Case Study Analysis: Celiac Disease and Type 1 Diabetes Mellitus
VerifiedAdded on 2023/06/09
|7
|1966
|74
Case Study
AI Summary
This case study analyzes the scenario of an 11-year-old girl, Emilia, diagnosed with celiac disease and subsequently type 1 diabetes. The assignment explores the intertwined nature of these autoimmune diseases, emphasizing shared genetic predispositions and environmental factors. It delves into the risk factors, including family history and gluten consumption, which can trigger inflammation and damage to the small intestine, leading to celiac disease. Furthermore, the case study examines the aetiology of type 1 diabetes, highlighting the role of genetic factors (IDDM1 region), viral infections, and cow milk consumption. The pathophysiology section explains the disruption of blood glucose regulation due to insulin deficiency and the resulting clinical manifestations such as increased urination, excessive thirst, and weight loss. The diagnosis and treatment sections detail the various tests used to detect type 1 diabetes, including random plasma glucose tests and HbA1c measurement, and discuss the management strategies, including gluten-free diets, insulin sensitizers, and insulin secretagogues. The analysis provides a comprehensive understanding of the disease processes, diagnostic methods, and treatment approaches for these related conditions.
CASE STUDY OF CELIAC DISEASE AND DIABETES
Name of the student:
Name of the university:
Name of the student:
Name of the university:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
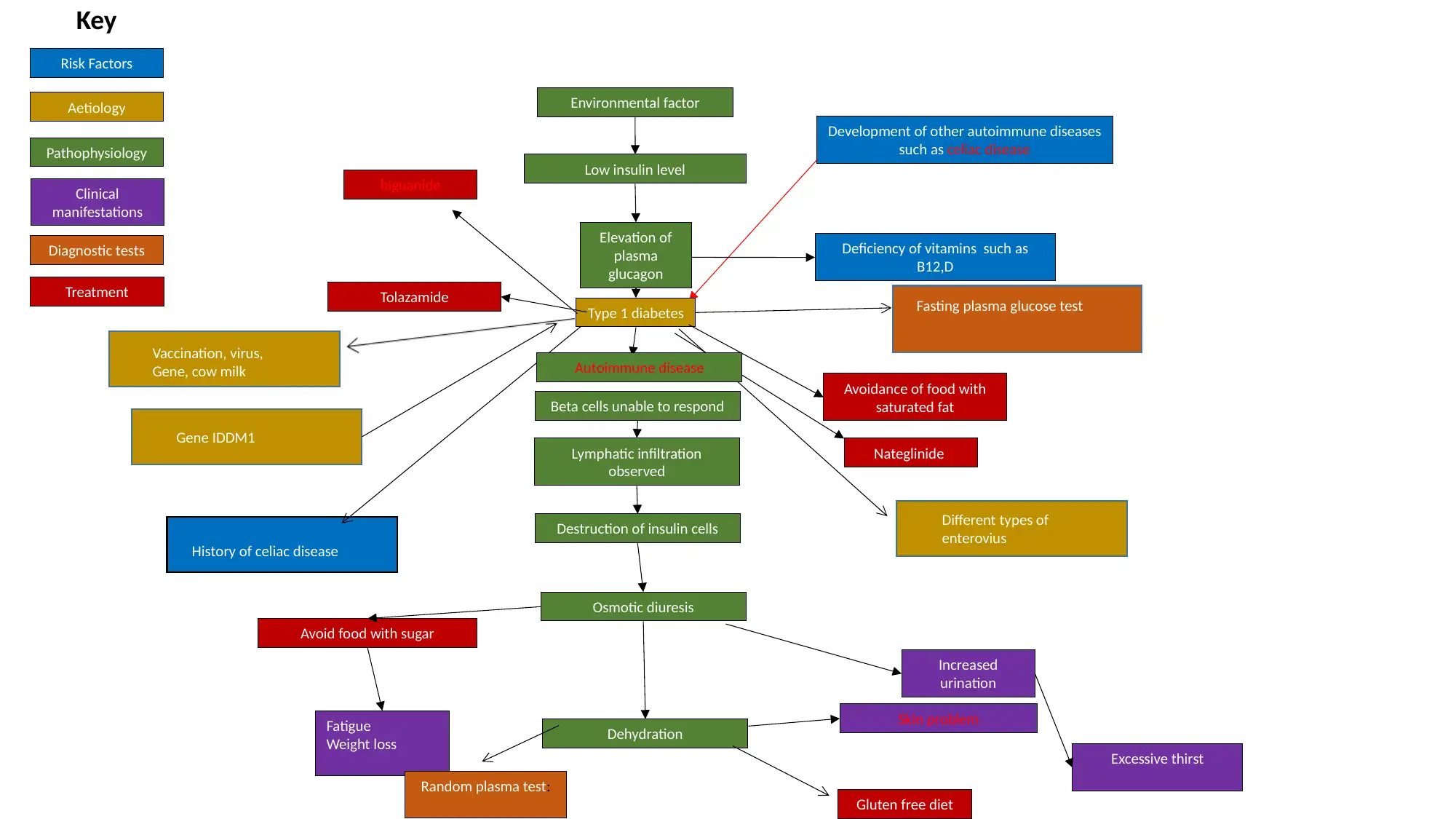
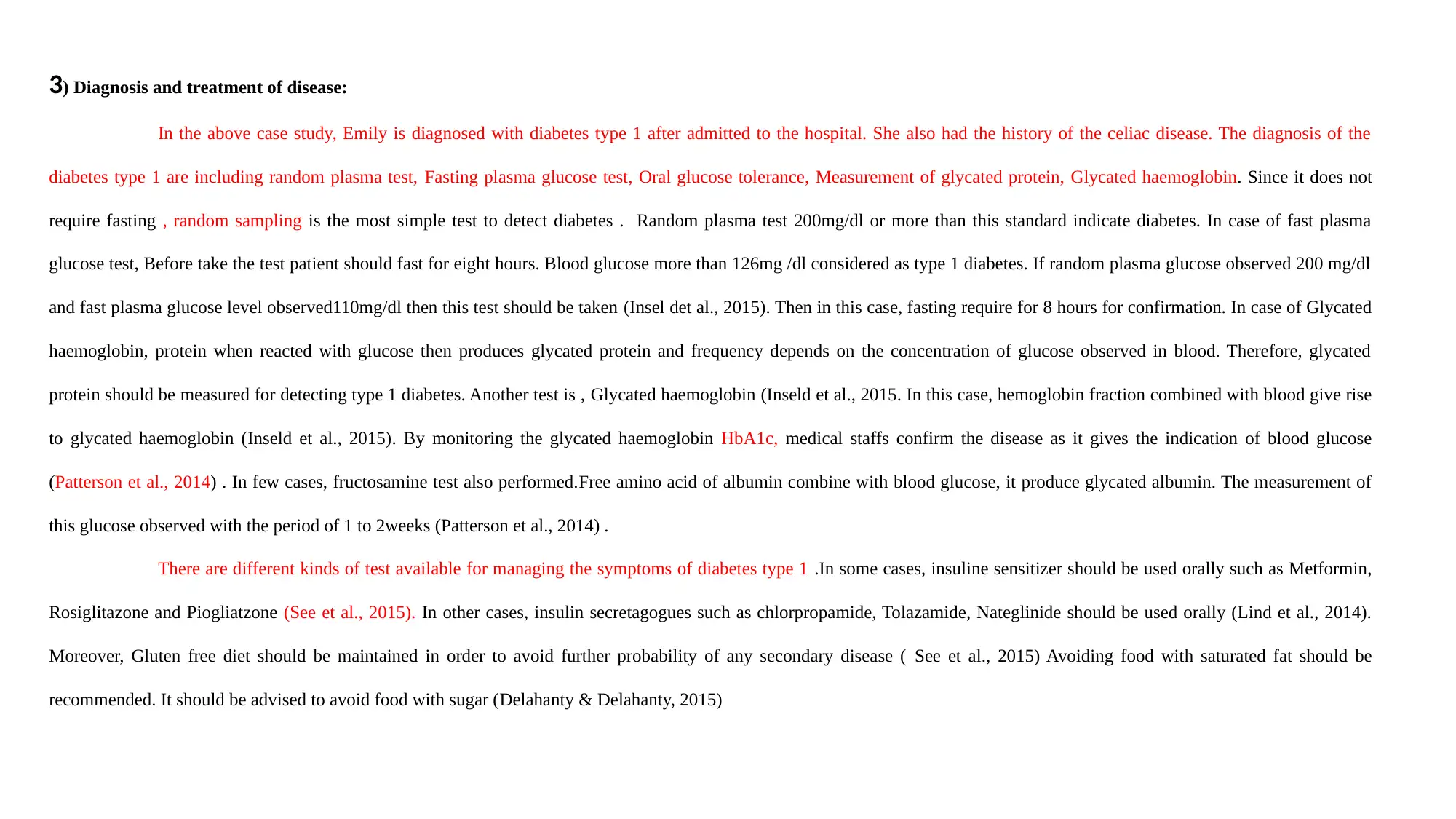
Environmental factor
Low insulin level
Elevation of
plasma
glucagon
Beta cells unable to respond
Pathophysiology
Risk Factors
Aetiology
Clinical
manifestations
Diagnostic tests
Treatment
Development of other autoimmune diseases
such as celiac disease
Increased
urination
Type 1 diabetes
Excessive thirst
Nateglinide
Tolazamide
Lymphatic infiltration
observed
Destruction of insulin cells
Osmotic diuresis
Dehydration
Fatigue
Weight loss
Deficiency of vitamins such as
B12,D
Avoid food with sugar
biguanide
Avoidance of food with
saturated fat
Random plasma test:
Key
Gluten free diet
Skin problem
Fasting plasma glucose test
Vaccination, virus,
Gene, cow milk
History of celiac disease
Gene IDDM1
Different types of
enterovius
Autoimmune disease
Low insulin level
Elevation of
plasma
glucagon
Beta cells unable to respond
Pathophysiology
Risk Factors
Aetiology
Clinical
manifestations
Diagnostic tests
Treatment
