Strategies for Addressing Vaccine Hesitancy: Communication & Skills
VerifiedAdded on 2022/09/14
|5
|4488
|17
Report
AI Summary
This report, contributed to Desklib, focuses on the critical issue of vaccine hesitancy and the essential communication and counselling skills required for public health professionals to address it effectively. The Italian law 119/2017 mandates childhood vaccinations, yet vaccine hesitancy remains a significant challenge. The report outlines the definition of vaccine hesitancy, its complexity, and the need for strategic communication approaches. It emphasizes the importance of basic health counselling skills, including active listening, empathy, and self-awareness, to build trust and address concerns. The report categorizes the population into groups based on their vaccine deficit (hesitant, unconcerned, active resisters, poorly reached) and suggests tailored communication strategies for each. It highlights the importance of understanding individual risk perceptions and the role of participatory communication models. The report also stresses the need for strategic communication planning and integrated collaboration among various institutions and services to improve vaccination rates and public health outcomes. This report provides valuable insights and practical strategies for healthcare workers and public health professionals.
Brief notes
195
Key words
• vaccination
• communication
• counselling
Communication and basic health
counselling skills to tackle vaccine
hesitancy
Valentina Possenti1, Anna Maria Luzi2, Anna Colucci2 and Barbara De Mei1
1Centro Nazionale per la Prevenzione delle Malattie e la Promozione della Salute, Istituto Superiore
di Sanità, Rome, Italy
2Dipartimento Malattie Infettive, Istituto Superiore di Sanità, Rome, Italy
Ann Ist Super Sanità 2019 | Vol. 55, No. 2: 195-199
DOI: 10.4415/ANN_19_02_12
INTRODUCTION
The law 119/2017, as conversionof the decree
73/2017, made ten childhood vaccinations (tetanus,
poliomyelitis, hepatitis B, diphtheria, pertussis, hae-
mophilus B, measles, mumps, rubella, chicken pox)
mandatory in Italy where coverage rates for various vac-
cine-preventable diseases have been decreasing since
2013 [1-3]. Vaccine hesitancy is defined as the reluc-
tance or refusal to vaccinate despite the availability of
vaccines [4], and enlisted among the ten major issues
that demand attention from the World Health Organi-
zation (WHO) and health partners in 2019 [5]. Namely,
it is a complex and context specific behaviour because it
varies across time, place and vaccines and is influenced
by a number of factors including issues of confidence,
complacency,and convenience.Vaccine-hesitantin-
dividuals constitute a heterogeneous group of people
who hold wide-ranged indecision on some vaccines as
well as on vaccination overall: they may accept vac-
cines but remain concerned, may refuse or delay some
vaccines but accept others, or may refuse all vaccines.
Basing on this complexity, to date immunization cover-
age are the proxy data mostly used even if it is known
that they are proven to be reliable for small samples
and vaccine decrease does not fully coincide with vac-
cine hesitancy [6]. This relevant issue in public health
broadly encompasses communication approaches that
public health professionals can adopt to address vac-
cine hesitancy effectively. An Italian study shows that,
even if paediatricians are favourable to vaccines and
vaccinations, gaps are retrieved between their overall
positive attitudes on one hand and knowledge, beliefs
and practices on the other hand, consequently affecting
their response capacity to address parents’ questions
[7]. In general, public health institutions should com-
municate using strategically established methods and
avoiding rushed communication which leads to imple-
menting wrong interventions and losing credibility. In
2010, the WHO suggested that to improve communi-
cation effectiveness within the healthcare system some
elements are needed, such as development of networks
and empowerment of communication competences [8-
14]. Moreover, within vaccine communication, public
health professionals deal with an even more highly com-
plex process that involves several different stakeholders
who are featured by own worldviews, perceptions and
needs. In this framework, vaccine communication does
not correspond to performing one-way informative in-
terventions or teaching, but initiates mutual dialogue
and reciprocal exchange among all people involved,
despite their different roles and diverse responsibilities.
It entails that communication methods and tools have
to be adequately aligned with the specific setting and
intended target groups. Both individuals and the com-
Address for correspondence: Valentina Possenti, Centro Nazionale per la Prevenzione delle Malattie e la Promozione della Salute, Istituto Superiore
di Sanità, Viale Regina Elena 299, 00161 Rome, Italy. E-mail: valentina.possenti@iss.it.
Abstract
The Italian law 119/2017 mandates ten childhood vaccinations to allow population aged
0-16 attend educational places and state school. This law enforcement is due to low
coverage rates for some vaccine-preventable diseases and to a complex phenomenon
known as vaccine hesitancy. Basic health counselling skills represent relevant resources
to let healthcare workers effectively address vaccine hesitancy in the population. We in-
dicated recommended communication approaches and basic health counselling skills to
be applied by public health professionals according to the specific target population with
vaccine deficit that means people not at all or partially reached by vaccinations. Public
health professionals are called to know, acquire, use, and adapt basic health counsel-
ling skills to effectively address vaccine hesitancy diversely affecting different groups of
population.
195
Key words
• vaccination
• communication
• counselling
Communication and basic health
counselling skills to tackle vaccine
hesitancy
Valentina Possenti1, Anna Maria Luzi2, Anna Colucci2 and Barbara De Mei1
1Centro Nazionale per la Prevenzione delle Malattie e la Promozione della Salute, Istituto Superiore
di Sanità, Rome, Italy
2Dipartimento Malattie Infettive, Istituto Superiore di Sanità, Rome, Italy
Ann Ist Super Sanità 2019 | Vol. 55, No. 2: 195-199
DOI: 10.4415/ANN_19_02_12
INTRODUCTION
The law 119/2017, as conversionof the decree
73/2017, made ten childhood vaccinations (tetanus,
poliomyelitis, hepatitis B, diphtheria, pertussis, hae-
mophilus B, measles, mumps, rubella, chicken pox)
mandatory in Italy where coverage rates for various vac-
cine-preventable diseases have been decreasing since
2013 [1-3]. Vaccine hesitancy is defined as the reluc-
tance or refusal to vaccinate despite the availability of
vaccines [4], and enlisted among the ten major issues
that demand attention from the World Health Organi-
zation (WHO) and health partners in 2019 [5]. Namely,
it is a complex and context specific behaviour because it
varies across time, place and vaccines and is influenced
by a number of factors including issues of confidence,
complacency,and convenience.Vaccine-hesitantin-
dividuals constitute a heterogeneous group of people
who hold wide-ranged indecision on some vaccines as
well as on vaccination overall: they may accept vac-
cines but remain concerned, may refuse or delay some
vaccines but accept others, or may refuse all vaccines.
