Case Study: Assessing and Managing Alex's Schizophrenia in Acute Care
VerifiedAdded on 2022/08/27
|10
|2581
|18
Report
AI Summary
This report focuses on the case of Alex, a patient admitted to an acute care mental health facility with acute symptoms of psychosis, diagnosed with schizophrenia induced by marijuana use. The report provides a detailed assessment of Alex's condition, including physical examination findings such as disorientation, elevated heart rate, high blood pressure, and high blood glucose levels, along with behavioral changes like increased food and drink consumption and aggression. It discusses the importance of the "Between the flags" safety net and the need for immediate interventions. A nursing management plan is proposed, prioritizing blood sugar management and behavior control, including insulin treatment, fluid replacement, and monitoring of vital signs. The report also outlines the involvement of a multidisciplinary team, including nurses, general practitioners, physiotherapists, psychiatrists, and other specialists. Furthermore, an ISBAR handover is presented, detailing the patient's situation, background, assessment, and recommendations. The report concludes by emphasizing the holistic approach required for Alex's care, addressing both his physical and mental health needs.

Running head: TRANSITIONING TO PRACTICE
TRANSITIONING TO PRACTICE
Name of the Student
Name of the university
Author’s note
TRANSITIONING TO PRACTICE
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1TRANSITIONING TO PRACTICE
Introduction
This report is related to a patient named Alex who had been admitted to the acute care
ward at the mental health facility. He had been admitted in to the locked ward due to hos acute
symptoms of psychosis. Alex had been diagnosed with the acute symptoms of Schizophrenia,
which is caused by the multiple uses of Marijuana.
The paper will give a detailed assessment of the patient, including the signs of
deterioration. A nursing management plan will be provided as per the assessment data and the
multidisciplinary team that might be necessary for Alex will also be discussed. The paper will
also provide a sample of ISBAR handover for Alex.
Assessment
The diagnosis and the assessment of the Schizophrenia includes a thorough Physical
examination, screenings and evaluation of the cognitive health. Additionally there are other
diagnostic criteria that can be used. The physical examination of ales will show that Ales is
unable to walk in a straight line. Alex is disoriented to both time and place. It has been stated by
Þórisdóttir, (2014), that disorientation is common in patients with drug induced schizophrenia.
This indicates to a more stable form of brain disorder, than just neurotransmitter dysfunction.
The heart rate and the blood pressure is found to be much higher in Alex than that of the
normal levels. A high resting heart rate and blood pressure in the youth predicts an increased
susceptibility of the anxiety disorder, schizophrenia. The increased heart rate in the
Schizophrenia patients might be due to the uptake of anti-psychotic drugs (Bär, 2015). Higher
Introduction
This report is related to a patient named Alex who had been admitted to the acute care
ward at the mental health facility. He had been admitted in to the locked ward due to hos acute
symptoms of psychosis. Alex had been diagnosed with the acute symptoms of Schizophrenia,
which is caused by the multiple uses of Marijuana.
The paper will give a detailed assessment of the patient, including the signs of
deterioration. A nursing management plan will be provided as per the assessment data and the
multidisciplinary team that might be necessary for Alex will also be discussed. The paper will
also provide a sample of ISBAR handover for Alex.
Assessment
The diagnosis and the assessment of the Schizophrenia includes a thorough Physical
examination, screenings and evaluation of the cognitive health. Additionally there are other
diagnostic criteria that can be used. The physical examination of ales will show that Ales is
unable to walk in a straight line. Alex is disoriented to both time and place. It has been stated by
Þórisdóttir, (2014), that disorientation is common in patients with drug induced schizophrenia.
This indicates to a more stable form of brain disorder, than just neurotransmitter dysfunction.
The heart rate and the blood pressure is found to be much higher in Alex than that of the
normal levels. A high resting heart rate and blood pressure in the youth predicts an increased
susceptibility of the anxiety disorder, schizophrenia. The increased heart rate in the
Schizophrenia patients might be due to the uptake of anti-psychotic drugs (Bär, 2015). Higher
2TRANSITIONING TO PRACTICE
pulse pressure has been found in patients with schizophrenia. Various types of medications used
in psychotic control increases the risk of developing high blood pressure.
On assessment, the blood glucose level of Alex has been much higher to the standard blood
glucose value. Patients with Schizophrenia have more chance of getting high blood glucose
level. This can be due to the fact, that patients with Schizophrenia might not follow the proper
diet and exercise (Suvisaari et al., 2016). Again, antipsychotic medicines on the other hand
increases the chance of contracting diabetes. Again, Schizophrenia has been associated with pre-
mature birth, stress and increased cortisol level increasing the chance of diabetes (Vancampfort
et al., 2013).
