Nursing Report: Social Determinants of Health in Diabetic Patients
VerifiedAdded on 2022/10/09
|8
|1587
|187
Report
AI Summary
This nursing report delves into the social determinants of health impacting diabetic patients, including healthcare access, education, economic stability, the built environment, and social support. It highlights how these factors influence self-management and overall health outcomes. The report discusses interventions such as patient education, self-management strategies, and family interventions to improve patient care and quality of life. It emphasizes the importance of addressing socioeconomic and environmental barriers to effectively manage diabetes, citing relevant research and studies to support its findings. The report concludes by advocating for a holistic approach to diabetes management that considers the complex interplay of social determinants and patient-centered care.
Running head: Nursing 1
Nursing
by
Course:
Tutor:
University:
Department:
Date:
Nursing
by
Course:
Tutor:
University:
Department:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Nursing 2
Social, Determinants of Health among Diabetic Patients
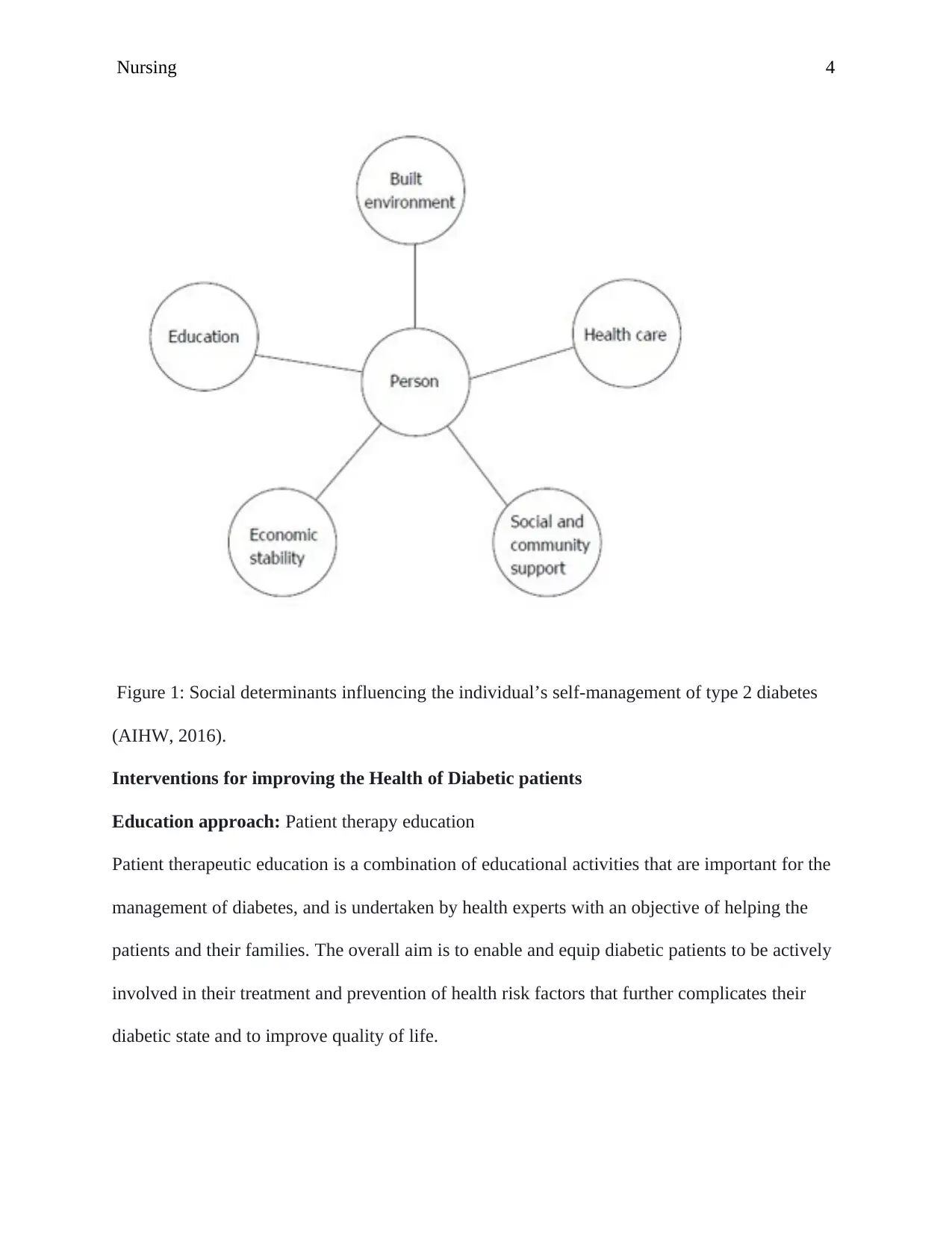
Diabetes is a chronic disease characterized by high levels of glucose in the blood. According to
the World Health Organization (WHO) (n.d.), social determinants are the conditions in which
individuals develop, live, operate and age, and the sickness management schemes are in place.