Development of other autoimmune diseases
such as celiac disease
Increased
urination
Type 1 diabetes
Excessive thirst
Nateglinide
Tolazamide
Lymphatic infiltration
observed
Destruction of insulin cells
Osmotic diuresis
Dehydration
Fatigue
Weight loss
Deficiency of vitamins such as
B12,D
Avoid food with sugar
biguanide
Avoidance of food with
saturated fat
Random plasma test:
Key
Gluten free diet
Skin problem
Fasting plasma glucose test
Vaccination, virus,
Gene, cow milk
History of celiac disease
Gene IDDM1
Different types of
enterovius
Autoimmune disease
In this scenario, Emilia is 11 year girl who admitted to the hospital due to 20hours of worse vomiting. She was diagnosed with celiac disease and tonsillitis. This scenario,
Emily might expose to gluten containing food such as wheat, barley and rye. Subsequently, over the time, the consumption of gluten leads to the inflammation and damage the lining of
small intestine. Eventually, diarrhoea, severe vomiting and behavioural issues observed. Gluten diet also leads to enlargement of tonsil ( Haynes et al., 2014). Therefore, her tonsillitis was
removed. When she was admitted to the hospital, she was diagnosed with type 1 diabetes. The major linked between two disease is both celiac and type 1diabetes are both autoimmune
disease affected by gluten.
