Case Study: Evidence-Based Practice for Scabies in Indigenous Children
VerifiedAdded on 2022/09/17
|1
|1590
|18
Practical Assignment
AI Summary
This assignment presents a case study focusing on a 10-year-old Aboriginal male paediatric patient, JK, who presented with scabies. The case study explores the prevalence and pathophysiology of scabies, particularly within the Aboriginal community, highlighting factors like unhygienic living conditions and lack of awareness. It emphasizes the importance of culturally competent nursing care and the application of the National Safety and Quality Health Service Standards. The assignment outlines evidence-based nursing interventions, including pharmacological treatments like topical ointments and health literacy initiatives for the patient and family. The solution also provides a detailed pathophysiology of scabies, discussing the mite's life cycle and transmission. The case study underscores the need for appropriate diagnosis, symptom management, and mite eradication to prevent further infections, referencing relevant research studies and guidelines.
Evidence based practice for treating scabies in indigenous paediatric patients
Introduction:
Scabies can be defined as a skin condition that is characterised by the manifestation of rashes and
intense itching. The condition can be explained as a dermatological condition which is caused by the
causative agent Sarcoptes scabei (Yeoh et al. 2017). The causative agent can be identified as an eight
legged microscopic mite and the infection manifests itself as an immunological response to the toxic
waste or allergens produced by the mite. Research studies have shown that the incidence of skin
infection or skin sores caused due to Group A streptococcus is extremely common within the aboriginal
community (Yeoh et al. 2016). Further, research studies also suggest that the recent years have
witnessed an increase in the incidence rate of skin infections among the children aged between 0 to 5
years who belong to the aboriginal and Torres Islander community (Esposito and Veraldi 2018). The
primary reasons that can be attributed to the high prevalence of scabies among the aboriginal
community members can be explained as living in unhygienic and crowded surroundings and lack of
awareness about the contagious causative agent and skin infections (Esposito and Veraldi his parents
and complained of severe itching and discomfort. 2018). This poster intends to present a case study of a
10 year old, male, aboriginal paediatric patient who presented to the outpatient department of XYZ
hospital with
Case Scenario:
JK was a 10 year old, aboriginal male who presented to the outpatient clinic
with his parents and his presenting complaint included intense itching,
redness and inflammation of the arm-pit area.
• Client background:
• Name: JK
• Age: 10
• Religion: Aboriginal Religion
• Family support: Lives with parents
• Residence: Tiwi Islands, Northern Territory
• Schooling: Pursuing fifth grade in Pularumpi school
• Medications: None
• Previous medical and surgical history: None
• Condition prior to nursing care: Redness, inflammation and visible skin
sores in the underarm area with persistent itching; absence of pain
sensation
• Cultural needs assessment: English is not the first language of the
patient and the patient as well as the patient’s family members, need
effective culturally competent nursing care so as to positively participate
in the care process to acquire positive patient outcome
Application of cultural safety framework to practice:
The National Safety and Quality Health Service Standards for nursing and midwifery
practice mentions that nurses and healthcare workers while caring for Aboriginal and
Torres Islander consumers must positively partner with the patients in the care
process and ensure cultural safety such that effective care is provided to the patients
(Safetyandquality.gov.au 2019). In order to ensure a culturally safe nursing care
intervention, the preference of the patient and his family members would be asked
and accordingly an aboriginal RN would be referred (Safetyandquality.gov.au 2019).
The rationale can be explained as ensuring convenience while communicating with
the nurse as the patient or the family members of the patient do not speak English as
their first language. This would ensure a culturally safe care delivery and would
alleviate the patient care outcome. In addition to this, as revealed by the evidence
base, scabies happens to be the most common skin infection that aboriginal children
experience. On account of the contagious nature of the skin infection, the parents of
the patient would be educated about the risk factors that could possibly trigger the
manifestation in them. Further, they would also be made aware about the importance
of ensuring patient hygiene so as to minimise the risk of the infection burden.
