Vaccination and the Law: Case Studies and Legal Frameworks
VerifiedAdded on 2022/09/14
|4
|3691
|10
Report
AI Summary
This report examines the complex interplay between vaccination and the law, focusing on the rights of individuals, particularly parents, versus the interests of public health. It explores the legal frameworks surrounding mandatory vaccination, consent, and the role of case law in determining the best interests of the child. The review analyzes key court cases, such as Gillick v West Norfolk & Wisbech Area Health Authority and Department of Health and Community Services (NT) v JWB and SMB (Marion’s case), to illustrate how courts balance parental rights with the need to protect children from vaccine-preventable diseases. The report also discusses the influence of anti-vaccination lobbies, the spread of misinformation, and the ethical considerations involved in vaccination policies. Furthermore, it highlights the role of government initiatives and the importance of achieving herd immunity through effective communication and incentives. The report concludes by emphasizing the ongoing debate and the challenges of balancing individual autonomy with the collective well-being of society.
849
PROFESSIONAL
REPRINTED FROM AFP VOL.44, NO.11, NOVEMBER 2015© The Royal Australian College of General practitioners 2015
Vaccination and the law
Rachael Heath Jeffery
ublic immunisation programs
reduce mortality and morbidity
in vaccine-preventable diseases,
and are considered to be safe by
governments, health advocates and
practitioners. However, there is strong
opposition to their implementation from
certain lobby groups,1 resulting in a
complex interaction between regulatory
bodies, parents, lobbyists and health
practitioners. Ensuing information and
misinformation has caused many parents
to question whether vaccinating their
child is acting in the child’s best interest.
Debate on whether vaccination
should be made mandatory through
law is vexed. It centres on the rights
of the community versus those of the
individual, in particular, the individual’s
right to make decisions in the best
interest of their child. The success of
vaccination has meant near or total
eradication of serious and often fatal
childhood illnesses. Ironically, it is
this success that has led to parental
complacency and has given rise to
concern that vaccine-preventable
diseases will return.
While it remains the responsibility
of parents to make the decision on
whether to vaccinate their child, legal
disputes have arisen between the child’s
parents, and between parents and the
state. Both sides acknowledge that
vaccination carries risk, but the degree
differs markedly, and the courts have
to arbitrate while maintaining the rights
and best interest of the child in every
instance.
Background
Debate on whether vaccination should
be made mandatory through law is
vexed and centres on the rights of the
community versus those of the individual
– in particular, their right to make
decisions in the best interest of their
child.
Objective
This review examines the role that
legislation and case law play in
determining whether it is in the child’s
best interest to be protected against
vaccine-preventable diseases.
Discussion
Legislating to make vaccination
mandatory raises conflicting issues.
Legal compulsion may impinge on
a parent’s right to choose what they
consider is in the best interest of their
child. The dilemma is whether achieving
herd immunity, in particular the
protection of children against serious and
preventable diseases, justifies infringing
on these rights.
Vaccination and public
health
Ideally, governments formulate their health
policies and regulations more broadly,
and are concerned with the national
interest. They take into account the risks
to individuals, including vulnerable groups
such as children. Parents, on the other
hand, are primarily concerned with the
wellbeing of their child. Understandably,
their decision is emotional and practical
when they weigh up the risks of
vaccination versus non-vaccination.
A wealth of information on the potential
side effects of vaccination is now
available. Unfortunately, misinformation
that instils fear about purported adverse
effects can result in a decrease in
coverage rates below those required to
achieve herd immunity. Typically, vaccine-
related reactions may include fever, rash
and upper respiratory tract symptoms;
however, lowest risk reactions such as
encephalitis can understandably cause the
most alarm because of the potentially fatal
consequences.2– 4
Encouragement and incentive to
vaccinate is best enshrined in policies and
delivered through effective communication
strategies. This is countered by the view
that legal enforcement resolves all those
cases where the parent is apathetic, plus
the law can be flexible to allow for those
who make a deliberate conscientious
objection.
Federal, state and territory governments
are concerned about the repercussions
of low vaccination rates in certain areas
and the potential of disease outbreaks,
P
PROFESSIONAL
REPRINTED FROM AFP VOL.44, NO.11, NOVEMBER 2015© The Royal Australian College of General practitioners 2015
Vaccination and the law
Rachael Heath Jeffery
ublic immunisation programs
reduce mortality and morbidity
in vaccine-preventable diseases,
and are considered to be safe by
governments, health advocates and
practitioners. However, there is strong
opposition to their implementation from
certain lobby groups,1 resulting in a
complex interaction between regulatory
bodies, parents, lobbyists and health
practitioners. Ensuing information and
misinformation has caused many parents
to question whether vaccinating their
child is acting in the child’s best interest.
Debate on whether vaccination
should be made mandatory through
law is vexed. It centres on the rights
of the community versus those of the
individual, in particular, the individual’s
right to make decisions in the best
interest of their child. The success of
vaccination has meant near or total
eradication of serious and often fatal
childhood illnesses. Ironically, it is
this success that has led to parental
complacency and has given rise to
concern that vaccine-preventable
diseases will return.
While it remains the responsibility
of parents to make the decision on
whether to vaccinate their child, legal
disputes have arisen between the child’s
parents, and between parents and the
state. Both sides acknowledge that
vaccination carries risk, but the degree
differs markedly, and the courts have
to arbitrate while maintaining the rights
and best interest of the child in every
instance.