1) Risk factor and aetiology of disease:
In above scenario, Emilia had history of celiac disease along with diabetes. According to evidences, if family members have the history of celiac disease then high chances are
offspring will also develop celiac disease in future.Moreover, in majority of the cases; those people have celiac disease also develop Type 1 diabetes due to the fact that they share same
over lapping genes .Approximately 40 loci associated with Type 1 diabetes out of which 39 associated Celiac disease. These genes RGS1, IL18RAP, CD26, CTLA4, ICOS, CCR5, IL2, IL21.In
future these genes give rise to other autoimmune diseases. Therefore, Emily developed diabetes type 1 . Another risk factor is Gluten containing diet. Gluten containing diet such as wheat,
barley and rye, both induce inflammation and subsequent autoimmune diseases such as celiac disease and type1diabetes.However, gluten free diet can lead to the deficiency of vitamin
b12 and D and other fat soluble vitamin (Zhang et al. 2015)
Emilia diagnosed with Diabetes type 1 when admitted to hospital .Aetiology of diabetes mellitus as follows:
Researchers identified specific genetic region called IDDM1 strongly responsible for type 1 diabetes. Some of the region also overlapped with celiac disease (Adlercreutz, et
al.2015).Different types of enterovius attachment can lead to the diabetes mellitus in few cases. Moreover, vaccinations of small pox. Tuberculosis also give rise to type 1 diabetes since
tuberculosis causes poor glycaemic control. Drinking cow milk has a link with occurrence of the diabetes Type 1(Willi et al., 2015).
Emily might expose to gluten containing food such as wheat, barley and rye. Subsequently, over the time, the consumption of gluten leads to the inflammation and damage the lining of
small intestine. Eventually, diarrhoea, severe vomiting and behavioural issues observed. Gluten diet also leads to enlargement of tonsil ( Haynes et al., 2014). Therefore, her tonsillitis was
removed. When she was admitted to the hospital, she was diagnosed with type 1 diabetes. The major linked between two disease is both celiac and type 1diabetes are both autoimmune
disease affected by gluten.
1) Risk factor and aetiology of disease:
In above scenario, Emilia had history of celiac disease along with diabetes. According to evidences, if family members have the history of celiac disease then high chances are
offspring will also develop celiac disease in future.Moreover, in majority of the cases; those people have celiac disease also develop Type 1 diabetes due to the fact that they share same
over lapping genes .Approximately 40 loci associated with Type 1 diabetes out of which 39 associated Celiac disease. These genes RGS1, IL18RAP, CD26, CTLA4, ICOS, CCR5, IL2, IL21.In
future these genes give rise to other autoimmune diseases. Therefore, Emily developed diabetes type 1 . Another risk factor is Gluten containing diet. Gluten containing diet such as wheat,
barley and rye, both induce inflammation and subsequent autoimmune diseases such as celiac disease and type1diabetes.However, gluten free diet can lead to the deficiency of vitamin
b12 and D and other fat soluble vitamin (Zhang et al. 2015)
Emilia diagnosed with Diabetes type 1 when admitted to hospital .Aetiology of diabetes mellitus as follows:
Researchers identified specific genetic region called IDDM1 strongly responsible for type 1 diabetes. Some of the region also overlapped with celiac disease (Adlercreutz, et
al.2015).Different types of enterovius attachment can lead to the diabetes mellitus in few cases. Moreover, vaccinations of small pox. Tuberculosis also give rise to type 1 diabetes since
tuberculosis causes poor glycaemic control. Drinking cow milk has a link with occurrence of the diabetes Type 1(Willi et al., 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2) Pathophysiology of the disease:
After admitted to the hospital Emily diagnosed with type 1 diabetes mellitus where she has history of celiac disease. Therefore, the pathophysiology of Type 1
daibetes as follows:
In diabetes mellitus, blood glucose level fluctuates rapidly and insulin level also become low or absent.In absence of insulin, plasma glucagon level elevated and pancreatic beta cell
unable to respond to all insulin secretary stimulation (Gong et al., 2015). Lymphatic infiltration observed by pancreas, as a result all insulin secretary cells destroyed. Subsequently,
insulin deficiency leads to the interruption of glucose uptake of muscles, lipolysis and ketogenesis. Extreme insulin deficiency leads to osmotic diuresis, dehydration .Eventually
patient excessively urinate and become extremely thirsty. Besides, elevated level of free fatty acid along with that diabetic ketoacidosis observed (Chiang et al., 2014).
