Salivary Tissue Case Study: Assessment and Management Strategies
VerifiedAdded on 2022/11/16
|21
|4038
|146
Case Study
AI Summary
This case study presents the assessment and management of a 45-year-old woman experiencing swelling below her lower jaw. The document meticulously details the diagnostic protocols, including extra and intra oral examinations, imaging techniques (ultrasonography, sialography, plain film radiographs, sialoendoscopy, MRI/CT scans), microbial culture tests, and biopsy, to determine the cause of the swelling, which is identified as sialolithiasis. The assessment also considers the patient's symptoms, such as "meal-time syndrome," and incorporates guidelines from the Royal College of Surgeons and NICE. The case study then explores various clinical management strategies, including lithotripsy, interventional sialography, sialoendoscopy, and gland-preserving surgery, while emphasizing the importance of patient preference and risk assessment in developing a personal care plan. The document also provides an overview of sialolithiasis, its causes, and its prevalence, highlighting the submandibular gland's susceptibility and the role of obstructive sialadenitis in the patient's condition.

Running head: SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Name of the Student
Name of the University
Author’s Note
SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Name of the Student
Name of the University
Author’s Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Case Study Topic:
A 45 year old woman attends the clinic, describing a history of swelling below her lower jaw
on the left side. The swelling is largest at meal times and gradually goes down. Assessment of
the case is required along with potential medical and therapeutic management of the patient.
Case Study Topic:
A 45 year old woman attends the clinic, describing a history of swelling below her lower jaw
on the left side. The swelling is largest at meal times and gradually goes down. Assessment of
the case is required along with potential medical and therapeutic management of the patient.
2SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Table of Contents
A. Introduction..............................................................................................................................3
B. Description of the case.............................................................................................................3
C. Procedure for assessment.........................................................................................................3
C. Diagnostic protocols................................................................................................................4
1. Extra and intra oral examinations.........................................................................................4
2. Imaging techniques...............................................................................................................5
a. Ultrasonography................................................................................................................6
b. Saliography.......................................................................................................................6
c. Plain film radiograph........................................................................................................7
d. Sialoendoscopy.................................................................................................................8
3. MRI or CT scans...................................................................................................................9
4. Microbial culture test..........................................................................................................10
5. Biopsy.................................................................................................................................10
D. Assessment of the case..........................................................................................................11
E. Possible Clinical Management strategies...............................................................................14
a. Lithotripsy (Conservative)...............................................................................................14
b. Interventional sialography...............................................................................................14
c. Sialoendoscopy................................................................................................................15
d. Gland-preserving surgery (endoscope assisted stone retrieval).......................................15
F. Conclusion..............................................................................................................................17
Table of Contents
A. Introduction..............................................................................................................................3
B. Description of the case.............................................................................................................3
C. Procedure for assessment.........................................................................................................3
C. Diagnostic protocols................................................................................................................4
1. Extra and intra oral examinations.........................................................................................4
2. Imaging techniques...............................................................................................................5
a. Ultrasonography................................................................................................................6
b. Saliography.......................................................................................................................6
c. Plain film radiograph........................................................................................................7
d. Sialoendoscopy.................................................................................................................8
3. MRI or CT scans...................................................................................................................9
4. Microbial culture test..........................................................................................................10
5. Biopsy.................................................................................................................................10
D. Assessment of the case..........................................................................................................11
E. Possible Clinical Management strategies...............................................................................14
a. Lithotripsy (Conservative)...............................................................................................14
b. Interventional sialography...............................................................................................14
c. Sialoendoscopy................................................................................................................15
d. Gland-preserving surgery (endoscope assisted stone retrieval).......................................15
F. Conclusion..............................................................................................................................17
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
G. References..............................................................................................................................18
A. Introduction
Swelling of the lower jaw might be caused by several factors namely blunt trauma,
infected glands in that region, diseased tooth, obstructed glands and so on. Moreover, there are
many causes, condition or diseases can lead to such swelling, stenosis or distress, for example:
radiation therapy, allergic reaction, autoimmune or granulomatous diseases, cases after trauma
or accident, anatomical variation or abnormalities, acute or chronic infections, or stones.
Proper assessment of the cause along with crucial analysis is required for correctly diagnosing
the cause and providing effective clinical management.
B. Description of the case
The patient, a 45 year old woman, has presented with swelling below her lower jaw on
the left side which enlarges to its maximum size during meal times and gradually goes down
post meal. The extensive examination is carried out, to check for infections and the address the
main causal point of the distress and swelling below the lower jaw.
C. Procedure for assessment
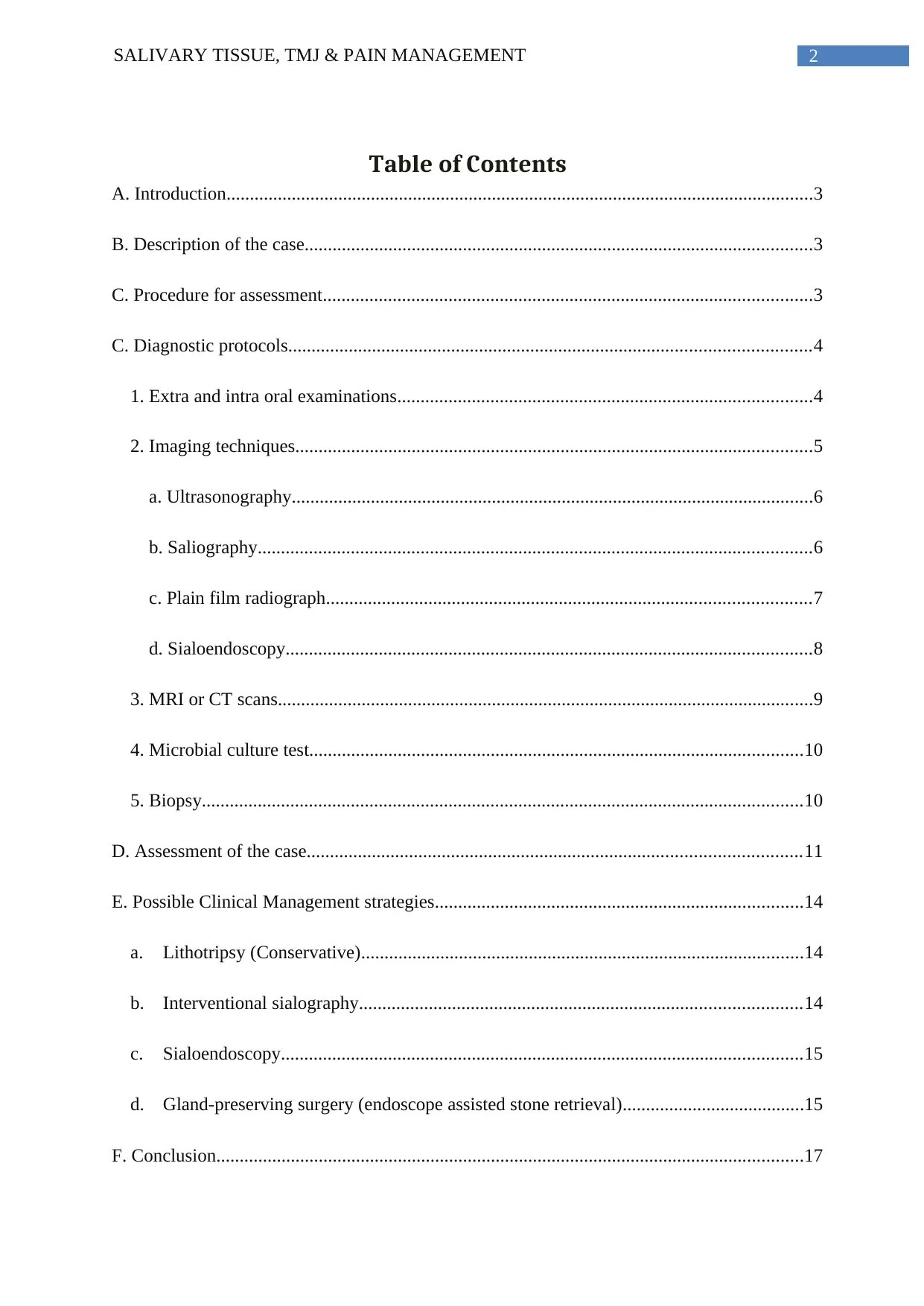
Diagnosis of lower jaw swelling and distress begins with a careful medical history,
head, and neck examination (Jonathan et al. 2002). Following the recommended guidelines of
the Royal College of Surgeon (scottishdental.org), the following points must be regarded while
assessing the medical case along with planning the clinical management strategies for personal
care plan.