Basing on this complexity, to date immunization cover-
age are the proxy data mostly used even if it is known
that they are proven to be reliable for small samples
and vaccine decrease does not fully coincide with vac-
cine hesitancy [6]. This relevant issue in public health
broadly encompasses communication approaches that
public health professionals can adopt to address vac-
cine hesitancy effectively. An Italian study shows that,
even if paediatricians are favourable to vaccines and
vaccinations, gaps are retrieved between their overall
positive attitudes on one hand and knowledge, beliefs
and practices on the other hand, consequently affecting
their response capacity to address parents’ questions
[7]. In general, public health institutions should com-
municate using strategically established methods and
avoiding rushed communication which leads to imple-
menting wrong interventions and losing credibility. In
2010, the WHO suggested that to improve communi-
cation effectiveness within the healthcare system some
elements are needed, such as development of networks
and empowerment of communication competences [8-
14]. Moreover, within vaccine communication, public
health professionals deal with an even more highly com-
plex process that involves several different stakeholders
who are featured by own worldviews, perceptions and
needs. In this framework, vaccine communication does
not correspond to performing one-way informative in-
terventions or teaching, but initiates mutual dialogue
and reciprocal exchange among all people involved,
despite their different roles and diverse responsibilities.
It entails that communication methods and tools have
to be adequately aligned with the specific setting and
intended target groups. Both individuals and the com-
Address for correspondence: Valentina Possenti, Centro Nazionale per la Prevenzione delle Malattie e la Promozione della Salute, Istituto Superiore
di Sanità, Viale Regina Elena 299, 00161 Rome, Italy. E-mail: valentina.possenti@iss.it.
Abstract
The Italian law 119/2017 mandates ten childhood vaccinations to allow population aged
0-16 attend educational places and state school. This law enforcement is due to low
coverage rates for some vaccine-preventable diseases and to a complex phenomenon
known as vaccine hesitancy. Basic health counselling skills represent relevant resources
to let healthcare workers effectively address vaccine hesitancy in the population. We in-
dicated recommended communication approaches and basic health counselling skills to
be applied by public health professionals according to the specific target population with
vaccine deficit that means people not at all or partially reached by vaccinations. Public
health professionals are called to know, acquire, use, and adapt basic health counsel-
ling skills to effectively address vaccine hesitancy diversely affecting different groups of
population.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Valentina Possenti, Anna Maria Luzi, Anna Colucciand Barbara De Mei
Brief notes
196
munity as a whole shall be effectively involved so that
homogenous, consistent and strategically coordinated
interventions can be implemented [15].
In particular, to effectively address vaccine hesitancy
in the general population, basic health counselling skills
represent relevant resources to professionals because
they are key elements to make healthcare workers cre-
ate effective relationships with people who can activate
their own resources and choose solutions that are con-
sistent with their needs. Basic counselling skills actually
stand for in fact the components of a well-structured
intervention aimed at helping people to actively face
health-related challenges.
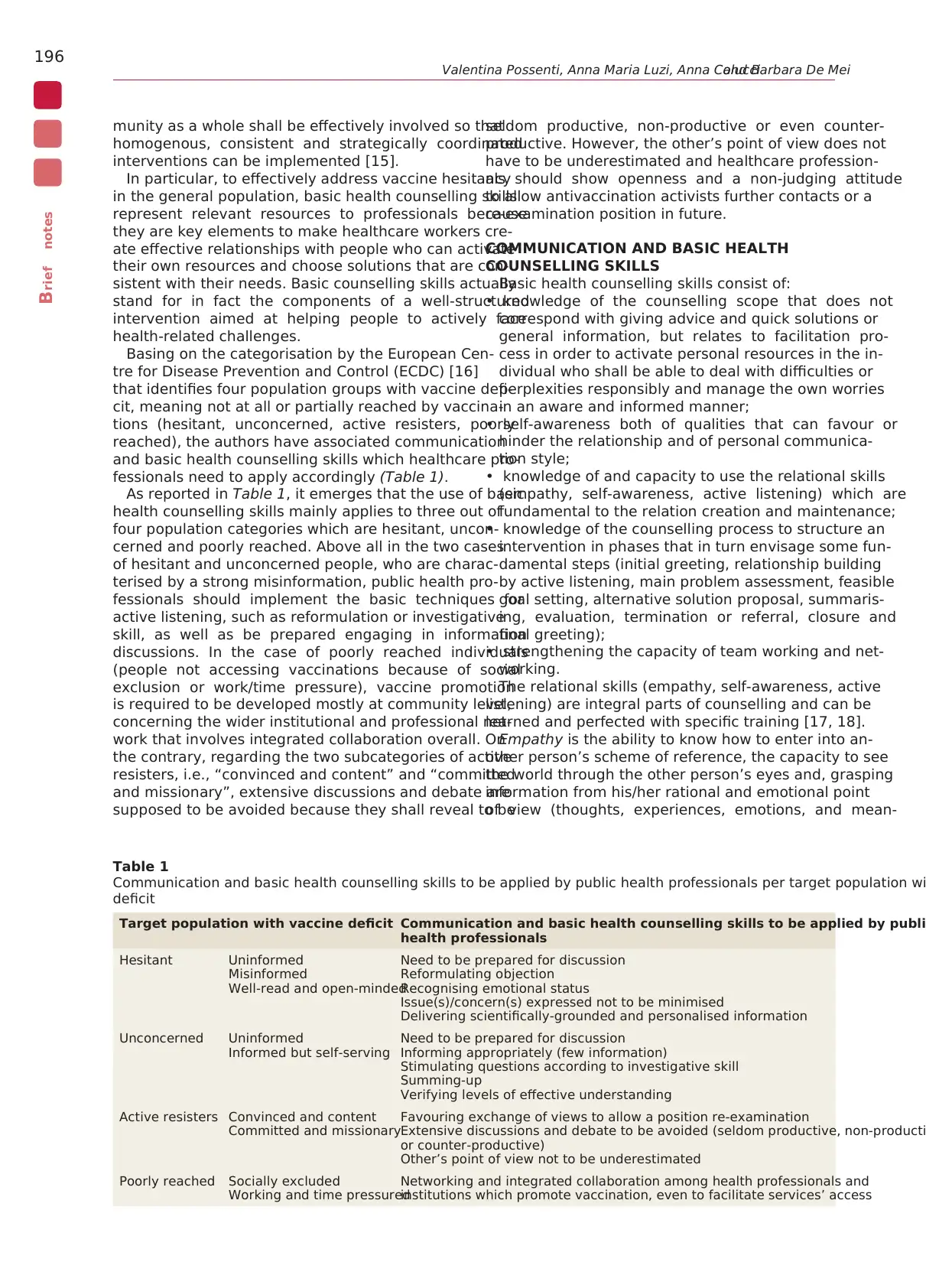
Basing on the categorisation by the European Cen-
tre for Disease Prevention and Control (ECDC) [16]
that identifies four population groups with vaccine defi-
cit, meaning not at all or partially reached by vaccina-
tions (hesitant, unconcerned, active resisters, poorly
reached), the authors have associated communication
and basic health counselling skills which healthcare pro-
fessionals need to apply accordingly (Table 1).
