Detailed Report on Nursing Care Plan for Status Asthmaticus
VerifiedAdded on 2024/04/25
|8
|1322
|407
Report
AI Summary
This report details a nursing care plan for a patient presenting with status asthmaticus, a severe asthma exacerbation. It covers the patient's presentation, underlying pathophysiology, clinical manifestations such as tachypnea, wheezing and cyanosis, and relevant laboratory findings. The report outlines nursing diagnoses including impaired gas exchange and ineffective airway clearance, and sets goals focused on establishing airway patency, assisting with breathing, and improving nutritional intake. It details nursing interventions such as oxygen therapy, bronchodilator administration, fluid management, and monitoring. A reflective report discusses the use of pulse oximetry for assessing oxygen saturation, highlighting its advantages and limitations. The report concludes with a list of references.
Contents
PART 1...............................................................................................................................................3
Information / Presentation and Interpretation.................................................................................3
Pathophysiology................................................................................................................................3
Clinical Manifestations......................................................................................................................4
Laboratory findings............................................................................................................................5
Decision / Diagnosis...........................................................................................................................5
Nursing goals.....................................................................................................................................5
Nursing Care Plan and management.................................................................................................6
PART 2 - Reflective report..................................................................................................................7
REFERENCES......................................................................................................................................8
1
PART 1...............................................................................................................................................3
Information / Presentation and Interpretation.................................................................................3
Pathophysiology................................................................................................................................3
Clinical Manifestations......................................................................................................................4
Laboratory findings............................................................................................................................5
Decision / Diagnosis...........................................................................................................................5
