CNA576 - Self-Management in Renal Nursing: Barriers and Solutions
VerifiedAdded on 2023/06/09
|9
|1910
|55
Report
AI Summary
This report examines self-management in renal nursing, focusing on the barriers to patient education and the promotion of self-management strategies. It highlights the increasing prevalence and cost of chronic kidney disease (CKD), emphasizing the importance of self-management in reducing patient burden and disease remission. Key barriers discussed include low patient awareness and health literacy, lack of motivation, and healthcare professional limitations such as time constraints and inadequate knowledge. The report also explores the Chronic Care Model as an evidence-based framework for supporting informed patients and collaborative healthcare teams. It concludes by stressing the importance of patient engagement in self-management programs and the need for effective evaluation methods in patient education. The report includes a lesson plan for self-management in kidney diseases, a feedback form example, and an illustration of the Chronic Care Model.
Self-Management in Renal Nursing
SELF-MANAGEMENT IN RENAL NURSING
By
Course
Tutor
University
Date
SELF-MANAGEMENT IN RENAL NURSING
By
Course
Tutor
University
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Self-Management in Renal Nursing 2
Introduction
Kidney diseases such as chronic kidney disease (CKD) have become one of the
leading causes of death around the world. Currently, there are 15.4 million people who have
been diagnosed with chronic kidney disease in the United Kingdom and this number is
expected to rise by the year 2025 to 42% of people 65 years and above who have been
diagnosed with the condition (Nazar et al. 2014). The number of people diagnosed with
kidney disease in the United States has increased by 20 to 25% within the last decade where
in 2004, 339 new cases of end-stage renal disease were reported per one million people
(Nazar et al. 2014).
In the United States, the amount of money spent on treating chronic and terminal
kidney disease amounts to 18.5 billion and from this amount, 16.3 billion USD is allocated to
dialysis which when applied to an individual patient amounts to 66,650USD per year (Nazar
et al.2014). The cost of treating kidney disease is high and it places a huge financial burden
on the patient and their family. This is why self-management has become important in
reducing this burden and also reducing chances of relapse or disease remission (Lin et al.
2013). The purpose of this paper will be to look at the potential barriers clinicians might face
when educating/promoting self-management and the evidence-based research available on
self-management.
Potential Barriers to Education and Promotion of Self-Management
Patients suffering from chronic diseases have had better health outcome when they
undertake patient education and self-management activities. However, some barriers exist
that prevent the proper education and self-management of chronic disease patients (Narva,
Norton & Boulware 2016). One of these barriers is the lack of patient awareness about their
illness and the health risks posed by that condition. According to Narva, Norton and
Introduction
Kidney diseases such as chronic kidney disease (CKD) have become one of the
leading causes of death around the world. Currently, there are 15.4 million people who have
been diagnosed with chronic kidney disease in the United Kingdom and this number is
expected to rise by the year 2025 to 42% of people 65 years and above who have been
diagnosed with the condition (Nazar et al. 2014). The number of people diagnosed with
kidney disease in the United States has increased by 20 to 25% within the last decade where
in 2004, 339 new cases of end-stage renal disease were reported per one million people
(Nazar et al. 2014).
In the United States, the amount of money spent on treating chronic and terminal
kidney disease amounts to 18.5 billion and from this amount, 16.3 billion USD is allocated to
dialysis which when applied to an individual patient amounts to 66,650USD per year (Nazar
et al.2014). The cost of treating kidney disease is high and it places a huge financial burden
on the patient and their family. This is why self-management has become important in
reducing this burden and also reducing chances of relapse or disease remission (Lin et al.
2013). The purpose of this paper will be to look at the potential barriers clinicians might face
when educating/promoting self-management and the evidence-based research available on
self-management.
