Report: Parental Attitudes on Childhood Vaccinations in Australia
VerifiedAdded on 2022/09/14
|7
|5431
|12
Report
AI Summary
This report presents the findings of a national online survey conducted in Australia in 2012, investigating parental attitudes, behaviors, and concerns regarding childhood vaccinations. The study aimed to describe parental views, identify factors associated with non-compliance with the National Immunisation Program Schedule (NIPS), and determine the primary sources of vaccination information. The survey included 452 parents of children under 18 years old, revealing that while 92% reported their children as up-to-date with vaccinations, 52% still had concerns. Key findings indicated that disagreeing with the safety of vaccines and obtaining information from alternative health practitioners were associated with non-compliance. General practitioners (GPs) were identified as the most influential source of vaccination information. The report emphasizes the crucial role of GPs in addressing parental concerns and improving vaccination compliance through education and communication. The study also highlights the public health implications of vaccine hesitancy and the importance of maintaining high vaccination coverage to prevent outbreaks of vaccine-preventable diseases.
145
RESEARCH
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017© The Royal Australian College of General Practitioners 2017
Parental attitudes, beliefs, behaviours
concerns towards childhood vaccinatio
in Australia: A national online survey
Maria Yui Kwan Chow, Margie Danchin, Harold W Willaby, Sonya Pemberton, Julie Leask
accine hesitancy is an issue of global concern in
developed and developing countries.1 MacDonald et al
characterise vaccine hesitancy as the degree of parents’
concerns regarding vaccines and vaccination, and place this on
a continuum.2 The most recent estimate for the proportion of
children affected in Australia by active vaccine refusal was 3.3%.3
However, these families are likely to represent only a portion
of vaccine-hesitant parents, with many continuing to vaccinate
according to the National Immunisation Program Schedule (NIPS)
despite having milder hesitancy than the more extreme case of
refusing all vaccines. The success of vaccination programs means
that vaccine-preventable diseases have been less frequently seen
in the past few decades. However, as outbreaks in a number of
countries attest, population immunity will be threatened if more
children do not comply with vaccination schedules.4
At present in Australia, there is high coverage for
recommended childhood vaccines. In 2012, the year that
this survey was conducted, children aged 24 months had
approximately 92.6% coverage and 1.5% of children were
affected by registered parental ‘conscientious objection’.5 Despite
this, any vaccine program is vulnerable to falls in coverage,
particularly when a vaccine safety scare arises. For example, in
the UK, the unsubstantiated measles, mumps and rubella (MMR)
autism scare led to a decline in MMR vaccination rates.6
The most recent national vaccine attitudes survey conducted
in 2001 found that the majority of parents with incompletely
immunised children (70%) were concerned about vaccine side
effects.7 This was particularly evident after the suspension of
CSL Fluvax because of a higher rate of febrile convulsions in
children. Our primary source of information regarding vaccination
uptake – the Australian Childhood Immunisation Register (ACIR)
– maintains the vaccination history of children up to seven years
of age. However, ACIR does not quantify the attitudes, beliefs
and concerns of individuals that underlie vaccination uptake and
objection.
Background and objectives
Vaccine hesitancy is a public health concern. The objectives
of this article were to describe Australian parents’ attitudes,
behaviours and concerns about vaccination, determine
the factors associated with vaccination non-compliance,
and provide sources of vaccination information for general
practitioners (GPs).
Methods
We conducted a nationally representative online survey of
Australian parents in 2012. We determined associations
between demographic and vaccination attitudes and behaviour.
Results
The 452 respondents were parents of children aged <18
years. Despite 92% reporting their child as up to date with
vaccination, 52% had concerns. Factors associated with non-
compliance included ‘disagreeing that vaccines are safe’ (odds
ratio [OR]: 2.79; 95% confidence interval [CI]: 1.00–7.76) and
‘obtaining information from alternative health practitioners’
(OR: 6.54; 95% CI: 1.71-25.00). The vast majority (83%) obtained
vaccination information from their GPs.
Discussion
GPs have pivotal roles in addressing concerns regarding
vaccination. Education and communication with parents will
improve their knowledge and trust in vaccination, thereby
improving vaccination compliance.
V
RESEARCH
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017© The Royal Australian College of General Practitioners 2017
Parental attitudes, beliefs, behaviours
concerns towards childhood vaccinatio
in Australia: A national online survey
Maria Yui Kwan Chow, Margie Danchin, Harold W Willaby, Sonya Pemberton, Julie Leask
accine hesitancy is an issue of global concern in
developed and developing countries.1 MacDonald et al
characterise vaccine hesitancy as the degree of parents’
concerns regarding vaccines and vaccination, and place this on
a continuum.2 The most recent estimate for the proportion of
children affected in Australia by active vaccine refusal was 3.3%.3
However, these families are likely to represent only a portion
of vaccine-hesitant parents, with many continuing to vaccinate
according to the National Immunisation Program Schedule (NIPS)
despite having milder hesitancy than the more extreme case of
refusing all vaccines. The success of vaccination programs means
that vaccine-preventable diseases have been less frequently seen
in the past few decades. However, as outbreaks in a number of
countries attest, population immunity will be threatened if more
children do not comply with vaccination schedules.4
At present in Australia, there is high coverage for
recommended childhood vaccines. In 2012, the year that
this survey was conducted, children aged 24 months had
approximately 92.6% coverage and 1.5% of children were
affected by registered parental ‘conscientious objection’.5 Despite
this, any vaccine program is vulnerable to falls in coverage,
particularly when a vaccine safety scare arises. For example, in
the UK, the unsubstantiated measles, mumps and rubella (MMR)
autism scare led to a decline in MMR vaccination rates.6
The most recent national vaccine attitudes survey conducted
in 2001 found that the majority of parents with incompletely
immunised children (70%) were concerned about vaccine side
effects.7 This was particularly evident after the suspension of
CSL Fluvax because of a higher rate of febrile convulsions in
children. Our primary source of information regarding vaccination
uptake – the Australian Childhood Immunisation Register (ACIR)
– maintains the vaccination history of children up to seven years
of age. However, ACIR does not quantify the attitudes, beliefs
and concerns of individuals that underlie vaccination uptake and
objection.
Background and objectives
Vaccine hesitancy is a public health concern. The objectives
of this article were to describe Australian parents’ attitudes,
behaviours and concerns about vaccination, determine
the factors associated with vaccination non-compliance,
and provide sources of vaccination information for general
practitioners (GPs).
Methods
We conducted a nationally representative online survey of
Australian parents in 2012. We determined associations
between demographic and vaccination attitudes and behaviour.
Results
The 452 respondents were parents of children aged <18
years. Despite 92% reporting their child as up to date with
vaccination, 52% had concerns. Factors associated with non-
compliance included ‘disagreeing that vaccines are safe’ (odds
ratio [OR]: 2.79; 95% confidence interval [CI]: 1.00–7.76) and
‘obtaining information from alternative health practitioners’
(OR: 6.54; 95% CI: 1.71-25.00). The vast majority (83%) obtained
vaccination information from their GPs.
Discussion
GPs have pivotal roles in addressing concerns regarding
vaccination. Education and communication with parents will
improve their knowledge and trust in vaccination, thereby
improving vaccination compliance.
V
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

146
RESEARCH CHILDHOOD VACCINATIONS
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017 © The Royal Australian College of General Practitioners 2017
Therefore, the aims of this study were to
identify Australian parents’ or caregivers’
(hereafter called ‘parents’):
• levels of support for the NIPS
• the proportion of parents with concerns
about vaccination
• use and influence of sources of
information
• associations between vaccination
attitudes and compliance with NIPS.
Methods
Study design
This study was a nationally representative
cross-sectional online survey of the
Australian general population aged ≥18
years. The survey was a collaboration
between the National Centre for
Immunisation Research and Surveillance
(NCIRS) and a documentary production
company, Genepool Productions. In this
study, we analysed data from parents of
children aged <18 years only.
Development of questionnaire
We developed a questionnaire based on
the following standardised national and
international surveys: New South Wales
Child Health Survey, New South Wales
Health Adult Health Survey, Queensland
Health Survey, US National Immunization
Healthstyles and UK Wave Survey. We were
also informed by qualitative and quantitative
research previously undertaken by the
authors of this study.8,9 Respondents were
asked if they were a parent, along with
other demographic questions. We then
identified:
• support levels for adult and childhood
vaccination
• concerns about vaccine-preventable
diseases
• perceptions about vaccine safety
• experiences in adverse events following
immunisation (AEFI)
• influenza vaccination status
• vaccination information sources and
their degree of influence on vaccination
decisions
• basic demographics.
