A Report on Strategic Commissioning and its Approaches in Healthcare
VerifiedAdded on 2023/04/22
|22
|5885
|133
Report
AI Summary
This report provides a comprehensive overview of strategic commissioning within the healthcare environment, with a particular focus on NHS England. It defines strategic commissioning as the planning and delivery of services to meet the needs of individuals and communities, emphasizing its role in driving quality, efficiency, and patient outcomes. The report explores the strategic commissioning framework, highlighting its key stages of analysis, planning, delivery, and review. It also delves into the purpose, values, and strategic objectives of NHS England's strategic commissioning plan, including its priorities, approach to transformation, and methods for involving patients, the public, and partners in developing a whole-system vision. The report further examines the importance of primary care transformation, the challenges faced by general practices, and the strategies for improving service delivery and patient access, ultimately aiming to enhance population health and well-being.
STRATEGIC AND COMMISSIONING
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Table of Contents
Introduction......................................................................................................................................1
Strategic Commissioning.................................................................................................................1
Strategic Commissioning Framework.............................................................................................5
Purpose, values and strategic objectives of NHS England Strategic Commissioning plan.........8
Priorities for NHS England..............................................................................................................9
Involving patients, public and partners in developing a whole system vision..........................11
Approach to delivering transformation......................................................................................12
Conclusion.....................................................................................................................................16
References......................................................................................................................................18
Introduction......................................................................................................................................1
Strategic Commissioning.................................................................................................................1
Strategic Commissioning Framework.............................................................................................5
Purpose, values and strategic objectives of NHS England Strategic Commissioning plan.........8
Priorities for NHS England..............................................................................................................9
Involving patients, public and partners in developing a whole system vision..........................11
Approach to delivering transformation......................................................................................12
Conclusion.....................................................................................................................................16
References......................................................................................................................................18
LIST OF FIGURES
Figure 1: IPC Commissioning Framework......................................................................................2
Figure 2: Model of Care..................................................................................................................7
Figure 3: Future Map.....................................................................................................................11
Figure 4: Areas for Excellence for Warrington.............................................................................13
Figure 5: Acuity and Complexity Model.......................................................................................15
Figure 1: IPC Commissioning Framework......................................................................................2
Figure 2: Model of Care..................................................................................................................7
Figure 3: Future Map.....................................................................................................................11
Figure 4: Areas for Excellence for Warrington.............................................................................13
Figure 5: Acuity and Complexity Model.......................................................................................15
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INTRODUCTION
In general, strategic commissioning can be defined as the planning and delivering
services and support for people in a new manner. However, it consist of identifying the needs of
individuals and communities so as to enable people in deciding what will be best for the needs
and expectations. Over the past decade, the role of commissioning, as a key driver of quality,
efficiency and outcomes for patients, has become increasingly important to the health system in
England. The NHS commissioning system was previously made up of primary care trusts and
specialized commissioning groups. Most of the NHS commissioning budget is now managed by
211 clinical commissioning groups (CCGs). These are groups of general practices which come
together in each area to commission the best services for their patients and population.
Nationally, NHS England commissions specialized services, primary care, offender healthcare
and some services for the armed forces. It has 27 area teams but is one single organization
operating to a common model with one board. In the present research report, researcher focuses
on exploring the range of contemporary approaches to strategic commissioning within the health
care environment.
STRATEGIC COMMISSIONING
In general, strategic commissioning refers to the process of specifying, securing and
monitoring services to meet people’s needs at a strategic level. However, this applies to all the
services, whether they are provided by local authority, NHS or other public agencies or by
voluntary sectors. Further, strategic commissioning consist of four crucial stages: to analyse,
plan, deliver and review (Ozcan, 2005). In other words, commissioning is essentially
transformational and not just transactional. It is all about developing and shaping the capacity
within the communities, markets and individual lives that will assist or support the citizen in
meeting their needs and aspirations regardless of age and disability.
Improving commissioning has been one of the major focus of many government
publications if considering the past few years. However, this consist of Our Health, Care, and
Our say, Putting People First, Strong and Prosperous Communities, Health Act etc. Further, in a
published commissioning framework for health and well-being which mainly focuses on the
perspective of whole health and care economy within the context of reforming systems to meet
the needs of individuals. In this regard, strategic commissioning for health and care sector aims
at:
1
In general, strategic commissioning can be defined as the planning and delivering
services and support for people in a new manner. However, it consist of identifying the needs of
individuals and communities so as to enable people in deciding what will be best for the needs
and expectations. Over the past decade, the role of commissioning, as a key driver of quality,
efficiency and outcomes for patients, has become increasingly important to the health system in
England. The NHS commissioning system was previously made up of primary care trusts and
specialized commissioning groups. Most of the NHS commissioning budget is now managed by
211 clinical commissioning groups (CCGs). These are groups of general practices which come
together in each area to commission the best services for their patients and population.