As reported in Table 1, it emerges that the use of basic
health counselling skills mainly applies to three out of
four population categories which are hesitant, uncon-
cerned and poorly reached. Above all in the two cases
of hesitant and unconcerned people, who are charac-
terised by a strong misinformation, public health pro-
fessionals should implement the basic techniques for
active listening, such as reformulation or investigative
skill, as well as be prepared engaging in information
discussions. In the case of poorly reached individuals
(people not accessing vaccinations because of social
exclusion or work/time pressure), vaccine promotion
is required to be developed mostly at community level,
concerning the wider institutional and professional net-
work that involves integrated collaboration overall. On
the contrary, regarding the two subcategories of active
resisters, i.e., “convinced and content” and “committed
and missionary”, extensive discussions and debate are
supposed to be avoided because they shall reveal to be
seldom productive, non-productive or even counter-
productive. However, the other’s point of view does not
have to be underestimated and healthcare profession-
als should show openness and a non-judging attitude
to allow antivaccination activists further contacts or a
re-examination position in future.
COMMUNICATION AND BASIC HEALTH
COUNSELLING SKILLS
Basic health counselling skills consist of:
• knowledge of the counselling scope that does not
correspond with giving advice and quick solutions or
general information, but relates to facilitation pro-
cess in order to activate personal resources in the in-
dividual who shall be able to deal with difficulties or
perplexities responsibly and manage the own worries
in an aware and informed manner;
• self-awareness both of qualities that can favour or
hinder the relationship and of personal communica-
tion style;
• knowledge of and capacity to use the relational skills
(empathy, self-awareness, active listening) which are
fundamental to the relation creation and maintenance;
• knowledge of the counselling process to structure an
intervention in phases that in turn envisage some fun-
damental steps (initial greeting, relationship building
by active listening, main problem assessment, feasible
goal setting, alternative solution proposal, summaris-
ing, evaluation, termination or referral, closure and
final greeting);
• strengthening the capacity of team working and net-
working.
The relational skills (empathy, self-awareness, active
listening) are integral parts of counselling and can be
learned and perfected with specific training [17, 18].
Empathy is the ability to know how to enter into an-
other person’s scheme of reference, the capacity to see
the world through the other person’s eyes and, grasping
information from his/her rational and emotional point
of view (thoughts, experiences, emotions, and mean-
Table 1
Communication and basic health counselling skills to be applied by public health professionals per target population wi
deficit
Target population with vaccine deficit Communication and basic health counselling skills to be applied by publi
health professionals
Hesitant Uninformed
Misinformed
Well-read and open-minded
Need to be prepared for discussion
Reformulating objection
Recognising emotional status
Issue(s)/concern(s) expressed not to be minimised
Delivering scientifically-grounded and personalised information
Unconcerned Uninformed
Informed but self-serving
Need to be prepared for discussion
Informing appropriately (few information)
Stimulating questions according to investigative skill
Summing-up
Verifying levels of effective understanding
Active resisters Convinced and content
Committed and missionary
Favouring exchange of views to allow a position re-examination
Extensive discussions and debate to be avoided (seldom productive, non-producti
or counter-productive)
Other’s point of view not to be underestimated
Poorly reached Socially excluded
Working and time pressured
Networking and integrated collaboration among health professionals and
institutions which promote vaccination, even to facilitate services’ access
Brief notes
196
munity as a whole shall be effectively involved so that
homogenous, consistent and strategically coordinated
interventions can be implemented [15].
In particular, to effectively address vaccine hesitancy
in the general population, basic health counselling skills
represent relevant resources to professionals because
they are key elements to make healthcare workers cre-
ate effective relationships with people who can activate
their own resources and choose solutions that are con-
sistent with their needs. Basic counselling skills actually
stand for in fact the components of a well-structured
intervention aimed at helping people to actively face
health-related challenges.
Basing on the categorisation by the European Cen-
tre for Disease Prevention and Control (ECDC) [16]
that identifies four population groups with vaccine defi-
cit, meaning not at all or partially reached by vaccina-
tions (hesitant, unconcerned, active resisters, poorly
reached), the authors have associated communication
and basic health counselling skills which healthcare pro-
fessionals need to apply accordingly (Table 1).
As reported in Table 1, it emerges that the use of basic
health counselling skills mainly applies to three out of
four population categories which are hesitant, uncon-
cerned and poorly reached. Above all in the two cases
of hesitant and unconcerned people, who are charac-
terised by a strong misinformation, public health pro-
fessionals should implement the basic techniques for
active listening, such as reformulation or investigative
skill, as well as be prepared engaging in information
discussions. In the case of poorly reached individuals
(people not accessing vaccinations because of social
exclusion or work/time pressure), vaccine promotion
is required to be developed mostly at community level,
concerning the wider institutional and professional net-
work that involves integrated collaboration overall. On
the contrary, regarding the two subcategories of active
resisters, i.e., “convinced and content” and “committed
and missionary”, extensive discussions and debate are
supposed to be avoided because they shall reveal to be
seldom productive, non-productive or even counter-
productive. However, the other’s point of view does not
have to be underestimated and healthcare profession-
als should show openness and a non-judging attitude
to allow antivaccination activists further contacts or a
re-examination position in future.
COMMUNICATION AND BASIC HEALTH
COUNSELLING SKILLS
Basic health counselling skills consist of:
• knowledge of the counselling scope that does not
correspond with giving advice and quick solutions or
general information, but relates to facilitation pro-
cess in order to activate personal resources in the in-
dividual who shall be able to deal with difficulties or
perplexities responsibly and manage the own worries
in an aware and informed manner;
• self-awareness both of qualities that can favour or
hinder the relationship and of personal communica-
tion style;
• knowledge of and capacity to use the relational skills
(empathy, self-awareness, active listening) which are
fundamental to the relation creation and maintenance;
• knowledge of the counselling process to structure an
intervention in phases that in turn envisage some fun-
damental steps (initial greeting, relationship building
by active listening, main problem assessment, feasible
goal setting, alternative solution proposal, summaris-
ing, evaluation, termination or referral, closure and
final greeting);
• strengthening the capacity of team working and net-
working.
The relational skills (empathy, self-awareness, active
listening) are integral parts of counselling and can be
learned and perfected with specific training [17, 18].
