Follow-up Efficacy of Exercise on Falls in Older Adults: Review
VerifiedAdded on 2022/08/23
|19
|17913
|16
Report
AI Summary
This report presents a systematic review and meta-analysis investigating the efficacy of physical exercise interventions on fall incidence and fall risk in healthy older adults during follow-up periods. The study analyzed 26 studies with 4739 participants, revealing a significant reduction in falls (32%) and fallers (22%) following exercise interventions compared to control groups. The review highlights the importance of posture-challenging exercises and emphasizes the need for understanding the physiological mechanisms underlying effective fall prevention. The findings suggest that physical exercise interventions are a valuable tool for reducing fall rates and risks in older adults, particularly when incorporating balance and stability exercises. The study underscores the importance of follow-up assessments to determine the long-term benefits of exercise programs.
S Y S T E M A TI C R E V I E W Open Access
Follow-up efficacy of physicalexercise
interventions on fallincidence and fallrisk
in healthy older adults:a systematic review
and meta-analysis
Azza Hamed1,2,3 , Sebastian Bohm1,2* , Falk Mersmann1,2 and Adamantios Arampatzis1,2*
Abstract
Background:The risk of falling and associated injuries increases with age.Therefore,the prevention of falls is a key
priority in geriatrics and is particularly based on physicalexercising,aiming to improve the age-related decline in
motor performance,which is crucialin response to posturalthreats.Although the benefits and specifications of
effective exercise programs have been welldocumented in pre-post design studies,that is during the treatment,
the definitive retention and transfer of these fall-related exercise benefits to the daily life fallrisk during follow-up
periods remains largely unclear.Accordingly,this meta-analysis investigates the efficacy of exercise interventions o
the follow-up risk of falling.
Methods:A systematic database search was conducted.A study was considered eligible if it examined the number
of falls (fallrate) and fallers (fallrisk) of healthy older adults (≥ 65 years) during a follow-up period after participa
in a randomized controlled physicalexercise intervention.The pooled estimates of the fallrate and fallrisk ratios
were calculated using a random-effects meta-analysis.Furthermore,the methodologicalquality and the risk of bias
were assessed.
Results:Twenty-six studies with 31 different intervention groups were included (4739 participants).The number of
falls was significantly (p <0.001) reduced by 32% (rate ratio 0.68,95% confidence interval0.58 to 0.80) and the
number of fallers by 22% (risk ratio 0.78,95% confidence interval0.68 to 0.89) following exercising when compared
with controls.Interventions that applied posture-challenging exercises showed the highest effects.The
methodologicalquality score was acceptable (73 ± 11%) and risk of bias low.
Conclusions:The present review and meta-analysis provide evidence that physicalexercise interventions have the
potentialto significantly reduce fallrate and risk in healthy older adults.Posture-challenging exercises might be
particularly considered when designing fallprevention interventions.
Keywords:Fallprevention,Physicaltraining interventions,Older adults,Fallrisk,Fallincidence,Posturaland balance
perturbations
* Correspondence:sebastian.bohm@hu-berlin.de;a.arampatzis@hu-berlin.de;
https://www.dtms.hu-berlin.de
1Department of Training and Movement Sciences,Humboldt-Universität zu
Berlin,Philippstr.13,Haus 11,10115 Berlin,Germany
Fulllist of author information is available at the end of the article
© The Author(s).2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.
Hamed et al.Sports Medicine - Open (2018) 4:56
https://doi.org/10.1186/s40798-018-0170-z
Follow-up efficacy of physicalexercise
interventions on fallincidence and fallrisk
in healthy older adults:a systematic review
and meta-analysis
Azza Hamed1,2,3 , Sebastian Bohm1,2* , Falk Mersmann1,2 and Adamantios Arampatzis1,2*
Abstract
Background:The risk of falling and associated injuries increases with age.Therefore,the prevention of falls is a key
priority in geriatrics and is particularly based on physicalexercising,aiming to improve the age-related decline in
motor performance,which is crucialin response to posturalthreats.Although the benefits and specifications of
effective exercise programs have been welldocumented in pre-post design studies,that is during the treatment,
the definitive retention and transfer of these fall-related exercise benefits to the daily life fallrisk during follow-up
periods remains largely unclear.Accordingly,this meta-analysis investigates the efficacy of exercise interventions o
the follow-up risk of falling.
Methods:A systematic database search was conducted.A study was considered eligible if it examined the number
of falls (fallrate) and fallers (fallrisk) of healthy older adults (≥ 65 years) during a follow-up period after participa
in a randomized controlled physicalexercise intervention.The pooled estimates of the fallrate and fallrisk ratios
were calculated using a random-effects meta-analysis.Furthermore,the methodologicalquality and the risk of bias
were assessed.
Results:Twenty-six studies with 31 different intervention groups were included (4739 participants).The number of
falls was significantly (p <0.001) reduced by 32% (rate ratio 0.68,95% confidence interval0.58 to 0.80) and the
number of fallers by 22% (risk ratio 0.78,95% confidence interval0.68 to 0.89) following exercising when compared
with controls.Interventions that applied posture-challenging exercises showed the highest effects.The
methodologicalquality score was acceptable (73 ± 11%) and risk of bias low.
Conclusions:The present review and meta-analysis provide evidence that physicalexercise interventions have the
potentialto significantly reduce fallrate and risk in healthy older adults.Posture-challenging exercises might be
particularly considered when designing fallprevention interventions.
Keywords:Fallprevention,Physicaltraining interventions,Older adults,Fallrisk,Fallincidence,Posturaland balance
perturbations
* Correspondence:sebastian.bohm@hu-berlin.de;a.arampatzis@hu-berlin.de;
https://www.dtms.hu-berlin.de
1Department of Training and Movement Sciences,Humboldt-Universität zu
Berlin,Philippstr.13,Haus 11,10115 Berlin,Germany
Fulllist of author information is available at the end of the article
© The Author(s).2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0
InternationalLicense (http://creativecommons.org/licenses/by/4.0/),which permits unrestricted use,distribution,and
reproduction in any medium,provided you give appropriate credit to the originalauthor(s) and the source,provide a link to
the Creative Commons license,and indicate if changes were made.
Hamed et al.Sports Medicine - Open (2018) 4:56
https://doi.org/10.1186/s40798-018-0170-z
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Key points
Physicalexerciseclearlyreducesthe follow-up risk
of falling.
Exercise interventions for fallprevention may include
stability-challenging conditions and perturbations.
Specification ofsuch exercises(alongside intensity)
and understandingof their physiologicalunderlying
effect is needed to ensure and improve effective reten-
tion of fall-related exercise benefits in the postinter-
vention follow-up.
Background
Aging is associated with a reduction ofthe functional
and physiologicalcapacity ofthe musculoskeletaland
central nervous systems,which significantlyaffects
motor performance [1–4].It is well evidenced that these
age-related declines increase the incidence offalls and
re-falls among older people [5],with one third ofolder
adults above 65 years falling atleastonce a year [6,7]
and increasing fallrates in even older ages [8–10].Falls
in older adults occur mainly during dynamic daily tasks
(e.g., walking and initiation of walking, and sitting down or
lowering) and in the absence ofexternalevents [11–13],
which indicatesa reduced ability ofeffective internal
controland execution ofregular dynamic movements.
In the face ofexternalhazards that occur during daily
life tasks,such impairments of motor responses lead to
even higherrisk of stability loss [14–17].When pos-
tural/dynamic stability cannot be maintained and a fall
eventoccurs,injury incidence isparticularly high in
older adults.Falls are one of the leading causesof
injury-related hospital admissions in this age group [18]
and are often followed by functionaldependence,ser-
ious or fatal injuries,fractures,and high morbidity [19].
The decline in motor performance is caused by di-
verseage-related changesacrossthe many different
levels of the human organism,e.g.,centralnervous and
musculoskeletal.Among others,muscle weakness with
aging,so-called sarcopenia [20],is a key factor that de-
terminesstability controland recovery responsesfol-
lowing sudden threats[21–25].The loss of muscle
mass,which occurs due to a reduced number of motor
units and size ofsingle muscle fibers,as wellas a de-
crease ofvoluntary activation [26–30],leads to a de-
cline ofthe muscle force capacity [1,2, 28,31,32].As
degenerative effects predominantly affect fast twitch fi-
bers [33]and muscle fascicle length decreases as well
[34],the mechanicalpower (productof force and vel-
ocity) as a predictor of the muscle’s functionalcapacity
during dynamic stability threats[35] is affected in a
twofold manner [36,37].Consequently,studies [21,22]
have demonstrated deficits in the execution offunda-
mentalstability controlmechanisms (e.g.,modulation
of the base ofsupportand counter segmentrotations
around the center ofmass [38]) in older adults,which
likely contributes to the limited ability to regain stabil-
ity following sudden unstable conditions [22].
Current reviews and guidelines regarding the preven-
tion of falls consistently recommend physicalexercises
[39–43]using strength,balance,mobility,and perturb-
ation training paradigms [40,43–45]to counteractthe
decline ofmotor performance.Moreover,Tai Chi con-
tains balance-challenging slowly performed movements
and has been recommended for fallprevention in older
adults [46,47].In fact,the body of randomized controlled
trialsshowsthattraining ofthis kind in healthy older
adultshas the potentialto improvestrength [48–52],
mobility [48, 52], stability, and balance control [50, 52, 53]
and reduce the risk of falling [54] and related injuries [40,
49,55,56],within and after the intervention period [52,
57,58].Previous meta-analyses allowed for conclusions
on the mosteffective characteristics ofexercise training
interventions with respect to the reduction of the risk of
falling [44,59,60].However,these meta-analyses did not
distinguish between studies thatassessed the effects oc-
curring during theintervention time and studiesthat
assessed only the follow-up period,i.e.,after finishing the
treatment. Thus, the question of how much of these bene-
fits of training persist over a longer time period and trans-
fer to daily life after completion (i.e.,follow-up effects) is
stillnot fully understood.As motor learning and neuro-
muscularplasticity in olderadultsis largely preserved
[61–67],older adults are capable of an improvement and
long-term retention ofeffective stability controlmecha-
nisms as wellas gains in functionalcapacities,both of
which are necessary to compensate for challenging bal-
ance conditions [64,68].Therefore,it can be argued that
exercise interventions may improve relevant key factors of
successfulreactive posturalresponses to sudden postural
threatsoccurring during dailylife. However,although
there is broad evidence on acute fall-related benefits of ex-
ercise interventions (e.g.,strength gains,stability control
improvements)[40,44, 49, 55, 56, 69],little is known
about how fallprevention interventions actually translate
into a reduction of falls in time periods after participation,
i.e.,retention or follow-up.Further,the small sample sizes
and diverse exercise approaches compromise the conclu-
sions drawn from single randomized controlled trials.
The scope of the current review is to provide an ana-
lysis ofhealthy older adults whose falloccurrences are
not co-affected by an additionalfactor,i.e.,a particular
pathology.Some impairmentsmay affectthe physio-
logicalresponsiveness to the training or would require
adjusted exercise delivery strategies(e.g.,group sizes
and supervision).Consequently,to avoid a bias due to
factors other than aging on the efficacy ofphysicalex-
ercise interventionsfor post intervention fallpreven-
tion, we included onlyhealthyolder adults in the
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 2 of 19
Physicalexerciseclearlyreducesthe follow-up risk
of falling.
Exercise interventions for fallprevention may include
stability-challenging conditions and perturbations.
Specification ofsuch exercises(alongside intensity)
and understandingof their physiologicalunderlying
effect is needed to ensure and improve effective reten-
tion of fall-related exercise benefits in the postinter-
vention follow-up.
Background
Aging is associated with a reduction ofthe functional
and physiologicalcapacity ofthe musculoskeletaland
central nervous systems,which significantlyaffects
motor performance [1–4].It is well evidenced that these
age-related declines increase the incidence offalls and
re-falls among older people [5],with one third ofolder
adults above 65 years falling atleastonce a year [6,7]
and increasing fallrates in even older ages [8–10].Falls
in older adults occur mainly during dynamic daily tasks
(e.g., walking and initiation of walking, and sitting down or
lowering) and in the absence ofexternalevents [11–13],
which indicatesa reduced ability ofeffective internal
controland execution ofregular dynamic movements.
In the face ofexternalhazards that occur during daily
life tasks,such impairments of motor responses lead to
even higherrisk of stability loss [14–17].When pos-
tural/dynamic stability cannot be maintained and a fall
eventoccurs,injury incidence isparticularly high in
older adults.Falls are one of the leading causesof
injury-related hospital admissions in this age group [18]
and are often followed by functionaldependence,ser-
ious or fatal injuries,fractures,and high morbidity [19].
The decline in motor performance is caused by di-
verseage-related changesacrossthe many different
levels of the human organism,e.g.,centralnervous and
musculoskeletal.Among others,muscle weakness with
aging,so-called sarcopenia [20],is a key factor that de-
terminesstability controland recovery responsesfol-
lowing sudden threats[21–25].The loss of muscle
mass,which occurs due to a reduced number of motor
units and size ofsingle muscle fibers,as wellas a de-
crease ofvoluntary activation [26–30],leads to a de-
cline ofthe muscle force capacity [1,2, 28,31,32].As
degenerative effects predominantly affect fast twitch fi-
bers [33]and muscle fascicle length decreases as well
[34],the mechanicalpower (productof force and vel-
ocity) as a predictor of the muscle’s functionalcapacity
during dynamic stability threats[35] is affected in a
twofold manner [36,37].Consequently,studies [21,22]
have demonstrated deficits in the execution offunda-
mentalstability controlmechanisms (e.g.,modulation
of the base ofsupportand counter segmentrotations
around the center ofmass [38]) in older adults,which
likely contributes to the limited ability to regain stabil-
ity following sudden unstable conditions [22].
Current reviews and guidelines regarding the preven-
tion of falls consistently recommend physicalexercises
[39–43]using strength,balance,mobility,and perturb-
ation training paradigms [40,43–45]to counteractthe
decline ofmotor performance.Moreover,Tai Chi con-
tains balance-challenging slowly performed movements
and has been recommended for fallprevention in older
adults [46,47].In fact,the body of randomized controlled
trialsshowsthattraining ofthis kind in healthy older
adultshas the potentialto improvestrength [48–52],
mobility [48, 52], stability, and balance control [50, 52, 53]
and reduce the risk of falling [54] and related injuries [40,
49,55,56],within and after the intervention period [52,
57,58].Previous meta-analyses allowed for conclusions
on the mosteffective characteristics ofexercise training
interventions with respect to the reduction of the risk of
falling [44,59,60].However,these meta-analyses did not
distinguish between studies thatassessed the effects oc-
curring during theintervention time and studiesthat
assessed only the follow-up period,i.e.,after finishing the
treatment. Thus, the question of how much of these bene-
fits of training persist over a longer time period and trans-
fer to daily life after completion (i.e.,follow-up effects) is
stillnot fully understood.As motor learning and neuro-
muscularplasticity in olderadultsis largely preserved
[61–67],older adults are capable of an improvement and
long-term retention ofeffective stability controlmecha-
nisms as wellas gains in functionalcapacities,both of
which are necessary to compensate for challenging bal-
ance conditions [64,68].Therefore,it can be argued that
exercise interventions may improve relevant key factors of
successfulreactive posturalresponses to sudden postural
threatsoccurring during dailylife. However,although
there is broad evidence on acute fall-related benefits of ex-
ercise interventions (e.g.,strength gains,stability control
improvements)[40,44, 49, 55, 56, 69],little is known
about how fallprevention interventions actually translate
into a reduction of falls in time periods after participation,
i.e.,retention or follow-up.Further,the small sample sizes
and diverse exercise approaches compromise the conclu-
sions drawn from single randomized controlled trials.