Potential Barriers to Education and Promotion of Self-Management
Patients suffering from chronic diseases have had better health outcome when they
undertake patient education and self-management activities. However, some barriers exist
that prevent the proper education and self-management of chronic disease patients (Narva,
Norton & Boulware 2016). One of these barriers is the lack of patient awareness about their
illness and the health risks posed by that condition. According to Narva, Norton and
Self-Management in Renal Nursing 3
Boulware (2016), the general public has a poorer understanding of the function of kidneys
when compared to their knowledge of the heart, lungs or brain. Even for patients suffering
from chronic kidney disease, their level of health literacy is low regarding their condition.
Health literacy as defined by the United States Health Resources and Services
Administration (2015) refers to the ability patients or health consumers have to acquire and
understand health information which they can use to make informed healthcare decisions.
Patients suffering from chronic kidney disease have a notably low health literacy which in
turn affects their educational and self-management behavior. Having a high level of literacy
and education has improved the health outcomes of diabetic patients considerably which is
why a lot of effort has to be put in teaching kidney disease patients about self-management
(Narva, Norton & Boulware 2016).
Another barrier to patient education and self-management is the readiness to learn of
the patient. The low perceived susceptibility to kidney disease affects the motivation of
patients to learn and seek more knowledge on chronic kidney disease. Also, because most
kidney diseases are asymptomatic, patients don’t have the sense of urgency to acquire
information or consult healthcare professionals about disease complications and symptoms
(Narva, Norton & Boulware 2016). Patients who have been diagnosed with chronic kidney
disease can easily become emotionally, psychologically and physically overwhelmed. This in
turn affects their motivation to learn and they avoid any educational material related to their
disease (Narva, Norton & Boulware 2016).
Healthcare professionals also present a barrier in the education of their patients
especially when they don’t prioritize chronic kidney conditions. They also face time
constraints during patient education especially for those working in primary care. This is
because they have a very limited amount of time to address the various health issues for every
Boulware (2016), the general public has a poorer understanding of the function of kidneys
when compared to their knowledge of the heart, lungs or brain. Even for patients suffering
from chronic kidney disease, their level of health literacy is low regarding their condition.
Health literacy as defined by the United States Health Resources and Services
Administration (2015) refers to the ability patients or health consumers have to acquire and
understand health information which they can use to make informed healthcare decisions.
Patients suffering from chronic kidney disease have a notably low health literacy which in
turn affects their educational and self-management behavior. Having a high level of literacy
and education has improved the health outcomes of diabetic patients considerably which is
why a lot of effort has to be put in teaching kidney disease patients about self-management
(Narva, Norton & Boulware 2016).
Another barrier to patient education and self-management is the readiness to learn of
the patient. The low perceived susceptibility to kidney disease affects the motivation of
patients to learn and seek more knowledge on chronic kidney disease. Also, because most
kidney diseases are asymptomatic, patients don’t have the sense of urgency to acquire
information or consult healthcare professionals about disease complications and symptoms
(Narva, Norton & Boulware 2016). Patients who have been diagnosed with chronic kidney
disease can easily become emotionally, psychologically and physically overwhelmed. This in
turn affects their motivation to learn and they avoid any educational material related to their
disease (Narva, Norton & Boulware 2016).
Healthcare professionals also present a barrier in the education of their patients
especially when they don’t prioritize chronic kidney conditions. They also face time
constraints during patient education especially for those working in primary care. This is
because they have a very limited amount of time to address the various health issues for every
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Self-Management in Renal Nursing 4
patient waiting to be seen (Yarnall et al. 2003). Another provider barrier is that clinicians feel
inadequate in their knowledge of kidney disease which affects their patient education. The
lengthy and descriptive kidney disease guidelines and the lack of guidance on how to educate
patients usually intimidates and confuses them which leads to the postponement of the
teaching session until a referral to a nephrologist is made. The lack of collaboration between
kidney specialists and primary care providers also plays a role in poor patient education
because they both assume that the other has performed education (Greer et al. 2015). To
overcome these barriers, patients need adequate support and effective educational strategies
which should be incorporated into their routine care (Narva, Norton & Boulware 2016).