Respondents who were current parents
of children aged <18 years answered extra
questions about vaccination attitudes,
vaccination decisions for their child,
their child’s compliance to the NIPS and
influenza vaccination status.
Sampling and data collection
An external research company, Australia
Online Research, recruited participants and
collected data. The sample was based on
an online panel of 100,000 people out of a
total of 5.3 million people who responded
to a national Australia Post survey
distributed to all Australian households.
The company sent unique invitation emails
to 9854 people using stratified sampling
methods to match the Australian census
data so that the demographic distribution
of invitees was comparable to that of the
Australian population. Each respondent
received $2 for a completed survey and
an opportunity to enter a $5000 cash prize
draw.
Australia Online Research is a member of
the Australian Market and Social Research
Society, and is required to abide by the
Code of Professional Behaviour (Code).10
Similarly to the Human Research Ethics
Committee, the Code requires the company
to have informed consent; to state that the
study is entirely voluntary and participants
can withdraw from the study at any time;
that the data collected are non-identifiable;
and that the data are stored appropriately.
Data analysis
We used SPSS 18 to analyse the data.
We generated descriptive statistics and
conducted chi-square tests of associations
between demographics and vaccination
attitudes, and between vaccination support
and compliance with the NIPS. Variables
with P values <0.25 were put into a
multivariate logistic regression model to
determine the factors associated with
vaccination support and compliance with
the NIPS.
Results
The cross-sectional online survey was
conducted between 18 and 26 April 2012.
In total, 1324 out of 9854 people completed
the survey (13.4%), of whom, 452 (34%)
were parents with children <18 years of
age. Forty-four per cent of respondents
were aged between 35 and 44 years; 43%
had a university degree; 392 (87%) were
primary caregivers; and 51% were female.
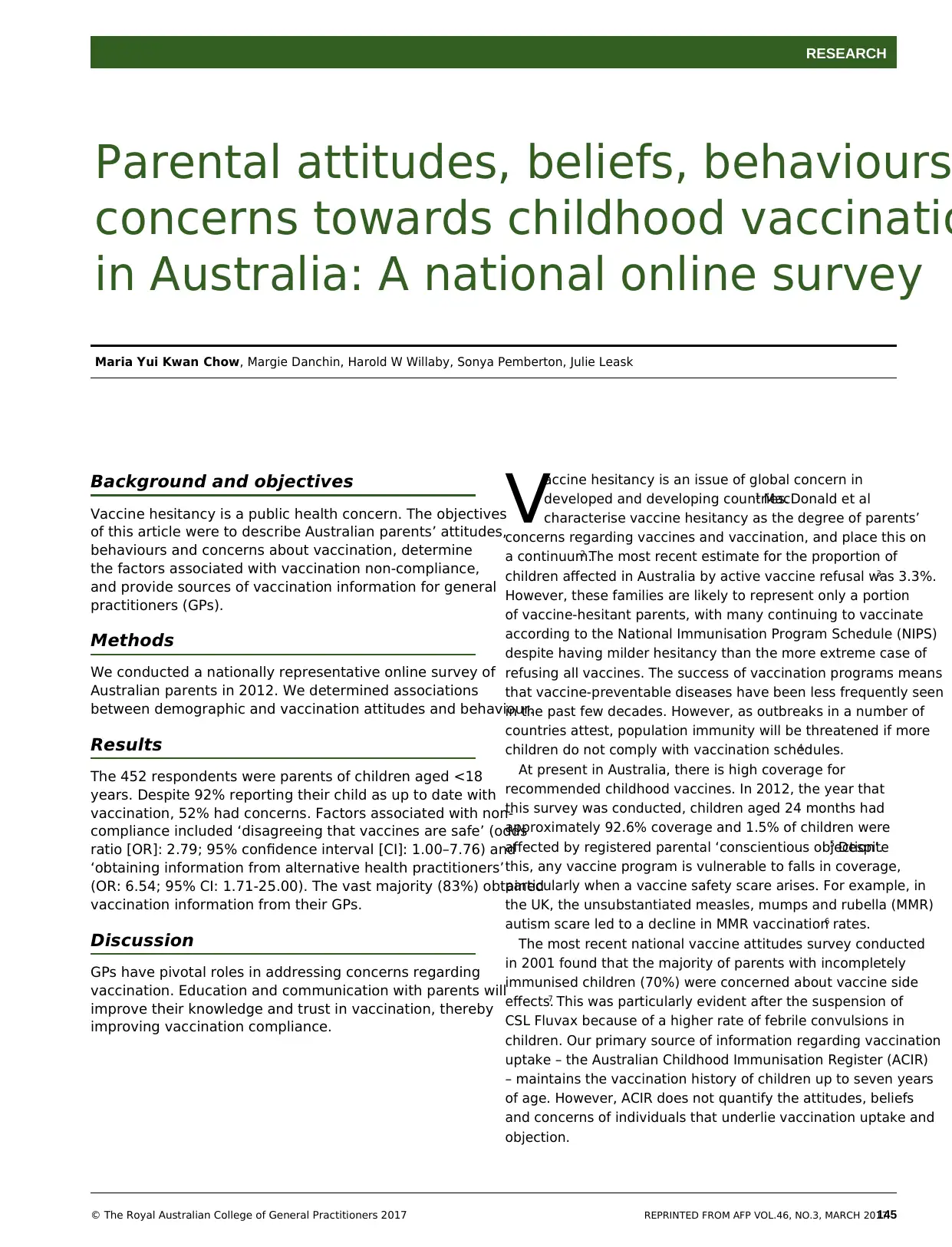
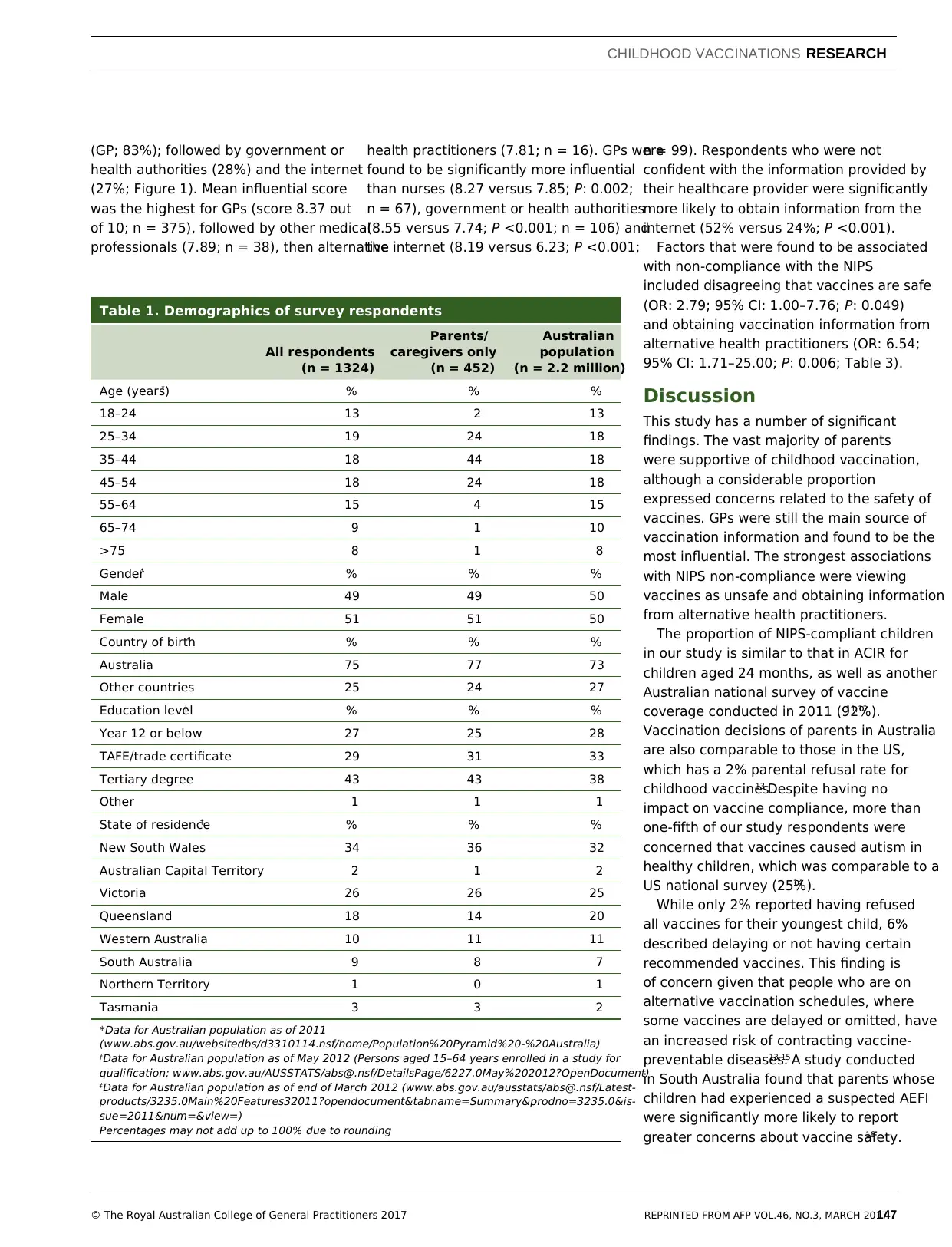
Table 1 shows the demographics of the
respondents and those of the Australian
population. The demographics of the parent
respondents were not significantly different
from those in the Australian population.
