Urinary Incontinence: Diagnosis, Treatment, and Lifestyle Changes
VerifiedAdded on 2023/04/24
|14
|1517
|449
Report
AI Summary
This report provides a comprehensive overview of urinary incontinence, a common health concern significantly affecting quality of life. It defines urinary incontinence and explores its various types, including stress, urge, functional, overflow, and mixed incontinence. The report details the signs and symptoms, such as leakage and sudden urges, along with the causes, including bladder neck mobility issues and overactive bladder disorders. It outlines diagnostic tests like medical history review, dipstick tests, and urodynamic tests. Treatment options discussed include medications like anticholinergics and neuromodulation, as well as surgical procedures such as periurethral injections and the Burch procedure. Lifestyle changes like pelvic floor exercises, PTNS, and the use of continence devices are also addressed. The report concludes by emphasizing the importance of reliable treatment procedures and accurate diagnosis for effective management of urinary incontinence, especially in women.
Urinary
Incontinenc
e
Student’s Name
Student Number
Incontinenc
e
Student’s Name
Student Number
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Topic Overview
Urinary incontinence is a common major health and
quality of life concern.
Urinary incontinence at unacceptable times also causes
social embarrassment which makes it a sensitive topic to
discuss.
Urinary incontinence is more common in females than in
males.
It significantly effects on a person’s family from an
economic, emotional, and interpersonal standpoint (Rizvi
& Ather, 2017).
Treatment depends on several factors, such as the type of
incontinence, the patient's age, general health, and their
mental state.
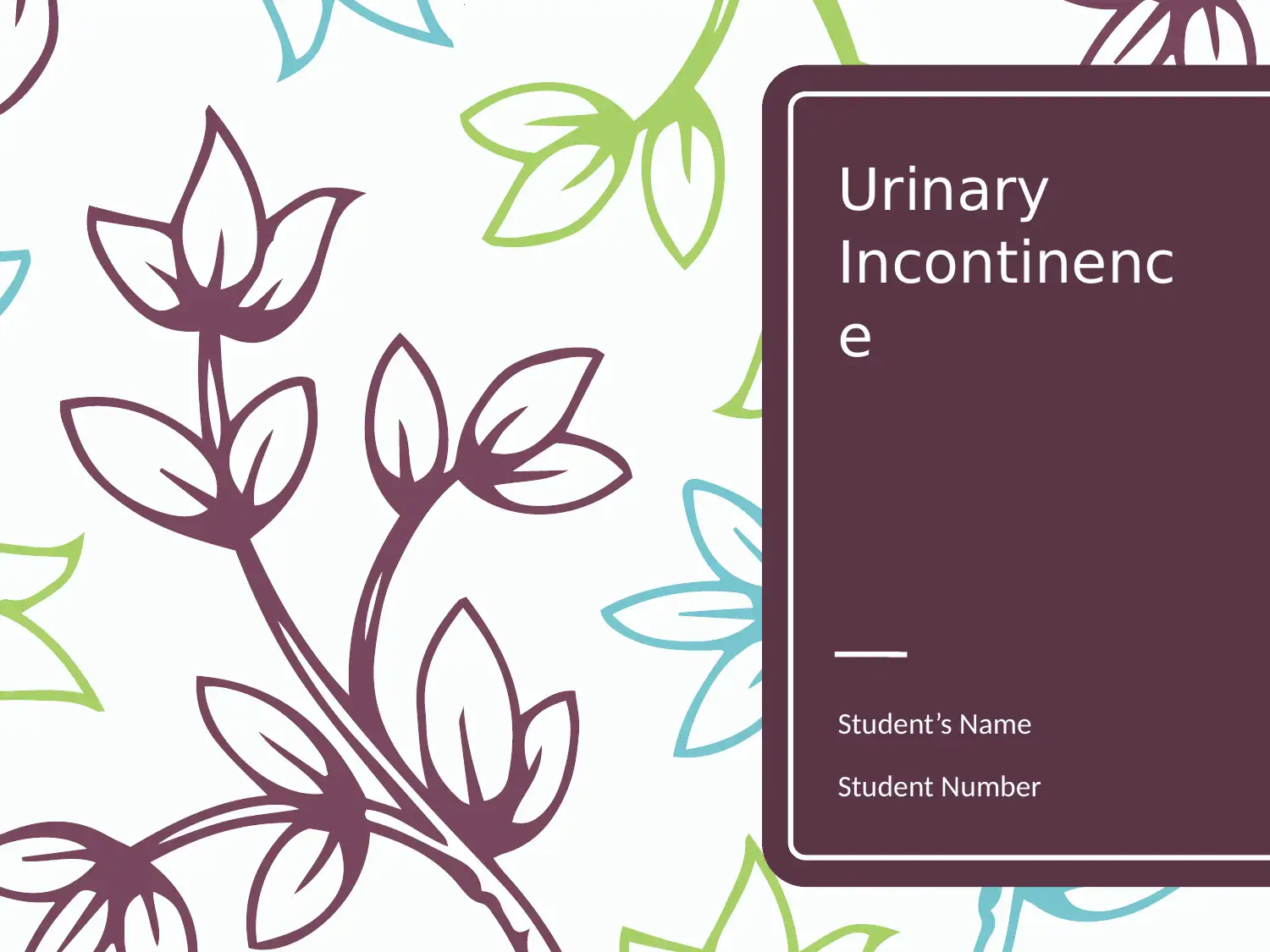
Source: What is Urinary Incontinence? Retrieve from
-
https://www.urologyhealth.org/urologic-conditions/urinary-
Urinary incontinence is a common major health and
quality of life concern.
Urinary incontinence at unacceptable times also causes
social embarrassment which makes it a sensitive topic to
discuss.
Urinary incontinence is more common in females than in
males.
It significantly effects on a person’s family from an
economic, emotional, and interpersonal standpoint (Rizvi
& Ather, 2017).
Treatment depends on several factors, such as the type of
incontinence, the patient's age, general health, and their
mental state.
Source: What is Urinary Incontinence? Retrieve from
-
https://www.urologyhealth.org/urologic-conditions/urinary-
Definition
Urinary incontinence is defined as
involuntary loss or leakage of urine
that cannot be controlled by the
bladder.
Control over the urinary sphincter
is either lost or weakened
Incontinence is not a disease. It is
inability to control the bladder due
to various reasons.
Source: Urinary Incontinence Treatment.
