Case Study Analysis: Ventral Septal Defect in Infant Mandy Gray
VerifiedAdded on 2022/09/12
|11
|5213
|33
Case Study
AI Summary
This case study focuses on Mandy Gray, a 2-month-old infant diagnosed with a large ventricular septal defect (VSD) and presenting with acute heart failure. The case details Mandy's history, including her parents' concerns about her breathing difficulties, poor feeding, and below-average growth. It provides a comprehensive overview of relevant data, including physical assessments, vital signs, laboratory results, and diagnostic imaging reports such as chest X-rays and echocardiograms. The case study emphasizes the clinical significance of the collected data, including an irregular heartbeat, cardiomegaly, and increased pulmonary blood flow. It delves into the medical management plan, detailing the rationale and expected outcomes of the prescribed treatments, including medications such as Furosemide, Captopril, and Digoxin. The study also explores the nursing assessments and interventions required to manage Mandy's condition, with a focus on the primary problem of perfusion and interrelated concepts such as gas exchange, clinical judgment, patient education, and communication. The case study concludes with a discussion of lab planning and the importance of monitoring BNP levels, highlighting the complexities of caring for an infant with a congenital heart defect and the critical role of nurses in providing comprehensive care.
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
Ventral Septal Defect
UNFOLDING Reasoning
Mandy Gray, 2 months old
Primary Concept
Perfusion
Interrelated Concepts (In order of emphasis)
• Gas Exchange
• Clinical Judgment
• Patient Education
• Communication
NCLEX Client Need Categories Percentage of Items from Each
Category/Subcategory
Covered in
Case Study
Safe and Effective Care Environment
✓ Management of Care 17-23% ✓
✓ Safety and Infection Control 9-15%
Health Promotion and Maintenance 6-12% ✓
Psychosocial Integrity 6-12% ✓
Physiological Integrity
✓ Basic Care and Comfort 6-12% ✓
✓ Pharmacological and Parenteral Therapies 12-18% ✓
✓ Reduction of Risk Potential 9-15% ✓
✓ Physiological Adaptation 11-17% ✓
Ventral Septal Defect
UNFOLDING Reasoning
Mandy Gray, 2 months old
Primary Concept
Perfusion
Interrelated Concepts (In order of emphasis)
• Gas Exchange
• Clinical Judgment
• Patient Education
• Communication
NCLEX Client Need Categories Percentage of Items from Each
Category/Subcategory
Covered in
Case Study
Safe and Effective Care Environment
✓ Management of Care 17-23% ✓
✓ Safety and Infection Control 9-15%
Health Promotion and Maintenance 6-12% ✓
Psychosocial Integrity 6-12% ✓
Physiological Integrity
✓ Basic Care and Comfort 6-12% ✓
✓ Pharmacological and Parenteral Therapies 12-18% ✓
✓ Reduction of Risk Potential 9-15% ✓
✓ Physiological Adaptation 11-17% ✓
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
History of Present Problem:
Mandy Gray is a two-month-old infant born with a large ventricular septal defect (VSD) that was diagnosed by
her pediatrician during her two-week infant check-up. The parents called her pediatric cardiology clinic
because Mandy was breathing faster and showed signs of increased work of breathing. Her mother states that
she is having difficulty nursing because she tires easily and then becomes fussy and cries because she is
hungry. Her height and weight are below the 25th percentile (wt: 4.5 kg. ht: 54 cm). Her Mom reports that
Mandy’s weight has increased by 8 ounces (240 g) in the last 24 hours. Her pediatric cardiologist is concerned
about worsening heart failure and Mancy will be admitted with a diagnosis of acute heart failure.
Personal/Social History:
Mandy is the first child of Jim and Jessica who were married two years ago. They were both raised in the
Catholic faith but are not active in the church. Both parents seem anxious about their infant daughter but
express hopefulness about the surgery to correct the problem. The surgery is scheduled in four months. Her
mother is an RN who works in a dermatology clinic. Since Mandy’s birth, her mother has stayed home to care
for Mandy because she is too medically fragile to be cared for in a daycare setting. Both of Jim’s parents are
deceased, and Jessica’s parents live in another state.
What data from the histories are RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential)
RELEVANT Data from Present Problem: Clinical Significance:
RELEVANT Data from Social History: Clinical Significance:
Patient Care Begins:
What VS data are RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential/Health Promotion and Maintenance)
RELEVANT VS Data: Clinical Significance:
Current VS: FLACC Behavioral Pain Assessment Scale:
T: 99.4 F/37.5 C (temporal) Face: 1
P: 210/min (regular) Legs: 0
R: 74/min Activity: 0
BP: 70/45 MAP: 50 Cry: 1
O2 sat: 90% on RA Consolability: 0
a. Breaths faster
b. Difficulty in breathing
c. Gets tired easily
d. Becomes precious and cries
e. Gained only 8 ounces and below 25% than normal
weight
Ventricular septal defect (VSD) means a small hole in heart. In VSD
oxygenated blood gets mixed with deoxygenated blood making the heart to
work harder to supply oxygen o the tissues present in Mandy’s body (Bhatla
et al. 2017). Therefore, she is having difficulty in breathing. While eating the
infant feels difficulty in breathing, hence do not eat however feels hungry and
try. As the baby is not eating does not gain weight.
Mandy is having surgery in 4 months Doctor does an incision in the chest wall and heart-lung machine is maintained for
blood circulation. The doctor closes the hole by stitching or by applying some
surgical material. Slowly, the heart tissue heals and after 6 months of surgery
Mandy’s heart hole will heal completely (Deri and English 2018).
P, R, BP, O2 sat The pulse rate (P) and the respiration is higher than normal as the baby is having
difficulty in breathing and her heart is not working due to mix of oxygenated and
deoxygenated blood (Jortveit et al. 2016). The increase in pulse rate occurs and
hence, due to less supply of oxygen (O2 sat) to the tissues, Mandy feels difficulty in
breathing (R). As Mandy is having heart disease her systolic pressure(BP) is lower
than the normal range (72-102)
History of Present Problem:
Mandy Gray is a two-month-old infant born with a large ventricular septal defect (VSD) that was diagnosed by
her pediatrician during her two-week infant check-up. The parents called her pediatric cardiology clinic
because Mandy was breathing faster and showed signs of increased work of breathing. Her mother states that
she is having difficulty nursing because she tires easily and then becomes fussy and cries because she is
hungry. Her height and weight are below the 25th percentile (wt: 4.5 kg. ht: 54 cm). Her Mom reports that
Mandy’s weight has increased by 8 ounces (240 g) in the last 24 hours. Her pediatric cardiologist is concerned
about worsening heart failure and Mancy will be admitted with a diagnosis of acute heart failure.
Personal/Social History:
Mandy is the first child of Jim and Jessica who were married two years ago. They were both raised in the
Catholic faith but are not active in the church. Both parents seem anxious about their infant daughter but
express hopefulness about the surgery to correct the problem. The surgery is scheduled in four months. Her
mother is an RN who works in a dermatology clinic. Since Mandy’s birth, her mother has stayed home to care
for Mandy because she is too medically fragile to be cared for in a daycare setting. Both of Jim’s parents are
deceased, and Jessica’s parents live in another state.
What data from the histories are RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential)
RELEVANT Data from Present Problem: Clinical Significance:
RELEVANT Data from Social History: Clinical Significance:
Patient Care Begins:
What VS data are RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential/Health Promotion and Maintenance)
RELEVANT VS Data: Clinical Significance:
Current VS: FLACC Behavioral Pain Assessment Scale:
T: 99.4 F/37.5 C (temporal) Face: 1
P: 210/min (regular) Legs: 0
R: 74/min Activity: 0
BP: 70/45 MAP: 50 Cry: 1
O2 sat: 90% on RA Consolability: 0
a. Breaths faster
b. Difficulty in breathing
c. Gets tired easily
d. Becomes precious and cries
e. Gained only 8 ounces and below 25% than normal
weight
Ventricular septal defect (VSD) means a small hole in heart. In VSD
oxygenated blood gets mixed with deoxygenated blood making the heart to
work harder to supply oxygen o the tissues present in Mandy’s body (Bhatla
et al. 2017). Therefore, she is having difficulty in breathing. While eating the
infant feels difficulty in breathing, hence do not eat however feels hungry and
try. As the baby is not eating does not gain weight.
Mandy is having surgery in 4 months Doctor does an incision in the chest wall and heart-lung machine is maintained for
blood circulation. The doctor closes the hole by stitching or by applying some
surgical material. Slowly, the heart tissue heals and after 6 months of surgery
Mandy’s heart hole will heal completely (Deri and English 2018).