Pathophysiology and Prevalence of Scabies:
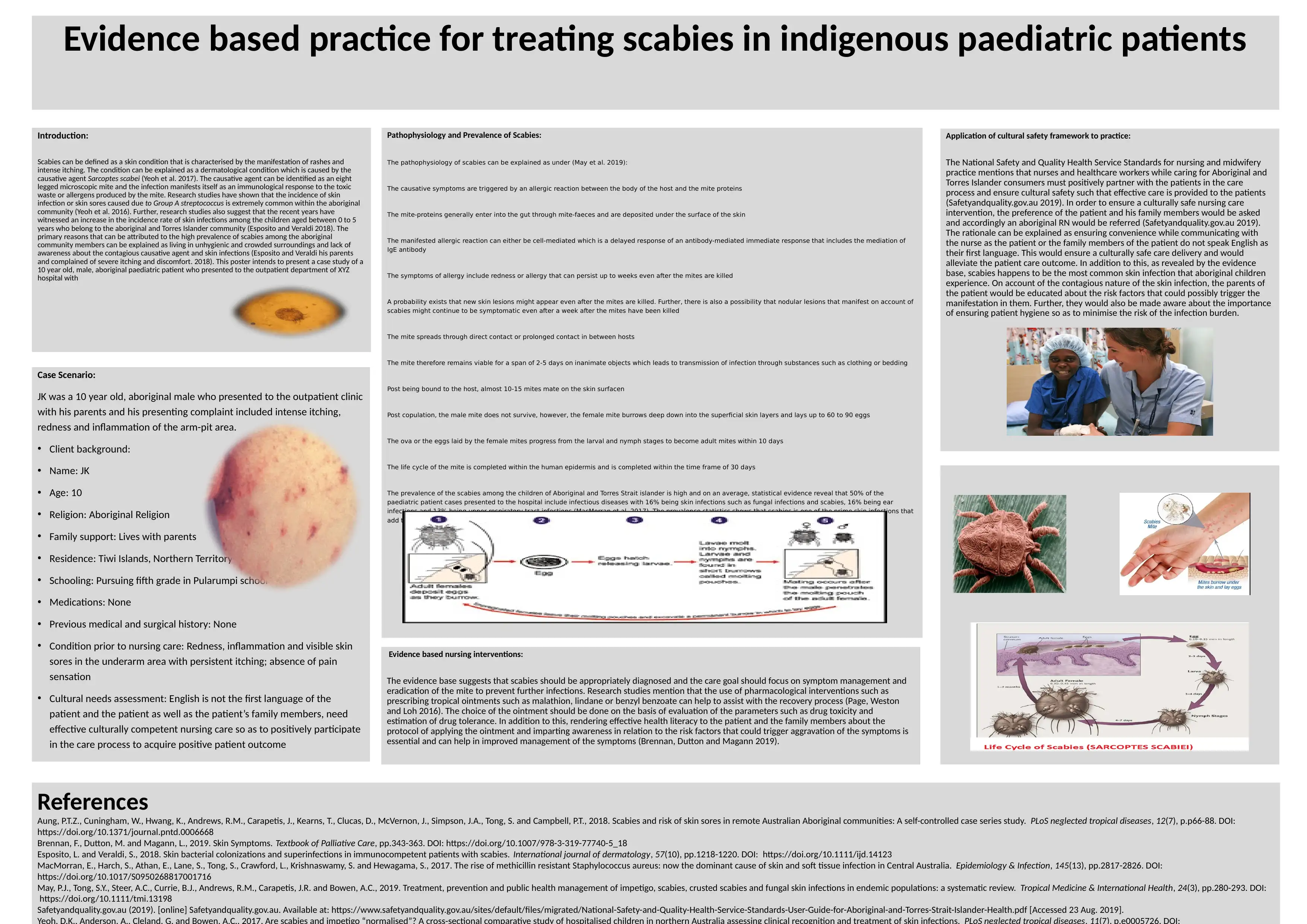
The pathophysiology of scabies can be explained as under (May et al. 2019):
The causative symptoms are triggered by an allergic reaction between the body of the host and the mite proteins
The mite-proteins generally enter into the gut through mite-faeces and are deposited under the surface of the skin
The manifested allergic reaction can either be cell-mediated which is a delayed response of an antibody-mediated immediate response that includes the mediation of
IgE antibody
The symptoms of allergy include redness or allergy that can persist up to weeks even after the mites are killed
A probability exists that new skin lesions might appear even after the mites are killed. Further, there is also a possibility that nodular lesions that manifest on account of
scabies might continue to be symptomatic even after a week after the mites have been killed
The mite spreads through direct contact or prolonged contact in between hosts
The mite therefore remains viable for a span of 2-5 days on inanimate objects which leads to transmission of infection through substances such as clothing or bedding
Post being bound to the host, almost 10-15 mites mate on the skin surfacen
Post copulation, the male mite does not survive, however, the female mite burrows deep down into the superficial skin layers and lays up to 60 to 90 eggs
The ova or the eggs laid by the female mites progress from the larval and nymph stages to become adult mites within 10 days
The life cycle of the mite is completed within the human epidermis and is completed within the time frame of 30 days
The prevalence of the scabies among the children of Aboriginal and Torres Strait islander is high and on an average, statistical evidence reveal that 50% of the
paediatric patient cases presented to the hospital include infectious diseases with 16% being skin infections such as fungal infections and scabies, 16% being ear
infections and 13% being upper respiratory tract infections (MacMorran et al. 2017). The prevalence statistics shows that scabies is one of the prime skin infections that
add to the disease burden of the patients.
Evidence based nursing interventions:
The evidence base suggests that scabies should be appropriately diagnosed and the care goal should focus on symptom management and