The social determinants of health among diabetic patients include health care, education,
economic stability, built environment, social and community support as illustrated in Figure 1.
Health care
Limited health care resources are a social determinant that can limit access to health facilities or
improve the likelihood of poor health outcomes. Aspects like transportation, neighbourhood
security and nutritious diet are components of the physical environment. If obstacles to these
variables exist among diabetic patients, this will lead to inaccessibility to resources among low-
income communities, thus magnifying the impacts. For instance, poor transportation in rural
areas may make it difficult to access health care services or healthy food (Walker,
Gebregziabher, Martin-Harris, & Egede, 2014). Thus, the absence of public transport in remote
or city regions may deter people from travelling to access better health care.
Education
Better academic achievement has been associated with enhanced health results, due to a higher
probability of socio-economic stability as opposed to those with lower educational levels.
Socioeconomic factors include the education level that also determines one’s ability to afford
health insurance coverage. Economically disadvantaged areas often lack main and epxert health
care providers, reducing access to health care for residents with chronic diseases such as
diabetes. Studies have indicated that the more educated individuals have higher chances of
Social, Determinants of Health among Diabetic Patients
Diabetes is a chronic disease characterized by high levels of glucose in the blood. According to
the World Health Organization (WHO) (n.d.), social determinants are the conditions in which
individuals develop, live, operate and age, and the sickness management schemes are in place.
The social determinants of health among diabetic patients include health care, education,
economic stability, built environment, social and community support as illustrated in Figure 1.
Health care
Limited health care resources are a social determinant that can limit access to health facilities or
improve the likelihood of poor health outcomes. Aspects like transportation, neighbourhood
security and nutritious diet are components of the physical environment. If obstacles to these
variables exist among diabetic patients, this will lead to inaccessibility to resources among low-
income communities, thus magnifying the impacts. For instance, poor transportation in rural
areas may make it difficult to access health care services or healthy food (Walker,
Gebregziabher, Martin-Harris, & Egede, 2014). Thus, the absence of public transport in remote
or city regions may deter people from travelling to access better health care.
Education
Better academic achievement has been associated with enhanced health results, due to a higher
probability of socio-economic stability as opposed to those with lower educational levels.
Socioeconomic factors include the education level that also determines one’s ability to afford
health insurance coverage. Economically disadvantaged areas often lack main and epxert health
care providers, reducing access to health care for residents with chronic diseases such as
diabetes. Studies have indicated that the more educated individuals have higher chances of
Nursing 3
accessing preventive healthcare such as consumption of nutritious diet and living an active life
thus, preventing obesity (Australia Institute of Health and Welfare (AIHW). (2016).
Economic stability
Economic stability has been recognized as a major determinant of health's social determinants.
There is a positive association between Income and health. Additionally, the key elements of
economic stability, including low economic status, jobs, food safety, and proper housing, are
related to health status. Employment is attributable to the health of a person as the rate of
unemployment rises, disease and premature death rise as well (Clark, & Utz, 2014).
