An Analysis of Sweat-Based Nanoparticle Sensors in Healthcare
VerifiedAdded on 2020/04/21
|8
|1122
|53
Report
AI Summary
This report provides an overview of sweat-based nanoparticle sensors and their application in healthcare, focusing on their role in diagnosing chronic diseases. It discusses the increasing use of these biosensors for continuous monitoring of patients, highlighting the benefits of non-invasive methods compared to traditional blood tests. The report explores the technology behind these sensors, including the use of iontophoresis to stimulate sweat secretion and the flexible sensor and microprocessor systems used to analyze sweat composition. It reviews the methodology, including experimental setups to determine sensor performance, and concludes with the potential of sweat-based nanoparticle biosensors for improving patient care and health monitoring. Several key references are included, covering advancements in wearable chemical sensors, diagnostic guidelines, and correlation between sweat and blood glucose levels.

1
Name:
Course:
Professor:
Date:
Name:
Course:
Professor:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Sweat-based wearable diagnostic sensors from nanoparticle
Introduction
The use of sweat-based nanoparticle sensors has been in increase in the past decade. These
biosensors are used in the diagnosis of different chronic ailments. Some of the ailments
require continuous check of some key factors for the patients. These tests are sometimes
expensive and painful thus being considered stress intensive due to repetitive blood
collection1. This has led to researches on sweat-based nanoparticle biosensor to enhance the
diagnosis of the different ailments. This paper will look at the developments which have
taken place concerning sweat-based sensor and the way they have been able to help the
industry. The nanoparticle biosensors are used to enhance continuous monitoring of patients
health factors such as glucose content. The key process which is connected with the use of
the sweat-based wearable biosensors is the iontophoresis.
Literature review
In treatment of the chronic diseases, blood samples are mostly used. The drawing of the
blood is painful experience for the patients. Sweat-based wearable biosensors have been
developed to ensure continuous monitoring of health of the patients is done without the
painful experiences2. The sensors are able to allow measurement of different parameters such
as heart and respiratory rates or even blood pressure. The new sweat-based nanoparticle
biosensor is able to measure the composition of human sweat. These biosensors have two key
1 K. Takei W. Honda, S. Harada, T. Arie, and S. Akita, Toward flexible and wearable human-
interactive health-monitoring devices. Adv Healthc Mater 4(4), 2015, 487–500.
2 A.J. Bandodkar, and J. Wang Non-invasive wearable electrochemical sensors: a review
Trends Biotechnol., 32 (7), 2014, pp. 363-37
Sweat-based wearable diagnostic sensors from nanoparticle
Introduction
The use of sweat-based nanoparticle sensors has been in increase in the past decade. These
biosensors are used in the diagnosis of different chronic ailments. Some of the ailments
require continuous check of some key factors for the patients. These tests are sometimes
expensive and painful thus being considered stress intensive due to repetitive blood
collection1. This has led to researches on sweat-based nanoparticle biosensor to enhance the
diagnosis of the different ailments. This paper will look at the developments which have
taken place concerning sweat-based sensor and the way they have been able to help the
industry. The nanoparticle biosensors are used to enhance continuous monitoring of patients
health factors such as glucose content. The key process which is connected with the use of
the sweat-based wearable biosensors is the iontophoresis.
Literature review
In treatment of the chronic diseases, blood samples are mostly used. The drawing of the
blood is painful experience for the patients. Sweat-based wearable biosensors have been
developed to ensure continuous monitoring of health of the patients is done without the
painful experiences2. The sensors are able to allow measurement of different parameters such
as heart and respiratory rates or even blood pressure. The new sweat-based nanoparticle
biosensor is able to measure the composition of human sweat. These biosensors have two key
1 K. Takei W. Honda, S. Harada, T. Arie, and S. Akita, Toward flexible and wearable human-
interactive health-monitoring devices. Adv Healthc Mater 4(4), 2015, 487–500.