Retrieve from -
https://www.pushya.org/urinary-
incontinence-treatment-ahmedabad.php
Urinary incontinence is defined as
involuntary loss or leakage of urine
that cannot be controlled by the
bladder.
Control over the urinary sphincter
is either lost or weakened
Incontinence is not a disease. It is
inability to control the bladder due
to various reasons.
Source: Urinary Incontinence Treatment.
Retrieve from -
https://www.pushya.org/urinary-
incontinence-treatment-ahmedabad.php
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Types of Urinary Incontinence
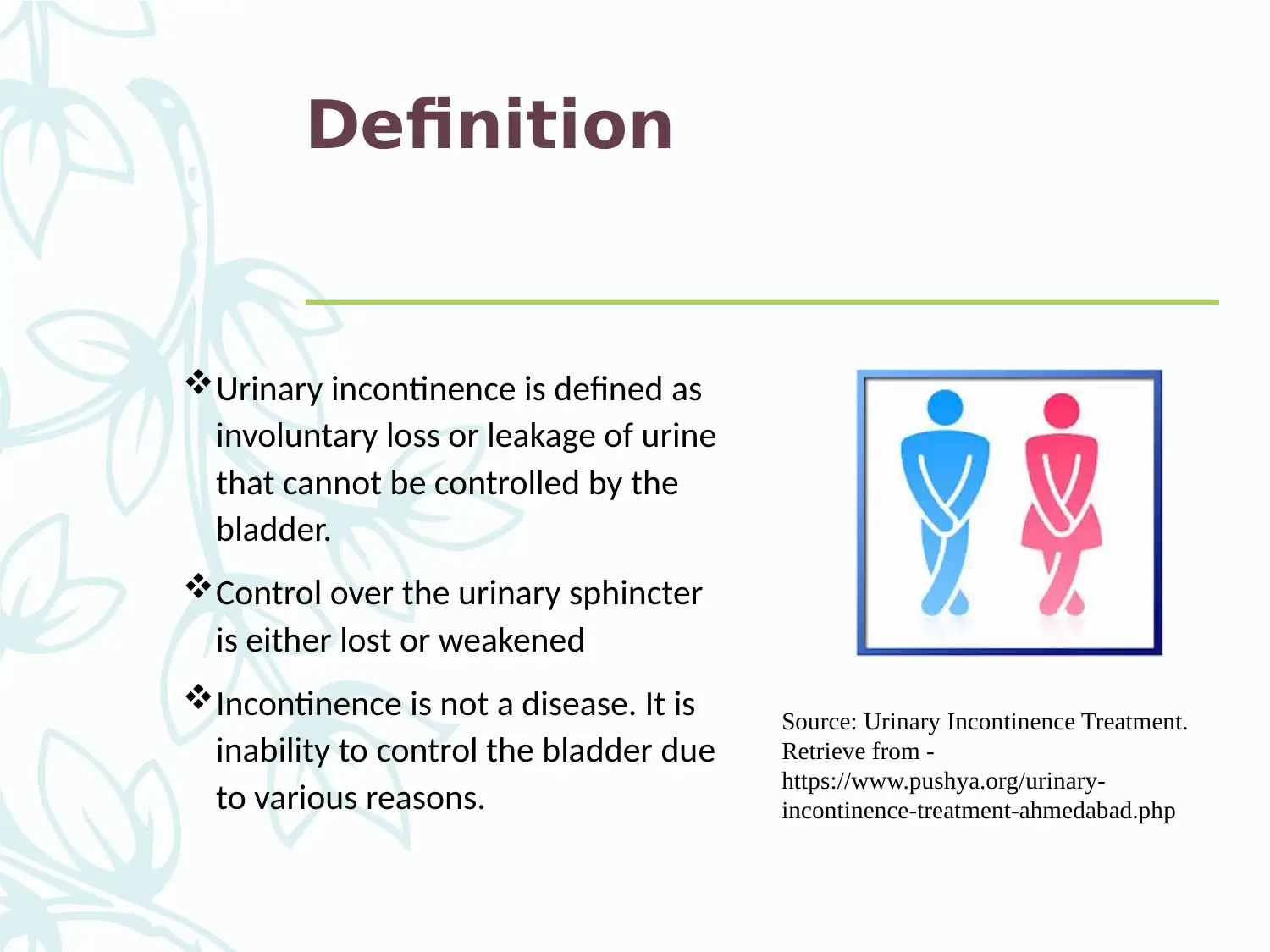
Stress incontinence (Milsom &
Gyhagen, 2018). Is the most
common type of inconsistency.
Urge Incontinence
Functional Incontinence
Overflow Incontinence
Mixed Incontinence
Source: Types of Urinary Incontinence retrieved
from https://www.lhsc.on.ca/women-s-health/types-
of-urinary-incontinence
Stress incontinence (Milsom &
Gyhagen, 2018). Is the most
common type of inconsistency.