P, R, BP, O2 sat The pulse rate (P) and the respiration is higher than normal as the baby is having
difficulty in breathing and her heart is not working due to mix of oxygenated and
deoxygenated blood (Jortveit et al. 2016). The increase in pulse rate occurs and
hence, due to less supply of oxygen (O2 sat) to the tissues, Mandy feels difficulty in
breathing (R). As Mandy is having heart disease her systolic pressure(BP) is lower
than the normal range (72-102)
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
What assessment data is RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential/Health Promotion & Maintenance)
RELEVANT Assessment Data: Clinical Significance:
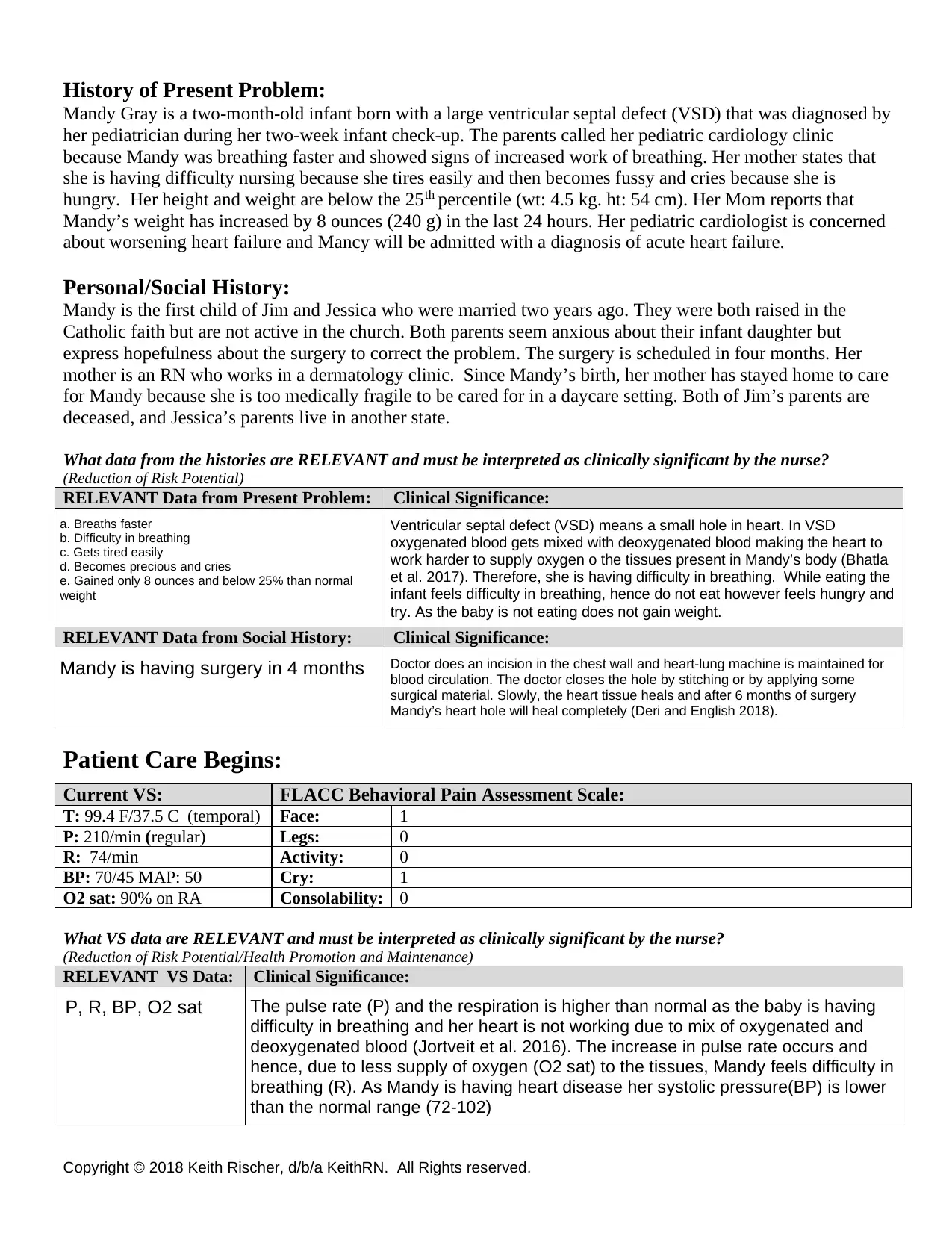
Cardiac Telemetry Strip:
Regular/Irregular: P wave present? PR: QRS: QT:
Interpretation:
Clinical Significance:
Current Assessment:
GENERAL
APPEARANCE:
Pale in color, quiet while in mother’s arms. Working moderately hard to breathe and
appears tired with eyes closing but startles awake with loud sounds or voice
RESP: Fine crackles at bases bilaterally. Grunting noted with expirations and mild to moderate
sub-costal retractions and slight nasal flaring
CARDIAC: Pallor noted at face and trunk; capillary refill is greater than 2 seconds. Grade 3/6
holosystolic murmur heard at 3rd, 4th, 5th intercostal space at the left sternal border. Apical
heart rate is rapid and peripheral pulses are equal, weak but palpable, lower extremities 1+
pitting edema
NEURO: Awake but appears tired. Responds to mother and father appropriately with an occasional
smile.
GI: Abdomen rounded, soft and non-tender, hepatosplenomegaly present, bowel sounds audible
GU: Per Mom, has only had one wet diaper today
SKIN: Skin integrity intact, skin turgor elastic
Pale in color, respiration, cardiac,
GU
The general, cardiac and respiratory assessment states that due a hole in
ventricular wall, Mandy is suffering and showing all these symptoms. The
level of oxygen is low in her blood, hence RBC count decreases causing
anemia and turning her skin pale. Moreover, she is not eating or drinking
therefore there is only wet diaper used whole day (Egbe et al. 2015). Even
the assessment showed that Mandy produces grunting sound while
expiration because of the difficulty she is having in breathing. As she is not
eating or drinking she is not getting energy and therefore she is often tired.
The data received highly significant with Mandy’s situation. Irregular heartbeat, ventricular hypertrophy, arterial enlargement all signify the presence of hole in her heart (ventricular wall) (Karonis et al. 2016).
What assessment data is RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential/Health Promotion & Maintenance)
RELEVANT Assessment Data: Clinical Significance:
Cardiac Telemetry Strip:
Regular/Irregular: P wave present? PR: QRS: QT:
Interpretation:
Clinical Significance:
Current Assessment:
GENERAL
APPEARANCE:
Pale in color, quiet while in mother’s arms. Working moderately hard to breathe and
appears tired with eyes closing but startles awake with loud sounds or voice
RESP: Fine crackles at bases bilaterally. Grunting noted with expirations and mild to moderate
sub-costal retractions and slight nasal flaring
CARDIAC: Pallor noted at face and trunk; capillary refill is greater than 2 seconds. Grade 3/6
holosystolic murmur heard at 3rd, 4th, 5th intercostal space at the left sternal border. Apical
heart rate is rapid and peripheral pulses are equal, weak but palpable, lower extremities 1+
pitting edema
NEURO: Awake but appears tired. Responds to mother and father appropriately with an occasional
smile.
GI: Abdomen rounded, soft and non-tender, hepatosplenomegaly present, bowel sounds audible
GU: Per Mom, has only had one wet diaper today
SKIN: Skin integrity intact, skin turgor elastic
Pale in color, respiration, cardiac,
GU
The general, cardiac and respiratory assessment states that due a hole in
ventricular wall, Mandy is suffering and showing all these symptoms. The
level of oxygen is low in her blood, hence RBC count decreases causing
anemia and turning her skin pale. Moreover, she is not eating or drinking
therefore there is only wet diaper used whole day (Egbe et al. 2015). Even
the assessment showed that Mandy produces grunting sound while
expiration because of the difficulty she is having in breathing. As she is not
eating or drinking she is not getting energy and therefore she is often tired.
The data received highly significant with Mandy’s situation. Irregular heartbeat, ventricular hypertrophy, arterial enlargement all signify the presence of hole in her heart (ventricular wall) (Karonis et al. 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
Radiology Reports:
What diagnostic results are RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
Radiology: Chest X-Ray
Results: Clinical Significance:
Cardiomegaly and increased
pulmonary blood flow
Radiology: Cardiac Echocardiogram
Results: Clinical Significance:
Large perimembranous
ventricular septal wall defect
(VSD)
Lab Results: Complete Blood Count (CBC)
WBC HGB PLTs % Neuts
Current: 8.0 10.2 205 60
Most Recent: 8.5 10.5 250 55
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND:
Improve/Worsening/Stable:
Basic Metabolic Panel (BMP)
Na K Gluc. Creat.
Current: 130 5.5 70 0.2
Most Recent: 133 4.5 80 0.3
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND:
Improve/Worsening/Stable:
MISC.Misc.
Mag Total Calcium Lactic Acid GFR PT/INR
Current: 1.6 9.0 17.1 55 0.95
Most Recent: 2.0 8.9 10.0 57 1.0
It signifies that left-to-right shunt where there is additional capacity of blood flow causing enlargement of heart chambers. Here
pulmonary artery increases and blood flow also increases. Impediment of blood flow produces hypertension in pulmonary
venous as well as resultant pulmonary edema.
The ECG data is highly significant in concluding that Mandy’s heart is not working
properly, hence she requires special attention. It also helped in identification that the
left ventricle outflow tract that is located under the aortic valve is not functioning
properly (An et al. 2015).
PLT (150-450)
WBC (6-17.5)
HGB (9-14)
HGB count is slightly low than the normal, it might be
due to less oxygenrated blood in the body as hence less
supply of healthy blood to the tissues (Kang et al. 2015)
Worsening
Na, K and Creatinine
(Creat) The nurse felt it clinically significant as Mandy’s is not eating
anything her level of nutrition is falling down, she is running out of
malnutrition.
Worsening
Radiology Reports:
What diagnostic results are RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
Radiology: Chest X-Ray
Results: Clinical Significance:
Cardiomegaly and increased
pulmonary blood flow
Radiology: Cardiac Echocardiogram
Results: Clinical Significance:
Large perimembranous
ventricular septal wall defect
(VSD)
Lab Results: Complete Blood Count (CBC)
WBC HGB PLTs % Neuts
Current: 8.0 10.2 205 60
Most Recent: 8.5 10.5 250 55
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND:
Improve/Worsening/Stable:
Basic Metabolic Panel (BMP)
Na K Gluc. Creat.
Current: 130 5.5 70 0.2
Most Recent: 133 4.5 80 0.3
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND:
Improve/Worsening/Stable:
MISC.Misc.
Mag Total Calcium Lactic Acid GFR PT/INR
Current: 1.6 9.0 17.1 55 0.95
Most Recent: 2.0 8.9 10.0 57 1.0
It signifies that left-to-right shunt where there is additional capacity of blood flow causing enlargement of heart chambers. Here
pulmonary artery increases and blood flow also increases. Impediment of blood flow produces hypertension in pulmonary
venous as well as resultant pulmonary edema.
The ECG data is highly significant in concluding that Mandy’s heart is not working
properly, hence she requires special attention. It also helped in identification that the
left ventricle outflow tract that is located under the aortic valve is not functioning
properly (An et al. 2015).
PLT (150-450)
WBC (6-17.5)
HGB (9-14)
HGB count is slightly low than the normal, it might be
due to less oxygenrated blood in the body as hence less
supply of healthy blood to the tissues (Kang et al. 2015)
Worsening
Na, K and Creatinine
(Creat) The nurse felt it clinically significant as Mandy’s is not eating
anything her level of nutrition is falling down, she is running out of
malnutrition.
