Challenges of Involving Service-Users in Health Services: A Report
VerifiedAdded on 2020/10/22
|12
|3772
|432
Report
AI Summary
This report delves into the challenges of involving service users, specifically mental health patients, within health services like the NHS. It analyzes issues such as patient reluctance, prejudices, and power imbalances, drawing upon the Health and Social Care Act 2012 and various sociological perspectives. The report explores the importance of doctor-patient relationships, communication, and the role of family and friends in supporting patient involvement. It also addresses challenges faced by mental health patients, including lack of funding, support, and the impact of professionalization. The report highlights the significance of clinical commissioning groups and the need for effective decision-making processes to improve the quality of care and treatment for service users. The report is intended to help health and social care providers develop better services for their patients.
HEALTH
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TABLE OF CONTENTS
INTRODUCTION...........................................................................................................................3
MAIN BODY...................................................................................................................................3
Critically explain the sociological perspectives based on the challenges identified in involving
service users ...............................................................................................................................7
CONCLUSION..............................................................................................................................10
REFERENCES..............................................................................................................................12
INTRODUCTION...........................................................................................................................3
MAIN BODY...................................................................................................................................3
Critically explain the sociological perspectives based on the challenges identified in involving
service users ...............................................................................................................................7
CONCLUSION..............................................................................................................................10
REFERENCES..............................................................................................................................12

Question chosen is: What are the challenges of involving service-users in health services? What
sociological perspectives can help us explain those challenges?
INTRODUCTION
Maintaining the health and social care and involving the service users within a health and
social care service is a big challenge for the organisation. For a health and social care setting,
such measures are significantly important in order to develop a good connectivity with their
service users or patients. It leads to growth of quality of health care services that are been offered
the organisation. The report will analyse the challenges that are been faced by a UK based health
and social care service provider like NHS. It will help in looking after the proper management of
the health and social measures that are been carried out by the organisation in a significant
manner. The report is presented in regard to mental health patients that are the major service user
at NHS.
ANALYSIS
In a health and social care setting like NHS, the proper planning of the services and
treatment measures is very important for the organisation in order to carry out the health and
social care measures and thus will help in meeting the functions of the health and social care
enterprise. The major challenge or issue for the organisation related to their patients is that is
causes the organisation to carry out the service measures in an effective and significant manner.
As per the health and social care act, 2012, a service user for the health care form is the citizen or
patient who needs medical attention and treatment. Their involvement will include their
treatment or consultation or deciding the treatment process form them. Thus planning the
service user involvement can be a major challenge for an organization like NHS. Besides this,
the involvement can be also based for research purpose.
The patients or the service users suffering from the disease like mental ailment will look
after planning of the treatment services and facilities which will help in carrying out of services
and thus will lead to rise in quality of treatment measures of mental diseases which are offered
by health and social care service provider in a significant manner. The sense of reluctance and
prejudices that are associated with these patients related to sexuality or disability are the effective
factor that impacts the suitable planning of the treatment measures which assist in execution of
the medical support for them. As patients or customers of NHS, suffering from a mental disease
sociological perspectives can help us explain those challenges?
INTRODUCTION
Maintaining the health and social care and involving the service users within a health and
social care service is a big challenge for the organisation. For a health and social care setting,
such measures are significantly important in order to develop a good connectivity with their
service users or patients. It leads to growth of quality of health care services that are been offered
the organisation. The report will analyse the challenges that are been faced by a UK based health
and social care service provider like NHS. It will help in looking after the proper management of
the health and social measures that are been carried out by the organisation in a significant
manner. The report is presented in regard to mental health patients that are the major service user
at NHS.
ANALYSIS
In a health and social care setting like NHS, the proper planning of the services and
treatment measures is very important for the organisation in order to carry out the health and
social care measures and thus will help in meeting the functions of the health and social care
enterprise. The major challenge or issue for the organisation related to their patients is that is
causes the organisation to carry out the service measures in an effective and significant manner.
As per the health and social care act, 2012, a service user for the health care form is the citizen or
patient who needs medical attention and treatment. Their involvement will include their
treatment or consultation or deciding the treatment process form them. Thus planning the
service user involvement can be a major challenge for an organization like NHS. Besides this,
the involvement can be also based for research purpose.
The patients or the service users suffering from the disease like mental ailment will look
after planning of the treatment services and facilities which will help in carrying out of services
and thus will lead to rise in quality of treatment measures of mental diseases which are offered
by health and social care service provider in a significant manner. The sense of reluctance and
prejudices that are associated with these patients related to sexuality or disability are the effective
factor that impacts the suitable planning of the treatment measures which assist in execution of
the medical support for them. As patients or customers of NHS, suffering from a mental disease
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
will be in need of specialised care, the organisation will look after the proper gathering and
evaluation of the treatment measures which are been carried out by the organisation.
However, these patients tend and prefer to be relatively adamant and to be aloof from any
sort of interaction due to physical, emotional, psychological or sociological factors such as age,
gender and ethics influence their involvement in the decision making and developing proper
services for them will be a major challenge for NHS (Shubber and et.al., 2016). As per various
statistics Thomas and et.al., (2016), every 4th person in UK is diagnosed with effective form of
one of the other mental disease. Thus, in this case their proper involvement and planning of the
service user interaction is very important. Handling such patients is a big challenge for the
organisation as they are not prone to much interaction and are reluctant towards any sort of
voluntary interaction or involvement for a medical service providing. Thus, it will lead to rise in
the carrying out of the effective health and social care measures by the organisation (Naslund
and et.al., 2016). As the number of mental cases is relatively high, proper and effective measures
are required to be observed by health and social care service providers. They will see through the
proper planning of the health care measures and hence enhances the quality of treatment and
medication from the service users or patients at a health and social care setting like NHS.
