Healthcare Report: PICOT Analysis of School-Based Asthma Interventions
VerifiedAdded on 2020/05/03
|7
|1539
|88
Report
AI Summary
This report conducts a PICOT analysis to address the problem of pediatric asthma, a chronic condition characterized by airway inflammation, leading to breathing difficulties, coughing, wheezing, and chest tightness. The study proposes school-based interventions as a solution to improve health outcomes and reduce hospital admissions among children with asthma. The interventions include increasing asthma knowledge, enhancing self-management skills through school nurses and drills, and involving parents in the management process. The report outlines the intervention's feasibility, organizational culture, and education plans for both parents and children, emphasizing lifestyle modifications, medication adherence, and trigger avoidance. The expected outcomes include improved health literacy, reduced hospital admissions, better quality of life, and cost savings. The report details methods to achieve these outcomes, such as self-management practices, partnerships between children, parents, and healthcare providers, and written asthma management plans. The analysis also highlights the positive impact on patients' quality of life and environmental changes, such as reduced allergens in the surroundings, while ensuring cost-effective care.

Running head: PICOT
PICOT
Name of the student:
Name of the university:
Author note:
PICOT
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
PICOT
Proposed problem:
Asthma mainly affects individuals by swelling of airways that are resulting in narrowing
of the airways which carry air form the nose and mouth to that of the lungs. Allergens or similar
compounds when enter the lungs may trigger sigma symptoms which involve troubled breathing,
coughing, wheezing as well as tightness of chest (Reznik et al., 2015). As there is no permanent
cure for asthma, one should try to live a disciplined lifestyle. They should be managed with
proper intervention and treatment. It is indeed very concerning to see the fact that when
prevalence rate of asthma is 7.6 in adults, it is higher in children for about 8.4 percent (Coelho et
