Tele-Rehabilitation: A Report on Discharged Patients' Needs
VerifiedAdded on 2021/05/31
|27
|7920
|271
Report
AI Summary
This report delves into the practice of tele-rehabilitation, specifically focusing on its application for patients discharged from hospitals. It introduces tele-rehabilitation as a method of providing rehabilitation services through communication and information technologies, encompassing various services like intervention, assessment, and counseling. The report highlights the implementation of tele-rehabilitation, illustrating how technological innovations enable healthcare professionals to deliver care remotely, including the use of online platforms, live feeds, and recorded sessions. It also outlines the roles of different staff members involved in tele-rehabilitation, such as doctors, nurses, ergophysiologists, psychologists, and IT personnel, and their respective responsibilities in patient care and program management. Furthermore, the report presents evidence supporting the effectiveness of tele-rehabilitation, citing successful applications in cardiology, chronic pain management, and mobility issues, while also acknowledging the need for further research. Overall, the report provides a comprehensive overview of tele-rehabilitation, its implementation strategies, the roles of healthcare professionals, and the evidence supporting its efficacy in improving patient outcomes. This report is a valuable resource for students and professionals seeking to understand and implement tele-rehabilitation practices.

Tele-Rehabilitation for Discharged Patients 1
Tele-Rehabilitation for Discharged Patients
By [Name]
Course
Professors’ Name
Institution
Location of Institution
Date
Tele-Rehabilitation for Discharged Patients
By [Name]
Course
Professors’ Name
Institution
Location of Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Tele-Rehabilitation for Discharged Patients 2
Introduction
Tele-rehabilitation is the process of giving rehabilitation services to patients through
communication and information technologies (Jackson et al. 2012, p.1088). In the clinical
field the term tele-rehabilitation comprises of many variety of rehabilitation services that
include intervention, monitoring, assessment, education, supervision, counselling and
consultation (Laver et al. 2013). The tele-rehabilitation services are usually done to children
and adults who have acquired injuries, developmental disorders or delays, and diseases by a
wide range of healthcare practitioners in the healthcare field (Piqueras et al. 2013, pp.392-
396). The professionals consists of the following of but are not limited to speech language
pathologist, physical therapist, rehabilitation physicians, nurses, occupational therapist,
rehabilitation engineers, audiologists, assistive technologists, dieticians, psychologists, and
teachers. The tele-rehabilitation has power to delivers rehabilitation services across all the
medical or healthcare areas and across all the lifespan. Tele-rehabilitation has a brad and
wide range of professionals, similarly, it has many types of services it can offer to all people
despite their ages (Koh et al. 2015, p. 151).
The services of tele-rehabilitation falls under two class according to Cook et al.
(2013) and Ambrosino et a. (2016) which include the clinical therapy and clinical assessment
which asses the ability of the patient to function in his or her own ecosystem (pp.1038-1047).
Tele-rehabilitation can provide rehabilitation services to patients who cannot go to the centres
due to factors like physical or mental disability, or because the time of travel is long and to
patients who have been already discharged from the hospitals. The discipline of tele-
rehabilitation services is rare and not many scholars have done research about it (Ambrosino
et al. 2016). There are two important areas to note in tele-rehabilitation which include coming
up with the system which has new data that can help the professional deliver rehabilitation
Introduction
Tele-rehabilitation is the process of giving rehabilitation services to patients through
communication and information technologies (Jackson et al. 2012, p.1088). In the clinical
field the term tele-rehabilitation comprises of many variety of rehabilitation services that
include intervention, monitoring, assessment, education, supervision, counselling and
consultation (Laver et al. 2013). The tele-rehabilitation services are usually done to children
and adults who have acquired injuries, developmental disorders or delays, and diseases by a
wide range of healthcare practitioners in the healthcare field (Piqueras et al. 2013, pp.392-
396). The professionals consists of the following of but are not limited to speech language
pathologist, physical therapist, rehabilitation physicians, nurses, occupational therapist,
rehabilitation engineers, audiologists, assistive technologists, dieticians, psychologists, and
teachers. The tele-rehabilitation has power to delivers rehabilitation services across all the
medical or healthcare areas and across all the lifespan. Tele-rehabilitation has a brad and
wide range of professionals, similarly, it has many types of services it can offer to all people
despite their ages (Koh et al. 2015, p. 151).
The services of tele-rehabilitation falls under two class according to Cook et al.
(2013) and Ambrosino et a. (2016) which include the clinical therapy and clinical assessment
which asses the ability of the patient to function in his or her own ecosystem (pp.1038-1047).
Tele-rehabilitation can provide rehabilitation services to patients who cannot go to the centres
due to factors like physical or mental disability, or because the time of travel is long and to
patients who have been already discharged from the hospitals. The discipline of tele-
rehabilitation services is rare and not many scholars have done research about it (Ambrosino
et al. 2016). There are two important areas to note in tele-rehabilitation which include coming
up with the system which has new data that can help the professional deliver rehabilitation
Tele-Rehabilitation for Discharged Patients 3
services online (Avila et al. 2014, pp. 1-5). Second, giving rehabilitation services which are
in line with the code of conducts of rehabilitation field (Avila et al. 2014, pp. 1-5).
Implementation of Tele-Rehabilitation for Patients after being discharged from
Hospital
The technological innovations in the healthcare field have allowed the medical
practitioners to come up with new ways of administering health services to patients both at
home and in the hospital (van den Berg et al. 2016, pp.1885-1892. The discharged patients
can also get medical attention and rehabilitation services through new technologies. The tele-
rehabilitation services are one of the many healthcare technological innovations. As
Siemonsma et al. (2014) reported, many patients who were placed in the intensive care units
due to the chronic diseases, disorders, or fatal accidents recover and go home (pp.2019-
2030).
