Surgical Site Infection: Intervention and Outcome Analysis Report
VerifiedAdded on 2021/06/17
|13
|3162
|58
Report
AI Summary
This report examines surgical site infections (SSIs), their impact on healthcare, and effective interventions. It presents a PICO question focusing on glycemic and hypothermia management to reduce SSI risks in surgical patients. The methodology involves a review of secondary databases like Google Scholar and PubMed, analyzing research and non-research articles published within the last 10-12 years. Key findings highlight the importance of glycemic control and normothermia. The report recommends implementing glycemic and hypothermia management strategies, involving key stakeholders such as surgeons, anesthesiologists, and infection control staff. It addresses potential barriers, including behavioral factors and surgical skill, and suggests strategies to overcome them. The report aims to provide evidence-based recommendations to improve surgical care and reduce the incidence of SSIs.

Running head: SURGICAL SITE INFECTION
SURGICAL SITE INFECTION
Name of the student:
Name of the University:
Author note:
SURGICAL SITE INFECTION
Name of the student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
SURGICAL SITE INFECTIONS
Background of Surgical site infection:
The current study focuses upon the aspect of surgical site infections (SSIs) and the
overall impact produce by it on the present healthcare system. The infections occur at the site
of surgery due to exposure to pathogens. The pathogens to which an individual in exposed
over here consists of bacteria and methicillin resistant Staphylococcus aureus. It have been
noted that atleast 5-11% of the people undergoing surgeries are the under the fear of
developing surgical site infections (Carvalho et al., 2017). The severity of the infections may
range from simple wound discharge to development of pressure ulcers. In the present context,
high rates of central line associated blood stream infections (CLABSI) have been seen to
occur which has resulted in increased care burden for the hospital.
The centre for Disease control have found out that in the year 2011 itself there were
157,500 cases of surgical site infections. Between 2006-2008, 16,147 SSIs were noted
following 849,659 operative procedures (Donovan et al., 2016). The CLABSI are seen to
occur at the rate of 0.8 per 1000 patients admitted and have been seen to significantly
increase the number of hospital stay days. It has been noted that in 75% of the complications
arising out of surgical site infections the patient has faced near death experience (Mimoz et
al., 2015). Some of the effective procedures which have been implemented within the
present context are active documentation along with provision of sufficient training to the
healthcare professionals looking after the patient within the intensive care units.
As suggested by Semple et al. (2015), the surgical site infection has been seen to
increase the number of hospital inpatient days along with high rates of readmission. A limited
infrastructural setup has been seen to make accommodation and treatment availability
difficult. The culturally and linguistically different background has been seen to influence the
relationship that exists between the patient and the healthcare professionals. As mentioned by
SURGICAL SITE INFECTIONS
Background of Surgical site infection:
The current study focuses upon the aspect of surgical site infections (SSIs) and the
overall impact produce by it on the present healthcare system. The infections occur at the site
of surgery due to exposure to pathogens. The pathogens to which an individual in exposed
over here consists of bacteria and methicillin resistant Staphylococcus aureus. It have been
noted that atleast 5-11% of the people undergoing surgeries are the under the fear of
developing surgical site infections (Carvalho et al., 2017). The severity of the infections may
range from simple wound discharge to development of pressure ulcers. In the present context,
high rates of central line associated blood stream infections (CLABSI) have been seen to
occur which has resulted in increased care burden for the hospital.
The centre for Disease control have found out that in the year 2011 itself there were
157,500 cases of surgical site infections. Between 2006-2008, 16,147 SSIs were noted
following 849,659 operative procedures (Donovan et al., 2016). The CLABSI are seen to
occur at the rate of 0.8 per 1000 patients admitted and have been seen to significantly
increase the number of hospital stay days. It has been noted that in 75% of the complications
arising out of surgical site infections the patient has faced near death experience (Mimoz et
al., 2015). Some of the effective procedures which have been implemented within the
present context are active documentation along with provision of sufficient training to the
healthcare professionals looking after the patient within the intensive care units.
As suggested by Semple et al. (2015), the surgical site infection has been seen to
increase the number of hospital inpatient days along with high rates of readmission. A limited
infrastructural setup has been seen to make accommodation and treatment availability
difficult. The culturally and linguistically different background has been seen to influence the
relationship that exists between the patient and the healthcare professionals. As mentioned by
2
SURGICAL SITE INFECTIONS
Tuuli et al. (2016), the communication gap which often arises within a multilingual
healthcare setup have been seen to affect the end quality of the treatment.
The assignment focuses to identify effective intervention to control the surgical site
infection to reduce the prevalence in an effective manner. In this regards the paper will
develop PICO question and identify relevant evidences to provide a proper recommendation
to address the PICO question. The following paper will also provide the implementation
process of the recommendation, strategy to involve stakeholders, barriers in the process of
implementation and process to measure the outcomes.