Built environment
It is usually recognized that exercise, among other advantages, helps control weight, fights
cardiovascular disease, increases mood, and expands life expectancy. The geography of a region
is sometimes not conducive to pedestrian traffic, and security issues deter outdoor activity. There
can simply be no available space for walking, cycling or jogging public spaces. The
neighbourhoods and built environment shapes live (Koh, Piotrowski, Kumanyika, & Fielding,
2011).
Social and community support
The degree of social support may differ amongst individuals and race; for instance, a study has
shown that diabetic Hispanic people have adopted self-management approach instead of medical
visits (Strom & Egede, 2012). In the same way higher, social support corresponds with enhanced
self-management results, it has been shown that the insight of adverse or low concentrations of
social support increases the danger of fewer self-management behaviours (Strom & Egede,
2012).
accessing preventive healthcare such as consumption of nutritious diet and living an active life
thus, preventing obesity (Australia Institute of Health and Welfare (AIHW). (2016).
Economic stability
Economic stability has been recognized as a major determinant of health's social determinants.
There is a positive association between Income and health. Additionally, the key elements of
economic stability, including low economic status, jobs, food safety, and proper housing, are
related to health status. Employment is attributable to the health of a person as the rate of
unemployment rises, disease and premature death rise as well (Clark, & Utz, 2014).
Built environment
It is usually recognized that exercise, among other advantages, helps control weight, fights
cardiovascular disease, increases mood, and expands life expectancy. The geography of a region
is sometimes not conducive to pedestrian traffic, and security issues deter outdoor activity. There
can simply be no available space for walking, cycling or jogging public spaces. The
neighbourhoods and built environment shapes live (Koh, Piotrowski, Kumanyika, & Fielding,
2011).
Social and community support
The degree of social support may differ amongst individuals and race; for instance, a study has
shown that diabetic Hispanic people have adopted self-management approach instead of medical
visits (Strom & Egede, 2012). In the same way higher, social support corresponds with enhanced
self-management results, it has been shown that the insight of adverse or low concentrations of
social support increases the danger of fewer self-management behaviours (Strom & Egede,
2012).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Nursing 4
Figure 1: Social determinants influencing the individual’s self-management of type 2 diabetes
(AIHW, 2016).
Interventions for improving the Health of Diabetic patients
Education approach: Patient therapy education
Patient therapeutic education is a combination of educational activities that are important for the
management of diabetes, and is undertaken by health experts with an objective of helping the
patients and their families. The overall aim is to enable and equip diabetic patients to be actively
involved in their treatment and prevention of health risk factors that further complicates their
diabetic state and to improve quality of life.
Figure 1: Social determinants influencing the individual’s self-management of type 2 diabetes
(AIHW, 2016).
Interventions for improving the Health of Diabetic patients
Education approach: Patient therapy education
Patient therapeutic education is a combination of educational activities that are important for the
management of diabetes, and is undertaken by health experts with an objective of helping the
patients and their families. The overall aim is to enable and equip diabetic patients to be actively
involved in their treatment and prevention of health risk factors that further complicates their
diabetic state and to improve quality of life.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Nursing 5
Patient therapy education involves initial assessment, data collection during interviewing,
clinical evaluation of the outcomes and determination of treatment approach. Different methods
can be used to enhance educational instruments depending on the patient need such as the use of
audiovisual methods (Dorresteijn, Kriegsman, Assendelft, & Valk, 2012).
Self-management
The complexity of managing and maintaining quality of life among diabetic patients necessitates
the need for fostering self-management. Self-care is the process that involves all activities to
foster and sustain well-being in the entire life independently. The purpose of adopting self-care is
to establish a healthy lifestyle. The nature of care comprises of healing, and activities associated
with the desire to cure all life hindrances; it necessitates the need to use medication to cure or
eradicate the course of diabetes. Furthermore, the individual that assists in self-care be it a health
expert or family member, must be cognizant of nature of diabetes and its predisposing factors.