According to parental reports for their
youngest child, 92% were fully immunised
according to the NIPS, 6% were under-
immunised or unimmunised and 2% were
unsure. For the influenza vaccine, 23%
indicated that their child received the
vaccine in 2011 and 13% of parents recalled
having a family member or a friend who
previously reported an AEFI (any type of
vaccine).
The vast majority of parents were
supportive of vaccination in children: 68%
strongly support, 26% generally support,
2% neutral, 2% generally oppose and
2% strongly oppose. When asked about
vaccination decisions for their youngest
child, 48% allowed their child to receive all
recommended vaccines with no concerns;
38% allowed for all vaccines but with few
concerns; 6% allowed for all vaccines but
with several concerns; 6% allowed some
vaccines only or to delay some; and 2% did
not allow their child to have any vaccines.
Parents’ perceptions towards vaccine-
preventable diseases varied. More than half
were very (26%) or fairly (27%) concerned,
35% were somewhat concerned and 12%
were not concerned. Perceptions towards
vaccine-preventable diseases did not differ
across primary and non-primary caregivers
(P: 0.49), nor across respondent age,
gender or education levels. Table 2 shows
parental attitudes towards vaccination.
While 90% of parents agreed that
vaccinations were safe for children, 23%
were concerned that vaccines were not
tested enough for safety, 21% believed that
vaccines could cause autism and 22% were
also concerned that their child’s immune
system could be weakened by vaccinations.
The vast majority of parents obtained
information from their general practitioner
RESEARCH CHILDHOOD VACCINATIONS
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017 © The Royal Australian College of General Practitioners 2017
Therefore, the aims of this study were to
identify Australian parents’ or caregivers’
(hereafter called ‘parents’):
• levels of support for the NIPS
• the proportion of parents with concerns
about vaccination
• use and influence of sources of
information
• associations between vaccination
attitudes and compliance with NIPS.
Methods
Study design
This study was a nationally representative
cross-sectional online survey of the
Australian general population aged ≥18
years. The survey was a collaboration
between the National Centre for
Immunisation Research and Surveillance
(NCIRS) and a documentary production
company, Genepool Productions. In this
study, we analysed data from parents of
children aged <18 years only.
Development of questionnaire
We developed a questionnaire based on
the following standardised national and
international surveys: New South Wales
Child Health Survey, New South Wales
Health Adult Health Survey, Queensland
Health Survey, US National Immunization
Healthstyles and UK Wave Survey. We were
also informed by qualitative and quantitative
research previously undertaken by the
authors of this study.8,9 Respondents were
asked if they were a parent, along with
other demographic questions. We then
identified:
• support levels for adult and childhood
vaccination
• concerns about vaccine-preventable
diseases
• perceptions about vaccine safety
• experiences in adverse events following
immunisation (AEFI)
• influenza vaccination status
• vaccination information sources and
their degree of influence on vaccination
decisions
• basic demographics.
Respondents who were current parents
of children aged <18 years answered extra
questions about vaccination attitudes,
vaccination decisions for their child,
their child’s compliance to the NIPS and
influenza vaccination status.
Sampling and data collection
An external research company, Australia
Online Research, recruited participants and
collected data. The sample was based on
an online panel of 100,000 people out of a
total of 5.3 million people who responded
to a national Australia Post survey
distributed to all Australian households.
The company sent unique invitation emails
to 9854 people using stratified sampling
methods to match the Australian census
data so that the demographic distribution
of invitees was comparable to that of the
Australian population. Each respondent
received $2 for a completed survey and
an opportunity to enter a $5000 cash prize
draw.
Australia Online Research is a member of
the Australian Market and Social Research
Society, and is required to abide by the
Code of Professional Behaviour (Code).10
Similarly to the Human Research Ethics
Committee, the Code requires the company
to have informed consent; to state that the
study is entirely voluntary and participants
can withdraw from the study at any time;
that the data collected are non-identifiable;
and that the data are stored appropriately.
Data analysis
We used SPSS 18 to analyse the data.
We generated descriptive statistics and
conducted chi-square tests of associations
between demographics and vaccination
attitudes, and between vaccination support
and compliance with the NIPS. Variables
with P values <0.25 were put into a
multivariate logistic regression model to
determine the factors associated with
vaccination support and compliance with
the NIPS.
Results
The cross-sectional online survey was
conducted between 18 and 26 April 2012.
In total, 1324 out of 9854 people completed
the survey (13.4%), of whom, 452 (34%)
were parents with children <18 years of
age. Forty-four per cent of respondents
were aged between 35 and 44 years; 43%
had a university degree; 392 (87%) were
primary caregivers; and 51% were female.
Table 1 shows the demographics of the
respondents and those of the Australian
population. The demographics of the parent
respondents were not significantly different
from those in the Australian population.
According to parental reports for their
youngest child, 92% were fully immunised
according to the NIPS, 6% were under-
immunised or unimmunised and 2% were
unsure. For the influenza vaccine, 23%
indicated that their child received the
vaccine in 2011 and 13% of parents recalled
having a family member or a friend who
previously reported an AEFI (any type of
vaccine).
The vast majority of parents were
supportive of vaccination in children: 68%
strongly support, 26% generally support,
2% neutral, 2% generally oppose and
2% strongly oppose. When asked about
vaccination decisions for their youngest
child, 48% allowed their child to receive all
recommended vaccines with no concerns;
38% allowed for all vaccines but with few
concerns; 6% allowed for all vaccines but
with several concerns; 6% allowed some
vaccines only or to delay some; and 2% did
not allow their child to have any vaccines.
Parents’ perceptions towards vaccine-
preventable diseases varied. More than half
were very (26%) or fairly (27%) concerned,
35% were somewhat concerned and 12%
were not concerned. Perceptions towards
vaccine-preventable diseases did not differ
across primary and non-primary caregivers
(P: 0.49), nor across respondent age,
gender or education levels. Table 2 shows
parental attitudes towards vaccination.
While 90% of parents agreed that
vaccinations were safe for children, 23%
were concerned that vaccines were not
tested enough for safety, 21% believed that
vaccines could cause autism and 22% were
also concerned that their child’s immune
system could be weakened by vaccinations.
The vast majority of parents obtained
information from their general practitioner
147
CHILDHOOD VACCINATIONS RESEARCH
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017© The Royal Australian College of General Practitioners 2017
n = 99). Respondents who were not
confident with the information provided by
their healthcare provider were significantly
more likely to obtain information from the
internet (52% versus 24%; P <0.001).