al., 2017). It has become the leading chronic disease in children resulting in missing schools and
poor quality lives.
Proposed solution:
The present healthcare system is mainly trying to implement interventions which can cut
out the chances of increased admission of the children in the hospital. This is mainly because
hospital admission results in flow of resources from the parents and increases anxiety and
tensions among parents (Coelho et al., 2017). Not only that, the medications which are provided
to children (when conditions become worse) are also costly.
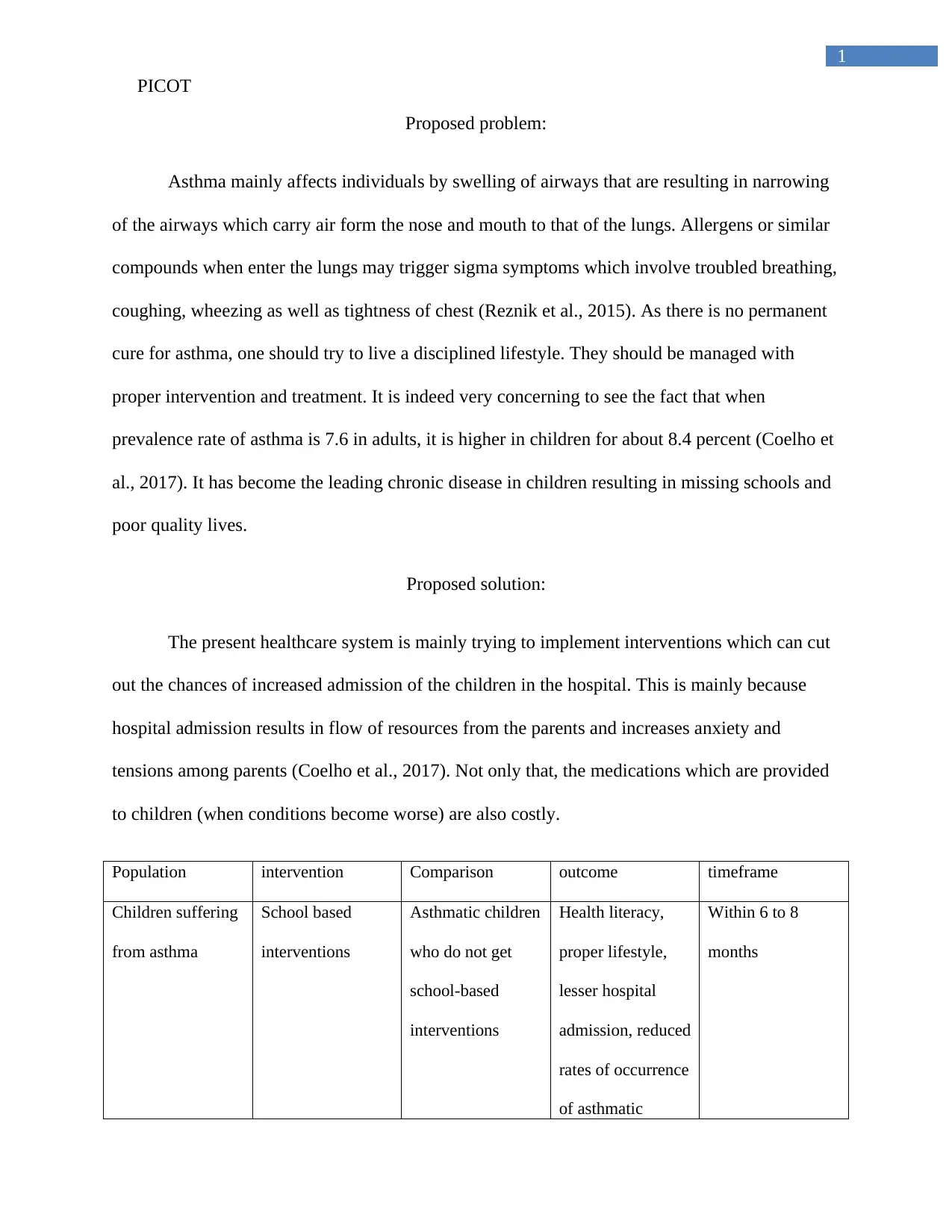
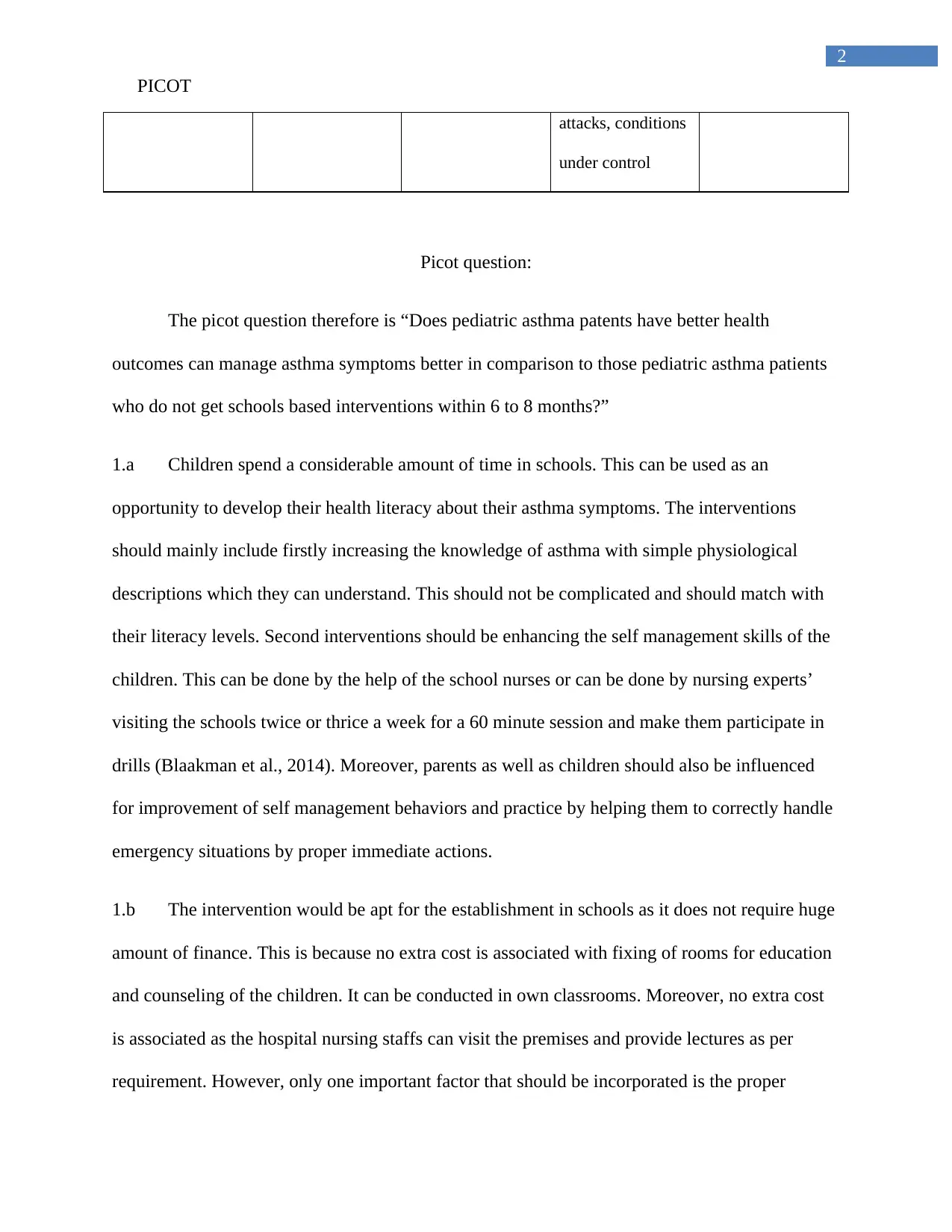
Population intervention Comparison outcome timeframe
Children suffering
from asthma
School based
interventions
Asthmatic children
who do not get
school-based
interventions
Health literacy,
proper lifestyle,
lesser hospital
admission, reduced
rates of occurrence
of asthmatic
Within 6 to 8
months
PICOT
Proposed problem:
Asthma mainly affects individuals by swelling of airways that are resulting in narrowing
of the airways which carry air form the nose and mouth to that of the lungs. Allergens or similar
compounds when enter the lungs may trigger sigma symptoms which involve troubled breathing,
coughing, wheezing as well as tightness of chest (Reznik et al., 2015). As there is no permanent
cure for asthma, one should try to live a disciplined lifestyle. They should be managed with
proper intervention and treatment. It is indeed very concerning to see the fact that when
prevalence rate of asthma is 7.6 in adults, it is higher in children for about 8.4 percent (Coelho et
al., 2017). It has become the leading chronic disease in children resulting in missing schools and
poor quality lives.
Proposed solution:
The present healthcare system is mainly trying to implement interventions which can cut
out the chances of increased admission of the children in the hospital. This is mainly because
hospital admission results in flow of resources from the parents and increases anxiety and
tensions among parents (Coelho et al., 2017). Not only that, the medications which are provided
to children (when conditions become worse) are also costly.
Population intervention Comparison outcome timeframe