Contreras, Sanchez, Martínez, Castillo, Mindiola (2017) also observes that the individual
receiving self-care should be knowledgeable regarding diabetes, its initial history, medication
and predisposing factors, and the effect of the reformatory actions.
Another aspect of selfcare for diabetic patients is nutritional management. This is important
because it aims at influencing behavioral factors such as physical activity and diet which are
critical in the prevention and management of diabetes. An expert nutritionist discusses with the
patients the effect of food on managing diabetes, benefits of diet, health food choice and how to
handle dietary choices by adequately distributing meals on a regular basis, using picture books
with examples of meals and learning how to interpret food labels correctly (Di Onofrio, Gallé, Di
Dio, Belfiore, & Liguori, 2018).
Patient therapy education involves initial assessment, data collection during interviewing,
clinical evaluation of the outcomes and determination of treatment approach. Different methods
can be used to enhance educational instruments depending on the patient need such as the use of
audiovisual methods (Dorresteijn, Kriegsman, Assendelft, & Valk, 2012).
Self-management
The complexity of managing and maintaining quality of life among diabetic patients necessitates
the need for fostering self-management. Self-care is the process that involves all activities to
foster and sustain well-being in the entire life independently. The purpose of adopting self-care is
to establish a healthy lifestyle. The nature of care comprises of healing, and activities associated
with the desire to cure all life hindrances; it necessitates the need to use medication to cure or
eradicate the course of diabetes. Furthermore, the individual that assists in self-care be it a health
expert or family member, must be cognizant of nature of diabetes and its predisposing factors.
Contreras, Sanchez, Martínez, Castillo, Mindiola (2017) also observes that the individual
receiving self-care should be knowledgeable regarding diabetes, its initial history, medication
and predisposing factors, and the effect of the reformatory actions.
Another aspect of selfcare for diabetic patients is nutritional management. This is important
because it aims at influencing behavioral factors such as physical activity and diet which are
critical in the prevention and management of diabetes. An expert nutritionist discusses with the
patients the effect of food on managing diabetes, benefits of diet, health food choice and how to
handle dietary choices by adequately distributing meals on a regular basis, using picture books
with examples of meals and learning how to interpret food labels correctly (Di Onofrio, Gallé, Di
Dio, Belfiore, & Liguori, 2018).
Nursing 6
Family intervention
Members of the family can share accountability for managing disease by providing support in
accompanying patients to clinical visits or aiding them in the injection of insulin and offering
emotional support in helping them to cope with their illness. Family members often have an
important effect on the psychological well-being of a patient through their communications and
attitudes, their choice to adhere to treatment recommendations, and their capacity to initiate and
retain changes in diet and exercise. The inclusion of family members help establish healty
lifestyles and foster individual awareness about the risk factors for diabetes (Dinkel, Tibbits,
Hanigan, Nielsen, Jorgensen, & Grant, 2017).
Family intervention
Members of the family can share accountability for managing disease by providing support in
accompanying patients to clinical visits or aiding them in the injection of insulin and offering
emotional support in helping them to cope with their illness. Family members often have an
important effect on the psychological well-being of a patient through their communications and
attitudes, their choice to adhere to treatment recommendations, and their capacity to initiate and
retain changes in diet and exercise. The inclusion of family members help establish healty
lifestyles and foster individual awareness about the risk factors for diabetes (Dinkel, Tibbits,
Hanigan, Nielsen, Jorgensen, & Grant, 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Nursing 7
References
Australia Institute of Health and Welfare (AIHW). (2016). Chapter 4 Determinants of health.
ABS cat. no. AUS. 199. Canberra: ABS. Retrieved from
https://www.aihw.gov.au/reports/australias-health/australias-health-2016/contents/
determinants
Clark, M. L., & Utz, S. W. (2014). Social determinants of type 2 diabetes and health in the
United States. World journal of diabetes, 5(3), 296.