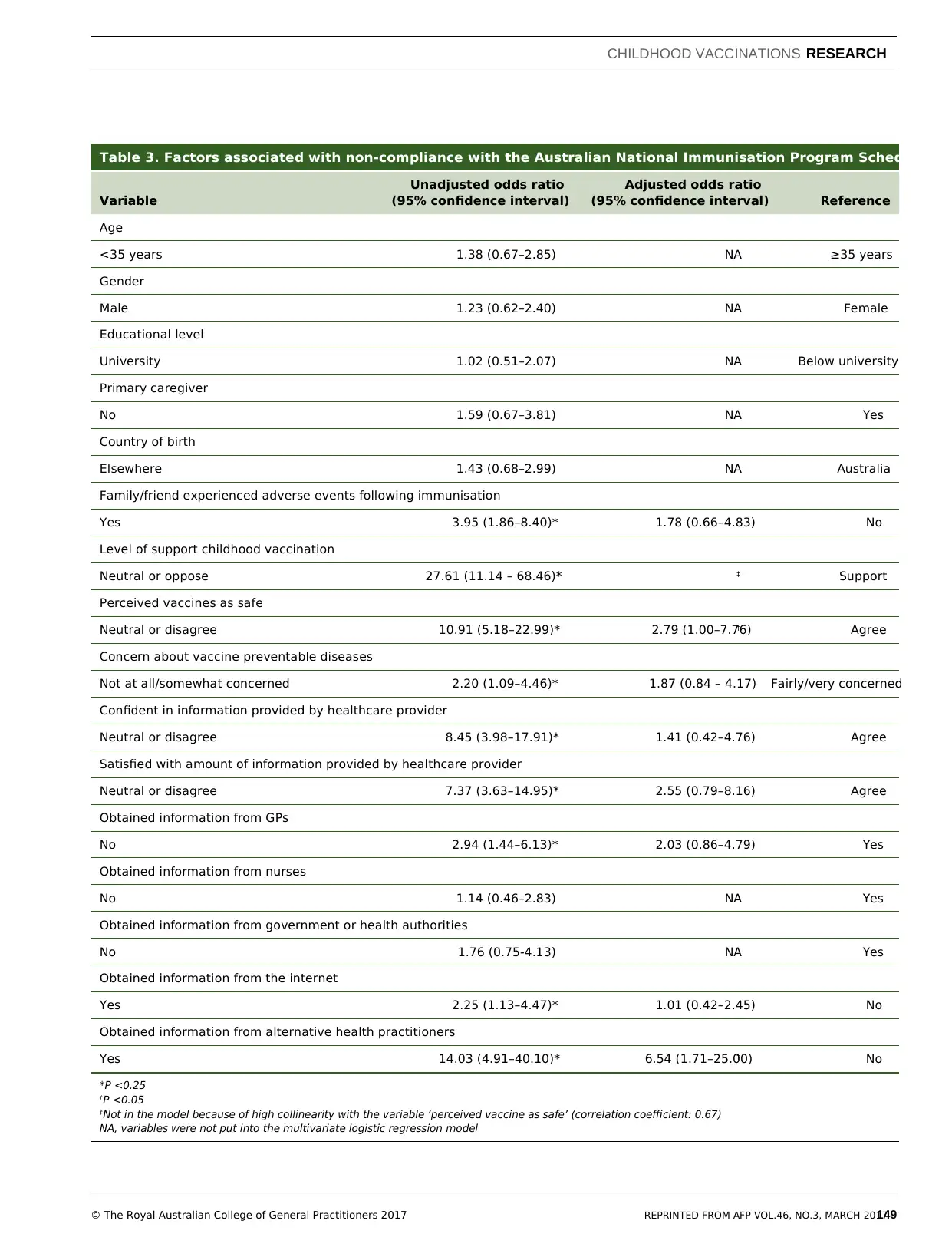
Factors that were found to be associated
with non-compliance with the NIPS
included disagreeing that vaccines are safe
(OR: 2.79; 95% CI: 1.00–7.76; P: 0.049)
and obtaining vaccination information from
alternative health practitioners (OR: 6.54;
95% CI: 1.71–25.00; P: 0.006; Table 3).
Discussion
This study has a number of significant
findings. The vast majority of parents
were supportive of childhood vaccination,
although a considerable proportion
expressed concerns related to the safety of
vaccines. GPs were still the main source of
vaccination information and found to be the
most influential. The strongest associations
with NIPS non-compliance were viewing
vaccines as unsafe and obtaining information
from alternative health practitioners.
The proportion of NIPS-compliant children
in our study is similar to that in ACIR for
children aged 24 months, as well as another
Australian national survey of vaccine
coverage conducted in 2011 (92%).11,12
Vaccination decisions of parents in Australia
are also comparable to those in the US,
which has a 2% parental refusal rate for
childhood vaccines.13 Despite having no
impact on vaccine compliance, more than
one-fifth of our study respondents were
concerned that vaccines caused autism in
healthy children, which was comparable to a
US national survey (25%).14
While only 2% reported having refused
all vaccines for their youngest child, 6%
described delaying or not having certain
recommended vaccines. This finding is
of concern given that people who are on
alternative vaccination schedules, where
some vaccines are delayed or omitted, have
an increased risk of contracting vaccine-
preventable diseases.13,15 A study conducted
in South Australia found that parents whose
children had experienced a suspected AEFI
were significantly more likely to report
greater concerns about vaccine safety.16
Table 1. Demographics of survey respondents
All respondents
(n = 1324)
Parents/
caregivers only
(n = 452)
Australian
population
(n = 2.2 million)
Age (years)* % % %
18–24 13 2 13
25–34 19 24 18
35–44 18 44 18
45–54 18 24 18
55–64 15 4 15
65–74 9 1 10
>75 8 1 8
Gender* % % %
Male 49 49 50
Female 51 51 50
Country of birth* % % %
Australia 75 77 73
Other countries 25 24 27
Education level† % % %
Year 12 or below 27 25 28
TAFE/trade certificate 29 31 33
Tertiary degree 43 43 38
Other 1 1 1
State of residence‡ % % %
New South Wales 34 36 32
Australian Capital Territory 2 1 2
Victoria 26 26 25
Queensland 18 14 20
Western Australia 10 11 11
South Australia 9 8 7
Northern Territory 1 0 1
Tasmania 3 3 2
*Data for Australian population as of 2011
(www.abs.gov.au/websitedbs/d3310114.nsf/home/Population%20Pyramid%20-%20Australia)
†Data for Australian population as of May 2012 (Persons aged 15–64 years enrolled in a study for
qualification; www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/6227.0May%202012?OpenDocument)
‡Data for Australian population as of end of March 2012 (www.abs.gov.au/ausstats/abs@.nsf/Latest-
products/3235.0Main%20Features32011?opendocument&tabname=Summary&prodno=3235.0&is-
sue=2011&num=&view=)
Percentages may not add up to 100% due to rounding
(GP; 83%); followed by government or
health authorities (28%) and the internet
(27%; Figure 1). Mean influential score
was the highest for GPs (score 8.37 out
of 10; n = 375), followed by other medical
professionals (7.89; n = 38), then alternative
health practitioners (7.81; n = 16). GPs were
found to be significantly more influential
than nurses (8.27 versus 7.85; P: 0.002;
n = 67), government or health authorities
(8.55 versus 7.74; P <0.001; n = 106) and
the internet (8.19 versus 6.23; P <0.001;
CHILDHOOD VACCINATIONS RESEARCH
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017© The Royal Australian College of General Practitioners 2017
n = 99). Respondents who were not
confident with the information provided by
their healthcare provider were significantly
more likely to obtain information from the
internet (52% versus 24%; P <0.001).
Factors that were found to be associated
with non-compliance with the NIPS
included disagreeing that vaccines are safe
(OR: 2.79; 95% CI: 1.00–7.76; P: 0.049)
and obtaining vaccination information from
alternative health practitioners (OR: 6.54;
95% CI: 1.71–25.00; P: 0.006; Table 3).
Discussion
This study has a number of significant
findings. The vast majority of parents
were supportive of childhood vaccination,
although a considerable proportion
expressed concerns related to the safety of
vaccines. GPs were still the main source of
vaccination information and found to be the
most influential. The strongest associations
with NIPS non-compliance were viewing
vaccines as unsafe and obtaining information
from alternative health practitioners.