Empathy is the ability to know how to enter into an-
other person’s scheme of reference, the capacity to see
the world through the other person’s eyes and, grasping
information from his/her rational and emotional point
of view (thoughts, experiences, emotions, and mean-
Table 1
Communication and basic health counselling skills to be applied by public health professionals per target population wi
deficit
Target population with vaccine deficit Communication and basic health counselling skills to be applied by publi
health professionals
Hesitant Uninformed
Misinformed
Well-read and open-minded
Need to be prepared for discussion
Reformulating objection
Recognising emotional status
Issue(s)/concern(s) expressed not to be minimised
Delivering scientifically-grounded and personalised information
Unconcerned Uninformed
Informed but self-serving
Need to be prepared for discussion
Informing appropriately (few information)
Stimulating questions according to investigative skill
Summing-up
Verifying levels of effective understanding
Active resisters Convinced and content
Committed and missionary
Favouring exchange of views to allow a position re-examination
Extensive discussions and debate to be avoided (seldom productive, non-producti
or counter-productive)
Other’s point of view not to be underestimated
Poorly reached Socially excluded
Working and time pressured
Networking and integrated collaboration among health professionals and
institutions which promote vaccination, even to facilitate services’ access
Vaccine hesitancy and communication
Brief notes
197
ings), to understand the person’s requests and needs.
By showing empathy, healthcare workers live “as if” they
were the others but staying separate from the others,
otherwise they would no longer be able to help people
and meet people needs. Being empathic does not mean
confusing the two viewpoints: empathy is in fact sup-
ported by distinction and not confusion. In the profes-
sional relationship between experts and lay public, em-
pathy contributes to maintain separation between the
two different roles [19-23].
Self-awareness relates to being familiar with the own
“inner world” that is the cultural reference scheme,
value system, perceptions, emotions, and personal con-
ceptual maps. Other factors to be aware of are: the con-
text, the self-observation and self-monitoring capacity,
the management of nonverbal and paraverbal language
that is the emotional expression underlying the verbal
content [17].
Active listening helps both professionals and people
focusing on the other’s point of view, it can be triggered
through bidirectional communicative channels that fa-
cilitate useful information exchange flows and participa-
tory processes. It is fully based on empathy and on ac-
cepting the other’s point of view, as well as on creating a
positive relationship and a non-judging approach [19].
To listen actively, the adoption of a reference method-
ology articulated in empathic reflecting is necessary. It
encompasses the use of four specific communicative
techniques:reformulation,clarification,investigative
skill, first-person messages [24]. In particular:
• reformulation corresponds with repeating what the
other has just said, using the same words or rephras-
ing in a more concise way by other terms, without
adding any other concepts or different content (“Then
you are telling me that…”, “This means that you think…”,
“In other words…”);
• clarification uses the outlining emotions associated
with the content communicated, referring to verbal,
paraverbal and non-verbal communication (“From the
look on your face it seems to me that you are worried”;
“From the tone of your voice, I can feel you are uncertain
about what I am saying”);
• the investigative skill is the ability to ask, selecting
the most appropriate question type according to the
specific situation: “open questions” to be preferred at
the beginning of the conversation because they allow
wider answer options, extend and deepen the rela-
tionship, encourage opinion and thought expression;
closed-ended questions are clearly defined, they in-
duce a unique answer, and often stress only one reply
option, limit the communication and make it more
focussed, demand only objective facts and sometimes
may seem restrictive and obstructing (“When…?”,
”Where?”, “Who?”). Questions starting with “Why” can
be perceived as accusatory, and should be preferably
avoided;
• the use of first-person messages helps to distinguish
between professional’s and another person’s opinions
contributing to avoid conflicts. This technique serves
also to create a non-judgmental and an autonomous
decision-making process (“I think that…”, “In my opin-
ion…”) [17, 18].
THE USE OF COMMUNICATION AND
BASIC HEALTH COUNSELLING SKILLS TO
ADDRESS VACCINE HESITANCY
As indicated, public health professionals need to
know, acquire and implement basic vaccine counselling
skills when dealing above all with seven out of nine chal-
lenging population groups, even if such these compe-
tences can be also helpful somehow with people totally
refusing vaccinations. Knowledge and correct use of
basic health counselling skills allow in fact healthcare
workers achieve an effective vaccine communication
because relying on a structured and personalised inter-
vention. Vaccine communication need to acknowledge
individual risk perception that does not depend only on
the effective hazard but to a greater extent also on the
outrage linked to it, basically related to emotional fac-
tors prevailing on the hazard itself [25-27]. Within vac-
cine communication, by “actively listening” to people
fears and being aware of the wide-ranged determinants
for the perceived risk, public health authorities have
better opportunities to understand and to deal with the
origin of perception [28-30]. Especially as far as par-
ticular groups are concerned, in the case of childhood
vaccinations the main parents’ fears and worries refer to
adverse reaction effects or vaccine safety [31, 2]. If peo-
ple perceive empathy and consideration to their doubts
and opinions, they will be in turn more willing to listen
and trust. On the contrary, when people perceive sense
of distance, the trust level would be reduced and emo-
tional components of perception prevail on the rational
part, not activating listening triggers even if adequate
scientific communication was developed. Vaccine com-
munication bases on the participatory communication
model featured by an interactive exchange assessment
overall, where the understanding of social and personal
issues is decisive to make scientific information a useful
knowledge to citizens [32, 33].
People should not perceive to be passively advised
as “just getting reassurance by experts”: in the current
communication approach the public sphere is put at the
centre of the whole process [25, 27].
If vaccine communication can be considered an in-
teractive process of information and opinion sharing
among individuals, groups and institutions, healthcare
workers provide people with constructive, up-to-date
and meaningful messages and direct-access informa-
tion services, using a varied range of tools in order to
allow them make the best possible decisions about their
own health. This make that an important step within
the counselling intervention relates to verifying levels
of effective understanding in people after having pro-
vided scientifically-grounded and personalised informa-
tion. Looking at the big picture as a whole, in fact, in a
multistakeholder scenario the position of public health
professionals toward individuals or communities is fun-
damental as per their key advocacy role in being at the
helm of the processes, from planning to development,
monitoring and evaluation. Such a framework neces-
sarily demands for strategic communication planning,
favoured by the integrated participation and collabora-
tion of institutions, services and systems involved at dif-
ferent levels (national, regional and local) [34-38].
Brief notes
197
ings), to understand the person’s requests and needs.
By showing empathy, healthcare workers live “as if” they
were the others but staying separate from the others,
otherwise they would no longer be able to help people
and meet people needs. Being empathic does not mean
confusing the two viewpoints: empathy is in fact sup-
ported by distinction and not confusion. In the profes-
sional relationship between experts and lay public, em-
pathy contributes to maintain separation between the
two different roles [19-23].