Children suffering
from asthma
School based
interventions
Asthmatic children
who do not get
school-based
interventions
Health literacy,
proper lifestyle,
lesser hospital
admission, reduced
rates of occurrence
of asthmatic
Within 6 to 8
months
2
PICOT
attacks, conditions
under control
Picot question:
The picot question therefore is “Does pediatric asthma patents have better health
outcomes can manage asthma symptoms better in comparison to those pediatric asthma patients
who do not get schools based interventions within 6 to 8 months?”
1.a Children spend a considerable amount of time in schools. This can be used as an
opportunity to develop their health literacy about their asthma symptoms. The interventions
should mainly include firstly increasing the knowledge of asthma with simple physiological
descriptions which they can understand. This should not be complicated and should match with
their literacy levels. Second interventions should be enhancing the self management skills of the
children. This can be done by the help of the school nurses or can be done by nursing experts’
visiting the schools twice or thrice a week for a 60 minute session and make them participate in
drills (Blaakman et al., 2014). Moreover, parents as well as children should also be influenced
for improvement of self management behaviors and practice by helping them to correctly handle
emergency situations by proper immediate actions.
1.b The intervention would be apt for the establishment in schools as it does not require huge
amount of finance. This is because no extra cost is associated with fixing of rooms for education
and counseling of the children. It can be conducted in own classrooms. Moreover, no extra cost
is associated as the hospital nursing staffs can visit the premises and provide lectures as per
requirement. However, only one important factor that should be incorporated is the proper
PICOT
attacks, conditions
under control
Picot question:
The picot question therefore is “Does pediatric asthma patents have better health
outcomes can manage asthma symptoms better in comparison to those pediatric asthma patients
who do not get schools based interventions within 6 to 8 months?”