Clinical manifestation may vary person to person. According to above scenario, Clinical manifestation of diabetes are such as increased urination, Excessive thirst
Skin problem, excessive hunger, fatigue, weight loss, numbness(Handelsman et al., 2015)
After admitted to the hospital Emily diagnosed with type 1 diabetes mellitus where she has history of celiac disease. Therefore, the pathophysiology of Type 1
daibetes as follows:
In diabetes mellitus, blood glucose level fluctuates rapidly and insulin level also become low or absent.In absence of insulin, plasma glucagon level elevated and pancreatic beta cell
unable to respond to all insulin secretary stimulation (Gong et al., 2015). Lymphatic infiltration observed by pancreas, as a result all insulin secretary cells destroyed. Subsequently,
insulin deficiency leads to the interruption of glucose uptake of muscles, lipolysis and ketogenesis. Extreme insulin deficiency leads to osmotic diuresis, dehydration .Eventually
patient excessively urinate and become extremely thirsty. Besides, elevated level of free fatty acid along with that diabetic ketoacidosis observed (Chiang et al., 2014).
Clinical manifestation may vary person to person. According to above scenario, Clinical manifestation of diabetes are such as increased urination, Excessive thirst
Skin problem, excessive hunger, fatigue, weight loss, numbness(Handelsman et al., 2015)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
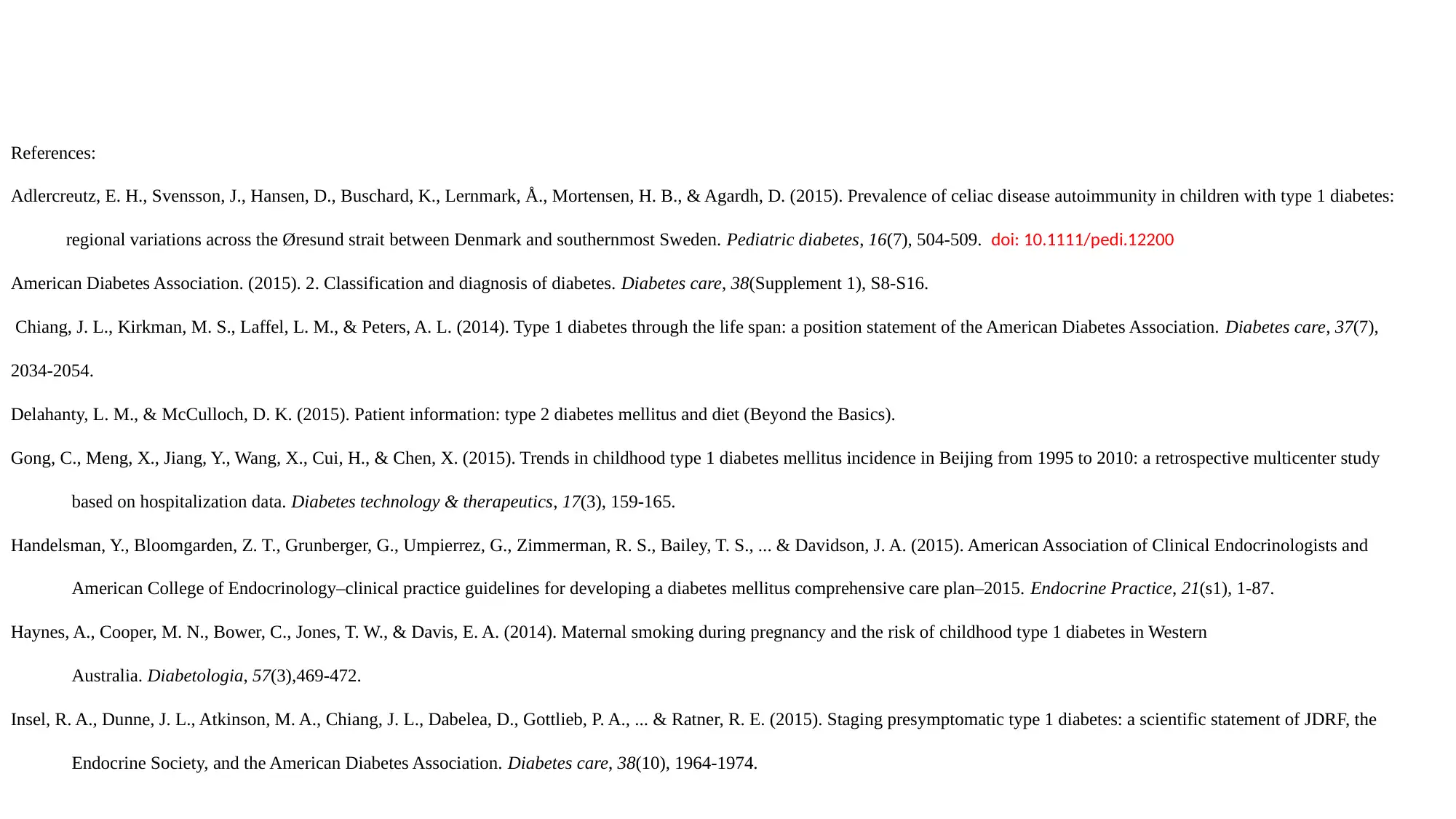
3) Diagnosis and treatment of disease:
In the above case study, Emily is diagnosed with diabetes type 1 after admitted to the hospital. She also had the history of the celiac disease. The diagnosis of the
diabetes type 1 are including random plasma test, Fasting plasma glucose test, Oral glucose tolerance, Measurement of glycated protein, Glycated haemoglobin. Since it does not
require fasting , random sampling is the most simple test to detect diabetes . Random plasma test 200mg/dl or more than this standard indicate diabetes. In case of fast plasma
glucose test, Before take the test patient should fast for eight hours. Blood glucose more than 126mg /dl considered as type 1 diabetes. If random plasma glucose observed 200 mg/dl
and fast plasma glucose level observed110mg/dl then this test should be taken (Insel det al., 2015). Then in this case, fasting require for 8 hours for confirmation. In case of Glycated
haemoglobin, protein when reacted with glucose then produces glycated protein and frequency depends on the concentration of glucose observed in blood. Therefore, glycated
protein should be measured for detecting type 1 diabetes. Another test is , Glycated haemoglobin (Inseld et al., 2015. In this case, hemoglobin fraction combined with blood give rise