2 A.J. Bandodkar, and J. Wang Non-invasive wearable electrochemical sensors: a review
Trends Biotechnol., 32 (7), 2014, pp. 363-37
3
parts which include a system of flexible sensors and microprocessor3. These microprocessor
sticks on the skin and are able to stimulate the sweat glands and then detect the composition
of the sweat. Electrical signals are used to detect the molecules and ions which are present on
the sweat. The sweat-based diagnostic sensors can also be used for monitoring the health
conditions of patients, drug developments and drug personalization. The use of sweat-based
biosensors is a non-invasive monitoring method used for monitoring the health conditions of
patients4. The sweat-based diagnostic nanoparticle biosensors are able to detect body factors
such as glucose and pH of body through the sweat analysis. The major method which is used
to stimulate the sweat secretion for this process is the iontophoresis. Through the sweat
secretions, the sweat-based diagnostic biosensor is able to continuously monitor the body
metabolites and electrolyte.
Figure 1: An example of sweat-based nanoparticle biosensor5
Methodology
3 P. M. Farrell, et al. Diagnosis of cystic fibrosis: Consensus guidelines from the Cystic
Fibrosis Foundation. J Pediatr 181S:S4–S15, 2017, p. 15-22.
4 D. P. Rose, et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE
Trans Biomed Eng 62(6), 2015, p.1457.
5 A. J., Bandodkar, I, Jeerapan and J., Wang. Wearable chemical sensors: Present challenges
and future prospects. ACS Sens. 1:, 2016, 464–482.
parts which include a system of flexible sensors and microprocessor3. These microprocessor
sticks on the skin and are able to stimulate the sweat glands and then detect the composition
of the sweat. Electrical signals are used to detect the molecules and ions which are present on
the sweat. The sweat-based diagnostic sensors can also be used for monitoring the health
conditions of patients, drug developments and drug personalization. The use of sweat-based
biosensors is a non-invasive monitoring method used for monitoring the health conditions of
patients4. The sweat-based diagnostic nanoparticle biosensors are able to detect body factors
such as glucose and pH of body through the sweat analysis. The major method which is used
to stimulate the sweat secretion for this process is the iontophoresis. Through the sweat
secretions, the sweat-based diagnostic biosensor is able to continuously monitor the body
metabolites and electrolyte.
Figure 1: An example of sweat-based nanoparticle biosensor5
Methodology
3 P. M. Farrell, et al. Diagnosis of cystic fibrosis: Consensus guidelines from the Cystic
Fibrosis Foundation. J Pediatr 181S:S4–S15, 2017, p. 15-22.
4 D. P. Rose, et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE
Trans Biomed Eng 62(6), 2015, p.1457.
5 A. J., Bandodkar, I, Jeerapan and J., Wang. Wearable chemical sensors: Present challenges
and future prospects. ACS Sens. 1:, 2016, 464–482.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
In the experiment to determine the performance of sweat based wearable nanoparticle
biosensor, several materials will be used. First, a patient suffering from chronic disease such
as diabetes will be required. In this experiment, the patient will be monitored through the
sweat produced to determine different characteristics such as the glucose value. In addition,
another key factor which will be analysed in this experiment is the sensitivity and
effectiveness of the sweat-based nanoparticle biosensors6. In order to determine the
effectiveness of the technology, the biosensors will be placed at a different distances from the
patient’s skin. The distance of contact will be able to indicate the amount of sweat the sensors
are able to come into contact with and therefore able to make conclusion on the sensitivity of
the biosensors7. The biosensor have two key parts, the flexible sensors and microprocessor
which analysis the sweat constituents.
6 S. Imani, et al. A wearable chemical-electrophysiological hybrid biosensing system for real-
time health and fitness monitoring. Nat Commun 7:11650, 2016, p. 65-83
7 J. Moyer, D. Wilson, I. Finkelshtein, B. Wong, and R. Potts, Correlation between sweat
glucose and blood glucose in subjects with diabetes. Diabetes Technol Ther 14(5), 2012,
398–402.