The proportion of NIPS-compliant children
in our study is similar to that in ACIR for
children aged 24 months, as well as another
Australian national survey of vaccine
coverage conducted in 2011 (92%).11,12
Vaccination decisions of parents in Australia
are also comparable to those in the US,
which has a 2% parental refusal rate for
childhood vaccines.13 Despite having no
impact on vaccine compliance, more than
one-fifth of our study respondents were
concerned that vaccines caused autism in
healthy children, which was comparable to a
US national survey (25%).14
While only 2% reported having refused
all vaccines for their youngest child, 6%
described delaying or not having certain
recommended vaccines. This finding is
of concern given that people who are on
alternative vaccination schedules, where
some vaccines are delayed or omitted, have
an increased risk of contracting vaccine-
preventable diseases.13,15 A study conducted
in South Australia found that parents whose
children had experienced a suspected AEFI
were significantly more likely to report
greater concerns about vaccine safety.16
Table 1. Demographics of survey respondents
All respondents
(n = 1324)
Parents/
caregivers only
(n = 452)
Australian
population
(n = 2.2 million)
Age (years)* % % %
18–24 13 2 13
25–34 19 24 18
35–44 18 44 18
45–54 18 24 18
55–64 15 4 15
65–74 9 1 10
>75 8 1 8
Gender* % % %
Male 49 49 50
Female 51 51 50
Country of birth* % % %
Australia 75 77 73
Other countries 25 24 27
Education level† % % %
Year 12 or below 27 25 28
TAFE/trade certificate 29 31 33
Tertiary degree 43 43 38
Other 1 1 1
State of residence‡ % % %
New South Wales 34 36 32
Australian Capital Territory 2 1 2
Victoria 26 26 25
Queensland 18 14 20
Western Australia 10 11 11
South Australia 9 8 7
Northern Territory 1 0 1
Tasmania 3 3 2
*Data for Australian population as of 2011
(www.abs.gov.au/websitedbs/d3310114.nsf/home/Population%20Pyramid%20-%20Australia)
†Data for Australian population as of May 2012 (Persons aged 15–64 years enrolled in a study for
qualification; www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/6227.0May%202012?OpenDocument)
‡Data for Australian population as of end of March 2012 (www.abs.gov.au/ausstats/abs@.nsf/Latest-
products/3235.0Main%20Features32011?opendocument&tabname=Summary&prodno=3235.0&is-
sue=2011&num=&view=)
Percentages may not add up to 100% due to rounding
(GP; 83%); followed by government or
health authorities (28%) and the internet
(27%; Figure 1). Mean influential score
was the highest for GPs (score 8.37 out
of 10; n = 375), followed by other medical
professionals (7.89; n = 38), then alternative
health practitioners (7.81; n = 16). GPs were
found to be significantly more influential
than nurses (8.27 versus 7.85; P: 0.002;
n = 67), government or health authorities
(8.55 versus 7.74; P <0.001; n = 106) and
the internet (8.19 versus 6.23; P <0.001;
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

148
RESEARCH CHILDHOOD VACCINATIONS
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017 © The Royal Australian College of General Practitioners 2017
However, our study did not find AEFI to be
related to vaccine non-compliance.
This study demonstrates the important
role GPs have in educating parents about
the risks and benefits of vaccination.
Interestingly, <20% of parents obtained
vaccination information from a nurse and,
together with government and health
authorities, they were significantly less
influential than GPs. Communication
frameworks have been developed to assist
healthcare providers to better communicate
with vaccine-hesitant parents.17,18
In medical
communication more broadly, effective
communication strategies depend on
the rapport and trust between GPs and
patients/parents. In addition, studies
have found that a recommendation to
vaccinate from a paediatric provider is
highly associated with uptake.19 However,
for parents who are not having their
children vaccinated, or hesitating to have
them vaccinated, strategies should be of a
guiding style to enable them to elicit their
own motivations to vaccinate, rather than
using a directing or debating format.17,18
GPs are increasingly likely to find parents
presenting with concerns that have been
amplified by internet searches. In this
study, internet use featured as the third
most common source for vaccination
information after ‘government or health
authorities’. Having the internet as a source
of information was associated with a lack
of confidence in information provided
by a healthcare provider. The quality and
reliability of vaccination information on the
internet can be highly variable, with easy
access to anti-vaccination websites.20 A
2012 study of US parents found those who
sought vaccine information on the internet
were more likely to have lower perceptions
of vaccine safety and have a non-medical
exemption to vaccination.21 Thus, GPs have
an important role to play in augmenting the
impact of online information.
In our study, non-compliance with the
NIPS was significantly associated with
obtaining information from alternative health
practitioners. Previous research has also
found that alternative health practitioners
were less likely to support vaccination,22,23
Table 2. Parental concerns, attitudes and behaviour towards vaccination
N = 452
Strongly agreed
or agreed with
statement (%)
I vaccinate my child to protect him/her 92
I believe that vaccinations are safe for children in general 90
I am confident in information provided by healthcare professional 89
I am satisfied with amount of information provided by healthcare
professional
85
I vaccinate my child to help protect the wider community 79
I am concerned about the distress to children of the injection itself 31
I am concerned about the increasing number of vaccines recommended
for children
25
I am concerned that vaccines are not tested enough for safety 23
I am concerned that children get too many vaccines during the first two
years of life
22
I am concerned that a child’s immune system could be weakened by
vaccinations
22
I am concerned that vaccines can cause autism in healthy children 21
I am concerned that vaccines are given to children to prevent diseases
that they are not likely to get
19
I prefer children to get natural immunity from the diseases rather than
immunity from the vaccines
16
I am concerned that vaccines are given to children to prevent diseases
that are not serious
14
Vaccination is not needed because others have vaccinated their children
and diseases have been controlled
7
Figure 1. Sources of vaccination information and its influence among parents
The bars represent the proportion of parents using the source. Multiple options could be selected,
so the total percentage is >100%. The figures above the bars represent the influential scores
(0 = Not influential to 10 = Extremely influential)
10%
20%
30%
40%
50%
60%
70%
80%
90%
0%
GP or family doctor
Goverment or health authorities
Searching for interest
Brochures or medical information
Friends
Nurse
Family members
Media
Other medical professional
Other
Alternative health practitioner
Going to a library
Groups opposed to vaccination
Groups in support of vaccinations
8.37
7.75 6.41
7.19 6.55 7.73 7.53 6.08
7.89 7.65 7.81 7.79 5.62 6.36
RESEARCH CHILDHOOD VACCINATIONS
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017 © The Royal Australian College of General Practitioners 2017
However, our study did not find AEFI to be
related to vaccine non-compliance.
This study demonstrates the important
role GPs have in educating parents about
the risks and benefits of vaccination.
Interestingly, <20% of parents obtained
vaccination information from a nurse and,
together with government and health
authorities, they were significantly less
influential than GPs. Communication
frameworks have been developed to assist
healthcare providers to better communicate
with vaccine-hesitant parents.17,18
In medical
communication more broadly, effective
communication strategies depend on
the rapport and trust between GPs and
patients/parents. In addition, studies
have found that a recommendation to
vaccinate from a paediatric provider is
highly associated with uptake.19 However,
for parents who are not having their
children vaccinated, or hesitating to have
them vaccinated, strategies should be of a
guiding style to enable them to elicit their
own motivations to vaccinate, rather than
using a directing or debating format.17,18
GPs are increasingly likely to find parents
presenting with concerns that have been
amplified by internet searches. In this
study, internet use featured as the third
most common source for vaccination
information after ‘government or health
authorities’. Having the internet as a source
of information was associated with a lack
of confidence in information provided
by a healthcare provider. The quality and
reliability of vaccination information on the
internet can be highly variable, with easy
access to anti-vaccination websites.20 A
2012 study of US parents found those who
sought vaccine information on the internet
were more likely to have lower perceptions
of vaccine safety and have a non-medical
exemption to vaccination.21 Thus, GPs have
an important role to play in augmenting the
impact of online information.