Urge Incontinence
Functional Incontinence
Overflow Incontinence
Mixed Incontinence
Source: Types of Urinary Incontinence retrieved
from https://www.lhsc.on.ca/women-s-health/types-
of-urinary-incontinence
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
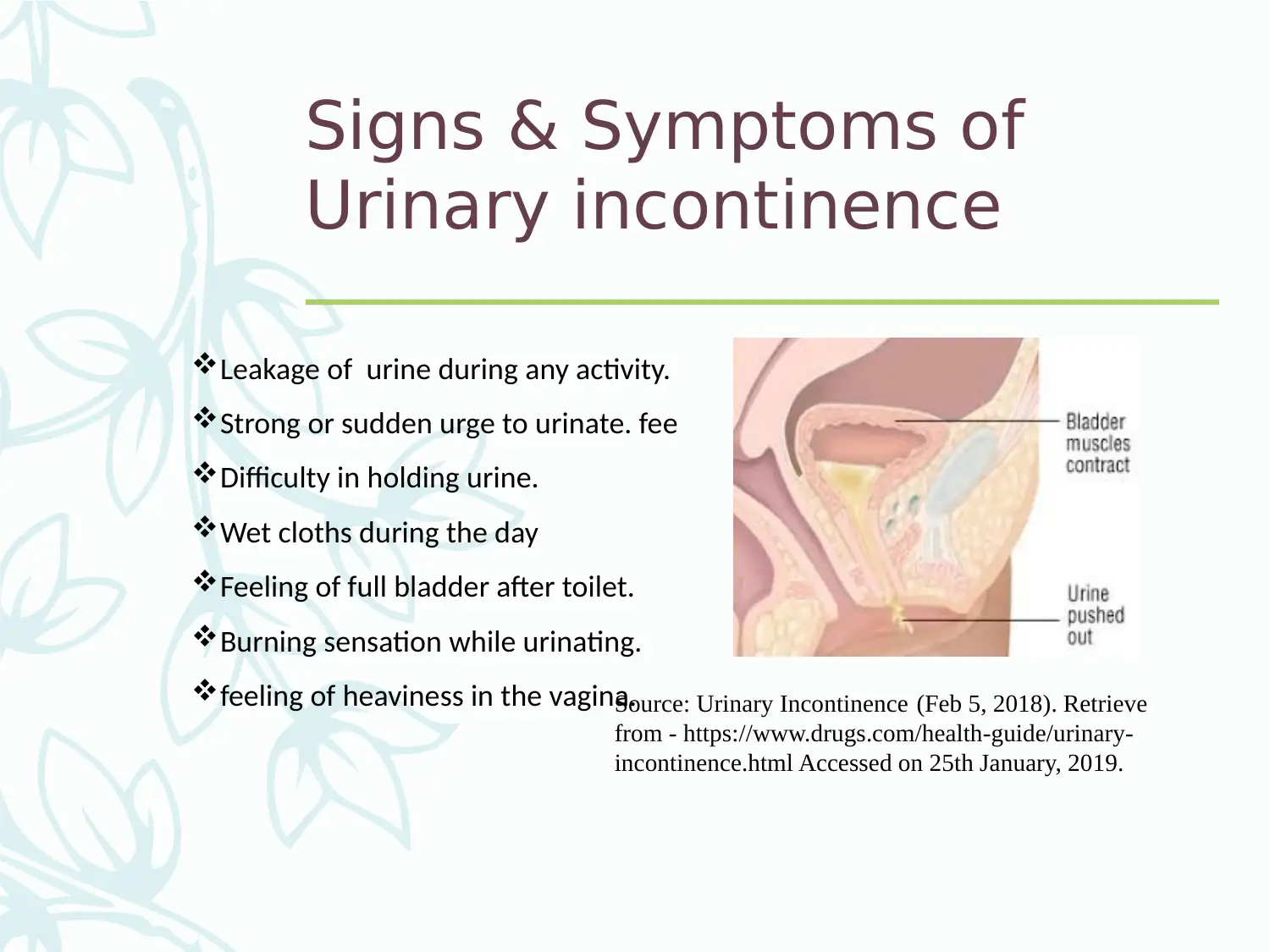
Signs & Symptoms of
Urinary incontinence
Leakage of urine during any activity.
Strong or sudden urge to urinate. fee
Difficulty in holding urine.
Wet cloths during the day
Feeling of full bladder after toilet.
Burning sensation while urinating.
feeling of heaviness in the vagina.Source: Urinary Incontinence (Feb 5, 2018). Retrieve
from - https://www.drugs.com/health-guide/urinary-
incontinence.html Accessed on 25th January, 2019.
Urinary incontinence
Leakage of urine during any activity.
Strong or sudden urge to urinate. fee
Difficulty in holding urine.
Wet cloths during the day
Feeling of full bladder after toilet.
Burning sensation while urinating.
feeling of heaviness in the vagina.Source: Urinary Incontinence (Feb 5, 2018). Retrieve
from - https://www.drugs.com/health-guide/urinary-
incontinence.html Accessed on 25th January, 2019.
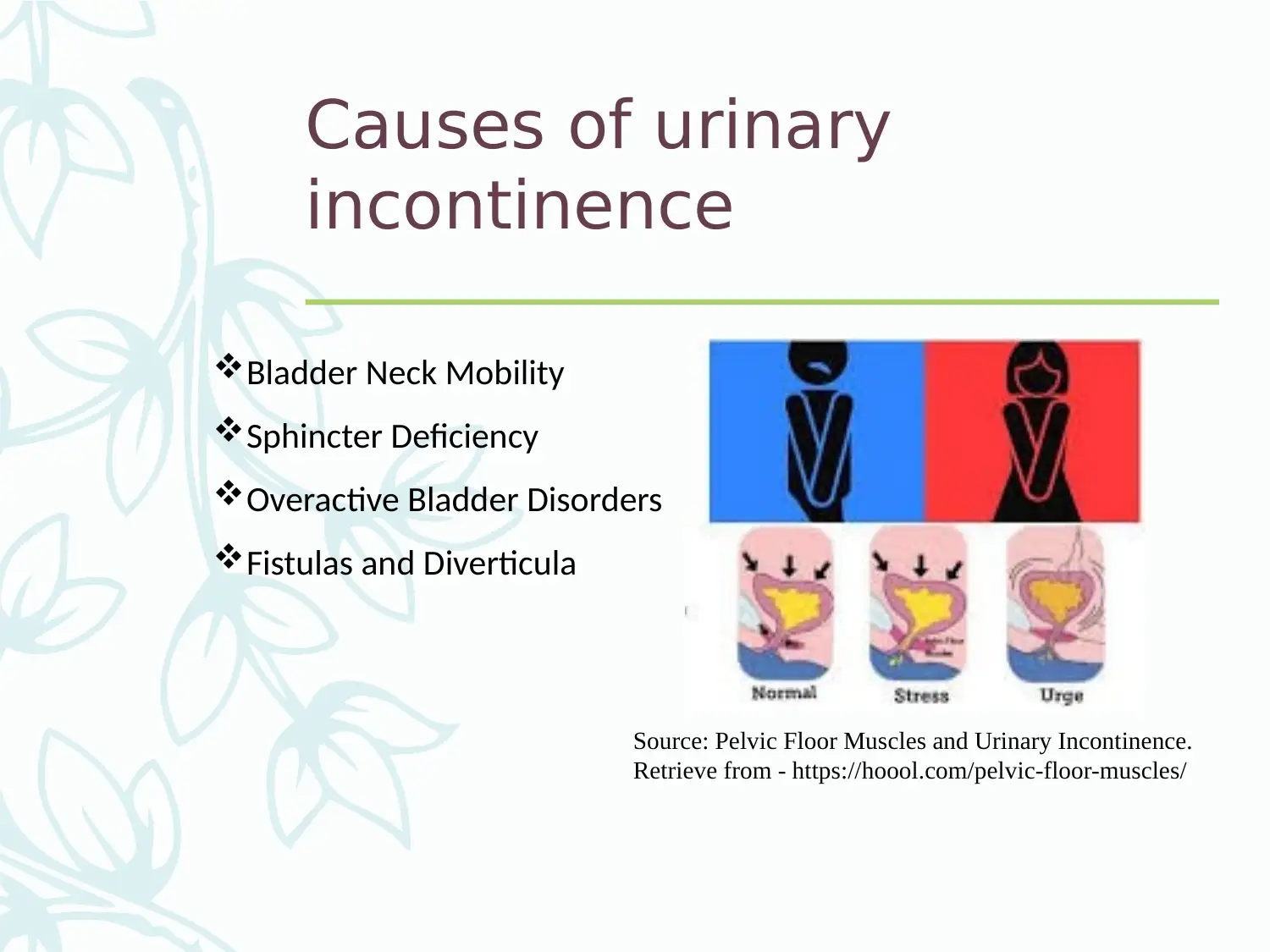
Causes of urinary
incontinence
Bladder Neck Mobility
Sphincter Deficiency
Overactive Bladder Disorders
Fistulas and Diverticula
Source: Pelvic Floor Muscles and Urinary Incontinence.