Worsening
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
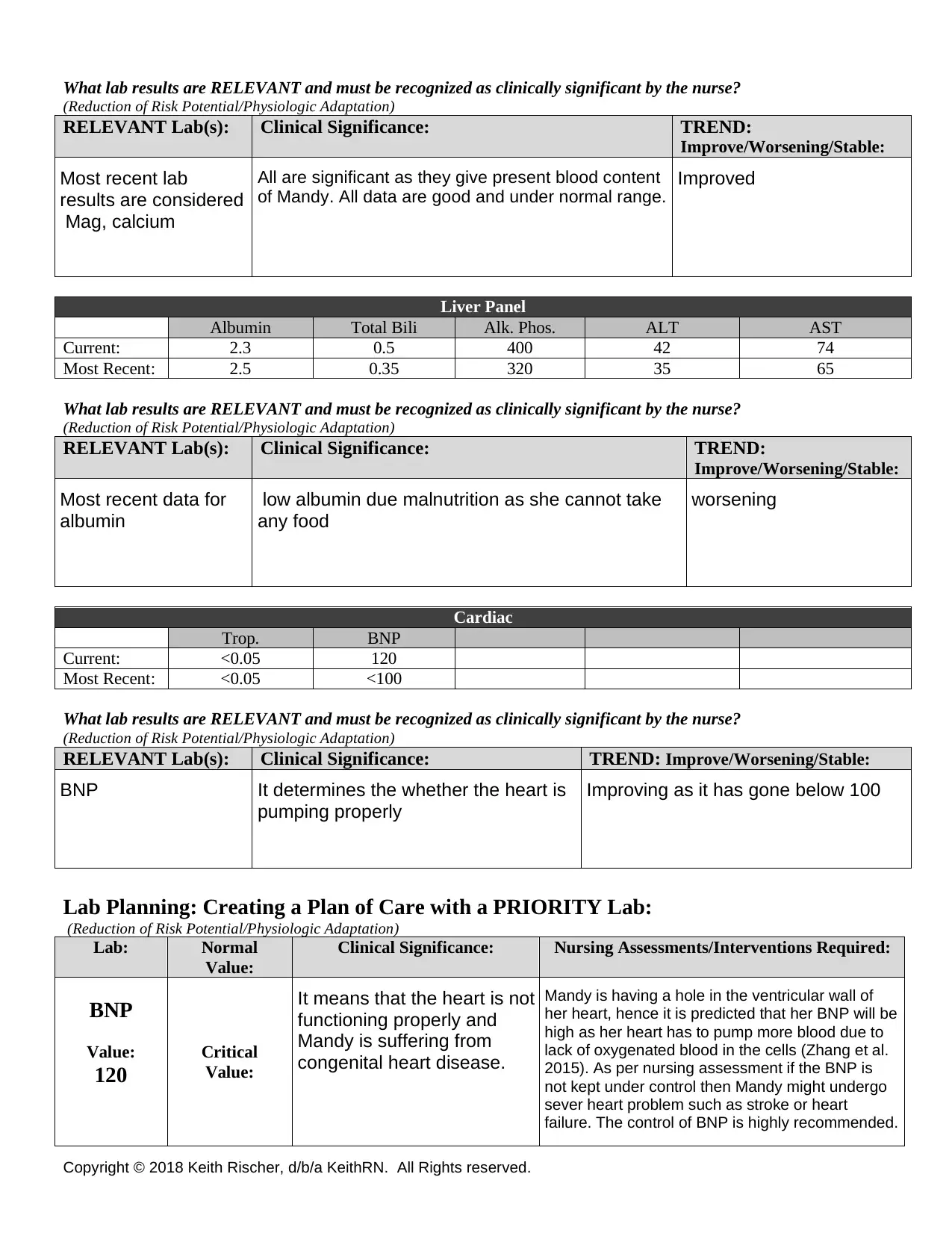
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND:
Improve/Worsening/Stable:
Liver Panel
Albumin Total Bili Alk. Phos. ALT AST
Current: 2.3 0.5 400 42 74
Most Recent: 2.5 0.35 320 35 65
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND:
Improve/Worsening/Stable:
Cardiac
Trop. BNP
Current: <0.05 120
Most Recent: <0.05 <100
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable:
Lab Planning: Creating a Plan of Care with a PRIORITY Lab:
(Reduction of Risk Potential/Physiologic Adaptation)
Lab: Normal
Value:
Clinical Significance: Nursing Assessments/Interventions Required:
BNP
Value:
120
Critical
Value:
Most recent lab
results are considered
Mag, calcium
All are significant as they give present blood content
of Mandy. All data are good and under normal range.
Improved
Most recent data for
albumin
low albumin due malnutrition as she cannot take
any food
worsening
BNP It determines the whether the heart is
pumping properly
Improving as it has gone below 100
It means that the heart is not
functioning properly and
Mandy is suffering from
congenital heart disease.
Mandy is having a hole in the ventricular wall of
her heart, hence it is predicted that her BNP will be
high as her heart has to pump more blood due to
lack of oxygenated blood in the cells (Zhang et al.
2015). As per nursing assessment if the BNP is
not kept under control then Mandy might undergo
sever heart problem such as stroke or heart
failure. The control of BNP is highly recommended.
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND:
Improve/Worsening/Stable:
Liver Panel
Albumin Total Bili Alk. Phos. ALT AST
Current: 2.3 0.5 400 42 74
Most Recent: 2.5 0.35 320 35 65
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND:
Improve/Worsening/Stable:
Cardiac
Trop. BNP
Current: <0.05 120
Most Recent: <0.05 <100
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
(Reduction of Risk Potential/Physiologic Adaptation)
RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable:
Lab Planning: Creating a Plan of Care with a PRIORITY Lab:
(Reduction of Risk Potential/Physiologic Adaptation)
Lab: Normal
Value:
Clinical Significance: Nursing Assessments/Interventions Required:
BNP
Value:
120
Critical
Value:
Most recent lab
results are considered
Mag, calcium
All are significant as they give present blood content
of Mandy. All data are good and under normal range.
Improved
Most recent data for
albumin
low albumin due malnutrition as she cannot take
any food
worsening
BNP It determines the whether the heart is
pumping properly
Improving as it has gone below 100
It means that the heart is not
functioning properly and
Mandy is suffering from
congenital heart disease.
Mandy is having a hole in the ventricular wall of
her heart, hence it is predicted that her BNP will be
high as her heart has to pump more blood due to
lack of oxygenated blood in the cells (Zhang et al.
2015). As per nursing assessment if the BNP is
not kept under control then Mandy might undergo
sever heart problem such as stroke or heart
failure. The control of BNP is highly recommended.
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
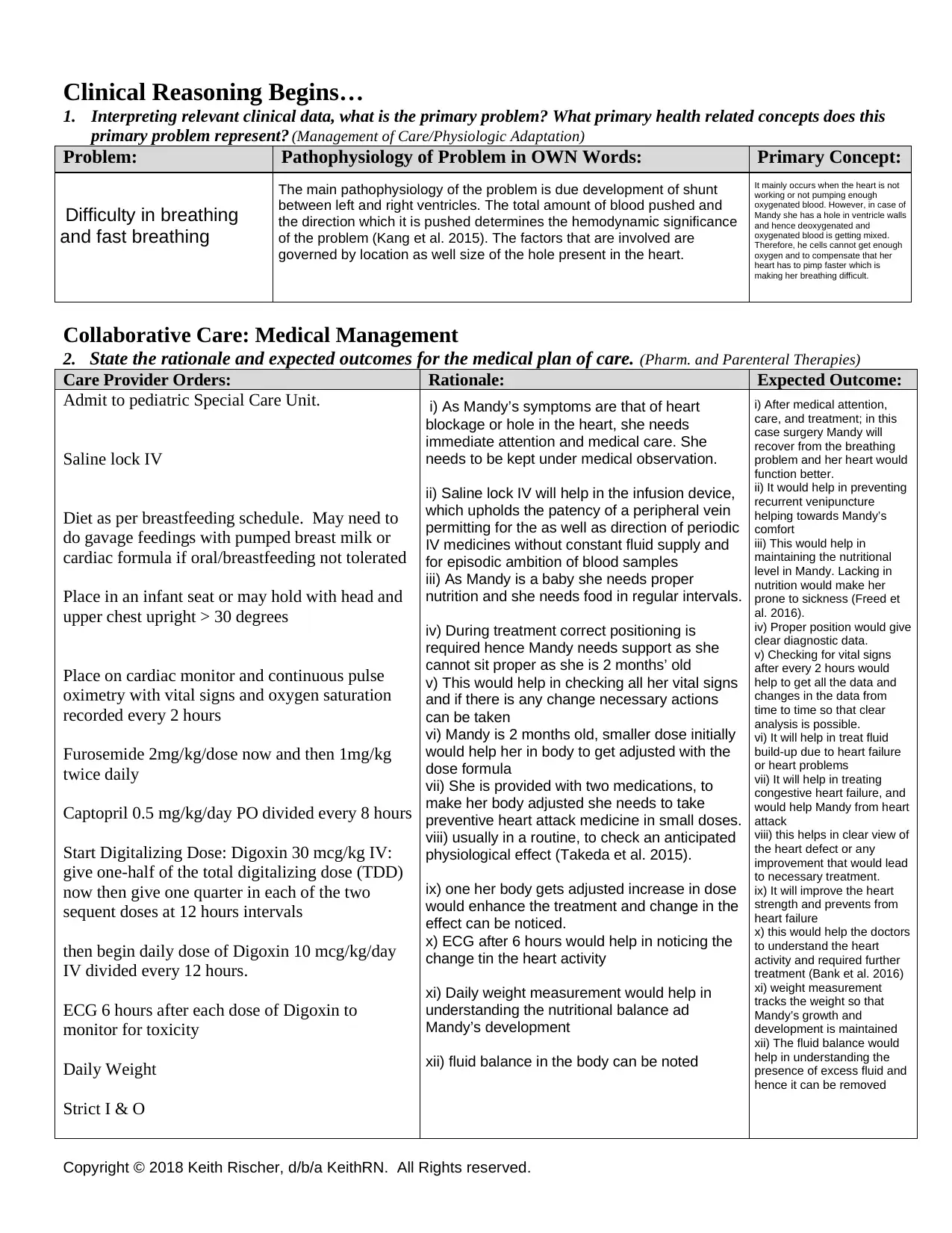
Clinical Reasoning Begins…
1. Interpreting relevant clinical data, what is the primary problem? What primary health related concepts does this
primary problem represent? (Management of Care/Physiologic Adaptation)
Problem: Pathophysiology of Problem in OWN Words: Primary Concept:
Collaborative Care: Medical Management
2. State the rationale and expected outcomes for the medical plan of care. (Pharm. and Parenteral Therapies)
Care Provider Orders: Rationale: Expected Outcome:
Admit to pediatric Special Care Unit.