Self-awareness relates to being familiar with the own
“inner world” that is the cultural reference scheme,
value system, perceptions, emotions, and personal con-
ceptual maps. Other factors to be aware of are: the con-
text, the self-observation and self-monitoring capacity,
the management of nonverbal and paraverbal language
that is the emotional expression underlying the verbal
content [17].
Active listening helps both professionals and people
focusing on the other’s point of view, it can be triggered
through bidirectional communicative channels that fa-
cilitate useful information exchange flows and participa-
tory processes. It is fully based on empathy and on ac-
cepting the other’s point of view, as well as on creating a
positive relationship and a non-judging approach [19].
To listen actively, the adoption of a reference method-
ology articulated in empathic reflecting is necessary. It
encompasses the use of four specific communicative
techniques:reformulation,clarification,investigative
skill, first-person messages [24]. In particular:
• reformulation corresponds with repeating what the
other has just said, using the same words or rephras-
ing in a more concise way by other terms, without
adding any other concepts or different content (“Then
you are telling me that…”, “This means that you think…”,
“In other words…”);
• clarification uses the outlining emotions associated
with the content communicated, referring to verbal,
paraverbal and non-verbal communication (“From the
look on your face it seems to me that you are worried”;
“From the tone of your voice, I can feel you are uncertain
about what I am saying”);
• the investigative skill is the ability to ask, selecting
the most appropriate question type according to the
specific situation: “open questions” to be preferred at
the beginning of the conversation because they allow
wider answer options, extend and deepen the rela-
tionship, encourage opinion and thought expression;
closed-ended questions are clearly defined, they in-
duce a unique answer, and often stress only one reply
option, limit the communication and make it more
focussed, demand only objective facts and sometimes
may seem restrictive and obstructing (“When…?”,
”Where?”, “Who?”). Questions starting with “Why” can
be perceived as accusatory, and should be preferably
avoided;
• the use of first-person messages helps to distinguish
between professional’s and another person’s opinions
contributing to avoid conflicts. This technique serves
also to create a non-judgmental and an autonomous
decision-making process (“I think that…”, “In my opin-
ion…”) [17, 18].
THE USE OF COMMUNICATION AND
BASIC HEALTH COUNSELLING SKILLS TO
ADDRESS VACCINE HESITANCY
As indicated, public health professionals need to
know, acquire and implement basic vaccine counselling
skills when dealing above all with seven out of nine chal-
lenging population groups, even if such these compe-
tences can be also helpful somehow with people totally
refusing vaccinations. Knowledge and correct use of
basic health counselling skills allow in fact healthcare
workers achieve an effective vaccine communication
because relying on a structured and personalised inter-
vention. Vaccine communication need to acknowledge
individual risk perception that does not depend only on
the effective hazard but to a greater extent also on the
outrage linked to it, basically related to emotional fac-
tors prevailing on the hazard itself [25-27]. Within vac-
cine communication, by “actively listening” to people
fears and being aware of the wide-ranged determinants
for the perceived risk, public health authorities have
better opportunities to understand and to deal with the
origin of perception [28-30]. Especially as far as par-
ticular groups are concerned, in the case of childhood
vaccinations the main parents’ fears and worries refer to
adverse reaction effects or vaccine safety [31, 2]. If peo-
ple perceive empathy and consideration to their doubts
and opinions, they will be in turn more willing to listen
and trust. On the contrary, when people perceive sense
of distance, the trust level would be reduced and emo-
tional components of perception prevail on the rational
part, not activating listening triggers even if adequate
scientific communication was developed. Vaccine com-
munication bases on the participatory communication
model featured by an interactive exchange assessment
overall, where the understanding of social and personal
issues is decisive to make scientific information a useful
knowledge to citizens [32, 33].
People should not perceive to be passively advised
as “just getting reassurance by experts”: in the current
communication approach the public sphere is put at the
centre of the whole process [25, 27].
If vaccine communication can be considered an in-
teractive process of information and opinion sharing
among individuals, groups and institutions, healthcare
workers provide people with constructive, up-to-date
and meaningful messages and direct-access informa-
tion services, using a varied range of tools in order to
allow them make the best possible decisions about their
own health. This make that an important step within
the counselling intervention relates to verifying levels
of effective understanding in people after having pro-
vided scientifically-grounded and personalised informa-
tion. Looking at the big picture as a whole, in fact, in a
multistakeholder scenario the position of public health
professionals toward individuals or communities is fun-
damental as per their key advocacy role in being at the
helm of the processes, from planning to development,
monitoring and evaluation. Such a framework neces-
sarily demands for strategic communication planning,
favoured by the integrated participation and collabora-
tion of institutions, services and systems involved at dif-
ferent levels (national, regional and local) [34-38].
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Valentina Possenti, Anna Maria Luzi, Anna Colucciand Barbara De Mei
Brief notes
198
The professional practice of healthcare workers is
framed in a specific organisational system and, more
broadly, in a complex context where they refer to other
stakeholders, institutions and media. Thus, health pro-
fessionals need to be aware of web-based and new media
for two reasons: on the one hand, knowing the kind of
information that flows through the net could be useful
to forestall some possible criticism; on the other hand,
groups on social networks may constitute extremely
valuable tools to keep individuals up to date with advices
and to promptly hinder false or ambiguous knowledge
they could have found on the web. Health information-
seeking behaviour on the web shows, in fact, how often
people turn first to the Internet both using information
to formulate their thoughts and making their own judge-
ments on preferred treatments [39]. Web 2.0, forums
and social networks, which enable two‐way and multi‐
way communication flows, have spread out anti-vacci-
nation voices to broader reach than ever before while,
years ago, they would have been restricted to certain
countries [40]. Health professionals are getting used to
situations where the “health blogger” or the “concerned
mother” are as important as – or even more influent
than – a general practitioner or paediatrician, strongly
influencing individual decision-making process [41-45].
Aware and skilled communication processes can facili-
tate relationships because even in presence of a world
wide web 2.0, they do represent significant tools for col-
laboration building and achieving shared solutions. The
public health goal is actually to stimulate professionals
to reflect upon the need to recognize, develop and adapt
basic health counselling skills in order to provide ade-
quate information and emotional support to people who
show hesitant attitudes towards vaccinations and can be
allowed to activate informed and responsible decisions.
Conflict of interest statement
There are no potential conflicts of interest or any fi-
nancial or personal relationships with other people or
organizations that could inappropriately bias conduct
and findings of this study.
Received on 16 October 2019.
Accepted on 16 May 2019.
