NUR2300: Infection Control Report on Sterile vs Normal Gloves
VerifiedAdded on 2022/11/10
|27
|4990
|74
Report
AI Summary
This report, prepared for a nursing practice course (NUR2300), investigates the effectiveness of sterile gloves compared to normal gloves in reducing the risk of infection during wound care. The assignment utilizes the PICO format to formulate a research question and includes a comprehensive search strategy using the CINAHL database. The report synthesizes findings from multiple research articles, including systematic reviews and randomized controlled trials, to evaluate the evidence. Key findings suggest that the use of sterile gloves does not necessarily lead to a lower incidence of infection compared to non-sterile gloves. The report also includes a critical appraisal of a systematic review using the JBI checklist, assessing its methodological rigor and validity. The conclusion highlights the highest level of evidence, the study's limitations, and the implications for nursing practice. The report provides detailed justifications for the chosen evidence, synthesis of the findings, and critical appraisal of the selected research articles.

Running head: NURSING
NUR2300 Evidence Based Nursing Practice
Name of the Student
Name of the University
Author Note
NUR2300 Evidence Based Nursing Practice
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING
Table of Contents
PART 1.......................................................................................................................................2
Summary................................................................................................................................2
Rationale................................................................................................................................2
Search strategy.......................................................................................................................3
Articles identified...................................................................................................................3
Justification............................................................................................................................4
PART 2.......................................................................................................................................5
Synthesis................................................................................................................................5
Highest evidence....................................................................................................................6
Critical appraisal tool.............................................................................................................6
Critical appraisal....................................................................................................................7
References................................................................................................................................11
Appendix..................................................................................................................................14
Search history.......................................................................................................................14
Links to five best evidences.................................................................................................16
Summary table.......................................................................................................................0
JBI critical appraisal checklist...............................................................................................0
Table of Contents
PART 1.......................................................................................................................................2
Summary................................................................................................................................2
Rationale................................................................................................................................2
Search strategy.......................................................................................................................3
Articles identified...................................................................................................................3
Justification............................................................................................................................4
PART 2.......................................................................................................................................5
Synthesis................................................................................................................................5
Highest evidence....................................................................................................................6
Critical appraisal tool.............................................................................................................6
Critical appraisal....................................................................................................................7
References................................................................................................................................11
Appendix..................................................................................................................................14
Search history.......................................................................................................................14
Links to five best evidences.................................................................................................16
Summary table.......................................................................................................................0
JBI critical appraisal checklist...............................................................................................0
2NURSING
PART 1
Infection control refers to the discipline that is associated with prevention of
healthcare-associated or nosocomial infection, and forms an essential and under-recognised
component of health and social care. In addition, infection control also addresses several
factors that are associated to the transmission of infection within healthcare setting, from
patient to patient, from staff to patient, from patient to staff, or amid staff (Kuhar, Pollock,
Yokoe, Howell & Chopra, 2018). Infection control also encompasses prevention,
investigation or monitoring and effective management of outbreaks of infection. Hence, the
major problem that will be addressed in this assignment is control of infection among people
who are being care for wound management.
Summary
The clinical practice of infection control comprises of several aspects such as, hand
hygiene, sterilization, and cleaning, personal protective equipment (PPE), disinfection, and
antimicrobial surfaces. PPE refers to the specialized clothing or apparatus that is worn by a
healthcare employee for defence against vulnerability to infection (Andersen, 2019). The
hazard of infection control that occurs in a healthcare setting is generally triggered by
exposure of the patients and/or healthcare staff to saliva, blood, aerosols, or other bodily
fluids that have the probability of carrying infectious pathogen, thus leading to the onset
HIV, Hepatitis C, or other pathogen that are either blood borne or bodily fluid borne
(Chowdhary, Voss & Meis, 2016).