Nationally, NHS England commissions specialized services, primary care, offender healthcare
and some services for the armed forces. It has 27 area teams but is one single organization
operating to a common model with one board. In the present research report, researcher focuses
on exploring the range of contemporary approaches to strategic commissioning within the health
care environment.
STRATEGIC COMMISSIONING
In general, strategic commissioning refers to the process of specifying, securing and
monitoring services to meet people’s needs at a strategic level. However, this applies to all the
services, whether they are provided by local authority, NHS or other public agencies or by
voluntary sectors. Further, strategic commissioning consist of four crucial stages: to analyse,
plan, deliver and review (Ozcan, 2005). In other words, commissioning is essentially
transformational and not just transactional. It is all about developing and shaping the capacity
within the communities, markets and individual lives that will assist or support the citizen in
meeting their needs and aspirations regardless of age and disability.
Improving commissioning has been one of the major focus of many government
publications if considering the past few years. However, this consist of Our Health, Care, and
Our say, Putting People First, Strong and Prosperous Communities, Health Act etc. Further, in a
published commissioning framework for health and well-being which mainly focuses on the
perspective of whole health and care economy within the context of reforming systems to meet
the needs of individuals. In this regard, strategic commissioning for health and care sector aims
at:
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

To place people at the centre while focusing on commissioning.
To identify and understand the needs of population as well as of individuals.
Making optimum utilisation of available information as well as sharing them properly.
Assuring quality in provision.
Promote wellbeing within the workforce.
Enhancing partnership working and improving the use of flexibilities and joint budgets.
Creating single health care vision (Bovaird, Briggsand Willis, 2014).
Enhancing the capabilities and leadership skills.
Furthermore, IPC commissioning framework is considered to be the most common
framework which consist of four key activities in the cycle of commissioning. However, it
emphasises on making sure that all four elements of the cycle such as: analyse, plan, do and
review are in sequence and of equal importance. Therefore, commissioners and contractors
should spend equal time, energy and attention on these four elements. It concentrates that
commissioning process should be equitable and transparent in nature to all the stakeholders.
Figure 1: IPC Commissioning Framework
(Source: Glasby, 2012)
In context to NHS England, it is responsible for the direct commissioning of services
outside the remit of clinical commissioning group which mainly consist of primary care, public
health, offender health, military and veteran health and specialised services. Along with this,
there are some CCGs which have been fully delegated towards the responsibility for
commissioning and contract management of primary medical care.
2
To identify and understand the needs of population as well as of individuals.
Making optimum utilisation of available information as well as sharing them properly.
Assuring quality in provision.
Promote wellbeing within the workforce.
Enhancing partnership working and improving the use of flexibilities and joint budgets.
Creating single health care vision (Bovaird, Briggsand Willis, 2014).
Enhancing the capabilities and leadership skills.
Furthermore, IPC commissioning framework is considered to be the most common
framework which consist of four key activities in the cycle of commissioning. However, it
emphasises on making sure that all four elements of the cycle such as: analyse, plan, do and
review are in sequence and of equal importance. Therefore, commissioners and contractors
should spend equal time, energy and attention on these four elements. It concentrates that
commissioning process should be equitable and transparent in nature to all the stakeholders.
Figure 1: IPC Commissioning Framework
(Source: Glasby, 2012)
In context to NHS England, it is responsible for the direct commissioning of services
outside the remit of clinical commissioning group which mainly consist of primary care, public
health, offender health, military and veteran health and specialised services. Along with this,
there are some CCGs which have been fully delegated towards the responsibility for
commissioning and contract management of primary medical care.