1.a Children spend a considerable amount of time in schools. This can be used as an
opportunity to develop their health literacy about their asthma symptoms. The interventions
should mainly include firstly increasing the knowledge of asthma with simple physiological
descriptions which they can understand. This should not be complicated and should match with
their literacy levels. Second interventions should be enhancing the self management skills of the
children. This can be done by the help of the school nurses or can be done by nursing experts’
visiting the schools twice or thrice a week for a 60 minute session and make them participate in
drills (Blaakman et al., 2014). Moreover, parents as well as children should also be influenced
for improvement of self management behaviors and practice by helping them to correctly handle
emergency situations by proper immediate actions.
1.b The intervention would be apt for the establishment in schools as it does not require huge
amount of finance. This is because no extra cost is associated with fixing of rooms for education
and counseling of the children. It can be conducted in own classrooms. Moreover, no extra cost
is associated as the hospital nursing staffs can visit the premises and provide lectures as per
requirement. However, only one important factor that should be incorporated is the proper
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
PICOT
training of the experts who would be sent to schools as they have to communicate with children.
Communication with children requires proper soft skills, empathy and also implementation of
proper humor and tricks to keep them engaged and make them feel involved. The nurse’s
communication style should be exciting so that children remain hooked to the classes without the
missing any information.
2. Organization culture:
The proposed solution is very much consistent with the community culture. Children go
to school to learn about different aspect which help them to make their future life happier and
prosperous. The knowledge help them to prepare the capability of rational thinking and thereby
lead a healthy and prosperous lives. Therefore, this is one of the best medium for spreading of
health literacy on asthma and asthma management information. This should gradually be made a
part of their curriculum so that they become capable to handle their asthma symptoms