Other than this, developing their interaction with other patients or service users in a
health and social care setting will complex and challenging for NHS. In accordance with findings
of Shubber and et.al., (2016), the proper communication or bonding may help out to some extent,
but effective planning of the services and treatment measures will influence the performance of
the mental health care service provider and helps in ensuring a rise in carrying out of the mental
treatment facilities. That will help in proper identification of their needs and ensuring their direct
involvement as the service user within the health and social care facilities that are been
developed by the health and social care services. This helps in raising the quality of treatment
measures.
In order to get their proper involvement within the decision making, treatment measures
and following of the health care services within the organisation, the support from their doctors,
care providers, family and friends can be taken. As per the views of Naslund and et.al., (2016),
proper awareness’s can increased on the individual or social level that will help in proper rise in
the treatment measures which enhances the quality of services and thus will lead to rise in the
evaluation of the treatment measures which are been carried out by the organisation.
However, these patients tend and prefer to be relatively adamant and to be aloof from any
sort of interaction due to physical, emotional, psychological or sociological factors such as age,
gender and ethics influence their involvement in the decision making and developing proper
services for them will be a major challenge for NHS (Shubber and et.al., 2016). As per various
statistics Thomas and et.al., (2016), every 4th person in UK is diagnosed with effective form of
one of the other mental disease. Thus, in this case their proper involvement and planning of the
service user interaction is very important. Handling such patients is a big challenge for the
organisation as they are not prone to much interaction and are reluctant towards any sort of
voluntary interaction or involvement for a medical service providing. Thus, it will lead to rise in