However, these patients do not recover completely, they always require rehabilitation
to enable them pass the emotional stress of what they suffered. Some of the patients may not
be able to go back for rehabilitation in the hospital facility because of reasons like insufficient
money and time (Kairy et al. 2016, pp.201-206). Therefore, tele-rehabilitation can come to
the aid of these kinds of patients. In the hospital I am working as an occupational therapist we
use tele-rehabilitation platform which comprise fine-grained and mature services which
support the online/real-time and off the internet connections between the hospital healthcare
workers and the patient. When there is an online or real-time interaction, a large hall is used
where a group of up to ten patients are rehabilitated with one medical professional that is
either me or my colleagues. For those that are online a high definition webcam is used to
connect the healthcare worker and the patient. The offline platform is where one of the
medical professional records a rehabilitation processes with a camera and the hospital posts
services online (Avila et al. 2014, pp. 1-5). Second, giving rehabilitation services which are
in line with the code of conducts of rehabilitation field (Avila et al. 2014, pp. 1-5).
Implementation of Tele-Rehabilitation for Patients after being discharged from
Hospital
The technological innovations in the healthcare field have allowed the medical
practitioners to come up with new ways of administering health services to patients both at
home and in the hospital (van den Berg et al. 2016, pp.1885-1892. The discharged patients
can also get medical attention and rehabilitation services through new technologies. The tele-
rehabilitation services are one of the many healthcare technological innovations. As
Siemonsma et al. (2014) reported, many patients who were placed in the intensive care units
due to the chronic diseases, disorders, or fatal accidents recover and go home (pp.2019-
2030).
However, these patients do not recover completely, they always require rehabilitation
to enable them pass the emotional stress of what they suffered. Some of the patients may not
be able to go back for rehabilitation in the hospital facility because of reasons like insufficient
money and time (Kairy et al. 2016, pp.201-206). Therefore, tele-rehabilitation can come to
the aid of these kinds of patients. In the hospital I am working as an occupational therapist we
use tele-rehabilitation platform which comprise fine-grained and mature services which
support the online/real-time and off the internet connections between the hospital healthcare
workers and the patient. When there is an online or real-time interaction, a large hall is used
where a group of up to ten patients are rehabilitated with one medical professional that is
either me or my colleagues. For those that are online a high definition webcam is used to
connect the healthcare worker and the patient. The offline platform is where one of the
medical professional records a rehabilitation processes with a camera and the hospital posts
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Tele-Rehabilitation for Discharged Patients 4
the information in the internet either YouTube or Facebook for patients to view later
especially those who missed the online session (Artz et al. 2015, p. 15).
Tele-rehabilitation service can be implemented by many healthcare workers in the
hospital are at home (Gregersen et al. 2016, p. 809). Personally I administer tele-
rehabilitation services at my house through my YouTube channel. For example, when I am
showing my patient who needs rehabilitation to walk properly, I record the details of what the
patients need to do by showing example using my assistant show all the steps to be followed
and then post the recording in my YouTube channel where my patients will get and watch the
video. At the hospital in my work place, the exercise is done online where the practitioners
show the patients what they need to do in the live feeds. The advantage of using live tele-
rehabilitation, there is immediate feedback from the patient. In other words patients and the
medical professional interact in real-time.
The tele-rehabilitation service can be implemented through many channels for
example, blogs and websites (Agostini et al. 2015, pp.202-213; Gregersen et al. 2016, p.
809). I use blog to write to my patients on what they need to do to overcome certain problem.
My hospital also has an official website where they post any information that can help
patients recover from emotional and physical stress; the data also help in the rehabilitation
process. The gadgets that can be used to implement the tele-rehabilitation services include the
smartphones, tablets, laptops and desktops and using the internet connection (Bernocchi et al.
2016, pp.106-115). Artz et al. (2015, p. 15) suggest that the new technological advancements
have improved the healthcare services.
the information in the internet either YouTube or Facebook for patients to view later
especially those who missed the online session (Artz et al. 2015, p. 15).
Tele-rehabilitation service can be implemented by many healthcare workers in the
hospital are at home (Gregersen et al. 2016, p. 809). Personally I administer tele-
rehabilitation services at my house through my YouTube channel. For example, when I am
showing my patient who needs rehabilitation to walk properly, I record the details of what the
patients need to do by showing example using my assistant show all the steps to be followed
and then post the recording in my YouTube channel where my patients will get and watch the
video. At the hospital in my work place, the exercise is done online where the practitioners
show the patients what they need to do in the live feeds. The advantage of using live tele-
rehabilitation, there is immediate feedback from the patient. In other words patients and the
medical professional interact in real-time.
The tele-rehabilitation service can be implemented through many channels for
example, blogs and websites (Agostini et al. 2015, pp.202-213; Gregersen et al. 2016, p.
809). I use blog to write to my patients on what they need to do to overcome certain problem.
My hospital also has an official website where they post any information that can help
patients recover from emotional and physical stress; the data also help in the rehabilitation
process. The gadgets that can be used to implement the tele-rehabilitation services include the
smartphones, tablets, laptops and desktops and using the internet connection (Bernocchi et al.