In the experiment to determine the performance of sweat based wearable nanoparticle
biosensor, several materials will be used. First, a patient suffering from chronic disease such
as diabetes will be required. In this experiment, the patient will be monitored through the
sweat produced to determine different characteristics such as the glucose value. In addition,
another key factor which will be analysed in this experiment is the sensitivity and
effectiveness of the sweat-based nanoparticle biosensors6. In order to determine the
effectiveness of the technology, the biosensors will be placed at a different distances from the
patient’s skin. The distance of contact will be able to indicate the amount of sweat the sensors
are able to come into contact with and therefore able to make conclusion on the sensitivity of
the biosensors7. The biosensor have two key parts, the flexible sensors and microprocessor
which analysis the sweat constituents.
6 S. Imani, et al. A wearable chemical-electrophysiological hybrid biosensing system for real-
time health and fitness monitoring. Nat Commun 7:11650, 2016, p. 65-83
7 J. Moyer, D. Wilson, I. Finkelshtein, B. Wong, and R. Potts, Correlation between sweat
glucose and blood glucose in subjects with diabetes. Diabetes Technol Ther 14(5), 2012,
398–402.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
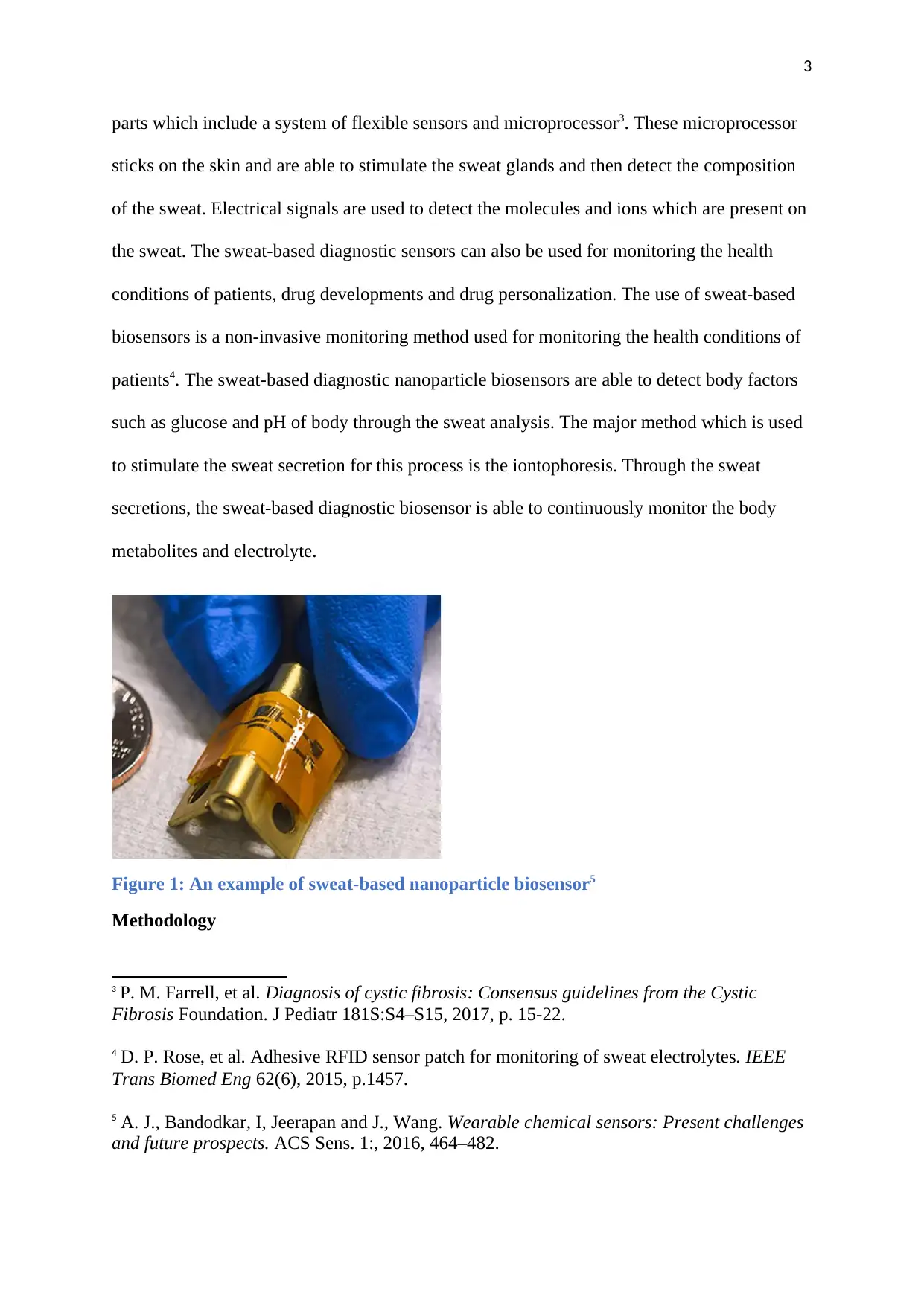
Figure 2: Sweat-based biosensor usage model8
In measuring the different factors, the sensor will be placed on the hand of the patient, and
the flexible sensors will stimulate the sweat glands. The microprocessor will detect the
presence of the sweat molecules and use them for analysis9. In this process, one of the
nanoparticle biosensor will be placed at 0.2 cm from the skin while another will be placed 1
cm from the skin. The ions amount in the sweat will be able to ignite electrical voltage in the