In our study, non-compliance with the
NIPS was significantly associated with
obtaining information from alternative health
practitioners. Previous research has also
found that alternative health practitioners
were less likely to support vaccination,22,23
Table 2. Parental concerns, attitudes and behaviour towards vaccination
N = 452
Strongly agreed
or agreed with
statement (%)
I vaccinate my child to protect him/her 92
I believe that vaccinations are safe for children in general 90
I am confident in information provided by healthcare professional 89
I am satisfied with amount of information provided by healthcare
professional
85
I vaccinate my child to help protect the wider community 79
I am concerned about the distress to children of the injection itself 31
I am concerned about the increasing number of vaccines recommended
for children
25
I am concerned that vaccines are not tested enough for safety 23
I am concerned that children get too many vaccines during the first two
years of life
22
I am concerned that a child’s immune system could be weakened by
vaccinations
22
I am concerned that vaccines can cause autism in healthy children 21
I am concerned that vaccines are given to children to prevent diseases
that they are not likely to get
19
I prefer children to get natural immunity from the diseases rather than
immunity from the vaccines
16
I am concerned that vaccines are given to children to prevent diseases
that are not serious
14
Vaccination is not needed because others have vaccinated their children
and diseases have been controlled
7
Figure 1. Sources of vaccination information and its influence among parents
The bars represent the proportion of parents using the source. Multiple options could be selected,
so the total percentage is >100%. The figures above the bars represent the influential scores
(0 = Not influential to 10 = Extremely influential)
10%
20%
30%
40%
50%
60%
70%
80%
90%
0%
GP or family doctor
Goverment or health authorities
Searching for interest
Brochures or medical information
Friends
Nurse
Family members
Media
Other medical professional
Other
Alternative health practitioner
Going to a library
Groups opposed to vaccination
Groups in support of vaccinations
8.37
7.75 6.41
7.19 6.55 7.73 7.53 6.08
7.89 7.65 7.81 7.79 5.62 6.36
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
149
CHILDHOOD VACCINATIONS RESEARCH
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017© The Royal Australian College of General Practitioners 2017
Table 3. Factors associated with non-compliance with the Australian National Immunisation Program Schedule
Variable
Unadjusted odds ratio
(95% confidence interval)
Adjusted odds ratio
(95% confidence interval) Reference
Age
<35 years 1.38 (0.67–2.85) NA ≥35 years
Gender
Male 1.23 (0.62–2.40) NA Female
Educational level
University 1.02 (0.51–2.07) NA Below university
Primary caregiver
No 1.59 (0.67–3.81) NA Yes
Country of birth
Elsewhere 1.43 (0.68–2.99) NA Australia
Family/friend experienced adverse events following immunisation
Yes 3.95 (1.86–8.40)* 1.78 (0.66–4.83) No
Level of support childhood vaccination
Neutral or oppose 27.61 (11.14 – 68.46)* ‡ Support
Perceived vaccines as safe
Neutral or disagree 10.91 (5.18–22.99)* 2.79 (1.00–7.76)† Agree
Concern about vaccine preventable diseases
Not at all/somewhat concerned 2.20 (1.09–4.46)* 1.87 (0.84 – 4.17) Fairly/very concerned
Confident in information provided by healthcare provider
Neutral or disagree 8.45 (3.98–17.91)* 1.41 (0.42–4.76) Agree
Satisfied with amount of information provided by healthcare provider
Neutral or disagree 7.37 (3.63–14.95)* 2.55 (0.79–8.16) Agree
Obtained information from GPs
No 2.94 (1.44–6.13)* 2.03 (0.86–4.79) Yes
Obtained information from nurses
No 1.14 (0.46–2.83) NA Yes
Obtained information from government or health authorities
No 1.76 (0.75-4.13) NA Yes
Obtained information from the internet
Yes 2.25 (1.13–4.47)* 1.01 (0.42–2.45) No
Obtained information from alternative health practitioners
Yes 14.03 (4.91–40.10)* 6.54 (1.71–25.00)† No
*P <0.25
† P <0.05
‡ Not in the model because of high collinearity with the variable ‘perceived vaccine as safe’ (correlation coefficient: 0.67)
NA, variables were not put into the multivariate logistic regression model
CHILDHOOD VACCINATIONS RESEARCH
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017© The Royal Australian College of General Practitioners 2017
Table 3. Factors associated with non-compliance with the Australian National Immunisation Program Schedule
Variable
Unadjusted odds ratio
(95% confidence interval)
Adjusted odds ratio
(95% confidence interval) Reference
Age
<35 years 1.38 (0.67–2.85) NA ≥35 years
Gender
Male 1.23 (0.62–2.40) NA Female
Educational level
University 1.02 (0.51–2.07) NA Below university
Primary caregiver
No 1.59 (0.67–3.81) NA Yes
Country of birth
Elsewhere 1.43 (0.68–2.99) NA Australia
Family/friend experienced adverse events following immunisation
Yes 3.95 (1.86–8.40)* 1.78 (0.66–4.83) No
Level of support childhood vaccination
Neutral or oppose 27.61 (11.14 – 68.46)* ‡ Support
Perceived vaccines as safe
Neutral or disagree 10.91 (5.18–22.99)* 2.79 (1.00–7.76)† Agree
Concern about vaccine preventable diseases
Not at all/somewhat concerned 2.20 (1.09–4.46)* 1.87 (0.84 – 4.17) Fairly/very concerned
Confident in information provided by healthcare provider
Neutral or disagree 8.45 (3.98–17.91)* 1.41 (0.42–4.76) Agree
Satisfied with amount of information provided by healthcare provider
Neutral or disagree 7.37 (3.63–14.95)* 2.55 (0.79–8.16) Agree
Obtained information from GPs
No 2.94 (1.44–6.13)* 2.03 (0.86–4.79) Yes
Obtained information from nurses
No 1.14 (0.46–2.83) NA Yes
Obtained information from government or health authorities
No 1.76 (0.75-4.13) NA Yes
Obtained information from the internet
Yes 2.25 (1.13–4.47)* 1.01 (0.42–2.45) No
Obtained information from alternative health practitioners
Yes 14.03 (4.91–40.10)* 6.54 (1.71–25.00)† No
*P <0.25
† P <0.05
‡ Not in the model because of high collinearity with the variable ‘perceived vaccine as safe’ (correlation coefficient: 0.67)
NA, variables were not put into the multivariate logistic regression model

150
RESEARCH CHILDHOOD VACCINATIONS
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017 © The Royal Australian College of General Practitioners 2017
and those who consulted alternative health
practitioners were significantly less likely
to receive recommended vaccines.24 Given
that this study is cross-sectional, we were
not able to determine whether parents
already concerned about vaccination look
to alternative health practitioners to answer
questions not addressed by their doctor, or
whether they identify more strongly with
the health model offered by alternative
health practitioners.
GPs can play a role in educating parents
and understanding their reasons for
approaching alternative health practitioners
without being judgemental. Wardle et al
also suggest disciplining health practitioners
and organisations through current legislative
arrangements for those who promote
false and misleading information about
vaccination.25 Financial incentives have been
proven to improve childhood vaccination
uptake.26 However, there is insufficient
quality evidence in relation to withholding
these payments (monetary sanctions) as a
way of improving compliance.
Limitations
Our study has some limitations. First,
there was a low response rate to the
initial invitation (13%) and the survey
was only weighted for the whole sample
group (n = 1324). Our study has a
higher proportion of respondents in the
35–44 years age group than in the general
population; this was expected because we
only included parents of children aged <18
years. Other than the age group distribution,
the demographics of the respondents were
comparable with the Australian population.
Second, the survey was cross-sectional; it
was not possible to determine the causal
relationship between the factors and
dependent variables. A prospective study
measuring attitudes then uptake would
provide more information on the reasons
underpinning parents’ vaccination decisions.
Third, vaccination status was ascertained
by parental report. A systematic review
found that parental recall overestimated
complete vaccination when compared
with provider records.27 Despite this,
the reported full vaccination and vaccine
objection rates were similar to nationally
reported rates (1.68% ACIR recorded
conscientious objection versus 2% in
our sample; 92.5% full compliance with
the NIPS at aged 2 years on ACIR versus
92% reporting their youngest child is fully
vaccinated in our study).28 Ideally, we
would have been able to verify individual
vaccine uptake with ACIR data – a
methodological recommendation for future
studies to pursue.
Conclusions
The majority of parents in this study
reported compliance and strong support
for the NIPS. Nevertheless, over half of
all parents or caregivers in this study
expressed some degree of concern
regarding vaccination of their child. GPs
are the most used and influential source
of information. They have a pivotal role in
communicating with parents regarding
childhood vaccinations and in providing
clear, evidence-based vaccine information
to help guide parents’ decision-making.
Implications for general
practice
Parents rely on GPs for vaccination
information more than any other
information sources. GPs can play an
active role in discussing and clarifying
parental concerns about vaccination.
They can use evidence-based vaccination
resources, such as fact sheets and
decision aids, and communication
frameworks to assist better
communication with parents.
Authors
Maria Yui Kwan Chow MIPH, PhD, Research Officer,
National Centre for Immunisation Research and
Surveillance, Kids Research Institute, The Children’s
Hospital at Westmead, Westmead, NSW; Discipline
of Paediatrics and Child Health, Sydney Medical
School, The Children’s Hospital at Westmead,
Westmead, NSW. ycho3792@uni.sydney.edu.au
Margie Danchin MBBS, FRACP, PhD, Senior Fellow,
Vaccine and Immunisation (VIRGo) and Rotavirus
Research Group, Murdoch Children’s Research
Institute, Parkville, Vic; School of Population and
Global health and Department of Paediatrics,
University of Melbourne, Parkville, Vic
Harold W Willaby BSc, MBA, PhD, Research Officer,
School of Public Health, Sydney Medical School, The
University of Sydney, Sydney, NSW
Sonya Pemberton, Creative Director, Genepool
Productions, Port Melbourne, Vic
Julie Leask Dip Health Sci, MPH, PhD, Associate
Professor, National Centre for Immunisation Research
and Surveillance, Kids Research Institute, The
Children’s Hospital at Westmead, Westmead, NSW;
School of Public Health, Sydney Medical School, The
University of Sydney, Sydney NSW
Competing interests: The survey was funded by
Genepool Productions, SBS Australia and Screen
Australia with in-kind contribution from Australia
Online Research, the National Centre for Immunisation
Research and Surveillance (NCIRS). Julie Leask is
supported by a National Health and Medical Research
Council (NHMRC) Career Development Fellowship.