Saline lock IV
Diet as per breastfeeding schedule. May need to
do gavage feedings with pumped breast milk or
cardiac formula if oral/breastfeeding not tolerated
Place in an infant seat or may hold with head and
upper chest upright > 30 degrees
Place on cardiac monitor and continuous pulse
oximetry with vital signs and oxygen saturation
recorded every 2 hours
Furosemide 2mg/kg/dose now and then 1mg/kg
twice daily
Captopril 0.5 mg/kg/day PO divided every 8 hours
Start Digitalizing Dose: Digoxin 30 mcg/kg IV:
give one-half of the total digitalizing dose (TDD)
now then give one quarter in each of the two
sequent doses at 12 hours intervals
then begin daily dose of Digoxin 10 mcg/kg/day
IV divided every 12 hours.
ECG 6 hours after each dose of Digoxin to
monitor for toxicity
Daily Weight
Strict I & O
Difficulty in breathing
and fast breathing
The main pathophysiology of the problem is due development of shunt
between left and right ventricles. The total amount of blood pushed and
the direction which it is pushed determines the hemodynamic significance
of the problem (Kang et al. 2015). The factors that are involved are
governed by location as well size of the hole present in the heart.
It mainly occurs when the heart is not
working or not pumping enough
oxygenated blood. However, in case of
Mandy she has a hole in ventricle walls
and hence deoxygenated and
oxygenated blood is getting mixed.
Therefore, he cells cannot get enough
oxygen and to compensate that her
heart has to pimp faster which is
making her breathing difficult.
i) As Mandy’s symptoms are that of heart
blockage or hole in the heart, she needs
immediate attention and medical care. She
needs to be kept under medical observation.
ii) Saline lock IV will help in the infusion device,
which upholds the patency of a peripheral vein
permitting for the as well as direction of periodic
IV medicines without constant fluid supply and
for episodic ambition of blood samples
iii) As Mandy is a baby she needs proper
nutrition and she needs food in regular intervals.
iv) During treatment correct positioning is
required hence Mandy needs support as she
cannot sit proper as she is 2 months’ old
v) This would help in checking all her vital signs
and if there is any change necessary actions
can be taken
vi) Mandy is 2 months old, smaller dose initially
would help her in body to get adjusted with the
dose formula
vii) She is provided with two medications, to
make her body adjusted she needs to take
preventive heart attack medicine in small doses.
viii) usually in a routine, to check an anticipated
physiological effect (Takeda et al. 2015).
ix) one her body gets adjusted increase in dose
would enhance the treatment and change in the
effect can be noticed.
x) ECG after 6 hours would help in noticing the
change tin the heart activity
xi) Daily weight measurement would help in
understanding the nutritional balance ad
Mandy’s development
xii) fluid balance in the body can be noted
i) After medical attention,
care, and treatment; in this
case surgery Mandy will
recover from the breathing
problem and her heart would
function better.
ii) It would help in preventing
recurrent venipuncture
helping towards Mandy’s
comfort
iii) This would help in
maintaining the nutritional
level in Mandy. Lacking in
nutrition would make her
prone to sickness (Freed et
al. 2016).
iv) Proper position would give
clear diagnostic data.
v) Checking for vital signs
after every 2 hours would
help to get all the data and
changes in the data from
time to time so that clear
analysis is possible.
vi) It will help in treat fluid
build-up due to heart failure
or heart problems
vii) It will help in treating
congestive heart failure, and
would help Mandy from heart
attack
viii) this helps in clear view of
the heart defect or any
improvement that would lead
to necessary treatment.
ix) It will improve the heart
strength and prevents from
heart failure
x) this would help the doctors
to understand the heart
activity and required further
treatment (Bank et al. 2016)
xi) weight measurement
tracks the weight so that
Mandy’s growth and
development is maintained
xii) The fluid balance would
help in understanding the
presence of excess fluid and
hence it can be removed
Clinical Reasoning Begins…
1. Interpreting relevant clinical data, what is the primary problem? What primary health related concepts does this
primary problem represent? (Management of Care/Physiologic Adaptation)
Problem: Pathophysiology of Problem in OWN Words: Primary Concept:
Collaborative Care: Medical Management
2. State the rationale and expected outcomes for the medical plan of care. (Pharm. and Parenteral Therapies)
Care Provider Orders: Rationale: Expected Outcome:
Admit to pediatric Special Care Unit.
Saline lock IV
Diet as per breastfeeding schedule. May need to
do gavage feedings with pumped breast milk or
cardiac formula if oral/breastfeeding not tolerated
Place in an infant seat or may hold with head and
upper chest upright > 30 degrees
Place on cardiac monitor and continuous pulse
oximetry with vital signs and oxygen saturation
recorded every 2 hours
Furosemide 2mg/kg/dose now and then 1mg/kg
twice daily
Captopril 0.5 mg/kg/day PO divided every 8 hours
Start Digitalizing Dose: Digoxin 30 mcg/kg IV:
give one-half of the total digitalizing dose (TDD)
now then give one quarter in each of the two
sequent doses at 12 hours intervals
then begin daily dose of Digoxin 10 mcg/kg/day
IV divided every 12 hours.
ECG 6 hours after each dose of Digoxin to
monitor for toxicity
Daily Weight
Strict I & O
Difficulty in breathing
and fast breathing
The main pathophysiology of the problem is due development of shunt
between left and right ventricles. The total amount of blood pushed and
the direction which it is pushed determines the hemodynamic significance
of the problem (Kang et al. 2015). The factors that are involved are
governed by location as well size of the hole present in the heart.
It mainly occurs when the heart is not
working or not pumping enough
oxygenated blood. However, in case of
Mandy she has a hole in ventricle walls
and hence deoxygenated and
oxygenated blood is getting mixed.
Therefore, he cells cannot get enough
oxygen and to compensate that her
heart has to pimp faster which is
making her breathing difficult.
i) As Mandy’s symptoms are that of heart
blockage or hole in the heart, she needs
immediate attention and medical care. She
needs to be kept under medical observation.
ii) Saline lock IV will help in the infusion device,
which upholds the patency of a peripheral vein
permitting for the as well as direction of periodic
IV medicines without constant fluid supply and
for episodic ambition of blood samples
iii) As Mandy is a baby she needs proper
nutrition and she needs food in regular intervals.
iv) During treatment correct positioning is
required hence Mandy needs support as she
cannot sit proper as she is 2 months’ old
v) This would help in checking all her vital signs
and if there is any change necessary actions
can be taken
vi) Mandy is 2 months old, smaller dose initially
would help her in body to get adjusted with the
dose formula
vii) She is provided with two medications, to
make her body adjusted she needs to take
preventive heart attack medicine in small doses.
viii) usually in a routine, to check an anticipated
physiological effect (Takeda et al. 2015).
ix) one her body gets adjusted increase in dose
would enhance the treatment and change in the
effect can be noticed.
x) ECG after 6 hours would help in noticing the
change tin the heart activity
xi) Daily weight measurement would help in
understanding the nutritional balance ad
Mandy’s development
xii) fluid balance in the body can be noted
i) After medical attention,
care, and treatment; in this
case surgery Mandy will
recover from the breathing
problem and her heart would
function better.
ii) It would help in preventing
recurrent venipuncture
helping towards Mandy’s
comfort
iii) This would help in
maintaining the nutritional
level in Mandy. Lacking in
nutrition would make her
prone to sickness (Freed et
al. 2016).
iv) Proper position would give
clear diagnostic data.
v) Checking for vital signs
after every 2 hours would
help to get all the data and
changes in the data from
time to time so that clear
analysis is possible.
vi) It will help in treat fluid
build-up due to heart failure
or heart problems
vii) It will help in treating
congestive heart failure, and
would help Mandy from heart
attack
viii) this helps in clear view of
the heart defect or any
improvement that would lead
to necessary treatment.
