Sebaceous Carcinoma: Atypical Presentation and Management - Case Study
VerifiedAdded on 2023/06/07
|9
|1886
|269
Case Study
AI Summary
This case study describes a 75-year-old male patient who presented with sebaceous carcinoma on his left cheek, a less common location for this type of skin cancer which typically affects the eyelids. The patient had a history of non-melanoma skin cancer and presented with a rapidly growing papule. Diagnosis involved a shave biopsy, and treatment included Mohs micrographic surgery. Immunohistochemistry results and the association with Muir-Torre syndrome are discussed. The case emphasizes the importance of early diagnosis and treatment for improved survival rates, highlighting that sebaceous carcinoma can occur in locations other than the eyelids. Desklib offers a variety of solved assignments and past papers for students.

SEBACEOUS CARCINOMA
NAME
INSTITUTION
TUTOR
DATE
NAME
INSTITUTION
TUTOR
DATE
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ABSTRACT
Objective: To describe the case of sebaceous carcinoma in a 75 year old patient who
presented with a swelling on the cheek.
Case summary: The case study was on a 75 year old man who presented with a
hyperkeratotic papule on the left cheek with keratin core that had been present for six months.
Perioperative diagnosis on the skin of the left zygoma indicated sebaceous carcinoma. Histologic
sections indicated skin with unremarkable epidermis. There was also proliferation of the
sebaceous lobules which had basaloid keratinocytes at the periphery and it showed sebaceous
differentiation at their centers. A subset of the neoplastic cells show mature sebaceous
differentiation. On immunohistochemistry, the tumor cells expressed nuclear factor XIIIa, EMA
and P63 and they were negative for CK20.
Discussion: Sebaceous carcinoma develop in any sebaceous gland whose function is
lubricating the skin. However, it mostly begins around the eyelids. In this case study, the cancer
developed at the left cheek of the patient and this is why this case was of particular interest. This
type of cancer if diagnosed early and treated, it is usually successful but can turn out to be deadly
if spreads rapidly. This type of cancer sometimes appear in the form of a sty and that is why
majority delay the diagnosis and this leads to death .It is therefore important that one makes an
appointment whenever they note any growth or swelling on the eye.
Conclusion: Sebaceous carcinoma is a very type of skin cancer that mostly attacks the
eyelids leading to swelling. It can be diagnosed through skin examination as well as microscopic
examination of biopsies that reveal certain features. Treatment is either through surgery or Mohr
surgery and radiotherapy.
Objective: To describe the case of sebaceous carcinoma in a 75 year old patient who
presented with a swelling on the cheek.
Case summary: The case study was on a 75 year old man who presented with a
hyperkeratotic papule on the left cheek with keratin core that had been present for six months.
Perioperative diagnosis on the skin of the left zygoma indicated sebaceous carcinoma. Histologic
sections indicated skin with unremarkable epidermis. There was also proliferation of the
sebaceous lobules which had basaloid keratinocytes at the periphery and it showed sebaceous
differentiation at their centers. A subset of the neoplastic cells show mature sebaceous
differentiation. On immunohistochemistry, the tumor cells expressed nuclear factor XIIIa, EMA
and P63 and they were negative for CK20.
Discussion: Sebaceous carcinoma develop in any sebaceous gland whose function is
lubricating the skin. However, it mostly begins around the eyelids. In this case study, the cancer
developed at the left cheek of the patient and this is why this case was of particular interest. This
type of cancer if diagnosed early and treated, it is usually successful but can turn out to be deadly
if spreads rapidly. This type of cancer sometimes appear in the form of a sty and that is why
majority delay the diagnosis and this leads to death .It is therefore important that one makes an
appointment whenever they note any growth or swelling on the eye.
Conclusion: Sebaceous carcinoma is a very type of skin cancer that mostly attacks the
eyelids leading to swelling. It can be diagnosed through skin examination as well as microscopic
examination of biopsies that reveal certain features. Treatment is either through surgery or Mohr
surgery and radiotherapy.