The scope of the current review is to provide an ana-
lysis ofhealthy older adults whose falloccurrences are
not co-affected by an additionalfactor,i.e.,a particular
pathology.Some impairmentsmay affectthe physio-
logicalresponsiveness to the training or would require
adjusted exercise delivery strategies(e.g.,group sizes
and supervision).Consequently,to avoid a bias due to
factors other than aging on the efficacy ofphysicalex-
ercise interventionsfor post intervention fallpreven-
tion, we included onlyhealthyolder adults in the
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 2 of 19
present review and meta-analysis.Therefore,the purpose
of the present review and meta-analysis was to investigate
the efficacy ofphysicalexercise interventionson post
intervention fallprevention in healthy older adults (i.e.,
withoutneurologicaldisease[e.g.,Parkinson’sdisease,
stroke,or dementia/cognitive impairment],serious visual
impairments [e.g.,cataract,glaucoma,or color blindness],
severe cardiac,pulmonary or musculoskeletaldisorders,
and severe osteoporosis,not living independently and not
taking psychotropic drugs,thatcould influence fallout-
comes).We searched forrandomized controlled trials,
examining the effect of different types and forms of phys-
icalexercises on fallrate (i.e.,number of fallevents) and
fall risk (i.e.,numberof fallers)during thefollow-up
period.For the respectivestudies,we calculated the
weighted average effect sizes and assessed the study qual-
ity and risk of bias.
Methods
Search strategy
Three electronic bibliographicdatabases(Web of
Science,MEDLINE, and Scopus)were systematically
searched (from inception tillAugust 2018)using a
combined set of terms related to physicalexercises (in-
terventions,exercises,exercising,training),older adult
subjects (elderly,old, aged,age,senior,geriatric,aging,
ageing)and falls (accidentalfall, falling,slip, tripping)
(see Additional file 1).Each term was mapped to MeSH
(Medical SubjectHeadings)and controlled termsif
available.Moreover,the reference listsof the eligible
studiesand of previousmeta-analyseswere screened
for additional suitable titles.
Study inclusion and exclusion criteria
The search results were evaluated at first by screening
the study titles.Thereafter,abstracts and further the full
textswere examined to determine theireligibility.A
study was included when the following inclusion cri-
teria were fulfilled:(a) investigation offall incidence
(fallrate) and/or number of fallers (fallrisk) during (b)
a follow-up period (started from the intervention’s end
point)of at least6 months after (c)a longitudinal(d)
randomized controlled (levelI) (e) physicalexercise
intervention (f )of at least4 weeks on (g)healthy,(h)
older adults(≥ 65 years).Studieswhich did not meet
the inclusion criteria in this stage were excluded,and
the respectiveexclusion reason was documented
(Fig.1).Finally,the reference lists of the eligible studies
and of previous meta-analyses were screened for further
articles.When a study presented differentgroupsor
intervention types and some ofthose did not meet the
criteria,only the group or intervention that fulfilled the
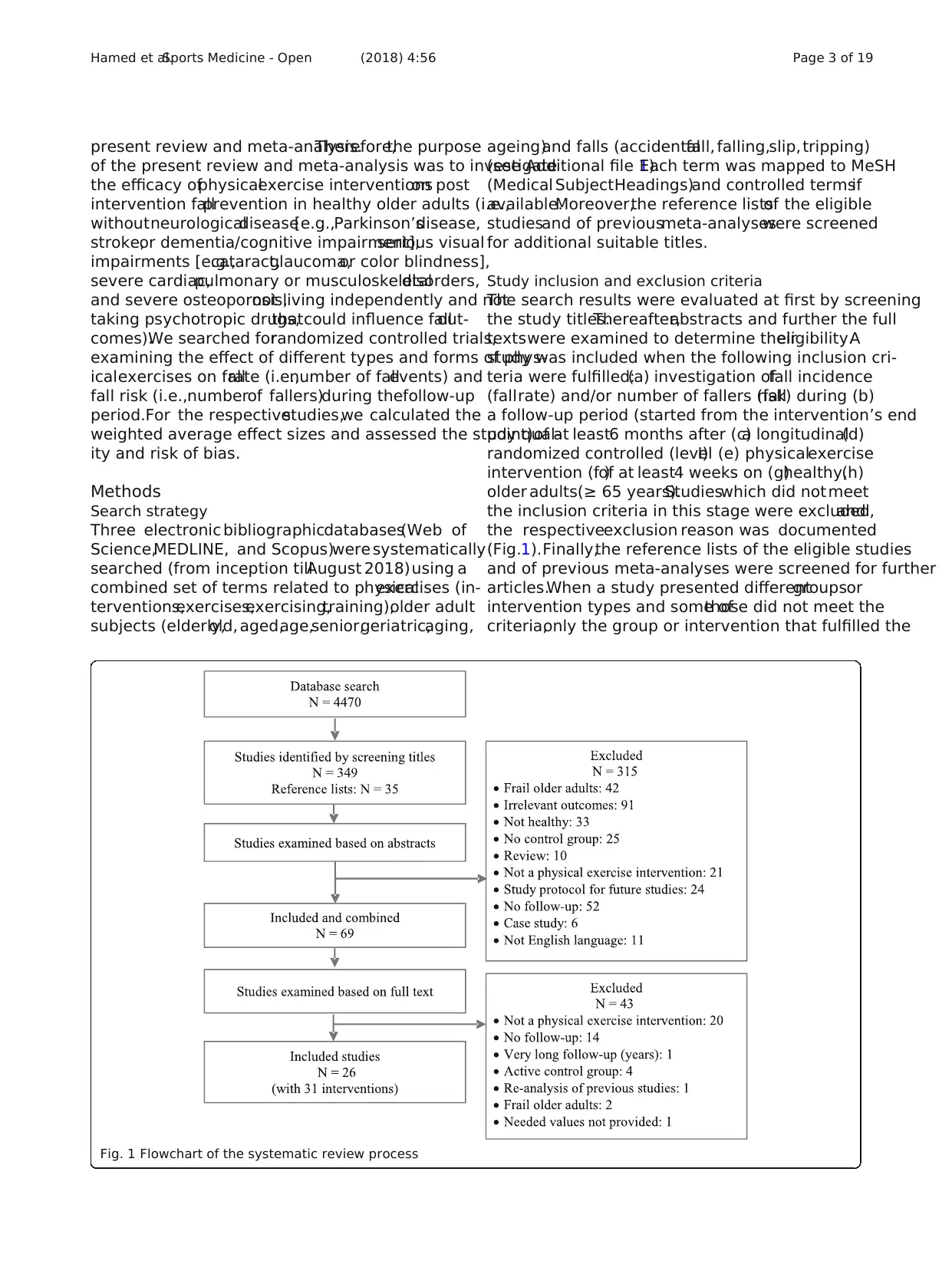
Fig. 1 Flowchart of the systematic review process
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 3 of 19
of the present review and meta-analysis was to investigate
the efficacy ofphysicalexercise interventionson post
intervention fallprevention in healthy older adults (i.e.,
withoutneurologicaldisease[e.g.,Parkinson’sdisease,
stroke,or dementia/cognitive impairment],serious visual
impairments [e.g.,cataract,glaucoma,or color blindness],
severe cardiac,pulmonary or musculoskeletaldisorders,
and severe osteoporosis,not living independently and not
taking psychotropic drugs,thatcould influence fallout-
comes).We searched forrandomized controlled trials,
examining the effect of different types and forms of phys-
icalexercises on fallrate (i.e.,number of fallevents) and
fall risk (i.e.,numberof fallers)during thefollow-up
period.For the respectivestudies,we calculated the
weighted average effect sizes and assessed the study qual-
ity and risk of bias.
Methods
Search strategy
Three electronic bibliographicdatabases(Web of
Science,MEDLINE, and Scopus)were systematically
searched (from inception tillAugust 2018)using a
combined set of terms related to physicalexercises (in-
terventions,exercises,exercising,training),older adult
subjects (elderly,old, aged,age,senior,geriatric,aging,
ageing)and falls (accidentalfall, falling,slip, tripping)
(see Additional file 1).Each term was mapped to MeSH
(Medical SubjectHeadings)and controlled termsif
available.Moreover,the reference listsof the eligible
studiesand of previousmeta-analyseswere screened
for additional suitable titles.
Study inclusion and exclusion criteria
The search results were evaluated at first by screening
the study titles.Thereafter,abstracts and further the full
textswere examined to determine theireligibility.A
study was included when the following inclusion cri-
teria were fulfilled:(a) investigation offall incidence
(fallrate) and/or number of fallers (fallrisk) during (b)
a follow-up period (started from the intervention’s end
point)of at least6 months after (c)a longitudinal(d)
randomized controlled (levelI) (e) physicalexercise
intervention (f )of at least4 weeks on (g)healthy,(h)
older adults(≥ 65 years).Studieswhich did not meet
the inclusion criteria in this stage were excluded,and
the respectiveexclusion reason was documented
(Fig.1).Finally,the reference lists of the eligible studies
and of previous meta-analyses were screened for further
articles.When a study presented differentgroupsor
intervention types and some ofthose did not meet the
criteria,only the group or intervention that fulfilled the
Fig. 1 Flowchart of the systematic review process
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 3 of 19
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
criteria was included.If an eligible study reported two or
more interventions of different types of physical exercises,
each intervention group wasincluded separately.Note
that studies with different follow-up durations and differ-
ent exercise interventionswere included,which might
cause heterogeneity.The systematic review process of the
present meta-analysis is presented in Fig. 1.
Study quality assessment and risk of bias
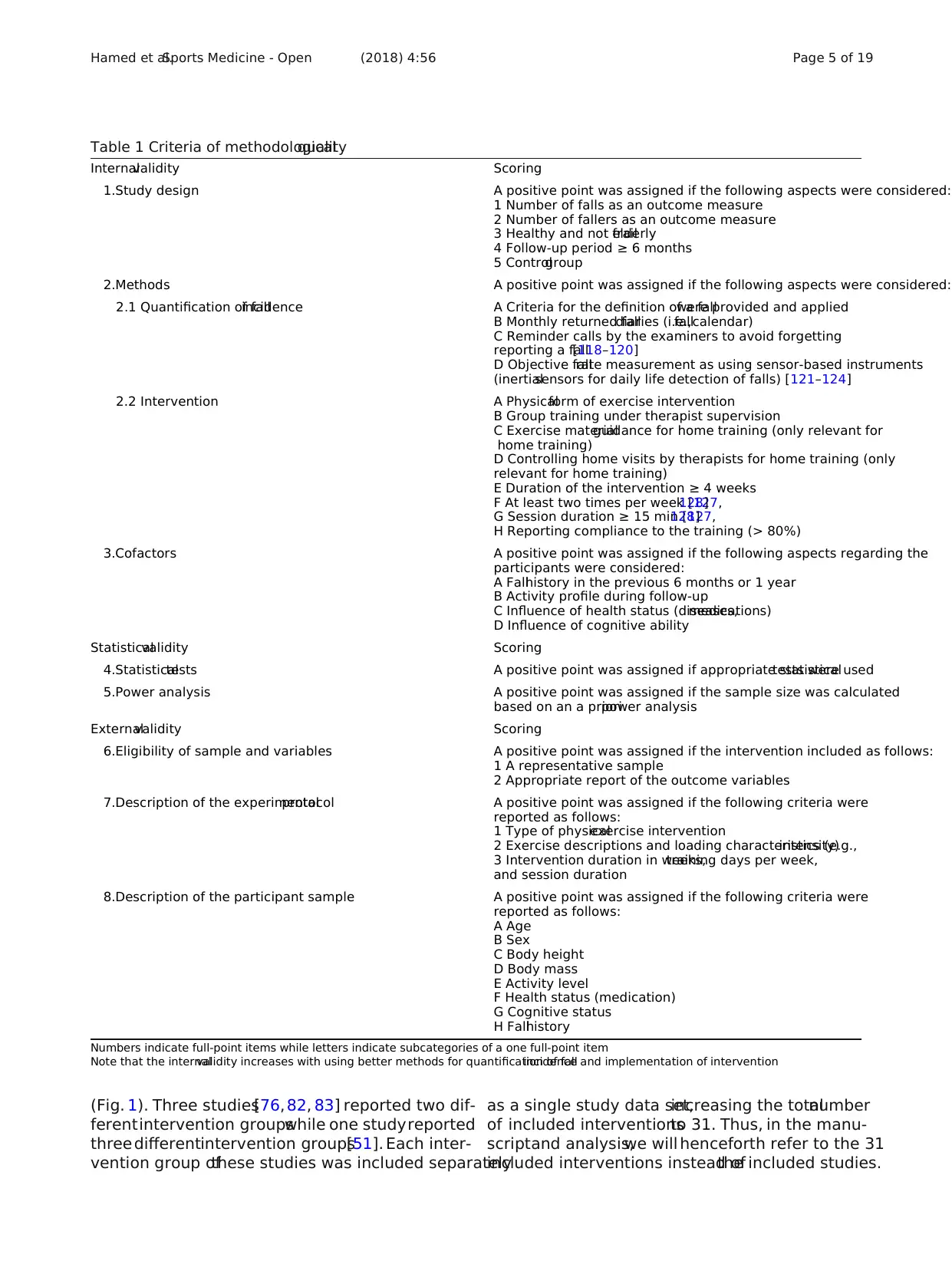
We customized a methodological quality scale to assess
the internal,statistical,and externalvalidity ofthe in-
cluded studies with regard to the concept of the present
meta-analysis (Table 1).A positive pointwas assigned
to each quality criterion ifit was fulfilled.The quality
score of each validity aspect(i.e.,internal,statistical,
and external)was expressed asthe numberof items
with a positive score in percent ofthe totalnumber of
items.Thus, 100% indicateshighestpossible quality.
The single section scores were then averaged to calcu-
late the overallmethodologicalquality ofeach study.
However,a low resultin the rating was notan exclu-
sion criterion butallowed foran adequate interpret-
ation of the single study outcomes in the context of the
scope ofthe currentmeta-analysis.The calculation of
the quality score ofeach validity section was done by
counting the number ofitems with positive signs and
dividing them bythe total numbersof items to be
expressed finally asa percentage.The single section
scoreswere then averagedto calculatethe overall
methodological quality of each study.
The risk of bias for each study was examined accord-
ing to the Cochrane risk ofbias tool[70] in which the
following biasitems were assessed:sequence gener-
ation,allocation concealment,blinding ofparticipants
and outcome assessors,incomplete outcome data,se-
lective outcome reporting,and other sources ofbias.
The publication biaswas tested by meansof Egger’s
test [71].
Data extraction
The data ofinterest were extracted and organized in a
table including all of the following information:authors’
names,participants’characteristics (age,sex,and num-
ber),exercise protocol(type and description ofexer-
cises),interventioncharacteristics,and duration of
follow-up period (for studieswith more than one
follow-up time point the latest one was chosen) as well
as the main outcomes.If the outcome parameters (i.e.,
number of falls and number of fallers) were not
reported in appropriate format (e.g.,percentages,odds
ratio,hazard ratio,or presented as a graph),the corre-
sponding authors were contacted and asked to provide
the missing values.Extracting the values visually from a
graph was the last option.To avoid double inclusion of
the sameparticipants,one study [72] was excluded
from the analysis as the data ofthe same participants
were re-analyzed already in another included study [73]
as stated by the authors.