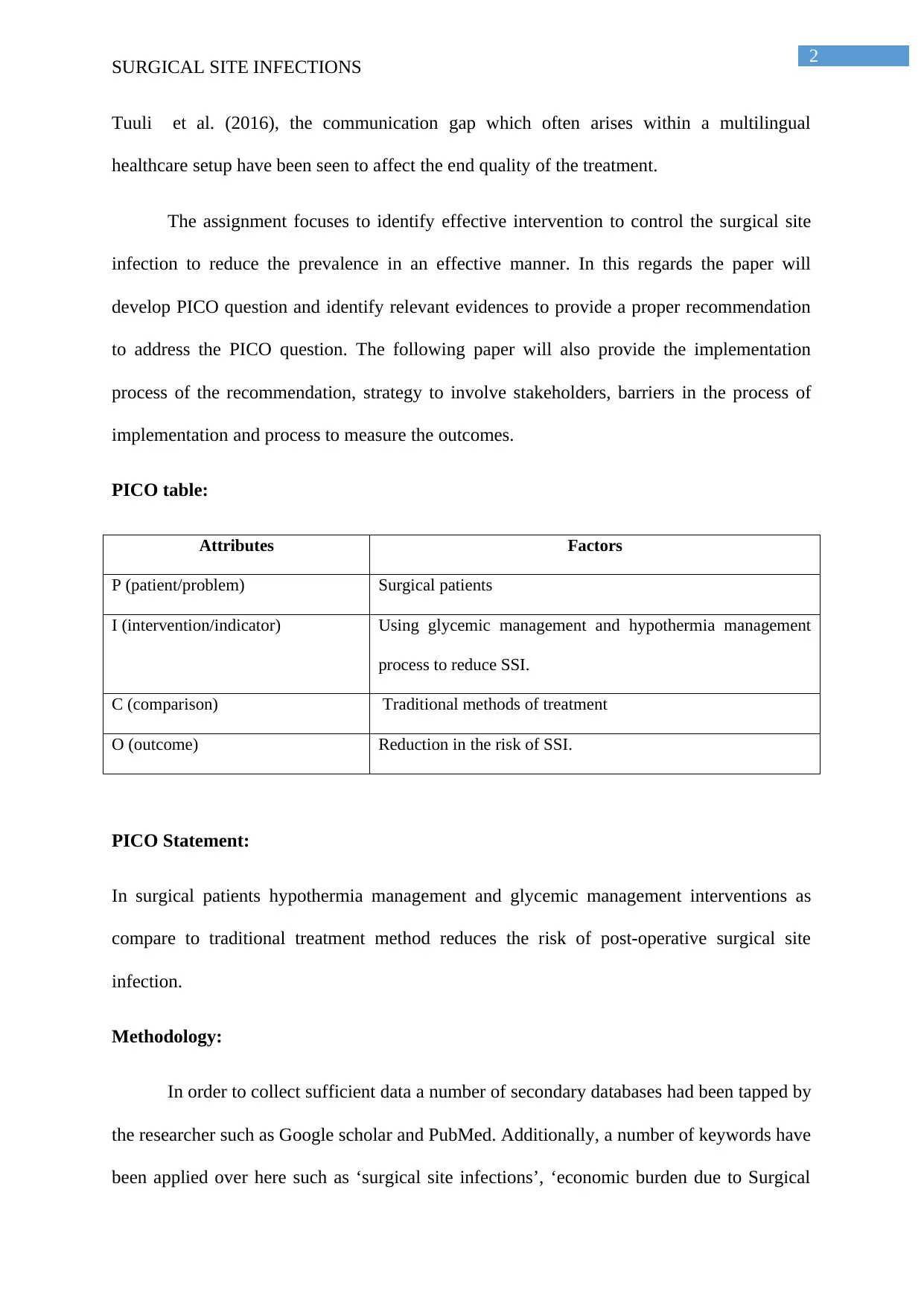
PICO table:
Attributes Factors
P (patient/problem) Surgical patients
I (intervention/indicator) Using glycemic management and hypothermia management
process to reduce SSI.
C (comparison) Traditional methods of treatment
O (outcome) Reduction in the risk of SSI.
PICO Statement:
In surgical patients hypothermia management and glycemic management interventions as
compare to traditional treatment method reduces the risk of post-operative surgical site
infection.
Methodology:
In order to collect sufficient data a number of secondary databases had been tapped by
the researcher such as Google scholar and PubMed. Additionally, a number of keywords have
been applied over here such as ‘surgical site infections’, ‘economic burden due to Surgical
SURGICAL SITE INFECTIONS
Tuuli et al. (2016), the communication gap which often arises within a multilingual
healthcare setup have been seen to affect the end quality of the treatment.
The assignment focuses to identify effective intervention to control the surgical site
infection to reduce the prevalence in an effective manner. In this regards the paper will
develop PICO question and identify relevant evidences to provide a proper recommendation
to address the PICO question. The following paper will also provide the implementation
process of the recommendation, strategy to involve stakeholders, barriers in the process of
implementation and process to measure the outcomes.
PICO table:
Attributes Factors
P (patient/problem) Surgical patients
I (intervention/indicator) Using glycemic management and hypothermia management
process to reduce SSI.
C (comparison) Traditional methods of treatment
O (outcome) Reduction in the risk of SSI.
PICO Statement:
In surgical patients hypothermia management and glycemic management interventions as
compare to traditional treatment method reduces the risk of post-operative surgical site
infection.
Methodology:
In order to collect sufficient data a number of secondary databases had been tapped by
the researcher such as Google scholar and PubMed. Additionally, a number of keywords have
been applied over here such as ‘surgical site infections’, ‘economic burden due to Surgical
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
SURGICAL SITE INFECTIONS
site infections’, ‘health implications of surgical site infections’. Therefore, apart from the
keywords which have been used over here, no additional searches have been taken into
consideration. The articles which have been published within the last 10-12 years only have
been taken into consideration. From 15 odd articles, four research based articles (level I) and
three non-research based articles (two articles- level IV and one article- level VII) have been
further taken into consideration for the purpose of evaluation. From the selected articles two
research articles and two non-research articles are described here.
Research asrticles:
1.Domingos, C., Iida, L., & Poveda, V. (2016). Glycemic control strategies and the
occurrence of surgical site infection: a systematic review. Revista Da Escola De Enfermagem
Da USP, 50(5), 868-874. doi: 10.1590/s0080-623420160000600022
The researchers have used systemic review of 8 relevant studies to answer the
research articles. Continuous infusion of insulin during surgery to control glycaemia has been
measured by the researchers and it has been identified that controlling glycaemia is one of the
most effective interventions to reduce the risk of SSI in surgical patients.
2.Sessler, D. I. (2016). Perioperative thermoregulation and heat balance. The
Lancet, 387(10038), 2655-2664.
The researchers have used systemic review and reviewed previous literatures from
MEDLINE published within 2000 to 2014. Thermoregulation and heat balance during
perioperative period. It has been found that hypothermia may leads to the risk of surgical
complication, thus core temperature need to be monitored during anesthesia and patient need
to be kept normothermic in order to reduce the risk of surgical site infection.
Non-research articles:
SURGICAL SITE INFECTIONS
site infections’, ‘health implications of surgical site infections’. Therefore, apart from the
keywords which have been used over here, no additional searches have been taken into
consideration. The articles which have been published within the last 10-12 years only have
been taken into consideration. From 15 odd articles, four research based articles (level I) and
three non-research based articles (two articles- level IV and one article- level VII) have been
further taken into consideration for the purpose of evaluation. From the selected articles two
research articles and two non-research articles are described here.
Research asrticles:
1.Domingos, C., Iida, L., & Poveda, V. (2016). Glycemic control strategies and the
occurrence of surgical site infection: a systematic review. Revista Da Escola De Enfermagem
Da USP, 50(5), 868-874. doi: 10.1590/s0080-623420160000600022
The researchers have used systemic review of 8 relevant studies to answer the
research articles. Continuous infusion of insulin during surgery to control glycaemia has been
measured by the researchers and it has been identified that controlling glycaemia is one of the
most effective interventions to reduce the risk of SSI in surgical patients.
2.Sessler, D. I. (2016). Perioperative thermoregulation and heat balance. The
Lancet, 387(10038), 2655-2664.