INTRODUCTION
Sebaceous carcinoma is a type of skin cancer. This condition is however very rare. It is
sometimes known as aggressive sebaceous carcinoma due to its ability to spread. It mostly attack
the eyelids. This form of cancer usually begin as a form lump on the eyelids1 .As the cancer
proceeds, there is bleeding or oozing from the eyelids. When it occurs on other parts of the body,
the appearance is usually yellowish lumps which may also bleed2. In this assignment, there will
be description of a case study in which a patient was suffering from sebaceous carcinoma.
1 A Acosta et al, (2018) Sebaceous carcinoma of the breast in a patient with a pathogenic BRCA2 (886delGT)
mutation - focus on histopathologic and immunohistochemical features. APMIS, 126(4),
353-356.doi:10.1111/apm.12826
2 J Brewer et al, (2016). Effect of Non-Hodgkin Lymphoma on Survival in Patients With Malignant Fibrous
Histiocytoma, Kaposi Sarcoma, and Sebaceous Carcinoma. Dermatologic Surgery, 42, S32-
S39. doi:10.1097/dss.0000000000000520
Sebaceous carcinoma is a type of skin cancer. This condition is however very rare. It is
sometimes known as aggressive sebaceous carcinoma due to its ability to spread. It mostly attack
the eyelids. This form of cancer usually begin as a form lump on the eyelids1 .As the cancer
proceeds, there is bleeding or oozing from the eyelids. When it occurs on other parts of the body,
the appearance is usually yellowish lumps which may also bleed2. In this assignment, there will
be description of a case study in which a patient was suffering from sebaceous carcinoma.
1 A Acosta et al, (2018) Sebaceous carcinoma of the breast in a patient with a pathogenic BRCA2 (886delGT)
mutation - focus on histopathologic and immunohistochemical features. APMIS, 126(4),
353-356.doi:10.1111/apm.12826
2 J Brewer et al, (2016). Effect of Non-Hodgkin Lymphoma on Survival in Patients With Malignant Fibrous
Histiocytoma, Kaposi Sarcoma, and Sebaceous Carcinoma. Dermatologic Surgery, 42, S32-
S39. doi:10.1097/dss.0000000000000520
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
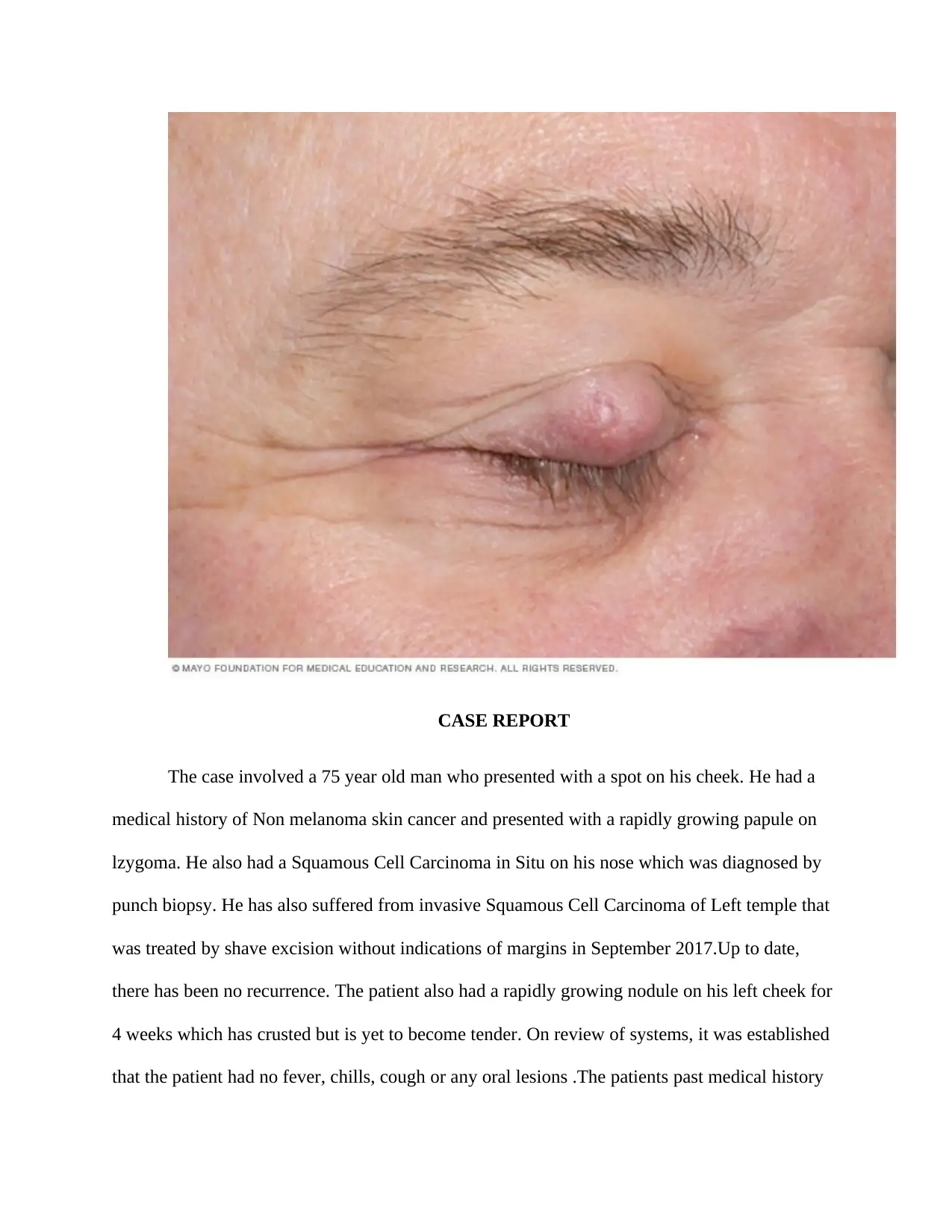
CASE REPORT
The case involved a 75 year old man who presented with a spot on his cheek. He had a
medical history of Non melanoma skin cancer and presented with a rapidly growing papule on
lzygoma. He also had a Squamous Cell Carcinoma in Situ on his nose which was diagnosed by