Rationale
PPE generally prevents direct contact with a possibly infectious agent and this is
typically accomplished by the formation of a physical barrier at the interface between the
healthcare worker and the infectious agent. Some of the most commonly used PPE include
PART 1
Infection control refers to the discipline that is associated with prevention of
healthcare-associated or nosocomial infection, and forms an essential and under-recognised
component of health and social care. In addition, infection control also addresses several
factors that are associated to the transmission of infection within healthcare setting, from
patient to patient, from staff to patient, from patient to staff, or amid staff (Kuhar, Pollock,
Yokoe, Howell & Chopra, 2018). Infection control also encompasses prevention,
investigation or monitoring and effective management of outbreaks of infection. Hence, the
major problem that will be addressed in this assignment is control of infection among people
who are being care for wound management.
Summary
The clinical practice of infection control comprises of several aspects such as, hand
hygiene, sterilization, and cleaning, personal protective equipment (PPE), disinfection, and
antimicrobial surfaces. PPE refers to the specialized clothing or apparatus that is worn by a
healthcare employee for defence against vulnerability to infection (Andersen, 2019). The
hazard of infection control that occurs in a healthcare setting is generally triggered by
exposure of the patients and/or healthcare staff to saliva, blood, aerosols, or other bodily
fluids that have the probability of carrying infectious pathogen, thus leading to the onset
HIV, Hepatitis C, or other pathogen that are either blood borne or bodily fluid borne
(Chowdhary, Voss & Meis, 2016).
Rationale
PPE generally prevents direct contact with a possibly infectious agent and this is
typically accomplished by the formation of a physical barrier at the interface between the
healthcare worker and the infectious agent. Some of the most commonly used PPE include
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
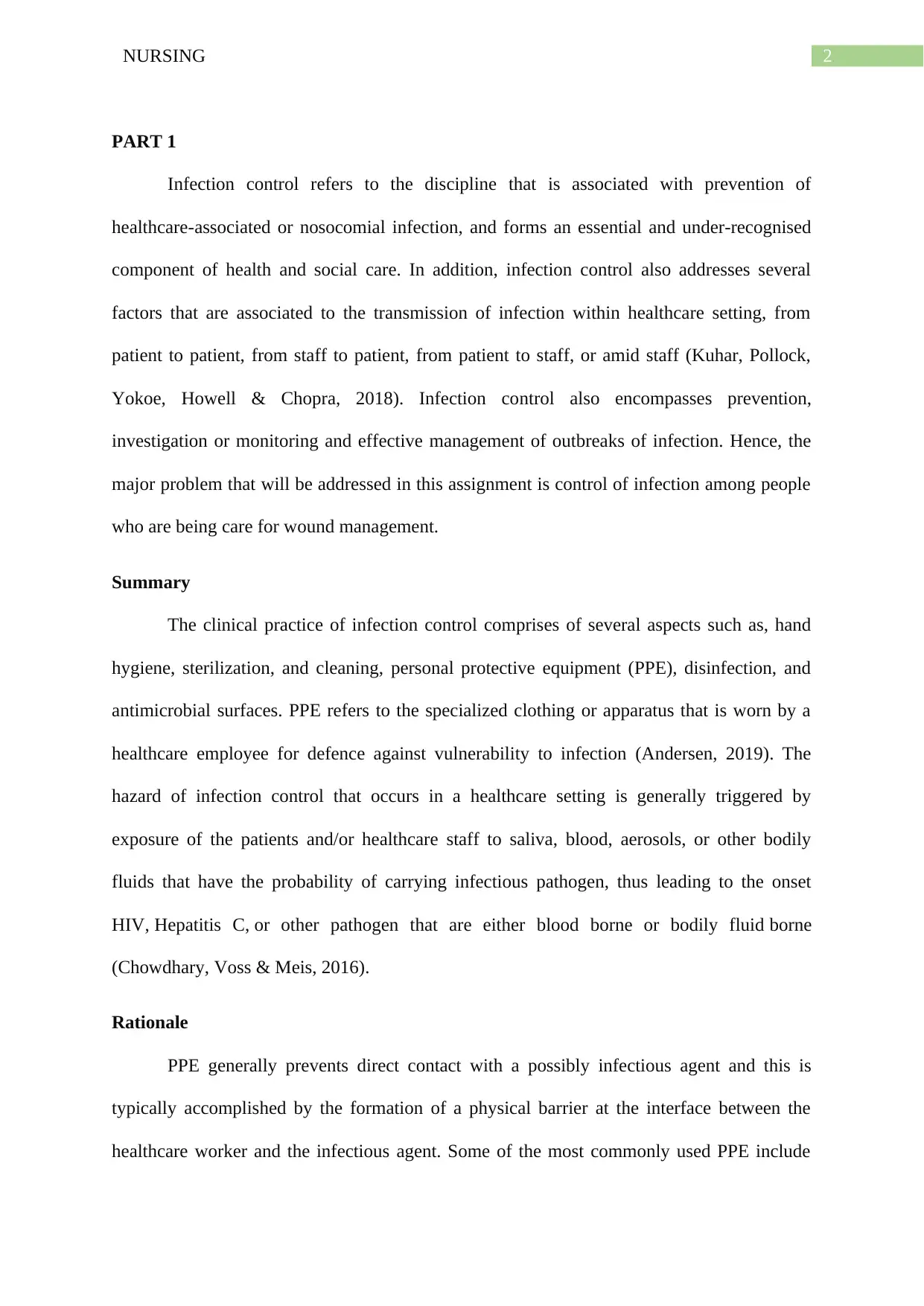
3NURSING
gowns, gloves, shoe covers, bonnets, CPR masks, face shields, surgical masks, goggles, and
respirators (Shrestha, Khouli, Bajracharya, House & Mugele, 2019). Research evidences