Background
Debate on whether vaccination should
be made mandatory through law is
vexed and centres on the rights of the
community versus those of the individual
– in particular, their right to make
decisions in the best interest of their
child.
Objective
This review examines the role that
legislation and case law play in
determining whether it is in the child’s
best interest to be protected against
vaccine-preventable diseases.
Discussion
Legislating to make vaccination
mandatory raises conflicting issues.
Legal compulsion may impinge on
a parent’s right to choose what they
consider is in the best interest of their
child. The dilemma is whether achieving
herd immunity, in particular the
protection of children against serious and
preventable diseases, justifies infringing
on these rights.
Vaccination and public
health
Ideally, governments formulate their health
policies and regulations more broadly,
and are concerned with the national
interest. They take into account the risks
to individuals, including vulnerable groups
such as children. Parents, on the other
hand, are primarily concerned with the
wellbeing of their child. Understandably,
their decision is emotional and practical
when they weigh up the risks of
vaccination versus non-vaccination.
A wealth of information on the potential
side effects of vaccination is now
available. Unfortunately, misinformation
that instils fear about purported adverse
effects can result in a decrease in
coverage rates below those required to
achieve herd immunity. Typically, vaccine-
related reactions may include fever, rash
and upper respiratory tract symptoms;
however, lowest risk reactions such as
encephalitis can understandably cause the
most alarm because of the potentially fatal
consequences.2– 4
Encouragement and incentive to
vaccinate is best enshrined in policies and
delivered through effective communication
strategies. This is countered by the view
that legal enforcement resolves all those
cases where the parent is apathetic, plus
the law can be flexible to allow for those
who make a deliberate conscientious
objection.
Federal, state and territory governments
are concerned about the repercussions
of low vaccination rates in certain areas
and the potential of disease outbreaks,
P
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
850
PROFESSIONAL VACCINATION AND THE LAW
REPRINTED FROM AFP VOL.44, NO.11, NOVEMBER 2015 © The Royal Australian College of General practitioners 2015
particularly in our increasingly mobile
population. The independent National
Health Performance Authority’s (NHPA’s)
report on childhood immunisation rates
found that despite the high percentage of
children who were fully immunised, there
was still a large number of children who
were not, or were only partly, immunised.
These cases were spread unevenly across
the country. For example, for children
aged five years, the report identified low
immunisation rates around Byron Bay
(about 67%) but high rates in the Illawarra
region (about 98%).5
Consent and the law
Until the late 20th century, common law
assumed that a person under 18 years
of age did not have the capacity to make
health decisions, including consenting
to (and by default declining) medical
treatment on their own behalf. This
position changed following the English
case Gillick v West Norfolk & Wisbech
Area Health Authority6 for determining a
child’s competence. This followed with the
High Court of Australia’s case Department
of Health and Community Services (NT)
v JWB and SMB (commonly known as
‘Marion’s case’).7
The two cases introduced the ‘mature
minor principle’, where minors (under
18 years of age) may be able to make
healthcare decisions on their own behalf
if they are assessed to be sufficiently
mature and intelligent to do so. It is in this
context that Australian courts would rule,
in assessing the best interest of the child,
whether the child refusing vaccination is
‘competent’ to make that decision.
Vaccination through case law
There have been a number of cases
in Australia and internationally where
courts have authorised the vaccination
of a child against the wishes of at least
one of the parents (Box 1). In all cases,
the judges ruled that they were acting in
the best interest of the child and based
their decision on the scientific evidence
presented, including risk assessments by
medical practitioners.
In one instance,8 the parents defied the
New South Wales Supreme Court’s order
to vaccinate and concealed the child until
the period of effectiveness had lapsed.
While the judge defended parens patriae
– the power and authority of the state to
protect persons who are unable to legally
act on their own behalf – this case shows
that monitoring compliance with the
court’s directions can present a problem,
particularly if treatments are ongoing.
Parens patriae may also empower the
courts to overturn the decisions of minors
who refuse treatment, no matter how
‘competent’ they are deemed to be.