Nursing goals.....................................................................................................................................5
Nursing Care Plan and management.................................................................................................6
PART 2 - Reflective report..................................................................................................................7
REFERENCES......................................................................................................................................8
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PART 1
Information / Presentation and Interpretation
As per the given case scenario, the presented symptoms indicate Status Asthmaticus. Status
asthmaticus is the term used to describe the severe attack of asthma which requires prompt
medical intervention. As patient has a history of asthma and now the symptoms do not
react to conventional medical therapy. These attacks are usually un-warned and sudden. It
causes hypoxia and low ventilation and decrease in bronchial diameter. This condition is
often due to increased exposure to precipitating agents like dust, exercise, pollutants and
allergens (Mutlu et al, 2002).
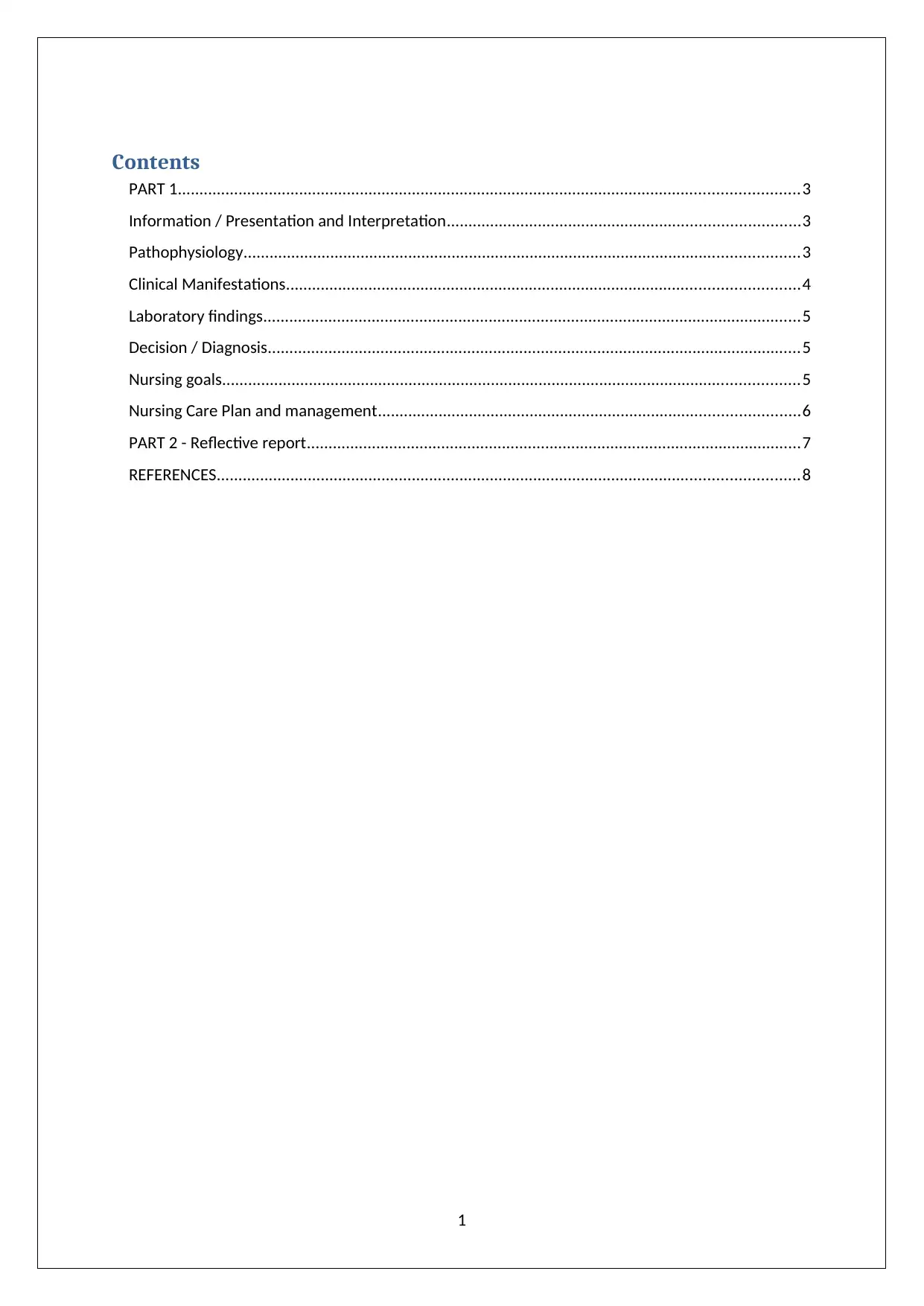
Pathophysiology
Status asthmaticus can occur suddenly or in response to the trigger. In given case scenario is
evident that cessation of use of preventer and continuous exposure to dust and allergens
triggered the condition of the patient (Afessa, Morales & Cury, 2001). Pathology progresses
by narrowing the airway causing inflammation and obstructive secretion. Triggers cause
inflammation and thickening of smooth muscles that leads to airway hyper-responsiveness.
This leads to hyper-secretion of mucus and adds to bronchospasm and asthma.
2
Information / Presentation and Interpretation
As per the given case scenario, the presented symptoms indicate Status Asthmaticus. Status
asthmaticus is the term used to describe the severe attack of asthma which requires prompt
medical intervention. As patient has a history of asthma and now the symptoms do not
react to conventional medical therapy. These attacks are usually un-warned and sudden. It
causes hypoxia and low ventilation and decrease in bronchial diameter. This condition is
often due to increased exposure to precipitating agents like dust, exercise, pollutants and
allergens (Mutlu et al, 2002).
Pathophysiology
Status asthmaticus can occur suddenly or in response to the trigger. In given case scenario is
evident that cessation of use of preventer and continuous exposure to dust and allergens
triggered the condition of the patient (Afessa, Morales & Cury, 2001). Pathology progresses
by narrowing the airway causing inflammation and obstructive secretion. Triggers cause
inflammation and thickening of smooth muscles that leads to airway hyper-responsiveness.
This leads to hyper-secretion of mucus and adds to bronchospasm and asthma.
2
(online source- https://clinicalgate.com/acute-parenchymal-disease-in-pediatric-patients/ ).