eradication of the mite to prevent further infections. Research studies mention that the use of pharmacological interventions such as
prescribing tropical ointments such as malathion, lindane or benzyl benzoate can help to assist with the recovery process (Page, Weston
and Loh 2016). The choice of the ointment should be done on the basis of evaluation of the parameters such as drug toxicity and
estimation of drug tolerance. In addition to this, rendering effective health literacy to the patient and the family members about the
protocol of applying the ointment and imparting awareness in relation to the risk factors that could trigger aggravation of the symptoms is
essential and can help in improved management of the symptoms (Brennan, Dutton and Magann 2019).
References
Aung, P.T.Z., Cuningham, W., Hwang, K., Andrews, R.M., Carapetis, J., Kearns, T., Clucas, D., McVernon, J., Simpson, J.A., Tong, S. and Campbell, P.T., 2018. Scabies and risk of skin sores in remote Australian Aboriginal communities: A self-controlled case series study. PLoS neglected tropical diseases, 12(7), p.p66-88. DOI:
https://doi.org/10.1371/journal.pntd.0006668
Brennan, F., Dutton, M. and Magann, L., 2019. Skin Symptoms. Textbook of Palliative Care, pp.343-363. DOI: https://doi.org/10.1007/978-3-319-77740-5_18
Esposito, L. and Veraldi, S., 2018. Skin bacterial colonizations and superinfections in immunocompetent patients with scabies. International journal of dermatology, 57(10), pp.1218-1220. DOI: https://doi.org/10.1111/ijd.14123
MacMorran, E., Harch, S., Athan, E., Lane, S., Tong, S., Crawford, L., Krishnaswamy, S. and Hewagama, S., 2017. The rise of methicillin resistant Staphylococcus aureus: now the dominant cause of skin and soft tissue infection in Central Australia. Epidemiology & Infection, 145(13), pp.2817-2826. DOI:
https://doi.org/10.1017/S0950268817001716
May, P.J., Tong, S.Y., Steer, A.C., Currie, B.J., Andrews, R.M., Carapetis, J.R. and Bowen, A.C., 2019. Treatment, prevention and public health management of impetigo, scabies, crusted scabies and fungal skin infections in endemic populations: a systematic review. Tropical Medicine & International Health, 24(3), pp.280-293. DOI:
https://doi.org/10.1111/tmi.13198
Safetyandquality.gov.au (2019). [online] Safetyandquality.gov.au. Available at: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-User-Guide-for-Aboriginal-and-Torres-Strait-Islander-Health.pdf [Accessed 23 Aug. 2019].