In another case, this time in the
UK,9 two children were deemed to be
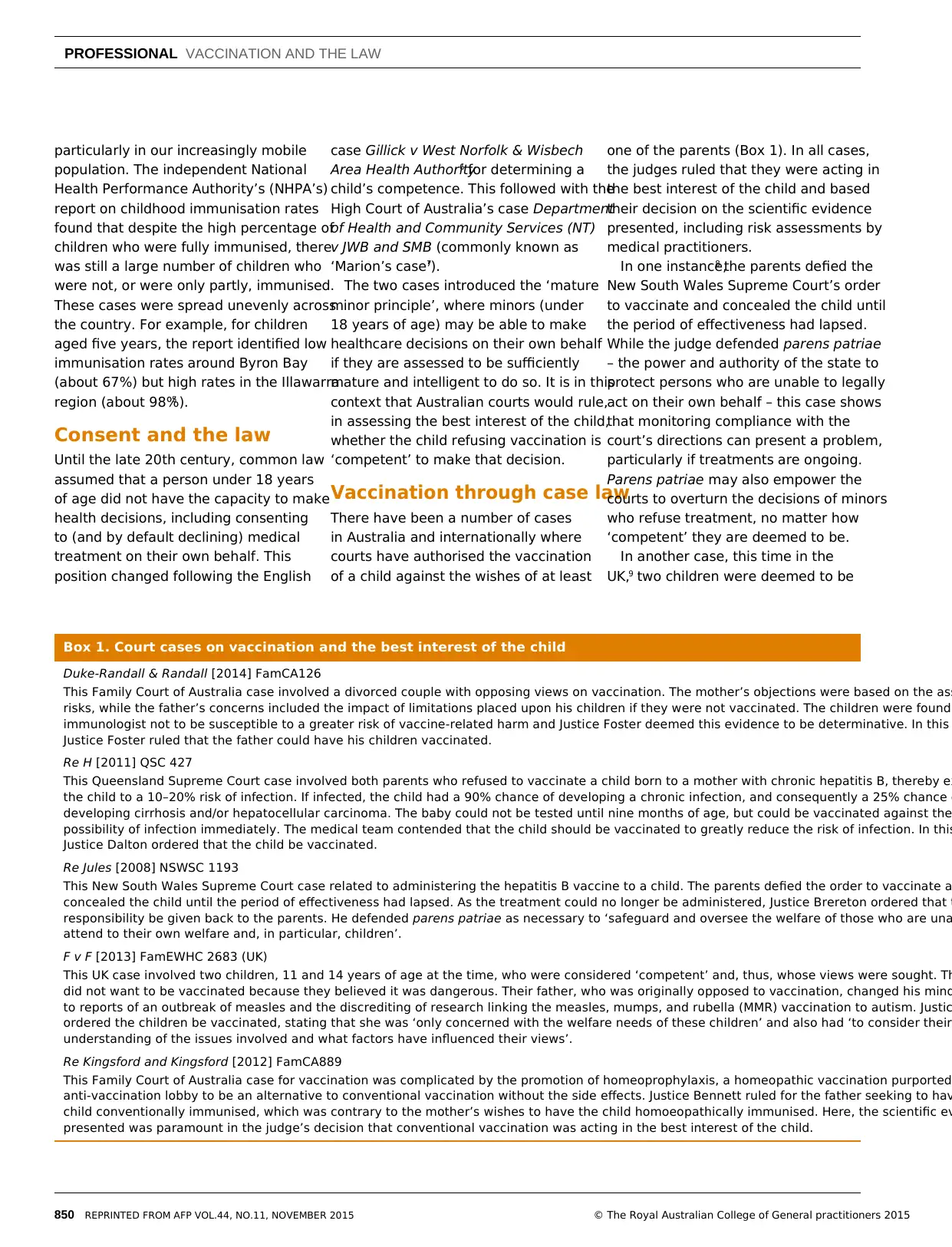
Box 1. Court cases on vaccination and the best interest of the child
Duke-Randall & Randall [2014] FamCA126
This Family Court of Australia case involved a divorced couple with opposing views on vaccination. The mother’s objections were based on the ass
risks, while the father’s concerns included the impact of limitations placed upon his children if they were not vaccinated. The children were found
immunologist not to be susceptible to a greater risk of vaccine-related harm and Justice Foster deemed this evidence to be determinative. In this
Justice Foster ruled that the father could have his children vaccinated.
Re H [2011] QSC 427
This Queensland Supreme Court case involved both parents who refused to vaccinate a child born to a mother with chronic hepatitis B, thereby ex
the child to a 10–20% risk of infection. If infected, the child had a 90% chance of developing a chronic infection, and consequently a 25% chance o
developing cirrhosis and/or hepatocellular carcinoma. The baby could not be tested until nine months of age, but could be vaccinated against the
possibility of infection immediately. The medical team contended that the child should be vaccinated to greatly reduce the risk of infection. In this
Justice Dalton ordered that the child be vaccinated.
Re Jules [2008] NSWSC 1193
This New South Wales Supreme Court case related to administering the hepatitis B vaccine to a child. The parents defied the order to vaccinate a
concealed the child until the period of effectiveness had lapsed. As the treatment could no longer be administered, Justice Brereton ordered that t
responsibility be given back to the parents. He defended parens patriae as necessary to ‘safeguard and oversee the welfare of those who are una
attend to their own welfare and, in particular, children’.
F v F [2013] FamEWHC 2683 (UK)
This UK case involved two children, 11 and 14 years of age at the time, who were considered ‘competent’ and, thus, whose views were sought. Th
did not want to be vaccinated because they believed it was dangerous. Their father, who was originally opposed to vaccination, changed his mind
to reports of an outbreak of measles and the discrediting of research linking the measles, mumps, and rubella (MMR) vaccination to autism. Justic
ordered the children be vaccinated, stating that she was ‘only concerned with the welfare needs of these children’ and also had ‘to consider their
understanding of the issues involved and what factors have influenced their views’.
Re Kingsford and Kingsford [2012] FamCA889
This Family Court of Australia case for vaccination was complicated by the promotion of homeoprophylaxis, a homeopathic vaccination purported
anti-vaccination lobby to be an alternative to conventional vaccination without the side effects. Justice Bennett ruled for the father seeking to hav
child conventionally immunised, which was contrary to the mother’s wishes to have the child homoeopathically immunised. Here, the scientific ev
presented was paramount in the judge’s decision that conventional vaccination was acting in the best interest of the child.