Retrieve from - https://hoool.com/pelvic-floor-muscles/
incontinence
Bladder Neck Mobility
Sphincter Deficiency
Overactive Bladder Disorders
Fistulas and Diverticula
Source: Pelvic Floor Muscles and Urinary Incontinence.
Retrieve from - https://hoool.com/pelvic-floor-muscles/
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
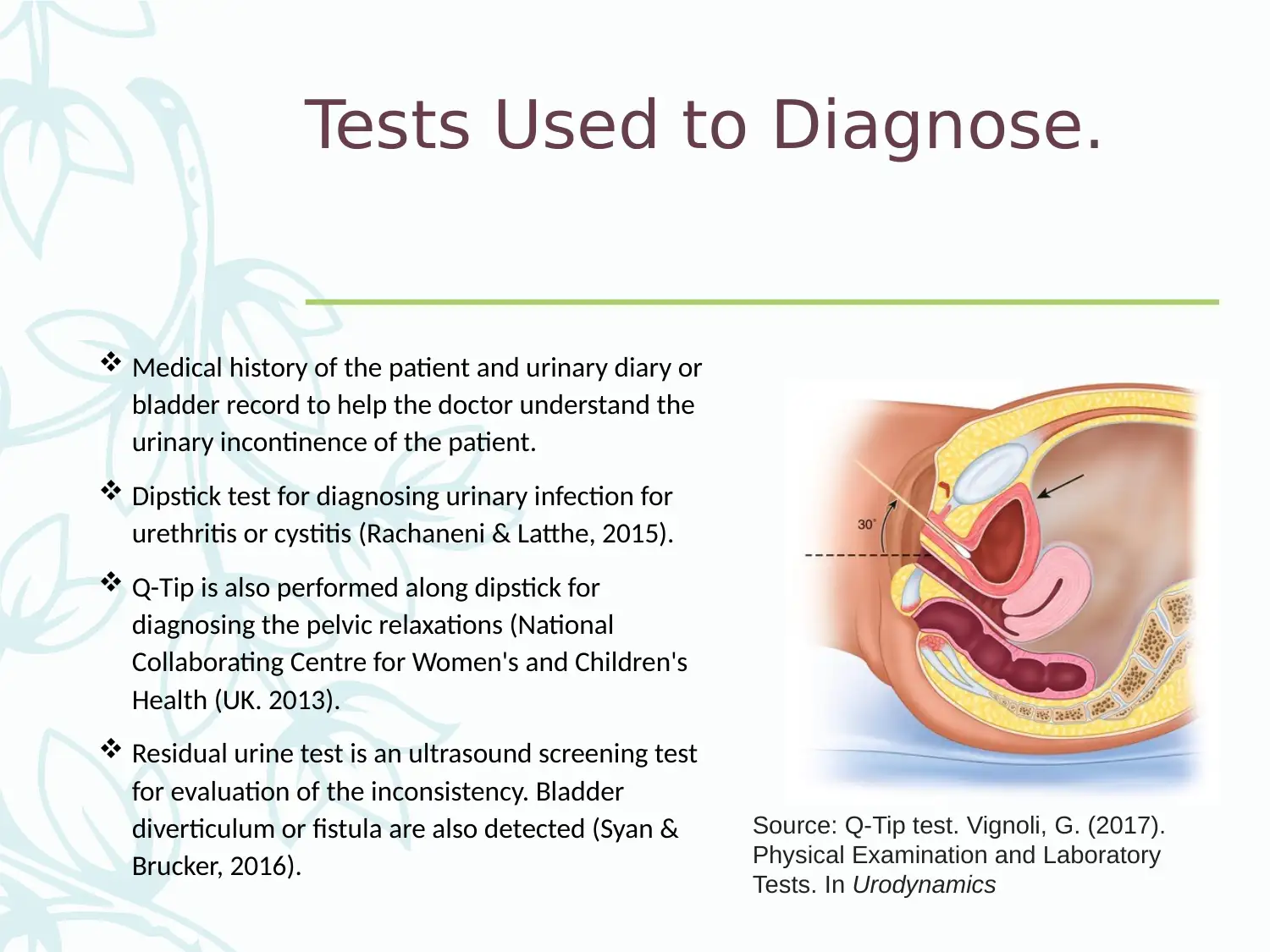
Tests Used to Diagnose.
Medical history of the patient and urinary diary or
bladder record to help the doctor understand the
urinary incontinence of the patient.
Dipstick test for diagnosing urinary infection for
urethritis or cystitis (Rachaneni & Latthe, 2015).
Q-Tip is also performed along dipstick for
diagnosing the pelvic relaxations (National
Collaborating Centre for Women's and Children's
Health (UK. 2013).
Residual urine test is an ultrasound screening test
for evaluation of the inconsistency. Bladder
diverticulum or fistula are also detected (Syan &
Brucker, 2016).
Source: Q-Tip test. Vignoli, G. (2017).
Physical Examination and Laboratory
Tests. In Urodynamics
Medical history of the patient and urinary diary or
bladder record to help the doctor understand the
urinary incontinence of the patient.
Dipstick test for diagnosing urinary infection for
urethritis or cystitis (Rachaneni & Latthe, 2015).
Q-Tip is also performed along dipstick for
diagnosing the pelvic relaxations (National
Collaborating Centre for Women's and Children's
Health (UK. 2013).
Residual urine test is an ultrasound screening test
for evaluation of the inconsistency. Bladder
diverticulum or fistula are also detected (Syan &
Brucker, 2016).