G. References..............................................................................................................................18
A. Introduction
Swelling of the lower jaw might be caused by several factors namely blunt trauma,
infected glands in that region, diseased tooth, obstructed glands and so on. Moreover, there are
many causes, condition or diseases can lead to such swelling, stenosis or distress, for example:
radiation therapy, allergic reaction, autoimmune or granulomatous diseases, cases after trauma
or accident, anatomical variation or abnormalities, acute or chronic infections, or stones.
Proper assessment of the cause along with crucial analysis is required for correctly diagnosing
the cause and providing effective clinical management.
B. Description of the case
The patient, a 45 year old woman, has presented with swelling below her lower jaw on
the left side which enlarges to its maximum size during meal times and gradually goes down
post meal. The extensive examination is carried out, to check for infections and the address the
main causal point of the distress and swelling below the lower jaw.
C. Procedure for assessment
Diagnosis of lower jaw swelling and distress begins with a careful medical history,
head, and neck examination (Jonathan et al. 2002). Following the recommended guidelines of
the Royal College of Surgeon (scottishdental.org), the following points must be regarded while
assessing the medical case along with planning the clinical management strategies for personal
care plan.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
C. Diagnostic protocols
1. Extra and intra oral examinations
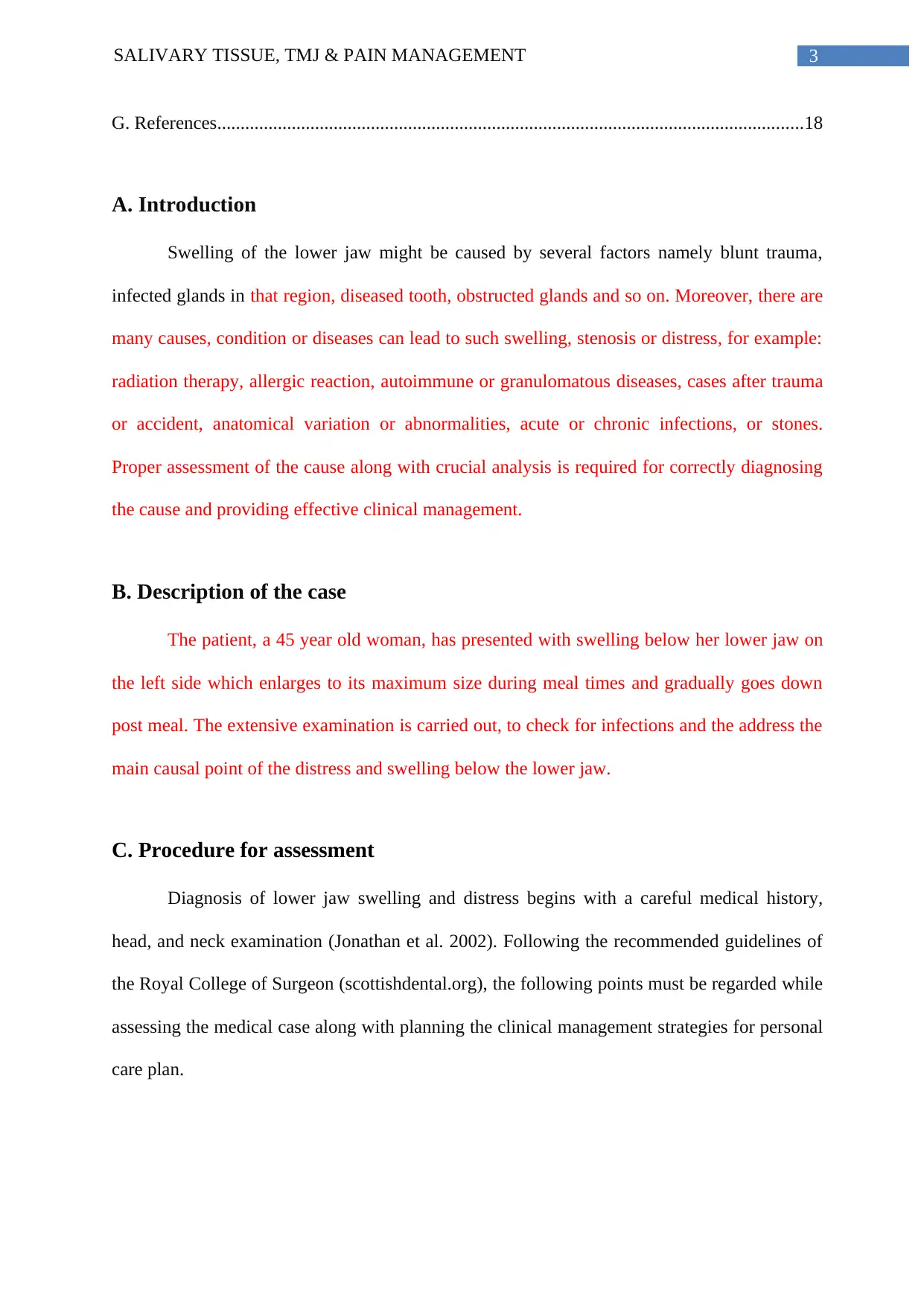
The extra oral examination to assess the asymmetry in the orofacial region and
limitation in opening, deviation or guarding, in addition, both lips should be examined by
palpation and visually for detection of any abnormality in the vermilion border and skin (Villa
et al. 2017). Digital palpation is highly recommended in case studies highlighted in the
Cochrane database (Figure 1 and 2), (Burghartz et al. 2018).
C. Diagnostic protocols
1. Extra and intra oral examinations
The extra oral examination to assess the asymmetry in the orofacial region and
limitation in opening, deviation or guarding, in addition, both lips should be examined by
palpation and visually for detection of any abnormality in the vermilion border and skin (Villa
et al. 2017). Digital palpation is highly recommended in case studies highlighted in the
Cochrane database (Figure 1 and 2), (Burghartz et al. 2018).
5SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Figure 1: Extra oral examination by digital palpation (Source: Villa et al. 2017)
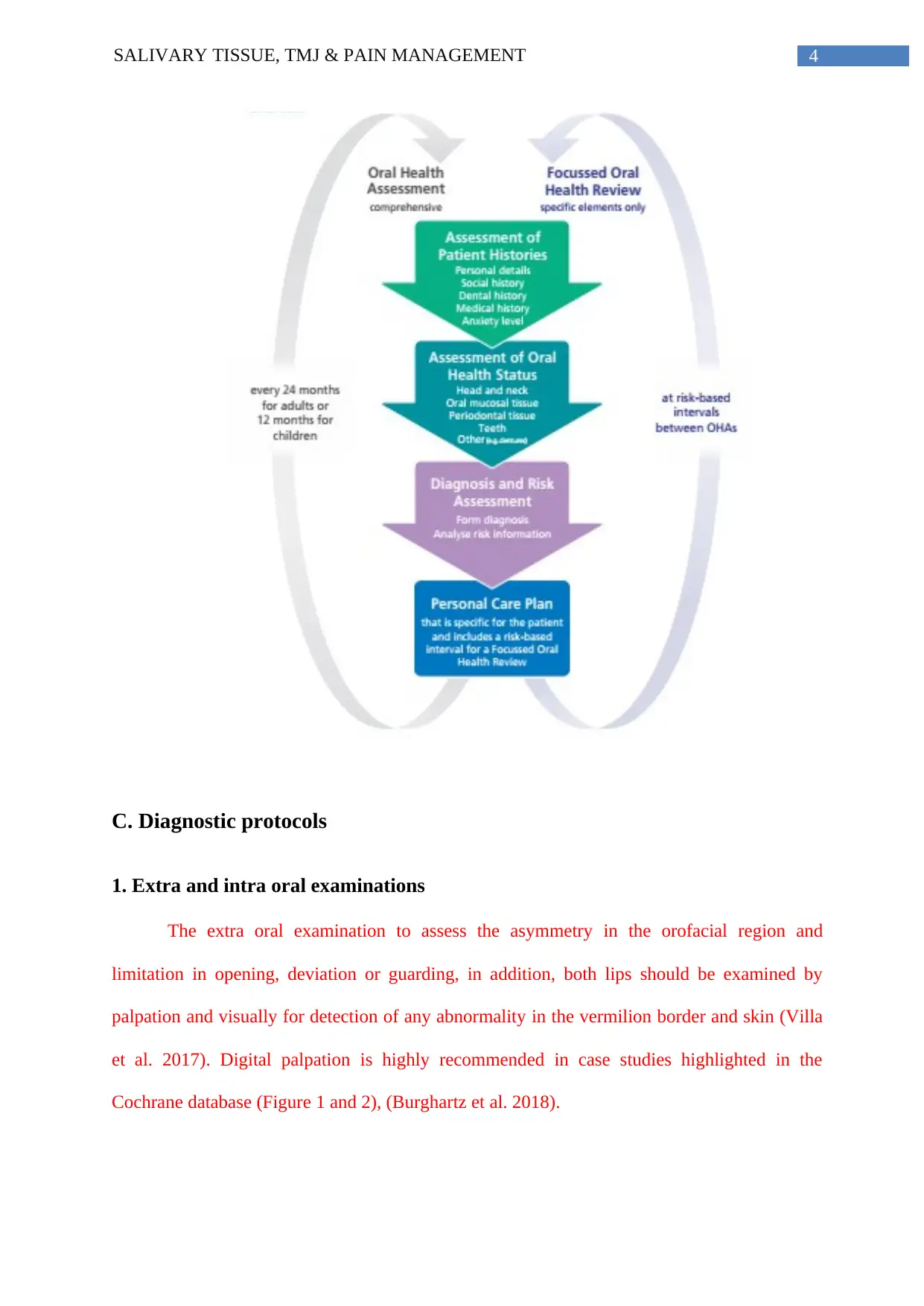
Figure 2: Intra oral investigation (Source: Villa et al. 2017).
In the intra oral examination assessment, systematic manner is essential to not miss the
anatomical structures; furthermore, each of the involved anatomical structures should be
palpated and visually inspected (Figure 2). For example: in case of oral lesion, size, texture,
and location, consistency, color, extent and tenderness are evaluated (Villa et al. 2017).
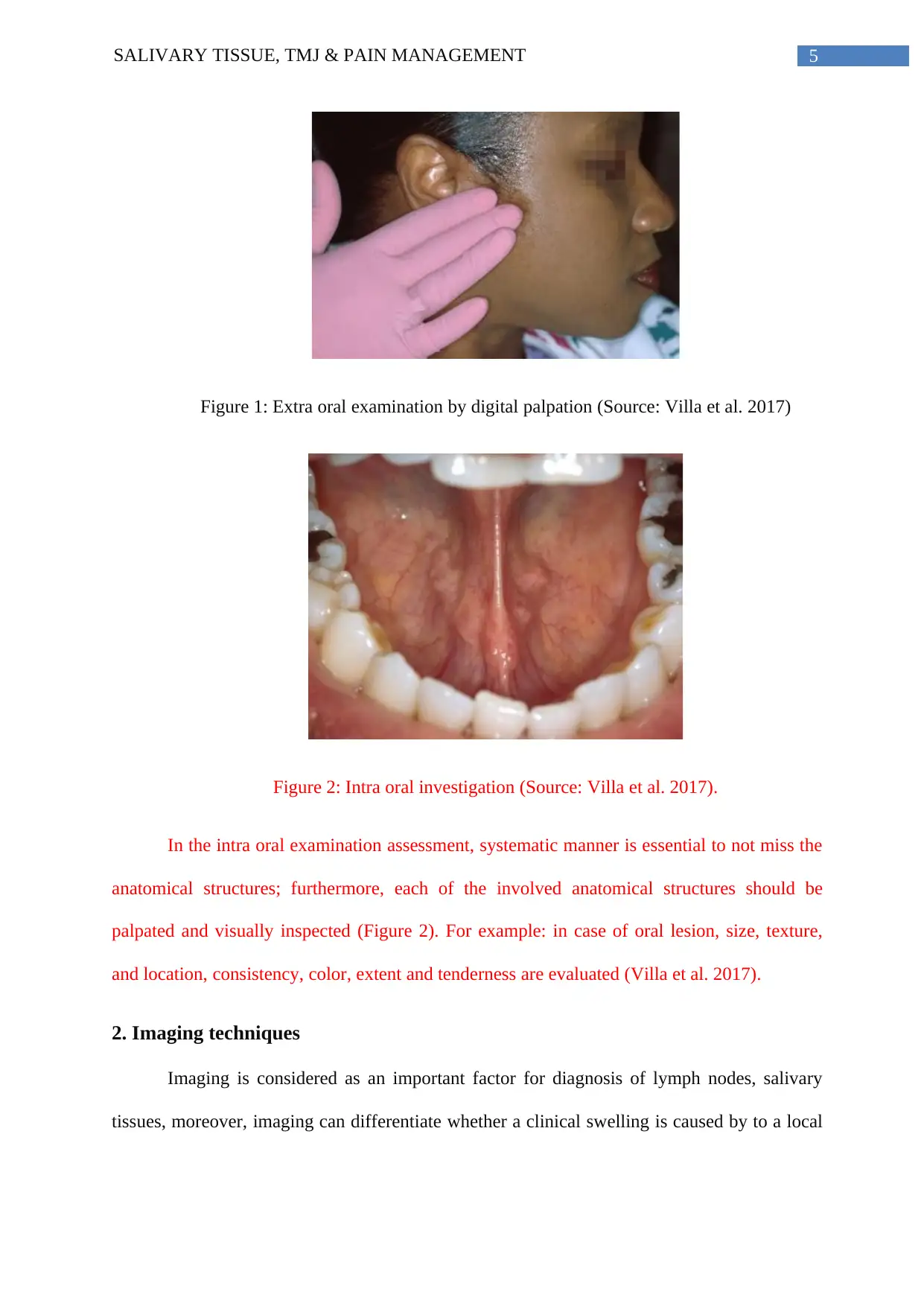
2. Imaging techniques
Imaging is considered as an important factor for diagnosis of lymph nodes, salivary
tissues, moreover, imaging can differentiate whether a clinical swelling is caused by to a local
Figure 1: Extra oral examination by digital palpation (Source: Villa et al. 2017)
Figure 2: Intra oral investigation (Source: Villa et al. 2017).