NCIRS is supported by the Department of Health
and Ageing, the NSW Department of Health and
the Children’s Hospital at Westmead. The data was
collected for use by the NCIRS, and to inform the
television documentary Jabbed: Love, fear and
vaccines broadcast on SBS on 26 May 2013. The
documentary can be viewed here at www.sbs.com.
au/ondemand/video/30004803525/Jabbed-Love-Fear-
And-Vaccines
Provenance and peer review: Not commissioned,
externally peer reviewed.
Acknowledgements
We would also like to thank NCIRS staff for providing
comments on data analysis.
References
1. Dube E, Laberge C, Guay M, Bramadat P, Roy R,
Bettinger J. Vaccine hesitancy: An overview. Hum
Vaccin Immunother 2013;9(8):1763–73.
2. MacDonald NE. Vaccine hesitancy:
Definition, scope and determinants. Vaccine
2015;33(34):4161–64.
3. Beard FH, Hull BP, Leask J, Dey A, McIntyre PB.
Trends and patterns in vaccination objection,
Australia, 2002–2013. Med J Aust 2016;204(7):275.
4. Plotkin SA OW, Offit PA, editors. Vaccines. 6th
edn. Philadelphia: Saunders Elsevier, 2013.
5. Department of Health. Immunise Australia
Program Vaccination Data. Canberra: DoH, 2015.
Available at www.immunise.health.gov.au/internet/
immunise/publishing.nsf/Content/vaccination-data
[Accessed 28 September 2016]
6. Dawson B, Apte SH. Measles outbreaks in
Australia: Obstacles to vaccination. Aust N Z J
Public Health. 2015;39(2):104–06.
7. Lawrence GL, Hull B, MacIntyre CR, McIntyre
PB. Reasons for incomplete immunisation among
Australian children: A national survey of parents.
Aust Fam Physician 2004;33(7):568–71.
8. Leask J, Chapman S, Hawe P, Burgess M. What
maintains parental support for vaccination when
challenged by anti-vaccination messages? A
qualitative study. Vaccine 2006;24(49-50):7238−45.
9. Chow MY, King C, Booy R, Leask J. Parents’
intentions and behaviour regarding seasonal
influenza vaccination for their children: A survey in
child-care centres in Sydney, Australia. J Ped Infect
Dis 2012;7(2):89–96
10. Australian Market & Social Research Society.
Code of professional behaviour. Glebe, NSW:
AMSRS, 2016. Available at www.amsrs.com.
au/professional-standards/code-of-professional-
behaviour [Accessed 1 December 2016].
RESEARCH CHILDHOOD VACCINATIONS
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017 © The Royal Australian College of General Practitioners 2017
and those who consulted alternative health
practitioners were significantly less likely
to receive recommended vaccines.24 Given
that this study is cross-sectional, we were
not able to determine whether parents
already concerned about vaccination look
to alternative health practitioners to answer
questions not addressed by their doctor, or
whether they identify more strongly with
the health model offered by alternative
health practitioners.
GPs can play a role in educating parents
and understanding their reasons for
approaching alternative health practitioners
without being judgemental. Wardle et al
also suggest disciplining health practitioners
and organisations through current legislative
arrangements for those who promote
false and misleading information about
vaccination.25 Financial incentives have been
proven to improve childhood vaccination
uptake.26 However, there is insufficient
quality evidence in relation to withholding
these payments (monetary sanctions) as a
way of improving compliance.
Limitations
Our study has some limitations. First,
there was a low response rate to the
initial invitation (13%) and the survey
was only weighted for the whole sample
group (n = 1324). Our study has a
higher proportion of respondents in the
35–44 years age group than in the general
population; this was expected because we
only included parents of children aged <18
years. Other than the age group distribution,
the demographics of the respondents were
comparable with the Australian population.
Second, the survey was cross-sectional; it
was not possible to determine the causal
relationship between the factors and
dependent variables. A prospective study
measuring attitudes then uptake would
provide more information on the reasons
underpinning parents’ vaccination decisions.
Third, vaccination status was ascertained
by parental report. A systematic review
found that parental recall overestimated
complete vaccination when compared
with provider records.27 Despite this,
the reported full vaccination and vaccine
objection rates were similar to nationally
reported rates (1.68% ACIR recorded
conscientious objection versus 2% in
our sample; 92.5% full compliance with
the NIPS at aged 2 years on ACIR versus
92% reporting their youngest child is fully
vaccinated in our study).28 Ideally, we
would have been able to verify individual
vaccine uptake with ACIR data – a
methodological recommendation for future
studies to pursue.
Conclusions
The majority of parents in this study
reported compliance and strong support
for the NIPS. Nevertheless, over half of
all parents or caregivers in this study
expressed some degree of concern
regarding vaccination of their child. GPs
are the most used and influential source
of information. They have a pivotal role in
communicating with parents regarding
childhood vaccinations and in providing
clear, evidence-based vaccine information
to help guide parents’ decision-making.
Implications for general
practice
Parents rely on GPs for vaccination
information more than any other
information sources. GPs can play an
active role in discussing and clarifying
parental concerns about vaccination.
They can use evidence-based vaccination
resources, such as fact sheets and
decision aids, and communication
frameworks to assist better
communication with parents.
Authors
Maria Yui Kwan Chow MIPH, PhD, Research Officer,
National Centre for Immunisation Research and
Surveillance, Kids Research Institute, The Children’s
Hospital at Westmead, Westmead, NSW; Discipline
of Paediatrics and Child Health, Sydney Medical
School, The Children’s Hospital at Westmead,
Westmead, NSW. ycho3792@uni.sydney.edu.au
Margie Danchin MBBS, FRACP, PhD, Senior Fellow,
Vaccine and Immunisation (VIRGo) and Rotavirus
Research Group, Murdoch Children’s Research
Institute, Parkville, Vic; School of Population and
Global health and Department of Paediatrics,
University of Melbourne, Parkville, Vic
Harold W Willaby BSc, MBA, PhD, Research Officer,
School of Public Health, Sydney Medical School, The
University of Sydney, Sydney, NSW
Sonya Pemberton, Creative Director, Genepool
Productions, Port Melbourne, Vic
Julie Leask Dip Health Sci, MPH, PhD, Associate
Professor, National Centre for Immunisation Research
and Surveillance, Kids Research Institute, The
Children’s Hospital at Westmead, Westmead, NSW;
School of Public Health, Sydney Medical School, The
University of Sydney, Sydney NSW
Competing interests: The survey was funded by
Genepool Productions, SBS Australia and Screen
Australia with in-kind contribution from Australia
Online Research, the National Centre for Immunisation
Research and Surveillance (NCIRS). Julie Leask is
supported by a National Health and Medical Research
Council (NHMRC) Career Development Fellowship.
NCIRS is supported by the Department of Health
and Ageing, the NSW Department of Health and
the Children’s Hospital at Westmead. The data was
collected for use by the NCIRS, and to inform the
television documentary Jabbed: Love, fear and
vaccines broadcast on SBS on 26 May 2013. The
documentary can be viewed here at www.sbs.com.
au/ondemand/video/30004803525/Jabbed-Love-Fear-
And-Vaccines
Provenance and peer review: Not commissioned,
externally peer reviewed.
Acknowledgements
We would also like to thank NCIRS staff for providing
comments on data analysis.
References
1. Dube E, Laberge C, Guay M, Bramadat P, Roy R,
Bettinger J. Vaccine hesitancy: An overview. Hum
Vaccin Immunother 2013;9(8):1763–73.
2. MacDonald NE. Vaccine hesitancy:
Definition, scope and determinants. Vaccine
2015;33(34):4161–64.
3. Beard FH, Hull BP, Leask J, Dey A, McIntyre PB.
Trends and patterns in vaccination objection,
Australia, 2002–2013. Med J Aust 2016;204(7):275.
4. Plotkin SA OW, Offit PA, editors. Vaccines. 6th
edn. Philadelphia: Saunders Elsevier, 2013.
5. Department of Health. Immunise Australia
Program Vaccination Data. Canberra: DoH, 2015.