PROFESSIONAL VACCINATION AND THE LAW
REPRINTED FROM AFP VOL.44, NO.11, NOVEMBER 2015 © The Royal Australian College of General practitioners 2015
particularly in our increasingly mobile
population. The independent National
Health Performance Authority’s (NHPA’s)
report on childhood immunisation rates
found that despite the high percentage of
children who were fully immunised, there
was still a large number of children who
were not, or were only partly, immunised.
These cases were spread unevenly across
the country. For example, for children
aged five years, the report identified low
immunisation rates around Byron Bay
(about 67%) but high rates in the Illawarra
region (about 98%).5
Consent and the law
Until the late 20th century, common law
assumed that a person under 18 years
of age did not have the capacity to make
health decisions, including consenting
to (and by default declining) medical
treatment on their own behalf. This
position changed following the English
case Gillick v West Norfolk & Wisbech
Area Health Authority6 for determining a
child’s competence. This followed with the
High Court of Australia’s case Department
of Health and Community Services (NT)
v JWB and SMB (commonly known as
‘Marion’s case’).7
The two cases introduced the ‘mature
minor principle’, where minors (under
18 years of age) may be able to make
healthcare decisions on their own behalf
if they are assessed to be sufficiently
mature and intelligent to do so. It is in this
context that Australian courts would rule,
in assessing the best interest of the child,
whether the child refusing vaccination is
‘competent’ to make that decision.
Vaccination through case law
There have been a number of cases
in Australia and internationally where
courts have authorised the vaccination
of a child against the wishes of at least
one of the parents (Box 1). In all cases,
the judges ruled that they were acting in
the best interest of the child and based
their decision on the scientific evidence
presented, including risk assessments by
medical practitioners.
In one instance,8 the parents defied the
New South Wales Supreme Court’s order
to vaccinate and concealed the child until
the period of effectiveness had lapsed.
While the judge defended parens patriae
– the power and authority of the state to
protect persons who are unable to legally
act on their own behalf – this case shows
that monitoring compliance with the
court’s directions can present a problem,
particularly if treatments are ongoing.
Parens patriae may also empower the
courts to overturn the decisions of minors
who refuse treatment, no matter how
‘competent’ they are deemed to be.
In another case, this time in the
UK,9 two children were deemed to be
Box 1. Court cases on vaccination and the best interest of the child
Duke-Randall & Randall [2014] FamCA126
This Family Court of Australia case involved a divorced couple with opposing views on vaccination. The mother’s objections were based on the ass
risks, while the father’s concerns included the impact of limitations placed upon his children if they were not vaccinated. The children were found
immunologist not to be susceptible to a greater risk of vaccine-related harm and Justice Foster deemed this evidence to be determinative. In this
Justice Foster ruled that the father could have his children vaccinated.
Re H [2011] QSC 427
This Queensland Supreme Court case involved both parents who refused to vaccinate a child born to a mother with chronic hepatitis B, thereby ex
the child to a 10–20% risk of infection. If infected, the child had a 90% chance of developing a chronic infection, and consequently a 25% chance o
developing cirrhosis and/or hepatocellular carcinoma. The baby could not be tested until nine months of age, but could be vaccinated against the
possibility of infection immediately. The medical team contended that the child should be vaccinated to greatly reduce the risk of infection. In this
Justice Dalton ordered that the child be vaccinated.
Re Jules [2008] NSWSC 1193
This New South Wales Supreme Court case related to administering the hepatitis B vaccine to a child. The parents defied the order to vaccinate a
concealed the child until the period of effectiveness had lapsed. As the treatment could no longer be administered, Justice Brereton ordered that t
responsibility be given back to the parents. He defended parens patriae as necessary to ‘safeguard and oversee the welfare of those who are una
attend to their own welfare and, in particular, children’.
F v F [2013] FamEWHC 2683 (UK)
This UK case involved two children, 11 and 14 years of age at the time, who were considered ‘competent’ and, thus, whose views were sought. Th
did not want to be vaccinated because they believed it was dangerous. Their father, who was originally opposed to vaccination, changed his mind
to reports of an outbreak of measles and the discrediting of research linking the measles, mumps, and rubella (MMR) vaccination to autism. Justic
ordered the children be vaccinated, stating that she was ‘only concerned with the welfare needs of these children’ and also had ‘to consider their
understanding of the issues involved and what factors have influenced their views’.
Re Kingsford and Kingsford [2012] FamCA889
This Family Court of Australia case for vaccination was complicated by the promotion of homeoprophylaxis, a homeopathic vaccination purported
anti-vaccination lobby to be an alternative to conventional vaccination without the side effects. Justice Bennett ruled for the father seeking to hav
child conventionally immunised, which was contrary to the mother’s wishes to have the child homoeopathically immunised. Here, the scientific ev
presented was paramount in the judge’s decision that conventional vaccination was acting in the best interest of the child.

851
VACCINATION AND THE LAW PROFESSIONAL
REPRINTED FROM AFP VOL.44, NO.11, NOVEMBER 2015© The Royal Australian College of General practitioners 2015
‘competent’ as they possessed the
necessary reasoning abilities to have
their views against vaccination taken into
account. However, the judge decided
for vaccination, stating she was ‘only
concerned with the welfare needs of
these children’. A decision by an Australian
court in this instance would be guided by
the Gillick and Marion cases.