In the intra oral examination assessment, systematic manner is essential to not miss the
anatomical structures; furthermore, each of the involved anatomical structures should be
palpated and visually inspected (Figure 2). For example: in case of oral lesion, size, texture,
and location, consistency, color, extent and tenderness are evaluated (Villa et al. 2017).
2. Imaging techniques
Imaging is considered as an important factor for diagnosis of lymph nodes, salivary
tissues, moreover, imaging can differentiate whether a clinical swelling is caused by to a local
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
lesion or diffuse process, and whether a mass has occurred in extraglandular region by
diseases, swelling or infection of adjacent structure (Mehanna et al. 2012).
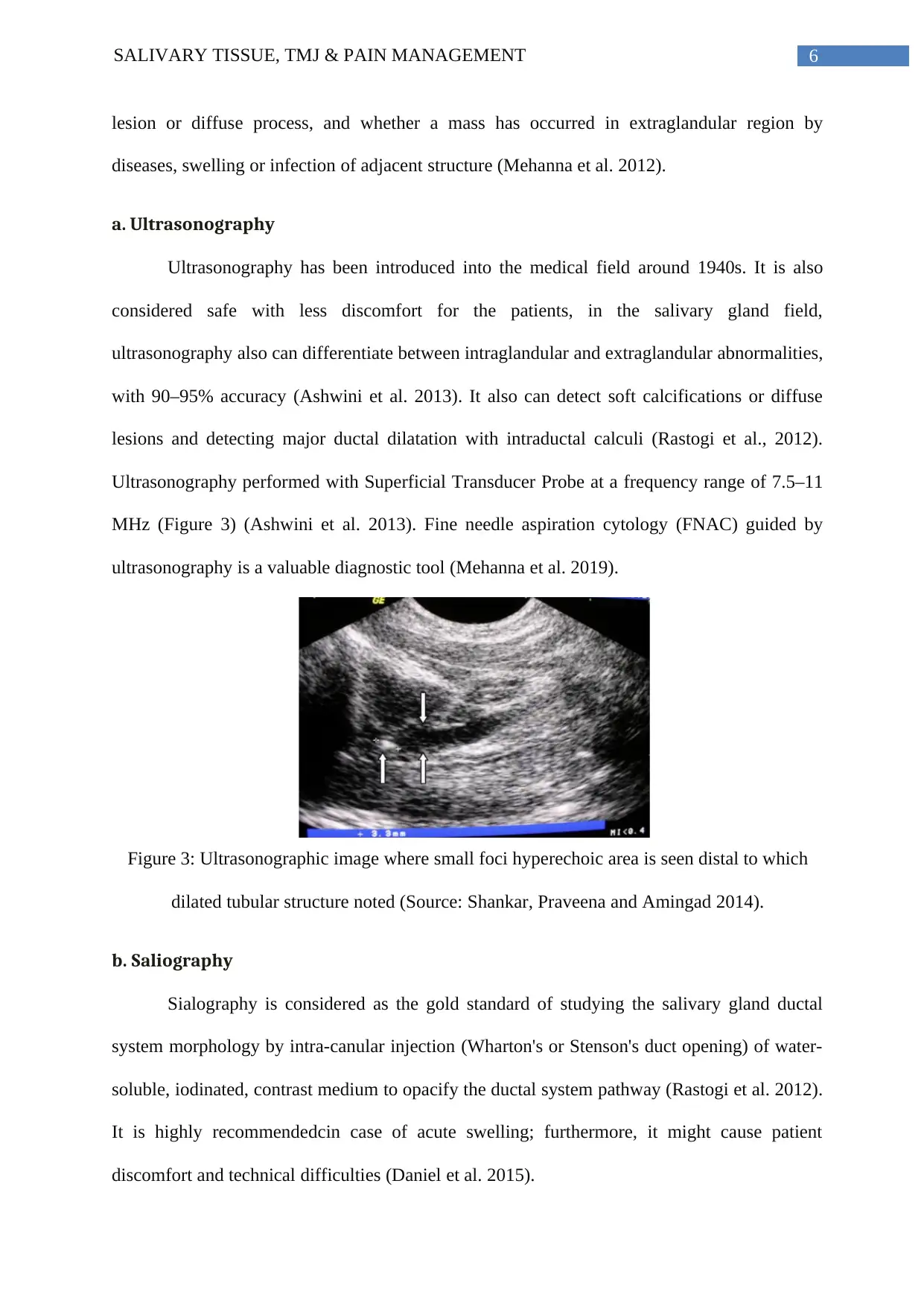
a. Ultrasonography
Ultrasonography has been introduced into the medical field around 1940s. It is also
considered safe with less discomfort for the patients, in the salivary gland field,
ultrasonography also can differentiate between intraglandular and extraglandular abnormalities,
with 90–95% accuracy (Ashwini et al. 2013). It also can detect soft calcifications or diffuse
lesions and detecting major ductal dilatation with intraductal calculi (Rastogi et al., 2012).
Ultrasonography performed with Superficial Transducer Probe at a frequency range of 7.5–11
MHz (Figure 3) (Ashwini et al. 2013). Fine needle aspiration cytology (FNAC) guided by
ultrasonography is a valuable diagnostic tool (Mehanna et al. 2019).
Figure 3: Ultrasonographic image where small foci hyperechoic area is seen distal to which
dilated tubular structure noted (Source: Shankar, Praveena and Amingad 2014).