Statistical analysis
The fall rate (i.e.,numberof falls) and fall risk (i.e.,
number of fallers) were calculated from the completion
time point of the intervention program until the end of
the follow-up duration asa fall incidence rateratio
(value of intervention group divided by value of control
group)and risk ratio for each study,respectively.The
risk ratio was considered to accountfor the effectof
multiple falls (more than one fallper person)[74]on
fall rate ratio.Thus, a fall rate ratio and/or risk ratio
below the value ofone means lower risk in the inter-
vention group than the untreated controlgroup,while
a value higher than one indicates a higher risk in the
intervention group.The relativerisk reduction was
used to re-express the risk ratio and rate ratio as per-
centage reduction in number of fallevents and number
of fallers [75].If the fall rate ratio or fallrisk ratio were
reported withoutthe raw valuesof fall eventsand
fallers [76–79],the ratios were taken directly from the
respective study and the standard error was calculated
from the 95% confidence intervals.
The single data were then pooled in a meta-analysis
to estimate the effect sizes as weighted average overall
fall rate and risk ratios,respectively.For this reason,a
random-effects modelof the generic inverse variance
method was used because it gives more weight to the
studies with smallstandard errors and takes into con-
sideration theheterogeneityof the included studies
[80,81].The presence of an overalleffect of a physical
exercise intervention on fallrate ratio and risk ratio
during follow-up was testedaccordingly[70]. The
meta-analysis statistics and respective forest plots were
performed using the software Review Manager(Ver-
sion 5.2.Copenhagen:The Nordic Cochrane Centre,
the Cochrane Collaboration,2014).
Results
Review statistics
A total number of4470 studies were recorded after the
database search (Fig. 1). The study titles were then checke
for eligibility and at the same time,the duplicates were re-
moved,yielding 349 potentially eligible studies.By review-
ing the abstracts,the number of potentially eligible studies
was 34.After reviewing the fulltext,24 studies remained
included.Screening ofthe reference lists ofthe included
studies and of previous meta-analyses yielded an additiona
35 related studies from which only two studies were eli-
gible after checking the abstract and the fulltext.Finally,
26 studieswereincluded in thecurrentmeta-analysis
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 4 of 19
more interventions of different types of physical exercises,
each intervention group wasincluded separately.Note
that studies with different follow-up durations and differ-
ent exercise interventionswere included,which might
cause heterogeneity.The systematic review process of the
present meta-analysis is presented in Fig. 1.
Study quality assessment and risk of bias
We customized a methodological quality scale to assess
the internal,statistical,and externalvalidity ofthe in-
cluded studies with regard to the concept of the present
meta-analysis (Table 1).A positive pointwas assigned
to each quality criterion ifit was fulfilled.The quality
score of each validity aspect(i.e.,internal,statistical,
and external)was expressed asthe numberof items
with a positive score in percent ofthe totalnumber of
items.Thus, 100% indicateshighestpossible quality.
The single section scores were then averaged to calcu-
late the overallmethodologicalquality ofeach study.
However,a low resultin the rating was notan exclu-
sion criterion butallowed foran adequate interpret-
ation of the single study outcomes in the context of the
scope ofthe currentmeta-analysis.The calculation of
the quality score ofeach validity section was done by
counting the number ofitems with positive signs and
dividing them bythe total numbersof items to be
expressed finally asa percentage.The single section
scoreswere then averagedto calculatethe overall
methodological quality of each study.
The risk of bias for each study was examined accord-
ing to the Cochrane risk ofbias tool[70] in which the
following biasitems were assessed:sequence gener-
ation,allocation concealment,blinding ofparticipants
and outcome assessors,incomplete outcome data,se-
lective outcome reporting,and other sources ofbias.
The publication biaswas tested by meansof Egger’s
test [71].
Data extraction
The data ofinterest were extracted and organized in a
table including all of the following information:authors’
names,participants’characteristics (age,sex,and num-
ber),exercise protocol(type and description ofexer-
cises),interventioncharacteristics,and duration of
follow-up period (for studieswith more than one
follow-up time point the latest one was chosen) as well
as the main outcomes.If the outcome parameters (i.e.,
number of falls and number of fallers) were not
reported in appropriate format (e.g.,percentages,odds
ratio,hazard ratio,or presented as a graph),the corre-
sponding authors were contacted and asked to provide
the missing values.Extracting the values visually from a
graph was the last option.To avoid double inclusion of
the sameparticipants,one study [72] was excluded
from the analysis as the data ofthe same participants
were re-analyzed already in another included study [73]
as stated by the authors.
Statistical analysis
The fall rate (i.e.,numberof falls) and fall risk (i.e.,
number of fallers) were calculated from the completion
time point of the intervention program until the end of
the follow-up duration asa fall incidence rateratio
(value of intervention group divided by value of control
group)and risk ratio for each study,respectively.The
risk ratio was considered to accountfor the effectof
multiple falls (more than one fallper person)[74]on
fall rate ratio.Thus, a fall rate ratio and/or risk ratio
below the value ofone means lower risk in the inter-
vention group than the untreated controlgroup,while
a value higher than one indicates a higher risk in the
intervention group.The relativerisk reduction was
used to re-express the risk ratio and rate ratio as per-
centage reduction in number of fallevents and number
of fallers [75].If the fall rate ratio or fallrisk ratio were
reported withoutthe raw valuesof fall eventsand
fallers [76–79],the ratios were taken directly from the
respective study and the standard error was calculated
from the 95% confidence intervals.
The single data were then pooled in a meta-analysis
to estimate the effect sizes as weighted average overall
fall rate and risk ratios,respectively.For this reason,a
random-effects modelof the generic inverse variance
method was used because it gives more weight to the
studies with smallstandard errors and takes into con-
sideration theheterogeneityof the included studies
[80,81].The presence of an overalleffect of a physical
exercise intervention on fallrate ratio and risk ratio
during follow-up was testedaccordingly[70]. The
meta-analysis statistics and respective forest plots were
performed using the software Review Manager(Ver-
sion 5.2.Copenhagen:The Nordic Cochrane Centre,
the Cochrane Collaboration,2014).
Results
Review statistics
A total number of4470 studies were recorded after the
database search (Fig. 1). The study titles were then checke
for eligibility and at the same time,the duplicates were re-
moved,yielding 349 potentially eligible studies.By review-
ing the abstracts,the number of potentially eligible studies
was 34.After reviewing the fulltext,24 studies remained
included.Screening ofthe reference lists ofthe included
studies and of previous meta-analyses yielded an additiona
35 related studies from which only two studies were eli-
gible after checking the abstract and the fulltext.Finally,
26 studieswereincluded in thecurrentmeta-analysis
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 4 of 19
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
(Fig. 1). Three studies[76, 82, 83] reported two dif-
ferentintervention groupswhile one studyreported
three differentintervention groups[51]. Each inter-
vention group ofthese studies was included separately
as a single study data set,increasing the totalnumber
of included interventionsto 31. Thus, in the manu-
scriptand analysis,we will henceforth refer to the 31
included interventions instead ofthe included studies.
Table 1 Criteria of methodologicalquality
Internalvalidity Scoring
1.Study design A positive point was assigned if the following aspects were considered:
1 Number of falls as an outcome measure
2 Number of fallers as an outcome measure
3 Healthy and not frailelderly
4 Follow-up period ≥ 6 months
5 Controlgroup
2.Methods A positive point was assigned if the following aspects were considered:
2.1 Quantification of fallincidence A Criteria for the definition of a fallwere provided and applied
B Monthly returned falldiaries (i.e.,fallcalendar)
C Reminder calls by the examiners to avoid forgetting
reporting a fall[118–120]
D Objective fallrate measurement as using sensor-based instruments
(inertialsensors for daily life detection of falls) [121–124]
2.2 Intervention A Physicalform of exercise intervention
B Group training under therapist supervision
C Exercise materialguidance for home training (only relevant for
home training)
D Controlling home visits by therapists for home training (only
relevant for home training)
E Duration of the intervention ≥ 4 weeks
F At least two times per week [127,128]
G Session duration ≥ 15 min [127,128]
H Reporting compliance to the training (> 80%)
3.Cofactors A positive point was assigned if the following aspects regarding the
participants were considered:
A Fallhistory in the previous 6 months or 1 year
B Activity profile during follow-up
C Influence of health status (diseases,medications)
D Influence of cognitive ability
Statisticalvalidity Scoring
4.Statisticaltests A positive point was assigned if appropriate statisticaltests were used
5.Power analysis A positive point was assigned if the sample size was calculated
based on an a prioripower analysis
Externalvalidity Scoring
6.Eligibility of sample and variables A positive point was assigned if the intervention included as follows:
1 A representative sample
2 Appropriate report of the outcome variables
7.Description of the experimentalprotocol A positive point was assigned if the following criteria were
reported as follows:
1 Type of physicalexercise intervention
2 Exercise descriptions and loading characteristics (e.g.,intensity)
3 Intervention duration in weeks,training days per week,
and session duration
8.Description of the participant sample A positive point was assigned if the following criteria were
reported as follows:
A Age
B Sex
C Body height
D Body mass
E Activity level
F Health status (medication)
G Cognitive status
H Fallhistory
Numbers indicate full-point items while letters indicate subcategories of a one full-point item
Note that the internalvalidity increases with using better methods for quantification of fallincidence and implementation of intervention
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 5 of 19
ferentintervention groupswhile one studyreported
three differentintervention groups[51]. Each inter-
vention group ofthese studies was included separately
as a single study data set,increasing the totalnumber
of included interventionsto 31. Thus, in the manu-
scriptand analysis,we will henceforth refer to the 31
included interventions instead ofthe included studies.
Table 1 Criteria of methodologicalquality
Internalvalidity Scoring
1.Study design A positive point was assigned if the following aspects were considered:
1 Number of falls as an outcome measure
2 Number of fallers as an outcome measure
3 Healthy and not frailelderly
4 Follow-up period ≥ 6 months
5 Controlgroup
2.Methods A positive point was assigned if the following aspects were considered:
2.1 Quantification of fallincidence A Criteria for the definition of a fallwere provided and applied
B Monthly returned falldiaries (i.e.,fallcalendar)
C Reminder calls by the examiners to avoid forgetting
reporting a fall[118–120]
D Objective fallrate measurement as using sensor-based instruments
(inertialsensors for daily life detection of falls) [121–124]
2.2 Intervention A Physicalform of exercise intervention
B Group training under therapist supervision
C Exercise materialguidance for home training (only relevant for
home training)
D Controlling home visits by therapists for home training (only
relevant for home training)
E Duration of the intervention ≥ 4 weeks
F At least two times per week [127,128]
G Session duration ≥ 15 min [127,128]
H Reporting compliance to the training (> 80%)
3.Cofactors A positive point was assigned if the following aspects regarding the
participants were considered:
A Fallhistory in the previous 6 months or 1 year
B Activity profile during follow-up
C Influence of health status (diseases,medications)
D Influence of cognitive ability
Statisticalvalidity Scoring
4.Statisticaltests A positive point was assigned if appropriate statisticaltests were used
5.Power analysis A positive point was assigned if the sample size was calculated
based on an a prioripower analysis
Externalvalidity Scoring
6.Eligibility of sample and variables A positive point was assigned if the intervention included as follows:
1 A representative sample
2 Appropriate report of the outcome variables
7.Description of the experimentalprotocol A positive point was assigned if the following criteria were
reported as follows:
1 Type of physicalexercise intervention
2 Exercise descriptions and loading characteristics (e.g.,intensity)
3 Intervention duration in weeks,training days per week,
and session duration
8.Description of the participant sample A positive point was assigned if the following criteria were
reported as follows:
A Age
B Sex
C Body height
D Body mass
E Activity level
F Health status (medication)
G Cognitive status
H Fallhistory
Numbers indicate full-point items while letters indicate subcategories of a one full-point item
Note that the internalvalidity increases with using better methods for quantification of fallincidence and implementation of intervention
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 5 of 19
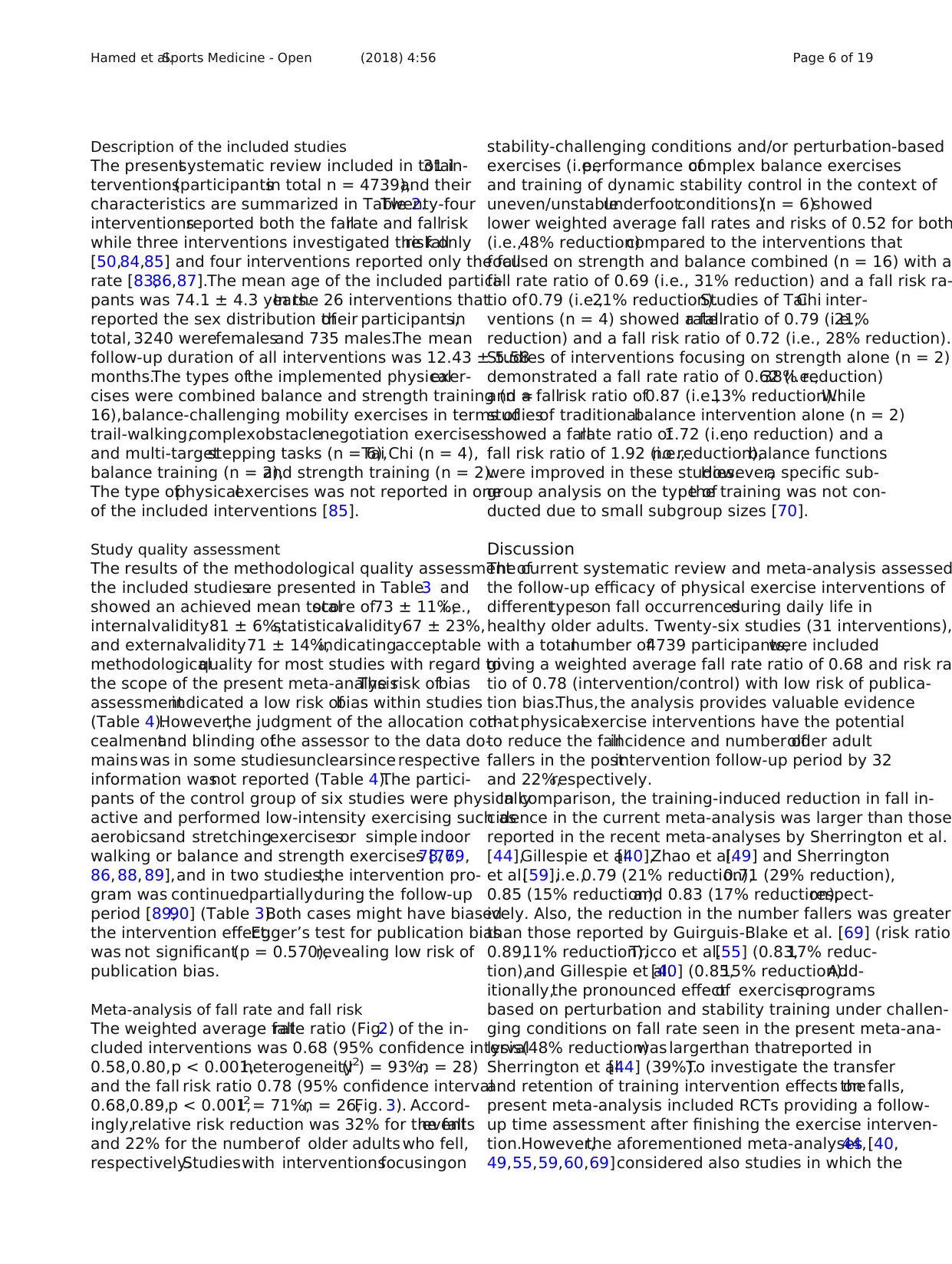
Description of the included studies
The presentsystematic review included in total31 in-
terventions(participantsin total n = 4739),and their
characteristics are summarized in Table 2.Twenty-four
interventionsreported both the fallrate and fallrisk
while three interventions investigated the fallrisk only
[50,84,85] and four interventions reported only the fall
rate [83,86,87].The mean age of the included partici-
pants was 74.1 ± 4.3 years.In the 26 interventions that
reported the sex distribution oftheir participants,in
total, 3240 werefemalesand 735 males.The mean
follow-up duration of all interventions was 12.43 ± 5.58
months.The types ofthe implemented physicalexer-
cises were combined balance and strength training (n =
16),balance-challenging mobility exercises in terms of
trail-walking,complexobstaclenegotiation exercises
and multi-targetstepping tasks (n = 6),Tai Chi (n = 4),
balance training (n = 2),and strength training (n = 2).