highlight the role of sterilisation as an effective method for preventing the transmission of
bacteria to and from patients, and recommend implementation of the process of cleaning
gloves or medical equipment, which come in contact with body fluids and bloodstream
(Gleser, Schwab, Solbach & Vonberg, 2018). This calls for the need of exploring the efficacy
of sterilised gloves, in comparison to normal gloves, in infection control. With the aim of
addressing the clinical practice of infection control, the PICO format was used for
development of the research question that is given below.
What is the effectiveness of using sterile gloves, in comparison to normal gloves
during wound care, for reducing risk of infection?
P (population) patients who need a wound care
I (intervention) sterile gloves
C (comparison) normal gloves
O (outcome) reduce the risk of infection
Search strategy
The search strategy that had been adopted for CINAHL database has been given in
appendix.
Articles identified
1. Brewer, J. D., Gonzalez, A. B., Baum, C. L., Arpey, C. J., Roenigk, R. K., Otley, C.
C., & Erwin, P. J. (2016). Comparison of sterile vs nonsterile gloves in cutaneous
surgery and common outpatient dental procedures: a systematic review and meta-
gowns, gloves, shoe covers, bonnets, CPR masks, face shields, surgical masks, goggles, and
respirators (Shrestha, Khouli, Bajracharya, House & Mugele, 2019). Research evidences
highlight the role of sterilisation as an effective method for preventing the transmission of
bacteria to and from patients, and recommend implementation of the process of cleaning
gloves or medical equipment, which come in contact with body fluids and bloodstream
(Gleser, Schwab, Solbach & Vonberg, 2018). This calls for the need of exploring the efficacy
of sterilised gloves, in comparison to normal gloves, in infection control. With the aim of
addressing the clinical practice of infection control, the PICO format was used for
development of the research question that is given below.
What is the effectiveness of using sterile gloves, in comparison to normal gloves
during wound care, for reducing risk of infection?
P (population) patients who need a wound care
I (intervention) sterile gloves
C (comparison) normal gloves
O (outcome) reduce the risk of infection
Search strategy
The search strategy that had been adopted for CINAHL database has been given in
appendix.