punch biopsy. He has also suffered from invasive Squamous Cell Carcinoma of Left temple that
was treated by shave excision without indications of margins in September 2017.Up to date,
there has been no recurrence. The patient also had a rapidly growing nodule on his left cheek for
4 weeks which has crusted but is yet to become tender. On review of systems, it was established
that the patient had no fever, chills, cough or any oral lesions .The patients past medical history
The case involved a 75 year old man who presented with a spot on his cheek. He had a
medical history of Non melanoma skin cancer and presented with a rapidly growing papule on
lzygoma. He also had a Squamous Cell Carcinoma in Situ on his nose which was diagnosed by
punch biopsy. He has also suffered from invasive Squamous Cell Carcinoma of Left temple that
was treated by shave excision without indications of margins in September 2017.Up to date,
there has been no recurrence. The patient also had a rapidly growing nodule on his left cheek for
4 weeks which has crusted but is yet to become tender. On review of systems, it was established
that the patient had no fever, chills, cough or any oral lesions .The patients past medical history
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
as well as social history, medications and any allergies were as well reviewed. It was established
that the patient’s family history has no contribution. On physical exam the patient was well
developed and well-nourished with no acute distress. On skin examination ,the scalp had an ill-
defined erythematous macules that had overlying adherent scales on the scalp .The face had an
ill-defined erythematous macules that had an overlying adhering scales on the forehead .There
was also a crust nodule that had keratin core on Lzygoma. The lips were normal as well as the
ears, the neck and the chest .The abdomen was also normal the assessment and plan included
neoplasm of uncertain behavior, zygoma .It was suspected to be Keratoacanthoma type
Squamous cell Carcinoma. After discussion on risks such as pain, bleeding, infection, recurrence
and scarring, consent was then obtained. The biopsy site was then adequately prepared using
alcohol, allowed to dry and then as infiltrated with 1% lidocaine with epinephrine .A shave
biopsy was then obtained using Derma blade /15 and the specimen taken to dernatopathology.