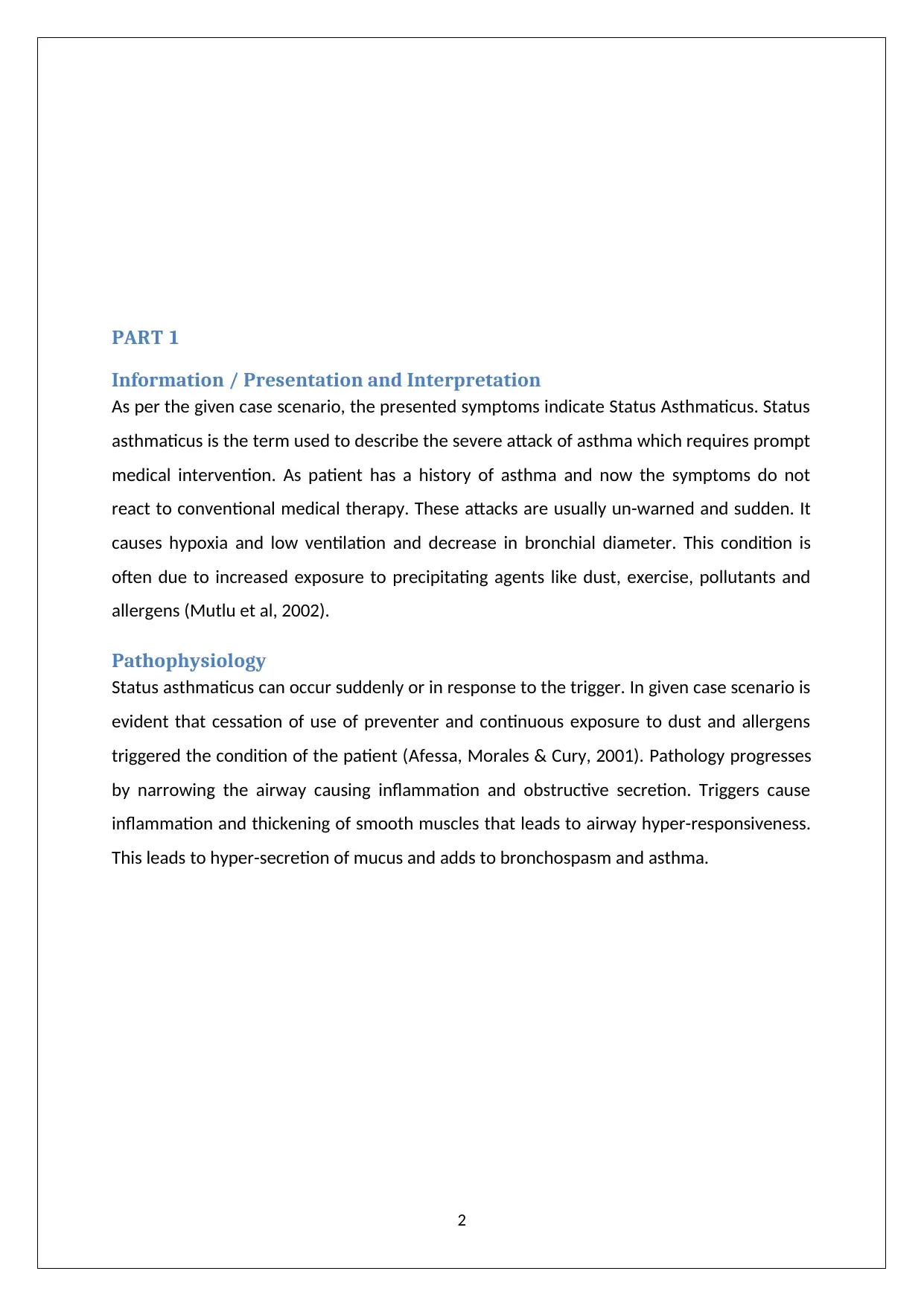
Clinical Manifestations
Symptoms presented by patient resemble that of status asthmaticus and usually are same
as symptoms of asthma but have a greater and severe face.
Tachypnea, (increased respiratory rate) with increased efforts of expiration.
Diminished breath sound, difficulty in speaking full sentences and talking in phrases.
Impaired mental function, anxiety, fatigue.
Continuous coughing
Tightness in chest
Cyanosis of lips
Wheezing
3
Clinical Manifestations
Symptoms presented by patient resemble that of status asthmaticus and usually are same
as symptoms of asthma but have a greater and severe face.
Tachypnea, (increased respiratory rate) with increased efforts of expiration.
Diminished breath sound, difficulty in speaking full sentences and talking in phrases.
Impaired mental function, anxiety, fatigue.
Continuous coughing
Tightness in chest
Cyanosis of lips
Wheezing
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
(online source- http://pendidikanpesakit.myhealth.gov.my/en/doctors-diagnose-
asthma ).
Laboratory findings
Primary pulmonary function test evaluates the lung volume and diffusing capacity of lungs.
Blood tests are indicated for ruling out allergens or medications which can induce status
asthmaticus, respiratory alkalosis is common finding as increased respiration increased the
blood pH.
Arterial blood gas test indicates increased pCO2 in the blood caused by increased
respiration is seen which is a medical alert and indicates respiratory failure (Houston, De
Navasquez & Trounce, 1953).
4
asthma ).
Laboratory findings
Primary pulmonary function test evaluates the lung volume and diffusing capacity of lungs.
Blood tests are indicated for ruling out allergens or medications which can induce status
asthmaticus, respiratory alkalosis is common finding as increased respiration increased the
blood pH.