Two of the most alarming condition for Alex, is that he had suddenly increased the
consumption of food and drinks and his behavior has deteriorated and he had become more
aggressive. Eating disorders have been associated with the symptoms of Schizophrenia. An
eating disorder is Bulimia Nervosa that is featured by recurrent episodes of binge eating followed
by repeated unsuitable compensatory behaviors to prevent the gaining of weight like self –
induced vomiting or fasting (Kouidrat et al., 2014). Binge eating disorder has been recognized as
an eating disorder that has been related to Schizophrenia (Kouidrat et al., 2014). Although, no
such evidences have been found about the association of eating disorder with Schizophrenia.
Alex should be kept in “Between the flags” which can be termed as a safety nets for the
patients who had been displaying deteriorating conditions. It is to ensure that the deteriorating
patient gets appropriate care. This is clearly evident from the case study that Alex’s condition is
deteriorating. It can be guessed that some of the visitors might have been providing with drugs to
Alex and if he is left untreated, then it can lead to mortality in the patient. Substance induced
pulse pressure has been found in patients with schizophrenia. Various types of medications used
in psychotic control increases the risk of developing high blood pressure.
On assessment, the blood glucose level of Alex has been much higher to the standard blood
glucose value. Patients with Schizophrenia have more chance of getting high blood glucose
level. This can be due to the fact, that patients with Schizophrenia might not follow the proper
diet and exercise (Suvisaari et al., 2016). Again, antipsychotic medicines on the other hand
increases the chance of contracting diabetes. Again, Schizophrenia has been associated with pre-
mature birth, stress and increased cortisol level increasing the chance of diabetes (Vancampfort
et al., 2013).
Two of the most alarming condition for Alex, is that he had suddenly increased the
consumption of food and drinks and his behavior has deteriorated and he had become more
aggressive. Eating disorders have been associated with the symptoms of Schizophrenia. An
eating disorder is Bulimia Nervosa that is featured by recurrent episodes of binge eating followed
by repeated unsuitable compensatory behaviors to prevent the gaining of weight like self –
induced vomiting or fasting (Kouidrat et al., 2014). Binge eating disorder has been recognized as
an eating disorder that has been related to Schizophrenia (Kouidrat et al., 2014). Although, no
such evidences have been found about the association of eating disorder with Schizophrenia.
Alex should be kept in “Between the flags” which can be termed as a safety nets for the
patients who had been displaying deteriorating conditions. It is to ensure that the deteriorating
patient gets appropriate care. This is clearly evident from the case study that Alex’s condition is
deteriorating. It can be guessed that some of the visitors might have been providing with drugs to
Alex and if he is left untreated, then it can lead to mortality in the patient. Substance induced
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3TRANSITIONING TO PRACTICE
Schizophrenia has been associated with a high level of mortality in the patient (Pain et al., 2017).
The “Between the flags” should use standard observation charts, incorporating the calling criteria
in the emergency departments (Hughes, Pain, Braithwaite & Hillman, 2014). All the charts will
have a trigger and track system such that the vital signs are graphed and are tracked over time.
The chart can involves two colored zones (yellow and red) representing the early and the late
warning signs for the decline (Pain et al., 2017).
Alex should be immediately assessed for the any issues followed by a complete physical
examination, measurement of the arterial blood gases to measure the amount of intoxication.
Some of the immediate tests that can be done includes the tests and screenings. This should
include tests that help to rule out the conditions having similar symptoms and screening for the
drugs and alcohols. Imaging studies can be made like CT scan or MRI, for the differential
diagnosis. Furthermore, a psychiatric assessment can be done like detecting the appearance and
demeanor and asking about the moods and thoughts, delusions, hallucinations, substance use and
the potential for suicide and violence. In case of serious condition, a multidisciplinary team can
be appointed. The mental health professional should use the criteria in the Diagnostic and the
Statistical Manual of the mental health disorders.
Schizophrenia has been associated with a high level of mortality in the patient (Pain et al., 2017).
The “Between the flags” should use standard observation charts, incorporating the calling criteria
in the emergency departments (Hughes, Pain, Braithwaite & Hillman, 2014). All the charts will
have a trigger and track system such that the vital signs are graphed and are tracked over time.
The chart can involves two colored zones (yellow and red) representing the early and the late
warning signs for the decline (Pain et al., 2017).
Alex should be immediately assessed for the any issues followed by a complete physical
examination, measurement of the arterial blood gases to measure the amount of intoxication.