successfully and do not lead to serious events (Rasberry et al., 2014). However, the organization
who should be initiating this campaign should properly plan the health promotion program
effectively and allocate proper resources and funds before initiating the implementation of the
project.
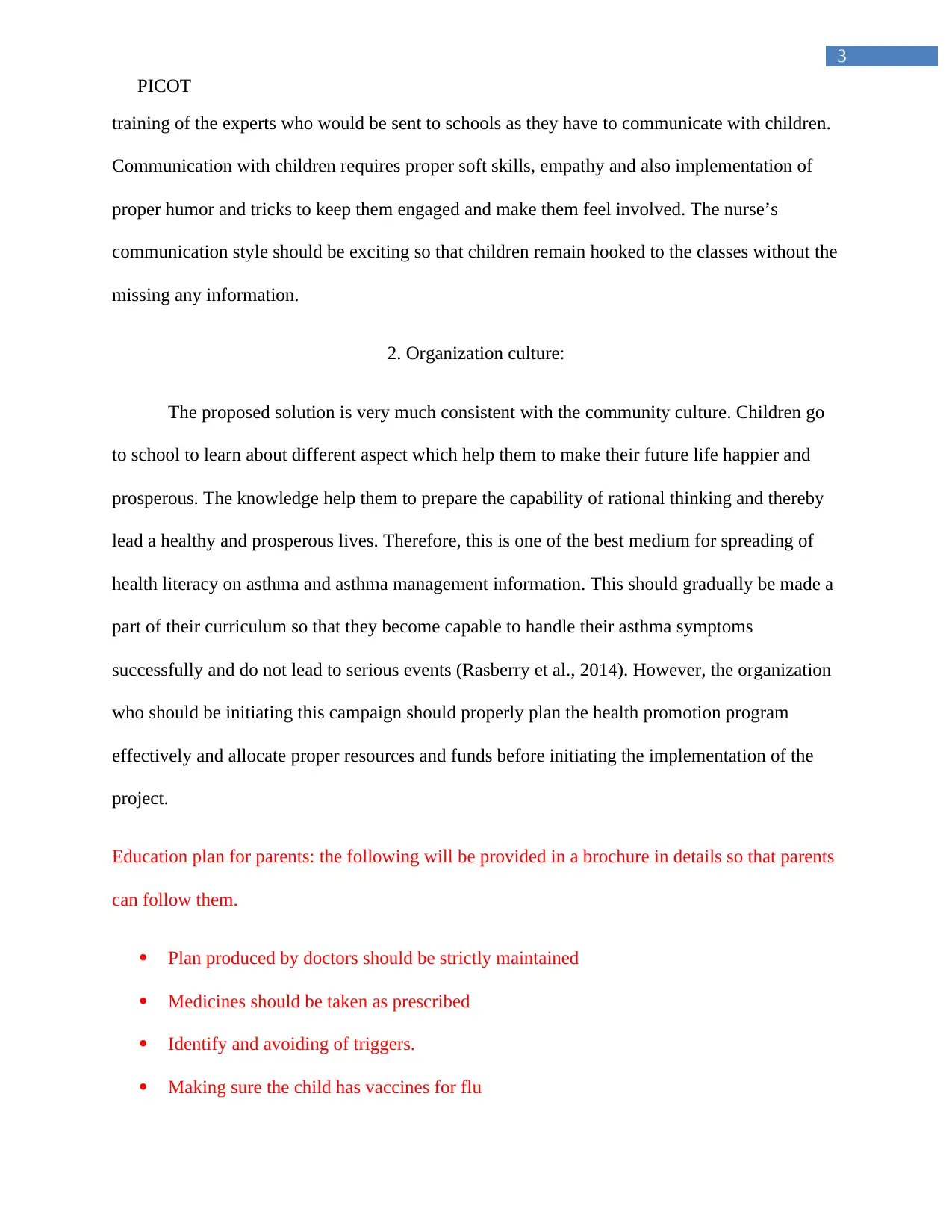
Education plan for parents: the following will be provided in a brochure in details so that parents
can follow them.
Plan produced by doctors should be strictly maintained
Medicines should be taken as prescribed
Identify and avoiding of triggers.
Making sure the child has vaccines for flu
PICOT
training of the experts who would be sent to schools as they have to communicate with children.
Communication with children requires proper soft skills, empathy and also implementation of
proper humor and tricks to keep them engaged and make them feel involved. The nurse’s
communication style should be exciting so that children remain hooked to the classes without the
missing any information.
2. Organization culture:
The proposed solution is very much consistent with the community culture. Children go
to school to learn about different aspect which help them to make their future life happier and
prosperous. The knowledge help them to prepare the capability of rational thinking and thereby
lead a healthy and prosperous lives. Therefore, this is one of the best medium for spreading of
health literacy on asthma and asthma management information. This should gradually be made a
part of their curriculum so that they become capable to handle their asthma symptoms
successfully and do not lead to serious events (Rasberry et al., 2014). However, the organization
who should be initiating this campaign should properly plan the health promotion program
effectively and allocate proper resources and funds before initiating the implementation of the
project.
Education plan for parents: the following will be provided in a brochure in details so that parents
can follow them.
Plan produced by doctors should be strictly maintained
Medicines should be taken as prescribed
Identify and avoiding of triggers.
Making sure the child has vaccines for flu
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
PICOT
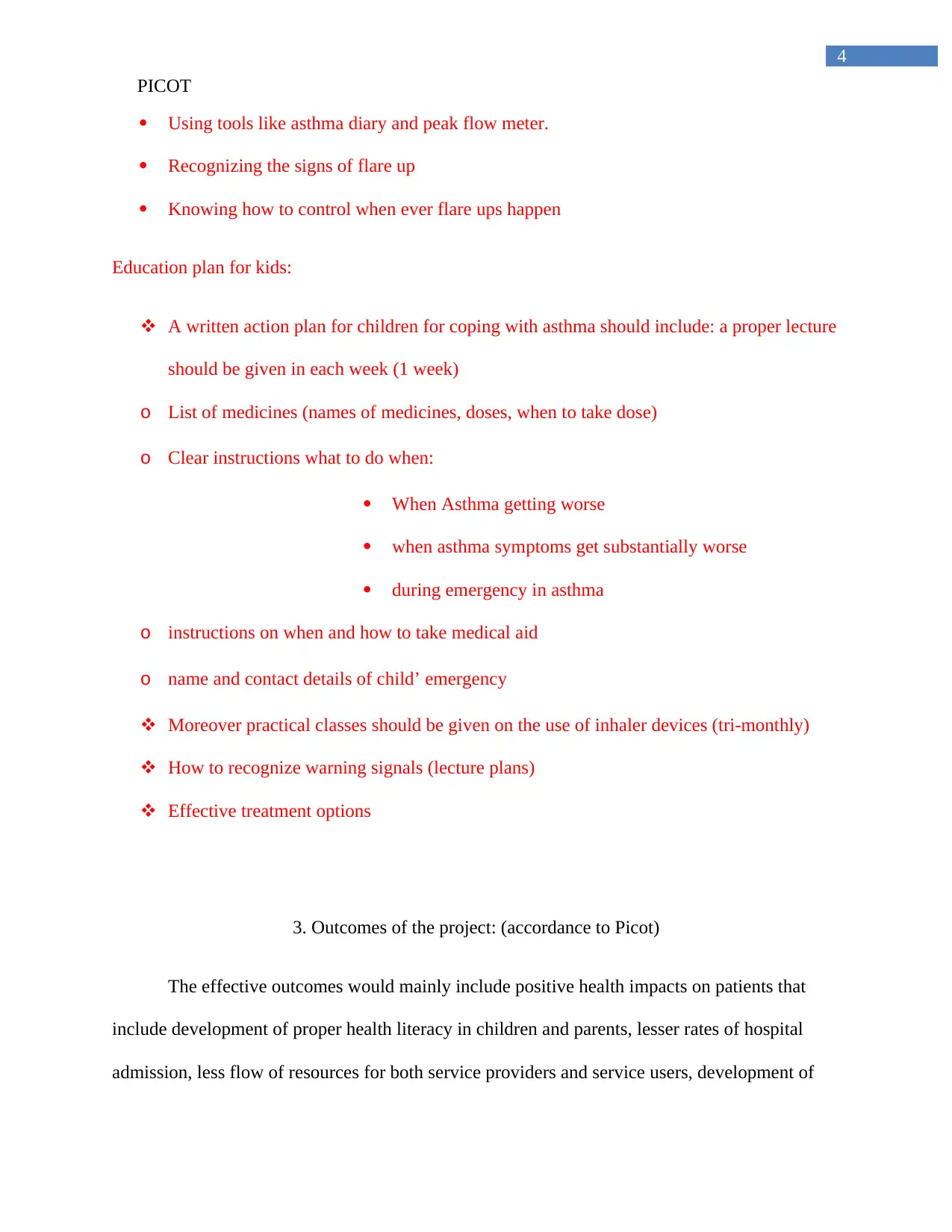
Using tools like asthma diary and peak flow meter.