2016, pp.106-115). Artz et al. (2015, p. 15) suggest that the new technological advancements
have improved the healthcare services.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Tele-Rehabilitation for Discharged Patients 5
Roles of some of the Tele-rehabilitation Staff
Implementation of the tele-rehabilitation programs for patients require work force
from different levels in the healthcare which include the medical professionals, information
technology personnel, and the marketing department (Bernocchi et al. 2016, pp.106-115).
The marketing department advertises the services offered by the tele-rehabilitation facility to
the discharged patients and give them links on how to join the program. In term of medical
services there is the doctor, nurse, ergophysiologist, physiotherapist, and psychologist (Jin et
al. 2015, p. 61; Vloothuis et al. 2015, p. 193; Kairy et al. 2016, pp.201-206).
The doctor has numerous roles in tele-rehabilitation which include one, preserving
the patients’ medical records and hi/her history (Kairy et al. 2016, pp.201-206). Second, the
doctor is also responsible for performing the clinical evaluation of the patient after and before
the tele-rehabilitation services. The doctor is also obligated to prescribe the medicine the
patient will use during rehabilitation program. Third, evaluation and assessment of the
capacity and which the patient can exercise and prescribe the tele-rehabilitation program and
exercise each patient can do in a day until they recover. Fourth, the doctor educates the
patients on what to do during rehabilitating and managing any emerging emergencies in the
hospital. Fifth, communicate with the patients frequently through phone to monitor how the
patient is doing and lastly the doctor is the one to recommend if the patient need
rehabilitation program or if the patient has recorded.
Nurses have also important roles in the tele-rehabilitation centre which include one, ,
preserving the patients’ medical records and hi/her history and providing patients with
education about the disease or disorder they are suffering from (Morales-Vidal & Ruland
2013, pp. 101-107; Miller et al. 2014, pp. 1-5). Second, the nurse do follow up and contact
patients either through telephones or any other means of communication to see and assess
Roles of some of the Tele-rehabilitation Staff
Implementation of the tele-rehabilitation programs for patients require work force
from different levels in the healthcare which include the medical professionals, information
technology personnel, and the marketing department (Bernocchi et al. 2016, pp.106-115).
The marketing department advertises the services offered by the tele-rehabilitation facility to
the discharged patients and give them links on how to join the program. In term of medical
services there is the doctor, nurse, ergophysiologist, physiotherapist, and psychologist (Jin et
al. 2015, p. 61; Vloothuis et al. 2015, p. 193; Kairy et al. 2016, pp.201-206).
The doctor has numerous roles in tele-rehabilitation which include one, preserving
the patients’ medical records and hi/her history (Kairy et al. 2016, pp.201-206). Second, the
doctor is also responsible for performing the clinical evaluation of the patient after and before
the tele-rehabilitation services. The doctor is also obligated to prescribe the medicine the
patient will use during rehabilitation program. Third, evaluation and assessment of the
capacity and which the patient can exercise and prescribe the tele-rehabilitation program and
exercise each patient can do in a day until they recover. Fourth, the doctor educates the
patients on what to do during rehabilitating and managing any emerging emergencies in the
hospital. Fifth, communicate with the patients frequently through phone to monitor how the
patient is doing and lastly the doctor is the one to recommend if the patient need
rehabilitation program or if the patient has recorded.
Nurses have also important roles in the tele-rehabilitation centre which include one, ,
preserving the patients’ medical records and hi/her history and providing patients with
education about the disease or disorder they are suffering from (Morales-Vidal & Ruland
2013, pp. 101-107; Miller et al. 2014, pp. 1-5). Second, the nurse do follow up and contact
patients either through telephones or any other means of communication to see and assess
Tele-Rehabilitation for Discharged Patients 6
how the patients are reacting to medication and solve any problem about the tele-
rehabilitation that may arise. Similar to doctors, nurses also have the obligation to attend to
emergencies. Third, nurses ensure that the patients are qualified for the tele-rehabilitation
program by checking all necessary forms provided by the service users. Fourth, the nurses are
in charge of the technological fitness equipment. They monitor the equipment to make sure
that they are functional and record any arising problem. Lastly, the nurses conduct and take
anthropometric measurements after the rehabilitation program is over and before the program
starts.
Ergophysiologists are important in that they evaluate and do assessment of the
physical ability of the patient to determine if they are qualified for tele-rehabilitation (Sarfo et
al. 2017, p. 203; Kizony et al. 2013; Miller et al. 2014, p. 1; Adinolfi et al 2016, p. 40). The
ergophysiologists also prescribe the quantity of exercise the patient will undergo and also
educate the patients on how to go about the prescribed training program. Lastly, the
ergophysiologists monitor how the patients are training and record and recommend the next
step for the patients. The psychologist in tele-rehabilitation service gives the patient
psychological support and advice. They also recommend if the patient can enrol in
rehabilitation program. The psychologists also assess and evaluate the psychological
behaviour of the patient and prescribe drugs for him or her.
The psychotherapist synchronises the therapy programs the patients are undergoing
and maintain the medical records of the patients (Chen, Xiao & De Bellis 2016, p. 74). The
psychotherapist reads the patients’ medical report and selects appropriate therapy for them
and then adds the therapy exercises in his YouTube account or that of the hospital. The
psychotherapist also has the obligation of evaluating and analysing the electrocardiogram
(ECG) and give report after consulting the doctor. The psychotherapist gives psychotherapy
how the patients are reacting to medication and solve any problem about the tele-
rehabilitation that may arise. Similar to doctors, nurses also have the obligation to attend to
emergencies. Third, nurses ensure that the patients are qualified for the tele-rehabilitation
program by checking all necessary forms provided by the service users. Fourth, the nurses are
in charge of the technological fitness equipment. They monitor the equipment to make sure
that they are functional and record any arising problem. Lastly, the nurses conduct and take
anthropometric measurements after the rehabilitation program is over and before the program
starts.