For purposes of maintaining hemostasis, Aluminum chloride was used. Antibiotic ointment and
clean dressing were also applied .The patient responded well to all the procedures. However,
both verbal and written wound care instructions were provided to the patient. The Actinic
keratosis which 5 of them were destroyed using liquid nitrogen cryotherapy. The patient also
tolerated to this procedure very well. The patient was to return to the clinic after 6 months.
The final diagnosis of skin left zygoma and shave biopsy indicated sebaceous carcinoma.
There was a plan to send the patient for Mohs and this was also discussed colonoscopy since this
was associated with Muir Torre syndrome. The patient was given the information and he was to
get with his PCP for colonoscopy because he has had that done 5 years ago. The patient was
informed about the sebaceous carcinoma and was therefore referred to Mohs. He was prescribed
aspirin which he stopped 7 days prior to the procedure.
that the patient’s family history has no contribution. On physical exam the patient was well
developed and well-nourished with no acute distress. On skin examination ,the scalp had an ill-
defined erythematous macules that had overlying adherent scales on the scalp .The face had an
ill-defined erythematous macules that had an overlying adhering scales on the forehead .There
was also a crust nodule that had keratin core on Lzygoma. The lips were normal as well as the
ears, the neck and the chest .The abdomen was also normal the assessment and plan included
neoplasm of uncertain behavior, zygoma .It was suspected to be Keratoacanthoma type
Squamous cell Carcinoma. After discussion on risks such as pain, bleeding, infection, recurrence
and scarring, consent was then obtained. The biopsy site was then adequately prepared using
alcohol, allowed to dry and then as infiltrated with 1% lidocaine with epinephrine .A shave
biopsy was then obtained using Derma blade /15 and the specimen taken to dernatopathology.
For purposes of maintaining hemostasis, Aluminum chloride was used. Antibiotic ointment and
clean dressing were also applied .The patient responded well to all the procedures. However,
both verbal and written wound care instructions were provided to the patient. The Actinic
keratosis which 5 of them were destroyed using liquid nitrogen cryotherapy. The patient also
tolerated to this procedure very well. The patient was to return to the clinic after 6 months.
The final diagnosis of skin left zygoma and shave biopsy indicated sebaceous carcinoma.
There was a plan to send the patient for Mohs and this was also discussed colonoscopy since this
was associated with Muir Torre syndrome. The patient was given the information and he was to
get with his PCP for colonoscopy because he has had that done 5 years ago. The patient was
informed about the sebaceous carcinoma and was therefore referred to Mohs. He was prescribed
aspirin which he stopped 7 days prior to the procedure.
The patient presented in clinic for Mohs micrographic surgery on the left cheek which
has been present for 6 months. The whole process was explained to the patient together with the
consequences. The Hibiclens scrub to the entire region was then performed. Anesthesia was
infiltrated while the patient was comfortably positioned. The apparent residual tumor was
debulked so as to obtain the best histology with minimal defects. After surgery, the biopsy was
then observed microscopically and the sections showed skin with unremarkable epidermis within
the dermis. There was also proliferation of sebaceous lobules that had basaloid keratinocytes at
the periphery and this indicate sebaceous differentiation in their centers. Neoplastic cells showed
mature sebaceous differentiation. Majority of mitosis were seen and there was nuclear atypia.
Overall, architectural growth was minimal infiltrative. On immunohistochemistry, the tumor
cells expressed nuclear factor XIIIa, EMA and finally P63 were all negative for the CK20 as well
neurofilament .Sebaceous neoplasms are mostly associated with the Muir- Torres syndrome.