Source: Q-Tip test. Vignoli, G. (2017).
Physical Examination and Laboratory
Tests. In Urodynamics
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
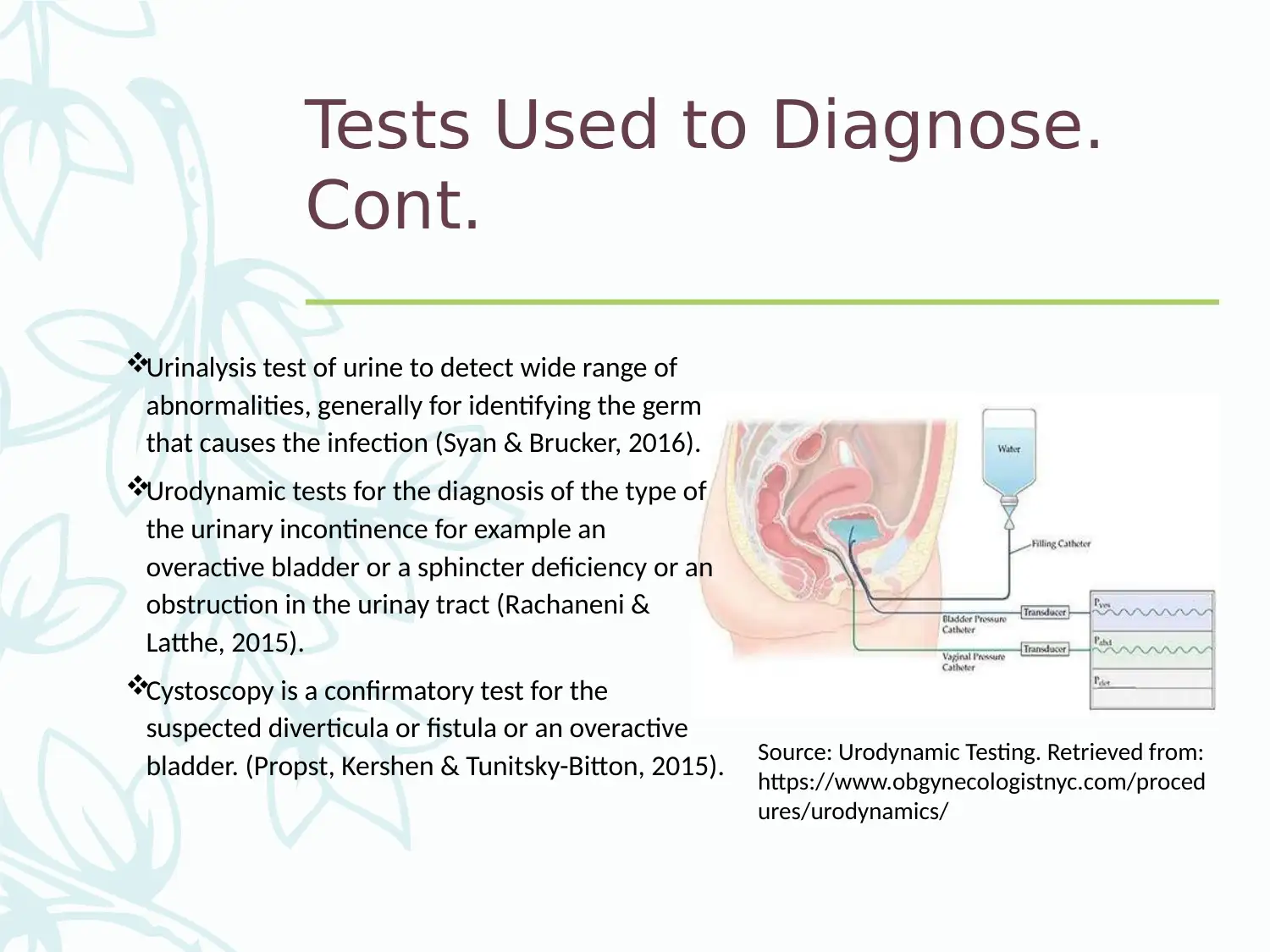
Tests Used to Diagnose.
Cont.
Urinalysis test of urine to detect wide range of
abnormalities, generally for identifying the germ
that causes the infection (Syan & Brucker, 2016).
Urodynamic tests for the diagnosis of the type of
the urinary incontinence for example an
overactive bladder or a sphincter deficiency or an
obstruction in the urinay tract (Rachaneni &
Latthe, 2015).
Cystoscopy is a confirmatory test for the
suspected diverticula or fistula or an overactive
bladder. (Propst, Kershen & Tunitsky-Bitton, 2015). Source: Urodynamic Testing. Retrieved from:
https://www.obgynecologistnyc.com/proced
ures/urodynamics/
Cont.
Urinalysis test of urine to detect wide range of
abnormalities, generally for identifying the germ
that causes the infection (Syan & Brucker, 2016).
Urodynamic tests for the diagnosis of the type of
the urinary incontinence for example an
overactive bladder or a sphincter deficiency or an
obstruction in the urinay tract (Rachaneni &
Latthe, 2015).