Ergophysiologists are important in that they evaluate and do assessment of the
physical ability of the patient to determine if they are qualified for tele-rehabilitation (Sarfo et
al. 2017, p. 203; Kizony et al. 2013; Miller et al. 2014, p. 1; Adinolfi et al 2016, p. 40). The
ergophysiologists also prescribe the quantity of exercise the patient will undergo and also
educate the patients on how to go about the prescribed training program. Lastly, the
ergophysiologists monitor how the patients are training and record and recommend the next
step for the patients. The psychologist in tele-rehabilitation service gives the patient
psychological support and advice. They also recommend if the patient can enrol in
rehabilitation program. The psychologists also assess and evaluate the psychological
behaviour of the patient and prescribe drugs for him or her.
The psychotherapist synchronises the therapy programs the patients are undergoing
and maintain the medical records of the patients (Chen, Xiao & De Bellis 2016, p. 74). The
psychotherapist reads the patients’ medical report and selects appropriate therapy for them
and then adds the therapy exercises in his YouTube account or that of the hospital. The
psychotherapist also has the obligation of evaluating and analysing the electrocardiogram
(ECG) and give report after consulting the doctor. The psychotherapist gives psychotherapy
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Tele-Rehabilitation for Discharged Patients 7
advice to the patients through phone calls or any other communication mediums. The
psychotherapist also monitors how the patients are conducting their rehabilitation online and
provide recommendations on where to improve the exercise. The medical records of patients
are confidential therefore, the other role of psychotherapist is to keep the records safe and
away from public eye.
There is another category of staff in the tele-rehabilitation centre that must be there
for the successful implementation of the rehabilitation programs of the discharged patients
(Chen, Xiao & De Bellis 2016, p. 77; Dalal, Doherty & Taylor 2015). The employees are the
information technology personnel. The information technology workers must be there to
ensure the digital part of tele-rehabilitation is running smoothly. The information technology
personnel’s role is to maintain the digital system of the hospital which includes the website,
the YouTube accounts and the blogs of the facility. The digital systems are the ones to ensure
that tele-rehabilitation program that has been recorded reach the intended patients. The
equipment at the hospital I am working at is technological in nature and need the information
technology personnel to monitor and maintain them to prevent malfunction.
Evidence for and against Tele-Rehabilitation and Determining Best Practice in
Rehabilitation Services
Evidence for Tele-Rehabilitation
A good number of researches have shown that tele-rehabilitation has proven to be a
success in many healthcare fields. The evidences have been seen in the field of cardiology
where success was seen when cardiac tele-rehabilitation of discharged patient was completely
healed in one of the Saudi Arabian Hospital (Zanaboni et al. 2016, p. 126). The patient’s
cardiac risk factors were reduced and the patient shown tremendous improvement without
advice to the patients through phone calls or any other communication mediums. The
psychotherapist also monitors how the patients are conducting their rehabilitation online and
provide recommendations on where to improve the exercise. The medical records of patients
are confidential therefore, the other role of psychotherapist is to keep the records safe and
away from public eye.
There is another category of staff in the tele-rehabilitation centre that must be there
for the successful implementation of the rehabilitation programs of the discharged patients
(Chen, Xiao & De Bellis 2016, p. 77; Dalal, Doherty & Taylor 2015). The employees are the
information technology personnel. The information technology workers must be there to
ensure the digital part of tele-rehabilitation is running smoothly. The information technology
personnel’s role is to maintain the digital system of the hospital which includes the website,
the YouTube accounts and the blogs of the facility. The digital systems are the ones to ensure
that tele-rehabilitation program that has been recorded reach the intended patients. The
equipment at the hospital I am working at is technological in nature and need the information
technology personnel to monitor and maintain them to prevent malfunction.