2
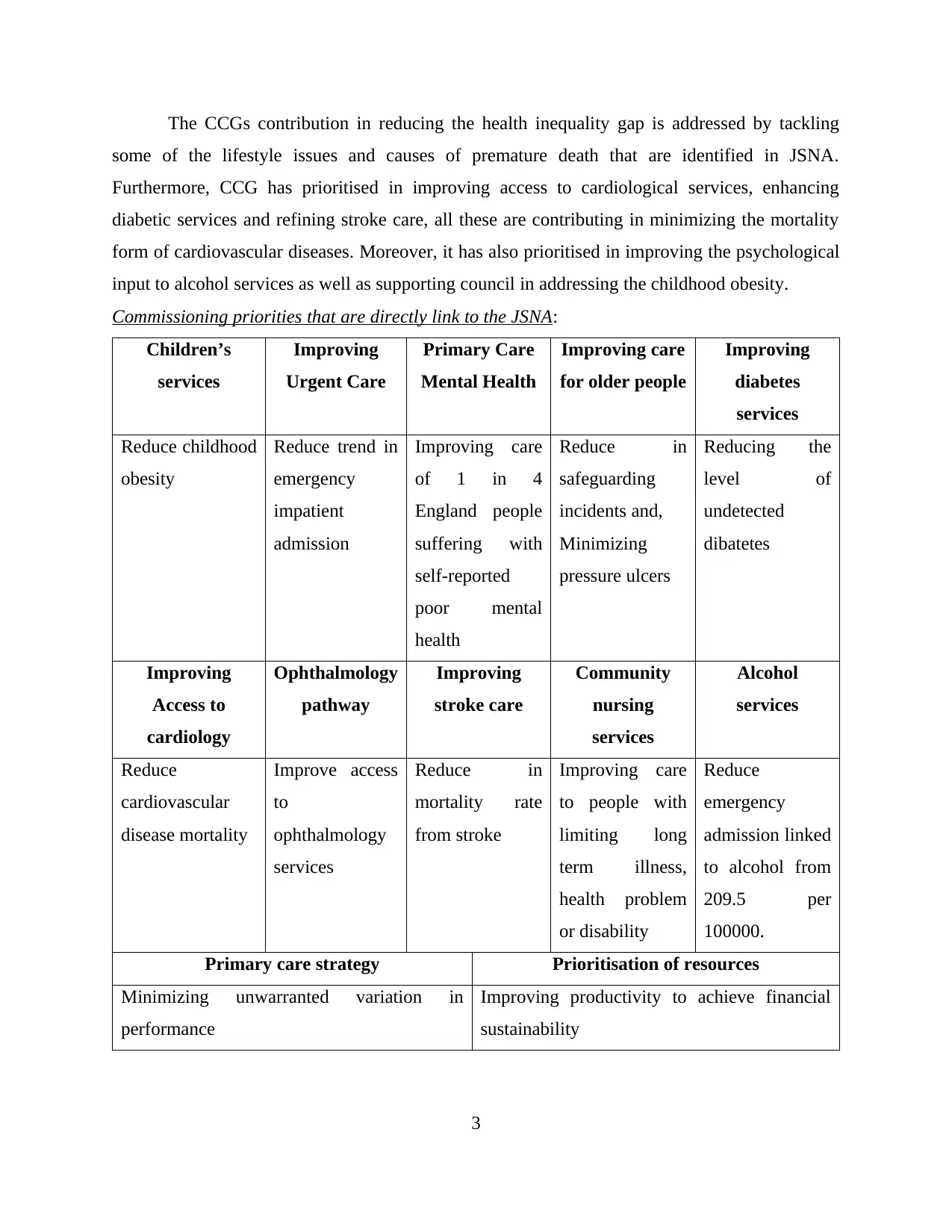
The CCGs contribution in reducing the health inequality gap is addressed by tackling
some of the lifestyle issues and causes of premature death that are identified in JSNA.
Furthermore, CCG has prioritised in improving access to cardiological services, enhancing
diabetic services and refining stroke care, all these are contributing in minimizing the mortality
form of cardiovascular diseases. Moreover, it has also prioritised in improving the psychological
input to alcohol services as well as supporting council in addressing the childhood obesity.
Commissioning priorities that are directly link to the JSNA:
Children’s
services
Improving
Urgent Care
Primary Care
Mental Health
Improving care
for older people
Improving
diabetes
services
Reduce childhood
obesity
Reduce trend in
emergency
impatient
admission
Improving care
of 1 in 4
England people
suffering with
self-reported
poor mental
health
Reduce in
safeguarding
incidents and,
Minimizing
pressure ulcers
Reducing the
level of
undetected
dibatetes
Improving
Access to
cardiology
Ophthalmology
pathway
Improving
stroke care
Community
nursing
services
Alcohol
services
Reduce
cardiovascular
disease mortality
Improve access
to
ophthalmology
services
Reduce in
mortality rate
from stroke
Improving care
to people with
limiting long
term illness,
health problem
or disability
Reduce
emergency
admission linked
to alcohol from
209.5 per
100000.
Primary care strategy Prioritisation of resources
Minimizing unwarranted variation in
performance
Improving productivity to achieve financial
sustainability
3
some of the lifestyle issues and causes of premature death that are identified in JSNA.
Furthermore, CCG has prioritised in improving access to cardiological services, enhancing
diabetic services and refining stroke care, all these are contributing in minimizing the mortality
form of cardiovascular diseases. Moreover, it has also prioritised in improving the psychological
input to alcohol services as well as supporting council in addressing the childhood obesity.
Commissioning priorities that are directly link to the JSNA:
Children’s
services
Improving
Urgent Care
Primary Care
Mental Health
Improving care
for older people
Improving
diabetes
services
Reduce childhood
obesity
Reduce trend in
emergency
impatient
admission
Improving care
of 1 in 4
England people
suffering with
self-reported
poor mental
health
Reduce in
safeguarding
incidents and,
Minimizing
pressure ulcers
Reducing the
level of
undetected
dibatetes
Improving
Access to
cardiology
Ophthalmology
pathway
Improving
stroke care
Community
nursing
services
Alcohol
services
Reduce
cardiovascular
disease mortality
Improve access
to
ophthalmology
services
Reduce in
mortality rate
from stroke
Improving care
to people with
limiting long
term illness,
health problem
or disability
Reduce
emergency
admission linked
to alcohol from
209.5 per
100000.