The researchers have used systemic review and reviewed previous literatures from
MEDLINE published within 2000 to 2014. Thermoregulation and heat balance during
perioperative period. It has been found that hypothermia may leads to the risk of surgical
complication, thus core temperature need to be monitored during anesthesia and patient need
to be kept normothermic in order to reduce the risk of surgical site infection.
Non-research articles:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
SURGICAL SITE INFECTIONS
1. Sadoskas, D., Suder, N., & Wukich, D. (2015). Perioperative Glycemic Control and the
Effect on Surgical Site Infections in Diabetic Patients Undergoing Foot and Ankle Surgery.
Foot & Ankle Specialist, 9(1), 24-30. doi: 10.1177/1938640015593077
The researchers have used retrospective study 348 patients with foot and ankle
surgery were selected for evaluation. Patients with high glucose level and low glucose level
have been measured. It has been recognized that one of the risk factors of SSI is preoperative
glycaemia and glycemic management could help to reduce the risk of SSI in an effective
manner.
2.Kotagal, M., Symons, R., Hirsch, I., Umpierrez, G., Dellinger, E., Farrokhi, E., & Flum, D.
(2015). Perioperative Hyperglycemia and Risk of Adverse Events Among Patients With and
Without Diabetes. Annals Of Surgery, 261(1), 97-103. doi: 10.1097/sla.0000000000000688
The researchers have used cohort study and recruited 40386 patients. Evaluation of
diabetes, periopoerative hyperglycemia associated with adverse surgical event has been done
to derive the conclusion. It has been found that risk of adverse surgical event is associated
with hyperglycemia and this is may be due to underuse of insulin.
SURGICAL SITE INFECTIONS
1. Sadoskas, D., Suder, N., & Wukich, D. (2015). Perioperative Glycemic Control and the
Effect on Surgical Site Infections in Diabetic Patients Undergoing Foot and Ankle Surgery.
Foot & Ankle Specialist, 9(1), 24-30. doi: 10.1177/1938640015593077
The researchers have used retrospective study 348 patients with foot and ankle
surgery were selected for evaluation. Patients with high glucose level and low glucose level
have been measured. It has been recognized that one of the risk factors of SSI is preoperative
glycaemia and glycemic management could help to reduce the risk of SSI in an effective
manner.
2.Kotagal, M., Symons, R., Hirsch, I., Umpierrez, G., Dellinger, E., Farrokhi, E., & Flum, D.
(2015). Perioperative Hyperglycemia and Risk of Adverse Events Among Patients With and
Without Diabetes. Annals Of Surgery, 261(1), 97-103. doi: 10.1097/sla.0000000000000688
The researchers have used cohort study and recruited 40386 patients. Evaluation of
diabetes, periopoerative hyperglycemia associated with adverse surgical event has been done
to derive the conclusion. It has been found that risk of adverse surgical event is associated
with hyperglycemia and this is may be due to underuse of insulin.
5
SURGICAL SITE INFECTIONS
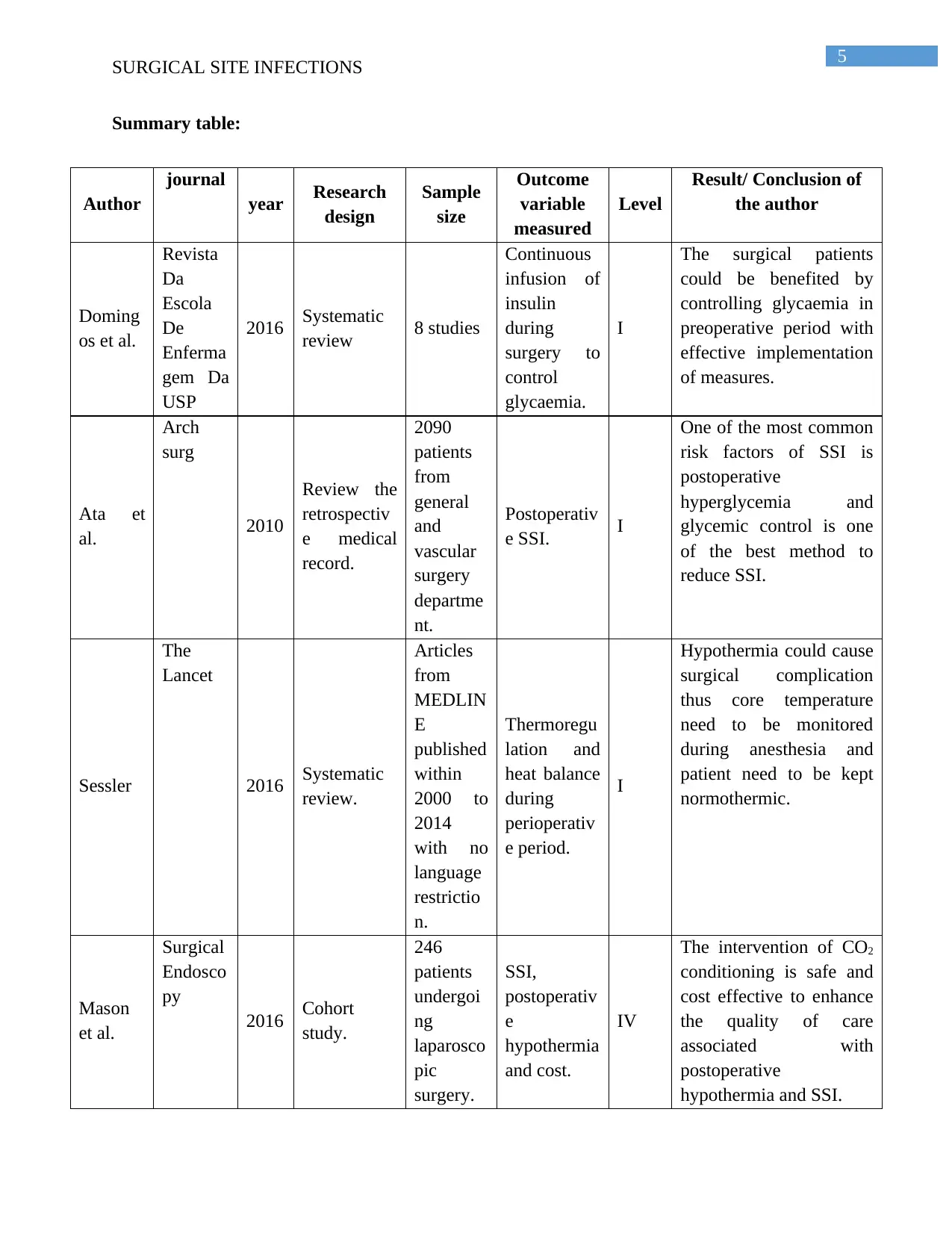
Summary table:
Author
journal
year Research
design
Sample
size
Outcome
variable
measured
Level
Result/ Conclusion of
the author
Doming
os et al.