The type ofphysicalexercises was not reported in one
of the included interventions [85].
Study quality assessment
The results of the methodological quality assessment of
the included studiesare presented in Table3 and
showed an achieved mean totalscore of73 ± 11%,i.e.,
internalvalidity81 ± 6%,statisticalvalidity67 ± 23%,
and externalvalidity71 ± 14%,indicatingacceptable
methodologicalquality for most studies with regard to
the scope of the present meta-analysis.The risk ofbias
assessmentindicated a low risk ofbias within studies
(Table 4).However,the judgment of the allocation con-
cealmentand blinding ofthe assessor to the data do-
mainswas in some studiesunclearsince respective
information wasnot reported (Table 4).The partici-
pants of the control group of six studies were physically
active and performed low-intensity exercising such as
aerobicsand stretchingexercisesor simple indoor
walking or balance and strength exercises [76,78,79,
86, 88, 89],and in two studies,the intervention pro-
gram was continuedpartiallyduring the follow-up
period [89,90] (Table 3).Both cases might have biased
the intervention effect.Egger’s test for publication bias
was not significant(p = 0.570),revealing low risk of
publication bias.
Meta-analysis of fall rate and fall risk
The weighted average fallrate ratio (Fig.2) of the in-
cluded interventions was 0.68 (95% confidence interval
0.58,0.80,p < 0.001,heterogeneity(I2) = 93%,n = 28)
and the fall risk ratio 0.78 (95% confidence interval
0.68,0.89,p < 0.001,I 2 = 71%,n = 26,Fig. 3). Accord-
ingly,relative risk reduction was 32% for the fallevents
and 22% for the numberof older adults who fell,
respectively.Studieswith interventionsfocusingon
stability-challenging conditions and/or perturbation-based
exercises (i.e.,performance ofcomplex balance exercises
and training of dynamic stability control in the context of
uneven/unstableunderfootconditions)(n = 6)showed
lower weighted average fall rates and risks of 0.52 for both
(i.e.,48% reduction)compared to the interventions that
focused on strength and balance combined (n = 16) with a
fall rate ratio of 0.69 (i.e., 31% reduction) and a fall risk ra-
tio of0.79 (i.e.,21% reduction).Studies of TaiChi inter-
ventions (n = 4) showed a fallrate ratio of 0.79 (i.e.,21%
reduction) and a fall risk ratio of 0.72 (i.e., 28% reduction).
Studies of interventions focusing on strength alone (n = 2)
demonstrated a fall rate ratio of 0.62 (i.e.,38% reduction)
and a fallrisk ratio of0.87 (i.e.,13% reduction).While
studiesof traditionalbalance intervention alone (n = 2)
showed a fallrate ratio of1.72 (i.e.,no reduction) and a
fall risk ratio of 1.92 (i.e.,no reduction),balance functions
were improved in these studies.However,a specific sub-
group analysis on the type ofthe training was not con-
ducted due to small subgroup sizes [70].
Discussion
The current systematic review and meta-analysis assessed
the follow-up efficacy of physical exercise interventions of
differenttypeson fall occurrencesduring daily life in
healthy older adults. Twenty-six studies (31 interventions),
with a totalnumber of4739 participants,were included
giving a weighted average fall rate ratio of 0.68 and risk ra
tio of 0.78 (intervention/control) with low risk of publica-
tion bias.Thus,the analysis provides valuable evidence
thatphysicalexercise interventions have the potential
to reduce the fallincidence and number ofolder adult
fallers in the postintervention follow-up period by 32
and 22%,respectively.
In comparison, the training-induced reduction in fall in-
cidence in the current meta-analysis was larger than those
reported in the recent meta-analyses by Sherrington et al.
[44],Gillespie et al.[40],Zhao et al.[49] and Sherrington
et al.[59],i.e.,0.79 (21% reduction),0.71 (29% reduction),
0.85 (15% reduction),and 0.83 (17% reduction),respect-
ively. Also, the reduction in the number fallers was greater
than those reported by Guirguis-Blake et al. [69] (risk ratio
0.89,11% reduction),Tricco et al.[55] (0.83,17% reduc-
tion),and Gillespie et al.[40] (0.85,15% reduction).Add-
itionally,the pronounced effectof exerciseprograms
based on perturbation and stability training under challen-
ging conditions on fall rate seen in the present meta-ana-
lysis(48% reduction)was largerthan thatreported in
Sherrington et al.[44] (39%).To investigate the transfer
and retention of training intervention effects on falls,the
present meta-analysis included RCTs providing a follow-
up time assessment after finishing the exercise interven-
tion.However,the aforementioned meta-analyses [40,44,
49,55,59,60,69]considered also studies in which the
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 6 of 19
The presentsystematic review included in total31 in-
terventions(participantsin total n = 4739),and their
characteristics are summarized in Table 2.Twenty-four
interventionsreported both the fallrate and fallrisk
while three interventions investigated the fallrisk only
[50,84,85] and four interventions reported only the fall
rate [83,86,87].The mean age of the included partici-
pants was 74.1 ± 4.3 years.In the 26 interventions that
reported the sex distribution oftheir participants,in
total, 3240 werefemalesand 735 males.The mean
follow-up duration of all interventions was 12.43 ± 5.58
months.The types ofthe implemented physicalexer-
cises were combined balance and strength training (n =
16),balance-challenging mobility exercises in terms of
trail-walking,complexobstaclenegotiation exercises
and multi-targetstepping tasks (n = 6),Tai Chi (n = 4),
balance training (n = 2),and strength training (n = 2).
The type ofphysicalexercises was not reported in one
of the included interventions [85].
Study quality assessment
The results of the methodological quality assessment of
the included studiesare presented in Table3 and
showed an achieved mean totalscore of73 ± 11%,i.e.,
internalvalidity81 ± 6%,statisticalvalidity67 ± 23%,
and externalvalidity71 ± 14%,indicatingacceptable
methodologicalquality for most studies with regard to
the scope of the present meta-analysis.The risk ofbias
assessmentindicated a low risk ofbias within studies
(Table 4).However,the judgment of the allocation con-
cealmentand blinding ofthe assessor to the data do-
mainswas in some studiesunclearsince respective
information wasnot reported (Table 4).The partici-
pants of the control group of six studies were physically
active and performed low-intensity exercising such as
aerobicsand stretchingexercisesor simple indoor
walking or balance and strength exercises [76,78,79,
86, 88, 89],and in two studies,the intervention pro-
gram was continuedpartiallyduring the follow-up
period [89,90] (Table 3).Both cases might have biased
the intervention effect.Egger’s test for publication bias
was not significant(p = 0.570),revealing low risk of
publication bias.
Meta-analysis of fall rate and fall risk
The weighted average fallrate ratio (Fig.2) of the in-
cluded interventions was 0.68 (95% confidence interval
0.58,0.80,p < 0.001,heterogeneity(I2) = 93%,n = 28)
and the fall risk ratio 0.78 (95% confidence interval
0.68,0.89,p < 0.001,I 2 = 71%,n = 26,Fig. 3). Accord-
ingly,relative risk reduction was 32% for the fallevents
and 22% for the numberof older adults who fell,
respectively.Studieswith interventionsfocusingon
stability-challenging conditions and/or perturbation-based
exercises (i.e.,performance ofcomplex balance exercises
and training of dynamic stability control in the context of
uneven/unstableunderfootconditions)(n = 6)showed
lower weighted average fall rates and risks of 0.52 for both
(i.e.,48% reduction)compared to the interventions that
focused on strength and balance combined (n = 16) with a
fall rate ratio of 0.69 (i.e., 31% reduction) and a fall risk ra-
tio of0.79 (i.e.,21% reduction).Studies of TaiChi inter-
ventions (n = 4) showed a fallrate ratio of 0.79 (i.e.,21%
reduction) and a fall risk ratio of 0.72 (i.e., 28% reduction).
Studies of interventions focusing on strength alone (n = 2)
demonstrated a fall rate ratio of 0.62 (i.e.,38% reduction)
and a fallrisk ratio of0.87 (i.e.,13% reduction).While
studiesof traditionalbalance intervention alone (n = 2)
showed a fallrate ratio of1.72 (i.e.,no reduction) and a
fall risk ratio of 1.92 (i.e.,no reduction),balance functions
were improved in these studies.However,a specific sub-
group analysis on the type ofthe training was not con-
ducted due to small subgroup sizes [70].
Discussion
The current systematic review and meta-analysis assessed
the follow-up efficacy of physical exercise interventions of
differenttypeson fall occurrencesduring daily life in
healthy older adults. Twenty-six studies (31 interventions),
with a totalnumber of4739 participants,were included
giving a weighted average fall rate ratio of 0.68 and risk ra
tio of 0.78 (intervention/control) with low risk of publica-
tion bias.Thus,the analysis provides valuable evidence
thatphysicalexercise interventions have the potential
to reduce the fallincidence and number ofolder adult
fallers in the postintervention follow-up period by 32
and 22%,respectively.
In comparison, the training-induced reduction in fall in-
cidence in the current meta-analysis was larger than those
reported in the recent meta-analyses by Sherrington et al.
[44],Gillespie et al.[40],Zhao et al.[49] and Sherrington
et al.[59],i.e.,0.79 (21% reduction),0.71 (29% reduction),
0.85 (15% reduction),and 0.83 (17% reduction),respect-
ively. Also, the reduction in the number fallers was greater
than those reported by Guirguis-Blake et al. [69] (risk ratio
0.89,11% reduction),Tricco et al.[55] (0.83,17% reduc-
tion),and Gillespie et al.[40] (0.85,15% reduction).Add-
itionally,the pronounced effectof exerciseprograms
based on perturbation and stability training under challen-
ging conditions on fall rate seen in the present meta-ana-
lysis(48% reduction)was largerthan thatreported in
Sherrington et al.[44] (39%).To investigate the transfer
and retention of training intervention effects on falls,the
present meta-analysis included RCTs providing a follow-
up time assessment after finishing the exercise interven-
tion.However,the aforementioned meta-analyses [40,44,
49,55,59,60,69]considered also studies in which the
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 6 of 19
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
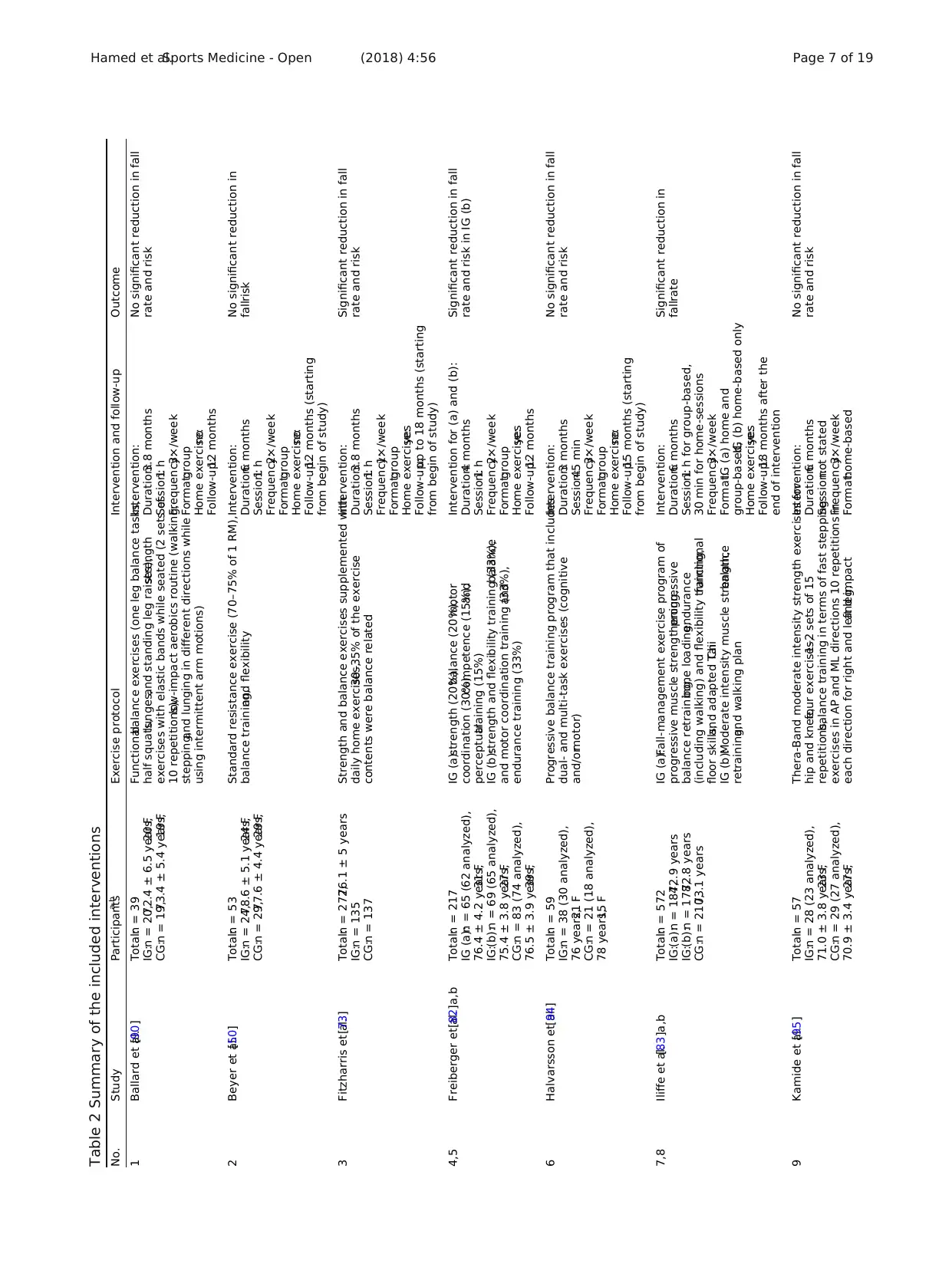
Table 2 Summary of the included interventions
No. Study Participantsa,b Exercise protocol Intervention and follow-up Outcome
1 Ballard et al.[90] Total:n = 39
IG:n = 20,72.4 ± 6.5 years,20 F
CG:n = 19,73.4 ± 5.4 years,19 F
Functionalbalance exercises (one leg balance tasks,
half squats,lunges,and standing leg raises),strength
exercises with elastic bands while seated (2 sets of
10 repetitions),low-impact aerobics routine (walking,
stepping,and lunging in different directions while
using intermittent arm motions)
Intervention:
Duration:3.8 months
Session:1 h
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:12 months
No significant reduction in fall
rate and risk
2 Beyer et al.[50] Total:n = 53
IG:n = 24,78.6 ± 5.1 years,24 F
CG:n = 29,77.6 ± 4.4 years,29 F
Standard resistance exercise (70–75% of 1 RM),
balance training,and flexibility
Intervention:
Duration:6 months
Session:1 h
Frequency:2×/week
Format:group
Home exercise:no
Follow-up:12 months (starting
from begin of study)