ix) It will improve the heart
strength and prevents from
heart failure
x) this would help the doctors
to understand the heart
activity and required further
treatment (Bank et al. 2016)
xi) weight measurement
tracks the weight so that
Mandy’s growth and
development is maintained
xii) The fluid balance would
help in understanding the
presence of excess fluid and
hence it can be removed
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
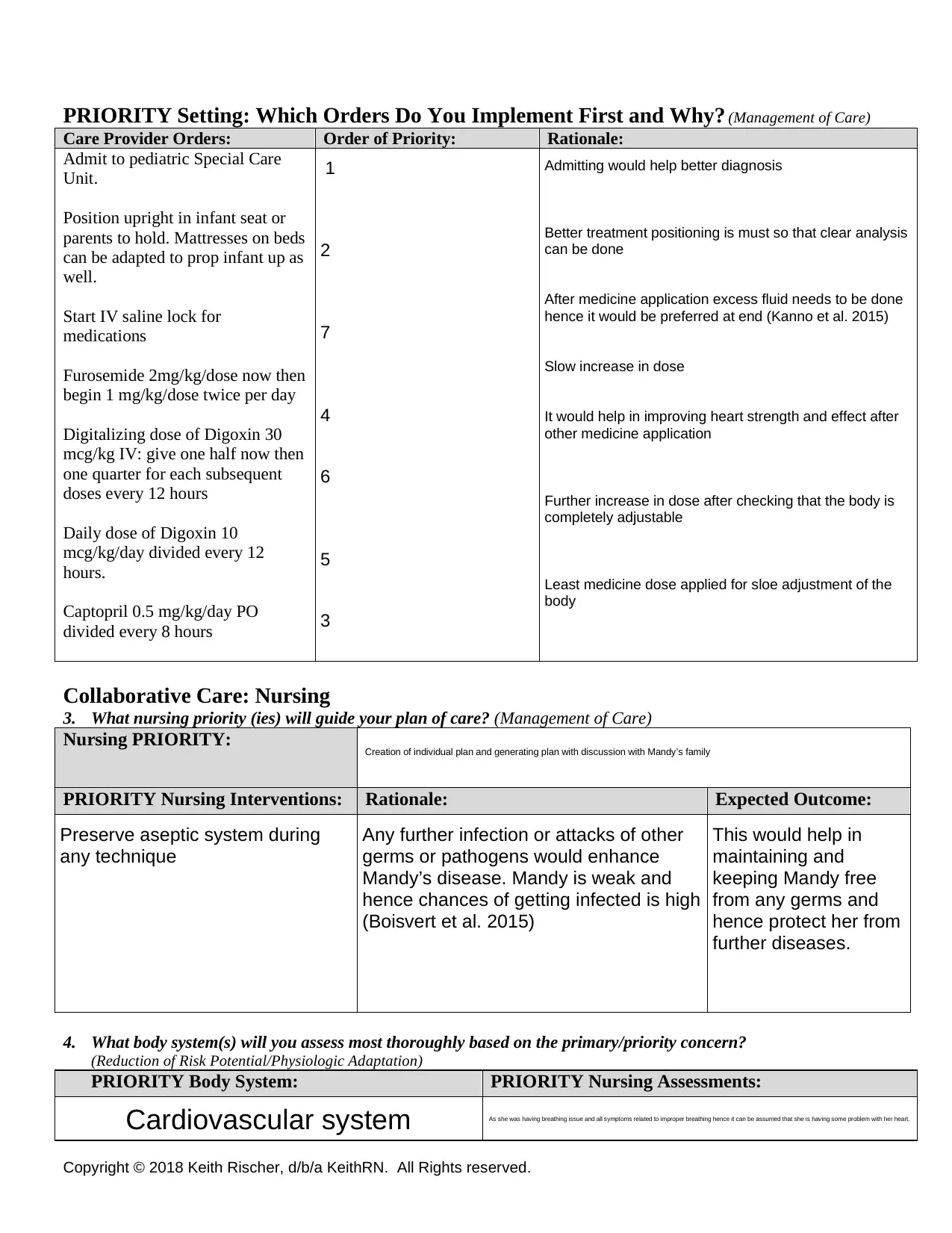
PRIORITY Setting: Which Orders Do You Implement First and Why? (Management of Care)
Care Provider Orders: Order of Priority: Rationale:
Admit to pediatric Special Care
Unit.
Position upright in infant seat or
parents to hold. Mattresses on beds
can be adapted to prop infant up as
well.
Start IV saline lock for
medications
Furosemide 2mg/kg/dose now then
begin 1 mg/kg/dose twice per day
Digitalizing dose of Digoxin 30
mcg/kg IV: give one half now then
one quarter for each subsequent
doses every 12 hours
Daily dose of Digoxin 10
mcg/kg/day divided every 12
hours.
Captopril 0.5 mg/kg/day PO
divided every 8 hours
Collaborative Care: Nursing
3. What nursing priority (ies) will guide your plan of care? (Management of Care)
Nursing PRIORITY:
PRIORITY Nursing Interventions: Rationale: Expected Outcome:
4. What body system(s) will you assess most thoroughly based on the primary/priority concern?
(Reduction of Risk Potential/Physiologic Adaptation)
PRIORITY Body System: PRIORITY Nursing Assessments:
1
2
7
4
6
5
3
Admitting would help better diagnosis
Better treatment positioning is must so that clear analysis
can be done
After medicine application excess fluid needs to be done
hence it would be preferred at end (Kanno et al. 2015)
Slow increase in dose
It would help in improving heart strength and effect after
other medicine application
Further increase in dose after checking that the body is
completely adjustable
Least medicine dose applied for sloe adjustment of the
body
Creation of individual plan and generating plan with discussion with Mandy’s family
Preserve aseptic system during
any technique
Any further infection or attacks of other
germs or pathogens would enhance
Mandy’s disease. Mandy is weak and
hence chances of getting infected is high
(Boisvert et al. 2015)
This would help in
maintaining and
keeping Mandy free
from any germs and
hence protect her from
further diseases.
Cardiovascular system As she was having breathing issue and all symptoms related to improper breathing hence it can be assumed that she is having some problem with her heart.
PRIORITY Setting: Which Orders Do You Implement First and Why? (Management of Care)
Care Provider Orders: Order of Priority: Rationale:
Admit to pediatric Special Care
Unit.
Position upright in infant seat or
parents to hold. Mattresses on beds
can be adapted to prop infant up as
well.
Start IV saline lock for
medications
Furosemide 2mg/kg/dose now then
begin 1 mg/kg/dose twice per day
Digitalizing dose of Digoxin 30
mcg/kg IV: give one half now then
one quarter for each subsequent
doses every 12 hours
Daily dose of Digoxin 10
mcg/kg/day divided every 12
hours.
Captopril 0.5 mg/kg/day PO
divided every 8 hours
Collaborative Care: Nursing
3. What nursing priority (ies) will guide your plan of care? (Management of Care)
Nursing PRIORITY:
PRIORITY Nursing Interventions: Rationale: Expected Outcome:
4. What body system(s) will you assess most thoroughly based on the primary/priority concern?
(Reduction of Risk Potential/Physiologic Adaptation)
PRIORITY Body System: PRIORITY Nursing Assessments:
1
2
7
4
6
5
3
Admitting would help better diagnosis
Better treatment positioning is must so that clear analysis
can be done
After medicine application excess fluid needs to be done
hence it would be preferred at end (Kanno et al. 2015)
Slow increase in dose
It would help in improving heart strength and effect after
other medicine application
Further increase in dose after checking that the body is
completely adjustable
Least medicine dose applied for sloe adjustment of the
body
Creation of individual plan and generating plan with discussion with Mandy’s family
Preserve aseptic system during
any technique
Any further infection or attacks of other
germs or pathogens would enhance
Mandy’s disease. Mandy is weak and
hence chances of getting infected is high
(Boisvert et al. 2015)
This would help in
maintaining and
keeping Mandy free
from any germs and
hence protect her from
further diseases.
Cardiovascular system As she was having breathing issue and all symptoms related to improper breathing hence it can be assumed that she is having some problem with her heart.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