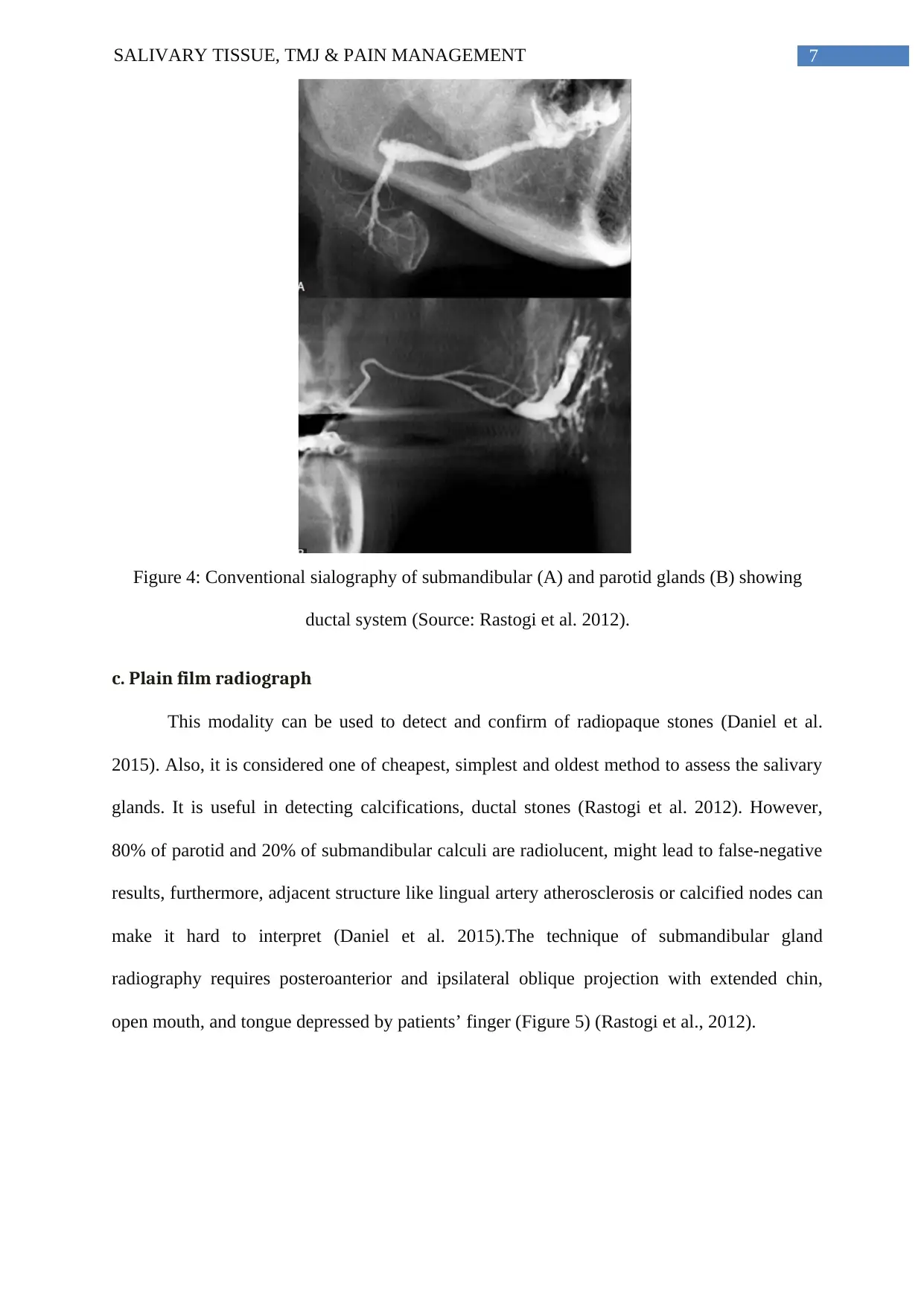
b. Saliography
Sialography is considered as the gold standard of studying the salivary gland ductal
system morphology by intra-canular injection (Wharton's or Stenson's duct opening) of water-
soluble, iodinated, contrast medium to opacify the ductal system pathway (Rastogi et al. 2012).
It is highly recommendedcin case of acute swelling; furthermore, it might cause patient
discomfort and technical difficulties (Daniel et al. 2015).
lesion or diffuse process, and whether a mass has occurred in extraglandular region by
diseases, swelling or infection of adjacent structure (Mehanna et al. 2012).
a. Ultrasonography
Ultrasonography has been introduced into the medical field around 1940s. It is also
considered safe with less discomfort for the patients, in the salivary gland field,
ultrasonography also can differentiate between intraglandular and extraglandular abnormalities,
with 90–95% accuracy (Ashwini et al. 2013). It also can detect soft calcifications or diffuse
lesions and detecting major ductal dilatation with intraductal calculi (Rastogi et al., 2012).
Ultrasonography performed with Superficial Transducer Probe at a frequency range of 7.5–11
MHz (Figure 3) (Ashwini et al. 2013). Fine needle aspiration cytology (FNAC) guided by
ultrasonography is a valuable diagnostic tool (Mehanna et al. 2019).
Figure 3: Ultrasonographic image where small foci hyperechoic area is seen distal to which
dilated tubular structure noted (Source: Shankar, Praveena and Amingad 2014).
b. Saliography
Sialography is considered as the gold standard of studying the salivary gland ductal
system morphology by intra-canular injection (Wharton's or Stenson's duct opening) of water-
soluble, iodinated, contrast medium to opacify the ductal system pathway (Rastogi et al. 2012).
It is highly recommendedcin case of acute swelling; furthermore, it might cause patient
discomfort and technical difficulties (Daniel et al. 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Figure 4: Conventional sialography of submandibular (A) and parotid glands (B) showing
ductal system (Source: Rastogi et al. 2012).
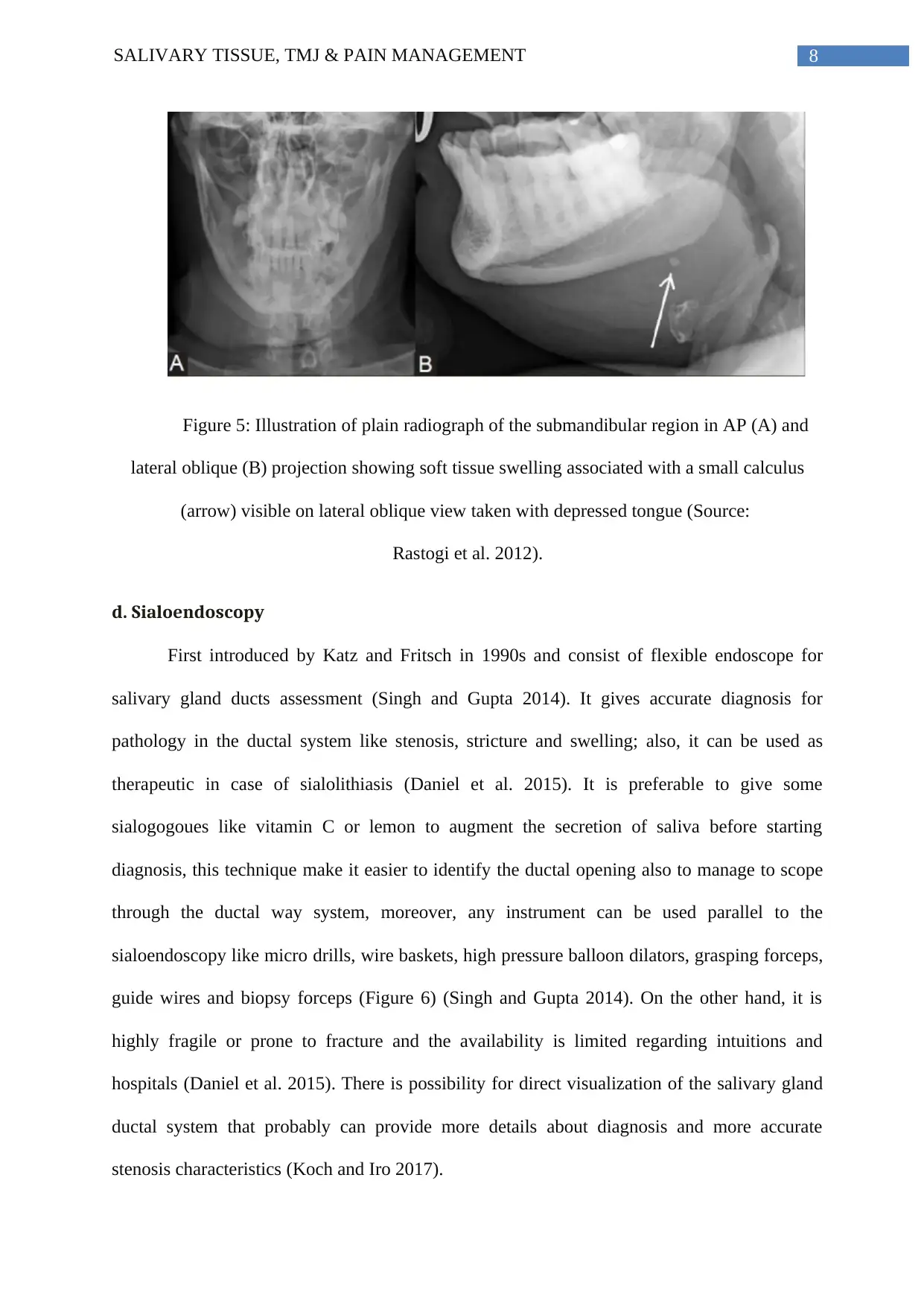
c. Plain film radiograph
This modality can be used to detect and confirm of radiopaque stones (Daniel et al.