Some of the immediate tests that can be done includes the tests and screenings. This should
include tests that help to rule out the conditions having similar symptoms and screening for the
drugs and alcohols. Imaging studies can be made like CT scan or MRI, for the differential
diagnosis. Furthermore, a psychiatric assessment can be done like detecting the appearance and
demeanor and asking about the moods and thoughts, delusions, hallucinations, substance use and
the potential for suicide and violence. In case of serious condition, a multidisciplinary team can
be appointed. The mental health professional should use the criteria in the Diagnostic and the
Statistical Manual of the mental health disorders.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4TRANSITIONING TO PRACTICE
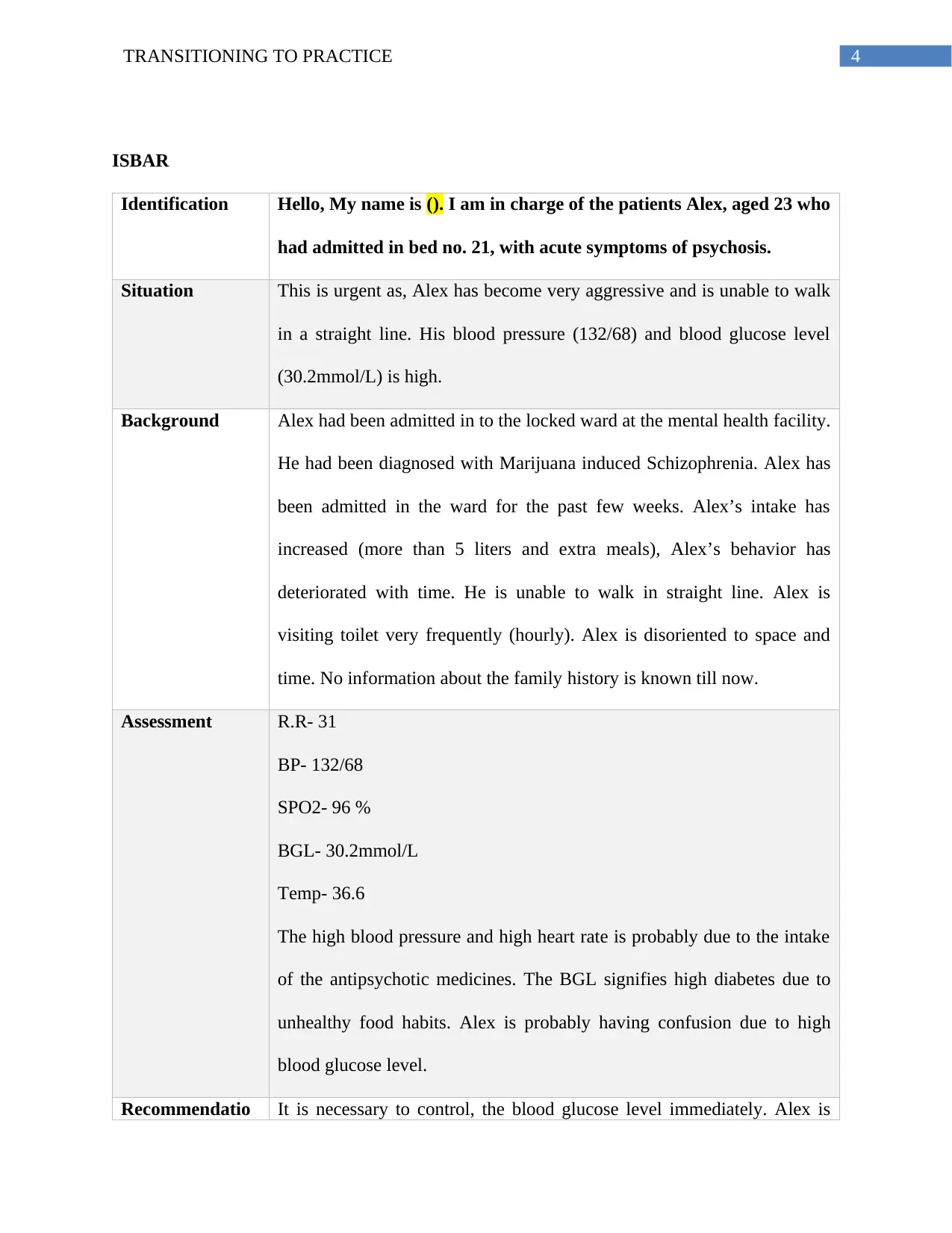
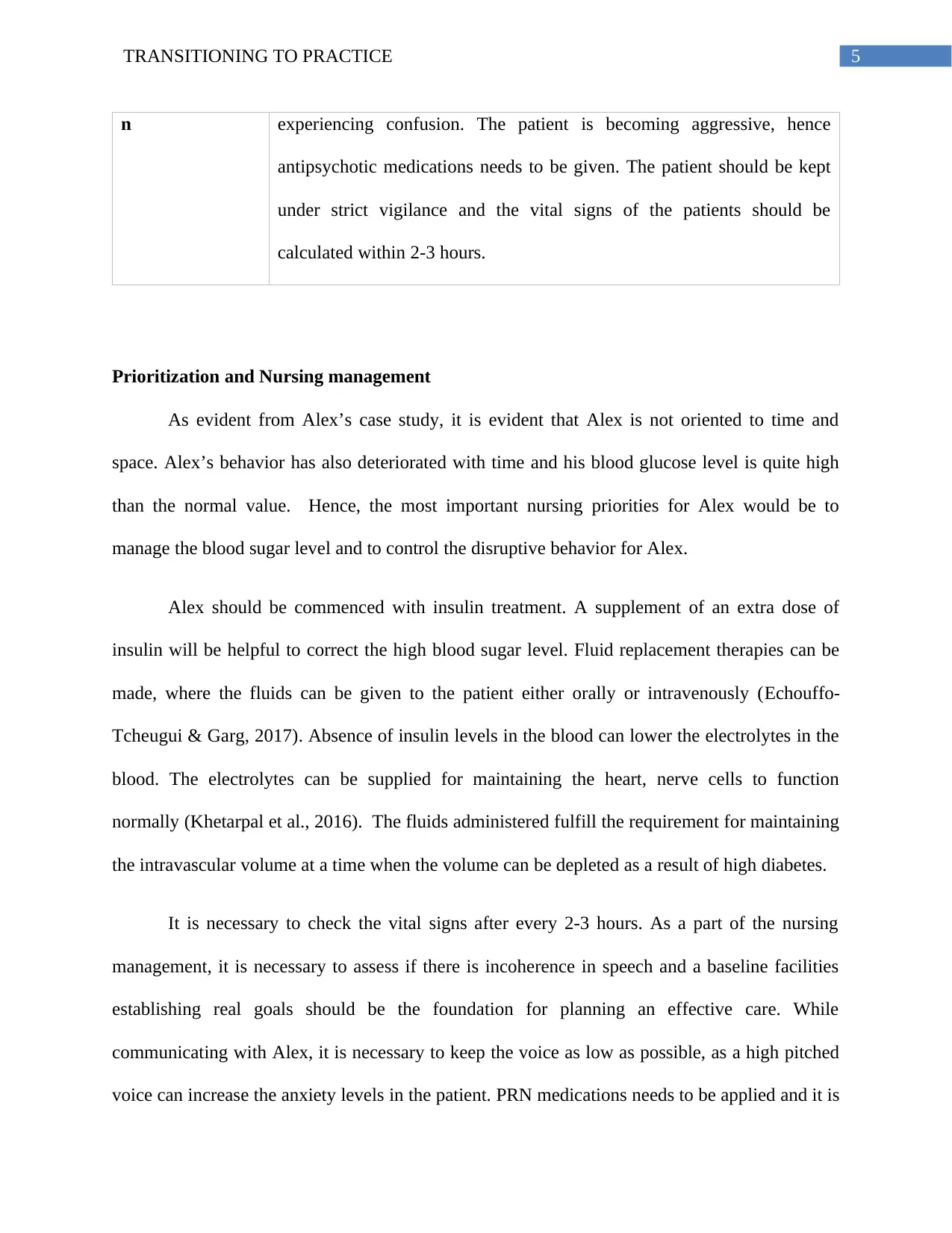
ISBAR
Identification Hello, My name is (). I am in charge of the patients Alex, aged 23 who
had admitted in bed no. 21, with acute symptoms of psychosis.
Situation This is urgent as, Alex has become very aggressive and is unable to walk
in a straight line. His blood pressure (132/68) and blood glucose level
(30.2mmol/L) is high.
Background Alex had been admitted in to the locked ward at the mental health facility.
He had been diagnosed with Marijuana induced Schizophrenia. Alex has
been admitted in the ward for the past few weeks. Alex’s intake has
increased (more than 5 liters and extra meals), Alex’s behavior has
deteriorated with time. He is unable to walk in straight line. Alex is
visiting toilet very frequently (hourly). Alex is disoriented to space and
time. No information about the family history is known till now.
Assessment R.R- 31
BP- 132/68
SPO2- 96 %
BGL- 30.2mmol/L
Temp- 36.6
The high blood pressure and high heart rate is probably due to the intake
of the antipsychotic medicines. The BGL signifies high diabetes due to
unhealthy food habits. Alex is probably having confusion due to high
blood glucose level.
Recommendatio It is necessary to control, the blood glucose level immediately. Alex is
ISBAR
Identification Hello, My name is (). I am in charge of the patients Alex, aged 23 who
had admitted in bed no. 21, with acute symptoms of psychosis.
Situation This is urgent as, Alex has become very aggressive and is unable to walk
in a straight line. His blood pressure (132/68) and blood glucose level
(30.2mmol/L) is high.