device. The electrical voltage generated will be proportional to the amount of ions present in
the sweat. The amount of constituents which will be detected on the sweat will be a clear
correlation of the amount of the same constituents on the blood10. The following diagram, on
8 D. P. Rose, et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE
Trans Biomed Eng 62(6), 2015, p.1465.
9 D. Wei, & A. Ivaska, Applications of ionic liquids in electrochemical sensors. Analytica
Chimica Acta 607, 2008, 126–135.
10 A. J., Bandodkar, I, Jeerapan and J., Wang. Wearable chemical sensors: Present challenges
and future prospects. ACS Sens. 1:, 2016, 464–482.
Figure 2: Sweat-based biosensor usage model8
In measuring the different factors, the sensor will be placed on the hand of the patient, and
the flexible sensors will stimulate the sweat glands. The microprocessor will detect the
presence of the sweat molecules and use them for analysis9. In this process, one of the
nanoparticle biosensor will be placed at 0.2 cm from the skin while another will be placed 1
cm from the skin. The ions amount in the sweat will be able to ignite electrical voltage in the
device. The electrical voltage generated will be proportional to the amount of ions present in
the sweat. The amount of constituents which will be detected on the sweat will be a clear
correlation of the amount of the same constituents on the blood10. The following diagram, on
8 D. P. Rose, et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE
Trans Biomed Eng 62(6), 2015, p.1465.
9 D. Wei, & A. Ivaska, Applications of ionic liquids in electrochemical sensors. Analytica
Chimica Acta 607, 2008, 126–135.
10 A. J., Bandodkar, I, Jeerapan and J., Wang. Wearable chemical sensors: Present challenges
and future prospects. ACS Sens. 1:, 2016, 464–482.