2015). Also, it is considered one of cheapest, simplest and oldest method to assess the salivary
glands. It is useful in detecting calcifications, ductal stones (Rastogi et al. 2012). However,
80% of parotid and 20% of submandibular calculi are radiolucent, might lead to false-negative
results, furthermore, adjacent structure like lingual artery atherosclerosis or calcified nodes can
make it hard to interpret (Daniel et al. 2015).The technique of submandibular gland
radiography requires posteroanterior and ipsilateral oblique projection with extended chin,
open mouth, and tongue depressed by patients’ finger (Figure 5) (Rastogi et al., 2012).
Figure 4: Conventional sialography of submandibular (A) and parotid glands (B) showing
ductal system (Source: Rastogi et al. 2012).
c. Plain film radiograph
This modality can be used to detect and confirm of radiopaque stones (Daniel et al.
2015). Also, it is considered one of cheapest, simplest and oldest method to assess the salivary
glands. It is useful in detecting calcifications, ductal stones (Rastogi et al. 2012). However,
80% of parotid and 20% of submandibular calculi are radiolucent, might lead to false-negative
results, furthermore, adjacent structure like lingual artery atherosclerosis or calcified nodes can
make it hard to interpret (Daniel et al. 2015).The technique of submandibular gland
radiography requires posteroanterior and ipsilateral oblique projection with extended chin,
open mouth, and tongue depressed by patients’ finger (Figure 5) (Rastogi et al., 2012).
8SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Figure 5: Illustration of plain radiograph of the submandibular region in AP (A) and
lateral oblique (B) projection showing soft tissue swelling associated with a small calculus
(arrow) visible on lateral oblique view taken with depressed tongue (Source:
Rastogi et al. 2012).
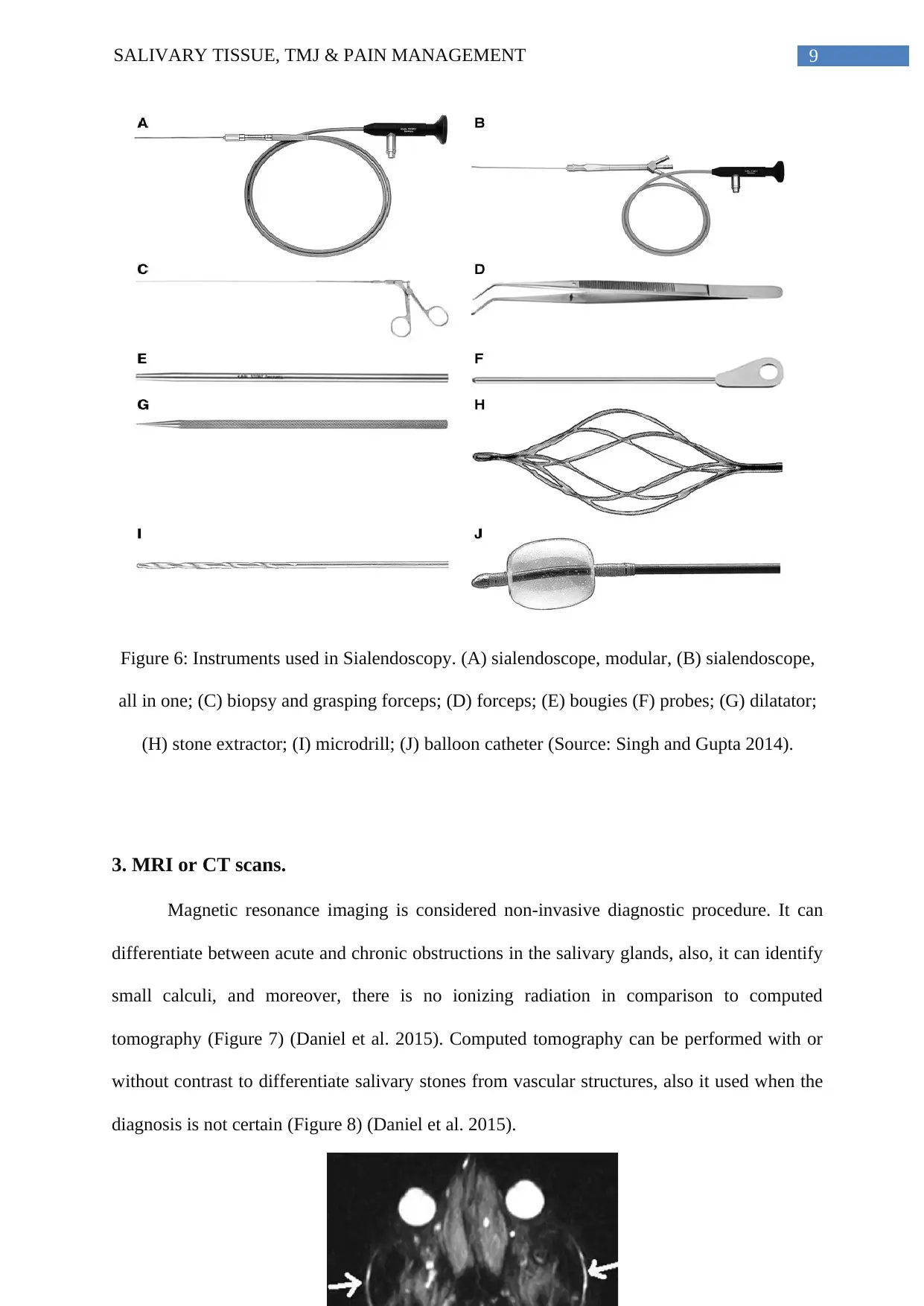
d. Sialoendoscopy
First introduced by Katz and Fritsch in 1990s and consist of flexible endoscope for
salivary gland ducts assessment (Singh and Gupta 2014). It gives accurate diagnosis for
pathology in the ductal system like stenosis, stricture and swelling; also, it can be used as
therapeutic in case of sialolithiasis (Daniel et al. 2015). It is preferable to give some
sialogogoues like vitamin C or lemon to augment the secretion of saliva before starting
diagnosis, this technique make it easier to identify the ductal opening also to manage to scope
through the ductal way system, moreover, any instrument can be used parallel to the
sialoendoscopy like micro drills, wire baskets, high pressure balloon dilators, grasping forceps,
guide wires and biopsy forceps (Figure 6) (Singh and Gupta 2014). On the other hand, it is
highly fragile or prone to fracture and the availability is limited regarding intuitions and
hospitals (Daniel et al. 2015). There is possibility for direct visualization of the salivary gland
ductal system that probably can provide more details about diagnosis and more accurate
stenosis characteristics (Koch and Iro 2017).