Contreras, F., Sanchez, M., Martínez, M. S., Castillo, M. C., & Mindiola, A. (2017).
Management and education in patients with diabetes mellitus. Med Clin Rev, 3(2), 1-7.
Dinkel, D., Tibbits, M., Hanigan, E., Nielsen, K., Jorgensen, L., & Grant, K. (2017). Healthy
Families: A Family-Based Community Intervention To Address Childhood
Obesity. Journal of community health nursing, 34(4), 190-202.
Di Onofrio, V., Gallé, F., Di Dio, M., Belfiore, P., & Liguori, G. (2018). Effects of nutrition
motivational intervention in patients affected by type 2 diabetes mellitus: a longitudinal
study in Naples, South Italy. BMC public health, 18(1), 1181.
Dorresteijn, J. A., Kriegsman, D. M., Assendelft, W. J., & Valk, G. D. (2012). Patient education
for preventing diabetic foot ulceration. Cochrane database of systematic reviews, (10).
Koh, H. K., Piotrowski, J. J., Kumanyika, S., & Fielding, J. E. (2011). Healthy people: a 2020
References
Australia Institute of Health and Welfare (AIHW). (2016). Chapter 4 Determinants of health.
ABS cat. no. AUS. 199. Canberra: ABS. Retrieved from
https://www.aihw.gov.au/reports/australias-health/australias-health-2016/contents/
determinants
Clark, M. L., & Utz, S. W. (2014). Social determinants of type 2 diabetes and health in the
United States. World journal of diabetes, 5(3), 296.
Contreras, F., Sanchez, M., Martínez, M. S., Castillo, M. C., & Mindiola, A. (2017).
Management and education in patients with diabetes mellitus. Med Clin Rev, 3(2), 1-7.
Dinkel, D., Tibbits, M., Hanigan, E., Nielsen, K., Jorgensen, L., & Grant, K. (2017). Healthy
Families: A Family-Based Community Intervention To Address Childhood
Obesity. Journal of community health nursing, 34(4), 190-202.
Di Onofrio, V., Gallé, F., Di Dio, M., Belfiore, P., & Liguori, G. (2018). Effects of nutrition
motivational intervention in patients affected by type 2 diabetes mellitus: a longitudinal
study in Naples, South Italy. BMC public health, 18(1), 1181.
Dorresteijn, J. A., Kriegsman, D. M., Assendelft, W. J., & Valk, G. D. (2012). Patient education
for preventing diabetic foot ulceration. Cochrane database of systematic reviews, (10).
Koh, H. K., Piotrowski, J. J., Kumanyika, S., & Fielding, J. E. (2011). Healthy people: a 2020
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Nursing 8
Strom, J. L., & Egede, L. E. (2012). The impact of social support on outcomes in adult
patients with type 2 diabetes: a systematic review. Current diabetes reports, 12(6), 769-
781.
Walker, R. J., Gebregziabher, M., Martin-Harris, B., & Egede, L. E. (2014). Independent effects
of socioeconomic and psychological social determinants of health on self-care and
outcomes in Type 2 diabetes. General hospital psychiatry, 36(6), 662-668.
World Health Organization. (WHO). (n.d.). The Determinants of Health. Retrieved from
https://www.who.int/hia/evidence/doh/en/
Strom, J. L., & Egede, L. E. (2012). The impact of social support on outcomes in adult
patients with type 2 diabetes: a systematic review. Current diabetes reports, 12(6), 769-
781.
Walker, R. J., Gebregziabher, M., Martin-Harris, B., & Egede, L. E. (2014). Independent effects
of socioeconomic and psychological social determinants of health on self-care and
outcomes in Type 2 diabetes. General hospital psychiatry, 36(6), 662-668.
World Health Organization. (WHO). (n.d.). The Determinants of Health. Retrieved from
https://www.who.int/hia/evidence/doh/en/
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