to glycated haemoglobin (Inseld et al., 2015). By monitoring the glycated haemoglobin HbA1c, medical staffs confirm the disease as it gives the indication of blood glucose
(Patterson et al., 2014) . In few cases, fructosamine test also performed.Free amino acid of albumin combine with blood glucose, it produce glycated albumin. The measurement of
this glucose observed with the period of 1 to 2weeks (Patterson et al., 2014) .
There are different kinds of test available for managing the symptoms of diabetes type 1 .In some cases, insuline sensitizer should be used orally such as Metformin,
Rosiglitazone and Piogliatzone (See et al., 2015). In other cases, insulin secretagogues such as chlorpropamide, Tolazamide, Nateglinide should be used orally (Lind et al., 2014).
Moreover, Gluten free diet should be maintained in order to avoid further probability of any secondary disease ( See et al., 2015) Avoiding food with saturated fat should be
recommended. It should be advised to avoid food with sugar (Delahanty & Delahanty, 2015)
In the above case study, Emily is diagnosed with diabetes type 1 after admitted to the hospital. She also had the history of the celiac disease. The diagnosis of the
diabetes type 1 are including random plasma test, Fasting plasma glucose test, Oral glucose tolerance, Measurement of glycated protein, Glycated haemoglobin. Since it does not
require fasting , random sampling is the most simple test to detect diabetes . Random plasma test 200mg/dl or more than this standard indicate diabetes. In case of fast plasma
glucose test, Before take the test patient should fast for eight hours. Blood glucose more than 126mg /dl considered as type 1 diabetes. If random plasma glucose observed 200 mg/dl
and fast plasma glucose level observed110mg/dl then this test should be taken (Insel det al., 2015). Then in this case, fasting require for 8 hours for confirmation. In case of Glycated
haemoglobin, protein when reacted with glucose then produces glycated protein and frequency depends on the concentration of glucose observed in blood. Therefore, glycated
protein should be measured for detecting type 1 diabetes. Another test is , Glycated haemoglobin (Inseld et al., 2015. In this case, hemoglobin fraction combined with blood give rise
to glycated haemoglobin (Inseld et al., 2015). By monitoring the glycated haemoglobin HbA1c, medical staffs confirm the disease as it gives the indication of blood glucose
(Patterson et al., 2014) . In few cases, fructosamine test also performed.Free amino acid of albumin combine with blood glucose, it produce glycated albumin. The measurement of
this glucose observed with the period of 1 to 2weeks (Patterson et al., 2014) .