Evidence-based Research on Self-Management Education
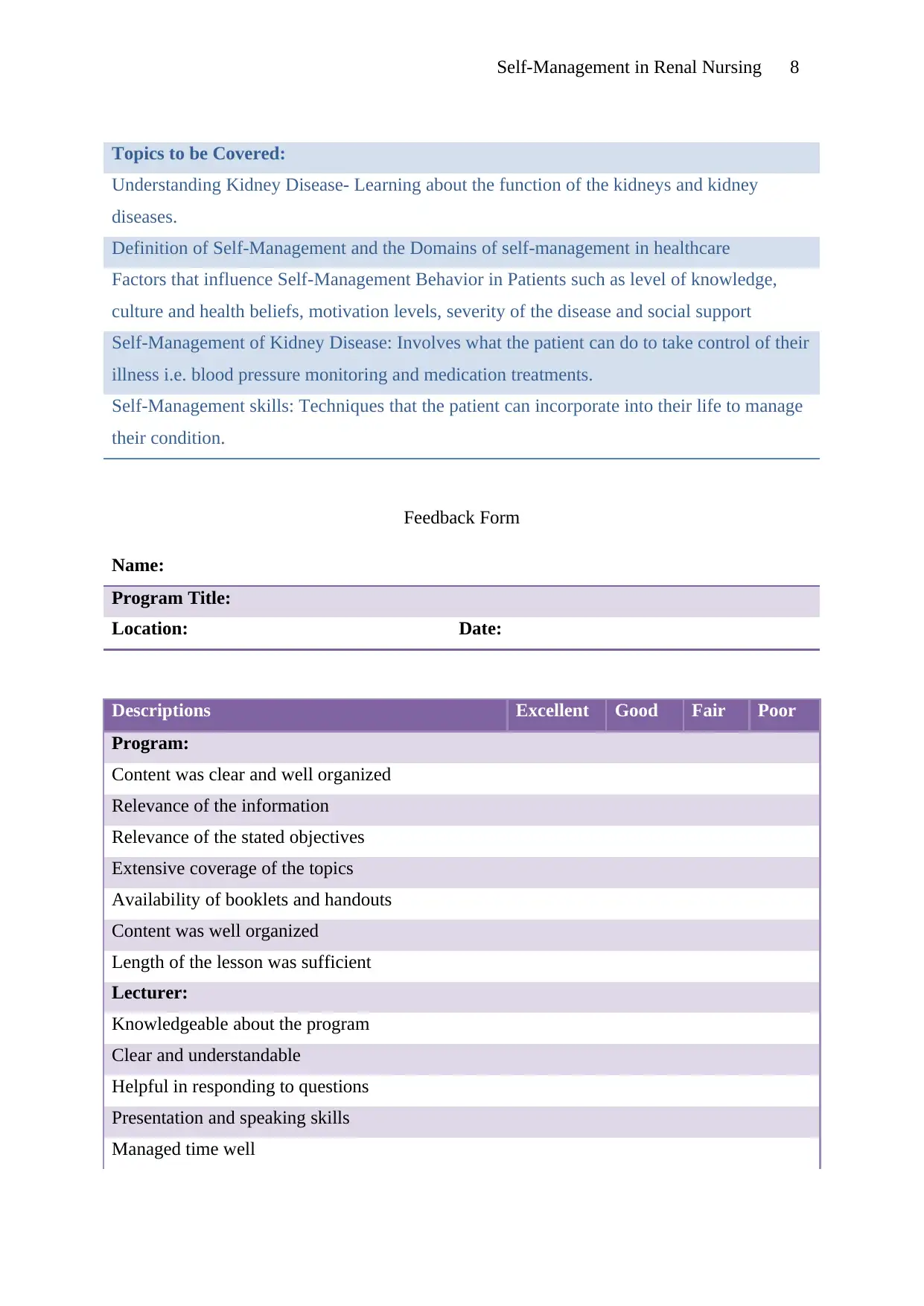
The chronic care model is an evidence-based framework that is used to support
patients who want to be well informed of their condition and prepare healthcare staff to
collaborate with the patient as they manage their illness (Epping-Jordan et al. 2004). This
model is being used in varying degrees in Sweden, the United Kingdom and other developed
countries to address self-management strategies for patients suffering from diabetes,
hypertension, chronic kidney disease and cancer. The care model was designed to improve
the health outcomes of chronic disease patients by having productive interactions with well
informed patients and healthcare teams (Parlour & Slater 2011).