Articles identified
1. Brewer, J. D., Gonzalez, A. B., Baum, C. L., Arpey, C. J., Roenigk, R. K., Otley, C.
C., & Erwin, P. J. (2016). Comparison of sterile vs nonsterile gloves in cutaneous
surgery and common outpatient dental procedures: a systematic review and meta-
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING
analysis. JAMA dermatology, 152(9), 1008-1014.
doi:10.1001/jamadermatol.2016.1965 (level 1.b)
2. Heal, C., Sriharan, S., Buttner, P. G., & Kimber, D. (2015). Comparing non‐sterile to
sterile gloves for minor surgery: a prospective randomised controlled non‐inferiority
trial. Medical Journal of Australia, 202(1), 27-31.
https://doi.org/10.5694/mja14.00314 (level 1.c)
3. Michener, M., Xia, Y., Larrymore, D., McGraw, T., & McCarthy, S. (2019). A
comparison of infection rates during skin cancer excisions using nonsterile vs sterile
gloves: A prospective randomized pilot study. Journal of cosmetic dermatology.
https://doi.org/10.1111/jocd.12860 (level 1.c)
4. Rietz, A., Barzin, A., Jones, K., & Mounsey, A. (2015). PURLs: Sterile or non-sterile
gloves for minor skin excisions?. The Journal of family practice, 64(11), 723.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5029541/pdf/JFP-64-723.pdf (level
4.a)
5. Steen, K. (2017). Sterile or non-sterile gloves in minor surgical procedures in general
practice. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny
raekke, 137(12-13), 885-889. DOI: 10.4045/tidsskr.16.0599 (level 1.b)
Justification
Of the five evidences that had been selected for the assignment, two were systematic
review, one was a narrative review, and two were randomised controlled trial (RCT). The
systematic review were selected since they contained an exhaustive summary of data that had
been gathered from formerly existing exploration, and were most probable to produce
accurate and dependable conclusions. The literature review was selected since it
encompassed modern-day information, together with fundamental findings, besides
theoretical involvement in the topic. The RCTs were based on primary research and
analysis. JAMA dermatology, 152(9), 1008-1014.
doi:10.1001/jamadermatol.2016.1965 (level 1.b)
2. Heal, C., Sriharan, S., Buttner, P. G., & Kimber, D. (2015). Comparing non‐sterile to
sterile gloves for minor surgery: a prospective randomised controlled non‐inferiority
trial. Medical Journal of Australia, 202(1), 27-31.
https://doi.org/10.5694/mja14.00314 (level 1.c)
3. Michener, M., Xia, Y., Larrymore, D., McGraw, T., & McCarthy, S. (2019). A
comparison of infection rates during skin cancer excisions using nonsterile vs sterile
gloves: A prospective randomized pilot study. Journal of cosmetic dermatology.
https://doi.org/10.1111/jocd.12860 (level 1.c)
4. Rietz, A., Barzin, A., Jones, K., & Mounsey, A. (2015). PURLs: Sterile or non-sterile
gloves for minor skin excisions?. The Journal of family practice, 64(11), 723.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5029541/pdf/JFP-64-723.pdf (level
4.a)
5. Steen, K. (2017). Sterile or non-sterile gloves in minor surgical procedures in general
practice. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny
raekke, 137(12-13), 885-889. DOI: 10.4045/tidsskr.16.0599 (level 1.b)
Justification
Of the five evidences that had been selected for the assignment, two were systematic
review, one was a narrative review, and two were randomised controlled trial (RCT). The
systematic review were selected since they contained an exhaustive summary of data that had
been gathered from formerly existing exploration, and were most probable to produce
accurate and dependable conclusions. The literature review was selected since it
encompassed modern-day information, together with fundamental findings, besides
theoretical involvement in the topic. The RCTs were based on primary research and
5NURSING
compared patient outcomes in both the groups (sterile and non-sterile gloves), thus minimised
bias and made causal inferences.