Primary care strategy Prioritisation of resources
Minimizing unwarranted variation in
performance
Improving productivity to achieve financial
sustainability
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Along with this, there are several principles of strategic commissioning of NHS England
are as follows:
Enabling the improvement of primary care.
To balance consistency and local flexibility (Dickinson, 2014).
Alignment with policy and compliance with legislation
Compliance with equality act, 2010.
A realistic balance between attention to detail and practical application.
A reasonable, proportionate and consistent approach across the four primary contractor
groups.
However, NHS is unique because of its system regarding general practices as it is a
medical home for the patients with lifelong medical record. In NHS, general practices are the
first point of access for several people, while high proportion of care is delivered close to the
patients’ homes with same clinical team. NHS England has served patients over 60 years and
providing them the high quality, value for money care etc. With changing environment, patients
are changing in terms of expectations and complexity. This clearly indicates that, if NHS have to
provide better quality of services to its patients then it is important to become more innovative
and creative within the approaches (Harris, Garnerand Perkins, 2015).
The NHS Five Year Forward View:
In October 2014, NHS England published the five year forward view which was
developed in collaboration with major institutions such as PHW, Monitor, HEE, CQC and TDA.
However, this helped in presenting new deal for general practices which also indeed focused on
funding in general practice. It mainly focused on two elements stabilising and new funding.
Further, this report assist in evaluating that, the new deal for general practices consist of:
Stabilising core funding for general practice nationally so as to make resources available
to primary care in different areas effectively.
Providing new funding options through different schemes for improving the access to
services.
Expanding quickly by training and developments to community nurses and other primary
care staff.
Increase the investment in recruitment and retention scheme for ensuring the employing
better and skilled personnel (Bovaird, Briggsand Willis, 2014).
4
are as follows:
Enabling the improvement of primary care.
To balance consistency and local flexibility (Dickinson, 2014).
Alignment with policy and compliance with legislation
Compliance with equality act, 2010.
A realistic balance between attention to detail and practical application.
A reasonable, proportionate and consistent approach across the four primary contractor
groups.
However, NHS is unique because of its system regarding general practices as it is a
medical home for the patients with lifelong medical record. In NHS, general practices are the
first point of access for several people, while high proportion of care is delivered close to the
patients’ homes with same clinical team. NHS England has served patients over 60 years and
providing them the high quality, value for money care etc. With changing environment, patients
are changing in terms of expectations and complexity. This clearly indicates that, if NHS have to
provide better quality of services to its patients then it is important to become more innovative
and creative within the approaches (Harris, Garnerand Perkins, 2015).
The NHS Five Year Forward View:
In October 2014, NHS England published the five year forward view which was
developed in collaboration with major institutions such as PHW, Monitor, HEE, CQC and TDA.
However, this helped in presenting new deal for general practices which also indeed focused on
funding in general practice. It mainly focused on two elements stabilising and new funding.
Further, this report assist in evaluating that, the new deal for general practices consist of:
Stabilising core funding for general practice nationally so as to make resources available
to primary care in different areas effectively.
Providing new funding options through different schemes for improving the access to
services.
Expanding quickly by training and developments to community nurses and other primary
care staff.
Increase the investment in recruitment and retention scheme for ensuring the employing
better and skilled personnel (Bovaird, Briggsand Willis, 2014).
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Expand funding to upgrade primary care infrastructure and scope of services.
STRATEGIC COMMISSIONING FRAMEWORK
The strategic commissioning framework aims to assist or support the primary carve
transformation across the Warrington. There are several components of this framework which
needs to be given proper attention and importance which mainly focused on transforming
primary care in Warrington.
General practices in Warrington are under stress and are bearing the burden of pressures
to satisfy the increasing and changing health needs. However, strategic commissioning
framework assist in setting ambitious and attractive vision of general practice that operates
without any border as well as forms of partnership with different health and care system. The
main purpose of this is to make sure that, patients are treated in the best possible manner and
efforts should be in context with patient’s centred coordinated care (Evans and et.al, 2015).
Further, this is promoted to various centres in each neighbourhood, developing community
which indeed supporting Londoners to stay healthy. In this, commissioning framework mainly
concentrated on function rather than form that assist in setting out new patients offers for all the
Londoners that can be offered to them by primary care teams in innovative ways.
Looking at the present condition due to several number of reasons, general practice of
NHS is unable to deliver what is exactly expected across Warrington. However, the main reason
behind this has been identified is related to funding for general practice which has been declining
over the last decade. At present only 7% of funds are allocated to general practice which indeed
creates major concerns for the primary care in constantly delivering the services to majority of
care patients in the NHS. Further, increasing funding will not only be the solution to this problem
as there are several aspects that general practice need to change which are as follows:
The way NHS deliver care: It is important for the management of NHS Warrington to
make sure that inside and outside of the practice they have to make use of best skill mix.
This will help in ensuring better services at primary, secondary, community, voluntary
and charity sectors (Willis, Bovairdand Glasby, 2012).