Evidence for and against Tele-Rehabilitation and Determining Best Practice in
Rehabilitation Services
Evidence for Tele-Rehabilitation
A good number of researches have shown that tele-rehabilitation has proven to be a
success in many healthcare fields. The evidences have been seen in the field of cardiology
where success was seen when cardiac tele-rehabilitation of discharged patient was completely
healed in one of the Saudi Arabian Hospital (Zanaboni et al. 2016, p. 126). The patient’s
cardiac risk factors were reduced and the patient shown tremendous improvement without
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Tele-Rehabilitation for Discharged Patients 8
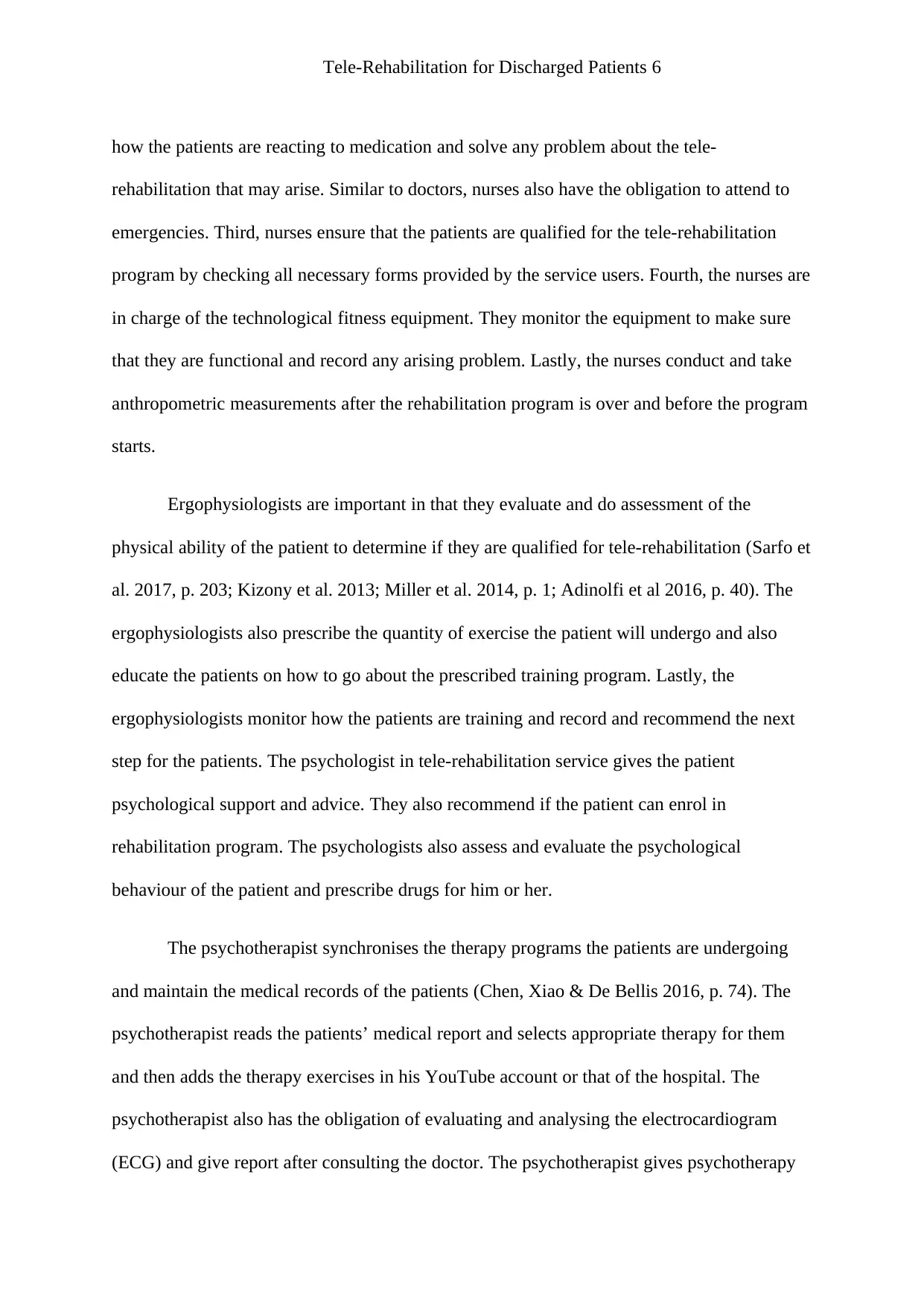
visiting the hospital. Another study by (Dobkin & Dorsch 2013, p. 331; Stylianides et al.
2013) shows that the doctors who used tele-rehabilitation method to treat discharged fellows
in Saudi Arabia who were suffering from chronic pain were successful. The study shows that
the use of tele-rehabilitation on the patient had a prolonged impact on the labour capability
which is essential for an individual suffering from problems which are complex and
pronging. Ivanova et al. (2015) did their research on another patient and the results were the
same. However, studies should be done to determine if at all the method is effective and
reliable.
Table 1: The study for tele-rehabilitation program on chronic pain (Ivanova et al. 2015)
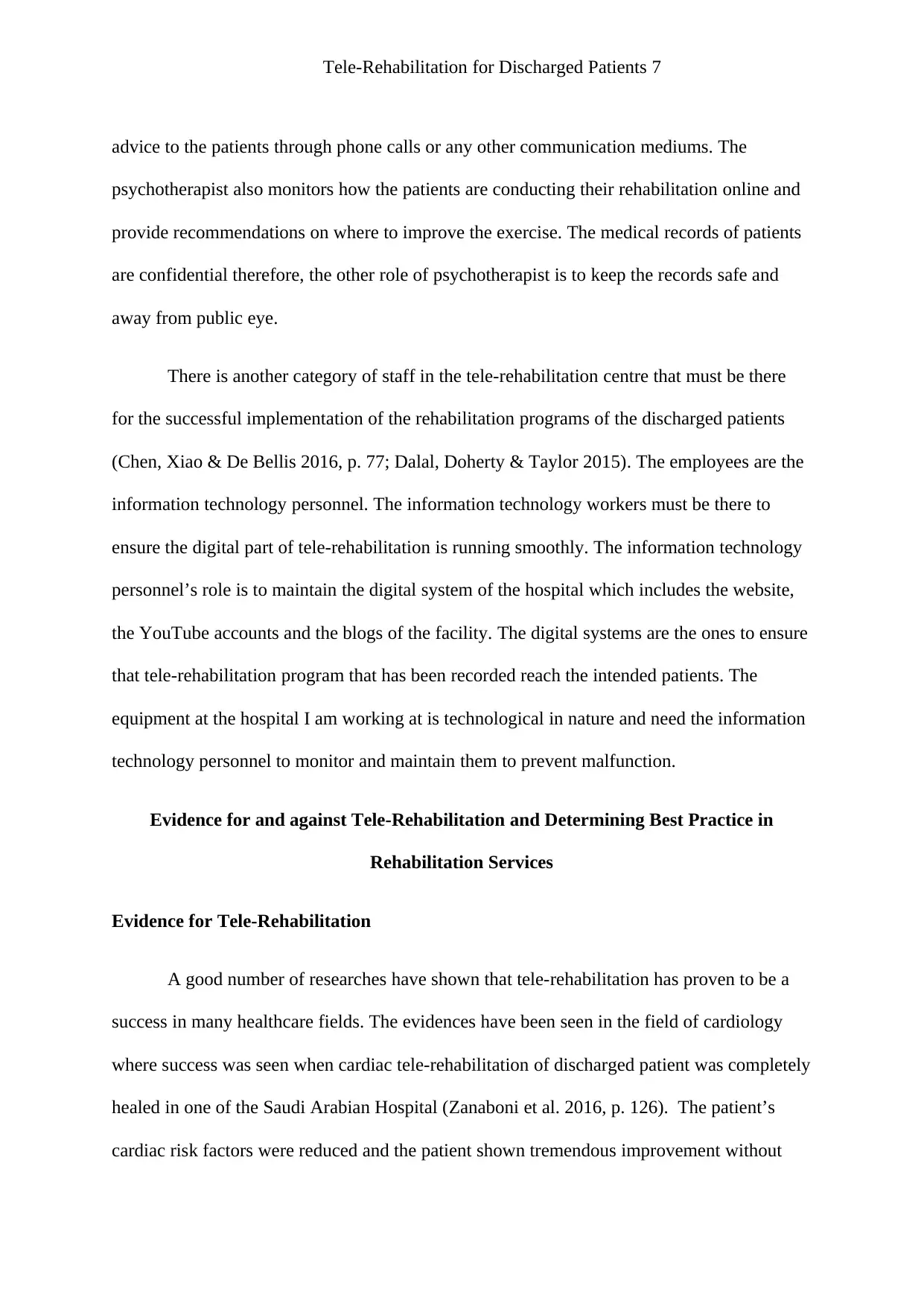
Another study done on discharged patient who suffered a fatal accident and have
mobility problem was also successful (Veras et al. 2016, p. 79). The study gives evidence that
TRH methods provide equal results as FTF and can be comfortably used in delivery services.
The table below shows the results of TRH on discharged patient who had mobility problems.
visiting the hospital. Another study by (Dobkin & Dorsch 2013, p. 331; Stylianides et al.
2013) shows that the doctors who used tele-rehabilitation method to treat discharged fellows
in Saudi Arabia who were suffering from chronic pain were successful. The study shows that
the use of tele-rehabilitation on the patient had a prolonged impact on the labour capability
which is essential for an individual suffering from problems which are complex and
pronging. Ivanova et al. (2015) did their research on another patient and the results were the
same. However, studies should be done to determine if at all the method is effective and
reliable.
Table 1: The study for tele-rehabilitation program on chronic pain (Ivanova et al. 2015)
Another study done on discharged patient who suffered a fatal accident and have