In early 2015, the gulf between pro-
and anti-vaccination groups was again
illustrated in a German regional court. It
decided for a doctor claiming a reward
from a biologist who had offered €100,000
for scientific evidence proving the measles
virus, but then refused to pay.10
Anti-vaccination lobby
Anti-vaccinationists have existed for as
long as vaccines and have always agitated
strongly against vaccination. Dr Sherri
Tenpenny regularly delivers seminars
on what she believes are the negative
impacts of vaccines on health. One of her
books was promoted as a ‘comprehensive
guide’ and explains why vaccines are
‘detrimental to yours and your child’s
health’, which she attributes to ‘vaccine
injuries’ such as autism, asthma and
autoimmune disorders.11
Dr Tenpenny has warned that ‘each
shot is a Russian roulette: you never
know which chamber has the bullet
that could kill you’.12 She argues that
adverse reactions listed in the package
inserts include encephalitis and criticises
‘deceptive research’, claiming a shot of
aluminium was used as the placebo during
a safety study with the Gardasil vaccine.11
The anti-vaccination movement has
increasingly used the internet and social
media to distribute largely unchecked,
alarmist and misleading material. It has
therefore been impossible to enforce
uniform ethical approaches from the pro-
and anti-vaccination advocates.
In some instances, courts and tribunals
have addressed the distribution of
misleading material regarding vaccination.
What remains unclear is whether the
anti-vaccination lobby is legally required
to adhere to the standards that health
professionals are, namely to conduct
themselves in a manner prescribed under
professional codes and legislation.13
Failure to comply could potentially result
in the loss of registration and/or practising
rights.14
In the New South Wales case of
Australian Vaccination Network Inc v
Health Care Complaints Commission,
Justice Adamson ordered that it was not
within the Commission’s jurisdiction15,16
to issue a public warning against the
Australian Vaccination Network in relation
to ‘engaging in misleading or deceptive
conduct in order to dissuade people
from being, or having their children,
vaccinated’.17 However, in February 2014,
following a jurisdictional change in the
law, the New South Wales Administrative
Decisions Tribunal upheld an order from
the Office of Fair Trading for the Australian
Vaccination Network to change its name
to the Australian Vaccination-Sceptics
Network to more accurately reflect the
advice it dispenses.
Federal, state and territory
vaccination initiatives
The Australian Government is
implementing its National Immunisation
Strategy for Australia 2013–2018 through a
set of strategic priorities,18 which includes:
• improving immunisation coverage
through secure and efficient supply of
vaccines
• community confidence
• a skilled immunisation workforce
• effective monitoring and analysis of
results.
Essential vaccines are provided free
of charge to eligible infants, children,
adolescents and adults, meeting
international goals set by the World Health
Organization. Vaccinations are monitored
under the independent NHPA, which was
set up under the National Health Reform
Act 2011. Program funding agreements
between governments are set up under
the National Partnership Agreement on
Essential Vaccines.18
State and territory governments are
instituting more requirements to ensure
children are vaccinated. In New South
Wales, the Public Health Act 2010 was
amended so that from 1 January 2014,
before enrolment at a childcare facility,
a parent/guardian is required to show
that their child is fully vaccinated for
their age, has a medical reason not to
be vaccinated or is on a recognised
catch-up schedule for their vaccinations.
Otherwise, they have to declare a
conscientious objection to vaccination.19
This followed prolonged measles
outbreaks in 2011 and 2013, and a
subsequent ‘No Jab No Play’ campaign,
which resulted from findings that some
communities in New South Wales had
vaccination rates under 50%.20 The
Queensland Government has announced
its intention to introduce similar
legislation in 2015. At the federal level,
vaccination eligibility requirements have
been introduced for entitlements such as
Family Tax Benefit B.
Compulsory vaccination has been
effective in preventing disease outbreaks,
and as such justifies government
intervention.21 However, debate on
mandatory vaccination must be open
and factual.22–24 Official exemptions
on various grounds address protests
regarding the ‘nanny state’ levelled
against governments; however,
exemption rates as low as 2% can
increase a community’s risk of disease
outbreaks, depending on the disease.
Fortunately, in the case of rotavirus, 80%
coverage resulted in significant herd
immunity and subsequent decrease in
hospitalisations.25
In accordance with legislation and case
law, it is in a child’s best interest to be
protected against vaccine-preventable
disease. It is also in the community’s
best interest that children are protected
against outbreak and spread of
disease. To date, this is best achieved
through programs that are accessible,
well communicated and supported
by law, so that parents can make
informed decisions. It also counters
the misinformation distributed by those
opposed to vaccination.
VACCINATION AND THE LAW PROFESSIONAL
REPRINTED FROM AFP VOL.44, NO.11, NOVEMBER 2015© The Royal Australian College of General practitioners 2015
‘competent’ as they possessed the
necessary reasoning abilities to have
their views against vaccination taken into
account. However, the judge decided
for vaccination, stating she was ‘only
concerned with the welfare needs of
these children’. A decision by an Australian
court in this instance would be guided by
the Gillick and Marion cases.