the carrying out of the effective health and social care measures by the organisation (Naslund
and et.al., 2016). As the number of mental cases is relatively high, proper and effective measures
are required to be observed by health and social care service providers. They will see through the
proper planning of the health care measures and hence enhances the quality of treatment and
medication from the service users or patients at a health and social care setting like NHS.
Other than this, developing their interaction with other patients or service users in a
health and social care setting will complex and challenging for NHS. In accordance with findings
of Shubber and et.al., (2016), the proper communication or bonding may help out to some extent,
but effective planning of the services and treatment measures will influence the performance of
the mental health care service provider and helps in ensuring a rise in carrying out of the mental
treatment facilities. That will help in proper identification of their needs and ensuring their direct
involvement as the service user within the health and social care facilities that are been
developed by the health and social care services. This helps in raising the quality of treatment
measures.
In order to get their proper involvement within the decision making, treatment measures
and following of the health care services within the organisation, the support from their doctors,
care providers, family and friends can be taken. As per the views of Naslund and et.al., (2016),
proper awareness’s can increased on the individual or social level that will help in proper rise in
the treatment measures which enhances the quality of services and thus will lead to rise in the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
involvement of service users suffering from any mental health issue at NHS. It also supports in
identifying their needs and health care requirements and take suitable measures as per feasibility.
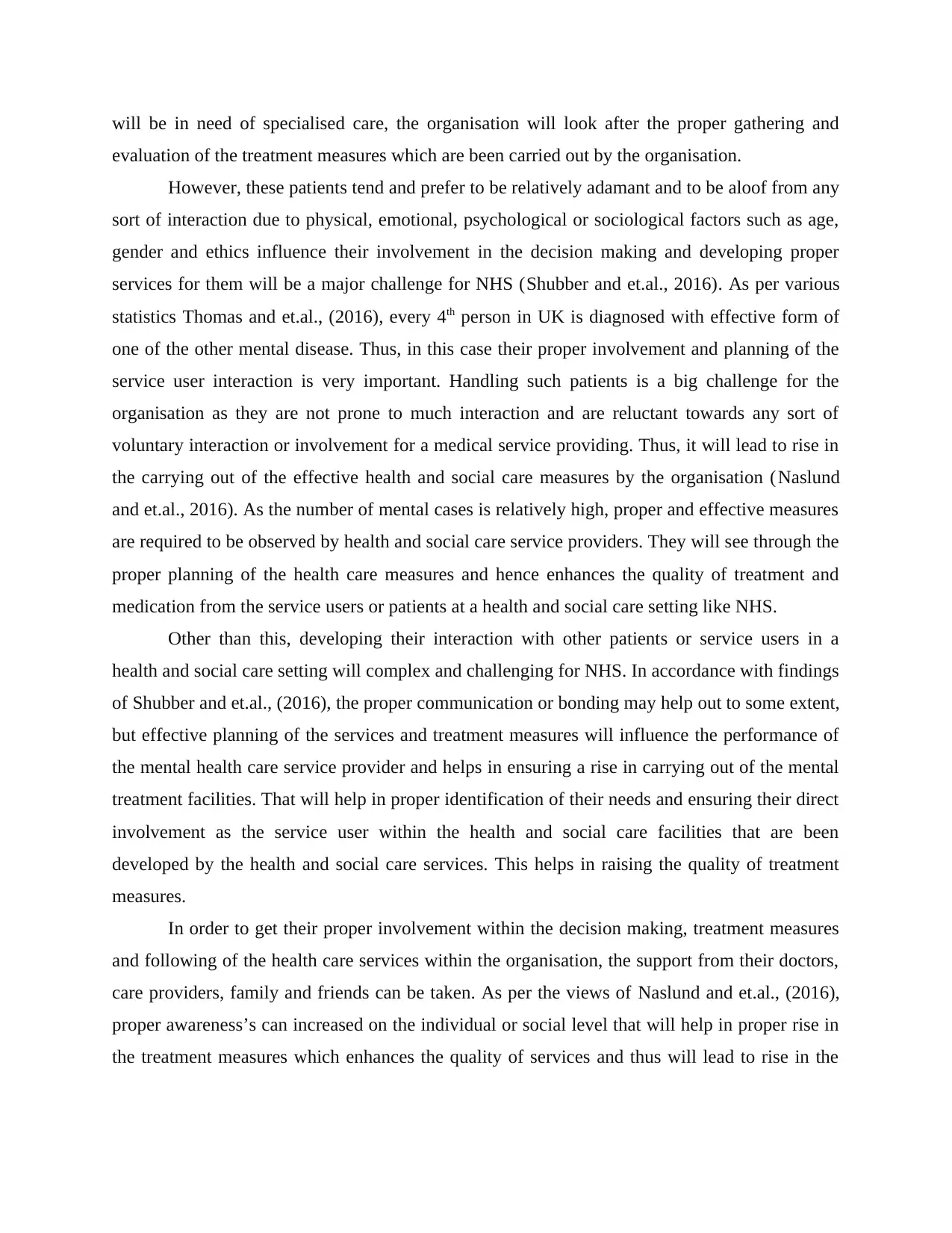
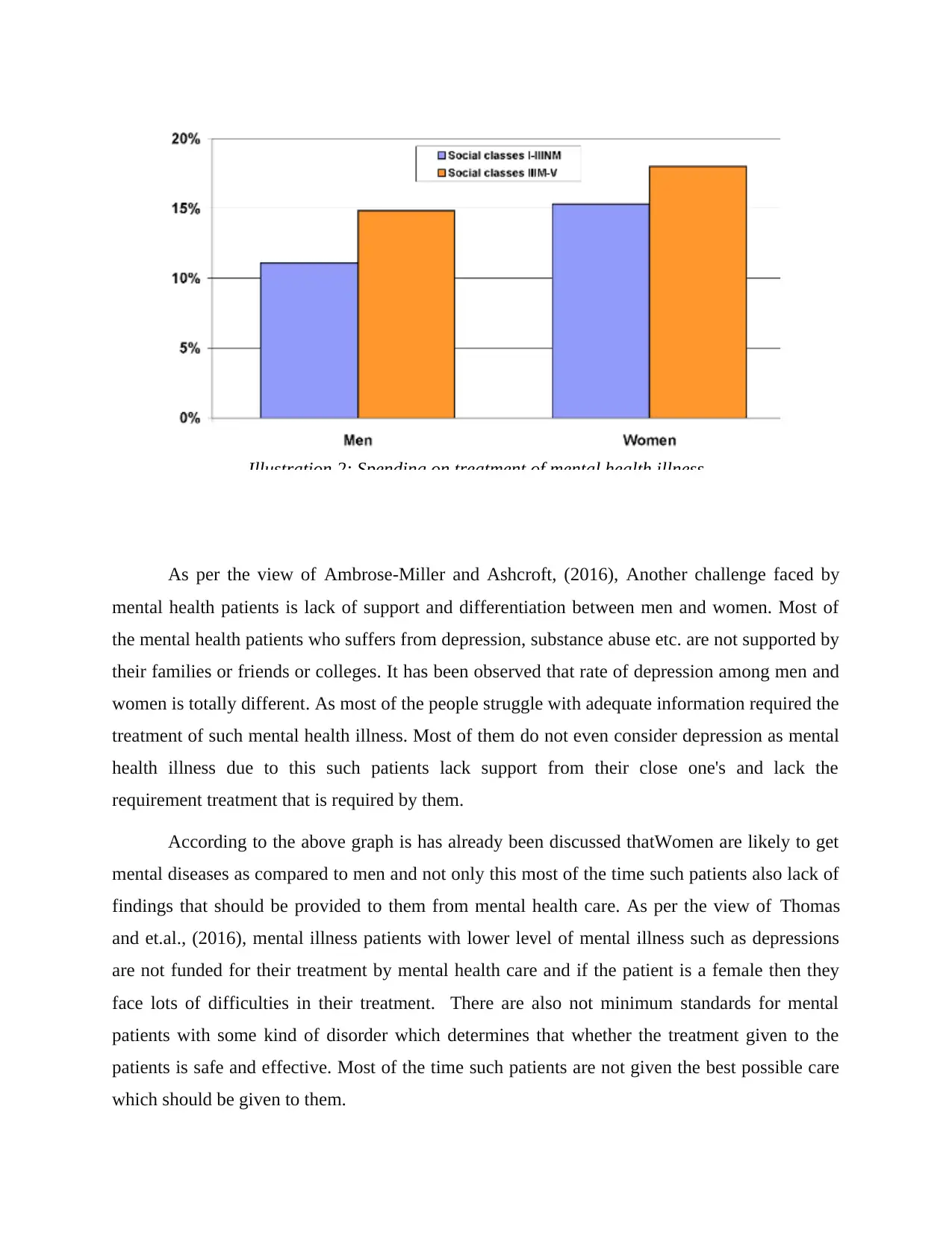
According to a survey conducted by Economies of mental health (2019), Mental health is
one of the major concern in many countries. One out of five people surfers from mental illness
and it is mostly seen in working individuals.