Revista
Da
Escola
De
Enferma
gem Da
USP
2016 Systematic
review 8 studies
Continuous
infusion of
insulin
during
surgery to
control
glycaemia.
I
The surgical patients
could be benefited by
controlling glycaemia in
preoperative period with
effective implementation
of measures.
Ata et
al.
Arch
surg
2010
Review the
retrospectiv
e medical
record.
2090
patients
from
general
and
vascular
surgery
departme
nt.
Postoperativ
e SSI. I
One of the most common
risk factors of SSI is
postoperative
hyperglycemia and
glycemic control is one
of the best method to
reduce SSI.
Sessler
The
Lancet
2016 Systematic
review.
Articles
from
MEDLIN
E
published
within
2000 to
2014
with no
language
restrictio
n.
Thermoregu
lation and
heat balance
during
perioperativ
e period.
I
Hypothermia could cause
surgical complication
thus core temperature
need to be monitored
during anesthesia and
patient need to be kept
normothermic.
Mason
et al.
Surgical
Endosco
py
2016 Cohort
study.
246
patients
undergoi
ng
laparosco
pic
surgery.
SSI,
postoperativ
e
hypothermia
and cost.
IV
The intervention of CO2
conditioning is safe and
cost effective to enhance
the quality of care
associated with
postoperative
hypothermia and SSI.
SURGICAL SITE INFECTIONS
Summary table:
Author
journal
year Research
design
Sample
size
Outcome
variable
measured
Level
Result/ Conclusion of
the author
Doming
os et al.
Revista
Da
Escola
De
Enferma
gem Da
USP
2016 Systematic
review 8 studies
Continuous
infusion of
insulin
during
surgery to
control
glycaemia.
I
The surgical patients
could be benefited by
controlling glycaemia in
preoperative period with
effective implementation
of measures.
Ata et
al.
Arch
surg
2010
Review the
retrospectiv
e medical
record.
2090
patients
from
general
and
vascular
surgery
departme
nt.
Postoperativ
e SSI. I
One of the most common
risk factors of SSI is
postoperative
hyperglycemia and
glycemic control is one
of the best method to
reduce SSI.
Sessler
The
Lancet
2016 Systematic
review.
Articles
from
MEDLIN
E
published
within
2000 to
2014
with no
language
restrictio
n.
Thermoregu
lation and
heat balance
during
perioperativ
e period.
I
Hypothermia could cause
surgical complication
thus core temperature
need to be monitored
during anesthesia and
patient need to be kept
normothermic.
Mason
et al.
Surgical
Endosco
py
2016 Cohort
study.
246
patients
undergoi
ng
laparosco
pic
surgery.
SSI,
postoperativ
e
hypothermia
and cost.
IV
The intervention of CO2
conditioning is safe and
cost effective to enhance
the quality of care
associated with
postoperative
hypothermia and SSI.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
SURGICAL SITE INFECTIONS
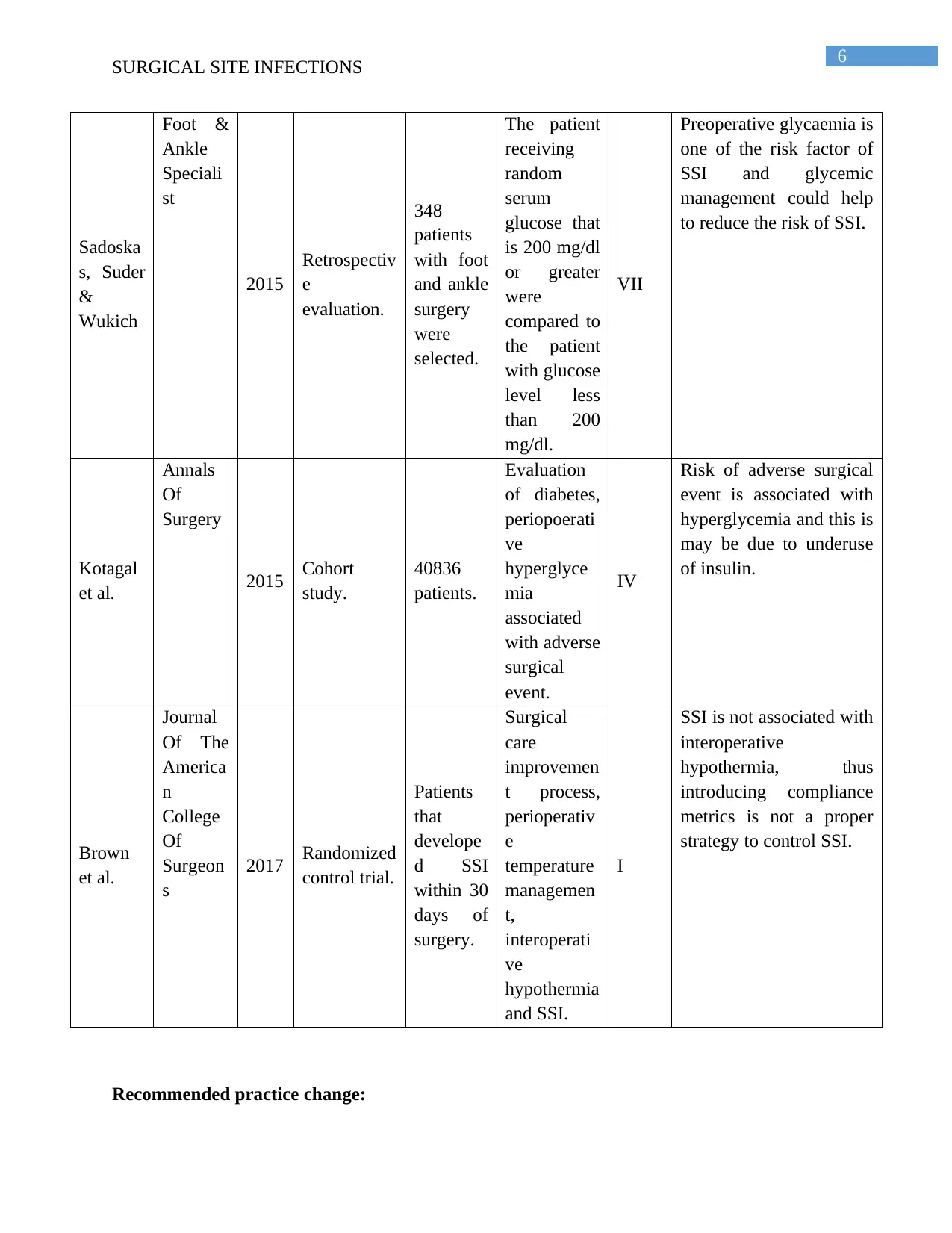
Sadoska
s, Suder
&
Wukich
Foot &
Ankle
Speciali
st
2015
Retrospectiv
e
evaluation.