The way we organise ourselves: This focuses on normal working hours and out of hours.
However, to enhance the quality of services within general practice it is important to
deliver unscheduled care in effective and efficient manner. Ensuring at every stage will
5
STRATEGIC COMMISSIONING FRAMEWORK
The strategic commissioning framework aims to assist or support the primary carve
transformation across the Warrington. There are several components of this framework which
needs to be given proper attention and importance which mainly focused on transforming
primary care in Warrington.
General practices in Warrington are under stress and are bearing the burden of pressures
to satisfy the increasing and changing health needs. However, strategic commissioning
framework assist in setting ambitious and attractive vision of general practice that operates
without any border as well as forms of partnership with different health and care system. The
main purpose of this is to make sure that, patients are treated in the best possible manner and
efforts should be in context with patient’s centred coordinated care (Evans and et.al, 2015).
Further, this is promoted to various centres in each neighbourhood, developing community
which indeed supporting Londoners to stay healthy. In this, commissioning framework mainly
concentrated on function rather than form that assist in setting out new patients offers for all the
Londoners that can be offered to them by primary care teams in innovative ways.
Looking at the present condition due to several number of reasons, general practice of
NHS is unable to deliver what is exactly expected across Warrington. However, the main reason
behind this has been identified is related to funding for general practice which has been declining
over the last decade. At present only 7% of funds are allocated to general practice which indeed
creates major concerns for the primary care in constantly delivering the services to majority of
care patients in the NHS. Further, increasing funding will not only be the solution to this problem
as there are several aspects that general practice need to change which are as follows:
The way NHS deliver care: It is important for the management of NHS Warrington to
make sure that inside and outside of the practice they have to make use of best skill mix.
This will help in ensuring better services at primary, secondary, community, voluntary
and charity sectors (Willis, Bovairdand Glasby, 2012).
The way we organise ourselves: This focuses on normal working hours and out of hours.
However, to enhance the quality of services within general practice it is important to
deliver unscheduled care in effective and efficient manner. Ensuring at every stage will
5
help entire course of NHS England in enhancing the services for Londoners and other
countries patients.
How we work together: In this, management of NHS is collaborating with different care
providers in those areas which are vulnerable, isolated and socially downgraded who are
at risk of becoming ill and least likely to seek out support to stay well. Furthermore,
developing experts working with secondary care practitioners so as to help them to
support in improving the skills and abilities at local level.
How we meet the different access needs: For this, management allowing patients to
choose from different range of services options which indeed assist in enabling the way
patients access to general practice.
How we use data: By assessing the needs and expectations of patients as well as
involving experts to improve the quality of clinical care. Along with this, data is used to
provide early warning for system failure, helps the care practitioners to see patients on
different site. Overall this assist NHS to deliver services in effective and efficient ways
which consist of remote care (e-health and telecare) (Dickinson and et.al, 2013).
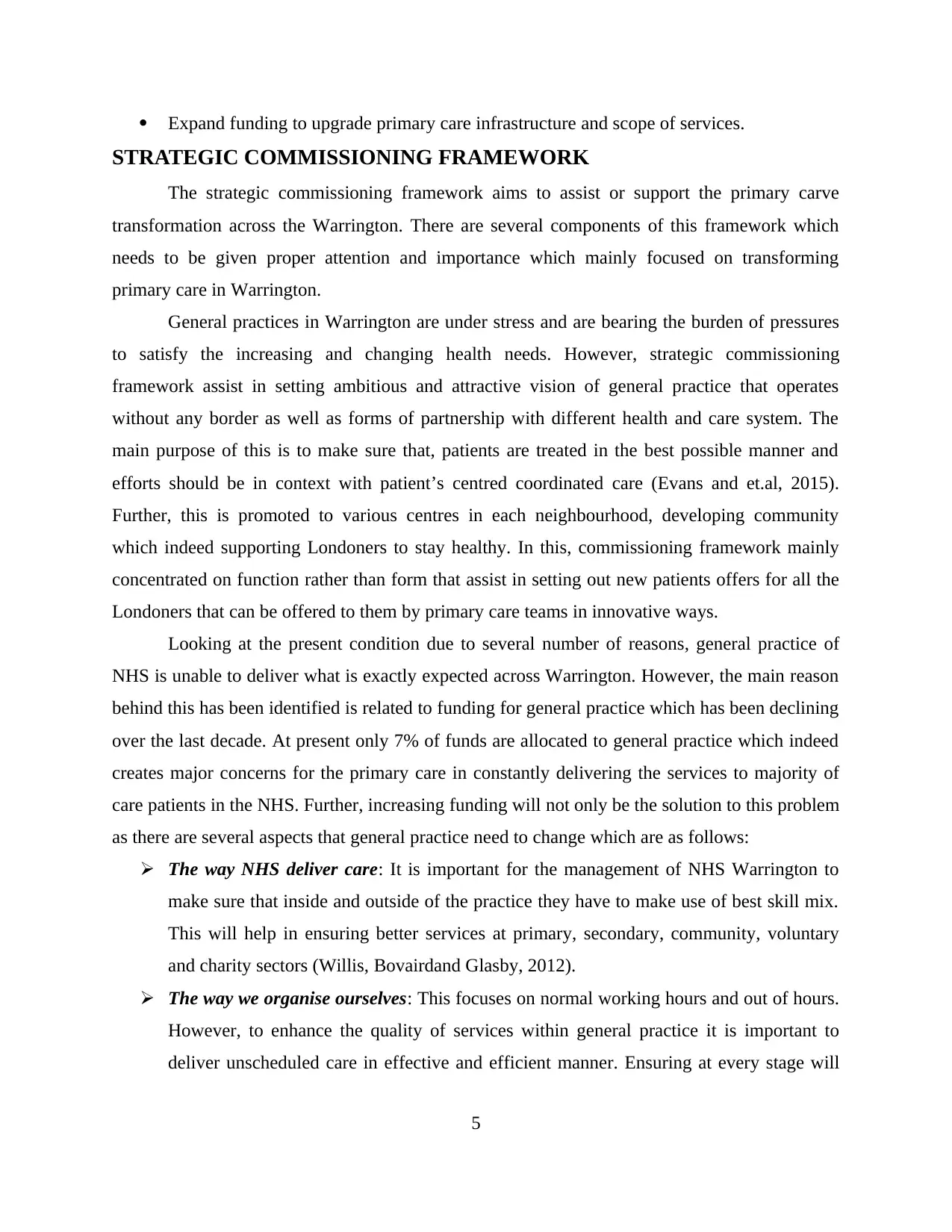
Model of Care