mobility problem was also successful (Veras et al. 2016, p. 79). The study gives evidence that
TRH methods provide equal results as FTF and can be comfortably used in delivery services.
The table below shows the results of TRH on discharged patient who had mobility problems.
Tele-Rehabilitation for Discharged Patients 9
Table 2: The study for THR for mobility (Veras et al. 2016, p. 79)
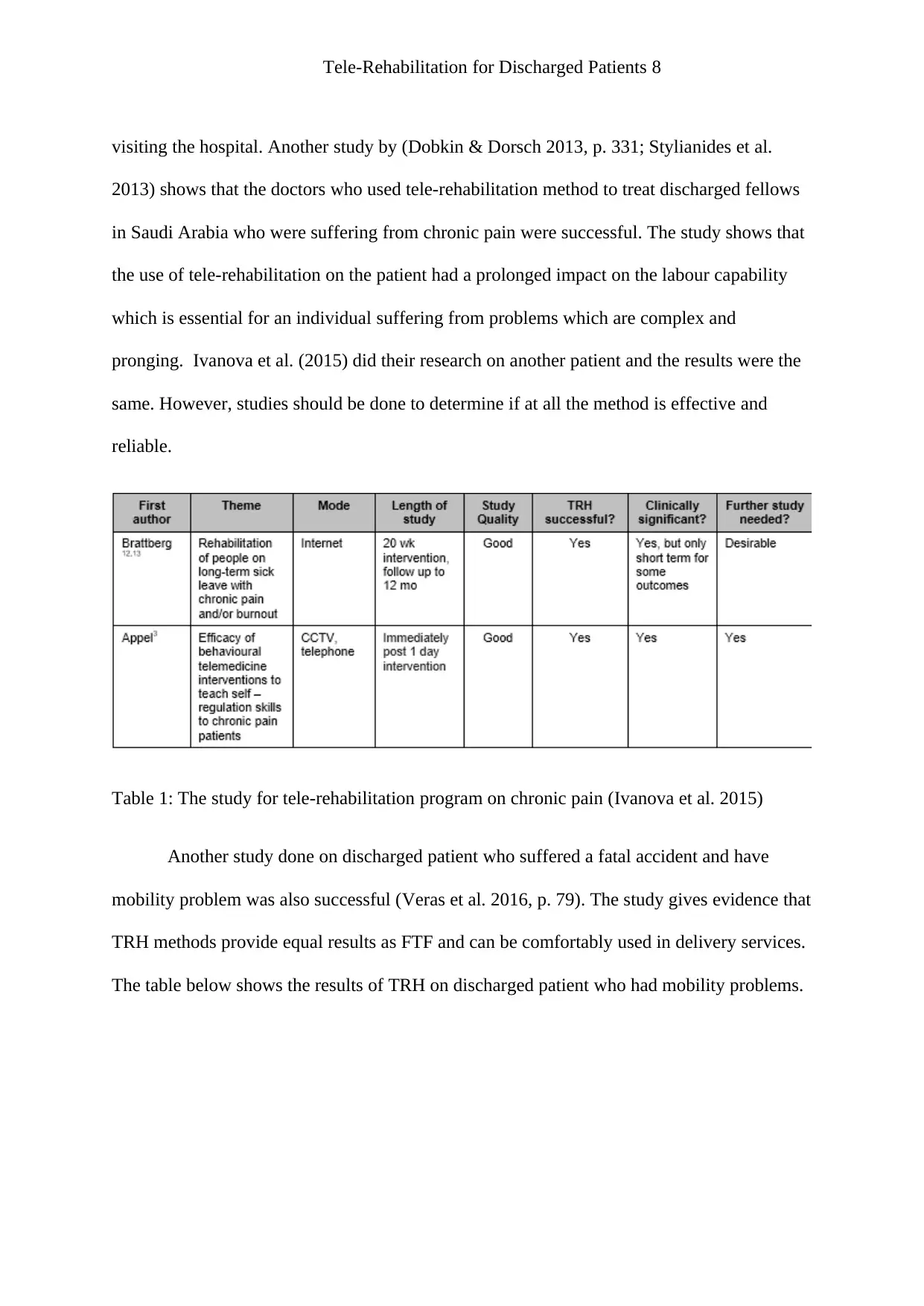
The other evidence was concerned with joint management. The study shows that
patients who suffered joint complications at a certain health facility in Saudi Arabia were
rehabilitated through THR and the outcome was astonishing (Fazio et al. 2016). The service
was done through the phone and was proven better and cost effective than FTF and UC by
the Saudi Arabia health department (Hoda et al. 2014). The table below shows the orthopedic
TRH service of discharged patients.
Table 3: The table shows tele-rehabilitation in orthopaedic rehabilitation program (Fazio et
al. 2016; Hoda et al. 2014)
Evidence against Tele-Rehabilitation
Table 2: The study for THR for mobility (Veras et al. 2016, p. 79)
The other evidence was concerned with joint management. The study shows that
patients who suffered joint complications at a certain health facility in Saudi Arabia were
rehabilitated through THR and the outcome was astonishing (Fazio et al. 2016). The service
was done through the phone and was proven better and cost effective than FTF and UC by
the Saudi Arabia health department (Hoda et al. 2014). The table below shows the orthopedic
TRH service of discharged patients.
Table 3: The table shows tele-rehabilitation in orthopaedic rehabilitation program (Fazio et
al. 2016; Hoda et al. 2014)
Evidence against Tele-Rehabilitation
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Tele-Rehabilitation for Discharged Patients 10
TRH is a cost-effective service and has been proven to be a success in many medical
fields. However, there are some evidences that the practice is not that effective compared to
one on one treatment of patient. Marzano, Lubkina and Rizakova (2015) argue that some
patients may ignore the prescription given by the doctors online and take the medicine
wrongly (Vol. 4, pp. 457-467). They say that most patients prefer to be treated and
rehabilitated by doctors on sight. Some of the fake doctors can take advantage of the online
platform which is not monitored by the government of Saudi Arabia to mislead patients.
Howard-Wilsher et al. (2016, p. 11) have concluded that some of the evidences supporting
the TRH practice are not yet complete. The scholar says that the cost-effectiveness of the
program is somehow costly.