Recognizing the signs of flare up
Knowing how to control when ever flare ups happen
Education plan for kids:
A written action plan for children for coping with asthma should include: a proper lecture
should be given in each week (1 week)
o List of medicines (names of medicines, doses, when to take dose)
o Clear instructions what to do when:
When Asthma getting worse
when asthma symptoms get substantially worse
during emergency in asthma
o instructions on when and how to take medical aid
o name and contact details of child’ emergency
Moreover practical classes should be given on the use of inhaler devices (tri-monthly)
How to recognize warning signals (lecture plans)
Effective treatment options
3. Outcomes of the project: (accordance to Picot)
The effective outcomes would mainly include positive health impacts on patients that
include development of proper health literacy in children and parents, lesser rates of hospital
admission, less flow of resources for both service providers and service users, development of
PICOT
Using tools like asthma diary and peak flow meter.
Recognizing the signs of flare up
Knowing how to control when ever flare ups happen
Education plan for kids:
A written action plan for children for coping with asthma should include: a proper lecture
should be given in each week (1 week)
o List of medicines (names of medicines, doses, when to take dose)
o Clear instructions what to do when:
When Asthma getting worse
when asthma symptoms get substantially worse
during emergency in asthma
o instructions on when and how to take medical aid
o name and contact details of child’ emergency
Moreover practical classes should be given on the use of inhaler devices (tri-monthly)
How to recognize warning signals (lecture plans)
Effective treatment options
3. Outcomes of the project: (accordance to Picot)
The effective outcomes would mainly include positive health impacts on patients that
include development of proper health literacy in children and parents, lesser rates of hospital
admission, less flow of resources for both service providers and service users, development of
5
PICOT
better quality life of the children, proper lifestyle modification and behaviors, proper protection
for allergens and irritants and many others
4 methods to achieve outcomes:
Importance of self management practice and behaviors.