No significant reduction in
fallrisk
3 Fitzharris et al.[73] Total:n = 272,76.1 ± 5 years
IG:n = 135
CG:n = 137
Strength and balance exercises supplemented with
daily home exercises,30–35% of the exercise
contents were balance related
Intervention:
Duration:3.8 months
Session:1 h
Frequency:1×/week
Format:group
Home exercise:yes
Follow-up:up to 18 months (starting
from begin of study)
Significant reduction in fall
rate and risk
4,5 Freiberger et al.[82]a,b Total:n = 217
IG (a):n = 65 (62 analyzed),
76.4 ± 4.2 years,31 F
IG:(b):n = 69 (65 analyzed),
75.4 ± 3.8 years,27 F
CG:n = 83 (74 analyzed),
76.5 ± 3.9 years,39 F
IG (a):strength (20%),balance (20%),motor
coordination (30%),competence (15%),and
perceptualtraining (15%)
IG (b):strength and flexibility training (33%),balance
and motor coordination training (33%),and
endurance training (33%)
Intervention for (a) and (b):
Duration:4 months
Session:1 h
Frequency:2×/week
Format:group
Home exercise:yes
Follow-up:12 months
Significant reduction in fall
rate and risk in IG (b)
6 Halvarsson et al.[94] Total:n = 59
IG:n = 38 (30 analyzed),
76 years,21 F
CG:n = 21 (18 analyzed),
78 years,15 F
Progressive balance training program that includes
dual- and multi-task exercises (cognitive
and/ormotor)
Intervention:
Duration:3 months
Session:45 min
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:15 months (starting
from begin of study)
No significant reduction in fall
rate and risk
7,8 Iliffe et al.[83]a,b Total:n = 572
IG:(a):n = 184,72.9 years
IG:(b):n = 178,72.8 years
CG:n = 210,73.1 years
IG (a):Fall-management exercise program of
progressive muscle strengthening,progressive
balance retraining,bone loading,endurance
(including walking) and flexibility training,functional
floor skills,and adapted TaiChi
IG (b):Moderate intensity muscle strength,balance
retraining,and walking plan
Intervention:
Duration:6 months
Session:1 h for group-based,
30 min for home-sessions
Frequency:3×/week
Format:IG (a) home and
group-based,IG (b) home-based only
Home exercise:yes
Follow-up:18 months after the
end of intervention
Significant reduction in
fallrate
9 Kamide et al.[95] Total:n = 57
IG:n = 28 (23 analyzed),
71.0 ± 3.8 years,23 F
CG:n = 29 (27 analyzed),
70.9 ± 3.4 years,27 F
Thera-Band moderate intensity strength exercises for
hip and knee,four exercises,1–2 sets of 15
repetitions,balance training in terms of fast stepping
exercises in AP and ML directions 10 repetitions in
each direction for right and left leg,and impact
Intervention:
Duration:6 months
Session:not stated
Frequency:3×/week
Format:home-based
No significant reduction in fall
rate and risk
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 7 of 19
No. Study Participantsa,b Exercise protocol Intervention and follow-up Outcome
1 Ballard et al.[90] Total:n = 39
IG:n = 20,72.4 ± 6.5 years,20 F
CG:n = 19,73.4 ± 5.4 years,19 F
Functionalbalance exercises (one leg balance tasks,
half squats,lunges,and standing leg raises),strength
exercises with elastic bands while seated (2 sets of
10 repetitions),low-impact aerobics routine (walking,
stepping,and lunging in different directions while
using intermittent arm motions)
Intervention:
Duration:3.8 months
Session:1 h
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:12 months
No significant reduction in fall
rate and risk
2 Beyer et al.[50] Total:n = 53
IG:n = 24,78.6 ± 5.1 years,24 F
CG:n = 29,77.6 ± 4.4 years,29 F
Standard resistance exercise (70–75% of 1 RM),
balance training,and flexibility
Intervention:
Duration:6 months
Session:1 h
Frequency:2×/week
Format:group
Home exercise:no
Follow-up:12 months (starting
from begin of study)
No significant reduction in
fallrisk
3 Fitzharris et al.[73] Total:n = 272,76.1 ± 5 years
IG:n = 135
CG:n = 137
Strength and balance exercises supplemented with
daily home exercises,30–35% of the exercise
contents were balance related
Intervention:
Duration:3.8 months
Session:1 h
Frequency:1×/week
Format:group
Home exercise:yes
Follow-up:up to 18 months (starting
from begin of study)
Significant reduction in fall
rate and risk
4,5 Freiberger et al.[82]a,b Total:n = 217
IG (a):n = 65 (62 analyzed),
76.4 ± 4.2 years,31 F
IG:(b):n = 69 (65 analyzed),
75.4 ± 3.8 years,27 F
CG:n = 83 (74 analyzed),
76.5 ± 3.9 years,39 F
IG (a):strength (20%),balance (20%),motor
coordination (30%),competence (15%),and
perceptualtraining (15%)
IG (b):strength and flexibility training (33%),balance
and motor coordination training (33%),and
endurance training (33%)
Intervention for (a) and (b):
Duration:4 months
Session:1 h
Frequency:2×/week
Format:group
Home exercise:yes
Follow-up:12 months
Significant reduction in fall
rate and risk in IG (b)
6 Halvarsson et al.[94] Total:n = 59
IG:n = 38 (30 analyzed),
76 years,21 F
CG:n = 21 (18 analyzed),
78 years,15 F
Progressive balance training program that includes
dual- and multi-task exercises (cognitive
and/ormotor)
Intervention:
Duration:3 months
Session:45 min
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:15 months (starting
from begin of study)
No significant reduction in fall
rate and risk
7,8 Iliffe et al.[83]a,b Total:n = 572
IG:(a):n = 184,72.9 years
IG:(b):n = 178,72.8 years
CG:n = 210,73.1 years
IG (a):Fall-management exercise program of
progressive muscle strengthening,progressive
balance retraining,bone loading,endurance
(including walking) and flexibility training,functional
floor skills,and adapted TaiChi
IG (b):Moderate intensity muscle strength,balance
retraining,and walking plan
Intervention:
Duration:6 months
Session:1 h for group-based,
30 min for home-sessions
Frequency:3×/week
Format:IG (a) home and
group-based,IG (b) home-based only
Home exercise:yes
Follow-up:18 months after the
end of intervention
Significant reduction in
fallrate
9 Kamide et al.[95] Total:n = 57
IG:n = 28 (23 analyzed),
71.0 ± 3.8 years,23 F
CG:n = 29 (27 analyzed),
70.9 ± 3.4 years,27 F
Thera-Band moderate intensity strength exercises for
hip and knee,four exercises,1–2 sets of 15
repetitions,balance training in terms of fast stepping
exercises in AP and ML directions 10 repetitions in
each direction for right and left leg,and impact
Intervention:
Duration:6 months
Session:not stated
Frequency:3×/week
Format:home-based
No significant reduction in fall
rate and risk
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 7 of 19
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
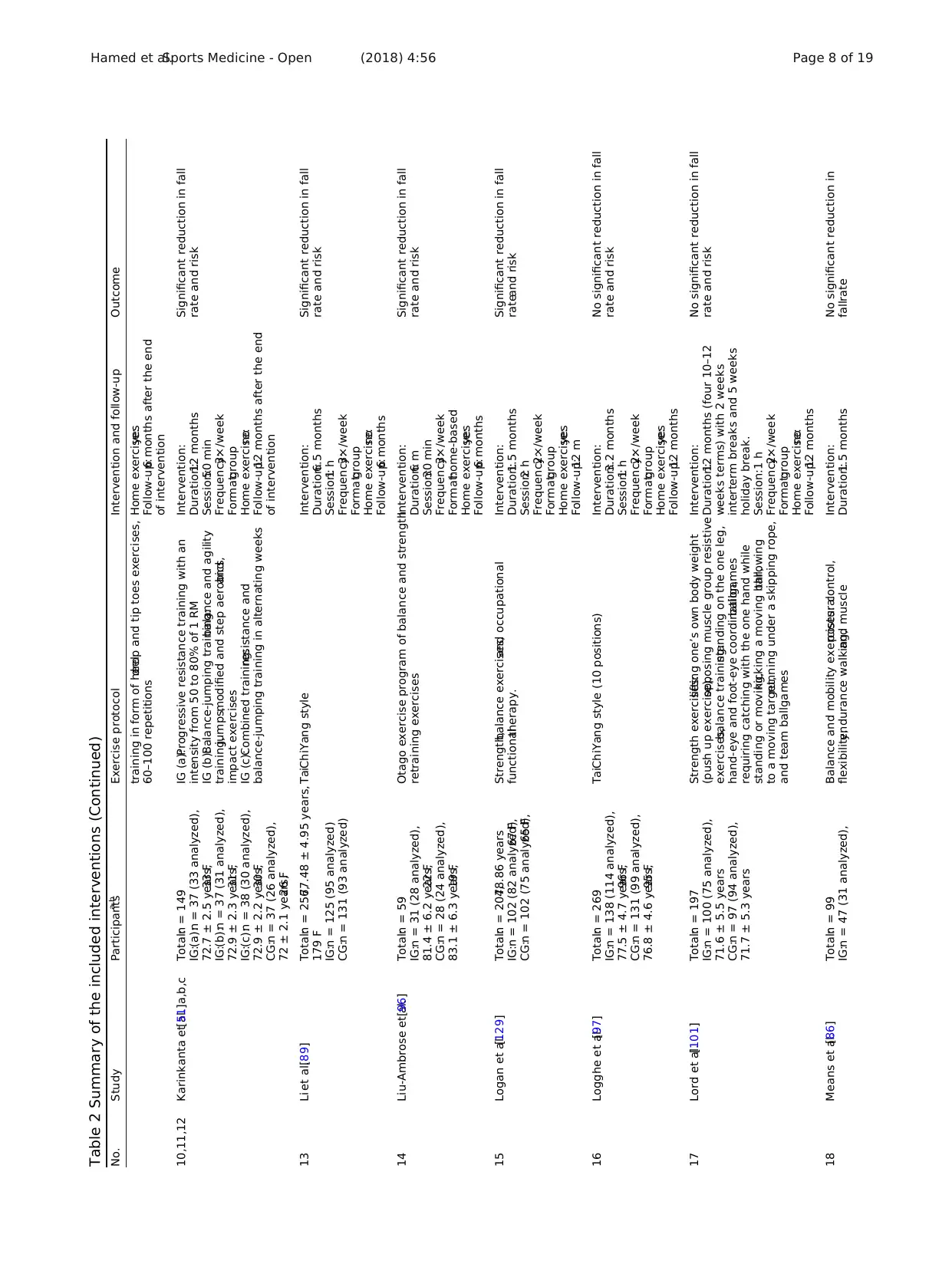
Table 2 Summary of the included interventions (Continued)
No. Study Participantsa,b Exercise protocol Intervention and follow-up Outcome
training in form of heeldrop and tip toes exercises,
60–100 repetitions
Home exercise:yes
Follow-up:6 months after the end
of intervention
10,11,12 Karinkanta et al.[51]a,b,c Total:n = 149
IG:(a):n = 37 (33 analyzed),
72.7 ± 2.5 years,33 F
IG:(b):n = 37 (31 analyzed),
72.9 ± 2.3 years,31 F
IG:(c):n = 38 (30 analyzed),
72.9 ± 2.2 years,30 F
CG:n = 37 (26 analyzed),
72 ± 2.1 years,26 F
IG (a):Progressive resistance training with an
intensity from 50 to 80% of 1 RM
IG (b):Balance-jumping training:balance and agility
training,jumps,modified and step aerobics,and
impact exercises
IG (c):Combined training:resistance and
balance-jumping training in alternating weeks
Intervention:
Duration:12 months
Session:50 min
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:12 months after the end
of intervention
Significant reduction in fall
rate and risk
13 Li et al.[89] Total:n = 256,77.48 ± 4.95 years,
179 F
IG:n = 125 (95 analyzed)
CG:n = 131 (93 analyzed)
TaiChiYang style Intervention:
Duration:6.5 months
Session:1 h
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:6 months
Significant reduction in fall
rate and risk
14 Liu-Ambrose et al.[96] Total:n = 59
IG:n = 31 (28 analyzed),
81.4 ± 6.2 years,22 F
CG:n = 28 (24 analyzed),
83.1 ± 6.3 years,19 F
Otago exercise program of balance and strength
retraining exercises
Intervention:
Duration:6 m
Session:30 min
Frequency:3×/week
Format:home-based
Home exercise:yes
Follow-up:6 months
Significant reduction in fall
rate and risk
15 Logan et al.[129] Total:n = 204,78.86 years
IG:n = 102 (82 analyzed),67 F
CG:n = 102 (75 analyzed),65 F
Strength,balance exercises,and occupational
functionaltherapy.
Intervention:
Duration:1.5 months
Session:2 h
Frequency:2×/week
Format:group
Home exercise:yes
Follow-up:12 m
Significant reduction in fall
rateand risk
16 Logghe et al.[97] Total:n = 269
IG:n = 138 (114 analyzed),
77.5 ± 4.7 years,96 F
CG:n = 131 (99 analyzed),
76.8 ± 4.6 years,95 F
TaiChiYang style (10 positions) Intervention:
Duration:3.2 months
Session:1 h
Frequency:2×/week
Format:group
Home exercise:yes
Follow-up:12 months
No significant reduction in fall
rate and risk
17 Lord et al.[101] Total:n = 197
IG:n = 100 (75 analyzed),
71.6 ± 5.5 years
CG:n = 97 (94 analyzed),
71.7 ± 5.3 years
Strength exercises:lifting one’s own body weight
(push up exercise),opposing muscle group resistive
exercises,balance training:standing on the one leg,
hand-eye and foot-eye coordination,ballgames
requiring catching with the one hand while
standing or moving,kicking a moving ball,throwing
to a moving target,running under a skipping rope,
and team ballgames
Intervention:
Duration:12 months (four 10–12
weeks terms) with 2 weeks
interterm breaks and 5 weeks
holiday break.
Session:1 h
Frequency:2×/week
Format:group
Home exercise:no
Follow-up:12 months
No significant reduction in fall
rate and risk
18 Means et al.[86] Total:n = 99
IG:n = 47 (31 analyzed),
Balance and mobility exercises:posturalcontrol,
flexibility,endurance walking,and muscle
Intervention:
Duration:1.5 months
No significant reduction in
fallrate
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 8 of 19
No. Study Participantsa,b Exercise protocol Intervention and follow-up Outcome
training in form of heeldrop and tip toes exercises,
60–100 repetitions
Home exercise:yes
Follow-up:6 months after the end
of intervention
10,11,12 Karinkanta et al.[51]a,b,c Total:n = 149
IG:(a):n = 37 (33 analyzed),
72.7 ± 2.5 years,33 F
IG:(b):n = 37 (31 analyzed),
72.9 ± 2.3 years,31 F
IG:(c):n = 38 (30 analyzed),
72.9 ± 2.2 years,30 F
CG:n = 37 (26 analyzed),
72 ± 2.1 years,26 F
IG (a):Progressive resistance training with an
intensity from 50 to 80% of 1 RM
IG (b):Balance-jumping training:balance and agility
training,jumps,modified and step aerobics,and
impact exercises
IG (c):Combined training:resistance and
balance-jumping training in alternating weeks
Intervention:
Duration:12 months
Session:50 min
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:12 months after the end
of intervention
Significant reduction in fall
rate and risk
13 Li et al.[89] Total:n = 256,77.48 ± 4.95 years,
179 F
IG:n = 125 (95 analyzed)
CG:n = 131 (93 analyzed)
TaiChiYang style Intervention:
Duration:6.5 months
Session:1 h
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:6 months
Significant reduction in fall
rate and risk
14 Liu-Ambrose et al.[96] Total:n = 59
IG:n = 31 (28 analyzed),
81.4 ± 6.2 years,22 F
CG:n = 28 (24 analyzed),
83.1 ± 6.3 years,19 F
Otago exercise program of balance and strength
retraining exercises
Intervention:
Duration:6 m
Session:30 min
Frequency:3×/week
Format:home-based
Home exercise:yes
Follow-up:6 months
Significant reduction in fall
rate and risk
15 Logan et al.[129] Total:n = 204,78.86 years
IG:n = 102 (82 analyzed),67 F
CG:n = 102 (75 analyzed),65 F
Strength,balance exercises,and occupational
functionaltherapy.