In early 2015, the gulf between pro-
and anti-vaccination groups was again
illustrated in a German regional court. It
decided for a doctor claiming a reward
from a biologist who had offered €100,000
for scientific evidence proving the measles
virus, but then refused to pay.10
Anti-vaccination lobby
Anti-vaccinationists have existed for as
long as vaccines and have always agitated
strongly against vaccination. Dr Sherri
Tenpenny regularly delivers seminars
on what she believes are the negative
impacts of vaccines on health. One of her
books was promoted as a ‘comprehensive
guide’ and explains why vaccines are
‘detrimental to yours and your child’s
health’, which she attributes to ‘vaccine
injuries’ such as autism, asthma and
autoimmune disorders.11
Dr Tenpenny has warned that ‘each
shot is a Russian roulette: you never
know which chamber has the bullet
that could kill you’.12 She argues that
adverse reactions listed in the package
inserts include encephalitis and criticises
‘deceptive research’, claiming a shot of
aluminium was used as the placebo during
a safety study with the Gardasil vaccine.11
The anti-vaccination movement has
increasingly used the internet and social
media to distribute largely unchecked,
alarmist and misleading material. It has
therefore been impossible to enforce
uniform ethical approaches from the pro-
and anti-vaccination advocates.
In some instances, courts and tribunals
have addressed the distribution of
misleading material regarding vaccination.
What remains unclear is whether the
anti-vaccination lobby is legally required
to adhere to the standards that health
professionals are, namely to conduct
themselves in a manner prescribed under
professional codes and legislation.13
Failure to comply could potentially result
in the loss of registration and/or practising
rights.14
In the New South Wales case of
Australian Vaccination Network Inc v
Health Care Complaints Commission,
Justice Adamson ordered that it was not
within the Commission’s jurisdiction15,16
to issue a public warning against the
Australian Vaccination Network in relation
to ‘engaging in misleading or deceptive
conduct in order to dissuade people
from being, or having their children,
vaccinated’.17 However, in February 2014,
following a jurisdictional change in the
law, the New South Wales Administrative
Decisions Tribunal upheld an order from
the Office of Fair Trading for the Australian
Vaccination Network to change its name
to the Australian Vaccination-Sceptics
Network to more accurately reflect the
advice it dispenses.
Federal, state and territory
vaccination initiatives
The Australian Government is
implementing its National Immunisation
Strategy for Australia 2013–2018 through a
set of strategic priorities,18 which includes:
• improving immunisation coverage
through secure and efficient supply of
vaccines
• community confidence
• a skilled immunisation workforce
• effective monitoring and analysis of
results.
Essential vaccines are provided free
of charge to eligible infants, children,
adolescents and adults, meeting
international goals set by the World Health
Organization. Vaccinations are monitored
under the independent NHPA, which was
set up under the National Health Reform
Act 2011. Program funding agreements
between governments are set up under
the National Partnership Agreement on
Essential Vaccines.18
State and territory governments are
instituting more requirements to ensure
children are vaccinated. In New South
Wales, the Public Health Act 2010 was
amended so that from 1 January 2014,
before enrolment at a childcare facility,
a parent/guardian is required to show
that their child is fully vaccinated for
their age, has a medical reason not to
be vaccinated or is on a recognised
catch-up schedule for their vaccinations.
Otherwise, they have to declare a
conscientious objection to vaccination.19
This followed prolonged measles
outbreaks in 2011 and 2013, and a
subsequent ‘No Jab No Play’ campaign,
which resulted from findings that some
communities in New South Wales had
vaccination rates under 50%.20 The
Queensland Government has announced
its intention to introduce similar
legislation in 2015. At the federal level,
vaccination eligibility requirements have
been introduced for entitlements such as
Family Tax Benefit B.
Compulsory vaccination has been
effective in preventing disease outbreaks,
and as such justifies government
intervention.21 However, debate on
mandatory vaccination must be open
and factual.22–24 Official exemptions
on various grounds address protests
regarding the ‘nanny state’ levelled
against governments; however,
exemption rates as low as 2% can
increase a community’s risk of disease
outbreaks, depending on the disease.
Fortunately, in the case of rotavirus, 80%
coverage resulted in significant herd
immunity and subsequent decrease in
hospitalisations.25
In accordance with legislation and case
law, it is in a child’s best interest to be
protected against vaccine-preventable
disease. It is also in the community’s
best interest that children are protected
against outbreak and spread of
disease. To date, this is best achieved
through programs that are accessible,
well communicated and supported
by law, so that parents can make
informed decisions. It also counters
the misinformation distributed by those
opposed to vaccination.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
852
PROFESSIONAL VACCINATION AND THE LAW
REPRINTED FROM AFP VOL.44, NO.11, NOVEMBER 2015 © The Royal Australian College of General practitioners 2015
Since this article’s submission, from 1
January 2016, conscientious objection will
be removed as an exemption category for
the Child Care Benefit, Child Care Rebate
and Family Tax Benefit Part A end of year
supplement.26 Existing exemptions on
medical or religious grounds will still apply
with the correct approval. Importantly,
immunisation requirements for payments
will also be extended to include children
of all ages except those under 12 months
(based on early childhood immunisation
status).26
Key points
• Vaccination reduces mortality and
morbidity in vaccine-preventable
diseases.
• Debate centres on the rights of the
community versus those of the
individual.
• Misinformation can result in a decrease
in coverage rates required for herd
immunity.
• A large number of children are not, or
are only partly, immunised, and these
cases are spread unevenly across
Australia.
• Courts have authorised the vaccination
of a child against the wishes of at least
one of the parents, in all cases acting in
the best interest of the child.
• The anti-vaccination movement has
distributed misinformation and it is
unclear whether it is legally required
to adhere to the same standards that
apply to health professionals.