The health care system for NHS is considered to be primary care oriented so that it
focuses on enhancing the population health and wellbeing. Further, this ensures improving the
overall functioning or level of customer’s satisfaction in different areas which consist of
specialized services, primary care, offender healthcare and some services related to the armed
forces. The main purpose behind employing this health care system is that it will help in
transformational commissioning functions such as redesigning of services within each areas as
well as focusing on transactional commissioning functions such as market management,
healthcare procurement, contract negotiation and monitoring, information analysis and risks
stratification.
In order to make sure that patients acquire the best possible services from this it is
important NHS Warrington to involve collaborative approach with voluntary and community
organisations, community health services, community pharmacies, mental health services, social
care and other partners (Board, 2013).
6
countries patients.
How we work together: In this, management of NHS is collaborating with different care
providers in those areas which are vulnerable, isolated and socially downgraded who are
at risk of becoming ill and least likely to seek out support to stay well. Furthermore,
developing experts working with secondary care practitioners so as to help them to
support in improving the skills and abilities at local level.
How we meet the different access needs: For this, management allowing patients to
choose from different range of services options which indeed assist in enabling the way
patients access to general practice.
How we use data: By assessing the needs and expectations of patients as well as
involving experts to improve the quality of clinical care. Along with this, data is used to
provide early warning for system failure, helps the care practitioners to see patients on
different site. Overall this assist NHS to deliver services in effective and efficient ways
which consist of remote care (e-health and telecare) (Dickinson and et.al, 2013).
Model of Care
The health care system for NHS is considered to be primary care oriented so that it
focuses on enhancing the population health and wellbeing. Further, this ensures improving the
overall functioning or level of customer’s satisfaction in different areas which consist of
specialized services, primary care, offender healthcare and some services related to the armed
forces. The main purpose behind employing this health care system is that it will help in
transformational commissioning functions such as redesigning of services within each areas as
well as focusing on transactional commissioning functions such as market management,
healthcare procurement, contract negotiation and monitoring, information analysis and risks
stratification.
In order to make sure that patients acquire the best possible services from this it is
important NHS Warrington to involve collaborative approach with voluntary and community
organisations, community health services, community pharmacies, mental health services, social
care and other partners (Board, 2013).
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Figure 2: Model of Care
(Source: Miller and Rees, 2014)
By the means of above defined model it can be evaluated that, sharing system for the
senior staff members clearly review that development and supportive learning that should
enhance the level of patient safety, clinical quality and positive outcomes for all practices
involved. By the means of this model, NHS will consist of several teams that will support care
coordination and will have arrangements in place for closer partnership with a wider range of
practitioners and specialist beyond general practice. NHS England has worked with Warrington’s
clinical commissioning groups to lead an open, transparent and collaborative process to engage
key stakeholders to provide feedback on its draft transforming primary care in Warrington.