Introduction:
Scabies can be defined as a skin condition that is characterised by the manifestation of rashes and
intense itching. The condition can be explained as a dermatological condition which is caused by the
causative agent Sarcoptes scabei (Yeoh et al. 2017). The causative agent can be identified as an eight
legged microscopic mite and the infection manifests itself as an immunological response to the toxic
waste or allergens produced by the mite. Research studies have shown that the incidence of skin
infection or skin sores caused due to Group A streptococcus is extremely common within the aboriginal
community (Yeoh et al. 2016). Further, research studies also suggest that the recent years have
witnessed an increase in the incidence rate of skin infections among the children aged between 0 to 5
years who belong to the aboriginal and Torres Islander community (Esposito and Veraldi 2018). The
primary reasons that can be attributed to the high prevalence of scabies among the aboriginal
community members can be explained as living in unhygienic and crowded surroundings and lack of
awareness about the contagious causative agent and skin infections (Esposito and Veraldi his parents
and complained of severe itching and discomfort. 2018). This poster intends to present a case study of a
10 year old, male, aboriginal paediatric patient who presented to the outpatient department of XYZ
hospital with
Case Scenario:
JK was a 10 year old, aboriginal male who presented to the outpatient clinic
with his parents and his presenting complaint included intense itching,
redness and inflammation of the arm-pit area.
• Client background:
• Name: JK
• Age: 10
• Religion: Aboriginal Religion
• Family support: Lives with parents
• Residence: Tiwi Islands, Northern Territory
• Schooling: Pursuing fifth grade in Pularumpi school
• Medications: None
• Previous medical and surgical history: None
• Condition prior to nursing care: Redness, inflammation and visible skin
sores in the underarm area with persistent itching; absence of pain
sensation
• Cultural needs assessment: English is not the first language of the
patient and the patient as well as the patient’s family members, need
effective culturally competent nursing care so as to positively participate
in the care process to acquire positive patient outcome
Application of cultural safety framework to practice:
The National Safety and Quality Health Service Standards for nursing and midwifery
practice mentions that nurses and healthcare workers while caring for Aboriginal and
Torres Islander consumers must positively partner with the patients in the care
process and ensure cultural safety such that effective care is provided to the patients
(Safetyandquality.gov.au 2019). In order to ensure a culturally safe nursing care
intervention, the preference of the patient and his family members would be asked
and accordingly an aboriginal RN would be referred (Safetyandquality.gov.au 2019).
The rationale can be explained as ensuring convenience while communicating with
the nurse as the patient or the family members of the patient do not speak English as
their first language. This would ensure a culturally safe care delivery and would
alleviate the patient care outcome. In addition to this, as revealed by the evidence
base, scabies happens to be the most common skin infection that aboriginal children
experience. On account of the contagious nature of the skin infection, the parents of
the patient would be educated about the risk factors that could possibly trigger the
manifestation in them. Further, they would also be made aware about the importance
of ensuring patient hygiene so as to minimise the risk of the infection burden.