Background Alex had been admitted in to the locked ward at the mental health facility.
He had been diagnosed with Marijuana induced Schizophrenia. Alex has
been admitted in the ward for the past few weeks. Alex’s intake has
increased (more than 5 liters and extra meals), Alex’s behavior has
deteriorated with time. He is unable to walk in straight line. Alex is
visiting toilet very frequently (hourly). Alex is disoriented to space and
time. No information about the family history is known till now.
Assessment R.R- 31
BP- 132/68
SPO2- 96 %
BGL- 30.2mmol/L
Temp- 36.6
The high blood pressure and high heart rate is probably due to the intake
of the antipsychotic medicines. The BGL signifies high diabetes due to
unhealthy food habits. Alex is probably having confusion due to high
blood glucose level.
Recommendatio It is necessary to control, the blood glucose level immediately. Alex is
5TRANSITIONING TO PRACTICE
n experiencing confusion. The patient is becoming aggressive, hence
antipsychotic medications needs to be given. The patient should be kept
under strict vigilance and the vital signs of the patients should be
calculated within 2-3 hours.
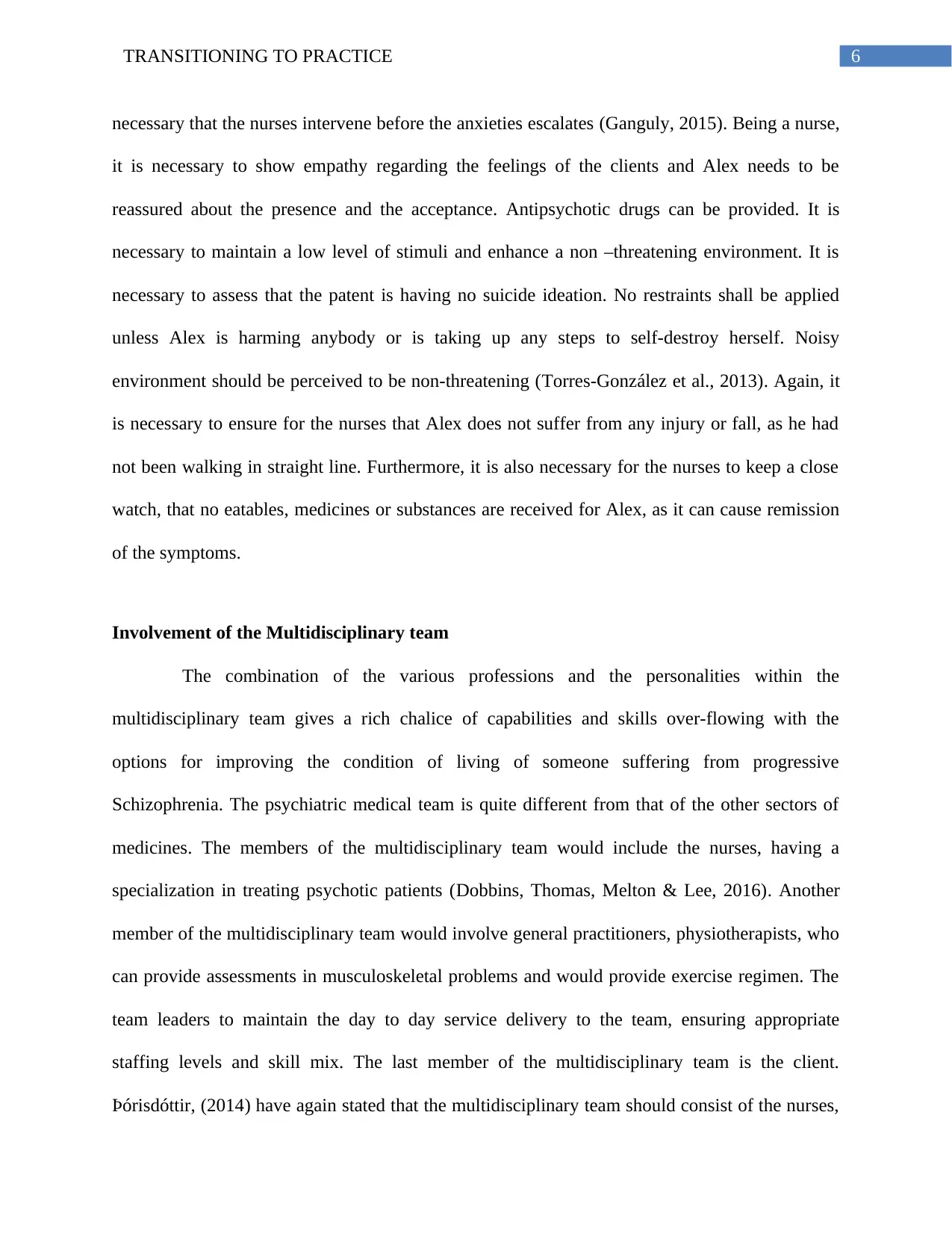
Prioritization and Nursing management
As evident from Alex’s case study, it is evident that Alex is not oriented to time and
space. Alex’s behavior has also deteriorated with time and his blood glucose level is quite high
than the normal value. Hence, the most important nursing priorities for Alex would be to
manage the blood sugar level and to control the disruptive behavior for Alex.