348
patients
with foot
and ankle
surgery
were
selected.
The patient
receiving
random
serum
glucose that
is 200 mg/dl
or greater
were
compared to
the patient
with glucose
level less
than 200
mg/dl.
VII
Preoperative glycaemia is
one of the risk factor of
SSI and glycemic
management could help
to reduce the risk of SSI.
Kotagal
et al.
Annals
Of
Surgery
2015 Cohort
study.
40836
patients.
Evaluation
of diabetes,
periopoerati
ve
hyperglyce
mia
associated
with adverse
surgical
event.
IV
Risk of adverse surgical
event is associated with
hyperglycemia and this is
may be due to underuse
of insulin.
Brown
et al.
Journal
Of The
America
n
College
Of
Surgeon
s
2017 Randomized
control trial.
Patients
that
develope
d SSI
within 30
days of
surgery.
Surgical
care
improvemen
t process,
perioperativ
e
temperature
managemen
t,
interoperati
ve
hypothermia
and SSI.
I
SSI is not associated with
interoperative
hypothermia, thus
introducing compliance
metrics is not a proper
strategy to control SSI.
Recommended practice change:
SURGICAL SITE INFECTIONS
Sadoska
s, Suder
&
Wukich
Foot &
Ankle
Speciali
st
2015
Retrospectiv
e
evaluation.
348
patients
with foot
and ankle
surgery
were
selected.
The patient
receiving
random
serum
glucose that
is 200 mg/dl
or greater
were
compared to
the patient
with glucose
level less
than 200
mg/dl.
VII
Preoperative glycaemia is
one of the risk factor of
SSI and glycemic
management could help
to reduce the risk of SSI.
Kotagal
et al.
Annals
Of
Surgery
2015 Cohort
study.
40836
patients.
Evaluation
of diabetes,
periopoerati
ve
hyperglyce
mia
associated
with adverse
surgical
event.
IV
Risk of adverse surgical
event is associated with
hyperglycemia and this is
may be due to underuse
of insulin.
Brown
et al.
Journal
Of The
America
n
College
Of
Surgeon
s
2017 Randomized
control trial.
Patients
that
develope
d SSI
within 30
days of
surgery.
Surgical
care
improvemen
t process,
perioperativ
e
temperature
managemen
t,
interoperati
ve
hypothermia
and SSI.
I
SSI is not associated with
interoperative
hypothermia, thus
introducing compliance
metrics is not a proper
strategy to control SSI.
Recommended practice change:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
SURGICAL SITE INFECTIONS
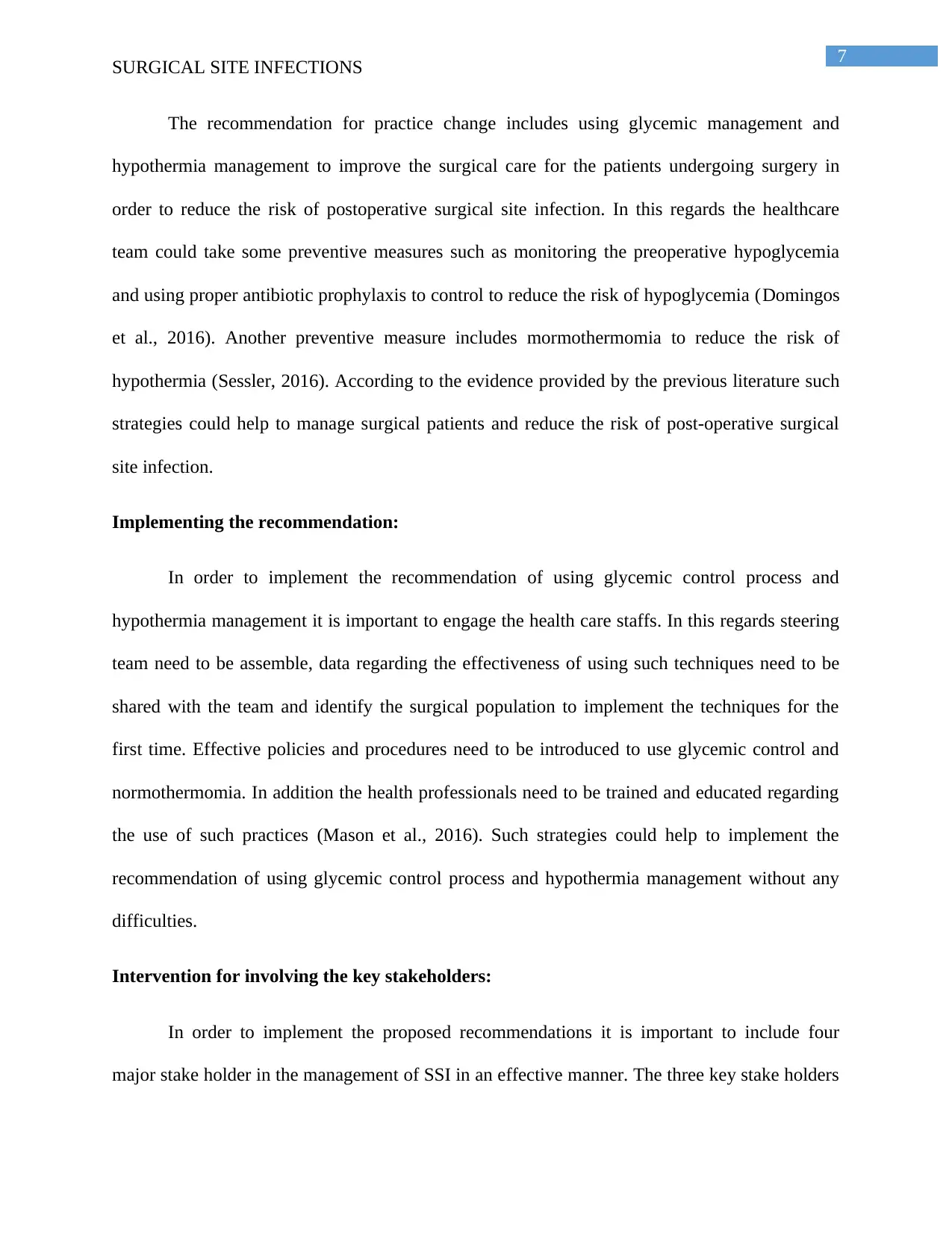
The recommendation for practice change includes using glycemic management and
hypothermia management to improve the surgical care for the patients undergoing surgery in
order to reduce the risk of postoperative surgical site infection. In this regards the healthcare
team could take some preventive measures such as monitoring the preoperative hypoglycemia
and using proper antibiotic prophylaxis to control to reduce the risk of hypoglycemia (Domingos
et al., 2016). Another preventive measure includes mormothermomia to reduce the risk of
hypothermia (Sessler, 2016). According to the evidence provided by the previous literature such
strategies could help to manage surgical patients and reduce the risk of post-operative surgical
site infection.