One of the major challenge is faced by lower income individuals, as per the view of Economies
of mental health (2019), Due to the lower income of individuals they spend less on their mental
illness treatment as compared to individual with higher incomes.
Ill
ustration 1: Mental illness in patients fashionable several
countries.
(Source: Economies of mental health. 2019)
identifying their needs and health care requirements and take suitable measures as per feasibility.
According to a survey conducted by Economies of mental health (2019), Mental health is
one of the major concern in many countries. One out of five people surfers from mental illness
and it is mostly seen in working individuals.
One of the major challenge is faced by lower income individuals, as per the view of Economies
of mental health (2019), Due to the lower income of individuals they spend less on their mental
illness treatment as compared to individual with higher incomes.
Ill
ustration 1: Mental illness in patients fashionable several
countries.
(Source: Economies of mental health. 2019)
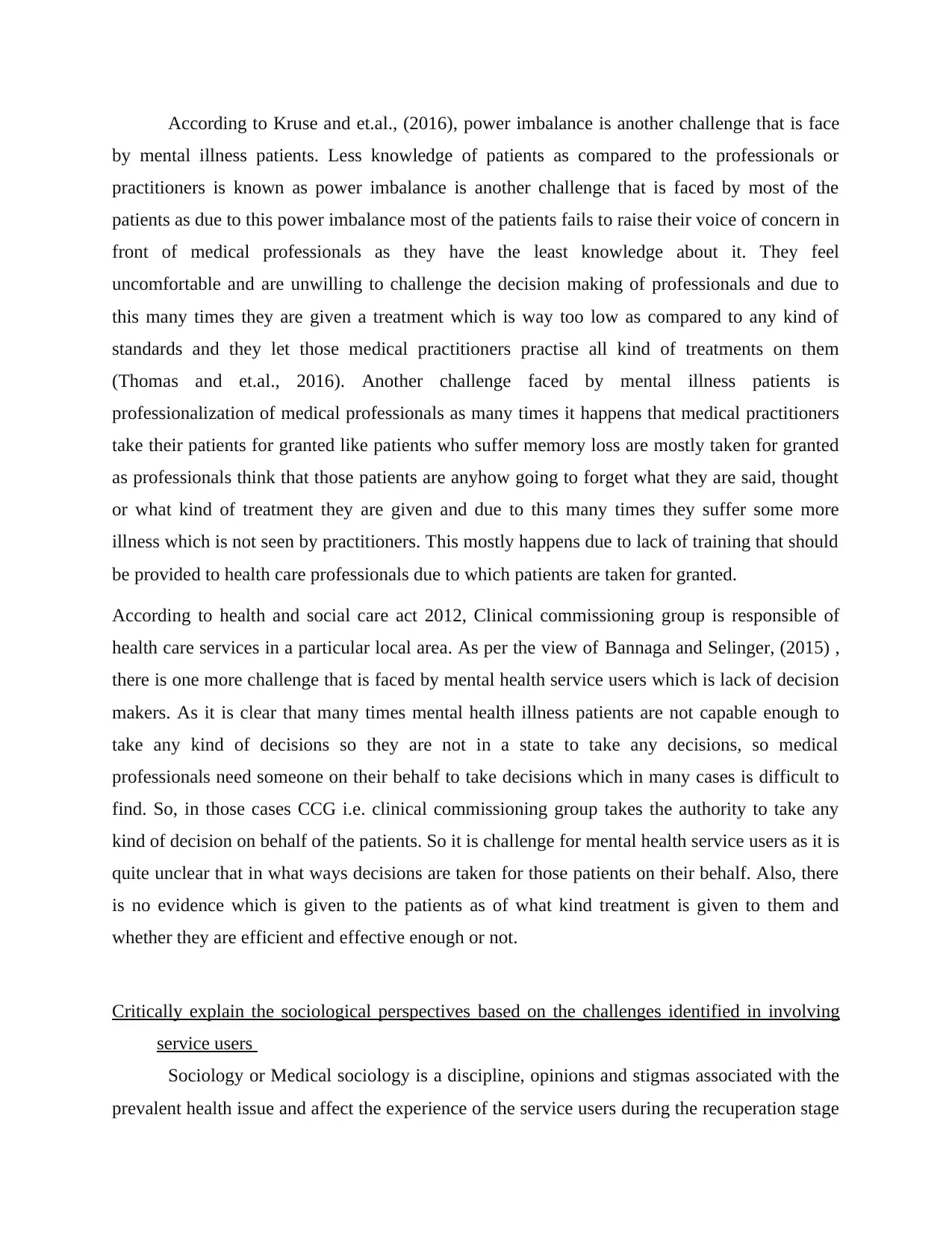
As per the view of Ambrose-Miller and Ashcroft, (2016), Another challenge faced by
mental health patients is lack of support and differentiation between men and women. Most of
the mental health patients who suffers from depression, substance abuse etc. are not supported by
their families or friends or colleges. It has been observed that rate of depression among men and
women is totally different. As most of the people struggle with adequate information required the
treatment of such mental health illness. Most of them do not even consider depression as mental
health illness due to this such patients lack support from their close one's and lack the
requirement treatment that is required by them.
According to the above graph is has already been discussed thatWomen are likely to get
mental diseases as compared to men and not only this most of the time such patients also lack of
findings that should be provided to them from mental health care. As per the view of Thomas
and et.al., (2016), mental illness patients with lower level of mental illness such as depressions
are not funded for their treatment by mental health care and if the patient is a female then they
face lots of difficulties in their treatment. There are also not minimum standards for mental
patients with some kind of disorder which determines that whether the treatment given to the
patients is safe and effective. Most of the time such patients are not given the best possible care
which should be given to them.