Alex should be commenced with insulin treatment. A supplement of an extra dose of
insulin will be helpful to correct the high blood sugar level. Fluid replacement therapies can be
made, where the fluids can be given to the patient either orally or intravenously (Echouffo-
Tcheugui & Garg, 2017). Absence of insulin levels in the blood can lower the electrolytes in the
blood. The electrolytes can be supplied for maintaining the heart, nerve cells to function
normally (Khetarpal et al., 2016). The fluids administered fulfill the requirement for maintaining
the intravascular volume at a time when the volume can be depleted as a result of high diabetes.
It is necessary to check the vital signs after every 2-3 hours. As a part of the nursing
management, it is necessary to assess if there is incoherence in speech and a baseline facilities
establishing real goals should be the foundation for planning an effective care. While
communicating with Alex, it is necessary to keep the voice as low as possible, as a high pitched
voice can increase the anxiety levels in the patient. PRN medications needs to be applied and it is
n experiencing confusion. The patient is becoming aggressive, hence
antipsychotic medications needs to be given. The patient should be kept
under strict vigilance and the vital signs of the patients should be
calculated within 2-3 hours.
Prioritization and Nursing management
As evident from Alex’s case study, it is evident that Alex is not oriented to time and
space. Alex’s behavior has also deteriorated with time and his blood glucose level is quite high
than the normal value. Hence, the most important nursing priorities for Alex would be to
manage the blood sugar level and to control the disruptive behavior for Alex.
Alex should be commenced with insulin treatment. A supplement of an extra dose of
insulin will be helpful to correct the high blood sugar level. Fluid replacement therapies can be
made, where the fluids can be given to the patient either orally or intravenously (Echouffo-
Tcheugui & Garg, 2017). Absence of insulin levels in the blood can lower the electrolytes in the
blood. The electrolytes can be supplied for maintaining the heart, nerve cells to function
normally (Khetarpal et al., 2016). The fluids administered fulfill the requirement for maintaining
the intravascular volume at a time when the volume can be depleted as a result of high diabetes.
It is necessary to check the vital signs after every 2-3 hours. As a part of the nursing
management, it is necessary to assess if there is incoherence in speech and a baseline facilities
establishing real goals should be the foundation for planning an effective care. While
communicating with Alex, it is necessary to keep the voice as low as possible, as a high pitched
voice can increase the anxiety levels in the patient. PRN medications needs to be applied and it is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6TRANSITIONING TO PRACTICE
necessary that the nurses intervene before the anxieties escalates (Ganguly, 2015). Being a nurse,
it is necessary to show empathy regarding the feelings of the clients and Alex needs to be
reassured about the presence and the acceptance. Antipsychotic drugs can be provided. It is
necessary to maintain a low level of stimuli and enhance a non –threatening environment. It is
necessary to assess that the patent is having no suicide ideation. No restraints shall be applied
unless Alex is harming anybody or is taking up any steps to self-destroy herself. Noisy
environment should be perceived to be non-threatening (Torres-González et al., 2013). Again, it
is necessary to ensure for the nurses that Alex does not suffer from any injury or fall, as he had
not been walking in straight line. Furthermore, it is also necessary for the nurses to keep a close
watch, that no eatables, medicines or substances are received for Alex, as it can cause remission
of the symptoms.
Involvement of the Multidisciplinary team
The combination of the various professions and the personalities within the
multidisciplinary team gives a rich chalice of capabilities and skills over-flowing with the
options for improving the condition of living of someone suffering from progressive
Schizophrenia. The psychiatric medical team is quite different from that of the other sectors of
medicines. The members of the multidisciplinary team would include the nurses, having a
specialization in treating psychotic patients (Dobbins, Thomas, Melton & Lee, 2016). Another
member of the multidisciplinary team would involve general practitioners, physiotherapists, who
can provide assessments in musculoskeletal problems and would provide exercise regimen. The
team leaders to maintain the day to day service delivery to the team, ensuring appropriate
staffing levels and skill mix. The last member of the multidisciplinary team is the client.