Arterial blood gas test indicates increased pCO2 in the blood caused by increased
respiration is seen which is a medical alert and indicates respiratory failure (Houston, De
Navasquez & Trounce, 1953).
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Decision / Diagnosis
Nursing diagnosis according to presented case can be given as following-
Impaired gas exchange
Infective airway clearance
Imbalanced nutrition
Nursing goals
Establish airway patency- this will help patient to breath properly and manage
respiratory balance.
Grant assistance with breathing- helping patient to breath with supplemental
breathing assistance will aid in the process of respiration.
Increase nutritional intake- proper nutrition will encourage hydration to body.
Try to reduce the progression of disease- administration of proper treatment and
environment for recovery and control of disease.
Educate patient about disease symptoms and treatment- patient should be educated
and informed about the symptoms and attacks and what to do while experiencing it,
this will help patient to know what to be done while experiencing an attack and how
to recover from it.
Nursing Care Plan and management
Monitoring the patient for first 12- 24 hrs. is very crucial in nursing intervention.
5
Nursing diagnosis according to presented case can be given as following-
Impaired gas exchange
Infective airway clearance
Imbalanced nutrition
Nursing goals
Establish airway patency- this will help patient to breath properly and manage
respiratory balance.
Grant assistance with breathing- helping patient to breath with supplemental
breathing assistance will aid in the process of respiration.
Increase nutritional intake- proper nutrition will encourage hydration to body.
Try to reduce the progression of disease- administration of proper treatment and
environment for recovery and control of disease.
Educate patient about disease symptoms and treatment- patient should be educated
and informed about the symptoms and attacks and what to do while experiencing it,
this will help patient to know what to be done while experiencing an attack and how
to recover from it.
Nursing Care Plan and management
Monitoring the patient for first 12- 24 hrs. is very crucial in nursing intervention.
5
Monitor oxygen saturation and respiratory rate continuously by recording BP and
ECG
Initially administer supplemental oxygen therapy to ease patient in breathing.
Administration of b- antagonist bronchodilators such as levalbuterol or albuterol and
sedatives (IV).
Assess patient for signs of dehydration and fluid therapy is indicated to rehydrate
the patient.
Corticosteroids are administered to clear the airway and ease of symptoms.
Magnesium sulphate is administered for smooth muscle relaxation to ease
breathing.
To correct respiratory acidosis and hypoxemia anticholinergic agents are prescribed.
In case of bronchial mucus assist the patient for mucus expectoration by performing
chest physiotherapy and use of mucolytic drugs (Corbridge & HAll, 1995).
If required secretions are to be removed by suctioning or bronchoscopy is indicated.
According to test and X-ray diagnosis administer any antibiotics if prescribed for any
respiratory infection.
Assist the patient in any activity he is doing and advise patient to conserve his energy
as much possible.
During the attack try to calm the patient act slow and responsive and help in
reducing their anxiety also stay with the patient during the attack goes on and till it
subsides.
Make sure patient is away from any allergens like flowers, pollens, dust etc.
PART 2 - Reflective report
6
ECG
Initially administer supplemental oxygen therapy to ease patient in breathing.
Administration of b- antagonist bronchodilators such as levalbuterol or albuterol and
sedatives (IV).
Assess patient for signs of dehydration and fluid therapy is indicated to rehydrate
the patient.
Corticosteroids are administered to clear the airway and ease of symptoms.
Magnesium sulphate is administered for smooth muscle relaxation to ease
breathing.
To correct respiratory acidosis and hypoxemia anticholinergic agents are prescribed.
In case of bronchial mucus assist the patient for mucus expectoration by performing
chest physiotherapy and use of mucolytic drugs (Corbridge & HAll, 1995).
If required secretions are to be removed by suctioning or bronchoscopy is indicated.
According to test and X-ray diagnosis administer any antibiotics if prescribed for any
respiratory infection.
Assist the patient in any activity he is doing and advise patient to conserve his energy
as much possible.
During the attack try to calm the patient act slow and responsive and help in
reducing their anxiety also stay with the patient during the attack goes on and till it
subsides.
Make sure patient is away from any allergens like flowers, pollens, dust etc.
PART 2 - Reflective report
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

In a patient presented with Status Asthmaticus to assess the oxygen saturation I used pulse
oximetre. It is a non-invasive method to monitor patient's oxygen saturation in blood. As
patient had symptoms of asthma in exaggerated version which indicates sudden
asthmaticus attack so the saturation of oxygen and carbon dioxide in blood is to be
monitored. For this purpose inexpensive and fast method according to me was using a pulse
oximetre. The device is used by placing on fingertip and device passes two wavelengths
which are absorbed by arterial blood and gives the reading of saturation of oxygen in
arterial blood leaving venous blood (Kianl et al, 2003).