Illustration 2: Spending on treatment of mental health illness
mental health patients is lack of support and differentiation between men and women. Most of
the mental health patients who suffers from depression, substance abuse etc. are not supported by
their families or friends or colleges. It has been observed that rate of depression among men and
women is totally different. As most of the people struggle with adequate information required the
treatment of such mental health illness. Most of them do not even consider depression as mental
health illness due to this such patients lack support from their close one's and lack the
requirement treatment that is required by them.
According to the above graph is has already been discussed thatWomen are likely to get
mental diseases as compared to men and not only this most of the time such patients also lack of
findings that should be provided to them from mental health care. As per the view of Thomas
and et.al., (2016), mental illness patients with lower level of mental illness such as depressions
are not funded for their treatment by mental health care and if the patient is a female then they
face lots of difficulties in their treatment. There are also not minimum standards for mental
patients with some kind of disorder which determines that whether the treatment given to the
patients is safe and effective. Most of the time such patients are not given the best possible care
which should be given to them.
Illustration 2: Spending on treatment of mental health illness
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
According to Kruse and et.al., (2016), power imbalance is another challenge that is face
by mental illness patients. Less knowledge of patients as compared to the professionals or
practitioners is known as power imbalance is another challenge that is faced by most of the
patients as due to this power imbalance most of the patients fails to raise their voice of concern in
front of medical professionals as they have the least knowledge about it. They feel
uncomfortable and are unwilling to challenge the decision making of professionals and due to
this many times they are given a treatment which is way too low as compared to any kind of
standards and they let those medical practitioners practise all kind of treatments on them
(Thomas and et.al., 2016). Another challenge faced by mental illness patients is
professionalization of medical professionals as many times it happens that medical practitioners
take their patients for granted like patients who suffer memory loss are mostly taken for granted
as professionals think that those patients are anyhow going to forget what they are said, thought
or what kind of treatment they are given and due to this many times they suffer some more
illness which is not seen by practitioners. This mostly happens due to lack of training that should
be provided to health care professionals due to which patients are taken for granted.
According to health and social care act 2012, Clinical commissioning group is responsible of
health care services in a particular local area. As per the view of Bannaga and Selinger, (2015) ,
there is one more challenge that is faced by mental health service users which is lack of decision
makers. As it is clear that many times mental health illness patients are not capable enough to
take any kind of decisions so they are not in a state to take any decisions, so medical
professionals need someone on their behalf to take decisions which in many cases is difficult to
find. So, in those cases CCG i.e. clinical commissioning group takes the authority to take any
kind of decision on behalf of the patients. So it is challenge for mental health service users as it is
quite unclear that in what ways decisions are taken for those patients on their behalf. Also, there
is no evidence which is given to the patients as of what kind treatment is given to them and
whether they are efficient and effective enough or not.
Critically explain the sociological perspectives based on the challenges identified in involving
service users
Sociology or Medical sociology is a discipline, opinions and stigmas associated with the
prevalent health issue and affect the experience of the service users during the recuperation stage
by mental illness patients. Less knowledge of patients as compared to the professionals or
practitioners is known as power imbalance is another challenge that is faced by most of the
patients as due to this power imbalance most of the patients fails to raise their voice of concern in
front of medical professionals as they have the least knowledge about it. They feel
uncomfortable and are unwilling to challenge the decision making of professionals and due to
this many times they are given a treatment which is way too low as compared to any kind of
standards and they let those medical practitioners practise all kind of treatments on them
(Thomas and et.al., 2016). Another challenge faced by mental illness patients is
professionalization of medical professionals as many times it happens that medical practitioners
take their patients for granted like patients who suffer memory loss are mostly taken for granted
as professionals think that those patients are anyhow going to forget what they are said, thought
or what kind of treatment they are given and due to this many times they suffer some more
illness which is not seen by practitioners. This mostly happens due to lack of training that should
be provided to health care professionals due to which patients are taken for granted.
According to health and social care act 2012, Clinical commissioning group is responsible of
health care services in a particular local area. As per the view of Bannaga and Selinger, (2015) ,
there is one more challenge that is faced by mental health service users which is lack of decision
makers. As it is clear that many times mental health illness patients are not capable enough to
take any kind of decisions so they are not in a state to take any decisions, so medical
professionals need someone on their behalf to take decisions which in many cases is difficult to
find. So, in those cases CCG i.e. clinical commissioning group takes the authority to take any
kind of decision on behalf of the patients. So it is challenge for mental health service users as it is
quite unclear that in what ways decisions are taken for those patients on their behalf. Also, there
is no evidence which is given to the patients as of what kind treatment is given to them and
whether they are efficient and effective enough or not.
Critically explain the sociological perspectives based on the challenges identified in involving
service users
Sociology or Medical sociology is a discipline, opinions and stigmas associated with the
prevalent health issue and affect the experience of the service users during the recuperation stage
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
(Lupton, 2017). This is an integral part in the policy making by the management of health and
social sector organizations and support the professionals in minimising the impact of challenges
in context to dealing with patients suffering from any mental health issue like dementia,
schizophrenia and more. Nevertheless, these assist in gaining insights of the shortcomings that
affect the service users during their treatment and medication parts.