However, service specification can be defined by patient’s voices, clinical leaders, current best
practice, innovation and best evidence. During the development of patients offer, framework has
focused on collaborating and engaging with clinicians, patients and other stakeholders in order to
identify and understand the needs and perspectives of different groups (Chambers and et.al,
2012). Furthermore, technology play significant role in health care provision because with the
help of this, senior practitioner can enhance the service delivery as well as enhance the access of
7
(Source: Miller and Rees, 2014)
By the means of above defined model it can be evaluated that, sharing system for the
senior staff members clearly review that development and supportive learning that should
enhance the level of patient safety, clinical quality and positive outcomes for all practices
involved. By the means of this model, NHS will consist of several teams that will support care
coordination and will have arrangements in place for closer partnership with a wider range of
practitioners and specialist beyond general practice. NHS England has worked with Warrington’s
clinical commissioning groups to lead an open, transparent and collaborative process to engage
key stakeholders to provide feedback on its draft transforming primary care in Warrington.
However, service specification can be defined by patient’s voices, clinical leaders, current best
practice, innovation and best evidence. During the development of patients offer, framework has
focused on collaborating and engaging with clinicians, patients and other stakeholders in order to
identify and understand the needs and perspectives of different groups (Chambers and et.al,
2012). Furthermore, technology play significant role in health care provision because with the
help of this, senior practitioner can enhance the service delivery as well as enhance the access of
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
medical services. In order to satisfy the needs it is important for maximizing the use of
technology available, empowering the patients and ensuring that there is link between processes
and services offered by the healthcare organisation to the patients. However, people should be
empowered with the information about their care so that they can make decision regarding what
services expected from the healthcare practitioners.
Purpose, values and strategic objectives of NHS England Strategic Commissioning plan
Purpose:
The main purpose of clinical commissioning group (CCG), is to improve and change the
lives of residents for their betterment. However, NHS wants to make real different in enhancing
the way people access health and social care services, so that they can acquire services as per
their expectations (McCray and Palmer, 2014).
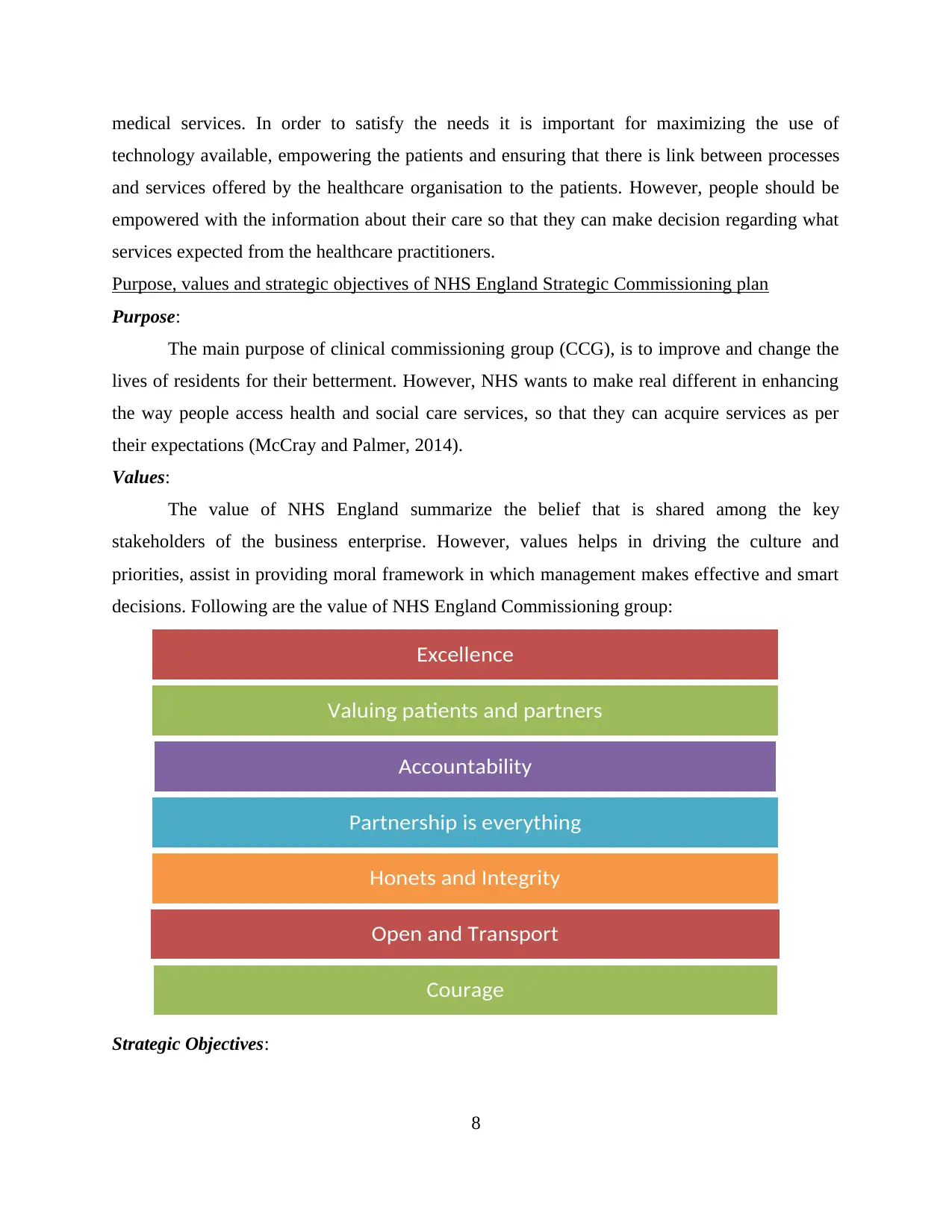
Values:
The value of NHS England summarize the belief that is shared among the key
stakeholders of the business enterprise. However, values helps in driving the culture and
priorities, assist in providing moral framework in which management makes effective and smart
decisions. Following are the value of NHS England Commissioning group:
Strategic Objectives:
8
Excellence
Valuing patients and partners
Accountability
Partnership is everything
Honets and Integrity
Open and Transport
Courage
technology available, empowering the patients and ensuring that there is link between processes
and services offered by the healthcare organisation to the patients. However, people should be
empowered with the information about their care so that they can make decision regarding what
services expected from the healthcare practitioners.