There are different kinds of test available for managing the symptoms of diabetes type 1 .In some cases, insuline sensitizer should be used orally such as Metformin,
Rosiglitazone and Piogliatzone (See et al., 2015). In other cases, insulin secretagogues such as chlorpropamide, Tolazamide, Nateglinide should be used orally (Lind et al., 2014).
Moreover, Gluten free diet should be maintained in order to avoid further probability of any secondary disease ( See et al., 2015) Avoiding food with saturated fat should be
recommended. It should be advised to avoid food with sugar (Delahanty & Delahanty, 2015)
References:
Adlercreutz, E. H., Svensson, J., Hansen, D., Buschard, K., Lernmark, Å., Mortensen, H. B., & Agardh, D. (2015). Prevalence of celiac disease autoimmunity in children with type 1 diabetes:
regional variations across the Øresund strait between Denmark and southernmost Sweden. Pediatric diabetes, 16(7), 504-509. doi: 10.1111/pedi.12200
American Diabetes Association. (2015). 2. Classification and diagnosis of diabetes. Diabetes care, 38(Supplement 1), S8-S16.
Chiang, J. L., Kirkman, M. S., Laffel, L. M., & Peters, A. L. (2014). Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes care, 37(7),
2034-2054.
Delahanty, L. M., & McCulloch, D. K. (2015). Patient information: type 2 diabetes mellitus and diet (Beyond the Basics).
Gong, C., Meng, X., Jiang, Y., Wang, X., Cui, H., & Chen, X. (2015). Trends in childhood type 1 diabetes mellitus incidence in Beijing from 1995 to 2010: a retrospective multicenter study
based on hospitalization data. Diabetes technology & therapeutics, 17(3), 159-165.
Handelsman, Y., Bloomgarden, Z. T., Grunberger, G., Umpierrez, G., Zimmerman, R. S., Bailey, T. S., ... & Davidson, J. A. (2015). American Association of Clinical Endocrinologists and
American College of Endocrinology–clinical practice guidelines for developing a diabetes mellitus comprehensive care plan–2015. Endocrine Practice, 21(s1), 1-87.
Haynes, A., Cooper, M. N., Bower, C., Jones, T. W., & Davis, E. A. (2014). Maternal smoking during pregnancy and the risk of childhood type 1 diabetes in Western
Australia. Diabetologia, 57(3),469-472.
Insel, R. A., Dunne, J. L., Atkinson, M. A., Chiang, J. L., Dabelea, D., Gottlieb, P. A., ... & Ratner, R. E. (2015). Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the
Endocrine Society, and the American Diabetes Association. Diabetes care, 38(10), 1964-1974.
Adlercreutz, E. H., Svensson, J., Hansen, D., Buschard, K., Lernmark, Å., Mortensen, H. B., & Agardh, D. (2015). Prevalence of celiac disease autoimmunity in children with type 1 diabetes:
regional variations across the Øresund strait between Denmark and southernmost Sweden. Pediatric diabetes, 16(7), 504-509. doi: 10.1111/pedi.12200
American Diabetes Association. (2015). 2. Classification and diagnosis of diabetes. Diabetes care, 38(Supplement 1), S8-S16.
Chiang, J. L., Kirkman, M. S., Laffel, L. M., & Peters, A. L. (2014). Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes care, 37(7),
2034-2054.
Delahanty, L. M., & McCulloch, D. K. (2015). Patient information: type 2 diabetes mellitus and diet (Beyond the Basics).
Gong, C., Meng, X., Jiang, Y., Wang, X., Cui, H., & Chen, X. (2015). Trends in childhood type 1 diabetes mellitus incidence in Beijing from 1995 to 2010: a retrospective multicenter study
based on hospitalization data. Diabetes technology & therapeutics, 17(3), 159-165.