The chronic care model includes a key component which is the role of self-
management programs whose aim is to empower chronic disease patients to take control of
their condition by managing their medications, measuring their blood pressure, monitoring
their symptoms and maintaining normality of their life (Epping-Jordan et al.2004). The model
has four components which are seen as important in the proper care of chronic illnesses and
these components are self-management support, healthcare delivery systems, patient support
patient waiting to be seen (Yarnall et al. 2003). Another provider barrier is that clinicians feel
inadequate in their knowledge of kidney disease which affects their patient education. The
lengthy and descriptive kidney disease guidelines and the lack of guidance on how to educate
patients usually intimidates and confuses them which leads to the postponement of the
teaching session until a referral to a nephrologist is made. The lack of collaboration between
kidney specialists and primary care providers also plays a role in poor patient education
because they both assume that the other has performed education (Greer et al. 2015). To
overcome these barriers, patients need adequate support and effective educational strategies
which should be incorporated into their routine care (Narva, Norton & Boulware 2016).
Evidence-based Research on Self-Management Education
The chronic care model is an evidence-based framework that is used to support
patients who want to be well informed of their condition and prepare healthcare staff to
collaborate with the patient as they manage their illness (Epping-Jordan et al. 2004). This
model is being used in varying degrees in Sweden, the United Kingdom and other developed
countries to address self-management strategies for patients suffering from diabetes,
hypertension, chronic kidney disease and cancer. The care model was designed to improve
the health outcomes of chronic disease patients by having productive interactions with well
informed patients and healthcare teams (Parlour & Slater 2011).
The chronic care model includes a key component which is the role of self-
management programs whose aim is to empower chronic disease patients to take control of
their condition by managing their medications, measuring their blood pressure, monitoring
their symptoms and maintaining normality of their life (Epping-Jordan et al.2004). The model
has four components which are seen as important in the proper care of chronic illnesses and
these components are self-management support, healthcare delivery systems, patient support
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Self-Management in Renal Nursing 5
in decision making and access to healthcare/clinical information (Epping-Jordan et al. 2004).
An illustration of the model is further shown in the appendix.
Conclusion
Self-management is important in managing chronic diseases, most of which are
curable when managed properly. It then becomes important for patients with chronic kidney
to engage in self-management programs and education where they can learn about their
disease and how to manage it properly. For patient education to be successful, evaluation
needs to be done which can be in the form of a question and answer session at the end of the
lesson, collecting feedback in the form of surveys, questionnaires or feedback forms.
in decision making and access to healthcare/clinical information (Epping-Jordan et al. 2004).
An illustration of the model is further shown in the appendix.
Conclusion
Self-management is important in managing chronic diseases, most of which are
curable when managed properly. It then becomes important for patients with chronic kidney
to engage in self-management programs and education where they can learn about their
disease and how to manage it properly. For patient education to be successful, evaluation
needs to be done which can be in the form of a question and answer session at the end of the
lesson, collecting feedback in the form of surveys, questionnaires or feedback forms.
Self-Management in Renal Nursing 6
References
Epping-Jordan, JE, Pruitt, SD, Bengoa R & Wagner, EH 2004, ‘Improving the quality of
healthcare for chronic conditions’, Quality and Safety in Healthcare, vol.13, no.4, pp.299-
305. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1743863/pdf/v013p00299.pdf [25 July 2018]
Greer, RC, Ameling, JM, Cavanaugh, KL, Jaar, BG, Grubbs, V, Andrews, CE, Ephraim, P,
Powe, NR, Lewis, J, Umeukeje, E, Gimenez, L, James, S & Boulware, LE 2015, ‘Specialist
and primary care physicians’ views on barriers to adequate preparation of patients for renal
replacement therapy: a qualitative study’, BMC Nephrology, vol. 16, no.37. Available from:
https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-015-0020-x. [25 July 2018].