Implementing the recommendation:
In order to implement the recommendation of using glycemic control process and
hypothermia management it is important to engage the health care staffs. In this regards steering
team need to be assemble, data regarding the effectiveness of using such techniques need to be
shared with the team and identify the surgical population to implement the techniques for the
first time. Effective policies and procedures need to be introduced to use glycemic control and
normothermomia. In addition the health professionals need to be trained and educated regarding
the use of such practices (Mason et al., 2016). Such strategies could help to implement the
recommendation of using glycemic control process and hypothermia management without any
difficulties.
Intervention for involving the key stakeholders:
In order to implement the proposed recommendations it is important to include four
major stake holder in the management of SSI in an effective manner. The three key stake holders
SURGICAL SITE INFECTIONS
The recommendation for practice change includes using glycemic management and
hypothermia management to improve the surgical care for the patients undergoing surgery in
order to reduce the risk of postoperative surgical site infection. In this regards the healthcare
team could take some preventive measures such as monitoring the preoperative hypoglycemia
and using proper antibiotic prophylaxis to control to reduce the risk of hypoglycemia (Domingos
et al., 2016). Another preventive measure includes mormothermomia to reduce the risk of
hypothermia (Sessler, 2016). According to the evidence provided by the previous literature such
strategies could help to manage surgical patients and reduce the risk of post-operative surgical
site infection.
Implementing the recommendation:
In order to implement the recommendation of using glycemic control process and
hypothermia management it is important to engage the health care staffs. In this regards steering
team need to be assemble, data regarding the effectiveness of using such techniques need to be
shared with the team and identify the surgical population to implement the techniques for the
first time. Effective policies and procedures need to be introduced to use glycemic control and
normothermomia. In addition the health professionals need to be trained and educated regarding
the use of such practices (Mason et al., 2016). Such strategies could help to implement the
recommendation of using glycemic control process and hypothermia management without any
difficulties.
Intervention for involving the key stakeholders:
In order to implement the proposed recommendations it is important to include four
major stake holder in the management of SSI in an effective manner. The three key stake holders
8
SURGICAL SITE INFECTIONS
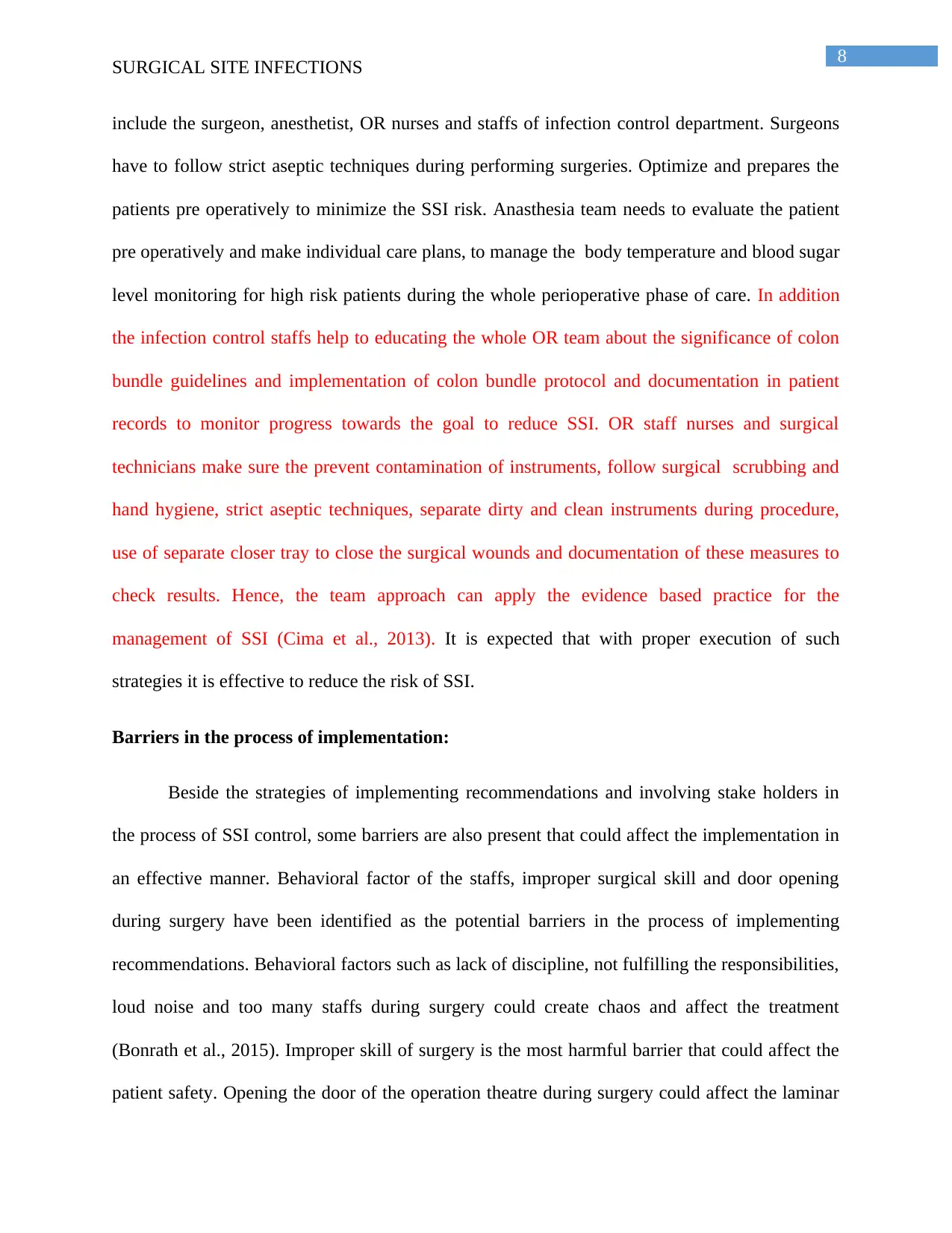
include the surgeon, anesthetist, OR nurses and staffs of infection control department. Surgeons
have to follow strict aseptic techniques during performing surgeries. Optimize and prepares the
patients pre operatively to minimize the SSI risk. Anasthesia team needs to evaluate the patient
pre operatively and make individual care plans, to manage the body temperature and blood sugar
level monitoring for high risk patients during the whole perioperative phase of care. In addition
the infection control staffs help to educating the whole OR team about the significance of colon
bundle guidelines and implementation of colon bundle protocol and documentation in patient
records to monitor progress towards the goal to reduce SSI. OR staff nurses and surgical
technicians make sure the prevent contamination of instruments, follow surgical scrubbing and
hand hygiene, strict aseptic techniques, separate dirty and clean instruments during procedure,
use of separate closer tray to close the surgical wounds and documentation of these measures to
check results. Hence, the team approach can apply the evidence based practice for the
management of SSI (Cima et al., 2013). It is expected that with proper execution of such
strategies it is effective to reduce the risk of SSI.