Advantages- Oximetry is a convenient procedure which is applicable in any setting from
intensive care to operable settings. Usage of oximetre is very easy and essential for an
emergency scenario. I used this method for its efficacy in emergency use and rapid results.
Limitations- this is not very effective and sole method to be used to monitor respiratory
capacity and sufficiency because it measures oxygen saturation in blood but does not
monitor ventilation and is incomplete for measuring respiratory sufficiency. Blood gas test in
laboratory gives the complete idea of carbon dioxide levels but oximetre does not measure
CO2 level which indicates that it is not a substitute for laboratory tests. (DeMeulenaere,
2007).
7
oximetre. It is a non-invasive method to monitor patient's oxygen saturation in blood. As
patient had symptoms of asthma in exaggerated version which indicates sudden
asthmaticus attack so the saturation of oxygen and carbon dioxide in blood is to be
monitored. For this purpose inexpensive and fast method according to me was using a pulse
oximetre. The device is used by placing on fingertip and device passes two wavelengths
which are absorbed by arterial blood and gives the reading of saturation of oxygen in
arterial blood leaving venous blood (Kianl et al, 2003).
Advantages- Oximetry is a convenient procedure which is applicable in any setting from
intensive care to operable settings. Usage of oximetre is very easy and essential for an
emergency scenario. I used this method for its efficacy in emergency use and rapid results.
Limitations- this is not very effective and sole method to be used to monitor respiratory
capacity and sufficiency because it measures oxygen saturation in blood but does not
monitor ventilation and is incomplete for measuring respiratory sufficiency. Blood gas test in
laboratory gives the complete idea of carbon dioxide levels but oximetre does not measure
CO2 level which indicates that it is not a substitute for laboratory tests. (DeMeulenaere,
2007).
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
1. Afessa, B., Morales, I., & Cury, J. D. (2001). Clinical course and outcome of patients
admitted to an ICU for status asthmaticus. CHEST Journal, 120(5), 1616-1621.
2. Corbridge, T. C., & HAll, J. B. (1995). The assessment and management of adults with
status asthmaticus. American journal of respiratory and critical care medicine,
151(5), 1296-1316.
3. DeMeulenaere, S. (2007). Pulse oximetry: uses and limitations. The Journal for Nurse
Practitioners, 3(5), 312-317.
4. Houston, J. C., De Navasquez, S., & Trounce, J. R. (1953). A clinical and pathological
study of fatal cases of status asthmaticus. Thorax, 8(3), 207.
5. Kianl, M. E., Al-Ali, A., Carothers, D., Lee, M., Pishney, J., & Weber, W. M. (2003). U.S.
Patent No. 6,658,276. Washington, DC: U.S. Patent and Trademark Office.
6. Mutlu, G. M., Factor, P., Schwartz, D. E., & Sznajder, J. I. (2002). Severe status
asthmaticus: management with permissive hypercapnia and inhalation anesthesia.
Critical care medicine, 30(2), 477-480.
8
1. Afessa, B., Morales, I., & Cury, J. D. (2001). Clinical course and outcome of patients
admitted to an ICU for status asthmaticus. CHEST Journal, 120(5), 1616-1621.
2. Corbridge, T. C., & HAll, J. B. (1995). The assessment and management of adults with
status asthmaticus. American journal of respiratory and critical care medicine,
151(5), 1296-1316.
3. DeMeulenaere, S. (2007). Pulse oximetry: uses and limitations. The Journal for Nurse
Practitioners, 3(5), 312-317.
4. Houston, J. C., De Navasquez, S., & Trounce, J. R. (1953). A clinical and pathological
study of fatal cases of status asthmaticus. Thorax, 8(3), 207.
5. Kianl, M. E., Al-Ali, A., Carothers, D., Lee, M., Pishney, J., & Weber, W. M. (2003). U.S.
Patent No. 6,658,276. Washington, DC: U.S. Patent and Trademark Office.
6. Mutlu, G. M., Factor, P., Schwartz, D. E., & Sznajder, J. I. (2002). Severe status
asthmaticus: management with permissive hypercapnia and inhalation anesthesia.
Critical care medicine, 30(2), 477-480.
8
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