REFERENCES
1. Italia. Legge 31 luglio 2017, n. 119. Conversione in leg-
ge, con modificazioni, del decreto-legge 7 giugno 2017,
n. 73, recante disposizioni urgenti in materia di preven-
zione vaccinale. Gazzetta Ufficiale della Repubblica
Italiana – Serie Generale n. 182, 05 agosto 2017. Avail-
able from: www.gazzettaufficiale.it/eli/id/2017/08/5/
17G00132/sg.
2. Giambi C, Fabiani M, D’Ancona F, et al. Parental vac-
cine hesitancy in Italy – Results from a national sur-
vey. Vaccine. 2018;36(6):779-87.doi:10.1016/j.vac-
cine.2017.12.074
3. Istituto Superiore di Sanità. EpiCentro. Il portale
dell’epidemiologia per la sanità pubblica. Morbillo, ul-
timi aggiornamenti. Available from: www.epicentro.iss.it/
problemi/morbillo/aggiornamenti.asp.
4. World Health Organization. Report of the SAGE work-
ing group on vaccine hesitancy. Geneva: WHO; 2014.
Available from: www.who.int/immunization/sage/meet-
ings/2014/october/SAGE_working_group_revised_re-
port_vaccine_hesitancy.pdf?ua=1.
5. World Health Organization. Ten threats to global health
in 2019. Geneva: WHO; 2019. Available from: www.who.
int/emergencies/ten-threats-to-global-health-in-2019.
6. Petrelli F, Contratti CM, Tanzi E, Grappasonni I. Vaccine
hesitancy, a public health problem. Ann Ig. 2018;30:86-
103. doi:10.7416/ai.2018.2200
7. Filia A, Bella A, D’Ancona F, Fabiani M, Giambi C,
Rizzo C, Ferrara L, Pascucci MG, Rota MC. Child-
hood vaccinations: knowledge, attitudes and practices
of paediatricians and factors associated with their con-
fidence in addressingparental concerns, Italy, 2016.
Euro Surveill. 2019;24(6):pii=1800275. doi: https://doi.
org/10.2807/1560-7917.ES.2019.24.6.1800275
8. Sweet M. Pandemic lessons learned from Australia. BMJ.
2009;339:424‐6.
9. Deirdre HD. The 2009 influenza pandemic. An indepen-
dent review of the UK response to the 2009 influenza
pandemic. 2010. Available from:
10. http://webarchive.nationalarchives.gov.uk/+/http://www.
cabinetoffice.gov.uk/media/416533/the2009influenza-
pandemic‐review.pdf.
11. Tay J, Ng YF, Cutter JL, James L. Influenza A
(H1N1/2009) pandemic in Singapore public health con-
trol measures implemented and lessons learnt. AAMS.
2010;39(4):313-24.
12. World Health Organization, Regional Office for Eu-
rope, University of Nottingham. Recommendations for
good practice in pandemic preparedness. Copenhagen,
Denmark: WHO Regional Office for Europe; 2010.
Available from: www.euro.who.int/__data/assets/pdf_
file/0017/128060/e94534.pdf.
13. World Health Organization. Report of the review com-
mittee on the functioning of the international health reg-
ulations (2005) in relation to Pandemic (H1N1) 2009.
Geneva: WHO; 2011. Available from: http://apps.who.
int/gb/ebwha/pdf_files/WHA64/A64_10‐en.pdf.
14. Greco D, Stern EK, Marks G. Review of ECDC’s re-
sponse to the influenza pandemic 2009-2010. Stockholm:
ECDC; 2011. Available from: http://ecdc.europa.eu/en/
aboutus/Key%20Documents/241111COR_Pandemic_
response.pdf.
15. World Health Organization. Public health measures dur-
ing the influenza A(H1N1) 2009 pandemic. Meeting
report. WHO Technical Consultation 26-28 October
2010, Gammarth, Tunisia. WHO; 2010. Available from:
http://whqlibdoc.who.int/hq/2011/WHO_HSE_GIP_
ITP_2011.3_eng.pdf.
16. ASSET. Action plan on science in society related issues in
epidemics and total pandemics. Action plan handbook.
Available from: www.asset-scienceinsociety.eu/outputs/
deliverables/action-plan-handbook.
17. European Centre for Disease Prevention and Control.
Let’s talk about protection. Stockholm: ECDC; 2016.
doi: 10.2900/573817
18. Luzi AM, De Mei B, Colucci A, Gallo P. Criteria for
standardizing counselling for HIV testing. Ann Ist Super
Sanità. 2010;46(1):42-50. doi: 10.4415/ANN_10_01_06
19. TELLME. Transparentcommunicationin epidemics:
Brief notes
198
The professional practice of healthcare workers is
framed in a specific organisational system and, more
broadly, in a complex context where they refer to other
stakeholders, institutions and media. Thus, health pro-
fessionals need to be aware of web-based and new media
for two reasons: on the one hand, knowing the kind of
information that flows through the net could be useful
to forestall some possible criticism; on the other hand,
groups on social networks may constitute extremely
valuable tools to keep individuals up to date with advices
and to promptly hinder false or ambiguous knowledge
they could have found on the web. Health information-
seeking behaviour on the web shows, in fact, how often
people turn first to the Internet both using information
to formulate their thoughts and making their own judge-
ments on preferred treatments [39]. Web 2.0, forums
and social networks, which enable two‐way and multi‐
way communication flows, have spread out anti-vacci-
nation voices to broader reach than ever before while,
years ago, they would have been restricted to certain
countries [40]. Health professionals are getting used to
situations where the “health blogger” or the “concerned
mother” are as important as – or even more influent
than – a general practitioner or paediatrician, strongly
influencing individual decision-making process [41-45].
Aware and skilled communication processes can facili-
tate relationships because even in presence of a world
wide web 2.0, they do represent significant tools for col-
laboration building and achieving shared solutions. The
public health goal is actually to stimulate professionals
to reflect upon the need to recognize, develop and adapt
basic health counselling skills in order to provide ade-
quate information and emotional support to people who
show hesitant attitudes towards vaccinations and can be
allowed to activate informed and responsible decisions.
Conflict of interest statement
There are no potential conflicts of interest or any fi-
nancial or personal relationships with other people or
organizations that could inappropriately bias conduct
and findings of this study.
Received on 16 October 2019.
Accepted on 16 May 2019.
REFERENCES
1. Italia. Legge 31 luglio 2017, n. 119. Conversione in leg-
ge, con modificazioni, del decreto-legge 7 giugno 2017,
n. 73, recante disposizioni urgenti in materia di preven-
zione vaccinale. Gazzetta Ufficiale della Repubblica
Italiana – Serie Generale n. 182, 05 agosto 2017. Avail-
able from: www.gazzettaufficiale.it/eli/id/2017/08/5/
17G00132/sg.