Available at www.immunise.health.gov.au/internet/
immunise/publishing.nsf/Content/vaccination-data
[Accessed 28 September 2016]
6. Dawson B, Apte SH. Measles outbreaks in
Australia: Obstacles to vaccination. Aust N Z J
Public Health. 2015;39(2):104–06.
7. Lawrence GL, Hull B, MacIntyre CR, McIntyre
PB. Reasons for incomplete immunisation among
Australian children: A national survey of parents.
Aust Fam Physician 2004;33(7):568–71.
8. Leask J, Chapman S, Hawe P, Burgess M. What
maintains parental support for vaccination when
challenged by anti-vaccination messages? A
qualitative study. Vaccine 2006;24(49-50):7238−45.
9. Chow MY, King C, Booy R, Leask J. Parents’
intentions and behaviour regarding seasonal
influenza vaccination for their children: A survey in
child-care centres in Sydney, Australia. J Ped Infect
Dis 2012;7(2):89–96
10. Australian Market & Social Research Society.
Code of professional behaviour. Glebe, NSW:
AMSRS, 2016. Available at www.amsrs.com.
au/professional-standards/code-of-professional-
behaviour [Accessed 1 December 2016].
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

151
CHILDHOOD VACCINATIONS RESEARCH
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017© The Royal Australian College of General Practitioners 2017
11. Berry JG, Gold MS, Ryan P, Duszynski KM,
Braunack-Mayer AJ, Vaccine Assessment Using
Linked Data Working Group. Public perspectives
on consent for the linkage of data to evaluate
vaccine safety. Vaccine 2012;30(28):4167–74.
12. Hull B, Dey A, Mahajan D, Menzies R, McIntyre
PB. Immunisation coverage annual report, 2009.
Commun Dis Intell 2011;35(2):132–48.
13. Dempsey AF, Schaffer S, Singer D, Butchart
A, Davis M, Freed GL. Alternative vaccination
schedule preferences among parents of young
children. Pediatrics 2011;128(5):848–56.
14. Freed GL, Clark SJ, Butchart AT, Singer DC, Davis
MM. Parental vaccine safety concerns in 2009.
Pediatrics 2010;125(4):654–59.
15. Rowhani-Rahbar A, Fireman B, Lewis E,
et al. Effect of age on the risk of fever and
seizures following immunization with measles-
containing vaccines in children. JAMA Pediatrics
2013;167(12):1111–17.
16. Parrella A, Gold M, Marshall H, Braunack-Mayer
A, Baghurst P. Parental perspectives of vaccine
safety and experience of adverse events following
immunisation. Vaccine 2013;31(16):2067–74.
17. Leask J, Kinnersley P, Jackson C, Cheater F,
Bedford H, Rowles G. Communicating with
parents about vaccination: A framework for health
professionals. BMC Pediatr. 2012;12:154.
18. Danchin M, Nolan T. A positive approach to
parents with concerns about vaccination for
the family physician. Aust Fam Physician
2014;43(10):690–94.
19. Opel DJ, Mangione-Smith R, Robinson JD,
Heritage J, et al. The influence of provider
communication behaviors on parental vaccine
acceptance and visit experience. Am J Pub Health
2015:e1–e7
20. Davies P, Chapman S, Leask J. Antivaccination
activists on the world wide web. Arch Dis Child
2002;87(1):22–25.
21. Jones AM, Omer SB, Bednarczyk RA, Halsey
NA, Moulton LH, Salmon DA. Parents’ source
of vaccine information and impact on vaccine
attitudes, beliefs and nonmedical exemptions. Adv
Prev Med 2012;2012:932741.
22. Busse JW, Wilson K, Campbell JB. Attitudes
towards vaccination among chiropractic and
naturopathic students. Vaccine 2008;26(49):
6237-43.
23. Schmidt K, Ernst E. MMR vaccination advice over
the internet. Vaccine 2003;21(11-12):1044−47.
24. Downey L, Tyree PT, Huebner CE, Lafferty WE.
Pediatric vaccination and vaccine-preventable
disease acquisition: Associations with care
by complementary and alternative medicine
providers. Matern Child Health J 2010;14(6):
922–30.
25. Wardle J, Stewart C, Parker M. Jabs and barbs:
Ways to address misleading vaccination and
immunisation information using currently available
strategies. J Law and Med 2013;21(1):159–78.
26. Lawrence GL, MacIntyre CR, Hull PB, McIntyre
PB. Effectiveness of the linkage of child care and
maternity payments to childhood immunisation.
Vaccine 2004;22(17–18):2345–50.
27. Miles M, Ryman TK, Dietz V, Zell E, Luman
ET. Validity of vaccination cards and parental
recall to estimate vaccination coverage: A
systematic review of the literature. Vaccine.
2013;31(12):1560–68.
28. Hull BP. Australian childhood immunisation
coverage. Commun Dis Intell 2014;38(2):E157.
CHILDHOOD VACCINATIONS RESEARCH
REPRINTED FROM AFP VOL.46, NO.3, MARCH 2017© The Royal Australian College of General Practitioners 2017
11. Berry JG, Gold MS, Ryan P, Duszynski KM,
Braunack-Mayer AJ, Vaccine Assessment Using
Linked Data Working Group. Public perspectives
on consent for the linkage of data to evaluate
vaccine safety. Vaccine 2012;30(28):4167–74.
12. Hull B, Dey A, Mahajan D, Menzies R, McIntyre
PB. Immunisation coverage annual report, 2009.
Commun Dis Intell 2011;35(2):132–48.
13. Dempsey AF, Schaffer S, Singer D, Butchart
A, Davis M, Freed GL. Alternative vaccination
schedule preferences among parents of young
children. Pediatrics 2011;128(5):848–56.
14. Freed GL, Clark SJ, Butchart AT, Singer DC, Davis
MM. Parental vaccine safety concerns in 2009.
Pediatrics 2010;125(4):654–59.
15. Rowhani-Rahbar A, Fireman B, Lewis E,
et al. Effect of age on the risk of fever and
seizures following immunization with measles-
containing vaccines in children. JAMA Pediatrics
2013;167(12):1111–17.
16. Parrella A, Gold M, Marshall H, Braunack-Mayer
A, Baghurst P. Parental perspectives of vaccine
safety and experience of adverse events following
immunisation. Vaccine 2013;31(16):2067–74.
17. Leask J, Kinnersley P, Jackson C, Cheater F,
Bedford H, Rowles G. Communicating with
parents about vaccination: A framework for health
professionals. BMC Pediatr. 2012;12:154.
18. Danchin M, Nolan T. A positive approach to
parents with concerns about vaccination for
the family physician. Aust Fam Physician
2014;43(10):690–94.
19. Opel DJ, Mangione-Smith R, Robinson JD,
Heritage J, et al. The influence of provider
communication behaviors on parental vaccine
acceptance and visit experience. Am J Pub Health
2015:e1–e7
20. Davies P, Chapman S, Leask J. Antivaccination
activists on the world wide web. Arch Dis Child
2002;87(1):22–25.
21. Jones AM, Omer SB, Bednarczyk RA, Halsey
NA, Moulton LH, Salmon DA. Parents’ source
of vaccine information and impact on vaccine
attitudes, beliefs and nonmedical exemptions. Adv
Prev Med 2012;2012:932741.
22. Busse JW, Wilson K, Campbell JB. Attitudes
towards vaccination among chiropractic and
naturopathic students. Vaccine 2008;26(49):
6237-43.
23. Schmidt K, Ernst E. MMR vaccination advice over
the internet. Vaccine 2003;21(11-12):1044−47.
24. Downey L, Tyree PT, Huebner CE, Lafferty WE.
Pediatric vaccination and vaccine-preventable
disease acquisition: Associations with care
by complementary and alternative medicine
providers. Matern Child Health J 2010;14(6):
922–30.
25. Wardle J, Stewart C, Parker M. Jabs and barbs:
Ways to address misleading vaccination and
immunisation information using currently available
strategies. J Law and Med 2013;21(1):159–78.
26. Lawrence GL, MacIntyre CR, Hull PB, McIntyre
PB. Effectiveness of the linkage of child care and
maternity payments to childhood immunisation.
Vaccine 2004;22(17–18):2345–50.
27. Miles M, Ryman TK, Dietz V, Zell E, Luman
ET. Validity of vaccination cards and parental
recall to estimate vaccination coverage: A
systematic review of the literature. Vaccine.
2013;31(12):1560–68.
28. Hull BP. Australian childhood immunisation
coverage. Commun Dis Intell 2014;38(2):E157.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