Intervention:
Duration:1.5 months
Session:2 h
Frequency:2×/week
Format:group
Home exercise:yes
Follow-up:12 m
Significant reduction in fall
rateand risk
16 Logghe et al.[97] Total:n = 269
IG:n = 138 (114 analyzed),
77.5 ± 4.7 years,96 F
CG:n = 131 (99 analyzed),
76.8 ± 4.6 years,95 F
TaiChiYang style (10 positions) Intervention:
Duration:3.2 months
Session:1 h
Frequency:2×/week
Format:group
Home exercise:yes
Follow-up:12 months
No significant reduction in fall
rate and risk
17 Lord et al.[101] Total:n = 197
IG:n = 100 (75 analyzed),
71.6 ± 5.5 years
CG:n = 97 (94 analyzed),
71.7 ± 5.3 years
Strength exercises:lifting one’s own body weight
(push up exercise),opposing muscle group resistive
exercises,balance training:standing on the one leg,
hand-eye and foot-eye coordination,ballgames
requiring catching with the one hand while
standing or moving,kicking a moving ball,throwing
to a moving target,running under a skipping rope,
and team ballgames
Intervention:
Duration:12 months (four 10–12
weeks terms) with 2 weeks
interterm breaks and 5 weeks
holiday break.
Session:1 h
Frequency:2×/week
Format:group
Home exercise:no
Follow-up:12 months
No significant reduction in fall
rate and risk
18 Means et al.[86] Total:n = 99
IG:n = 47 (31 analyzed),
Balance and mobility exercises:posturalcontrol,
flexibility,endurance walking,and muscle
Intervention:
Duration:1.5 months
No significant reduction in
fallrate
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 8 of 19
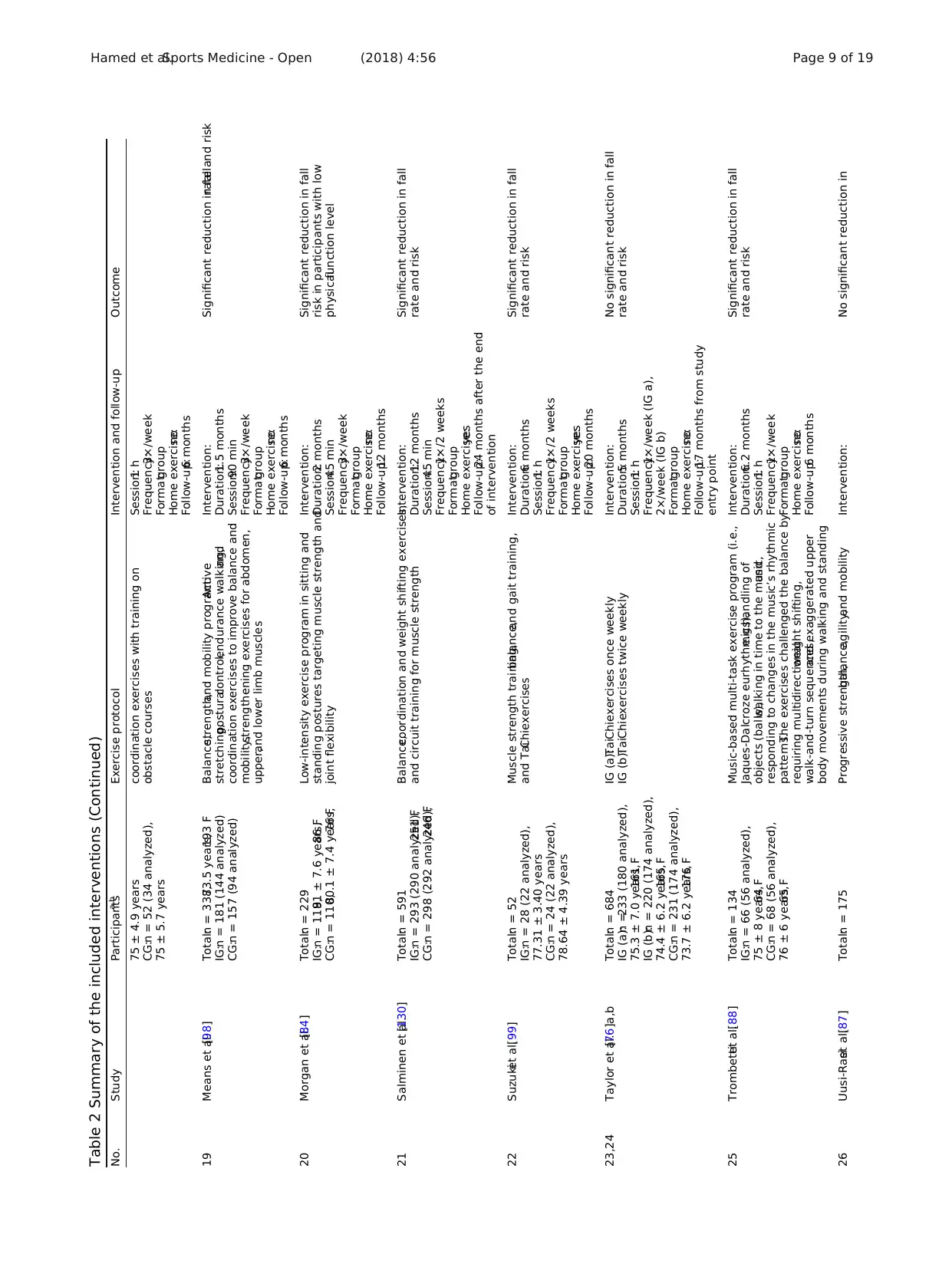
Table 2 Summary of the included interventions (Continued)
No. Study Participantsa,b Exercise protocol Intervention and follow-up Outcome
75 ± 4.9 years
CG:n = 52 (34 analyzed),
75 ± 5.7 years
coordination exercises with training on
obstacle courses
Session:1 h
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:6 months
19 Means et al.[98] Total:n = 338,73.5 years,193 F
IG:n = 181 (144 analyzed)
CG:n = 157 (94 analyzed)
Balance,strength,and mobility program:Active
stretching,posturalcontrol,endurance walking,and
coordination exercises to improve balance and
mobility,strengthening exercises for abdomen,
upper,and lower limb muscles
Intervention:
Duration:1.5 months
Session:90 min
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:6 months
Significant reduction in fallrate and risk
20 Morgan et al.[84] Total:n = 229
IG:n = 119,81 ± 7.6 years,86 F
CG:n = 110,80.1 ± 7.4 years,76 F
Low-intensity exercise program in sitting and
standing postures targeting muscle strength and
joint flexibility
Intervention:
Duration:2 months
Session:45 min
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:12 months
Significant reduction in fall
risk in participants with low
physicalfunction level
21 Salminen et al.[130] Total:n = 591
IG:n = 293 (290 analyzed),251 F
CG:n = 298 (292 analyzed),246 F
Balance,coordination and weight shifting exercises,
and circuit training for muscle strength
Intervention:
Duration:12 months
Session:45 min
Frequency:1×/2 weeks
Format:group
Home exercise:yes
Follow-up:24 months after the end
of intervention
Significant reduction in fall
rate and risk
22 Suzukiet al.[99] Total:n = 52
IG:n = 28 (22 analyzed),
77.31 ± 3.40 years
CG:n = 24 (22 analyzed),
78.64 ± 4.39 years
Muscle strength training,balance,and gait training,
and TaiChiexercises
Intervention:
Duration:6 months
Session:1 h
Frequency:1×/2 weeks
Format:group
Home exercise:yes
Follow-up:20 months
Significant reduction in fall
rate and risk
23,24 Taylor et al.[76]a,b Total:n = 684
IG (a):n =233 (180 analyzed),
75.3 ± 7.0 years,161 F
IG (b):n = 220 (174 analyzed),
74.4 ± 6.2 years,165 F
CG:n = 231 (174 analyzed),
73.7 ± 6.2 years,176 F
IG (a):TaiChiexercises once weekly
IG (b):TaiChiexercises twice weekly
Intervention:
Duration:5 months
Session:1 h
Frequency:1×/week (IG a),
2×/week (IG b)
Format:group
Home exercise:no
Follow-up:17 months from study
entry point
No significant reduction in fall
rate and risk
25 Trombettiet al.[88] Total:n = 134
IG:n = 66 (56 analyzed),
75 ± 8 years,64 F
CG:n = 68 (56 analyzed),
76 ± 6 years,65 F
Music-based multi-task exercise program (i.e.,
Jaques-Dalcroze eurhythmics),e.g.,handling of
objects (balls),walking in time to the music,and
responding to changes in the music’s rhythmic
patterns.The exercises challenged the balance by
requiring multidirectionalweight shifting,
walk-and-turn sequences,and exaggerated upper
body movements during walking and standing
Intervention:
Duration:6.2 months
Session:1 h
Frequency:1×/week
Format:group
Home exercise:no
Follow-up:6 months
Significant reduction in fall
rate and risk
26 Uusi-Rasiet al.[87] Total:n = 175 Progressive strength,balance,agility,and mobility Intervention: No significant reduction in
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 9 of 19
No. Study Participantsa,b Exercise protocol Intervention and follow-up Outcome
75 ± 4.9 years
CG:n = 52 (34 analyzed),
75 ± 5.7 years
coordination exercises with training on
obstacle courses
Session:1 h
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:6 months
19 Means et al.[98] Total:n = 338,73.5 years,193 F
IG:n = 181 (144 analyzed)
CG:n = 157 (94 analyzed)
Balance,strength,and mobility program:Active
stretching,posturalcontrol,endurance walking,and
coordination exercises to improve balance and
mobility,strengthening exercises for abdomen,
upper,and lower limb muscles
Intervention:
Duration:1.5 months
Session:90 min
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:6 months
Significant reduction in fallrate and risk
20 Morgan et al.[84] Total:n = 229
IG:n = 119,81 ± 7.6 years,86 F
CG:n = 110,80.1 ± 7.4 years,76 F
Low-intensity exercise program in sitting and
standing postures targeting muscle strength and
joint flexibility
Intervention:
Duration:2 months
Session:45 min
Frequency:3×/week
Format:group
Home exercise:no
Follow-up:12 months
Significant reduction in fall
risk in participants with low
physicalfunction level
21 Salminen et al.[130] Total:n = 591
IG:n = 293 (290 analyzed),251 F
CG:n = 298 (292 analyzed),246 F
Balance,coordination and weight shifting exercises,
and circuit training for muscle strength
Intervention:
Duration:12 months
Session:45 min
Frequency:1×/2 weeks
Format:group
Home exercise:yes
Follow-up:24 months after the end
of intervention
Significant reduction in fall
rate and risk
22 Suzukiet al.[99] Total:n = 52
IG:n = 28 (22 analyzed),
77.31 ± 3.40 years
CG:n = 24 (22 analyzed),
78.64 ± 4.39 years
Muscle strength training,balance,and gait training,
and TaiChiexercises
Intervention:
Duration:6 months
Session:1 h
Frequency:1×/2 weeks
Format:group
Home exercise:yes
Follow-up:20 months
Significant reduction in fall
rate and risk
23,24 Taylor et al.[76]a,b Total:n = 684
IG (a):n =233 (180 analyzed),
75.3 ± 7.0 years,161 F
IG (b):n = 220 (174 analyzed),
74.4 ± 6.2 years,165 F
CG:n = 231 (174 analyzed),
73.7 ± 6.2 years,176 F
IG (a):TaiChiexercises once weekly
IG (b):TaiChiexercises twice weekly
Intervention:
Duration:5 months
Session:1 h
Frequency:1×/week (IG a),
2×/week (IG b)
Format:group
Home exercise:no
Follow-up:17 months from study
entry point
No significant reduction in fall
rate and risk
25 Trombettiet al.[88] Total:n = 134
IG:n = 66 (56 analyzed),
75 ± 8 years,64 F
CG:n = 68 (56 analyzed),
76 ± 6 years,65 F
Music-based multi-task exercise program (i.e.,
Jaques-Dalcroze eurhythmics),e.g.,handling of
objects (balls),walking in time to the music,and
responding to changes in the music’s rhythmic
patterns.The exercises challenged the balance by
requiring multidirectionalweight shifting,
walk-and-turn sequences,and exaggerated upper
body movements during walking and standing
Intervention:
Duration:6.2 months
Session:1 h
Frequency:1×/week
Format:group
Home exercise:no
Follow-up:6 months
Significant reduction in fall
rate and risk
26 Uusi-Rasiet al.[87] Total:n = 175 Progressive strength,balance,agility,and mobility Intervention: No significant reduction in
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 9 of 19
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
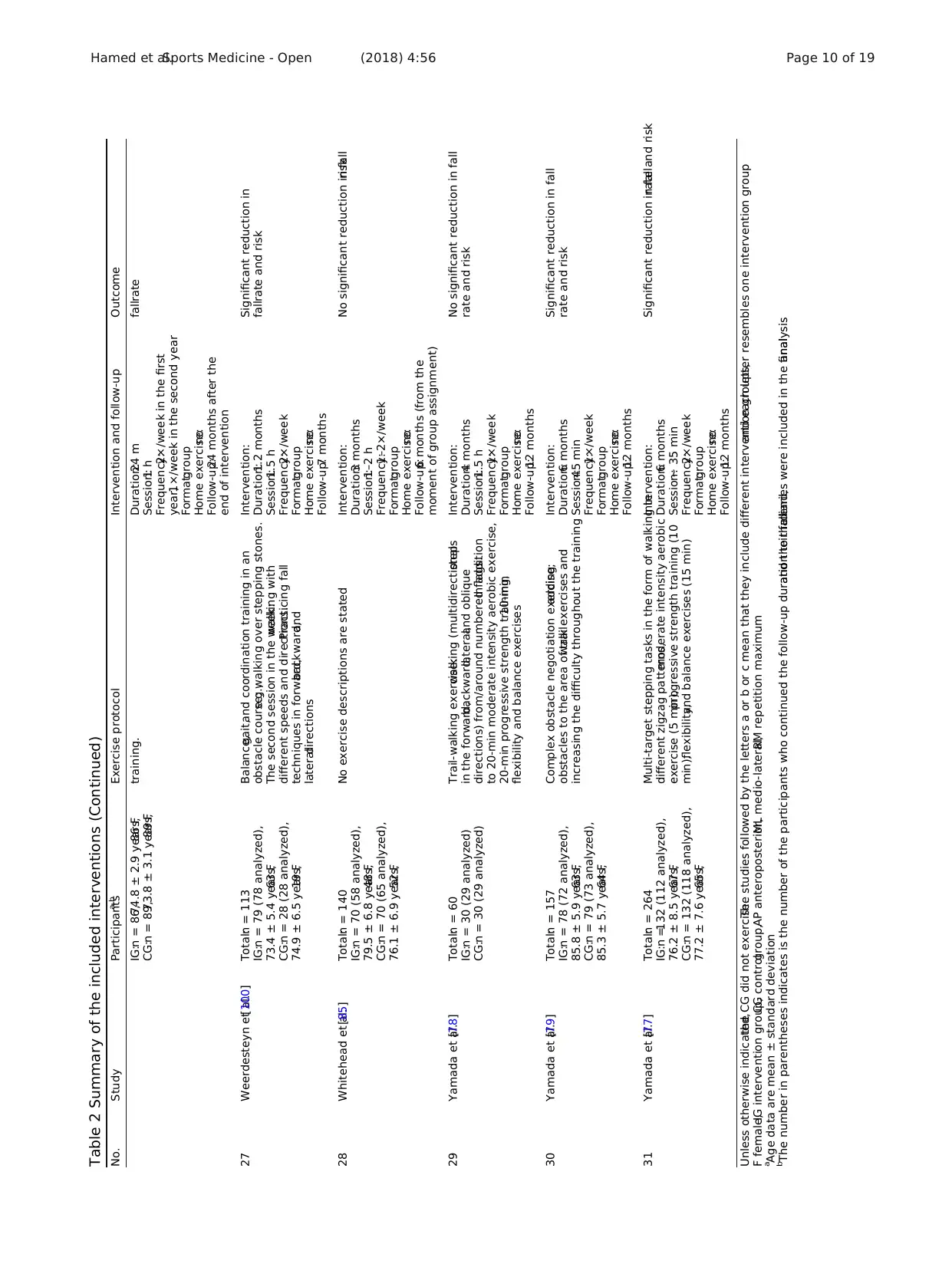
Table 2 Summary of the included interventions (Continued)
No. Study Participantsa,b Exercise protocol Intervention and follow-up Outcome
IG:n = 86,74.8 ± 2.9 years,86 F
CG:n = 89,73.8 ± 3.1 years,89 F
training. Duration:24 m
Session:1 h
Frequency:2×/week in the first
year,1×/week in the second year
Format:group
Home exercise:no
Follow-up:24 months after the
end of intervention
fallrate
27 Weerdesteyn et al.[100] Total:n = 113
IG:n = 79 (78 analyzed),
73.4 ± 5.4 years,63 F
CG:n = 28 (28 analyzed),
74.9 ± 6.5 years,19 F
Balance,gait,and coordination training in an
obstacle course;e.g.,walking over stepping stones.