Þórisdóttir, (2014) have again stated that the multidisciplinary team should consist of the nurses,
necessary that the nurses intervene before the anxieties escalates (Ganguly, 2015). Being a nurse,
it is necessary to show empathy regarding the feelings of the clients and Alex needs to be
reassured about the presence and the acceptance. Antipsychotic drugs can be provided. It is
necessary to maintain a low level of stimuli and enhance a non –threatening environment. It is
necessary to assess that the patent is having no suicide ideation. No restraints shall be applied
unless Alex is harming anybody or is taking up any steps to self-destroy herself. Noisy
environment should be perceived to be non-threatening (Torres-González et al., 2013). Again, it
is necessary to ensure for the nurses that Alex does not suffer from any injury or fall, as he had
not been walking in straight line. Furthermore, it is also necessary for the nurses to keep a close
watch, that no eatables, medicines or substances are received for Alex, as it can cause remission
of the symptoms.
Involvement of the Multidisciplinary team
The combination of the various professions and the personalities within the
multidisciplinary team gives a rich chalice of capabilities and skills over-flowing with the
options for improving the condition of living of someone suffering from progressive
Schizophrenia. The psychiatric medical team is quite different from that of the other sectors of
medicines. The members of the multidisciplinary team would include the nurses, having a
specialization in treating psychotic patients (Dobbins, Thomas, Melton & Lee, 2016). Another
member of the multidisciplinary team would involve general practitioners, physiotherapists, who
can provide assessments in musculoskeletal problems and would provide exercise regimen. The
team leaders to maintain the day to day service delivery to the team, ensuring appropriate
staffing levels and skill mix. The last member of the multidisciplinary team is the client.
Þórisdóttir, (2014) have again stated that the multidisciplinary team should consist of the nurses,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7TRANSITIONING TO PRACTICE
psychiatrists, clinical nurse, specialist, psychologists, social workers and the occupational
therapists, medical secretaries and sometimes people from other fields like counselling,
advocacy workers, care workers. Apart from the psychotherapist, Alex would require a mental
health nurse, an occupational therapist, who would Alex to conduct his daily activities of living
after the recovery and can also recommend him to community based services that can help him
financially.
In conclusion, it can be said the main clinical priorities for Alex, is to maintain his high
blood sugar level and his increased psychiatric symptoms. It is necessary to start the insulin and
the fluid replacement therapies. Apart from this, the nursing interventions includes monitoring of
the vital signs. The multidisciplinary team member that will be required are the psychiatric
nurses, doctors, mental health nurse and an occupational therapist. Moreover, Alex would require
a holistic care of approach that will heal his mind and his body.
psychiatrists, clinical nurse, specialist, psychologists, social workers and the occupational
therapists, medical secretaries and sometimes people from other fields like counselling,
advocacy workers, care workers. Apart from the psychotherapist, Alex would require a mental
health nurse, an occupational therapist, who would Alex to conduct his daily activities of living
after the recovery and can also recommend him to community based services that can help him
financially.
In conclusion, it can be said the main clinical priorities for Alex, is to maintain his high
blood sugar level and his increased psychiatric symptoms. It is necessary to start the insulin and
the fluid replacement therapies. Apart from this, the nursing interventions includes monitoring of
the vital signs. The multidisciplinary team member that will be required are the psychiatric
nurses, doctors, mental health nurse and an occupational therapist. Moreover, Alex would require
a holistic care of approach that will heal his mind and his body.
8TRANSITIONING TO PRACTICE
References
Bär K. J. (2015). Cardiac Autonomic Dysfunction in Patients with Schizophrenia and Their
Healthy Relatives - A Small Review. Frontiers in neurology, 6, 139.
https://doi.org/10.3389/fneur.2015.00139
Dobbins, M. I., Thomas, S. A., Melton, S. L. S., & Lee, S. (2016). Integrated care and the
evolution of the multidisciplinary team. Primary Care: Clinics in Office Practice, 43(2),
177-190.
Echouffo-Tcheugui, J. B., & Garg, R. (2017). Management of hyperglycemia and diabetes in the
emergency department. Current diabetes reports, 17(8), 56.
Ganguly, P. (2015). A Framework for the Holistic Management of Schizophrenia. Xlibris
Corporation.
Hughes, C., Pain, C., Braithwaite, J., & Hillman, K. (2014). ‘Between the flags’: implementing a
rapid response system at scale. BMJ Qual Saf, 23(9), 714-717.
http://dx.doi.org/10.1136/bmjqs-2014-002845
Khetarpal, R., Chatrath, V., Kaur, J., Bala, A., & Singh, H. (2016). Impact of different
intravenous fluids on blood glucose levels in nondiabetic patients undergoing elective
major noncardiac surgeries. Anesthesia, essays and researches, 10(3), 425–431.
https://doi.org/10.4103/0259-1162.176411
References
Bär K. J. (2015). Cardiac Autonomic Dysfunction in Patients with Schizophrenia and Their
Healthy Relatives - A Small Review. Frontiers in neurology, 6, 139.
https://doi.org/10.3389/fneur.2015.00139
Dobbins, M. I., Thomas, S. A., Melton, S. L. S., & Lee, S. (2016). Integrated care and the
evolution of the multidisciplinary team. Primary Care: Clinics in Office Practice, 43(2),
177-190.