Development of partnership between children, parents and primary healthcare
practitioners for proper management
Proper instruction on inhaler techniques
Written asthma management plan and brochures
Avoiding the risk of experiencing asthma by proper lifestyle and behavioral modification
(Harris et al., 2015)
5. Outcome impact:
If the initiatives are taken by the organization with proper association with the schools of
the locality it would help in preventing many unfortunate cases and suffering of patients by
developing patient quality life. Moreover, it would help in making environmental changes by
schools authorities, parents in their homes and other . This will reduce chances of allergens in
surrounding (Neuharth-Prichette & Getch, 2016). Moreover, it will also ensure cost saving for
resources (both for service users and service providers) at the same time of providing care. this
would increase the efficiency of the process.
PICOT
better quality life of the children, proper lifestyle modification and behaviors, proper protection
for allergens and irritants and many others
4 methods to achieve outcomes:
Importance of self management practice and behaviors.
Development of partnership between children, parents and primary healthcare
practitioners for proper management
Proper instruction on inhaler techniques
Written asthma management plan and brochures
Avoiding the risk of experiencing asthma by proper lifestyle and behavioral modification
(Harris et al., 2015)
5. Outcome impact:
If the initiatives are taken by the organization with proper association with the schools of
the locality it would help in preventing many unfortunate cases and suffering of patients by
developing patient quality life. Moreover, it would help in making environmental changes by
schools authorities, parents in their homes and other . This will reduce chances of allergens in
surrounding (Neuharth-Prichette & Getch, 2016). Moreover, it will also ensure cost saving for
resources (both for service users and service providers) at the same time of providing care. this
would increase the efficiency of the process.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
PICOT
References:
Blaakman, S. W., Cohen, A., Fagnano, M., & Halterman, J. S. (2014). Asthma medication
adherence among urban teens: A qualitative analysis of barriers, facilitators and
experiences with school-based care. Journal of Asthma, 51(5), 522-529.
Coelho, A. C. C., de Souza-Machado, C., & Souza-Machado, A. (2017). School intervention in
asthma for adolescents: it is time to act. Paediatric respiratory reviews, 23, 50-52.
Harris, K. M., Kneale, D., Lasserson, T. J., McDonald, V. M., Grigg, J., & Thomas, J. (2015).
School‐based self management interventions for asthma in children and adolescents: a
mixed methods systematic review. The Cochrane Library.
Neuharth-Pritchett, S., & Getch, Y. Q. (2016). The Effectiveness of a Brief Asthma Education
Intervention for Child Care Providers and Primary School Teachers. Early Childhood
Education Journal, 44(6), 555-561.
Rasberry, C. N., Cheung, K., Buckley, R., Dunville, R., Daniels, B., Cook, D., ... & Dean, B.
(2014). Indicators of asthma control among students in a rural, school-based asthma
management program. Journal of Asthma, 51(8), 876-885.
Reznik, M., Bauman, L. J., Okelo, S., & Halterman, J. S. (2015). Asthma identification and
medication administration forms in New York City schools. Annals of allergy, asthma &
immunology: official publication of the American College of Allergy, Asthma, &
Immunology, 114(1), 67.
PICOT
References:
Blaakman, S. W., Cohen, A., Fagnano, M., & Halterman, J. S. (2014). Asthma medication
adherence among urban teens: A qualitative analysis of barriers, facilitators and
experiences with school-based care. Journal of Asthma, 51(5), 522-529.
Coelho, A. C. C., de Souza-Machado, C., & Souza-Machado, A. (2017). School intervention in
asthma for adolescents: it is time to act. Paediatric respiratory reviews, 23, 50-52.
Harris, K. M., Kneale, D., Lasserson, T. J., McDonald, V. M., Grigg, J., & Thomas, J. (2015).
School‐based self management interventions for asthma in children and adolescents: a
mixed methods systematic review. The Cochrane Library.
Neuharth-Pritchett, S., & Getch, Y. Q. (2016). The Effectiveness of a Brief Asthma Education
Intervention for Child Care Providers and Primary School Teachers. Early Childhood
Education Journal, 44(6), 555-561.
Rasberry, C. N., Cheung, K., Buckley, R., Dunville, R., Daniels, B., Cook, D., ... & Dean, B.
(2014). Indicators of asthma control among students in a rural, school-based asthma
management program. Journal of Asthma, 51(8), 876-885.
Reznik, M., Bauman, L. J., Okelo, S., & Halterman, J. S. (2015). Asthma identification and
medication administration forms in New York City schools. Annals of allergy, asthma &
immunology: official publication of the American College of Allergy, Asthma, &
Immunology, 114(1), 67.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