• The National Immunisation Strategy for
Australia 2013–2018 sets out strategic
priorities and meets international goals
set by the World Health Organization.
• On 1 January 2014, New South Wales
legislated requirements to ensure
children are appropriately vaccinated
before enrolment at a childcare facility.
Author
Rachael C Heath Jeffery BAppSc (Hons), medical
student, Australian National University Medical
School, Canberra, ACT. u4535769@anu.edu.au
Competing interests: None.
Provenance and peer review: Not commissioned,
externally peer reviewed.
References
1. Vines T, Faunce T. Civil liberties and the critics
of safe vaccination: Australian Vaccination
Network Inc v Health Care Complaints
Commission [2012] NSWSC 110. J Law Med
2012;20:44–58.
2. Peltola H, Hemonen OP. Frequency of true
adverse reactions to measles-mumps-rubella
vaccine. Lancet 1986;1:939–42.
3. Fenichel GM. Neurological complications of
immunization. Ann Neurol 1982;12:119–29.
4. Adetunji J. Schoolgirl dies after cervical cancer
vaccination. The Guardian 2009 September
29. Available at www.guardian.co.uk/uk/2009/
sep/28/hpv-cervical-cancer-vaccine-death
[Accessed 18 August 2014].
5. National Health Performance Authority. Healthy
Communities: Immunisation rates for children
in 2012–13. NHPA: Canberra, 2014.
6. Gillick v West Norfolk and Wisbech Area Health
Authority [1986] AC 112.
7. Department of Health and Community Services
(NT) v JWB and SMB (1992) 175 CLR 218.
8. Director-General, Department of Community
Services. Re Jules [2008]. NSWSC 1193:7.
9. F v F [2013] Fam EWHC 2683.
10. Bajekal N. German biologist who denied
measles exists ordered to pay more than
100,000. Time World 2015 March 13. Available
at http://time.com/3743883/german-biologist-
measles-pay [Accessed 15 March 2015].
11. Tenpenny S. Saying no to vaccines: A resource
guide for all ages. New York: NMA Media Press,
2008.
12. Tenpenny S. The ten reasons to say no to
vaccines. Vaccination Council 2011 January
9. Available at www.vaccinationcouncil.
org/2011/01/09/the-ten-reasons-to-say-no-to-
vaccines [Accessed 10 February 2015].
13. Health Practitioner Regulation National Law,
s 139B(1)(a)(i), adopted by New South Wales
through the Health Practitioner Regulation
(Adoption of National Law) Act 2009 (NSW).
14. Health Practitioner Regulation National Law
2009 (NSW), s 55.
15. The Australian Traditional-Medicine Society.
Submission to the Committee on the HCCC
Inquiry into False or Misleading Health-related
Information or Practices. December 2013.
16. Australian Vaccination Network Inc v Health
Care Complaints Commission [2012] NSWSC
110.
17. Evans L, HCCC investigator. Investigation report
regarding the Australian Vaccination Network.
Ms Meryl Dorey (File No 09/01695 & 10/00002)
(7 July 2010) p 2 (Investigation Report).
Available at www.stopavn.com/documents/
HCCC-Report.pdf [Accessed 31 August 2014].
18. Department of Health. National Immunisation
Strategy for Australia 2013–2018. Canberra:
Department of Health, 2013.
19. Public Health Amendment (Vaccination of
Children Attending Child Care Facilities) Act
2013 (NSW Bills) No 127.
20. National Health Performance Authority. Healthy
communities: Immunisation rates for children in
2011–12. Canberra: NHPA, 2013.
21. Salmon DA, Teret SP, MacIntyre CR, et al.
Compulsory vaccination and conscientious or
philosophical exemptions: Past, present, and
future. Lancet 2006;367:436–42.
22. Javitt G, Berkowitz D, Gostin LO. Assessing
mandatory HPV vaccination: Who should call the
shots? J Law Med Ethics 2008;36:384–95.
23. Regan DG, Philp DJ, Hocking JS, et al. Modeling
the population-level impact of vaccination on the
transmission of human papillomavirus type 16 in
Australia. Sex Health 2007;4:147–63.
24. Zimmerman RK. Ethical analysis of HPV vaccine
policy options. Vaccine 2006;24:4812–20.
25. Dey A, Wang H, Menzies R, Macartney
K. Changes in hospitalisations for acute
gastroenteritis in Australia after the national
rotavirus vaccination program. Med J Aust
2012;197:453–57.
26. Australian Government Department of
Social Services. Strengthening immunisation
requirements: Fact sheet. Canberra: 2015.
Available at www.dss.gov.au/sites/default/
files/documents/04_2015/immunisation_fact_
sheet_-_12_april_2015.docx [Accessed 14
September 2015].
PROFESSIONAL VACCINATION AND THE LAW
REPRINTED FROM AFP VOL.44, NO.11, NOVEMBER 2015 © The Royal Australian College of General practitioners 2015
Since this article’s submission, from 1
January 2016, conscientious objection will
be removed as an exemption category for
the Child Care Benefit, Child Care Rebate
and Family Tax Benefit Part A end of year
supplement.26 Existing exemptions on
medical or religious grounds will still apply
with the correct approval. Importantly,
immunisation requirements for payments
will also be extended to include children
of all ages except those under 12 months
(based on early childhood immunisation
status).26
Key points
• Vaccination reduces mortality and
morbidity in vaccine-preventable
diseases.