6
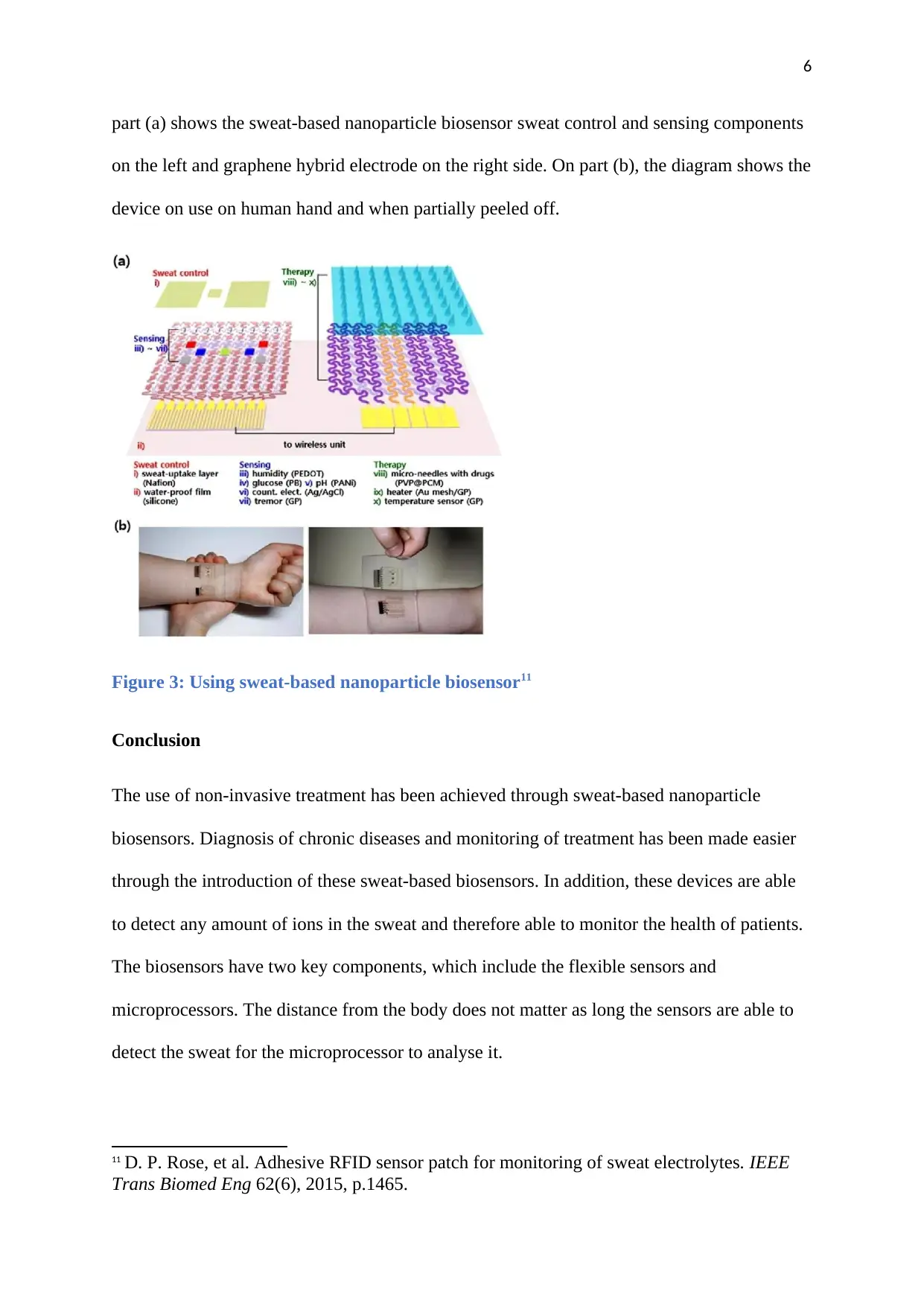
part (a) shows the sweat-based nanoparticle biosensor sweat control and sensing components
on the left and graphene hybrid electrode on the right side. On part (b), the diagram shows the
device on use on human hand and when partially peeled off.
Figure 3: Using sweat-based nanoparticle biosensor11
Conclusion
The use of non-invasive treatment has been achieved through sweat-based nanoparticle
biosensors. Diagnosis of chronic diseases and monitoring of treatment has been made easier
through the introduction of these sweat-based biosensors. In addition, these devices are able
to detect any amount of ions in the sweat and therefore able to monitor the health of patients.