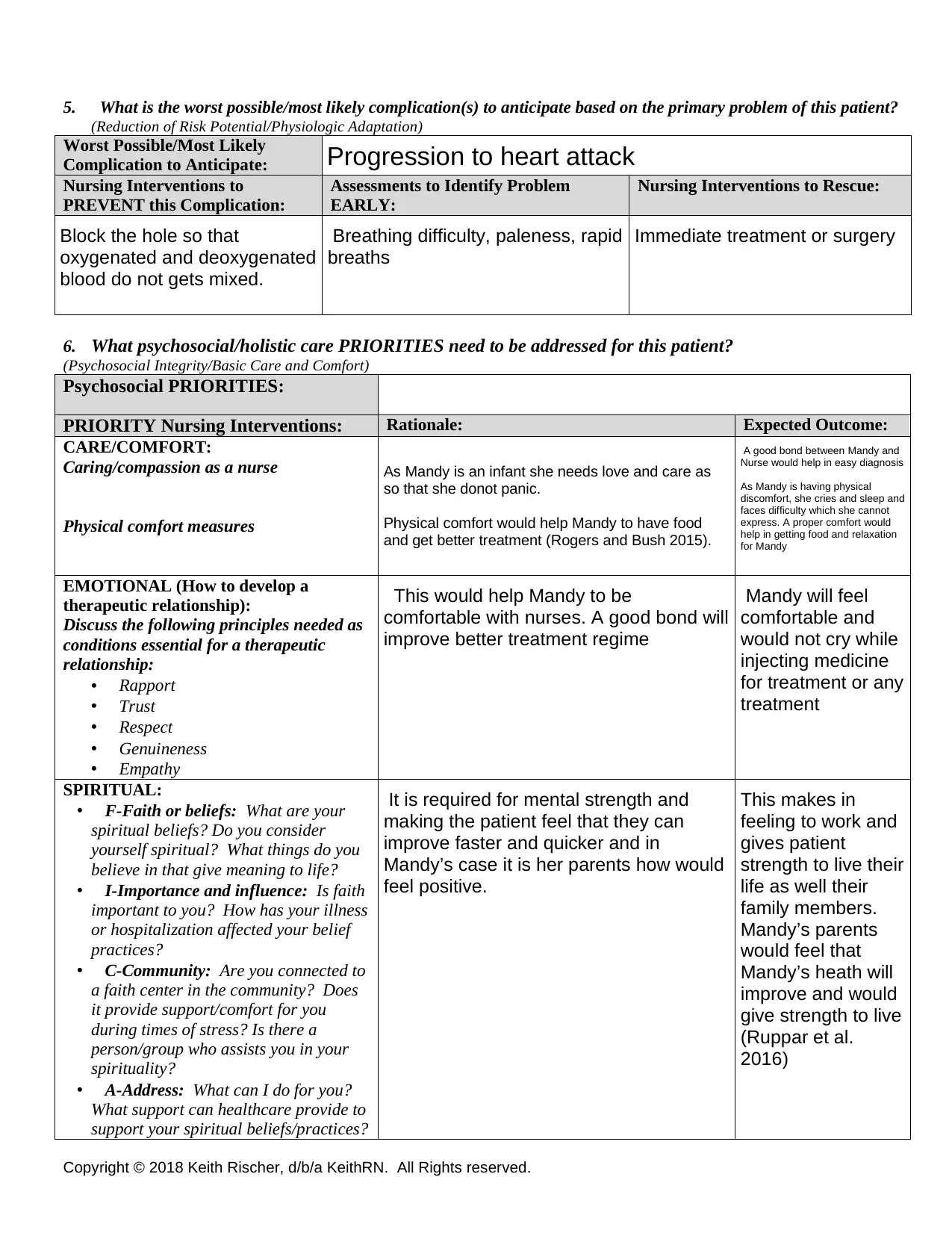
5. What is the worst possible/most likely complication(s) to anticipate based on the primary problem of this patient?
(Reduction of Risk Potential/Physiologic Adaptation)
Worst Possible/Most Likely
Complication to Anticipate:
Nursing Interventions to
PREVENT this Complication:
Assessments to Identify Problem
EARLY:
Nursing Interventions to Rescue:
6. What psychosocial/holistic care PRIORITIES need to be addressed for this patient?
(Psychosocial Integrity/Basic Care and Comfort)
Psychosocial PRIORITIES:
PRIORITY Nursing Interventions: Rationale: Expected Outcome:
CARE/COMFORT:
Caring/compassion as a nurse
Physical comfort measures
EMOTIONAL (How to develop a
therapeutic relationship):
Discuss the following principles needed as
conditions essential for a therapeutic
relationship:
• Rapport
• Trust
• Respect
• Genuineness
• Empathy
SPIRITUAL:
• F-Faith or beliefs: What are your
spiritual beliefs? Do you consider
yourself spiritual? What things do you
believe in that give meaning to life?
• I-Importance and influence: Is faith
important to you? How has your illness
or hospitalization affected your belief
practices?
• C-Community: Are you connected to
a faith center in the community? Does
it provide support/comfort for you
during times of stress? Is there a
person/group who assists you in your
spirituality?
• A-Address: What can I do for you?
What support can healthcare provide to
support your spiritual beliefs/practices?
Progression to heart attack
Block the hole so that
oxygenated and deoxygenated
blood do not gets mixed.
Breathing difficulty, paleness, rapid
breaths
Immediate treatment or surgery
As Mandy is an infant she needs love and care as
so that she donot panic.
Physical comfort would help Mandy to have food
and get better treatment (Rogers and Bush 2015).
A good bond between Mandy and
Nurse would help in easy diagnosis
As Mandy is having physical
discomfort, she cries and sleep and
faces difficulty which she cannot
express. A proper comfort would
help in getting food and relaxation
for Mandy
This would help Mandy to be
comfortable with nurses. A good bond will
improve better treatment regime
Mandy will feel
comfortable and
would not cry while
injecting medicine
for treatment or any
treatment
It is required for mental strength and
making the patient feel that they can
improve faster and quicker and in
Mandy’s case it is her parents how would
feel positive.
This makes in
feeling to work and
gives patient
strength to live their
life as well their
family members.
Mandy’s parents
would feel that
Mandy’s heath will
improve and would
give strength to live
(Ruppar et al.
2016)
5. What is the worst possible/most likely complication(s) to anticipate based on the primary problem of this patient?
(Reduction of Risk Potential/Physiologic Adaptation)
Worst Possible/Most Likely
Complication to Anticipate:
Nursing Interventions to
PREVENT this Complication:
Assessments to Identify Problem
EARLY:
Nursing Interventions to Rescue:
6. What psychosocial/holistic care PRIORITIES need to be addressed for this patient?
(Psychosocial Integrity/Basic Care and Comfort)
Psychosocial PRIORITIES:
PRIORITY Nursing Interventions: Rationale: Expected Outcome:
CARE/COMFORT:
Caring/compassion as a nurse
Physical comfort measures
EMOTIONAL (How to develop a
therapeutic relationship):
Discuss the following principles needed as
conditions essential for a therapeutic
relationship:
• Rapport
• Trust
• Respect
• Genuineness
• Empathy
SPIRITUAL:
• F-Faith or beliefs: What are your
spiritual beliefs? Do you consider
yourself spiritual? What things do you
believe in that give meaning to life?
• I-Importance and influence: Is faith
important to you? How has your illness
or hospitalization affected your belief
practices?
• C-Community: Are you connected to
a faith center in the community? Does
it provide support/comfort for you
during times of stress? Is there a
person/group who assists you in your
spirituality?
• A-Address: What can I do for you?
What support can healthcare provide to
support your spiritual beliefs/practices?
Progression to heart attack
Block the hole so that
oxygenated and deoxygenated
blood do not gets mixed.
Breathing difficulty, paleness, rapid
breaths
Immediate treatment or surgery
As Mandy is an infant she needs love and care as
so that she donot panic.
Physical comfort would help Mandy to have food
and get better treatment (Rogers and Bush 2015).
A good bond between Mandy and
Nurse would help in easy diagnosis
As Mandy is having physical
discomfort, she cries and sleep and
faces difficulty which she cannot
express. A proper comfort would
help in getting food and relaxation
for Mandy
This would help Mandy to be
comfortable with nurses. A good bond will
improve better treatment regime
Mandy will feel
comfortable and
would not cry while
injecting medicine
for treatment or any
treatment
It is required for mental strength and
making the patient feel that they can
improve faster and quicker and in
Mandy’s case it is her parents how would
feel positive.
This makes in
feeling to work and
gives patient
strength to live their
life as well their
family members.
Mandy’s parents
would feel that
Mandy’s heath will
improve and would
give strength to live
(Ruppar et al.
2016)
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
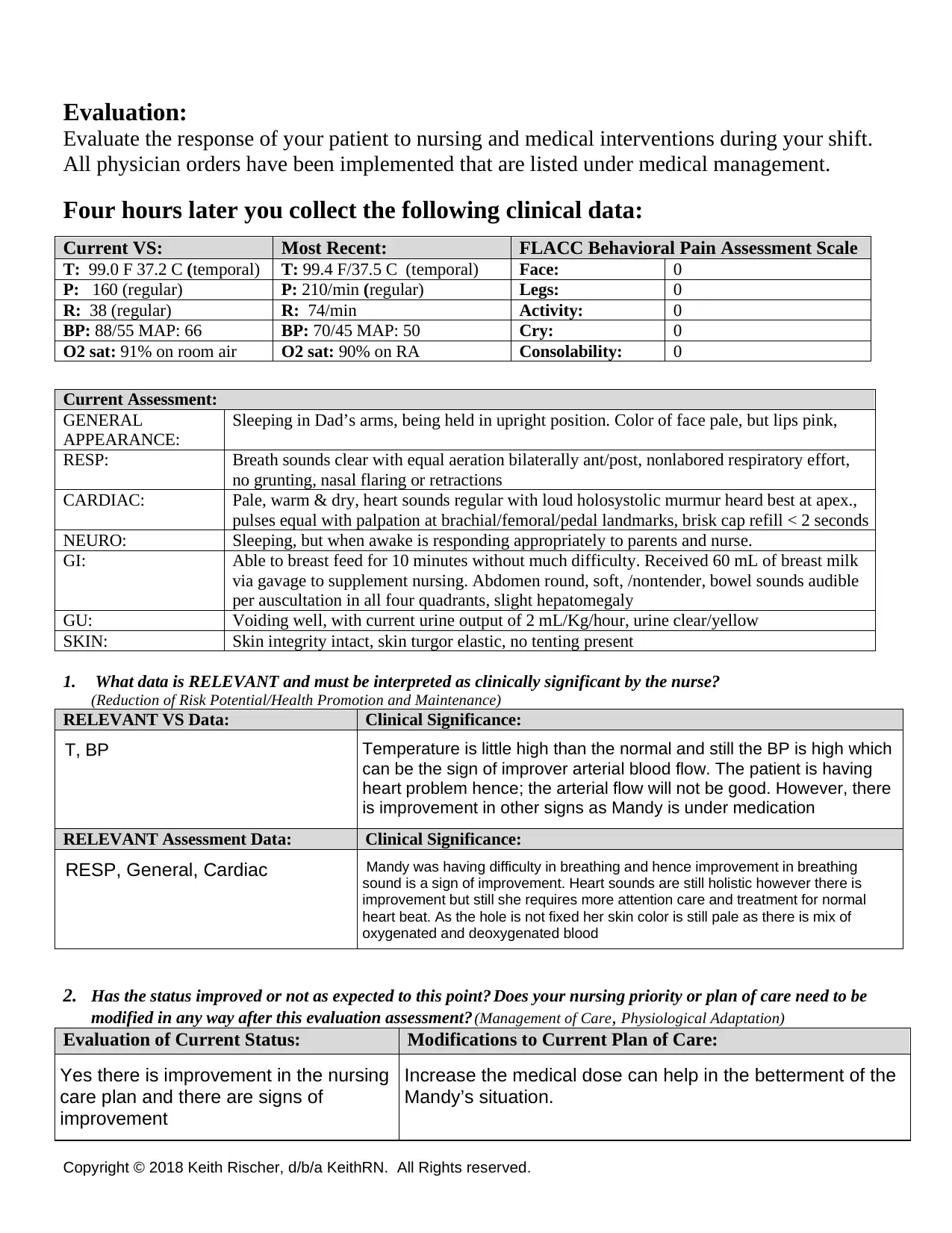
Evaluation:
Evaluate the response of your patient to nursing and medical interventions during your shift.
All physician orders have been implemented that are listed under medical management.
