of
lowering elevated blood pressure, thus protecting the internal organs like the heart and the
brain from further damage. The patients subjected to this therapy were administered 60 mg of
oral nimodipine, after an interval of four hours, unless the systolic blood pressure was less
than 140 mm Hg. The therapy also comprised of 0.9% normal saline administration at a rate
of 1 mL/kg/hour, in addition to 5% 250 ml albumin solution. This treatment modality was
correct for reducing hypertension among the SAH patients since it has previously proved
effective in reducing hypertension. However, the researchers found that failure of the
treatment could be accredited to an increased susceptibility of severe disability or death
among the patients, aneurysm coiling (43% versus 20%; P=0.004), admission troponin I level
>0.3 μg/L (64% versus 28%; P=0.001), and association of >1 symptomatic vascular territory
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7LITERATURE REVIEW
at onset (39% versus 22%; P=0.02), which made them highlight the need of implementing
endovascular therapy for blood pressure management.
It has been postulated by Sacco and Delibert (2018) that hazardous and sustained rise
in intracranial pressure (ICP) acts as a significant risk factor for any patient who has suffered
a severe brain injury. Elevated intracranial pressure that fails to show response to initial
treatment are also considered refractory, or rICP. Taking into consideration the fact that such
patients are at an increased susceptibility of secondary brain injury and enduring loss of
function, the researchers stated that major pharmacological blood pressure management
techniques include interventions for agitation and pain, and administration of osmotic
diuretics and hypertonic saline (HTS). They were also correct in stating that remifentanil and
fentanyl are commonly used for the lowering hypertension, owing to their action on the
opioid receptors, located in the central nervous system, thus producing pain relief. They also
elaborated on the use of sedative agents like benzodiazepine and osmotic diuretics such as,
mannitol for lowering intracranial metabolism.
Showing similarity to the aforementioned pharmacological interventions, Sacco and
Davis (2019) also elaborated on several non-pharmacological strategies for the management
of increased blood pressure. Some of the common interventions discussed by the researchers
include neurologic monitoring (multimodal monitoring and bedside assessment), targeted
temperature management, fluid and electrolyte maintenance, ventilatory support, and surgical
intervention. They were correct in stating that appropriate positioning and respiratory and
hemodynamic monitoring and support of the patients bring about a decrease in ICP, thereby
improving CBF. Furthermore, it was also found that in order to reduce elevated ICP, patients
must be subjected to hyperventilation and fluid and electrolyte maintenance. Conducting
hyperventilation with target PaCO2 near 30-35 mm Hg results in vasodilation, thereby
increasing the pressure. The administration of fluid management was further supported by the
at onset (39% versus 22%; P=0.02), which made them highlight the need of implementing
endovascular therapy for blood pressure management.
It has been postulated by Sacco and Delibert (2018) that hazardous and sustained rise
in intracranial pressure (ICP) acts as a significant risk factor for any patient who has suffered
a severe brain injury. Elevated intracranial pressure that fails to show response to initial
treatment are also considered refractory, or rICP. Taking into consideration the fact that such
patients are at an increased susceptibility of secondary brain injury and enduring loss of
function, the researchers stated that major pharmacological blood pressure management
techniques include interventions for agitation and pain, and administration of osmotic
diuretics and hypertonic saline (HTS). They were also correct in stating that remifentanil and
fentanyl are commonly used for the lowering hypertension, owing to their action on the
opioid receptors, located in the central nervous system, thus producing pain relief. They also
elaborated on the use of sedative agents like benzodiazepine and osmotic diuretics such as,
mannitol for lowering intracranial metabolism.