Health Resources and Services Administration 2015, About Health Literacy; secondary
Health Resources and Services Administration. Available from:
http://www.hrsa.gov/publichealth/healthliteracy/healthlitabout.html. [25 July 2018].
Lin, C, Tsai, F, Lin, H, Hwang, S & Chen, HC 2013, ‘Effects of a self-management program
on patients with early-stage chronic kidney disease: a pilot study’, Applied Nursing Research,
vol.26, pp.151-156. Available from:
https://www.researchgate.net/publication/235879913_Effects_of_a_self-
management_program_on_patients_with_early-
stage_chronic_kidney_disease_A_pilot_study. [25 July 2018].
Narva, AS, Norton, JM & Boulware, LE 2016, ‘Educating patients about CKD: the path to
self-management and patient-centered care’, Clinical Journal of the American Society of
Nephrology, vol.11, no.4, pp.694-703. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4822666/ [25 July 2018].
References
Epping-Jordan, JE, Pruitt, SD, Bengoa R & Wagner, EH 2004, ‘Improving the quality of
healthcare for chronic conditions’, Quality and Safety in Healthcare, vol.13, no.4, pp.299-
305. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1743863/pdf/v013p00299.pdf [25 July 2018]
Greer, RC, Ameling, JM, Cavanaugh, KL, Jaar, BG, Grubbs, V, Andrews, CE, Ephraim, P,
Powe, NR, Lewis, J, Umeukeje, E, Gimenez, L, James, S & Boulware, LE 2015, ‘Specialist
and primary care physicians’ views on barriers to adequate preparation of patients for renal
replacement therapy: a qualitative study’, BMC Nephrology, vol. 16, no.37. Available from:
https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-015-0020-x. [25 July 2018].
Health Resources and Services Administration 2015, About Health Literacy; secondary
Health Resources and Services Administration. Available from:
http://www.hrsa.gov/publichealth/healthliteracy/healthlitabout.html. [25 July 2018].
Lin, C, Tsai, F, Lin, H, Hwang, S & Chen, HC 2013, ‘Effects of a self-management program
on patients with early-stage chronic kidney disease: a pilot study’, Applied Nursing Research,
vol.26, pp.151-156. Available from:
https://www.researchgate.net/publication/235879913_Effects_of_a_self-
management_program_on_patients_with_early-
stage_chronic_kidney_disease_A_pilot_study. [25 July 2018].
Narva, AS, Norton, JM & Boulware, LE 2016, ‘Educating patients about CKD: the path to
self-management and patient-centered care’, Clinical Journal of the American Society of
Nephrology, vol.11, no.4, pp.694-703. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4822666/ [25 July 2018].
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Self-Management in Renal Nursing 7
Nazar, CMJ, Kindratt, TB, Ahmad, SMA, Ahmed, M & Anderson, J 2014, ‘Barriers to the
successful practice of chronic kidney diseases at the primary healthcare level; a systematic
review’, Journal of Renal Injury Prevention, vol. 3, no.3, pp.61-67. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4206053/.[25 July 2018].
Parlour, R & Slater P 2011, An evaluation of the effectiveness of a self-management
programme, June 2011, Office of the Nursing and Midwifery Services Director. Available
from: https://www.icgp-education.ie/chronic-condition-self-management/Evaluation-of-a-
Self-Management-Programme.pdf [25 July 2018]
Yarnall, KSH, Pollak, KI, Ostbye, T & Krause, KM 2003, ‘Primary care: is there enough
time for prevention’, American Journal of Public Health, vol.93, no.4, pp.635-641. Available
from: https://warwick.ac.uk/fac/med/study/ugr/mbchb/phase1_08/semester2/
healthpsychology/session5/yarnall_2003.pdf. [25 July 2018].