compared patient outcomes in both the groups (sterile and non-sterile gloves), thus minimised
bias and made causal inferences.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING
PART 2
Synthesis
Findings from Heal, Sriharan, Buttner and Kimber (2015) suggested that when 493
patients who had been subjected to minor skin excision between 30 June 2012-28 March
2013 were allocated to two groups comprising of sterile and non-sterile gloves, incidence of
infection was found to be significantly non-inferior in the group of non-sterile gloves (NSG)
(8.7%; 95% CI, 4.9%–12.6%), in comparison to incidence in control group (SG) (9.3%; 95%
CI, 7.4%–11.1%). There was a 95% CI in infection rate difference that was -4.0% to 2.9%, (-
0.6%), and failed to attain the 7% predetermined margin. This was supported by Michener,
Xia, Larrymore, McGraw and McCarthy (2019) who also determined the incidence of
infection among surgical skin excision patients in outpatient department. Of the total 106
total wounds, 0 of 53 were found to be infected in NSG group, compared to 0/53 in SG
group at the time of initial screening during post-excision process (P = 0.99). Furthermore,
0.321 average wound inflammation score for NSG group confirmed their efficacy. However,
Steen (2017) argued that there is limited evidence for the efficacy of sterile and/or clean
gloves during surgery, on the outcomes of wound infection. They could not provide any
evidence for difference in frequency of infection among patients.
This was supported by Brewer et al. (2016) who suggested that there was no
significant difference in post-operative surgical site infection (SSI) rates between outpatient
surgeries that had been performed with SG and NSG. They conducted a systematic review
and found that of 228 patients who were reported to have postoperative SSI, 107 were in the
NSG group and 121 in the SG group. Moreover, general relative risk for SSI was 1.06 in
NSG group (95% CI, 0.81-1.39). Rietz, Barzin, Jones and Mounsey (2015) while numerous
studies in more than a few healthcare settings have found that NSG are non-inferior, in
PART 2
Synthesis
Findings from Heal, Sriharan, Buttner and Kimber (2015) suggested that when 493
patients who had been subjected to minor skin excision between 30 June 2012-28 March
2013 were allocated to two groups comprising of sterile and non-sterile gloves, incidence of
infection was found to be significantly non-inferior in the group of non-sterile gloves (NSG)
(8.7%; 95% CI, 4.9%–12.6%), in comparison to incidence in control group (SG) (9.3%; 95%
CI, 7.4%–11.1%). There was a 95% CI in infection rate difference that was -4.0% to 2.9%, (-
0.6%), and failed to attain the 7% predetermined margin. This was supported by Michener,
Xia, Larrymore, McGraw and McCarthy (2019) who also determined the incidence of
infection among surgical skin excision patients in outpatient department. Of the total 106
total wounds, 0 of 53 were found to be infected in NSG group, compared to 0/53 in SG
group at the time of initial screening during post-excision process (P = 0.99). Furthermore,
0.321 average wound inflammation score for NSG group confirmed their efficacy. However,
Steen (2017) argued that there is limited evidence for the efficacy of sterile and/or clean
gloves during surgery, on the outcomes of wound infection. They could not provide any
evidence for difference in frequency of infection among patients.
This was supported by Brewer et al. (2016) who suggested that there was no
significant difference in post-operative surgical site infection (SSI) rates between outpatient
surgeries that had been performed with SG and NSG. They conducted a systematic review
and found that of 228 patients who were reported to have postoperative SSI, 107 were in the
NSG group and 121 in the SG group. Moreover, general relative risk for SSI was 1.06 in
NSG group (95% CI, 0.81-1.39). Rietz, Barzin, Jones and Mounsey (2015) while numerous
studies in more than a few healthcare settings have found that NSG are non-inferior, in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING
comparison to SG for the prevention of SSI, following minor skin operations, there is non-
existence of evidence to encourage family physicians to adopt usage of NSG for infection
control.
Highest evidence
The systematic review and meta-analysis conducted by Brewer et al. (2016) can be
considered as the highest level of evidence owing to the fact that it adequately addressed all
components of the aforementioned PICO question. The research article provided definite
answers to the precise research question by collecting and summarising all available
empirical substantiation that effortlessly fit in the inclusion and exclusion criteria (Creswell
& Creswell, 2017). Moreover, usage of statistical approaches in the meta-analysis facilitated
in associating the outcomes of individual research that had been assimilated in the review,
thus increasing its trustworthiness. The motive for seeing it as the utmost evidence can be
attributed to the presence of evidently demarcated research purposes, reproducible and
unambiguous research procedure, and existence of a methodical search tactic for mining all
pertinent articles. In addition, by joining outcomes from different articles, the meta-analysis
augmented the sample size, thus the authority to discover the outcome of interest.