Cystoscopy is a confirmatory test for the
suspected diverticula or fistula or an overactive
bladder. (Propst, Kershen & Tunitsky-Bitton, 2015). Source: Urodynamic Testing. Retrieved from:
https://www.obgynecologistnyc.com/proced
ures/urodynamics/
Treatment or Management
Options/Medications for topic
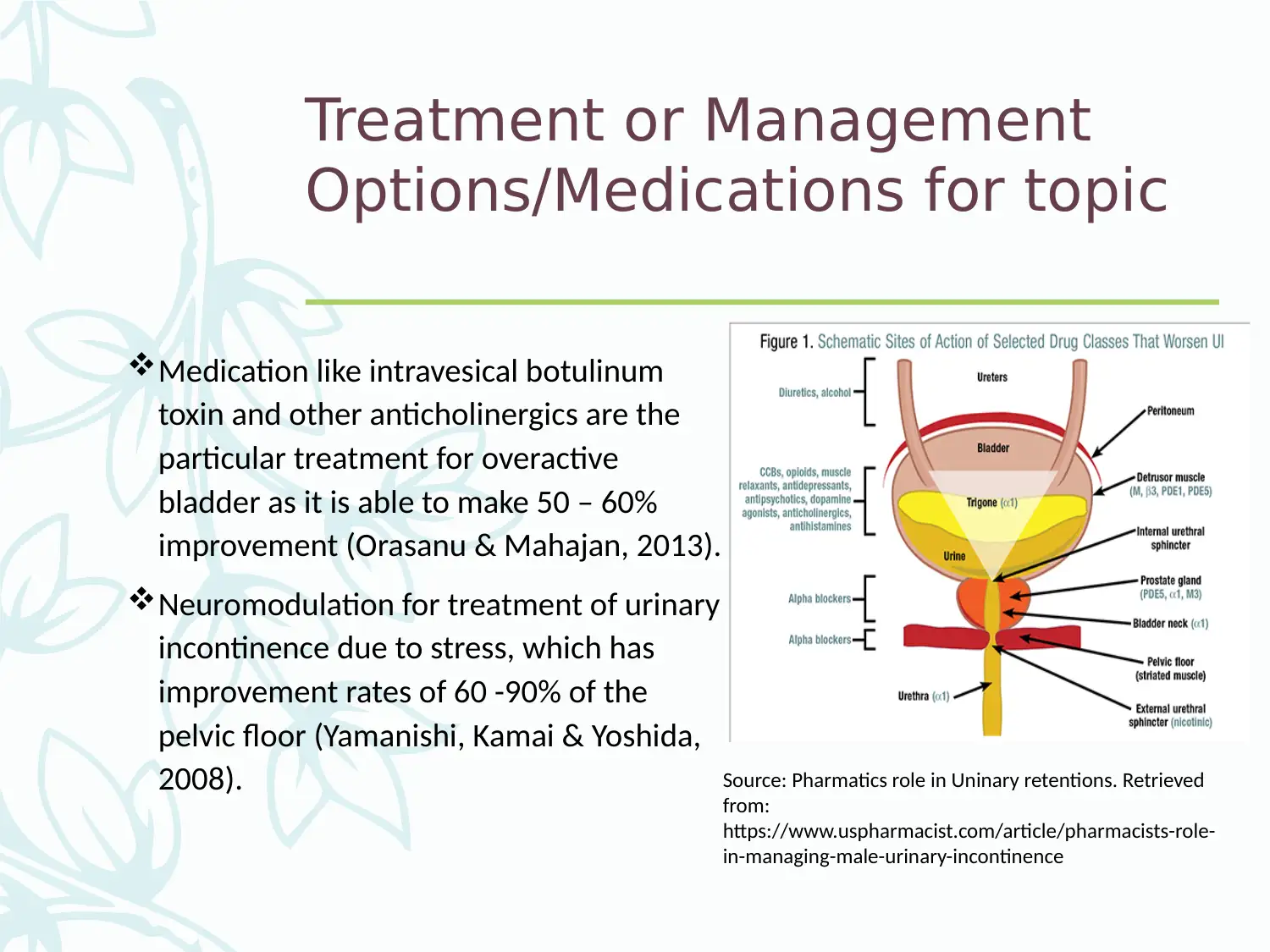
Medication like intravesical botulinum
toxin and other anticholinergics are the
particular treatment for overactive
bladder as it is able to make 50 – 60%
improvement (Orasanu & Mahajan, 2013).
Neuromodulation for treatment of urinary
incontinence due to stress, which has
improvement rates of 60 -90% of the
pelvic floor (Yamanishi, Kamai & Yoshida,
2008). Source: Pharmatics role in Uninary retentions. Retrieved
from:
https://www.uspharmacist.com/article/pharmacists-role-
in-managing-male-urinary-incontinence
Options/Medications for topic
Medication like intravesical botulinum
toxin and other anticholinergics are the
particular treatment for overactive
bladder as it is able to make 50 – 60%
improvement (Orasanu & Mahajan, 2013).
Neuromodulation for treatment of urinary
incontinence due to stress, which has
improvement rates of 60 -90% of the
pelvic floor (Yamanishi, Kamai & Yoshida,
2008). Source: Pharmatics role in Uninary retentions. Retrieved
from:
https://www.uspharmacist.com/article/pharmacists-role-
in-managing-male-urinary-incontinence
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Treatment or Management
Options/Medications for topic
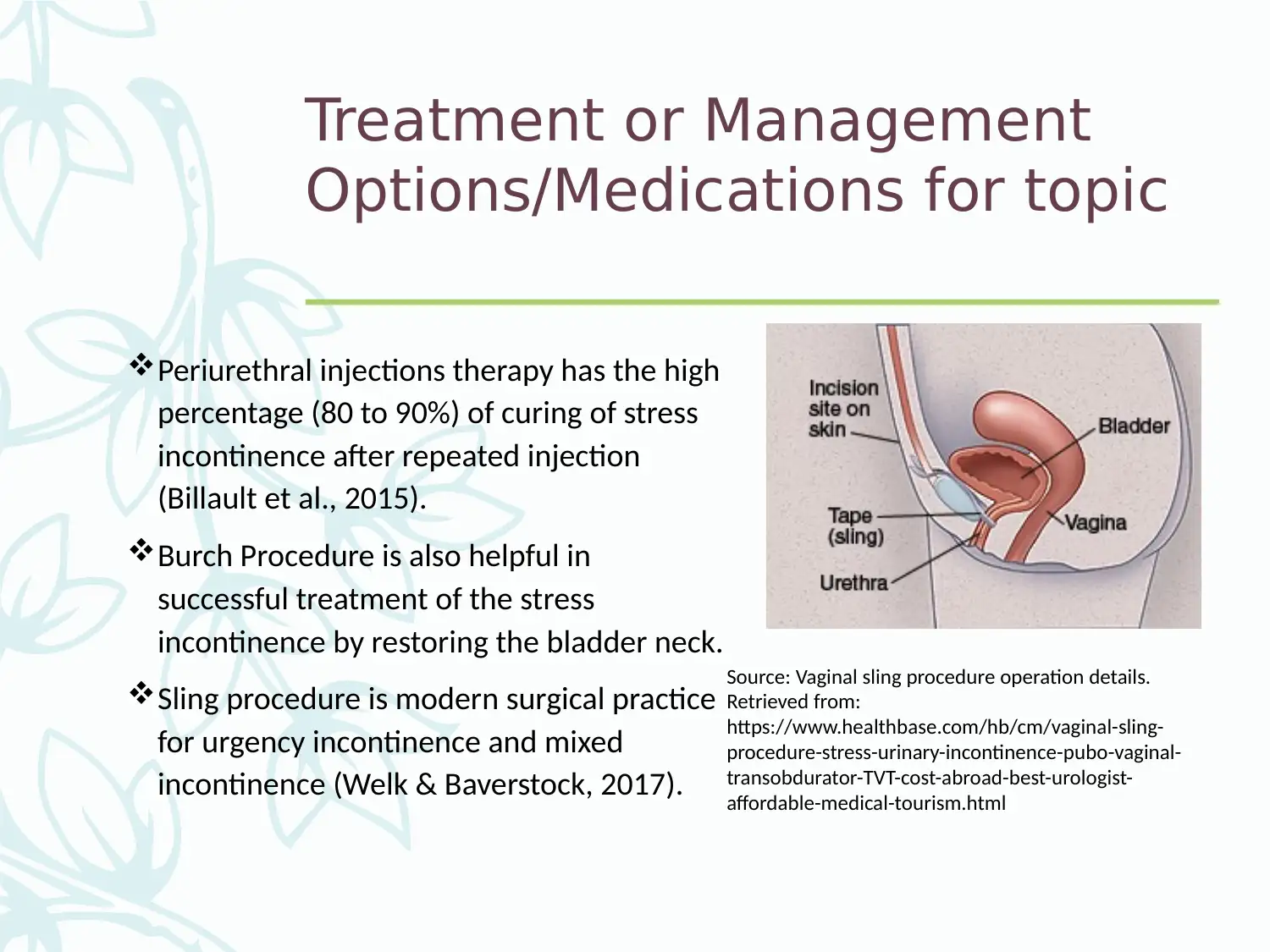
Periurethral injections therapy has the high
percentage (80 to 90%) of curing of stress
incontinence after repeated injection
(Billault et al., 2015).