DISCUSSION
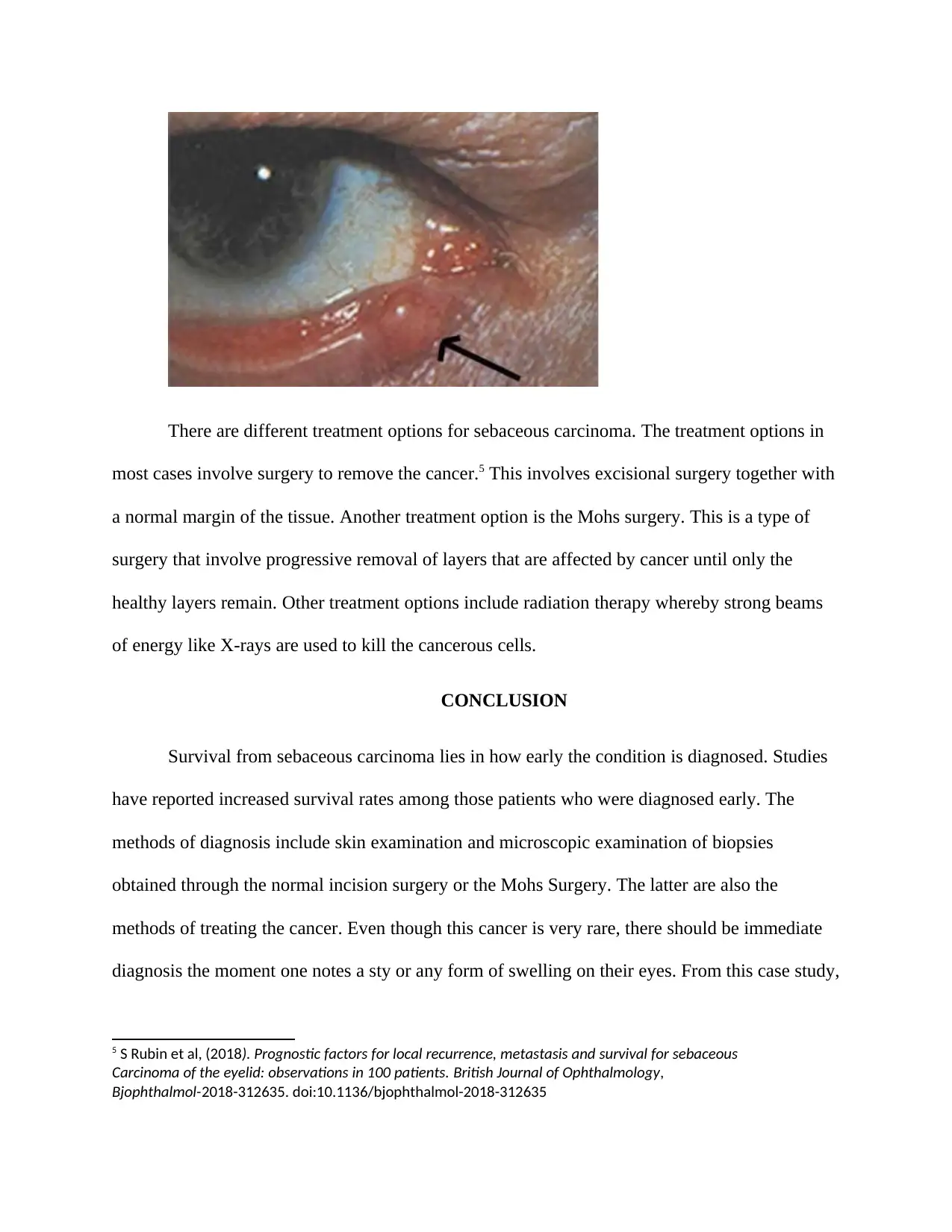
Sebaceous carcinoma is a rare cancer that often attack the eyelids and cause swelling.
There are different methods that can be used to diagnose sebaceous carcinoma3 .This was
particular case study was of particular interest since unlike many other sebaceous carcinomas
that develop at the eyelids, this was one was at the left cheek. The most common methods
include skin examination for reddening. An eye examination can also be carried out to check if
the eyelids are swollen4 .The final method that can be used to diagnose the condition is skin
biopsy. This involves removing a small portion of tissue for further testing.