2. Giambi C, Fabiani M, D’Ancona F, et al. Parental vac-
cine hesitancy in Italy – Results from a national sur-
vey. Vaccine. 2018;36(6):779-87.doi:10.1016/j.vac-
cine.2017.12.074
3. Istituto Superiore di Sanità. EpiCentro. Il portale
dell’epidemiologia per la sanità pubblica. Morbillo, ul-
timi aggiornamenti. Available from: www.epicentro.iss.it/
problemi/morbillo/aggiornamenti.asp.
4. World Health Organization. Report of the SAGE work-
ing group on vaccine hesitancy. Geneva: WHO; 2014.
Available from: www.who.int/immunization/sage/meet-
ings/2014/october/SAGE_working_group_revised_re-
port_vaccine_hesitancy.pdf?ua=1.
5. World Health Organization. Ten threats to global health
in 2019. Geneva: WHO; 2019. Available from: www.who.
int/emergencies/ten-threats-to-global-health-in-2019.
6. Petrelli F, Contratti CM, Tanzi E, Grappasonni I. Vaccine
hesitancy, a public health problem. Ann Ig. 2018;30:86-
103. doi:10.7416/ai.2018.2200
7. Filia A, Bella A, D’Ancona F, Fabiani M, Giambi C,
Rizzo C, Ferrara L, Pascucci MG, Rota MC. Child-
hood vaccinations: knowledge, attitudes and practices
of paediatricians and factors associated with their con-
fidence in addressingparental concerns, Italy, 2016.
Euro Surveill. 2019;24(6):pii=1800275. doi: https://doi.
org/10.2807/1560-7917.ES.2019.24.6.1800275
8. Sweet M. Pandemic lessons learned from Australia. BMJ.
2009;339:424‐6.
9. Deirdre HD. The 2009 influenza pandemic. An indepen-
dent review of the UK response to the 2009 influenza
pandemic. 2010. Available from:
10. http://webarchive.nationalarchives.gov.uk/+/http://www.
cabinetoffice.gov.uk/media/416533/the2009influenza-
pandemic‐review.pdf.
11. Tay J, Ng YF, Cutter JL, James L. Influenza A
(H1N1/2009) pandemic in Singapore public health con-
trol measures implemented and lessons learnt. AAMS.
2010;39(4):313-24.
12. World Health Organization, Regional Office for Eu-
rope, University of Nottingham. Recommendations for
good practice in pandemic preparedness. Copenhagen,
Denmark: WHO Regional Office for Europe; 2010.
Available from: www.euro.who.int/__data/assets/pdf_
file/0017/128060/e94534.pdf.
13. World Health Organization. Report of the review com-
mittee on the functioning of the international health reg-
ulations (2005) in relation to Pandemic (H1N1) 2009.
Geneva: WHO; 2011. Available from: http://apps.who.
int/gb/ebwha/pdf_files/WHA64/A64_10‐en.pdf.
14. Greco D, Stern EK, Marks G. Review of ECDC’s re-
sponse to the influenza pandemic 2009-2010. Stockholm:
ECDC; 2011. Available from: http://ecdc.europa.eu/en/
aboutus/Key%20Documents/241111COR_Pandemic_
response.pdf.
15. World Health Organization. Public health measures dur-
ing the influenza A(H1N1) 2009 pandemic. Meeting
report. WHO Technical Consultation 26-28 October
2010, Gammarth, Tunisia. WHO; 2010. Available from:
http://whqlibdoc.who.int/hq/2011/WHO_HSE_GIP_
ITP_2011.3_eng.pdf.
16. ASSET. Action plan on science in society related issues in
epidemics and total pandemics. Action plan handbook.
Available from: www.asset-scienceinsociety.eu/outputs/
deliverables/action-plan-handbook.
17. European Centre for Disease Prevention and Control.
Let’s talk about protection. Stockholm: ECDC; 2016.
doi: 10.2900/573817
18. Luzi AM, De Mei B, Colucci A, Gallo P. Criteria for
standardizing counselling for HIV testing. Ann Ist Super
Sanità. 2010;46(1):42-50. doi: 10.4415/ANN_10_01_06
19. TELLME. Transparentcommunicationin epidemics:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Vaccine hesitancy and communication
Brief notes
199
learning lessons from experience,deliveringeffective
messages, providing evidence. Practical guide for health
risk communication. New communication strategies for
institutional actors. Available from: www.tellmeproject.
eu/node/390.
20. Rogers CR. La terapia centrata sul cliente. Firenze: Mar-
tinelli; 1989.
21. Watzlavick P, Beavin JH, Jackson DD. Pragmatica della
comunicazione umana. Boringhieri; 1976.
22. Gadotti G (Ed). La comunicazione sociale. Soggetti,
strumenti e linguaggi. Milano: Arcipelago; 2001.
23. Gadotti G, Bernocchi R. La pubblicità sociale. Maneg-
giare con cura. Roma: Carocci; 2010.
24. Polesana MA. La pubblicità intelligente. L’uso dell’ironia
in pubblicità. Milano: Franco Angeli; 2005.
25. De Mei B, Luzi AM. Le competenze di counselling per
una gestione consapevole delle reazioni personali e dei
comportamenti dell’operatore nella relazione professio-
nale. Dossier. Milano: Zadig; 2011.
26. TELLME. Transparentcommunicationin epidemics:
Learning Lessons from experience, delivering effective
messages, providing evidence. A new model for risk com-
munication in health. Available from: www.tellmeproject.
eu/node/314.
27. Sandman PM. Risk = Hazard + Outrage: Coping with
controversy about utility risks. Engineering News-Re-
cord; 1999. p. A19-A23.
28. Covello VT. Social and behavioral research on risk: uses
in risk management decisionmaking. In: Covello VT,
Mumpower JL, Stallen PJ, Uppuluri VRR (Eds). Envi-
ronmental impact assessment, technology assessment,
and risk analysis. Berlin, Heidelberg, New York, Tokyo:
Springer-Verlag; 1985.
29. European Commission. Assessment report on EU‐wide
pandemic vaccine strategies. 2010. Available from: http://
ec.europa.eu/health/communicable_diseases/docs/assess-
ment_vaccine_en.pdf.
30. Centers for Disease Control and Prevention. Provider re-
sources for vaccine conversations with parents. Available
from: www.cdc.gov/vaccines/hcp/conversations/about-
vacc-conversations.html.
31. Sjoberg L. Risk Perception by the public and by experts:
a dilemma in risk management. Human Ecology Review.
1999;6(2):1-9.
