SOAP Note Analysis and Treatment Plan: Lab Assessment Test
VerifiedAdded on 2022/09/27
|5
|795
|41
Practical Assignment
AI Summary
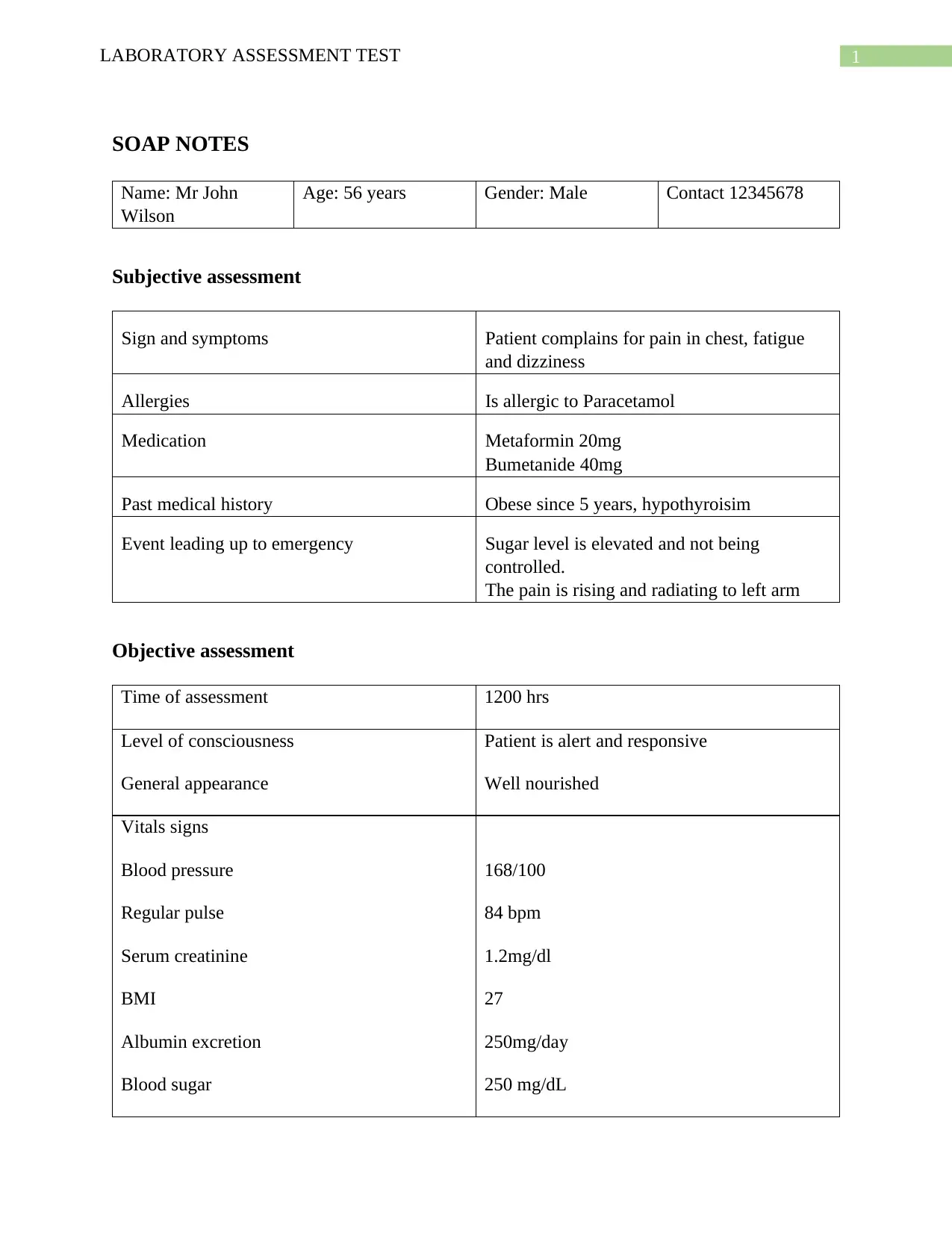
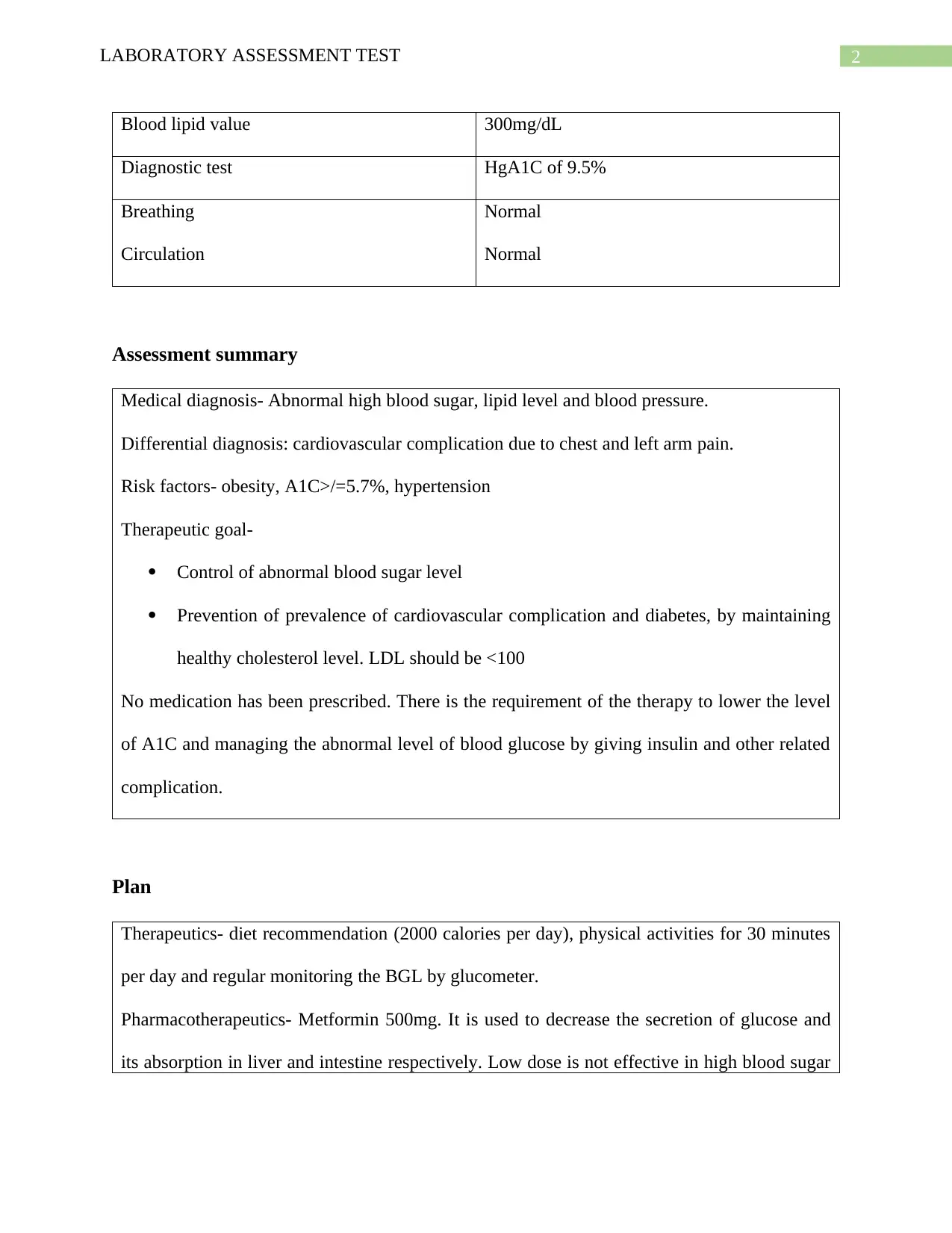
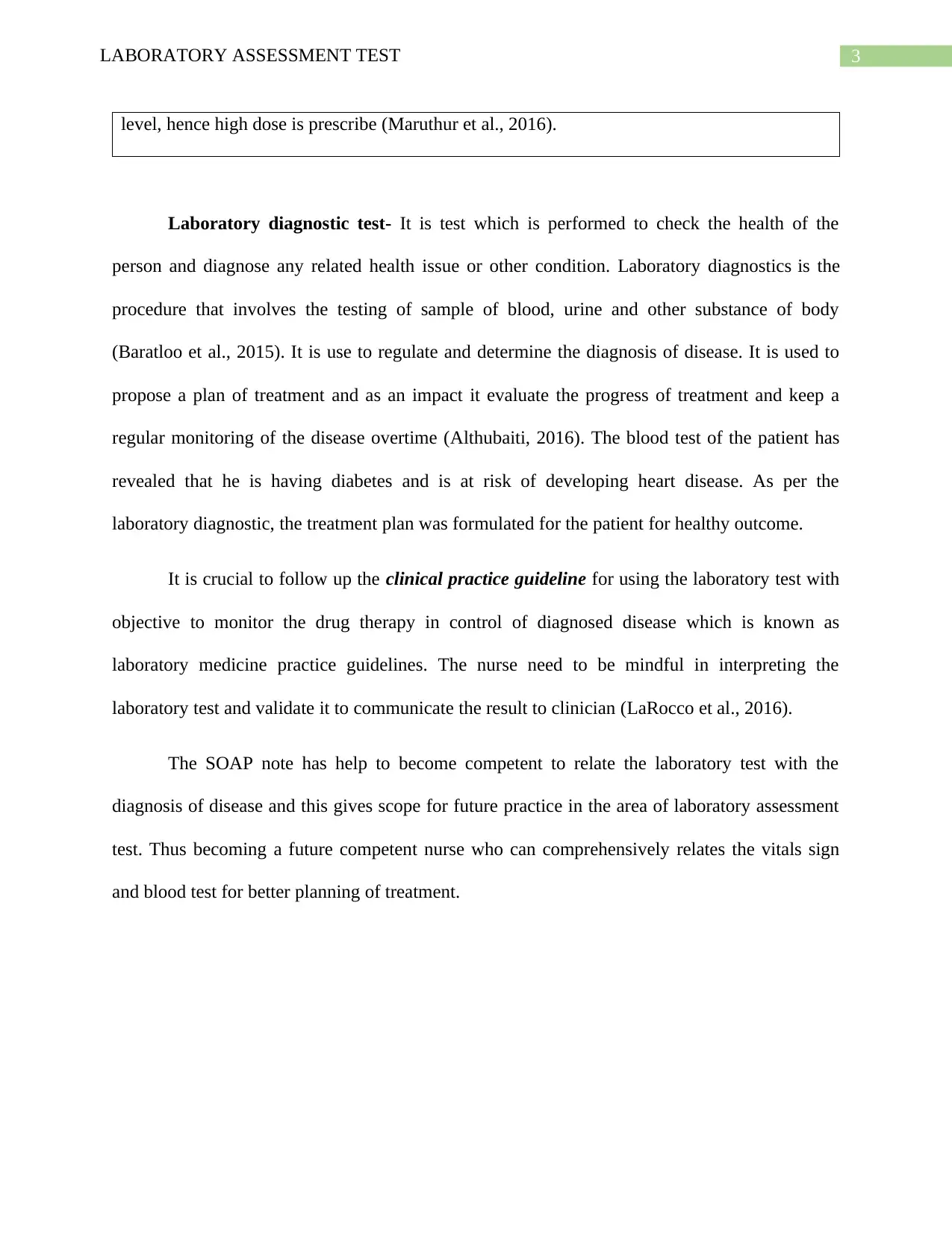
This document presents a SOAP (Subjective, Objective, Assessment, Plan) note based on a laboratory assessment test for a 56-year-old male patient, Mr. John Wilson. The subjective assessment reveals complaints of chest pain, fatigue, and dizziness, along with allergies to Paracetamol. The objective assessment includes vital signs such as elevated blood pressure (168/100) and a high blood sugar level (250 mg/dL), alongside diagnostic tests like an HgA1C of 9.5%. The assessment summarizes a medical diagnosis of abnormally high blood sugar, lipid levels, and blood pressure, with a differential diagnosis of potential cardiovascular complications. The therapeutic goals include controlling blood sugar levels and preventing cardiovascular complications. The plan outlines diet recommendations (2000 calories per day), physical activity, and pharmacotherapeutics using Metformin 500mg, alongside regular monitoring of blood glucose levels. The document emphasizes the importance of laboratory diagnostic tests in diagnosing diseases, formulating treatment plans, and monitoring treatment progress. It references various studies on the effectiveness of laboratory tests and the importance of interpreting results accurately for effective patient care, concluding with a reference list.
1 out of 5







![[object Object]](/_next/static/media/star-bottom.7253800d.svg)