3 Robert Kyllo, keegan Brady & Einsten Hurst, (2015). Sebaceous Carcinoma. Dermatologic
Surgery, 41(1), 1-15. doi:10.1097/dss.0000000000000152
4 J North et al,(2018) Cell of origin and mutation pattern define three clinically distinct classes of
Sebaceous carcinoma. Nature Communications, 9(1). doi:10.1038/s41467-018-04008-y
has been present for 6 months. The whole process was explained to the patient together with the
consequences. The Hibiclens scrub to the entire region was then performed. Anesthesia was
infiltrated while the patient was comfortably positioned. The apparent residual tumor was
debulked so as to obtain the best histology with minimal defects. After surgery, the biopsy was
then observed microscopically and the sections showed skin with unremarkable epidermis within
the dermis. There was also proliferation of sebaceous lobules that had basaloid keratinocytes at
the periphery and this indicate sebaceous differentiation in their centers. Neoplastic cells showed
mature sebaceous differentiation. Majority of mitosis were seen and there was nuclear atypia.
Overall, architectural growth was minimal infiltrative. On immunohistochemistry, the tumor
cells expressed nuclear factor XIIIa, EMA and finally P63 were all negative for the CK20 as well
neurofilament .Sebaceous neoplasms are mostly associated with the Muir- Torres syndrome.
DISCUSSION
Sebaceous carcinoma is a rare cancer that often attack the eyelids and cause swelling.
There are different methods that can be used to diagnose sebaceous carcinoma3 .This was
particular case study was of particular interest since unlike many other sebaceous carcinomas
that develop at the eyelids, this was one was at the left cheek. The most common methods
include skin examination for reddening. An eye examination can also be carried out to check if
the eyelids are swollen4 .The final method that can be used to diagnose the condition is skin
biopsy. This involves removing a small portion of tissue for further testing.
3 Robert Kyllo, keegan Brady & Einsten Hurst, (2015). Sebaceous Carcinoma. Dermatologic
Surgery, 41(1), 1-15. doi:10.1097/dss.0000000000000152
4 J North et al,(2018) Cell of origin and mutation pattern define three clinically distinct classes of
Sebaceous carcinoma. Nature Communications, 9(1). doi:10.1038/s41467-018-04008-y
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
There are different treatment options for sebaceous carcinoma. The treatment options in
most cases involve surgery to remove the cancer.5 This involves excisional surgery together with
a normal margin of the tissue. Another treatment option is the Mohs surgery. This is a type of
surgery that involve progressive removal of layers that are affected by cancer until only the
healthy layers remain. Other treatment options include radiation therapy whereby strong beams
of energy like X-rays are used to kill the cancerous cells.
CONCLUSION
Survival from sebaceous carcinoma lies in how early the condition is diagnosed. Studies
have reported increased survival rates among those patients who were diagnosed early. The
methods of diagnosis include skin examination and microscopic examination of biopsies
obtained through the normal incision surgery or the Mohs Surgery. The latter are also the
methods of treating the cancer. Even though this cancer is very rare, there should be immediate
diagnosis the moment one notes a sty or any form of swelling on their eyes. From this case study,
5 S Rubin et al, (2018). Prognostic factors for local recurrence, metastasis and survival for sebaceous
Carcinoma of the eyelid: observations in 100 patients. British Journal of Ophthalmology,
Bjophthalmol-2018-312635. doi:10.1136/bjophthalmol-2018-312635
most cases involve surgery to remove the cancer.5 This involves excisional surgery together with
a normal margin of the tissue. Another treatment option is the Mohs surgery. This is a type of
surgery that involve progressive removal of layers that are affected by cancer until only the
healthy layers remain. Other treatment options include radiation therapy whereby strong beams
of energy like X-rays are used to kill the cancerous cells.