Showing similarity to the aforementioned pharmacological interventions, Sacco and
Davis (2019) also elaborated on several non-pharmacological strategies for the management
of increased blood pressure. Some of the common interventions discussed by the researchers
include neurologic monitoring (multimodal monitoring and bedside assessment), targeted
temperature management, fluid and electrolyte maintenance, ventilatory support, and surgical
intervention. They were correct in stating that appropriate positioning and respiratory and
hemodynamic monitoring and support of the patients bring about a decrease in ICP, thereby
improving CBF. Furthermore, it was also found that in order to reduce elevated ICP, patients
must be subjected to hyperventilation and fluid and electrolyte maintenance. Conducting
hyperventilation with target PaCO2 near 30-35 mm Hg results in vasodilation, thereby
increasing the pressure. The administration of fluid management was further supported by the
8LITERATURE REVIEW
fact that 0.9% saline (NS) administration causes hypotension, thus enhancing health
outcomes.
These findings were supported by Markey et al. (2016) who elaborated on the use
of acetazolamide for management of idiopathic intracranial hypertension, based on its
impacts on CSF secretion modification at the choroid plexus. This drug was proved to trigger
the inhibition of enzyme carbonic anhydrase, thereby catalysing the transformation of carbon
dioxide and water to bicarbonate and hydrogen ions, thereby decreasing CSF secretion. The
researchers were also correct in stating that furosemide and topiramate, a migraine
prophylactic and antiepileptic have gained attention in recent years for the management of
increased blood pressure, owing to their action as carbonic anhydrase inhibitors, eventually
decreasing the blood pressure. Some surgical interventions that were considered effective by
the researchers were CSF diversion, optic nerve sheath fenestration, and dural venous sinus
stenting. These findings are in accordance with those presented by Satti, Leishangthem and
Chaudry (2015) who suggested that patients who report signs and symptoms of refractory
idiopathic intracranial hypertension are usually subjected to CSF diversion as the first-line
intervention. It was found that of the 435 patients who underwent CSF diversion,
improvements were observed amid 80% cases of headache, 54% in vision, and 70% in
papilledema. The effects of this intervention were further supported by presence of 7.6% and
32.9% major and minor complications, respectively.
According to Alshami et al. (2018) an estimated 86 million Americans aged more
than 20 years report an increase in blood pressure, and this increases their risks of suffering
from SAH and cerebrovascular accidents. The researchers were correct in stating that agents
such as, nicardipine, labetalol, and clevidipine have been identified effective for management
of elevated blood pressure. Nonetheless, they stated that administration of sodium
nitroprusside, a potent vasodilator, must be avoided owing to the particular concern of
fact that 0.9% saline (NS) administration causes hypotension, thus enhancing health
outcomes.
These findings were supported by Markey et al. (2016) who elaborated on the use
of acetazolamide for management of idiopathic intracranial hypertension, based on its
impacts on CSF secretion modification at the choroid plexus. This drug was proved to trigger
the inhibition of enzyme carbonic anhydrase, thereby catalysing the transformation of carbon
dioxide and water to bicarbonate and hydrogen ions, thereby decreasing CSF secretion. The
researchers were also correct in stating that furosemide and topiramate, a migraine
prophylactic and antiepileptic have gained attention in recent years for the management of
increased blood pressure, owing to their action as carbonic anhydrase inhibitors, eventually
decreasing the blood pressure. Some surgical interventions that were considered effective by
the researchers were CSF diversion, optic nerve sheath fenestration, and dural venous sinus
stenting. These findings are in accordance with those presented by Satti, Leishangthem and
Chaudry (2015) who suggested that patients who report signs and symptoms of refractory
idiopathic intracranial hypertension are usually subjected to CSF diversion as the first-line
intervention. It was found that of the 435 patients who underwent CSF diversion,
improvements were observed amid 80% cases of headache, 54% in vision, and 70% in
papilledema. The effects of this intervention were further supported by presence of 7.6% and
32.9% major and minor complications, respectively.