Handelsman, Y., Bloomgarden, Z. T., Grunberger, G., Umpierrez, G., Zimmerman, R. S., Bailey, T. S., ... & Davidson, J. A. (2015). American Association of Clinical Endocrinologists and
American College of Endocrinology–clinical practice guidelines for developing a diabetes mellitus comprehensive care plan–2015. Endocrine Practice, 21(s1), 1-87.
Haynes, A., Cooper, M. N., Bower, C., Jones, T. W., & Davis, E. A. (2014). Maternal smoking during pregnancy and the risk of childhood type 1 diabetes in Western
Australia. Diabetologia, 57(3),469-472.
Insel, R. A., Dunne, J. L., Atkinson, M. A., Chiang, J. L., Dabelea, D., Gottlieb, P. A., ... & Ratner, R. E. (2015). Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the
Endocrine Society, and the American Diabetes Association. Diabetes care, 38(10), 1964-1974.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Laitinen, A. U., Agardh, D., Kivelä, L., Huhtala, H., Lähdeaho, M. L., Kaukinen, K., & Kurppa, K. (2017). Coeliac patients detected during type 1 diabetes
surveillance had similar issues to those diagnosed on a clinical basis. Acta Paediatrica, 106(4), 639-646.
Lind, M., Svensson, A. M., Kosiborod, M., Gudbjörnsdottir, S., Pivodic, A., Wedel, H., ... & Rosengren, A. (2014). Glycemic control and excess mortality in
type 1 diabetes. New England Journal of Medicine, 371(21), 1972-1982.
Patterson, C., Guariguata, L., Dahlquist, G., Soltész, G., Ogle, G., & Silink, M. (2014). Diabetes in the young–a global view and worldwide estimates of
numbers of children with type 1 diabetes. Diabetes research and clinical practice, 103(2), 161-175.
See, J. A., Kaukinen, K., Makharia, G. K., Gibson, P. R., & Murray, J. A. (2015). Practical insights into gluten-free diets. Nature Reviews Gastroenterology &
Hepatology, 12(10), 580.
Zhang, M. X., Pan, G. T., Guo, J. F., Li, B. Y., Qin, L. Q., & Zhang, Z. L. (2015). Vitamin D deficiency increases the risk of gestational diabetes mellitus: a
meta-analysis of observational studies. Nutrients, 7(10), 8366-8375.
Willi, S. M., Miller, K. M., DiMeglio, L. A., Klingensmith, G. J., Simmons, J. H., Tamborlane, W. V., ... & Lipman, T. H. (2015). Racial-ethnic disparities in
management and outcomes among children with type 1 diabetes. Pediatrics, peds-2014.
surveillance had similar issues to those diagnosed on a clinical basis. Acta Paediatrica, 106(4), 639-646.
Lind, M., Svensson, A. M., Kosiborod, M., Gudbjörnsdottir, S., Pivodic, A., Wedel, H., ... & Rosengren, A. (2014). Glycemic control and excess mortality in
type 1 diabetes. New England Journal of Medicine, 371(21), 1972-1982.
Patterson, C., Guariguata, L., Dahlquist, G., Soltész, G., Ogle, G., & Silink, M. (2014). Diabetes in the young–a global view and worldwide estimates of
numbers of children with type 1 diabetes. Diabetes research and clinical practice, 103(2), 161-175.
See, J. A., Kaukinen, K., Makharia, G. K., Gibson, P. R., & Murray, J. A. (2015). Practical insights into gluten-free diets. Nature Reviews Gastroenterology &
Hepatology, 12(10), 580.
Zhang, M. X., Pan, G. T., Guo, J. F., Li, B. Y., Qin, L. Q., & Zhang, Z. L. (2015). Vitamin D deficiency increases the risk of gestational diabetes mellitus: a
meta-analysis of observational studies. Nutrients, 7(10), 8366-8375.
Willi, S. M., Miller, K. M., DiMeglio, L. A., Klingensmith, G. J., Simmons, J. H., Tamborlane, W. V., ... & Lipman, T. H. (2015). Racial-ethnic disparities in
management and outcomes among children with type 1 diabetes. Pediatrics, peds-2014.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.