Doctor-Patient Relationship: It is one of the most important factor in terms of treatment of
mental health illness patients in many ways. It is extremely important for to have a better
communication and better relationship between them For the effectiveness of the treatment.
Good doctor patient relationship in mental health illness treatment is extremely important as it
helps the doctors in collecting complete patients medical information, helps in better
achievement of therapy results as well as prevents unnecessary bitterness or legal harassment. It
is important to have a better doctor patient relationship in order to build trust so that treatment
given to patients is effective enough (Enzinger and et.al., 2015). This also helps the doctors to
understand their patients more clearly as most of the mental illness patients do not open up to
anyone till they do not have trust or faith in that person. This trust helps the doctors to connect
with their patients more clearly so that they can provide them with correct treatment so that it is
effective and efficient enough to cure patients.
If this relationship is not good then it can create various challenges for both patients and
doctors like lack of support which will increase trust issues within professionals and patients.
This can be solved by doing or conducting various activities which will help both doctors and
patients to build trust within each other.
Medical Model: This is one of the important models to understand the entire history of patients
including physical exam, complaints, tests, diagnosis, treatment and prognosis. There is a mental
illness medical model which is mostly used by professionals to understand the outward
symptoms which is mostly classified as syndrome. Thus, professionals sometimes tend to follow
prejudiced notions while treating the patients (Corrigan, 2016). Gradually, the shifts in the
behavioural changes also help them to continue with the prescribed treatment plan or make
necessary changes for better patient centred care approachability. Patients with mental health
problems face types of issues while coping with the chosen treatment plans like using drugs,
electro conclusive therapy.
social sector organizations and support the professionals in minimising the impact of challenges
in context to dealing with patients suffering from any mental health issue like dementia,
schizophrenia and more. Nevertheless, these assist in gaining insights of the shortcomings that
affect the service users during their treatment and medication parts.
Doctor-Patient Relationship: It is one of the most important factor in terms of treatment of
mental health illness patients in many ways. It is extremely important for to have a better
communication and better relationship between them For the effectiveness of the treatment.
Good doctor patient relationship in mental health illness treatment is extremely important as it
helps the doctors in collecting complete patients medical information, helps in better
achievement of therapy results as well as prevents unnecessary bitterness or legal harassment. It
is important to have a better doctor patient relationship in order to build trust so that treatment
given to patients is effective enough (Enzinger and et.al., 2015). This also helps the doctors to
understand their patients more clearly as most of the mental illness patients do not open up to
anyone till they do not have trust or faith in that person. This trust helps the doctors to connect
with their patients more clearly so that they can provide them with correct treatment so that it is
effective and efficient enough to cure patients.
If this relationship is not good then it can create various challenges for both patients and
doctors like lack of support which will increase trust issues within professionals and patients.
This can be solved by doing or conducting various activities which will help both doctors and
patients to build trust within each other.
Medical Model: This is one of the important models to understand the entire history of patients
including physical exam, complaints, tests, diagnosis, treatment and prognosis. There is a mental
illness medical model which is mostly used by professionals to understand the outward
symptoms which is mostly classified as syndrome. Thus, professionals sometimes tend to follow
prejudiced notions while treating the patients (Corrigan, 2016). Gradually, the shifts in the
behavioural changes also help them to continue with the prescribed treatment plan or make
necessary changes for better patient centred care approachability. Patients with mental health
problems face types of issues while coping with the chosen treatment plans like using drugs,
electro conclusive therapy.
Such challenging issue led to differences in opinions and create misunderstanding
between the service users and the professional working on the case. For this, transparent
communication channels must be established and is possible only when the expert physician acts
as a democratic authority figure. (Gordon,2016) He/She not only guides the users but also
address their queries for improving the greater patient involvement. This would help both the
service users and the professionals in decision making and also clear the contributing factors that
bring the communication gaps.
Medical Power: It is defined as the health care power which comes under a legal framework and
shed light on the durability and reliability factor to make decisions on the behalf of the service
user's behalf. This is basically a tool to designate a trusted individual to take all the important
decisions related to the service user regarding the complete treatment plan (Kelly, 2016). When a
service user is suffering from any mental health issue such as anxiety, bipolar disorder, dementia
etc., the person is unable to take decisions rationally and might not be in proper conditions to
take it and thus, a medical power is required.
Furthermore, the challenges mentioned above including power imbalance where the
knowledge gap between patients and professionals proved as barrier in exchanging information
and the lack of professionalism among the practitioners also impacted the sociological aspects.
These can be overcome by adopting this medical power of attorney to have clear communication
channels with the concerned authority who has got a legal say and take decisions without being
judgemental (Brazier and Cave, 2016). Moreover, this paves path of respect and dignity to treat
the mental health related patients properly and in an organised manner. This helps in giving
solutions to improve the patient centred care.
Lay Perspectives: This is the folk conceptual perspectives which emphasis on understanding the
cultural diversities or any models related to the health and illness. It highlights the suggestions
and recommendations given by the non professionals that affected the mental health patients
adversely or beneficially. Several practices and belief systems have been adopted here for
removing the impact of diseases or any other mental illness through means of non medical
aspects (Reddy and Mythri,2016). Moreover, this is also practised by the families to mitigate the
ill effects but leads to some ambiguity and unreasonable evidence. Few beliefs are sensible,
however others are unique and unconventional.
between the service users and the professional working on the case. For this, transparent
communication channels must be established and is possible only when the expert physician acts
as a democratic authority figure. (Gordon,2016) He/She not only guides the users but also
address their queries for improving the greater patient involvement. This would help both the
service users and the professionals in decision making and also clear the contributing factors that
bring the communication gaps.