Determining Best Practice in Rehabilitation Services
Rehabilitation services should be done in the best practices therein. There are some of
the criteria to be followed to determine the best practice for tele-rehabilitation. The first
determination is the qualification of the professional performing the practice. If I can reflect
on my profession, a person must be qualified and registered with the department of health of
government of Saudi Arabia for him/she to conduct rehabilitation activities. Unqualified
persons cannot provide the best rehabilitation services. The second determinant is the
equipment used for rehabilitation. They must be certified equipment and recognised by the
government of Saudi Arabia. Gao et al. (2015) reported that the facility providing both tele-
rehabilitation and normal rehabilitation must be registered to produce such services (pp.95-
102).
The role of a leader and how to manage/lead change in the clinical setting
TRH is a cost-effective service and has been proven to be a success in many medical
fields. However, there are some evidences that the practice is not that effective compared to
one on one treatment of patient. Marzano, Lubkina and Rizakova (2015) argue that some
patients may ignore the prescription given by the doctors online and take the medicine
wrongly (Vol. 4, pp. 457-467). They say that most patients prefer to be treated and
rehabilitated by doctors on sight. Some of the fake doctors can take advantage of the online
platform which is not monitored by the government of Saudi Arabia to mislead patients.
Howard-Wilsher et al. (2016, p. 11) have concluded that some of the evidences supporting
the TRH practice are not yet complete. The scholar says that the cost-effectiveness of the
program is somehow costly.
Determining Best Practice in Rehabilitation Services
Rehabilitation services should be done in the best practices therein. There are some of
the criteria to be followed to determine the best practice for tele-rehabilitation. The first
determination is the qualification of the professional performing the practice. If I can reflect
on my profession, a person must be qualified and registered with the department of health of
government of Saudi Arabia for him/she to conduct rehabilitation activities. Unqualified
persons cannot provide the best rehabilitation services. The second determinant is the
equipment used for rehabilitation. They must be certified equipment and recognised by the
government of Saudi Arabia. Gao et al. (2015) reported that the facility providing both tele-
rehabilitation and normal rehabilitation must be registered to produce such services (pp.95-
102).