According to Alshami et al. (2018) an estimated 86 million Americans aged more
than 20 years report an increase in blood pressure, and this increases their risks of suffering
from SAH and cerebrovascular accidents. The researchers were correct in stating that agents
such as, nicardipine, labetalol, and clevidipine have been identified effective for management
of elevated blood pressure. Nonetheless, they stated that administration of sodium
nitroprusside, a potent vasodilator, must be avoided owing to the particular concern of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9LITERATURE REVIEW
increasing ICP, followed by a subsequent reduction in CBF. Individualised management of
increased blood pressure, following SAH was explained by Silverman et al. (2019) who
found that there existed a high correlation between non-invasive (NIRS) and invasive (ICP)
modalities for calculation of MAPopt (r=0.91, p=0.01). Presence of 51.4% median time
within the optimal range for blood pressure and linear association of percent time beyond LA
with poor functional outcomes also illustrated that calculating tailored autoregulation-based
BP targets helps in reducing risks for poor health outcomes.
According to Mollan et al. (2016) administration of the carbonic anhydrase inhibitor,
acetazolamide helps in bringing about clinical improvements in the patient, thereby reducing
the intracranial pressure. They supported the statement by using findings from the Neuro-
Ophthalmologic Research Disease Investigator Consortium (NORDIC) where 500 mg dosing
of acetazolamide enhanced the primary outcome, and improved patient health outcomes.
Nonetheless, Hutchinson et al. (2016) argued that implementing decompressive craniectomy
among patients who have suffered from traumatic brain injury, and report signs of refractory
intracranial hypertension, brought about noteworthy decrease in rates of mortality and also
reduced severe disability. On subjecting the patients to decompressive craniectomy, the GOS-
E distributions were 6.9% death among 201 patients assigned to surgical group, in
comparison to 48.9% amid 188 patients who were assigned to the medical group, thereby
helping the researchers highlight the effectiveness of conducting decompressive craniectomy
for blood pressure management.
Conclusion
Thus, it can be concluded that SAH refers to a condition characterised by the
extravasation of blood inside the subarachnoid space located between the pia and arachnoid
mater. The condition occurs in numerous clinical contexts, with the most prevalent being
cases of head trauma. Nonetheless, the common usage of the term SAH refers to non-
increasing ICP, followed by a subsequent reduction in CBF. Individualised management of
increased blood pressure, following SAH was explained by Silverman et al. (2019) who
found that there existed a high correlation between non-invasive (NIRS) and invasive (ICP)
modalities for calculation of MAPopt (r=0.91, p=0.01). Presence of 51.4% median time
within the optimal range for blood pressure and linear association of percent time beyond LA
with poor functional outcomes also illustrated that calculating tailored autoregulation-based
BP targets helps in reducing risks for poor health outcomes.
According to Mollan et al. (2016) administration of the carbonic anhydrase inhibitor,
acetazolamide helps in bringing about clinical improvements in the patient, thereby reducing
the intracranial pressure. They supported the statement by using findings from the Neuro-
Ophthalmologic Research Disease Investigator Consortium (NORDIC) where 500 mg dosing
of acetazolamide enhanced the primary outcome, and improved patient health outcomes.
Nonetheless, Hutchinson et al. (2016) argued that implementing decompressive craniectomy
among patients who have suffered from traumatic brain injury, and report signs of refractory
intracranial hypertension, brought about noteworthy decrease in rates of mortality and also
reduced severe disability. On subjecting the patients to decompressive craniectomy, the GOS-
E distributions were 6.9% death among 201 patients assigned to surgical group, in
comparison to 48.9% amid 188 patients who were assigned to the medical group, thereby
helping the researchers highlight the effectiveness of conducting decompressive craniectomy
for blood pressure management.
Conclusion
Thus, it can be concluded that SAH refers to a condition characterised by the
extravasation of blood inside the subarachnoid space located between the pia and arachnoid
mater. The condition occurs in numerous clinical contexts, with the most prevalent being
cases of head trauma. Nonetheless, the common usage of the term SAH refers to non-
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10LITERATURE REVIEW
traumatic haemorrhage, which typically occurs in the situation of a ruptured cerebral
aneurysm. Owing to the fact that increased blood pressure has been identified as a major risk
factor among patients, it is essential for the healthcare professionals to administer
medications and other non-pharmacological interventions that would reduce hypertension,
and enhance health outcomes.
traumatic haemorrhage, which typically occurs in the situation of a ruptured cerebral
aneurysm. Owing to the fact that increased blood pressure has been identified as a major risk
factor among patients, it is essential for the healthcare professionals to administer
medications and other non-pharmacological interventions that would reduce hypertension,
and enhance health outcomes.