Echouffo-Tcheugui, J. B., & Garg, R. (2017). Management of hyperglycemia and diabetes in the
emergency department. Current diabetes reports, 17(8), 56.
Ganguly, P. (2015). A Framework for the Holistic Management of Schizophrenia. Xlibris
Corporation.
Hughes, C., Pain, C., Braithwaite, J., & Hillman, K. (2014). ‘Between the flags’: implementing a
rapid response system at scale. BMJ Qual Saf, 23(9), 714-717.
http://dx.doi.org/10.1136/bmjqs-2014-002845
Khetarpal, R., Chatrath, V., Kaur, J., Bala, A., & Singh, H. (2016). Impact of different
intravenous fluids on blood glucose levels in nondiabetic patients undergoing elective
major noncardiac surgeries. Anesthesia, essays and researches, 10(3), 425–431.
https://doi.org/10.4103/0259-1162.176411
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9TRANSITIONING TO PRACTICE
Kouidrat, Y., Amad, A., Lalau, J. D., & Loas, G. (2014). Eating disorders in schizophrenia:
implications for research and management. Schizophrenia research and treatment, 2014,
791573. https://doi.org/10.1155/2014/791573
Kouidrat, Y., Amad, A., Lalau, J. D., & Loas, G. (2014). Eating disorders in schizophrenia:
implications for research and management. Schizophrenia research and treatment, 2014,
791573. https://doi.org/10.1155/2014/791573
Pain, C., Green, M., Duff, C., Hyland, D., Pantle, A., Fitzpatrick, K., & Hughes, C. (2017).
Between the flags: implementing a safety-net system at scale to recognise and manage
deteriorating patients in the New South Wales Public Health System. International
journal for quality in health care, 29(1), 130-136.
Suvisaari, J., Keinänen, J., Eskelinen, S., & Mantere, O. (2016). Diabetes and schizophrenia.
Current diabetes reports, 16(2), 16.
Þórisdóttir, J. G. (2014). Follow-up interventions and measurement instruments for patients
suffering from psychotic disorder: A literature review.
Torres-González, F., Ibanez-Casas, I., Saldivia, S., Ballester, D., Grandon, P., Moreno-Kuestner,
B., ... & Gómez-Beneyto, M. (2014). Unmet needs in the management of schizophrenia.
Neuropsychiatric disease and treatment, 10, 97.
Vancampfort, D., De Hert, M., Sweers, K., De Herdt, A., Detraux, J., & Probst, M. (2013).
Diabetes, physical activity participation and exercise capacity in patients with
schizophrenia. Psychiatry and Clinical Neurosciences, 67(6), 451-456.
Kouidrat, Y., Amad, A., Lalau, J. D., & Loas, G. (2014). Eating disorders in schizophrenia:
implications for research and management. Schizophrenia research and treatment, 2014,
791573. https://doi.org/10.1155/2014/791573
Kouidrat, Y., Amad, A., Lalau, J. D., & Loas, G. (2014). Eating disorders in schizophrenia:
implications for research and management. Schizophrenia research and treatment, 2014,
791573. https://doi.org/10.1155/2014/791573
Pain, C., Green, M., Duff, C., Hyland, D., Pantle, A., Fitzpatrick, K., & Hughes, C. (2017).
Between the flags: implementing a safety-net system at scale to recognise and manage
deteriorating patients in the New South Wales Public Health System. International
journal for quality in health care, 29(1), 130-136.
Suvisaari, J., Keinänen, J., Eskelinen, S., & Mantere, O. (2016). Diabetes and schizophrenia.
Current diabetes reports, 16(2), 16.
Þórisdóttir, J. G. (2014). Follow-up interventions and measurement instruments for patients
suffering from psychotic disorder: A literature review.
Torres-González, F., Ibanez-Casas, I., Saldivia, S., Ballester, D., Grandon, P., Moreno-Kuestner,
B., ... & Gómez-Beneyto, M. (2014). Unmet needs in the management of schizophrenia.
Neuropsychiatric disease and treatment, 10, 97.
Vancampfort, D., De Hert, M., Sweers, K., De Herdt, A., Detraux, J., & Probst, M. (2013).
Diabetes, physical activity participation and exercise capacity in patients with
schizophrenia. Psychiatry and Clinical Neurosciences, 67(6), 451-456.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