The second session in the week:walking with
different speeds and directions.Practicing fall
techniques in forward,backward,and
lateraldirections
Intervention:
Duration:1.2 months
Session:1.5 h
Frequency:2×/week
Format:group
Home exercise:no
Follow-up:7 months
Significant reduction in
fallrate and risk
28 Whitehead et al.[85] Total:n = 140
IG:n = 70 (58 analyzed),
79.5 ± 6.8 years,48 F
CG:n = 70 (65 analyzed),
76.1 ± 6.9 years,52 F
No exercise descriptions are stated Intervention:
Duration:3 months
Session:1–2 h
Frequency:1–2×/week
Format:group
Home exercise:no
Follow-up:6 months (from the
moment of group assignment)
No significant reduction in fallrisk
29 Yamada et al.[78] Total:n = 60
IG:n = 30 (29 analyzed)
CG:n = 30 (29 analyzed)
Trail-walking exercise:walking (multidirectionalsteps
in the forward,backward,lateral,and oblique
directions) from/around numbered flags.In addition
to 20-min moderate intensity aerobic exercise,
20-min progressive strength training,10-min
flexibility and balance exercises
Intervention:
Duration:4 months
Session:1.5 h
Frequency:1×/week
Format:group
Home exercise:no
Follow-up:12 months
No significant reduction in fall
rate and risk
30 Yamada et al.[79] Total:n = 157
IG:n = 78 (72 analyzed),
85.8 ± 5.9 years,63 F
CG:n = 79 (73 analyzed),
85.3 ± 5.7 years,64 F
Complex obstacle negotiation exercise;adding
obstacles to the area of trailwalk exercises and
increasing the difficulty throughout the training
Intervention:
Duration:6 months
Session:45 min
Frequency:1×/week
Format:group
Home exercise:no
Follow-up:12 months
Significant reduction in fall
rate and risk
31 Yamada et al.[77] Total:n = 264
IG:n =132 (112 analyzed),
76.2 ± 8.5 years,67 F
CG:n = 132 (118 analyzed),
77.2 ± 7.6 years,65 F
Multi-target stepping tasks in the form of walking in
different zigzag patterns,moderate intensity aerobic
exercise (5 min),progressive strength training (10
min),flexibility,and balance exercises (15 min)
Intervention:
Duration:6 months
Session:~ 35 min
Frequency:2×/week
Format:group
Home exercise:no
Follow-up:12 months
Significant reduction in fallrate and risk
Unless otherwise indicated,the CG did not exercise.The studies followed by the letters a or b or c mean that they include different intervention groups,and each letter resembles one intervention group
F female,IG intervention group,CG controlgroup,AP anteroposterior,ML medio-lateral,RM repetition maximum
a
Age data are mean ± standard deviation
b
The number in parentheses indicates is the number of the participants who continued the follow-up duration to the end,and their falldiaries were included in the finalanalysis
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 10 of 19
No. Study Participantsa,b Exercise protocol Intervention and follow-up Outcome
IG:n = 86,74.8 ± 2.9 years,86 F
CG:n = 89,73.8 ± 3.1 years,89 F
training. Duration:24 m
Session:1 h
Frequency:2×/week in the first
year,1×/week in the second year
Format:group
Home exercise:no
Follow-up:24 months after the
end of intervention
fallrate
27 Weerdesteyn et al.[100] Total:n = 113
IG:n = 79 (78 analyzed),
73.4 ± 5.4 years,63 F
CG:n = 28 (28 analyzed),
74.9 ± 6.5 years,19 F
Balance,gait,and coordination training in an
obstacle course;e.g.,walking over stepping stones.
The second session in the week:walking with
different speeds and directions.Practicing fall
techniques in forward,backward,and
lateraldirections
Intervention:
Duration:1.2 months
Session:1.5 h
Frequency:2×/week
Format:group
Home exercise:no
Follow-up:7 months
Significant reduction in
fallrate and risk
28 Whitehead et al.[85] Total:n = 140
IG:n = 70 (58 analyzed),
79.5 ± 6.8 years,48 F
CG:n = 70 (65 analyzed),
76.1 ± 6.9 years,52 F
No exercise descriptions are stated Intervention:
Duration:3 months
Session:1–2 h
Frequency:1–2×/week
Format:group
Home exercise:no
Follow-up:6 months (from the
moment of group assignment)
No significant reduction in fallrisk
29 Yamada et al.[78] Total:n = 60
IG:n = 30 (29 analyzed)
CG:n = 30 (29 analyzed)
Trail-walking exercise:walking (multidirectionalsteps
in the forward,backward,lateral,and oblique
directions) from/around numbered flags.In addition
to 20-min moderate intensity aerobic exercise,
20-min progressive strength training,10-min
flexibility and balance exercises
Intervention:
Duration:4 months
Session:1.5 h
Frequency:1×/week
Format:group
Home exercise:no
Follow-up:12 months
No significant reduction in fall
rate and risk
30 Yamada et al.[79] Total:n = 157
IG:n = 78 (72 analyzed),
85.8 ± 5.9 years,63 F
CG:n = 79 (73 analyzed),
85.3 ± 5.7 years,64 F
Complex obstacle negotiation exercise;adding
obstacles to the area of trailwalk exercises and
increasing the difficulty throughout the training
Intervention:
Duration:6 months
Session:45 min
Frequency:1×/week
Format:group
Home exercise:no
Follow-up:12 months
Significant reduction in fall
rate and risk
31 Yamada et al.[77] Total:n = 264
IG:n =132 (112 analyzed),
76.2 ± 8.5 years,67 F
CG:n = 132 (118 analyzed),
77.2 ± 7.6 years,65 F
Multi-target stepping tasks in the form of walking in
different zigzag patterns,moderate intensity aerobic
exercise (5 min),progressive strength training (10
min),flexibility,and balance exercises (15 min)
Intervention:
Duration:6 months
Session:~ 35 min
Frequency:2×/week
Format:group
Home exercise:no
Follow-up:12 months
Significant reduction in fallrate and risk
Unless otherwise indicated,the CG did not exercise.The studies followed by the letters a or b or c mean that they include different intervention groups,and each letter resembles one intervention group
F female,IG intervention group,CG controlgroup,AP anteroposterior,ML medio-lateral,RM repetition maximum
a
Age data are mean ± standard deviation
b
The number in parentheses indicates is the number of the participants who continued the follow-up duration to the end,and their falldiaries were included in the finalanalysis
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 10 of 19
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
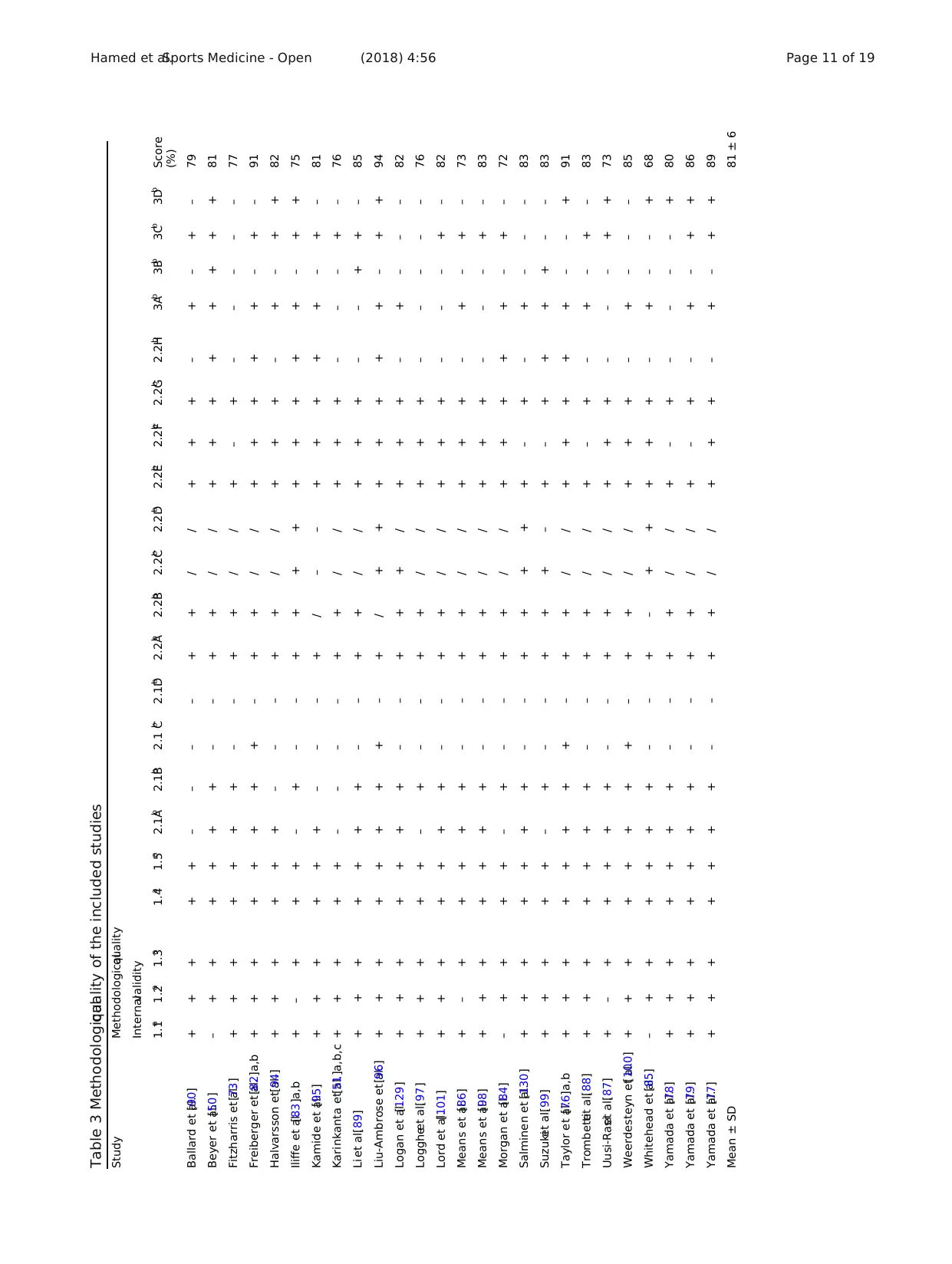
Table 3 Methodologicalquality of the included studies
Study Methodologicalquality
Internalvalidity
1.1a 1.2a 1.3a 1.4a 1.5a 2.1Ab 2.1Bb 2.1 Cb 2.1Db 2.2Ab 2.2Bb 2.2Cb 2.2Db 2.2Eb 2.2Fb 2.2Gb 2.2Hb 3Ab 3Bb 3Cb 3Db Score
(%)
Ballard et al.[90] + + + + + – – – – + + / / + + + – + – + – 79
Beyer et al.[50] – + + + + + + – – + + / / + + + + + + + + 81
Fitzharris et al.[73] + + + + + + + – – + + / / + – + – – – – – 77
Freiberger et al.[82]a,b + + + + + + + + – + + / / + + + + + – + – 91
Halvarsson et al.[94] + + + + + + – – – + + / / + + + – + – + + 82
Iliffe et al.[83]a,b + – + + + – + – – + + + + + + + + + – + + 75
Kamide et al.[95] + + + + + + – – – + / – – + + + + + – + – 81
Karinkanta et al.[51]a,b,c + + + + + – – – – + + / / + + + – – – + – 76
Li et al.[89] + + + + + + + – – + + / / + + + – – + + – 85
Liu-Ambrose et al.[96] + + + + + + + + – + / + + + + + + + – + + 94
Logan et al.[129] + + + + + + + – – + + + / + + + – + – – – 82
Loggheet al.[97] + + + + + – + – – + + / / + + + – – – – – 76
Lord et al.[101] + + + + + + + – – + + / / + + + – – – + – 82
Means et al.[86] + – + + + + + – – + + / / + + + – + – + – 73
Means et al.[98] + + + + + + + – – + + / / + + + – – – + – 83
Morgan et al.[84] – + + + + – + – – + + / / + + + + + – + – 72
Salminen et al.[130] + + + + + + + – – + + + + + – + – + – – – 83
Suzukiet al.[99] + + + + + – + – – + + + – + – + + + + – – 83
Taylor et al.[76]a,b + + + + + + + + – + + / / + + + + + – – + 91
Trombettiet al.[88] + + + + + + + – – + + / / + – + – + – + – 83
Uusi-Rasiet al.[87] + – + + + + + – – + + / / + + + – – – + + 73
Weerdesteyn et al.[100] + + + + + + + + – + + / / + + + – + – – – 85
Whitehead et al.[85] – + + + + + + – – + – + + + + + – + – – + 68
Yamada et al.[78] + + + + + + + – – + + / / + – + – – – – + 80
Yamada et al.[79] + + + + + + + – – + + / / + – + – + – + + 86
Yamada et al.[77] + + + + + + + – – + + / / + + + – + – + + 89
Mean ± SD 81 ± 6
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 11 of 19
Study Methodologicalquality
Internalvalidity
1.1a 1.2a 1.3a 1.4a 1.5a 2.1Ab 2.1Bb 2.1 Cb 2.1Db 2.2Ab 2.2Bb 2.2Cb 2.2Db 2.2Eb 2.2Fb 2.2Gb 2.2Hb 3Ab 3Bb 3Cb 3Db Score
(%)
Ballard et al.[90] + + + + + – – – – + + / / + + + – + – + – 79
Beyer et al.[50] – + + + + + + – – + + / / + + + + + + + + 81
Fitzharris et al.[73] + + + + + + + – – + + / / + – + – – – – – 77
Freiberger et al.[82]a,b + + + + + + + + – + + / / + + + + + – + – 91
Halvarsson et al.[94] + + + + + + – – – + + / / + + + – + – + + 82
Iliffe et al.[83]a,b + – + + + – + – – + + + + + + + + + – + + 75
Kamide et al.[95] + + + + + + – – – + / – – + + + + + – + – 81
Karinkanta et al.[51]a,b,c + + + + + – – – – + + / / + + + – – – + – 76