Medical Power: It is defined as the health care power which comes under a legal framework and
shed light on the durability and reliability factor to make decisions on the behalf of the service
user's behalf. This is basically a tool to designate a trusted individual to take all the important
decisions related to the service user regarding the complete treatment plan (Kelly, 2016). When a
service user is suffering from any mental health issue such as anxiety, bipolar disorder, dementia
etc., the person is unable to take decisions rationally and might not be in proper conditions to
take it and thus, a medical power is required.
Furthermore, the challenges mentioned above including power imbalance where the
knowledge gap between patients and professionals proved as barrier in exchanging information
and the lack of professionalism among the practitioners also impacted the sociological aspects.
These can be overcome by adopting this medical power of attorney to have clear communication
channels with the concerned authority who has got a legal say and take decisions without being
judgemental (Brazier and Cave, 2016). Moreover, this paves path of respect and dignity to treat
the mental health related patients properly and in an organised manner. This helps in giving
solutions to improve the patient centred care.
Lay Perspectives: This is the folk conceptual perspectives which emphasis on understanding the
cultural diversities or any models related to the health and illness. It highlights the suggestions
and recommendations given by the non professionals that affected the mental health patients
adversely or beneficially. Several practices and belief systems have been adopted here for
removing the impact of diseases or any other mental illness through means of non medical
aspects (Reddy and Mythri,2016). Moreover, this is also practised by the families to mitigate the
ill effects but leads to some ambiguity and unreasonable evidence. Few beliefs are sensible,
however others are unique and unconventional.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Moreover, the challenges faced by the service users might become more difficult due to
these lay perspectives. However, the professionals must bridge this difference by understanding
and using their beliefs into their practice. This would be beneficial in treating the patients with
better accessibility. Along with, several programs must be organised to generate awareness
among the service users, their families and the practitioners (Ebadi and et.al., 2016). Such steps
would help in knowing the strengths and weaknesses of the perspectives at the societal levels in
more profound manner.
Inequalities: Health care inequalities is refereed as the disparity between individuals or one
group of people when compared to others. Herein when service users get discriminated due to
economic or socio-cultural aspects which has direct and indirect impact on the overall treatment
plan and might also influence the working practices of the practitioners. People with mental
health issues are discriminated due to their weird behavioural changes and uncertainty in attitude
with respect to the surroundings (Phelan and Link, 2015). Their entire treatment procedure is
significant in terms of giving quality and delivery of health and social care services.
This is possible only when the challenges such as partial decision making process, lack of
knowledge and skills set with lack of transparent communication are overcome through giving
equal treatment to the disabled, men, women and children. Moreover, the professionals must try
to be neutral and follow the ethical standards with proper code of conduct to fulfil the duties
systematically. They must try to be unbiased and impartial and must give equal time and
attention to all the patients.
CONCLUSION
It has been summarised that mental health problems are on an increasing levels due to
onset of digital technologies and addiction to several components. This has also described about
the challenges that has been faced by the service users when taking services regarding the
treatment plans and taking medication. They must be involved in the entire process due to better
performance of tasks through increasing an understanding about the sociological perspectives in
terms of inequalities, medical power etc.
In regard to the same, there must be adoption of few strategic planning to improve the
patient centred care by involving them in organized modes. It must be made compulsory for the
professionals to follow the principles and code of conduct under the regulatory bodies like
these lay perspectives. However, the professionals must bridge this difference by understanding
and using their beliefs into their practice. This would be beneficial in treating the patients with
better accessibility. Along with, several programs must be organised to generate awareness
among the service users, their families and the practitioners (Ebadi and et.al., 2016). Such steps
would help in knowing the strengths and weaknesses of the perspectives at the societal levels in
more profound manner.
Inequalities: Health care inequalities is refereed as the disparity between individuals or one
group of people when compared to others. Herein when service users get discriminated due to
economic or socio-cultural aspects which has direct and indirect impact on the overall treatment
plan and might also influence the working practices of the practitioners. People with mental
health issues are discriminated due to their weird behavioural changes and uncertainty in attitude
with respect to the surroundings (Phelan and Link, 2015). Their entire treatment procedure is
significant in terms of giving quality and delivery of health and social care services.
This is possible only when the challenges such as partial decision making process, lack of
knowledge and skills set with lack of transparent communication are overcome through giving
equal treatment to the disabled, men, women and children. Moreover, the professionals must try
to be neutral and follow the ethical standards with proper code of conduct to fulfil the duties
systematically. They must try to be unbiased and impartial and must give equal time and
attention to all the patients.
CONCLUSION
It has been summarised that mental health problems are on an increasing levels due to
onset of digital technologies and addiction to several components. This has also described about
the challenges that has been faced by the service users when taking services regarding the
treatment plans and taking medication. They must be involved in the entire process due to better
performance of tasks through increasing an understanding about the sociological perspectives in
terms of inequalities, medical power etc.
In regard to the same, there must be adoption of few strategic planning to improve the
patient centred care by involving them in organized modes. It must be made compulsory for the
professionals to follow the principles and code of conduct under the regulatory bodies like
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Clinical Commissioning Groups (CCG) and other such medical institutions. It would help in
maintenance of qualitative delivery of services. Along with, proper training sessions must be
conducted to make the practitioners more responsible in completing their duties. This would reap
benefits in maintaining the workplace environment and help the service users efficiently. As it
has already discussed above that it is important to build relationship between doctors and patients
so for this different kinds of activities can also be conducted in order to build relationship and
trust between doctors and patients.
maintenance of qualitative delivery of services. Along with, proper training sessions must be
conducted to make the practitioners more responsible in completing their duties. This would reap
benefits in maintaining the workplace environment and help the service users efficiently. As it
has already discussed above that it is important to build relationship between doctors and patients
so for this different kinds of activities can also be conducted in order to build relationship and
trust between doctors and patients.