32. Lambert TW, Soskolne LC, Bergum V, Howell J, Dosse-
tor JB. Ethical perspectives for public and environmental
health: fostering autonomy and the right to know. Envi-
ronmental Health Perspectives. 2003;111(2):133-7.
33. Leiss W, Krewski D. Risk communication: theory and
practice. In: Leiss W (Ed). Prospects and problems in risk
communication. Waterloo, Ontario: University of Water-
loo Press; 1989. p. 89-112.
34. Slovic P. The perception of risk. London and Sterling:
Earthscan Publ. Ltd; 2000.
35. Biasio LR. Vaccine hesitancy and health literacy.
Hum Vaccin Immunother. 2017;13(3):701-2.doi:
10.1080/21645515.2016.1243633
36. Beck U. La società del rischio. Roma: Carrocci Editore;
2000.
37. Biocca M. La comunicazione sul rischio per la salute. Nel
Teatro di Sagredo: verso una seconda modernità. Torino:
Centro Scientifico Editore; 2002. (Comunicazione in
Sanità Vol. 6).
38. Leiss W. Three phases in the evolution of risk commu-
nication practice. Annals of the American Academy of
Political and Social Science. 1996;545:85-94.
39. National Research Council. Improving risk communica-
tion. Washington, DC: National Academy Press; 1989.
40. Kata A. Anti-vaccine activists, Web 2.0 and the post-
modern paradigm. An overview of tactics and tropes
used online by the anti-vaccination movement. Vaccine.
2012;30:3778-89.
41. European Centre for Disease Prevention and Control.
Communication on immunisation – building trust”. Tech-
nical document. Stockholm: ECDC; 2012.
42. CDC Facebook page. Available from: https://www.face-
book.com/CDC/.
43. Markoff J. Entrepreneurs see a Web guided by common
sense. New York Times; 2006.
44. De Mei B, Luzi AM. Il valore aggiunto delle competenze
di counselling per una comunicazione efficace in ambito
professionale. Dossier. Milano: Zadig; 2011.
45. Catalan-Matamoros D, Peñafiel-Saiz C. How is com-
munication of vaccines in traditional media: a systematic
review. Perspectives in Public Health. 2018;138(4). doi:
10.1177/1757913918780142
Brief notes
199
learning lessons from experience,deliveringeffective
messages, providing evidence. Practical guide for health
risk communication. New communication strategies for
institutional actors. Available from: www.tellmeproject.
eu/node/390.
20. Rogers CR. La terapia centrata sul cliente. Firenze: Mar-
tinelli; 1989.
21. Watzlavick P, Beavin JH, Jackson DD. Pragmatica della
comunicazione umana. Boringhieri; 1976.
22. Gadotti G (Ed). La comunicazione sociale. Soggetti,
strumenti e linguaggi. Milano: Arcipelago; 2001.
23. Gadotti G, Bernocchi R. La pubblicità sociale. Maneg-
giare con cura. Roma: Carocci; 2010.
24. Polesana MA. La pubblicità intelligente. L’uso dell’ironia
in pubblicità. Milano: Franco Angeli; 2005.
25. De Mei B, Luzi AM. Le competenze di counselling per
una gestione consapevole delle reazioni personali e dei
comportamenti dell’operatore nella relazione professio-
nale. Dossier. Milano: Zadig; 2011.
26. TELLME. Transparentcommunicationin epidemics:
Learning Lessons from experience, delivering effective
messages, providing evidence. A new model for risk com-
munication in health. Available from: www.tellmeproject.
eu/node/314.
27. Sandman PM. Risk = Hazard + Outrage: Coping with
controversy about utility risks. Engineering News-Re-
cord; 1999. p. A19-A23.
28. Covello VT. Social and behavioral research on risk: uses
in risk management decisionmaking. In: Covello VT,
Mumpower JL, Stallen PJ, Uppuluri VRR (Eds). Envi-
ronmental impact assessment, technology assessment,
and risk analysis. Berlin, Heidelberg, New York, Tokyo:
Springer-Verlag; 1985.
29. European Commission. Assessment report on EU‐wide
pandemic vaccine strategies. 2010. Available from: http://
ec.europa.eu/health/communicable_diseases/docs/assess-
ment_vaccine_en.pdf.
30. Centers for Disease Control and Prevention. Provider re-
sources for vaccine conversations with parents. Available
from: www.cdc.gov/vaccines/hcp/conversations/about-
vacc-conversations.html.
31. Sjoberg L. Risk Perception by the public and by experts:
a dilemma in risk management. Human Ecology Review.
1999;6(2):1-9.
32. Lambert TW, Soskolne LC, Bergum V, Howell J, Dosse-
tor JB. Ethical perspectives for public and environmental
health: fostering autonomy and the right to know. Envi-
ronmental Health Perspectives. 2003;111(2):133-7.
33. Leiss W, Krewski D. Risk communication: theory and
practice. In: Leiss W (Ed). Prospects and problems in risk
communication. Waterloo, Ontario: University of Water-
loo Press; 1989. p. 89-112.
34. Slovic P. The perception of risk. London and Sterling:
Earthscan Publ. Ltd; 2000.
35. Biasio LR. Vaccine hesitancy and health literacy.
Hum Vaccin Immunother. 2017;13(3):701-2.doi:
10.1080/21645515.2016.1243633
36. Beck U. La società del rischio. Roma: Carrocci Editore;
2000.
37. Biocca M. La comunicazione sul rischio per la salute. Nel
Teatro di Sagredo: verso una seconda modernità. Torino:
Centro Scientifico Editore; 2002. (Comunicazione in
Sanità Vol. 6).
38. Leiss W. Three phases in the evolution of risk commu-
nication practice. Annals of the American Academy of
Political and Social Science. 1996;545:85-94.
39. National Research Council. Improving risk communica-
tion. Washington, DC: National Academy Press; 1989.
40. Kata A. Anti-vaccine activists, Web 2.0 and the post-
modern paradigm. An overview of tactics and tropes
used online by the anti-vaccination movement. Vaccine.
2012;30:3778-89.
41. European Centre for Disease Prevention and Control.
Communication on immunisation – building trust”. Tech-
nical document. Stockholm: ECDC; 2012.
42. CDC Facebook page. Available from: https://www.face-
book.com/CDC/.
43. Markoff J. Entrepreneurs see a Web guided by common
sense. New York Times; 2006.
44. De Mei B, Luzi AM. Il valore aggiunto delle competenze
di counselling per una comunicazione efficace in ambito
professionale. Dossier. Milano: Zadig; 2011.
45. Catalan-Matamoros D, Peñafiel-Saiz C. How is com-
munication of vaccines in traditional media: a systematic
review. Perspectives in Public Health. 2018;138(4). doi:
10.1177/1757913918780142
1 out of 5
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.