Figure 5: Illustration of plain radiograph of the submandibular region in AP (A) and
lateral oblique (B) projection showing soft tissue swelling associated with a small calculus
(arrow) visible on lateral oblique view taken with depressed tongue (Source:
Rastogi et al. 2012).
d. Sialoendoscopy
First introduced by Katz and Fritsch in 1990s and consist of flexible endoscope for
salivary gland ducts assessment (Singh and Gupta 2014). It gives accurate diagnosis for
pathology in the ductal system like stenosis, stricture and swelling; also, it can be used as
therapeutic in case of sialolithiasis (Daniel et al. 2015). It is preferable to give some
sialogogoues like vitamin C or lemon to augment the secretion of saliva before starting
diagnosis, this technique make it easier to identify the ductal opening also to manage to scope
through the ductal way system, moreover, any instrument can be used parallel to the
sialoendoscopy like micro drills, wire baskets, high pressure balloon dilators, grasping forceps,
guide wires and biopsy forceps (Figure 6) (Singh and Gupta 2014). On the other hand, it is
highly fragile or prone to fracture and the availability is limited regarding intuitions and
hospitals (Daniel et al. 2015). There is possibility for direct visualization of the salivary gland
ductal system that probably can provide more details about diagnosis and more accurate
stenosis characteristics (Koch and Iro 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Figure 6: Instruments used in Sialendoscopy. (A) sialendoscope, modular, (B) sialendoscope,
all in one; (C) biopsy and grasping forceps; (D) forceps; (E) bougies (F) probes; (G) dilatator;
(H) stone extractor; (I) microdrill; (J) balloon catheter (Source: Singh and Gupta 2014).
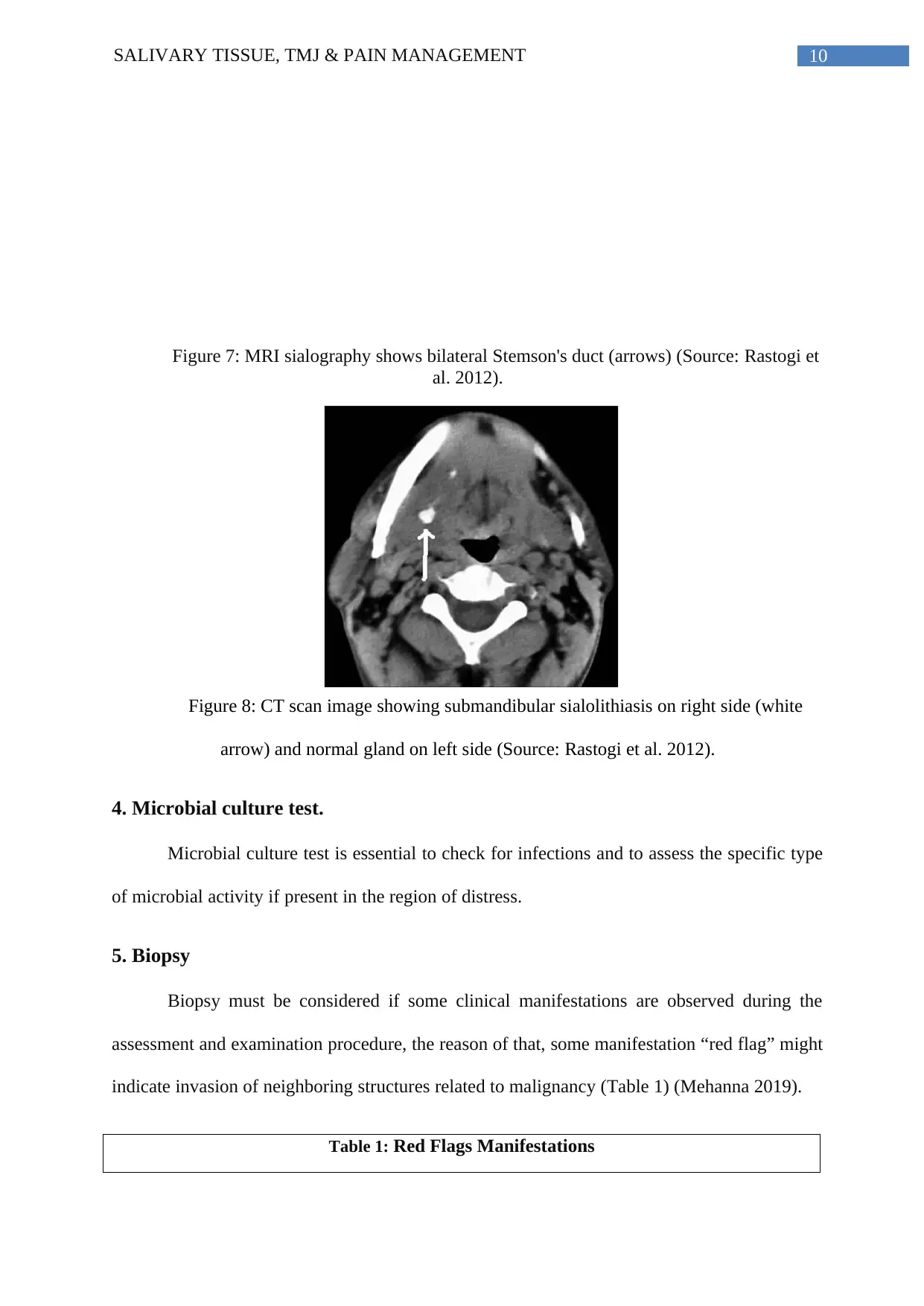
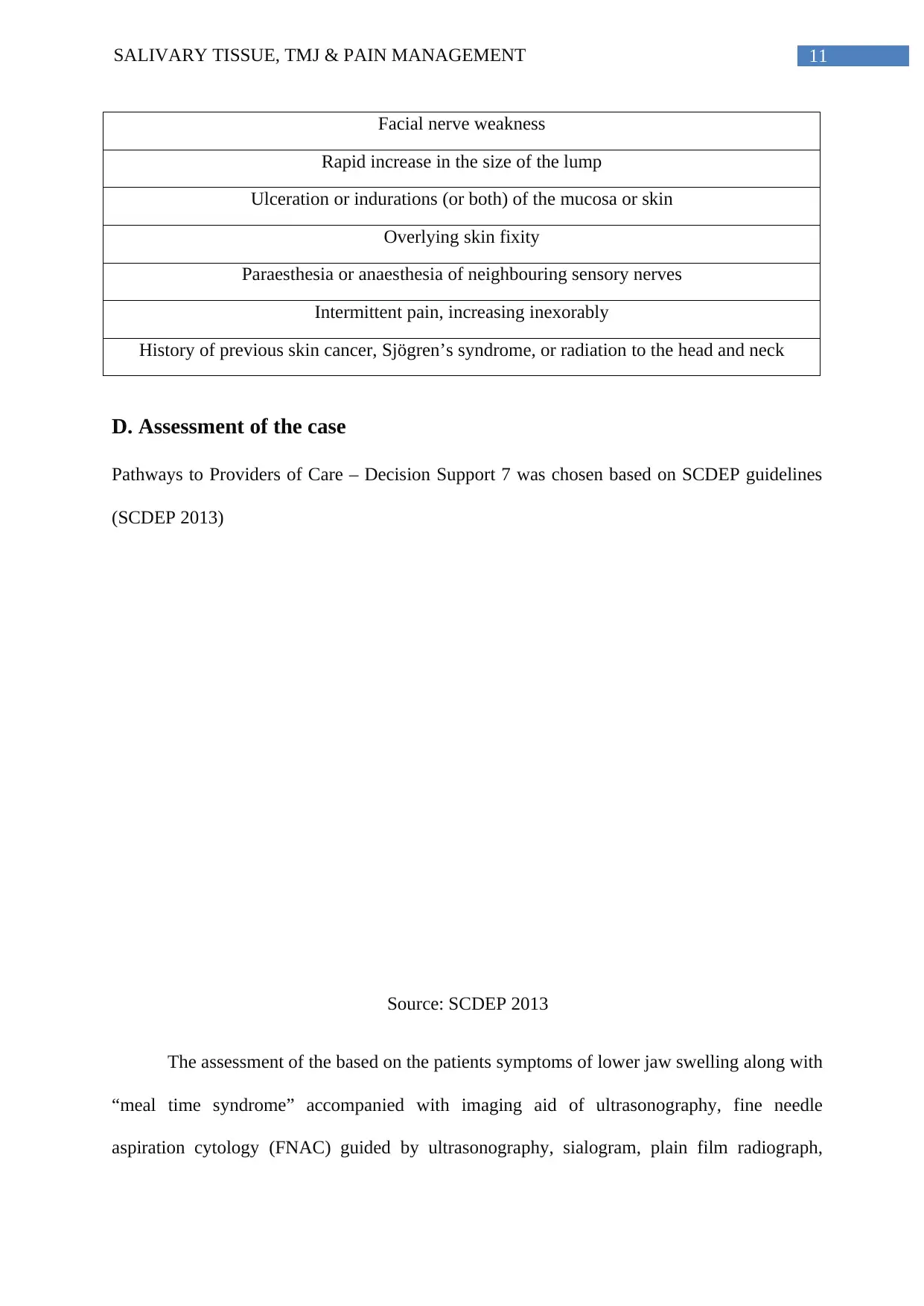
3. MRI or CT scans.
Magnetic resonance imaging is considered non-invasive diagnostic procedure. It can
differentiate between acute and chronic obstructions in the salivary glands, also, it can identify
small calculi, and moreover, there is no ionizing radiation in comparison to computed
tomography (Figure 7) (Daniel et al. 2015). Computed tomography can be performed with or
without contrast to differentiate salivary stones from vascular structures, also it used when the
diagnosis is not certain (Figure 8) (Daniel et al. 2015).
Figure 6: Instruments used in Sialendoscopy. (A) sialendoscope, modular, (B) sialendoscope,
all in one; (C) biopsy and grasping forceps; (D) forceps; (E) bougies (F) probes; (G) dilatator;
(H) stone extractor; (I) microdrill; (J) balloon catheter (Source: Singh and Gupta 2014).
3. MRI or CT scans.
Magnetic resonance imaging is considered non-invasive diagnostic procedure. It can
differentiate between acute and chronic obstructions in the salivary glands, also, it can identify
small calculi, and moreover, there is no ionizing radiation in comparison to computed
tomography (Figure 7) (Daniel et al. 2015). Computed tomography can be performed with or
without contrast to differentiate salivary stones from vascular structures, also it used when the