The role of a leader and how to manage/lead change in the clinical setting
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Tele-Rehabilitation for Discharged Patients 11
The role of a leader in clinical setting
Leaders are important figure in the clinical setting and they are the overseers of every
activity taking place in the clinics. Many scholars have done studies and the results are that
leadership is a vital body in any institutional setting. Ivanova et al. (2015) reported that
leaders who are hardworking, disciplined and highly motivational are responsible from
changing organizations from good to excellent. According to Gao et al. (2015, p.95) such
great leaders in an organisation help in employing staff who are also capable of changing the
firms.
The leaders come up with great developmental strategies which see the success of the
organisation to the next level. Artz et al. (2015, p. 15) did study on the roles of the healthcare
leaders and come up with some great results. In the study Artz et al state that healthcare
facilities also see the leadership as important factor. Ivanova et al. (2015) also did some
studies about healthcare leaders and suggested that successful leaders in medical field have
the passion to improve the quality of health services, and work tirelessly to ensure that the
healthcare facilities they are running are up to speed with current trends and technology.
Howard-Wilsher et al. (2016, p. 11) argues that leadership in healthcare is responsible for
setting the objectives of the firms, creating and executing action plans and strategies and
coming up with rooms for change in the facilities. Artz et al. (2015, p. 15) and Ivanova et al.
(2015) argue that leaders in the healthcare setting ensure that the safety of patients is
protected by making the healthcare environment safe for them.
In tele-rehabilitation centres, the services of leaders are highly required in that they
are responsible for checking if every activity is moving as planned (Mayo 2016). Leaders in
TRH are responsible for recruiting new qualified staffs and help improve the production of
The role of a leader in clinical setting
Leaders are important figure in the clinical setting and they are the overseers of every
activity taking place in the clinics. Many scholars have done studies and the results are that
leadership is a vital body in any institutional setting. Ivanova et al. (2015) reported that
leaders who are hardworking, disciplined and highly motivational are responsible from
changing organizations from good to excellent. According to Gao et al. (2015, p.95) such
great leaders in an organisation help in employing staff who are also capable of changing the
firms.
The leaders come up with great developmental strategies which see the success of the
organisation to the next level. Artz et al. (2015, p. 15) did study on the roles of the healthcare
leaders and come up with some great results. In the study Artz et al state that healthcare
facilities also see the leadership as important factor. Ivanova et al. (2015) also did some
studies about healthcare leaders and suggested that successful leaders in medical field have
the passion to improve the quality of health services, and work tirelessly to ensure that the
healthcare facilities they are running are up to speed with current trends and technology.
Howard-Wilsher et al. (2016, p. 11) argues that leadership in healthcare is responsible for
setting the objectives of the firms, creating and executing action plans and strategies and
coming up with rooms for change in the facilities. Artz et al. (2015, p. 15) and Ivanova et al.
(2015) argue that leaders in the healthcare setting ensure that the safety of patients is
protected by making the healthcare environment safe for them.
In tele-rehabilitation centres, the services of leaders are highly required in that they
are responsible for checking if every activity is moving as planned (Mayo 2016). Leaders in
TRH are responsible for recruiting new qualified staffs and help improve the production of
Tele-Rehabilitation for Discharged Patients 12
TRH services. Another role of leaders in the clinics is to supervise every activity in the
organisation. Leaders also keep the patients records safe and away from public eye. Another
role of leaders in healthcare is integrating care laterally with various disciplines. In healthcare
there are many departments which need each other so that it can be easy to provide quality
healthcare services to the patients (Oatis et al. 2014). A leader’s role in this scenario is to
coordinate the two different departments who need each other to work together for example
psychologist and psychotherapist. Leaders also solve problems whenever they arise in
healthcare that is between the employees and patients or among the employees, or even
among the patients. The last and important role of a leader in the clinical setting is to protect
his/her employees and patients from external harm.
How to lead change in the clinical setting
Tousignant et al. (2014) states that leaders must use the leadership models also known
as leadership theory to bring change in organisations. The model developed by James
Scouller has three designs which strengthen the weakness of other leadership theories
(Tousignant et al. 2014). It has three Ps that is Public, Private and Personal leadership (Dalal,
Doherty & Taylor 2015).
TRH services. Another role of leaders in the clinics is to supervise every activity in the
organisation. Leaders also keep the patients records safe and away from public eye. Another
role of leaders in healthcare is integrating care laterally with various disciplines. In healthcare
there are many departments which need each other so that it can be easy to provide quality
healthcare services to the patients (Oatis et al. 2014). A leader’s role in this scenario is to
coordinate the two different departments who need each other to work together for example
psychologist and psychotherapist. Leaders also solve problems whenever they arise in
healthcare that is between the employees and patients or among the employees, or even
among the patients. The last and important role of a leader in the clinical setting is to protect
his/her employees and patients from external harm.
How to lead change in the clinical setting
Tousignant et al. (2014) states that leaders must use the leadership models also known
as leadership theory to bring change in organisations. The model developed by James
Scouller has three designs which strengthen the weakness of other leadership theories
(Tousignant et al. 2014). It has three Ps that is Public, Private and Personal leadership (Dalal,
Doherty & Taylor 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 27
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