Appendices
Lesson Plan for Self-Management in Kidney Diseases
Target Audience: Patients diagnosed with Chronic Kidney Disease
Resources to be used: PowerPoint Presentation, instructional materials, booklets
Nazar, CMJ, Kindratt, TB, Ahmad, SMA, Ahmed, M & Anderson, J 2014, ‘Barriers to the
successful practice of chronic kidney diseases at the primary healthcare level; a systematic
review’, Journal of Renal Injury Prevention, vol. 3, no.3, pp.61-67. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4206053/.[25 July 2018].
Parlour, R & Slater P 2011, An evaluation of the effectiveness of a self-management
programme, June 2011, Office of the Nursing and Midwifery Services Director. Available
from: https://www.icgp-education.ie/chronic-condition-self-management/Evaluation-of-a-
Self-Management-Programme.pdf [25 July 2018]
Yarnall, KSH, Pollak, KI, Ostbye, T & Krause, KM 2003, ‘Primary care: is there enough
time for prevention’, American Journal of Public Health, vol.93, no.4, pp.635-641. Available
from: https://warwick.ac.uk/fac/med/study/ugr/mbchb/phase1_08/semester2/
healthpsychology/session5/yarnall_2003.pdf. [25 July 2018].
Appendices
Lesson Plan for Self-Management in Kidney Diseases
Target Audience: Patients diagnosed with Chronic Kidney Disease
Resources to be used: PowerPoint Presentation, instructional materials, booklets
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Self-Management in Renal Nursing 8
Topics to be Covered:
Understanding Kidney Disease- Learning about the function of the kidneys and kidney
diseases.
Definition of Self-Management and the Domains of self-management in healthcare
Factors that influence Self-Management Behavior in Patients such as level of knowledge,
culture and health beliefs, motivation levels, severity of the disease and social support
Self-Management of Kidney Disease: Involves what the patient can do to take control of their
illness i.e. blood pressure monitoring and medication treatments.
Self-Management skills: Techniques that the patient can incorporate into their life to manage
their condition.
Feedback Form
Name:
Program Title:
Location: Date:
Descriptions Excellent Good Fair Poor
Program:
Content was clear and well organized
Relevance of the information
Relevance of the stated objectives
Extensive coverage of the topics
Availability of booklets and handouts
Content was well organized
Length of the lesson was sufficient
Lecturer:
Knowledgeable about the program
Clear and understandable
Helpful in responding to questions
Presentation and speaking skills
Managed time well
Topics to be Covered:
Understanding Kidney Disease- Learning about the function of the kidneys and kidney
diseases.
Definition of Self-Management and the Domains of self-management in healthcare
Factors that influence Self-Management Behavior in Patients such as level of knowledge,
culture and health beliefs, motivation levels, severity of the disease and social support
Self-Management of Kidney Disease: Involves what the patient can do to take control of their
illness i.e. blood pressure monitoring and medication treatments.
Self-Management skills: Techniques that the patient can incorporate into their life to manage
their condition.
Feedback Form
Name:
Program Title:
Location: Date:
Descriptions Excellent Good Fair Poor
Program:
Content was clear and well organized
Relevance of the information
Relevance of the stated objectives
Extensive coverage of the topics
Availability of booklets and handouts
Content was well organized
Length of the lesson was sufficient
Lecturer:
Knowledgeable about the program
Clear and understandable
Helpful in responding to questions
Presentation and speaking skills
Managed time well

Self-Management in Renal Nursing 9
Covered all topics
Overall program evaluation
Additional Comments:
The Chronic Care Model (Epping-Jordan et al. 2004)
Functional and Clinical Outcomes
Community
Resources and
Policies
Health System; Organization of Health Care
Support in self-management, healthcare delivery systems,
support in decision making and health information
Well informed patient Prepared healthcare
teams
Covered all topics
Overall program evaluation
Additional Comments:
The Chronic Care Model (Epping-Jordan et al. 2004)
Functional and Clinical Outcomes
Community
Resources and
Policies
Health System; Organization of Health Care
Support in self-management, healthcare delivery systems,
support in decision making and health information
Well informed patient Prepared healthcare
teams
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