Burch Procedure is also helpful in
successful treatment of the stress
incontinence by restoring the bladder neck.
Sling procedure is modern surgical practice
for urgency incontinence and mixed
incontinence (Welk & Baverstock, 2017).
Source: Vaginal sling procedure operation details.
Retrieved from:
https://www.healthbase.com/hb/cm/vaginal-sling-
procedure-stress-urinary-incontinence-pubo-vaginal-
transobdurator-TVT-cost-abroad-best-urologist-
affordable-medical-tourism.html
Options/Medications for topic
Periurethral injections therapy has the high
percentage (80 to 90%) of curing of stress
incontinence after repeated injection
(Billault et al., 2015).
Burch Procedure is also helpful in
successful treatment of the stress
incontinence by restoring the bladder neck.
Sling procedure is modern surgical practice
for urgency incontinence and mixed
incontinence (Welk & Baverstock, 2017).
Source: Vaginal sling procedure operation details.
Retrieved from:
https://www.healthbase.com/hb/cm/vaginal-sling-
procedure-stress-urinary-incontinence-pubo-vaginal-
transobdurator-TVT-cost-abroad-best-urologist-
affordable-medical-tourism.html
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Prognosis/Lifestyle Changes
for people having topic.
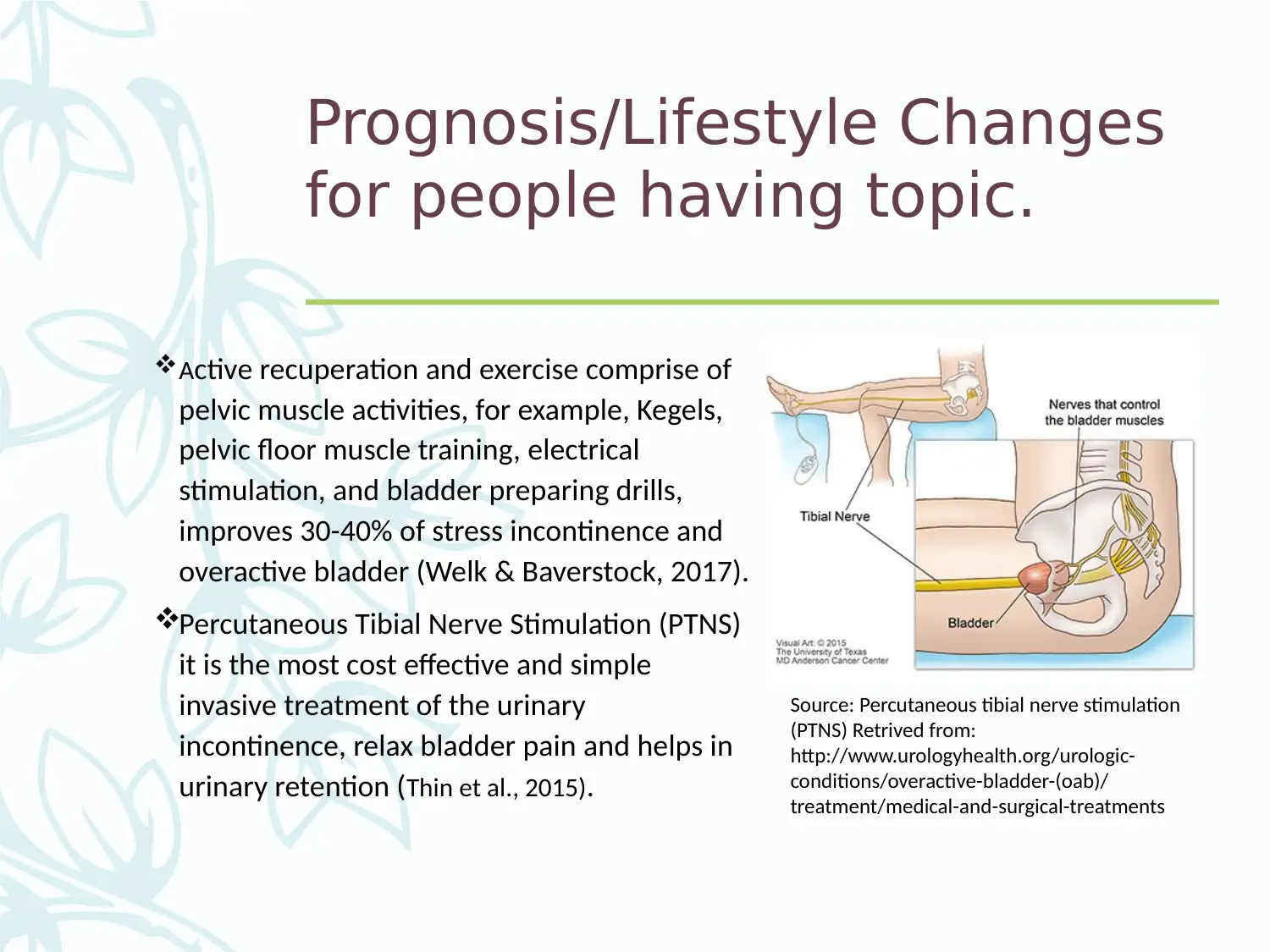
Active recuperation and exercise comprise of
pelvic muscle activities, for example, Kegels,
pelvic floor muscle training, electrical
stimulation, and bladder preparing drills,
improves 30-40% of stress incontinence and
overactive bladder (Welk & Baverstock, 2017).