Four hours later you collect the following clinical data:
1. What data is RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential/Health Promotion and Maintenance)
RELEVANT VS Data: Clinical Significance:
RELEVANT Assessment Data: Clinical Significance:
2. Has the status improved or not as expected to this point? Does your nursing priority or plan of care need to be
modified in any way after this evaluation assessment? (Management of Care, Physiological Adaptation)
Evaluation of Current Status: Modifications to Current Plan of Care:
Current VS: Most Recent: FLACC Behavioral Pain Assessment Scale
T: 99.0 F 37.2 C (temporal) T: 99.4 F/37.5 C (temporal) Face: 0
P: 160 (regular) P: 210/min (regular) Legs: 0
R: 38 (regular) R: 74/min Activity: 0
BP: 88/55 MAP: 66 BP: 70/45 MAP: 50 Cry: 0
O2 sat: 91% on room air O2 sat: 90% on RA Consolability: 0
Current Assessment:
GENERAL
APPEARANCE:
Sleeping in Dad’s arms, being held in upright position. Color of face pale, but lips pink,
RESP: Breath sounds clear with equal aeration bilaterally ant/post, nonlabored respiratory effort,
no grunting, nasal flaring or retractions
CARDIAC: Pale, warm & dry, heart sounds regular with loud holosystolic murmur heard best at apex.,
pulses equal with palpation at brachial/femoral/pedal landmarks, brisk cap refill < 2 seconds
NEURO: Sleeping, but when awake is responding appropriately to parents and nurse.
GI: Able to breast feed for 10 minutes without much difficulty. Received 60 mL of breast milk
via gavage to supplement nursing. Abdomen round, soft, /nontender, bowel sounds audible
per auscultation in all four quadrants, slight hepatomegaly
GU: Voiding well, with current urine output of 2 mL/Kg/hour, urine clear/yellow
SKIN: Skin integrity intact, skin turgor elastic, no tenting present
T, BP Temperature is little high than the normal and still the BP is high which
can be the sign of improver arterial blood flow. The patient is having
heart problem hence; the arterial flow will not be good. However, there
is improvement in other signs as Mandy is under medication
RESP, General, Cardiac Mandy was having difficulty in breathing and hence improvement in breathing
sound is a sign of improvement. Heart sounds are still holistic however there is
improvement but still she requires more attention care and treatment for normal
heart beat. As the hole is not fixed her skin color is still pale as there is mix of
oxygenated and deoxygenated blood
Yes there is improvement in the nursing
care plan and there are signs of
improvement
Increase the medical dose can help in the betterment of the
Mandy’s situation.
Evaluation:
Evaluate the response of your patient to nursing and medical interventions during your shift.
All physician orders have been implemented that are listed under medical management.
Four hours later you collect the following clinical data:
1. What data is RELEVANT and must be interpreted as clinically significant by the nurse?
(Reduction of Risk Potential/Health Promotion and Maintenance)
RELEVANT VS Data: Clinical Significance:
RELEVANT Assessment Data: Clinical Significance:
2. Has the status improved or not as expected to this point? Does your nursing priority or plan of care need to be
modified in any way after this evaluation assessment? (Management of Care, Physiological Adaptation)
Evaluation of Current Status: Modifications to Current Plan of Care:
Current VS: Most Recent: FLACC Behavioral Pain Assessment Scale
T: 99.0 F 37.2 C (temporal) T: 99.4 F/37.5 C (temporal) Face: 0
P: 160 (regular) P: 210/min (regular) Legs: 0
R: 38 (regular) R: 74/min Activity: 0
BP: 88/55 MAP: 66 BP: 70/45 MAP: 50 Cry: 0
O2 sat: 91% on room air O2 sat: 90% on RA Consolability: 0
Current Assessment:
GENERAL
APPEARANCE:
Sleeping in Dad’s arms, being held in upright position. Color of face pale, but lips pink,
RESP: Breath sounds clear with equal aeration bilaterally ant/post, nonlabored respiratory effort,
no grunting, nasal flaring or retractions
CARDIAC: Pale, warm & dry, heart sounds regular with loud holosystolic murmur heard best at apex.,
pulses equal with palpation at brachial/femoral/pedal landmarks, brisk cap refill < 2 seconds
NEURO: Sleeping, but when awake is responding appropriately to parents and nurse.
GI: Able to breast feed for 10 minutes without much difficulty. Received 60 mL of breast milk
via gavage to supplement nursing. Abdomen round, soft, /nontender, bowel sounds audible
per auscultation in all four quadrants, slight hepatomegaly
GU: Voiding well, with current urine output of 2 mL/Kg/hour, urine clear/yellow
SKIN: Skin integrity intact, skin turgor elastic, no tenting present
T, BP Temperature is little high than the normal and still the BP is high which
can be the sign of improver arterial blood flow. The patient is having
heart problem hence; the arterial flow will not be good. However, there
is improvement in other signs as Mandy is under medication
RESP, General, Cardiac Mandy was having difficulty in breathing and hence improvement in breathing
sound is a sign of improvement. Heart sounds are still holistic however there is
improvement but still she requires more attention care and treatment for normal
heart beat. As the hole is not fixed her skin color is still pale as there is mix of
oxygenated and deoxygenated blood
Yes there is improvement in the nursing
care plan and there are signs of
improvement
Increase the medical dose can help in the betterment of the
Mandy’s situation.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
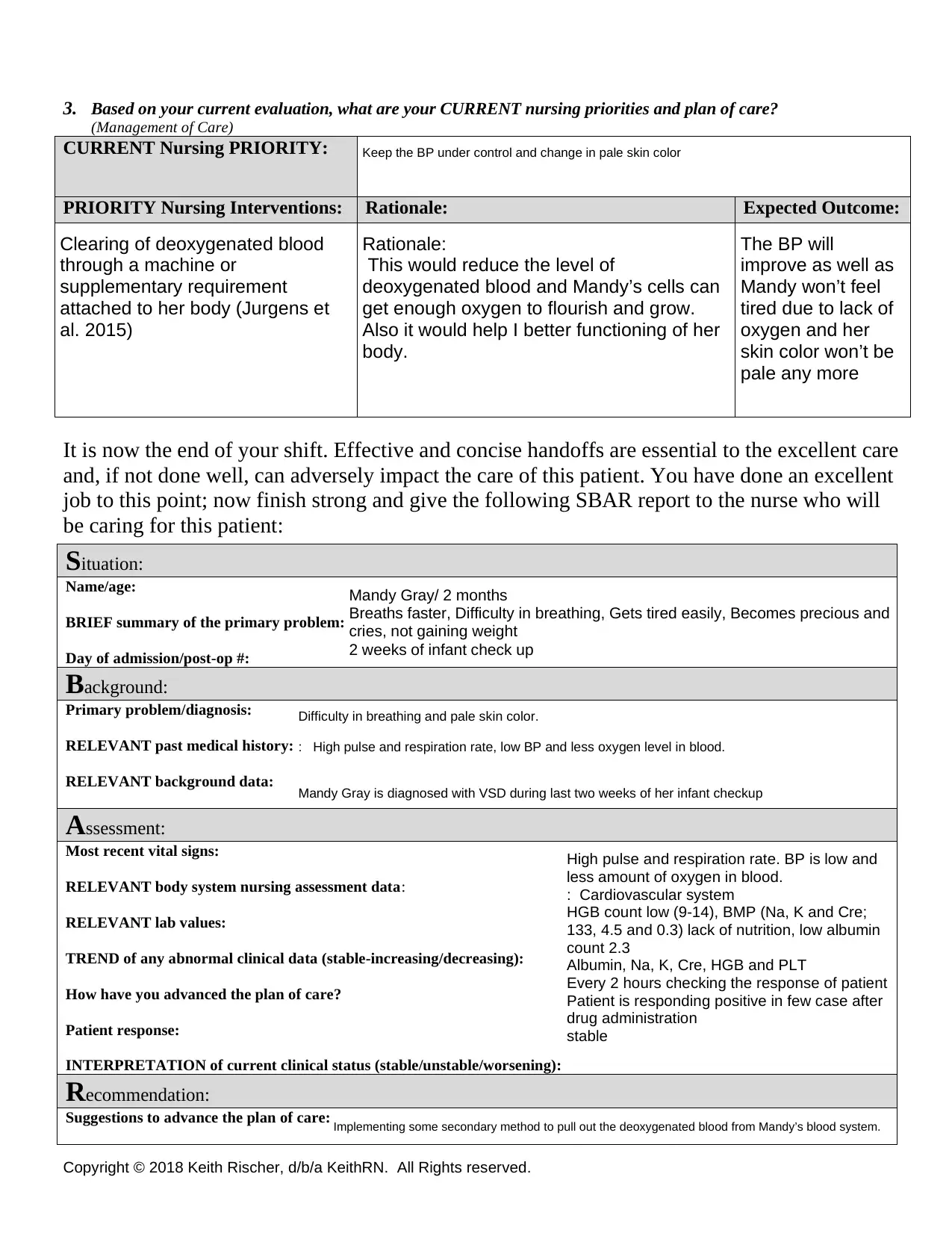
3. Based on your current evaluation, what are your CURRENT nursing priorities and plan of care?
(Management of Care)
CURRENT Nursing PRIORITY:
PRIORITY Nursing Interventions: Rationale: Expected Outcome:
It is now the end of your shift. Effective and concise handoffs are essential to the excellent care
and, if not done well, can adversely impact the care of this patient. You have done an excellent
job to this point; now finish strong and give the following SBAR report to the nurse who will
be caring for this patient:
Situation:
Name/age:
BRIEF summary of the primary problem:
Day of admission/post-op #:
Background:
Primary problem/diagnosis:
RELEVANT past medical history:
RELEVANT background data:
Assessment:
Most recent vital signs:
RELEVANT body system nursing assessment data:
RELEVANT lab values:
TREND of any abnormal clinical data (stable-increasing/decreasing):
How have you advanced the plan of care?
Patient response:
INTERPRETATION of current clinical status (stable/unstable/worsening):
Recommendation:
Suggestions to advance the plan of care:
Keep the BP under control and change in pale skin color
Clearing of deoxygenated blood
through a machine or
supplementary requirement
attached to her body (Jurgens et
al. 2015)
Rationale:
This would reduce the level of
deoxygenated blood and Mandy’s cells can
get enough oxygen to flourish and grow.
Also it would help I better functioning of her
body.
The BP will
improve as well as
Mandy won’t feel
tired due to lack of
oxygen and her
skin color won’t be
pale any more
Mandy Gray/ 2 months
Breaths faster, Difficulty in breathing, Gets tired easily, Becomes precious and
cries, not gaining weight
2 weeks of infant check up
Difficulty in breathing and pale skin color.