Li et al.[89] + + + + + + + – – + + / / + + + – – + + – 85
Liu-Ambrose et al.[96] + + + + + + + + – + / + + + + + + + – + + 94
Logan et al.[129] + + + + + + + – – + + + / + + + – + – – – 82
Loggheet al.[97] + + + + + – + – – + + / / + + + – – – – – 76
Lord et al.[101] + + + + + + + – – + + / / + + + – – – + – 82
Means et al.[86] + – + + + + + – – + + / / + + + – + – + – 73
Means et al.[98] + + + + + + + – – + + / / + + + – – – + – 83
Morgan et al.[84] – + + + + – + – – + + / / + + + + + – + – 72
Salminen et al.[130] + + + + + + + – – + + + + + – + – + – – – 83
Suzukiet al.[99] + + + + + – + – – + + + – + – + + + + – – 83
Taylor et al.[76]a,b + + + + + + + + – + + / / + + + + + – – + 91
Trombettiet al.[88] + + + + + + + – – + + / / + – + – + – + – 83
Uusi-Rasiet al.[87] + – + + + + + – – + + / / + + + – – – + + 73
Weerdesteyn et al.[100] + + + + + + + + – + + / / + + + – + – – – 85
Whitehead et al.[85] – + + + + + + – – + – + + + + + – + – – + 68
Yamada et al.[78] + + + + + + + – – + + / / + – + – – – – + 80
Yamada et al.[79] + + + + + + + – – + + / / + – + – + – + + 86
Yamada et al.[77] + + + + + + + – – + + / / + + + – + – + + 89
Mean ± SD 81 ± 6
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 11 of 19
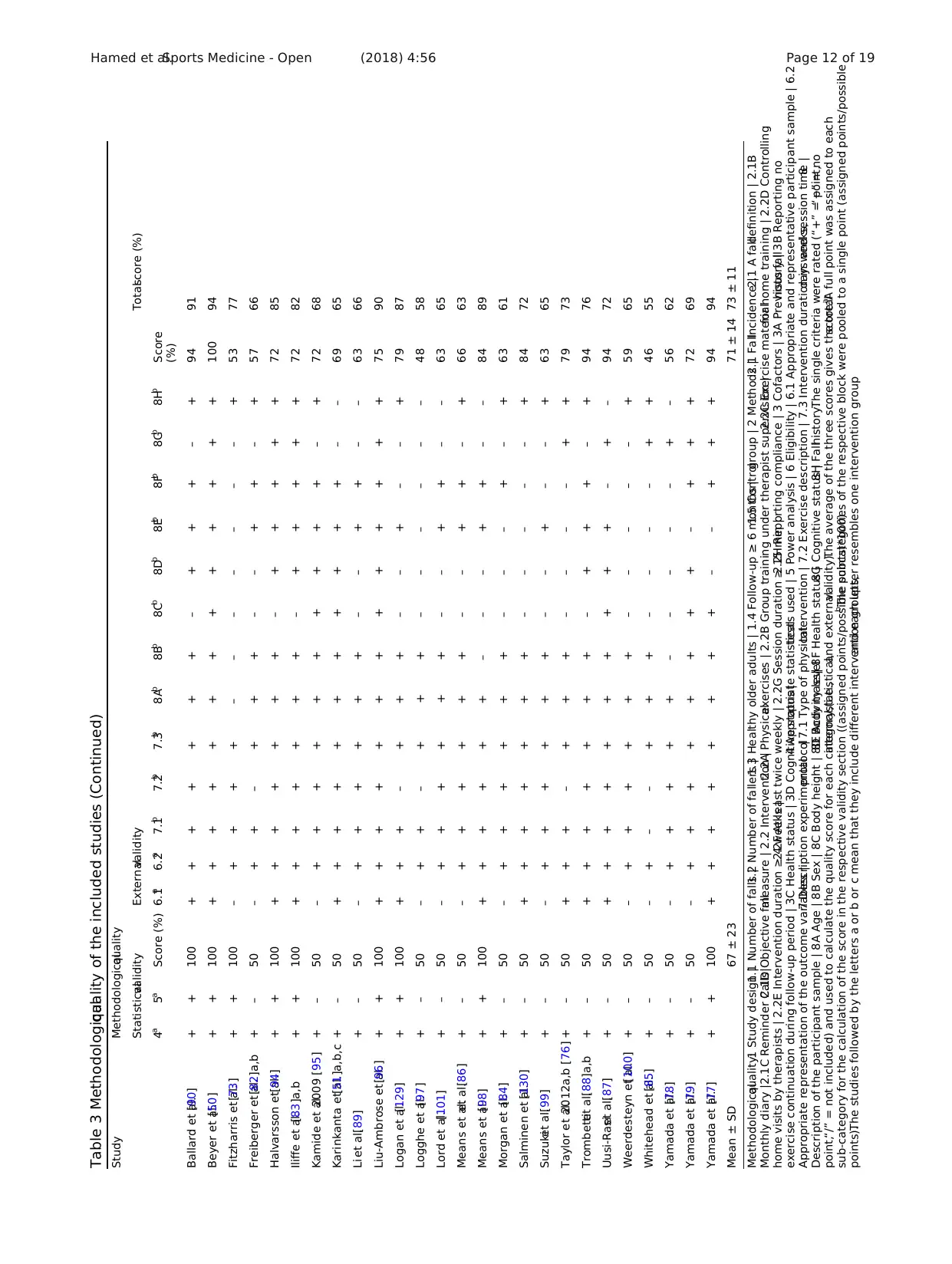
Table 3 Methodologicalquality of the included studies (Continued)
Study Methodologicalquality
Statisticalvalidity Externalvalidity Totalscore (%)
4a 5a Score (%) 6.1a 6.2a 7.1b 7.2b 7.3b 8Ab 8Bb 8Cb 8Db 8Eb 8Fb 8Gb 8Hb Score
(%)
Ballard et al.[90] + + 100 + + + + + + + – + + + – + 94 91
Beyer et al.[50] + + 100 + + + + + + + + + + + + + 100 94
Fitzharris et al.[73] + + 100 – + + + + – – – – – – – + 53 77
Freiberger et al.[82]a,b + – 50 – + + – + + + – – + + – + 57 66
Halvarsson et al.[94] + + 100 + + + + + + + – + + + + + 72 85
Iliffe et al.[83]a,b + + 100 + + + + + + + – + + + + + 72 82
Kamide et al.2009 [95] + – 50 – + + + + + + + + + + – + 72 68
Karinkanta et al.[51]a,b,c + – 50 + + + + + + + + + + + – – 69 65
Li et al.[89] + – 50 – + + + + + + – – + + – – 63 66
Liu-Ambrose et al.[96] + + 100 + + + + + + + + + + + + + 75 90
Logan et al.[129] + + 100 + + + – + + + – – + – – + 79 87
Logghe et al.[97] + – 50 – + + – + + + – – – – – – 48 58
Lord et al.[101] + – 50 – + + + + + + – – + + – – 63 65
Means et al.et al.[86] + – 50 – + + + + + + – – + + – + 66 63
Means et al.[98] + + 100 + + + + + + – – – + + – – 84 89
Morgan et al.[84] + – 50 – + + + + + + – – – + – + 63 61
Salminen et al.[130] + – 50 + + + + + + + – – – – – + 84 72
Suzukiet al.[99] + – 50 – + + + + + + – – + – – + 63 65
Taylor et al.2012a,b [76] + – 50 + + + – + + + – – – – + + 79 73
Trombettiet al.[88]a,b + – 50 + + + + + + + – + + + – + 94 76
Uusi-Rasiet al.[87] + – 50 + + + + + + + + + + – + – 94 72
Weerdesteyn et al.[100] + – 50 – + + + + + + – – – – – + 59 65
Whitehead et al.[85] + – 50 – + – – + + + – – – – + + 46 55
Yamada et al.[78] + – 50 – + + + + + – – – – – + – 56 62
Yamada et al.[79] + – 50 – + + + + + + + + – + + + 72 69
Yamada et al.[77] + + 100 + + + + + + + + – – + + + 94 94
Mean ± SD 67 ± 23 71 ± 14 73 ± 11
Methodologicalquality:1 Study design |1.1 Number of falls |1.2 Number of fallers |1.3 Healthy older adults | 1.4 Follow-up ≥ 6 months |1.5 Controlgroup | 2 Methods |2.1 FallIncidence |2.1 A falldefinition | 2.1B
Monthly diary |2.1C Reminder Calls|2.1D Objective fallmeasure | 2.2 Intervention |2.2A Physicalexercises | 2.2B Group training under therapist supervision |2.2C Exercise materialfor home training | 2.2D Controlling
home visits by therapists | 2.2E Intervention duration ≥ 4 weeks |2.2F At least twice weekly | 2.2G Session duration ≥ 15 min |2.2H Reporting compliance | 3 Cofactors | 3A Previous fallhistory | 3B Reporting no
exercise continuation during follow-up period | 3C Health status | 3D Cognitive status |4 Appropriate statisticaltests used | 5 Power analysis | 6 Eligibility | 6.1 Appropriate and representative participant sample | 6.2
Appropriate representation of the outcome variables |7 Description experimentalprotocol| 7.1 Type of physicalIntervention | 7.2 Exercise description | 7.3 Intervention duration in weeks,days and session time |8
Description of the participant sample | 8A Age | 8B Sex | 8C Body height | 8D Body mass|8E Activity level| 8F Health status |8G Cognitive status |8H Fallhistory.The single criteria were rated (“+” = point,“−” = no
point,“/” = not included) and used to calculate the quality score for each category (i.e.,internal,statistical,and externalvalidity).The average of the three scores gives the totalscore.a
A full point was assigned to each
sub-category for the calculation of the score in the respective validity section ((assigned points/possible points)*100).b
The subcategories of the respective block were pooled to a single point (assigned points/possible
points).The studies followed by the letters a or b or c mean that they include different intervention groups,and each letter resembles one intervention group
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 12 of 19
Study Methodologicalquality
Statisticalvalidity Externalvalidity Totalscore (%)
4a 5a Score (%) 6.1a 6.2a 7.1b 7.2b 7.3b 8Ab 8Bb 8Cb 8Db 8Eb 8Fb 8Gb 8Hb Score
(%)
Ballard et al.[90] + + 100 + + + + + + + – + + + – + 94 91
Beyer et al.[50] + + 100 + + + + + + + + + + + + + 100 94
Fitzharris et al.[73] + + 100 – + + + + – – – – – – – + 53 77
Freiberger et al.[82]a,b + – 50 – + + – + + + – – + + – + 57 66
Halvarsson et al.[94] + + 100 + + + + + + + – + + + + + 72 85
Iliffe et al.[83]a,b + + 100 + + + + + + + – + + + + + 72 82
Kamide et al.2009 [95] + – 50 – + + + + + + + + + + – + 72 68
Karinkanta et al.[51]a,b,c + – 50 + + + + + + + + + + + – – 69 65
Li et al.[89] + – 50 – + + + + + + – – + + – – 63 66
Liu-Ambrose et al.[96] + + 100 + + + + + + + + + + + + + 75 90
Logan et al.[129] + + 100 + + + – + + + – – + – – + 79 87
Logghe et al.[97] + – 50 – + + – + + + – – – – – – 48 58
Lord et al.[101] + – 50 – + + + + + + – – + + – – 63 65
Means et al.et al.[86] + – 50 – + + + + + + – – + + – + 66 63
Means et al.[98] + + 100 + + + + + + – – – + + – – 84 89
Morgan et al.[84] + – 50 – + + + + + + – – – + – + 63 61
Salminen et al.[130] + – 50 + + + + + + + – – – – – + 84 72
Suzukiet al.[99] + – 50 – + + + + + + – – + – – + 63 65
Taylor et al.2012a,b [76] + – 50 + + + – + + + – – – – + + 79 73
Trombettiet al.[88]a,b + – 50 + + + + + + + – + + + – + 94 76
Uusi-Rasiet al.[87] + – 50 + + + + + + + + + + – + – 94 72
Weerdesteyn et al.[100] + – 50 – + + + + + + – – – – – + 59 65
Whitehead et al.[85] + – 50 – + – – + + + – – – – + + 46 55
Yamada et al.[78] + – 50 – + + + + + – – – – – + – 56 62
Yamada et al.[79] + – 50 – + + + + + + + + – + + + 72 69
Yamada et al.[77] + + 100 + + + + + + + + – – + + + 94 94
Mean ± SD 67 ± 23 71 ± 14 73 ± 11
Methodologicalquality:1 Study design |1.1 Number of falls |1.2 Number of fallers |1.3 Healthy older adults | 1.4 Follow-up ≥ 6 months |1.5 Controlgroup | 2 Methods |2.1 FallIncidence |2.1 A falldefinition | 2.1B
Monthly diary |2.1C Reminder Calls|2.1D Objective fallmeasure | 2.2 Intervention |2.2A Physicalexercises | 2.2B Group training under therapist supervision |2.2C Exercise materialfor home training | 2.2D Controlling
home visits by therapists | 2.2E Intervention duration ≥ 4 weeks |2.2F At least twice weekly | 2.2G Session duration ≥ 15 min |2.2H Reporting compliance | 3 Cofactors | 3A Previous fallhistory | 3B Reporting no
exercise continuation during follow-up period | 3C Health status | 3D Cognitive status |4 Appropriate statisticaltests used | 5 Power analysis | 6 Eligibility | 6.1 Appropriate and representative participant sample | 6.2
Appropriate representation of the outcome variables |7 Description experimentalprotocol| 7.1 Type of physicalIntervention | 7.2 Exercise description | 7.3 Intervention duration in weeks,days and session time |8
Description of the participant sample | 8A Age | 8B Sex | 8C Body height | 8D Body mass|8E Activity level| 8F Health status |8G Cognitive status |8H Fallhistory.The single criteria were rated (“+” = point,“−” = no
point,“/” = not included) and used to calculate the quality score for each category (i.e.,internal,statistical,and externalvalidity).The average of the three scores gives the totalscore.a
A full point was assigned to each
sub-category for the calculation of the score in the respective validity section ((assigned points/possible points)*100).b
The subcategories of the respective block were pooled to a single point (assigned points/possible
points).The studies followed by the letters a or b or c mean that they include different intervention groups,and each letter resembles one intervention group
Hamed et al.Sports Medicine - Open (2018) 4:56 Page 12 of 19
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