Pathophysiology and Prevalence of Scabies:
The pathophysiology of scabies can be explained as under (May et al. 2019):
The causative symptoms are triggered by an allergic reaction between the body of the host and the mite proteins
The mite-proteins generally enter into the gut through mite-faeces and are deposited under the surface of the skin
The manifested allergic reaction can either be cell-mediated which is a delayed response of an antibody-mediated immediate response that includes the mediation of
IgE antibody
The symptoms of allergy include redness or allergy that can persist up to weeks even after the mites are killed
A probability exists that new skin lesions might appear even after the mites are killed. Further, there is also a possibility that nodular lesions that manifest on account of
scabies might continue to be symptomatic even after a week after the mites have been killed
The mite spreads through direct contact or prolonged contact in between hosts
The mite therefore remains viable for a span of 2-5 days on inanimate objects which leads to transmission of infection through substances such as clothing or bedding
Post being bound to the host, almost 10-15 mites mate on the skin surfacen
Post copulation, the male mite does not survive, however, the female mite burrows deep down into the superficial skin layers and lays up to 60 to 90 eggs
The ova or the eggs laid by the female mites progress from the larval and nymph stages to become adult mites within 10 days
The life cycle of the mite is completed within the human epidermis and is completed within the time frame of 30 days
The prevalence of the scabies among the children of Aboriginal and Torres Strait islander is high and on an average, statistical evidence reveal that 50% of the
paediatric patient cases presented to the hospital include infectious diseases with 16% being skin infections such as fungal infections and scabies, 16% being ear
infections and 13% being upper respiratory tract infections (MacMorran et al. 2017). The prevalence statistics shows that scabies is one of the prime skin infections that
add to the disease burden of the patients.
Evidence based nursing interventions:
The evidence base suggests that scabies should be appropriately diagnosed and the care goal should focus on symptom management and
eradication of the mite to prevent further infections. Research studies mention that the use of pharmacological interventions such as
prescribing tropical ointments such as malathion, lindane or benzyl benzoate can help to assist with the recovery process (Page, Weston
and Loh 2016). The choice of the ointment should be done on the basis of evaluation of the parameters such as drug toxicity and
estimation of drug tolerance. In addition to this, rendering effective health literacy to the patient and the family members about the
protocol of applying the ointment and imparting awareness in relation to the risk factors that could trigger aggravation of the symptoms is
essential and can help in improved management of the symptoms (Brennan, Dutton and Magann 2019).
References
Aung, P.T.Z., Cuningham, W., Hwang, K., Andrews, R.M., Carapetis, J., Kearns, T., Clucas, D., McVernon, J., Simpson, J.A., Tong, S. and Campbell, P.T., 2018. Scabies and risk of skin sores in remote Australian Aboriginal communities: A self-controlled case series study. PLoS neglected tropical diseases, 12(7), p.p66-88. DOI:
https://doi.org/10.1371/journal.pntd.0006668
Brennan, F., Dutton, M. and Magann, L., 2019. Skin Symptoms. Textbook of Palliative Care, pp.343-363. DOI: https://doi.org/10.1007/978-3-319-77740-5_18
Esposito, L. and Veraldi, S., 2018. Skin bacterial colonizations and superinfections in immunocompetent patients with scabies. International journal of dermatology, 57(10), pp.1218-1220. DOI: https://doi.org/10.1111/ijd.14123
MacMorran, E., Harch, S., Athan, E., Lane, S., Tong, S., Crawford, L., Krishnaswamy, S. and Hewagama, S., 2017. The rise of methicillin resistant Staphylococcus aureus: now the dominant cause of skin and soft tissue infection in Central Australia. Epidemiology & Infection, 145(13), pp.2817-2826. DOI:
https://doi.org/10.1017/S0950268817001716
May, P.J., Tong, S.Y., Steer, A.C., Currie, B.J., Andrews, R.M., Carapetis, J.R. and Bowen, A.C., 2019. Treatment, prevention and public health management of impetigo, scabies, crusted scabies and fungal skin infections in endemic populations: a systematic review. Tropical Medicine & International Health, 24(3), pp.280-293. DOI:
https://doi.org/10.1111/tmi.13198
Safetyandquality.gov.au (2019). [online] Safetyandquality.gov.au. Available at: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-User-Guide-for-Aboriginal-and-Torres-Strait-Islander-Health.pdf [Accessed 23 Aug. 2019].
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