Barriers in the process of implementation:
Beside the strategies of implementing recommendations and involving stake holders in
the process of SSI control, some barriers are also present that could affect the implementation in
an effective manner. Behavioral factor of the staffs, improper surgical skill and door opening
during surgery have been identified as the potential barriers in the process of implementing
recommendations. Behavioral factors such as lack of discipline, not fulfilling the responsibilities,
loud noise and too many staffs during surgery could create chaos and affect the treatment
(Bonrath et al., 2015). Improper skill of surgery is the most harmful barrier that could affect the
patient safety. Opening the door of the operation theatre during surgery could affect the laminar
SURGICAL SITE INFECTIONS
include the surgeon, anesthetist, OR nurses and staffs of infection control department. Surgeons
have to follow strict aseptic techniques during performing surgeries. Optimize and prepares the
patients pre operatively to minimize the SSI risk. Anasthesia team needs to evaluate the patient
pre operatively and make individual care plans, to manage the body temperature and blood sugar
level monitoring for high risk patients during the whole perioperative phase of care. In addition
the infection control staffs help to educating the whole OR team about the significance of colon
bundle guidelines and implementation of colon bundle protocol and documentation in patient
records to monitor progress towards the goal to reduce SSI. OR staff nurses and surgical
technicians make sure the prevent contamination of instruments, follow surgical scrubbing and
hand hygiene, strict aseptic techniques, separate dirty and clean instruments during procedure,
use of separate closer tray to close the surgical wounds and documentation of these measures to
check results. Hence, the team approach can apply the evidence based practice for the
management of SSI (Cima et al., 2013). It is expected that with proper execution of such
strategies it is effective to reduce the risk of SSI.
Barriers in the process of implementation:
Beside the strategies of implementing recommendations and involving stake holders in
the process of SSI control, some barriers are also present that could affect the implementation in
an effective manner. Behavioral factor of the staffs, improper surgical skill and door opening
during surgery have been identified as the potential barriers in the process of implementing
recommendations. Behavioral factors such as lack of discipline, not fulfilling the responsibilities,
loud noise and too many staffs during surgery could create chaos and affect the treatment
(Bonrath et al., 2015). Improper skill of surgery is the most harmful barrier that could affect the
patient safety. Opening the door of the operation theatre during surgery could affect the laminar
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
SURGICAL SITE INFECTIONS
air flow and facilitate the entry of pathogens thus, could increase the risk of infection (Koehler et
al., 2013).
Strategies to overcome the barriers:
Proper education and training regarding surgery management need to be provided to the
clinicians and other staffs. Policies and procedure regarding maintain rules and disciplines need
to be introduced. Allowing required staffs only during surgery to minimize the chaos is
important. Finally, involving highly skilled surgeon that have the knowledge of handling tissue
appropriately need to be appointed to reduce the effect of the barriers (Bonrath et al., 2015).
Indicator to measure the outcome:
In order to measure the outcome it is important to monitor the colorectal or other
infections rate ones in a month. Proper documentation of data collected from monitoring process.
It is required to share the data with forum and wider nursing team. Collecting the staff input is
also important to identify the area of development (Semple et al., 2015). Such process could help
to evaluate the outcome in an effective manner.
SURGICAL SITE INFECTIONS
air flow and facilitate the entry of pathogens thus, could increase the risk of infection (Koehler et
al., 2013).
Strategies to overcome the barriers:
Proper education and training regarding surgery management need to be provided to the
clinicians and other staffs. Policies and procedure regarding maintain rules and disciplines need
to be introduced. Allowing required staffs only during surgery to minimize the chaos is
important. Finally, involving highly skilled surgeon that have the knowledge of handling tissue
appropriately need to be appointed to reduce the effect of the barriers (Bonrath et al., 2015).
Indicator to measure the outcome:
In order to measure the outcome it is important to monitor the colorectal or other
infections rate ones in a month. Proper documentation of data collected from monitoring process.
It is required to share the data with forum and wider nursing team. Collecting the staff input is
also important to identify the area of development (Semple et al., 2015). Such process could help
to evaluate the outcome in an effective manner.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
SURGICAL SITE INFECTIONS
References:
Ata, A., Lee, J., Bestle, S., Desemone, J., & Stain, S. (2010). Postoperative Hyperglycemia and
Surgical Site Infection in General Surgery Patients. Arch Surg, 145(9), 858-864.
Bonrath, E. M., Dedy, N. J., Gordon, L. E., & Grantcharov, T. P. (2015). Comprehensive
surgical coaching enhances surgical skill in the operating room. Annals of surgery, 262(2), 205-
212.
Brown, M., Curry, T., Hyder, J., Berbari, E., Truty, M., & Schroeder, D. et al. (2017).
Intraoperative Hypothermia and Surgical Site Infections in Patients with Class I/Clean Wounds:
A Case-Control Study. Journal Of The American College Of Surgeons, 224(2), 160-171. doi:
10.1016/j.jamcollsurg.2016.10.050
Carvalho, R. L. R. D., Campos, C. C., Franco, L. M. D. C., Rocha, A. D. M., & Ercole, F. F.