Critical appraisal tool
The JBI checklist that has been formulated for critically assessing systematic reviews
was carefully chosen for evaluating the article mentioned in the previous section. Reason for
choosing this article can be attributed to the fact that JBI is a worldwide, association based
research and development association and the aforementioned critical appraisal tool has been
framed by JBI workers, following which they have been subjected to peer review and
approved by the JBI Scientific Committee (Joanna Briggs Institute, 2013).
comparison to SG for the prevention of SSI, following minor skin operations, there is non-
existence of evidence to encourage family physicians to adopt usage of NSG for infection
control.
Highest evidence
The systematic review and meta-analysis conducted by Brewer et al. (2016) can be
considered as the highest level of evidence owing to the fact that it adequately addressed all
components of the aforementioned PICO question. The research article provided definite
answers to the precise research question by collecting and summarising all available
empirical substantiation that effortlessly fit in the inclusion and exclusion criteria (Creswell
& Creswell, 2017). Moreover, usage of statistical approaches in the meta-analysis facilitated
in associating the outcomes of individual research that had been assimilated in the review,
thus increasing its trustworthiness. The motive for seeing it as the utmost evidence can be
attributed to the presence of evidently demarcated research purposes, reproducible and
unambiguous research procedure, and existence of a methodical search tactic for mining all
pertinent articles. In addition, by joining outcomes from different articles, the meta-analysis
augmented the sample size, thus the authority to discover the outcome of interest.
Critical appraisal tool
The JBI checklist that has been formulated for critically assessing systematic reviews
was carefully chosen for evaluating the article mentioned in the previous section. Reason for
choosing this article can be attributed to the fact that JBI is a worldwide, association based
research and development association and the aforementioned critical appraisal tool has been
framed by JBI workers, following which they have been subjected to peer review and
approved by the JBI Scientific Committee (Joanna Briggs Institute, 2013).
8NURSING
Critical appraisal
The review question was clearly stated and distinct. The research question based on
which this systematic review had been conducted focused on determining whether the usage
of SG versus NSG in outpatient cutaneous processes created any impact on post-operative
wound infection rates. Also referred to as SSI, post-operative wound infection complicates
the course of recovery of most patients and typically occur within the first month of being
subjected to a surgical procedure, at a region of the body where the surgery was performed
(Chen et al., 2015). The research question was explicit owing to the fact that surgical wounds
generally become infected by the action of bacteria, notwithstanding the presence of bacteria
on the skin of the patient, or its transmission to the patient, following direct contact with
infected persons. Wound infections are either deep (tissue and muscle), superficial (skin
only), or spread to different organs where the surgery had been performed. In addition,
though majority of SSIs have been found to be uncomplicated, other cases might be more
challenging and severe to manage, such as, deep soft tissue necrotizing infections
(Kaoutzanis et al., 2015).
When such infections occur in the patient, multiple reoperations and/or extensive
surgical debridement are often required, and can also be life-threatening. Furthermore, the
extent and location of infection, in addition to the clinical condition of the patient also
governs the wound management approach. Thus, it can be stated that the research question
addressed a well-focused issue. Researchers have often mentioned that it is imperative to
formulate an exact inclusion and exclusion criteria that aids in determining the features, based
on which potential evidences are incorporated in an investigation (Peters et al., 2015).
Besides, presence of such eligibility criteria also supports to exclude pieces of scholarly
evidences that are not pertinent to the phenomenon that is currently being investigated. The
researchers clearly stated that they included observational comparative and randomised
Critical appraisal
The review question was clearly stated and distinct. The research question based on
which this systematic review had been conducted focused on determining whether the usage
of SG versus NSG in outpatient cutaneous processes created any impact on post-operative
wound infection rates. Also referred to as SSI, post-operative wound infection complicates
the course of recovery of most patients and typically occur within the first month of being
subjected to a surgical procedure, at a region of the body where the surgery was performed
(Chen et al., 2015). The research question was explicit owing to the fact that surgical wounds
generally become infected by the action of bacteria, notwithstanding the presence of bacteria
on the skin of the patient, or its transmission to the patient, following direct contact with
infected persons. Wound infections are either deep (tissue and muscle), superficial (skin
only), or spread to different organs where the surgery had been performed. In addition,
though majority of SSIs have been found to be uncomplicated, other cases might be more
challenging and severe to manage, such as, deep soft tissue necrotizing infections
(Kaoutzanis et al., 2015).