: High pulse and respiration rate, low BP and less oxygen level in blood.
Mandy Gray is diagnosed with VSD during last two weeks of her infant checkup
High pulse and respiration rate. BP is low and
less amount of oxygen in blood.
: Cardiovascular system
HGB count low (9-14), BMP (Na, K and Cre;
133, 4.5 and 0.3) lack of nutrition, low albumin
count 2.3
Albumin, Na, K, Cre, HGB and PLT
Every 2 hours checking the response of patient
Patient is responding positive in few case after
drug administration
stable
Implementing some secondary method to pull out the deoxygenated blood from Mandy’s blood system.
3. Based on your current evaluation, what are your CURRENT nursing priorities and plan of care?
(Management of Care)
CURRENT Nursing PRIORITY:
PRIORITY Nursing Interventions: Rationale: Expected Outcome:
It is now the end of your shift. Effective and concise handoffs are essential to the excellent care
and, if not done well, can adversely impact the care of this patient. You have done an excellent
job to this point; now finish strong and give the following SBAR report to the nurse who will
be caring for this patient:
Situation:
Name/age:
BRIEF summary of the primary problem:
Day of admission/post-op #:
Background:
Primary problem/diagnosis:
RELEVANT past medical history:
RELEVANT background data:
Assessment:
Most recent vital signs:
RELEVANT body system nursing assessment data:
RELEVANT lab values:
TREND of any abnormal clinical data (stable-increasing/decreasing):
How have you advanced the plan of care?
Patient response:
INTERPRETATION of current clinical status (stable/unstable/worsening):
Recommendation:
Suggestions to advance the plan of care:
Keep the BP under control and change in pale skin color
Clearing of deoxygenated blood
through a machine or
supplementary requirement
attached to her body (Jurgens et
al. 2015)
Rationale:
This would reduce the level of
deoxygenated blood and Mandy’s cells can
get enough oxygen to flourish and grow.
Also it would help I better functioning of her
body.
The BP will
improve as well as
Mandy won’t feel
tired due to lack of
oxygen and her
skin color won’t be
pale any more
Mandy Gray/ 2 months
Breaths faster, Difficulty in breathing, Gets tired easily, Becomes precious and
cries, not gaining weight
2 weeks of infant check up
Difficulty in breathing and pale skin color.
: High pulse and respiration rate, low BP and less oxygen level in blood.
Mandy Gray is diagnosed with VSD during last two weeks of her infant checkup
High pulse and respiration rate. BP is low and
less amount of oxygen in blood.
: Cardiovascular system
HGB count low (9-14), BMP (Na, K and Cre;
133, 4.5 and 0.3) lack of nutrition, low albumin
count 2.3
Albumin, Na, K, Cre, HGB and PLT
Every 2 hours checking the response of patient
Patient is responding positive in few case after
drug administration
stable
Implementing some secondary method to pull out the deoxygenated blood from Mandy’s blood system.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Copyright © 2018 Keith Rischer, d/b/a KeithRN. All Rights reserved.
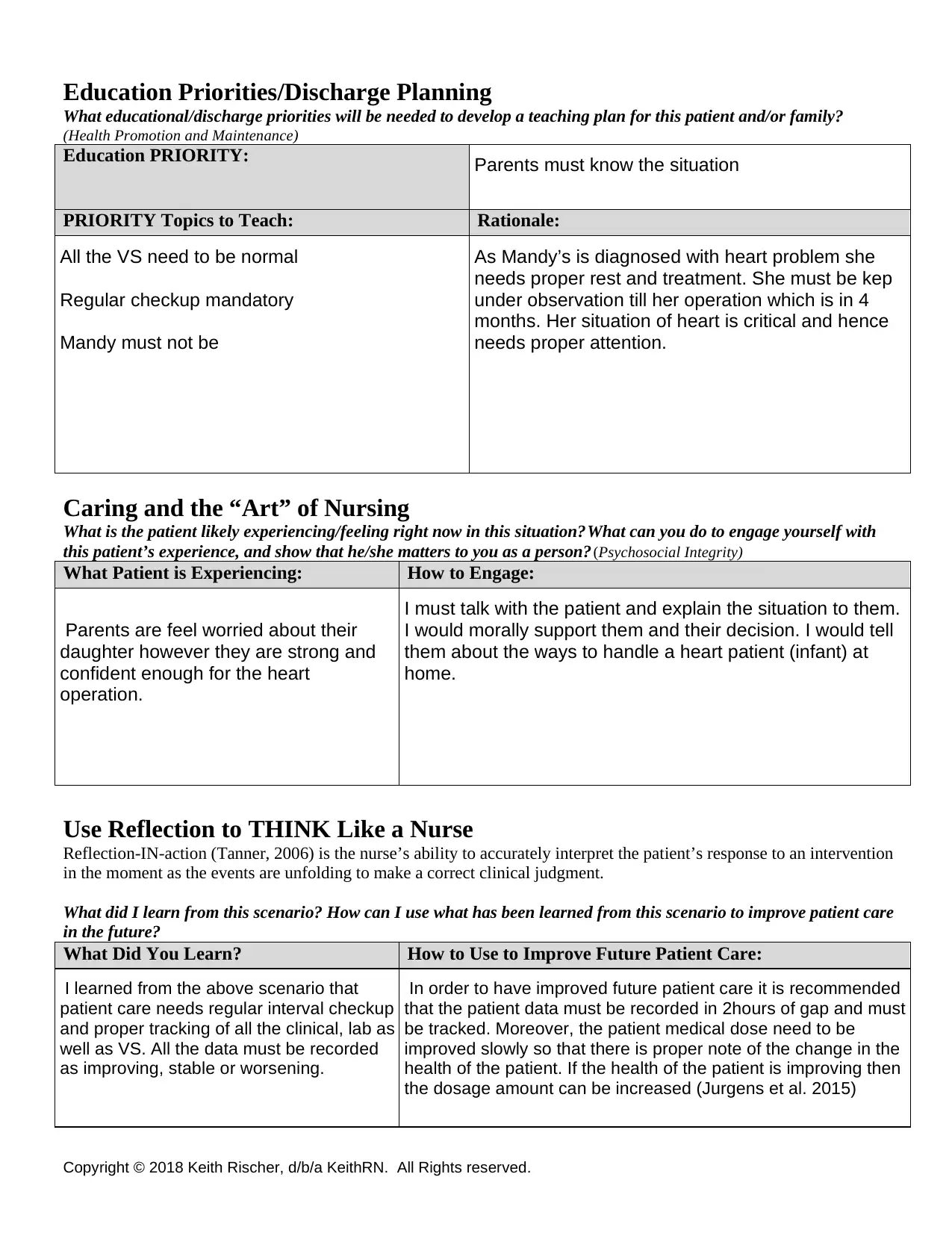
Education Priorities/Discharge Planning
What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family?
(Health Promotion and Maintenance)
Education PRIORITY:
PRIORITY Topics to Teach: Rationale:
Caring and the “Art” of Nursing
What is the patient likely experiencing/feeling right now in this situation? What can you do to engage yourself with
this patient’s experience, and show that he/she matters to you as a person? (Psychosocial Integrity)
What Patient is Experiencing: How to Engage:
Use Reflection to THINK Like a Nurse
Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention
in the moment as the events are unfolding to make a correct clinical judgment.
What did I learn from this scenario? How can I use what has been learned from this scenario to improve patient care
in the future?
What Did You Learn? How to Use to Improve Future Patient Care:
Parents must know the situation
All the VS need to be normal
Regular checkup mandatory
Mandy must not be
As Mandy’s is diagnosed with heart problem she
needs proper rest and treatment. She must be kep
under observation till her operation which is in 4
months. Her situation of heart is critical and hence
needs proper attention.
Parents are feel worried about their
daughter however they are strong and
confident enough for the heart
operation.
I must talk with the patient and explain the situation to them.
I would morally support them and their decision. I would tell
them about the ways to handle a heart patient (infant) at
home.
I learned from the above scenario that
patient care needs regular interval checkup
and proper tracking of all the clinical, lab as
well as VS. All the data must be recorded
as improving, stable or worsening.
In order to have improved future patient care it is recommended
that the patient data must be recorded in 2hours of gap and must
be tracked. Moreover, the patient medical dose need to be
improved slowly so that there is proper note of the change in the
health of the patient. If the health of the patient is improving then
the dosage amount can be increased (Jurgens et al. 2015)
Education Priorities/Discharge Planning
What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family?
(Health Promotion and Maintenance)
Education PRIORITY:
PRIORITY Topics to Teach: Rationale:
Caring and the “Art” of Nursing
What is the patient likely experiencing/feeling right now in this situation? What can you do to engage yourself with
this patient’s experience, and show that he/she matters to you as a person? (Psychosocial Integrity)
What Patient is Experiencing: How to Engage:
Use Reflection to THINK Like a Nurse
Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention
in the moment as the events are unfolding to make a correct clinical judgment.
What did I learn from this scenario? How can I use what has been learned from this scenario to improve patient care
in the future?
What Did You Learn? How to Use to Improve Future Patient Care:
Parents must know the situation
All the VS need to be normal
Regular checkup mandatory
Mandy must not be
As Mandy’s is diagnosed with heart problem she
needs proper rest and treatment. She must be kep
under observation till her operation which is in 4
months. Her situation of heart is critical and hence
needs proper attention.
Parents are feel worried about their
daughter however they are strong and
confident enough for the heart
operation.
I must talk with the patient and explain the situation to them.
I would morally support them and their decision. I would tell
them about the ways to handle a heart patient (infant) at
home.
I learned from the above scenario that
patient care needs regular interval checkup
and proper tracking of all the clinical, lab as
well as VS. All the data must be recorded
as improving, stable or worsening.
In order to have improved future patient care it is recommended
that the patient data must be recorded in 2hours of gap and must
be tracked. Moreover, the patient medical dose need to be
improved slowly so that there is proper note of the change in the
health of the patient. If the health of the patient is improving then
the dosage amount can be increased (Jurgens et al. 2015)
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