• Debate centres on the rights of the
community versus those of the
individual.
• Misinformation can result in a decrease
in coverage rates required for herd
immunity.
• A large number of children are not, or
are only partly, immunised, and these
cases are spread unevenly across
Australia.
• Courts have authorised the vaccination
of a child against the wishes of at least
one of the parents, in all cases acting in
the best interest of the child.
• The anti-vaccination movement has
distributed misinformation and it is
unclear whether it is legally required
to adhere to the same standards that
apply to health professionals.
• The National Immunisation Strategy for
Australia 2013–2018 sets out strategic
priorities and meets international goals
set by the World Health Organization.
• On 1 January 2014, New South Wales
legislated requirements to ensure
children are appropriately vaccinated
before enrolment at a childcare facility.
Author
Rachael C Heath Jeffery BAppSc (Hons), medical
student, Australian National University Medical
School, Canberra, ACT. u4535769@anu.edu.au
Competing interests: None.
Provenance and peer review: Not commissioned,
externally peer reviewed.
References
1. Vines T, Faunce T. Civil liberties and the critics
of safe vaccination: Australian Vaccination
Network Inc v Health Care Complaints
Commission [2012] NSWSC 110. J Law Med
2012;20:44–58.
2. Peltola H, Hemonen OP. Frequency of true
adverse reactions to measles-mumps-rubella
vaccine. Lancet 1986;1:939–42.
3. Fenichel GM. Neurological complications of
immunization. Ann Neurol 1982;12:119–29.
4. Adetunji J. Schoolgirl dies after cervical cancer
vaccination. The Guardian 2009 September
29. Available at www.guardian.co.uk/uk/2009/
sep/28/hpv-cervical-cancer-vaccine-death
[Accessed 18 August 2014].
5. National Health Performance Authority. Healthy
Communities: Immunisation rates for children
in 2012–13. NHPA: Canberra, 2014.
6. Gillick v West Norfolk and Wisbech Area Health
Authority [1986] AC 112.
7. Department of Health and Community Services
(NT) v JWB and SMB (1992) 175 CLR 218.
8. Director-General, Department of Community
Services. Re Jules [2008]. NSWSC 1193:7.
9. F v F [2013] Fam EWHC 2683.
10. Bajekal N. German biologist who denied
measles exists ordered to pay more than
100,000. Time World 2015 March 13. Available
at http://time.com/3743883/german-biologist-
measles-pay [Accessed 15 March 2015].
11. Tenpenny S. Saying no to vaccines: A resource
guide for all ages. New York: NMA Media Press,
2008.
12. Tenpenny S. The ten reasons to say no to
vaccines. Vaccination Council 2011 January
9. Available at www.vaccinationcouncil.
org/2011/01/09/the-ten-reasons-to-say-no-to-
vaccines [Accessed 10 February 2015].
13. Health Practitioner Regulation National Law,
s 139B(1)(a)(i), adopted by New South Wales
through the Health Practitioner Regulation
(Adoption of National Law) Act 2009 (NSW).
14. Health Practitioner Regulation National Law
2009 (NSW), s 55.
15. The Australian Traditional-Medicine Society.
Submission to the Committee on the HCCC
Inquiry into False or Misleading Health-related
Information or Practices. December 2013.
16. Australian Vaccination Network Inc v Health
Care Complaints Commission [2012] NSWSC
110.
17. Evans L, HCCC investigator. Investigation report
regarding the Australian Vaccination Network.
Ms Meryl Dorey (File No 09/01695 & 10/00002)
(7 July 2010) p 2 (Investigation Report).
Available at www.stopavn.com/documents/
HCCC-Report.pdf [Accessed 31 August 2014].
18. Department of Health. National Immunisation
Strategy for Australia 2013–2018. Canberra:
Department of Health, 2013.
19. Public Health Amendment (Vaccination of
Children Attending Child Care Facilities) Act
2013 (NSW Bills) No 127.
20. National Health Performance Authority. Healthy
communities: Immunisation rates for children in
2011–12. Canberra: NHPA, 2013.
21. Salmon DA, Teret SP, MacIntyre CR, et al.
Compulsory vaccination and conscientious or
philosophical exemptions: Past, present, and
future. Lancet 2006;367:436–42.
22. Javitt G, Berkowitz D, Gostin LO. Assessing
mandatory HPV vaccination: Who should call the
shots? J Law Med Ethics 2008;36:384–95.
23. Regan DG, Philp DJ, Hocking JS, et al. Modeling
the population-level impact of vaccination on the
transmission of human papillomavirus type 16 in
Australia. Sex Health 2007;4:147–63.
24. Zimmerman RK. Ethical analysis of HPV vaccine
policy options. Vaccine 2006;24:4812–20.
25. Dey A, Wang H, Menzies R, Macartney
K. Changes in hospitalisations for acute
gastroenteritis in Australia after the national
rotavirus vaccination program. Med J Aust
2012;197:453–57.
26. Australian Government Department of
Social Services. Strengthening immunisation
requirements: Fact sheet. Canberra: 2015.
Available at www.dss.gov.au/sites/default/
files/documents/04_2015/immunisation_fact_
sheet_-_12_april_2015.docx [Accessed 14
September 2015].
1 out of 4
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