When such infections occur in the patient, multiple reoperations and/or extensive
surgical debridement are often required, and can also be life-threatening. Furthermore, the
extent and location of infection, in addition to the clinical condition of the patient also
governs the wound management approach. Thus, it can be stated that the research question
addressed a well-focused issue. Researchers have often mentioned that it is imperative to
formulate an exact inclusion and exclusion criteria that aids in determining the features, based
on which potential evidences are incorporated in an investigation (Peters et al., 2015).
Besides, presence of such eligibility criteria also supports to exclude pieces of scholarly
evidences that are not pertinent to the phenomenon that is currently being investigated. The
researchers clearly stated that they included observational comparative and randomised
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING
controlled trials in the review. In addition, those articles that focused on patients who had
been subjected to outpatient mucosal and cutaneous surgery, such as, standard excisions,
laceration repair, MMS, and tooth extractions, with the use of SG or NSG were only
incorporated in the review.
Search strategy generally refers to the pre-determined agenda that comprises of
specific search phrases and key terms, which are used for probing evidences from several
electronic databases. Therefore, formulation of an explicit search plan aids in replicating alike
results later on (McGowan et al., 2016). The systematic review was conducted by the
researchers in the expanded electronic database of Ovid EMBASE, Scopus, EBSCO
Cumulative Index to Nursing and Allied Health Literature, Web of Science, and Ovid
Cochrane Central Register of Controlled Trials, with the use of medical subject headings
(MeSH) and key words. The terms used for article extraction were namely, gloves,
dermatologic surgical procedures, surgical, sterile, surgical infections, clean, and non-sterile.
However, the year of article publishing varied in the aforementioned databases. Hence,
presence of a well-defined search strategy provided a comprehensive overview of the
procedures that had been followed by the researchers.
According to McGowan et al. (2016) it is necessary to conduct an investigation in
different electronic databases, in addition to the major bibliographic citation databases for
retrieving all articles that pertinent to the research question. However, grey literature and
unpublished manuscripts were not incorporated in the review, thereby increasing the
possibility of excluding articles that addressed the research question. They clearly mentioned
that all studies included in the review were assessed based on the Cochrane collaboration
guidelines for determining the risk of potential bias.
controlled trials in the review. In addition, those articles that focused on patients who had
been subjected to outpatient mucosal and cutaneous surgery, such as, standard excisions,
laceration repair, MMS, and tooth extractions, with the use of SG or NSG were only
incorporated in the review.
Search strategy generally refers to the pre-determined agenda that comprises of
specific search phrases and key terms, which are used for probing evidences from several
electronic databases. Therefore, formulation of an explicit search plan aids in replicating alike
results later on (McGowan et al., 2016). The systematic review was conducted by the
researchers in the expanded electronic database of Ovid EMBASE, Scopus, EBSCO
Cumulative Index to Nursing and Allied Health Literature, Web of Science, and Ovid
Cochrane Central Register of Controlled Trials, with the use of medical subject headings
(MeSH) and key words. The terms used for article extraction were namely, gloves,
dermatologic surgical procedures, surgical, sterile, surgical infections, clean, and non-sterile.
However, the year of article publishing varied in the aforementioned databases. Hence,
presence of a well-defined search strategy provided a comprehensive overview of the
procedures that had been followed by the researchers.