REFERENCES
Books and Journals
Ambrose-Miller, W. and Ashcroft, R., 2016. Challenges faced by social workers as members of
interprofessional collaborative health care teams. Health & social work. 41(2). pp.101-
109.
Bannaga, A.S. and Selinger, C.P., 2015. Inflammatory bowel disease and anxiety: links, risks,
and challenges faced. Clinical and experimental gastroenterology. 8. p.111.
Brazier, M. and Cave, E., 2016. Medicine, patients and the law. Oxford University Press.
Corrigan, P.W., 2016. Resolving mental illness stigma: should we seek normalcy or
solidarity?. The British Journal of Psychiatry.208(4). pp.314-315.
Ebadi, S.H. and et.al., 2016. Curricular Content for Pupils' Mental Health. International
Education Studies.9(12). pp.137-147.
Enzinger, A.C., and et.al., 2015. Outcomes of prognostic disclosure: associations with
prognostic understanding, distress, and relationship with physician among patients with
advanced cancer. Journal of clinical oncology. 33(32). p.3809.
Gordon, J.S., 2016. Helping survivors of domestic violence: The effectiveness of medical, mental
health, and community services. Routledge.
Kelly, B.D., 2016. Dignity, mental health and human rights: coercion and the law. Routledge.
Kruse, C.S., and et.al., 2016. Challenges and opportunities of big data in health care: a
systematic review. JMIR medical informatics. 4(4). p.e38.
Lupton, D. ed., 2017. Self-tracking, health and medicine: Sociological perspectives. Routledge.
Naslund, J.A., and et.al., 2016. The future of mental health care: peer-to-peer support and social
media. Epidemiology and psychiatric sciences. 25(2). pp.113-122.
Phelan, J.C. and Link, B.G., 2015. Is racism a fundamental cause of inequalities in
health?. Annual Review of Sociology.41. pp.311-330.
Reddy, M.S. and Mythri, S.V., 2016. Health-care ethics and the free market value system. Indian
journal of psychological medicine.38(5). p.371.
Shubber, Z., and et.al., 2016. Patient-reported barriers to adherence to antiretroviral therapy: a
systematic review and meta-analysis. PLoS medicine. 13(11). p.e1002183.
Thomas, B.E., and et.al., 2016. Psycho-socio-economic issues challenging multidrug resistant
tuberculosis patients: a systematic review. PloS one. 11(1). p.e0147397.
Online
Economies of mental health. 2019. [Online]. Available through:
<https://wol.iza.org/articles/economics-of-mental-health/long>
Books and Journals
Ambrose-Miller, W. and Ashcroft, R., 2016. Challenges faced by social workers as members of
interprofessional collaborative health care teams. Health & social work. 41(2). pp.101-
109.
Bannaga, A.S. and Selinger, C.P., 2015. Inflammatory bowel disease and anxiety: links, risks,
and challenges faced. Clinical and experimental gastroenterology. 8. p.111.
Brazier, M. and Cave, E., 2016. Medicine, patients and the law. Oxford University Press.
Corrigan, P.W., 2016. Resolving mental illness stigma: should we seek normalcy or
solidarity?. The British Journal of Psychiatry.208(4). pp.314-315.
Ebadi, S.H. and et.al., 2016. Curricular Content for Pupils' Mental Health. International
Education Studies.9(12). pp.137-147.
Enzinger, A.C., and et.al., 2015. Outcomes of prognostic disclosure: associations with
prognostic understanding, distress, and relationship with physician among patients with
advanced cancer. Journal of clinical oncology. 33(32). p.3809.
Gordon, J.S., 2016. Helping survivors of domestic violence: The effectiveness of medical, mental
health, and community services. Routledge.
Kelly, B.D., 2016. Dignity, mental health and human rights: coercion and the law. Routledge.
Kruse, C.S., and et.al., 2016. Challenges and opportunities of big data in health care: a
systematic review. JMIR medical informatics. 4(4). p.e38.
Lupton, D. ed., 2017. Self-tracking, health and medicine: Sociological perspectives. Routledge.
Naslund, J.A., and et.al., 2016. The future of mental health care: peer-to-peer support and social
media. Epidemiology and psychiatric sciences. 25(2). pp.113-122.
Phelan, J.C. and Link, B.G., 2015. Is racism a fundamental cause of inequalities in
health?. Annual Review of Sociology.41. pp.311-330.
Reddy, M.S. and Mythri, S.V., 2016. Health-care ethics and the free market value system. Indian
journal of psychological medicine.38(5). p.371.
Shubber, Z., and et.al., 2016. Patient-reported barriers to adherence to antiretroviral therapy: a
systematic review and meta-analysis. PLoS medicine. 13(11). p.e1002183.
Thomas, B.E., and et.al., 2016. Psycho-socio-economic issues challenging multidrug resistant
tuberculosis patients: a systematic review. PloS one. 11(1). p.e0147397.
Online
Economies of mental health. 2019. [Online]. Available through:
<https://wol.iza.org/articles/economics-of-mental-health/long>
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