(2017). Incidence and risk factors for surgical site infection in general surgeries. Revista latino-
americana de enfermagem, 25.
Cima, R., Dankbar, E., Lovely, J., Pendlimari, R., Aronhalt, K., Nehring, S., ... & Team, C. S. S.
I. R. (2013). Colorectal surgery surgical site infection reduction program: a national surgical
quality improvement program–driven multidisciplinary single-institution experience. Journal of
the American College of Surgeons, 216(1), 23-33.
Domingos, C., Iida, L., & Poveda, V. (2016). Glycemic control strategies and the occurrence of
surgical site infection: a systematic review. Revista Da Escola De Enfermagem Da USP, 50(5),
868-874. doi: 10.1590/s0080-623420160000600022
SURGICAL SITE INFECTIONS
References:
Ata, A., Lee, J., Bestle, S., Desemone, J., & Stain, S. (2010). Postoperative Hyperglycemia and
Surgical Site Infection in General Surgery Patients. Arch Surg, 145(9), 858-864.
Bonrath, E. M., Dedy, N. J., Gordon, L. E., & Grantcharov, T. P. (2015). Comprehensive
surgical coaching enhances surgical skill in the operating room. Annals of surgery, 262(2), 205-
212.
Brown, M., Curry, T., Hyder, J., Berbari, E., Truty, M., & Schroeder, D. et al. (2017).
Intraoperative Hypothermia and Surgical Site Infections in Patients with Class I/Clean Wounds:
A Case-Control Study. Journal Of The American College Of Surgeons, 224(2), 160-171. doi:
10.1016/j.jamcollsurg.2016.10.050
Carvalho, R. L. R. D., Campos, C. C., Franco, L. M. D. C., Rocha, A. D. M., & Ercole, F. F.
(2017). Incidence and risk factors for surgical site infection in general surgeries. Revista latino-
americana de enfermagem, 25.
Cima, R., Dankbar, E., Lovely, J., Pendlimari, R., Aronhalt, K., Nehring, S., ... & Team, C. S. S.
I. R. (2013). Colorectal surgery surgical site infection reduction program: a national surgical
quality improvement program–driven multidisciplinary single-institution experience. Journal of
the American College of Surgeons, 216(1), 23-33.
Domingos, C., Iida, L., & Poveda, V. (2016). Glycemic control strategies and the occurrence of
surgical site infection: a systematic review. Revista Da Escola De Enfermagem Da USP, 50(5),
868-874. doi: 10.1590/s0080-623420160000600022
11
SURGICAL SITE INFECTIONS
Koehler, R. J., Amsdell, S., Arendt, E. A., Bisson, L. J., Bramen, J. P., Butler, A., ... & Warme,
W. J. (2013). The arthroscopic surgical skill evaluation tool (ASSET). The American journal of
sports medicine, 41(6), 1229-1237.
Kotagal, M., Symons, R., Hirsch, I., Umpierrez, G., Dellinger, E., Farrokhi, E., & Flum, D.
(2015). Perioperative Hyperglycemia and Risk of Adverse Events Among Patients With and
Without Diabetes. Annals Of Surgery, 261(1), 97-103. doi: 10.1097/sla.0000000000000688
Mason, S., Kinross, J., Hendricks, J., & Arulampalam, T. (2016). Postoperative hypothermia and
surgical site infection following peritoneal insufflation with warm, humidified carbon dioxide
during laparoscopic colorectal surgery: a cohort study with cost-effectiveness analysis. Surgical
Endoscopy, 31(4), 1923-1929. doi: 10.1007/s00464-016-5195-0
Mimoz, O., Lucet, J. C., Kerforne, T., Pascal, J., Souweine, B., Goudet, V., ... & Friggeri, A.
(2015). Skin antisepsis with chlorhexidine–alcohol versus povidone iodine–alcohol, with and
without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an
open-label, multicentre, randomised, controlled, two-by-two factorial trial. The
Lancet, 386(10008), 2069-2077.
Sadoskas, D., Suder, N., & Wukich, D. (2015). Perioperative Glycemic Control and the Effect on
Surgical Site Infections in Diabetic Patients Undergoing Foot and Ankle Surgery. Foot & Ankle
Specialist, 9(1), 24-30. doi: 10.1177/1938640015593077
Semple, J. L., Sharpe, S., Murnaghan, M. L., Theodoropoulos, J., & Metcalfe, K. A. (2015).
Using a mobile app for monitoring post-operative quality of recovery of patients at home: a
feasibility study. JMIR mHealth and uHealth, 3(1).
SURGICAL SITE INFECTIONS
Koehler, R. J., Amsdell, S., Arendt, E. A., Bisson, L. J., Bramen, J. P., Butler, A., ... & Warme,
W. J. (2013). The arthroscopic surgical skill evaluation tool (ASSET). The American journal of
sports medicine, 41(6), 1229-1237.
Kotagal, M., Symons, R., Hirsch, I., Umpierrez, G., Dellinger, E., Farrokhi, E., & Flum, D.
(2015). Perioperative Hyperglycemia and Risk of Adverse Events Among Patients With and
Without Diabetes. Annals Of Surgery, 261(1), 97-103. doi: 10.1097/sla.0000000000000688
Mason, S., Kinross, J., Hendricks, J., & Arulampalam, T. (2016). Postoperative hypothermia and
surgical site infection following peritoneal insufflation with warm, humidified carbon dioxide
during laparoscopic colorectal surgery: a cohort study with cost-effectiveness analysis. Surgical
Endoscopy, 31(4), 1923-1929. doi: 10.1007/s00464-016-5195-0
Mimoz, O., Lucet, J. C., Kerforne, T., Pascal, J., Souweine, B., Goudet, V., ... & Friggeri, A.
(2015). Skin antisepsis with chlorhexidine–alcohol versus povidone iodine–alcohol, with and
without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an
open-label, multicentre, randomised, controlled, two-by-two factorial trial. The
Lancet, 386(10008), 2069-2077.
Sadoskas, D., Suder, N., & Wukich, D. (2015). Perioperative Glycemic Control and the Effect on
Surgical Site Infections in Diabetic Patients Undergoing Foot and Ankle Surgery. Foot & Ankle
Specialist, 9(1), 24-30. doi: 10.1177/1938640015593077
Semple, J. L., Sharpe, S., Murnaghan, M. L., Theodoropoulos, J., & Metcalfe, K. A. (2015).
Using a mobile app for monitoring post-operative quality of recovery of patients at home: a
feasibility study. JMIR mHealth and uHealth, 3(1).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