Percutaneous Tibial Nerve Stimulation (PTNS)
it is the most cost effective and simple
invasive treatment of the urinary
incontinence, relax bladder pain and helps in
urinary retention (Thin et al., 2015).
Source: Percutaneous tibial nerve stimulation
(PTNS) Retrived from:
http://www.urologyhealth.org/urologic-
conditions/overactive-bladder-(oab)/
treatment/medical-and-surgical-treatments
for people having topic.
Active recuperation and exercise comprise of
pelvic muscle activities, for example, Kegels,
pelvic floor muscle training, electrical
stimulation, and bladder preparing drills,
improves 30-40% of stress incontinence and
overactive bladder (Welk & Baverstock, 2017).
Percutaneous Tibial Nerve Stimulation (PTNS)
it is the most cost effective and simple
invasive treatment of the urinary
incontinence, relax bladder pain and helps in
urinary retention (Thin et al., 2015).
Source: Percutaneous tibial nerve stimulation
(PTNS) Retrived from:
http://www.urologyhealth.org/urologic-
conditions/overactive-bladder-(oab)/
treatment/medical-and-surgical-treatments
Prognosis/Lifestyle Changes
for people having topic.
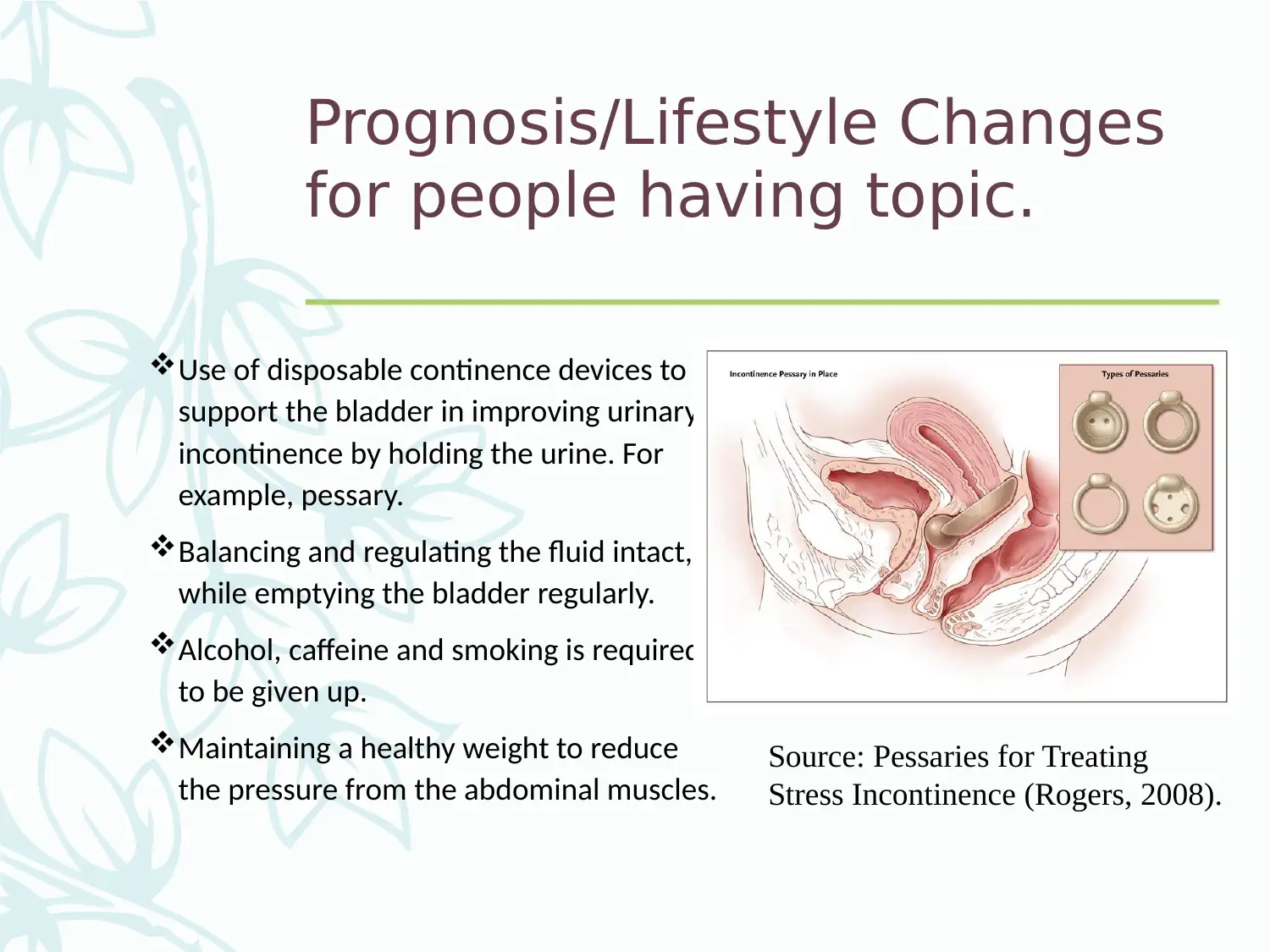
Use of disposable continence devices to
support the bladder in improving urinary
incontinence by holding the urine. For
example, pessary.
Balancing and regulating the fluid intact,
while emptying the bladder regularly.
Alcohol, caffeine and smoking is required
to be given up.
Maintaining a healthy weight to reduce
the pressure from the abdominal muscles.
Source: Pessaries for Treating
Stress Incontinence (Rogers, 2008).
for people having topic.
Use of disposable continence devices to
support the bladder in improving urinary
incontinence by holding the urine. For
example, pessary.
Balancing and regulating the fluid intact,
while emptying the bladder regularly.
Alcohol, caffeine and smoking is required
to be given up.
Maintaining a healthy weight to reduce
the pressure from the abdominal muscles.
Source: Pessaries for Treating
Stress Incontinence (Rogers, 2008).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.