diagnosis is not certain (Figure 8) (Daniel et al. 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Figure 7: MRI sialography shows bilateral Stemson's duct (arrows) (Source: Rastogi et
al. 2012).
Figure 8: CT scan image showing submandibular sialolithiasis on right side (white
arrow) and normal gland on left side (Source: Rastogi et al. 2012).
4. Microbial culture test.
Microbial culture test is essential to check for infections and to assess the specific type
of microbial activity if present in the region of distress.
5. Biopsy
Biopsy must be considered if some clinical manifestations are observed during the
assessment and examination procedure, the reason of that, some manifestation “red flag” might
indicate invasion of neighboring structures related to malignancy (Table 1) (Mehanna 2019).
Table 1: Red Flags Manifestations
Figure 7: MRI sialography shows bilateral Stemson's duct (arrows) (Source: Rastogi et
al. 2012).
Figure 8: CT scan image showing submandibular sialolithiasis on right side (white
arrow) and normal gland on left side (Source: Rastogi et al. 2012).
4. Microbial culture test.
Microbial culture test is essential to check for infections and to assess the specific type
of microbial activity if present in the region of distress.
5. Biopsy
Biopsy must be considered if some clinical manifestations are observed during the
assessment and examination procedure, the reason of that, some manifestation “red flag” might
indicate invasion of neighboring structures related to malignancy (Table 1) (Mehanna 2019).
Table 1: Red Flags Manifestations
11SALIVARY TISSUE, TMJ & PAIN MANAGEMENT
Facial nerve weakness
Rapid increase in the size of the lump
Ulceration or indurations (or both) of the mucosa or skin
Overlying skin fixity
Paraesthesia or anaesthesia of neighbouring sensory nerves
Intermittent pain, increasing inexorably
History of previous skin cancer, Sjögren’s syndrome, or radiation to the head and neck
D. Assessment of the case
Pathways to Providers of Care – Decision Support 7 was chosen based on SCDEP guidelines
(SCDEP 2013)
Source: SCDEP 2013
The assessment of the based on the patients symptoms of lower jaw swelling along with
“meal time syndrome” accompanied with imaging aid of ultrasonography, fine needle
aspiration cytology (FNAC) guided by ultrasonography, sialogram, plain film radiograph,
Facial nerve weakness
Rapid increase in the size of the lump
Ulceration or indurations (or both) of the mucosa or skin
Overlying skin fixity
Paraesthesia or anaesthesia of neighbouring sensory nerves
Intermittent pain, increasing inexorably
History of previous skin cancer, Sjögren’s syndrome, or radiation to the head and neck
D. Assessment of the case
Pathways to Providers of Care – Decision Support 7 was chosen based on SCDEP guidelines
(SCDEP 2013)
Source: SCDEP 2013
The assessment of the based on the patients symptoms of lower jaw swelling along with
“meal time syndrome” accompanied with imaging aid of ultrasonography, fine needle
aspiration cytology (FNAC) guided by ultrasonography, sialogram, plain film radiograph,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