Purpose, values and strategic objectives of NHS England Strategic Commissioning plan
Purpose:
The main purpose of clinical commissioning group (CCG), is to improve and change the
lives of residents for their betterment. However, NHS wants to make real different in enhancing
the way people access health and social care services, so that they can acquire services as per
their expectations (McCray and Palmer, 2014).
Values:
The value of NHS England summarize the belief that is shared among the key
stakeholders of the business enterprise. However, values helps in driving the culture and
priorities, assist in providing moral framework in which management makes effective and smart
decisions. Following are the value of NHS England Commissioning group:
Strategic Objectives:
8
Excellence
Valuing patients and partners
Accountability
Partnership is everything
Honets and Integrity
Open and Transport
Courage
There are several strategic objectives that are needed to support the achievement of
overall vision of the cited firm. However, development of these objectives are based on the
followed structure which is incorporated with feedbacks from associated stakeholders. Further,
these objectives are denoted as “Planning for Patients”.
Improving the healthy life expectancy for the people of England.
Minimizing or reducing the inequalities at the time of providing services.
To encourage all the commissioned services in order to support delivery of the NHS
constitution for the entire population (Transforming Primary Care in London: A
Strategic Commissioning Framework, 2015).
Constantly improving the quality of commissioned.
Attaining sustainable financial balance.
Developing and maintaining highly effective and motivated workforce.
Making sure that sound governance arrangements are in place.
Promoting the incorporation of proper integration of commissioned services.
PRIORITIES FOR NHS ENGLAND
Priorities are essential in order to illustrate the important of work or activities. Herein,
priorities for NHS England sets out the factors that are driving the plan for change or
modifications within the healthcare of Warrington. There are several areas of health in which
Warrington is doing relatively well or improving at good rate.
On the basis of health outcomes and impact of major diseases:
Life expectancy of cited place is increasing as the gap between Warrington and England
is decreasing especially in context to males.
Along with this, internal inequalities gap in life expectancy has decreased in the town.
The death rate in affluent areas of Warrington has reduced.
Considering the health related behaviours and individual lifestyle factor:
Smoking rates have decreased as compared to the average for England.
The percentage of women smoking during the pregnancy is low in the cited city.
Since 2004, number of people cycling in Warrington has increased (Strategic
Commissioning plan, 2015).
There are several areas where still there is need of improvement for the Warrington:
Population Deprivation
9
overall vision of the cited firm. However, development of these objectives are based on the
followed structure which is incorporated with feedbacks from associated stakeholders. Further,
these objectives are denoted as “Planning for Patients”.
Improving the healthy life expectancy for the people of England.
Minimizing or reducing the inequalities at the time of providing services.
To encourage all the commissioned services in order to support delivery of the NHS
constitution for the entire population (Transforming Primary Care in London: A
Strategic Commissioning Framework, 2015).
Constantly improving the quality of commissioned.
Attaining sustainable financial balance.
Developing and maintaining highly effective and motivated workforce.
Making sure that sound governance arrangements are in place.
Promoting the incorporation of proper integration of commissioned services.
PRIORITIES FOR NHS ENGLAND
Priorities are essential in order to illustrate the important of work or activities. Herein,
priorities for NHS England sets out the factors that are driving the plan for change or
modifications within the healthcare of Warrington. There are several areas of health in which
Warrington is doing relatively well or improving at good rate.
On the basis of health outcomes and impact of major diseases:
Life expectancy of cited place is increasing as the gap between Warrington and England
is decreasing especially in context to males.
Along with this, internal inequalities gap in life expectancy has decreased in the town.
The death rate in affluent areas of Warrington has reduced.
Considering the health related behaviours and individual lifestyle factor:
Smoking rates have decreased as compared to the average for England.
The percentage of women smoking during the pregnancy is low in the cited city.
Since 2004, number of people cycling in Warrington has increased (Strategic
Commissioning plan, 2015).
There are several areas where still there is need of improvement for the Warrington:
Population Deprivation
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 22
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