11LITERATURE REVIEW
References
Alshami, A., Romero, C., Avila, A. and Varon, J., 2018. Management of Acute Hypertension
in Cerebrovascular Accidents. Ann Hypertens. 2018; 1 (1), 1002.
Aveyard, H., 2014. Doing a literature review in health and social care: A practical guide.
McGraw-Hill Education (UK).
Bala, A., Gnanalingham, S. and Gnanalingham, K., 2019. Thrombosis of abdominal aorta
precipitating fatal subarachnoid haemorrhage. BMJ case reports, 12(2).
Fahmy, J., Boumrah, T., Trippier, S., Hainsworth, A., Madigan, J., Pereira, E., Shtaya, A. and
Minhas, P., 2019. P117 Predictive factors of outcome in poor grade subarachnoid
haemorrhage (SAH). Journal of Neurology, Neurosurgery and Psychiatry, 90(3), p.e52.
Francoeur, C.L. and Mayer, S.A., 2016. Management of delayed cerebral ischemia after
subarachnoid hemorrhage. Critical care, 20(1), p.277.
Hutchinson, P.J., Kolias, A.G., Timofeev, I.S., Corteen, E.A., Czosnyka, M., Timothy, J.,
Anderson, I., Bulters, D.O., Belli, A., Eynon, C.A. and Wadley, J., 2016. Trial of
decompressive craniectomy for traumatic intracranial hypertension. New England Journal of
Medicine, 375(12), pp.1119-1130.
Long, C.Y., Huang, G.Q., Du, Q., Zhou, L.Q. and Zhou, J.H., 2019. The dynamic expression
of aquaporins 1 and 4 in rats with hydrocephalus induced by subarachnoid
haemorrhage. Folia Neuropathologica, 57(2), pp.182-195.
Macdonald, R.L. and Schweizer, T.A., 2017. Spontaneous subarachnoid haemorrhage. The
Lancet, 389(10069), pp.655-666.
References
Alshami, A., Romero, C., Avila, A. and Varon, J., 2018. Management of Acute Hypertension
in Cerebrovascular Accidents. Ann Hypertens. 2018; 1 (1), 1002.
Aveyard, H., 2014. Doing a literature review in health and social care: A practical guide.
McGraw-Hill Education (UK).
Bala, A., Gnanalingham, S. and Gnanalingham, K., 2019. Thrombosis of abdominal aorta
precipitating fatal subarachnoid haemorrhage. BMJ case reports, 12(2).
Fahmy, J., Boumrah, T., Trippier, S., Hainsworth, A., Madigan, J., Pereira, E., Shtaya, A. and
Minhas, P., 2019. P117 Predictive factors of outcome in poor grade subarachnoid
haemorrhage (SAH). Journal of Neurology, Neurosurgery and Psychiatry, 90(3), p.e52.
Francoeur, C.L. and Mayer, S.A., 2016. Management of delayed cerebral ischemia after
subarachnoid hemorrhage. Critical care, 20(1), p.277.
Hutchinson, P.J., Kolias, A.G., Timofeev, I.S., Corteen, E.A., Czosnyka, M., Timothy, J.,
Anderson, I., Bulters, D.O., Belli, A., Eynon, C.A. and Wadley, J., 2016. Trial of
decompressive craniectomy for traumatic intracranial hypertension. New England Journal of
Medicine, 375(12), pp.1119-1130.
Long, C.Y., Huang, G.Q., Du, Q., Zhou, L.Q. and Zhou, J.H., 2019. The dynamic expression
of aquaporins 1 and 4 in rats with hydrocephalus induced by subarachnoid
haemorrhage. Folia Neuropathologica, 57(2), pp.182-195.
Macdonald, R.L. and Schweizer, T.A., 2017. Spontaneous subarachnoid haemorrhage. The
Lancet, 389(10069), pp.655-666.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