CONCLUSION
Survival from sebaceous carcinoma lies in how early the condition is diagnosed. Studies
have reported increased survival rates among those patients who were diagnosed early. The
methods of diagnosis include skin examination and microscopic examination of biopsies
obtained through the normal incision surgery or the Mohs Surgery. The latter are also the
methods of treating the cancer. Even though this cancer is very rare, there should be immediate
diagnosis the moment one notes a sty or any form of swelling on their eyes. From this case study,
5 S Rubin et al, (2018). Prognostic factors for local recurrence, metastasis and survival for sebaceous
Carcinoma of the eyelid: observations in 100 patients. British Journal of Ophthalmology,
Bjophthalmol-2018-312635. doi:10.1136/bjophthalmol-2018-312635
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
it is apparently clear that sebaceous carcinoma does not necessarily arise from the eyelids but at
other locations like the cheek.
Bibliography
other locations like the cheek.
Bibliography
Articles
Acosta, A. M., Al Rasheed, M. R., Xu, H., Salibay, C., & Pins, M. R. (2018). Sebaceous
Carcinoma of the breast in a patient with a pathogenic BRCA2 (886delGT) mutation - focus
On histopathologic and immunohistochemical features. APMIS, 126(4), 353-356.
doi:10.1111/apm.12826
Brewer, J. D., Shana felt, T. D., Cerhan, J. R., Call, T. G., Weaver, A. L., & Otley, C. C.
(2016). Effect of Non-Hodgkin Lymphoma on Survival in Patients With Malignant Fibrous
Histiocytoma, Kaposi Sarcoma, and Sebaceous Carcinoma. Dermatologic Surgery, 42, S32-
S39. doi:10.1097/dss.0000000000000520
Kyllo, R. L., Brady, K. L., & Hurst, E. A. (2015). Sebaceous Carcinoma. Dermatologic
Surgery, 41(1), 1-15. doi:10.1097/dss.0000000000000152
North, J. P., Golovato, J., Vaske, C. J., Sanborn, J. Z., Nguyen, A., Wu, W., … Cho, R. J.
(2018). Cell of origin and mutation pattern define three clinically distinct classes of
sebaceous carcinoma. Nature Communications, 9(1). doi:10.1038/s41467-018-04008-y
Sa, H., Rubin, M. L., Xu, S., Ning, J., Tetzlaff, M., Sagiv, O., … Esmaeli, B. (2018).
Prognostic factors for local recurrence, metastasis and survival for sebaceous
carcinoma of the eyelid: observations in 100 patients. British Journal of Ophthalmology,
bjophthalmol-2018-312635. doi:10.1136/bjophthalmol-2018-312635
Acosta, A. M., Al Rasheed, M. R., Xu, H., Salibay, C., & Pins, M. R. (2018). Sebaceous
Carcinoma of the breast in a patient with a pathogenic BRCA2 (886delGT) mutation - focus
On histopathologic and immunohistochemical features. APMIS, 126(4), 353-356.
doi:10.1111/apm.12826
Brewer, J. D., Shana felt, T. D., Cerhan, J. R., Call, T. G., Weaver, A. L., & Otley, C. C.
(2016). Effect of Non-Hodgkin Lymphoma on Survival in Patients With Malignant Fibrous
Histiocytoma, Kaposi Sarcoma, and Sebaceous Carcinoma. Dermatologic Surgery, 42, S32-
S39. doi:10.1097/dss.0000000000000520
Kyllo, R. L., Brady, K. L., & Hurst, E. A. (2015). Sebaceous Carcinoma. Dermatologic
Surgery, 41(1), 1-15. doi:10.1097/dss.0000000000000152
North, J. P., Golovato, J., Vaske, C. J., Sanborn, J. Z., Nguyen, A., Wu, W., … Cho, R. J.
(2018). Cell of origin and mutation pattern define three clinically distinct classes of
sebaceous carcinoma. Nature Communications, 9(1). doi:10.1038/s41467-018-04008-y
Sa, H., Rubin, M. L., Xu, S., Ning, J., Tetzlaff, M., Sagiv, O., … Esmaeli, B. (2018).
Prognostic factors for local recurrence, metastasis and survival for sebaceous
carcinoma of the eyelid: observations in 100 patients. British Journal of Ophthalmology,
bjophthalmol-2018-312635. doi:10.1136/bjophthalmol-2018-312635
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