The biosensors have two key components, which include the flexible sensors and
microprocessors. The distance from the body does not matter as long the sensors are able to
detect the sweat for the microprocessor to analyse it.
11 D. P. Rose, et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE
Trans Biomed Eng 62(6), 2015, p.1465.
part (a) shows the sweat-based nanoparticle biosensor sweat control and sensing components
on the left and graphene hybrid electrode on the right side. On part (b), the diagram shows the
device on use on human hand and when partially peeled off.
Figure 3: Using sweat-based nanoparticle biosensor11
Conclusion
The use of non-invasive treatment has been achieved through sweat-based nanoparticle
biosensors. Diagnosis of chronic diseases and monitoring of treatment has been made easier
through the introduction of these sweat-based biosensors. In addition, these devices are able
to detect any amount of ions in the sweat and therefore able to monitor the health of patients.
The biosensors have two key components, which include the flexible sensors and
microprocessors. The distance from the body does not matter as long the sensors are able to
detect the sweat for the microprocessor to analyse it.
11 D. P. Rose, et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE
Trans Biomed Eng 62(6), 2015, p.1465.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
Bibliography
Bandodkar A. J, Jeerapan I, and Wang J., Wearable chemical sensors: Present challenges
and future prospects. ACS Sens. 1:, 2016.
Bandodkar, A.J. and Wang J. Non-invasive wearable electrochemical sensors: a review
Farrell P. M, et al. Diagnosis of cystic fibrosis: Consensus guidelines from the Cystic Fibrosis
Foundation. J Pediatr 181S:S4–S15, 2017, p. 15-22.
Imani, S. et al. wearable chemical–electrophysiological hybrid biosensing system for real-
time health and fitness monitoring. Nat. Commun. 7, 11650, 2016,p. 65-83, p. 205.
Moyer J, Wilson D, Finkelshtein I, Wong B, and Potts R, Correlation between sweat glucose
and blood glucose in subjects with diabetes. Diabetes Technol Ther 14(5), 2012, 398–402.
Rose D. P, et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE
Trans Biomed Eng 62(6), 2015, 1457–1465.
Takei K, Honda W, Harada S, Arie T, and Akita S., Toward flexible and wearable human-
interactive health-monitoring devices. Adv Healthc Mater 4(4), 2015, 487–500.
Trends Biotechnol., 32 (7), 2014.
Bibliography
Bandodkar A. J, Jeerapan I, and Wang J., Wearable chemical sensors: Present challenges
and future prospects. ACS Sens. 1:, 2016.
Bandodkar, A.J. and Wang J. Non-invasive wearable electrochemical sensors: a review
Farrell P. M, et al. Diagnosis of cystic fibrosis: Consensus guidelines from the Cystic Fibrosis
Foundation. J Pediatr 181S:S4–S15, 2017, p. 15-22.
Imani, S. et al. wearable chemical–electrophysiological hybrid biosensing system for real-
time health and fitness monitoring. Nat. Commun. 7, 11650, 2016,p. 65-83, p. 205.
Moyer J, Wilson D, Finkelshtein I, Wong B, and Potts R, Correlation between sweat glucose
and blood glucose in subjects with diabetes. Diabetes Technol Ther 14(5), 2012, 398–402.
Rose D. P, et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE
Trans Biomed Eng 62(6), 2015, 1457–1465.
Takei K, Honda W, Harada S, Arie T, and Akita S., Toward flexible and wearable human-
interactive health-monitoring devices. Adv Healthc Mater 4(4), 2015, 487–500.
Trends Biotechnol., 32 (7), 2014.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

8
Wei, D. & Ivaska, A. Applications of ionic liquids in electrochemical sensors. Analytica
Chimica Acta 607, 2008, 126–135.
Wei, D. & Ivaska, A. Applications of ionic liquids in electrochemical sensors. Analytica
Chimica Acta 607, 2008, 126–135.
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