According to McGowan et al. (2016) it is necessary to conduct an investigation in
different electronic databases, in addition to the major bibliographic citation databases for
retrieving all articles that pertinent to the research question. However, grey literature and
unpublished manuscripts were not incorporated in the review, thereby increasing the
possibility of excluding articles that addressed the research question. They clearly mentioned
that all studies included in the review were assessed based on the Cochrane collaboration
guidelines for determining the risk of potential bias.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING
According to LoBiondo-Wood and Haber (2014) the process of critical assessment
generally involves methodical and cautious investigation of the consequences regarding a
specific examination in order to judge the worth, significance and reliability in a certain
context. A principal feature that can lessen systematic bias or error at the time of piloting
systematic review is the presence of two or more associates of the review team, who self-
reliantly complete valuation of the selected articles. The researchers stated that two
independent reviewers ABGJ and JDB conducted a quality assessment of the articles using
the Newcastle-Ottawa Scale and the QUOROM statement. Furthermore, they also resolved
all discrepancies related to critical assessment by forming a consensus, thus eliminating bias
in the results.
Systematic reviews largely depend on appropriate synthesis of the collected
evidences. The researchers elaborated on the fact that the primary outcome of their
investigation was post-operative wound SSI. However, the researchers failed to provide
adequate evidence on the secondary outcome for the systematic review. Moreover, the
researchers also addressed heterogeneity and inconsistencies by using the QUOROM
statement for meta-analysis. Following extraction of all data, the findings were analysed with
the use of the Review Manager software (version 5.3; Cochrane). Later on, the researchers
performed a subgroup meta-analysis for all the articles. Publication bias generally occurs
when articles that contain positive findings demonstrate an increased likelihood of being
published, in comparison to negative finding studies (Sanchez-Tojar et al., 2018). However,
the researchers stated that there was no major discrepancy or outlier amid the observational
studies, thus suggesting minimal risk of bias.
It is imperative for a review to provide comprehensive recommendations for future
clinical practice, which in turn will help in the formulation of essential healthcare policies.
The researchers clearly stated that at the time of considering particular surgical strategies and
According to LoBiondo-Wood and Haber (2014) the process of critical assessment
generally involves methodical and cautious investigation of the consequences regarding a
specific examination in order to judge the worth, significance and reliability in a certain
context. A principal feature that can lessen systematic bias or error at the time of piloting
systematic review is the presence of two or more associates of the review team, who self-
reliantly complete valuation of the selected articles. The researchers stated that two
independent reviewers ABGJ and JDB conducted a quality assessment of the articles using
the Newcastle-Ottawa Scale and the QUOROM statement. Furthermore, they also resolved
all discrepancies related to critical assessment by forming a consensus, thus eliminating bias
in the results.
Systematic reviews largely depend on appropriate synthesis of the collected
evidences. The researchers elaborated on the fact that the primary outcome of their
investigation was post-operative wound SSI. However, the researchers failed to provide
adequate evidence on the secondary outcome for the systematic review. Moreover, the
researchers also addressed heterogeneity and inconsistencies by using the QUOROM
statement for meta-analysis. Following extraction of all data, the findings were analysed with
the use of the Review Manager software (version 5.3; Cochrane). Later on, the researchers
performed a subgroup meta-analysis for all the articles. Publication bias generally occurs
when articles that contain positive findings demonstrate an increased likelihood of being
published, in comparison to negative finding studies (Sanchez-Tojar et al., 2018). However,
the researchers stated that there was no major discrepancy or outlier amid the observational
studies, thus suggesting minimal risk of bias.
It is imperative for a review to provide comprehensive recommendations for future
clinical practice, which in turn will help in the formulation of essential healthcare policies.
The researchers clearly stated that at the time of considering particular surgical strategies and
11NURSING
practices, numerous factors should be measured, together with the possible significances of
opposing the recognised sterile glove usage and the latent challenges this could arise, from a
medicolegal perspective. They also focused on the need of acknowledging patient perspective
for usage of sterile procedures. Moreover, they also highlighted the importance of conducting
future research for determining the impact of surgery complexity and duration on post-
operative SSI development.
practices, numerous factors should be measured, together with the possible significances of
opposing the recognised sterile glove usage and the latent challenges this could arise, from a
medicolegal perspective. They also focused on the need of acknowledging patient perspective
for usage of sterile procedures. Moreover, they also highlighted the importance of conducting
future research for determining the impact of surgery complexity and duration on post-
operative SSI development.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 27
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





