Conducting a Literature Review on Value-Based Care in Healthcare
VerifiedAdded on 2022/11/28
|13
|3403
|284
Report
AI Summary
This report presents a comprehensive literature review on value-based care (VBC), examining its implementation and impact on healthcare outcomes. The review explores the evolution of VBC, contrasting it with traditional fee-for-service models, and highlighting its focus on patient value and cost-effectiveness. The study delves into various research papers and studies, including those by Colldén and Hellström, Zipfel et al., Damberg et al., and Elf et al., to analyze the application of implementation science within VBC frameworks. It investigates the use of tools like the Consolidated Framework of Implementation Research (CFIR) and Change Models (ICM) to improve the effectiveness of VBC initiatives. The report also outlines the methodology, including search strategies and data collection methods, and proposes a timeline for future research, including primary data collection through surveys and evaluations of healthcare amenities. The recommendations emphasize the significance of team-based care delivery in VBC and its influence on healthcare professional burnout.

Running head: REPORT ON VALUE BASED-CARE
VALUE BASED-CARE
Name of the student
Name of the university
Author’s name
VALUE BASED-CARE
Name of the student
Name of the university
Author’s name
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1VALUE BASED-CARE
Title
"Conducting a literature review by gathering primary data on how value-based care helps in
the improvement of health care."
Background
Transition contributes to every life's many facets. Most of those shifts are apparent, but
some take individuals by chance, like the adjustments that the healthcare system is currently
fundamentally changing. There had been a moment when the number of people they did care for
was all that made a difference to healthcare professionals, but this is shifting now. Individuals
are requesting value-based care, and this requirement has been met slowly by the
healthcare sector (White, Dudley-Brown and Terhaar 2016). Health care systems in countries
such as the United Kingdom and the United States have been working in recent years to measure
the comparative cost-efficiency and efficiency of various medical interventions (Britto et al.
2018). Cost and medical intervention efficiency measurement has been used to check the
economic condition of a particular organization. This strategy, recognized as value-based
medicine, accompanied the advancement of evidence-based medicine and widened the idea to
provide a specific cost-benefit analysis, focusing on the value supplied to patients instead of the
conventional model where payments were made for the number of facilities provided.
Health systems have invested heavily in employing physicians or building models to
optimize costs and quality of treatment to align the clinical and financial interests of physicians
and hospitals (White, Dudley-Brown and Terhaar 2016). Nevertheless, other businesses find that
just appointing doctors does not automatically produce the desired outcomes. A review of a
Title
"Conducting a literature review by gathering primary data on how value-based care helps in
the improvement of health care."
Background
Transition contributes to every life's many facets. Most of those shifts are apparent, but
some take individuals by chance, like the adjustments that the healthcare system is currently
fundamentally changing. There had been a moment when the number of people they did care for
was all that made a difference to healthcare professionals, but this is shifting now. Individuals
are requesting value-based care, and this requirement has been met slowly by the
healthcare sector (White, Dudley-Brown and Terhaar 2016). Health care systems in countries
such as the United Kingdom and the United States have been working in recent years to measure
the comparative cost-efficiency and efficiency of various medical interventions (Britto et al.
2018). Cost and medical intervention efficiency measurement has been used to check the
economic condition of a particular organization. This strategy, recognized as value-based
medicine, accompanied the advancement of evidence-based medicine and widened the idea to
provide a specific cost-benefit analysis, focusing on the value supplied to patients instead of the
conventional model where payments were made for the number of facilities provided.
Health systems have invested heavily in employing physicians or building models to
optimize costs and quality of treatment to align the clinical and financial interests of physicians
and hospitals (White, Dudley-Brown and Terhaar 2016). Nevertheless, other businesses find that
just appointing doctors does not automatically produce the desired outcomes. A review of a
2VALUE BASED-CARE
report in 2018 shows positive interrelationships with improved results in having access to key
data and including physicians in decision making (Britto et al. 2018). The key data and inclusion
of general physicians in decision making has been linked in such a way that a positive correlation
always exists. Value-based healthcare professionals (hospital staffs and doctors) are paid based
on patient health results. The value-based service programs honor organizations for their efforts
in strengthening patients ' health, raising the consequences and incidences of chronic diseases,
and leading healthier lives on facts (Britto et al. 2018).
Value-based care is distinguished from a fee-for-service or capitalized method in which
facilities are charged on the basis of a health care delivery. In many instances, discrete programs
are introduced and seldom form part of a structured value-based healthcare plan. This condition
makes the service more practical and effective since value is considered for the process. The
value of value-based health care derives from the calculation of health outcomes against the
expense of treatment (French, Guzman et al. 2016). A formulation centered on evaluating
outcomes, and leads to changes in efficiency, is value-based healthcare (VBHC). Nevertheless,
as with applying research, VBHC does not provide a systematic approach to change.
In many patient policies, an important objective is an improvement in the quality of care
thus reducing costs (Baumhauer and Bozic 2016). Value-based health care (VBHC) seeks to
restructure healthcare and maximize consumer value. The ' satisfaction ' is defined in VBHC as
health outcomes related to costs that are relevant to the patient. Porter indicated that this aim can
be achieved by monitoring of outcomes and medical costs that can help to identify differences of
performance throughout the whole clinical process. Experts suggest that the increased capacity
can be established and the quality of care enhanced on the basis of this insight into outcomes.
VBHC is now used as a paradigm to enhance register results and to promote more effective
report in 2018 shows positive interrelationships with improved results in having access to key
data and including physicians in decision making (Britto et al. 2018). The key data and inclusion
of general physicians in decision making has been linked in such a way that a positive correlation
always exists. Value-based healthcare professionals (hospital staffs and doctors) are paid based
on patient health results. The value-based service programs honor organizations for their efforts
in strengthening patients ' health, raising the consequences and incidences of chronic diseases,
and leading healthier lives on facts (Britto et al. 2018).
Value-based care is distinguished from a fee-for-service or capitalized method in which
facilities are charged on the basis of a health care delivery. In many instances, discrete programs
are introduced and seldom form part of a structured value-based healthcare plan. This condition
makes the service more practical and effective since value is considered for the process. The
value of value-based health care derives from the calculation of health outcomes against the
expense of treatment (French, Guzman et al. 2016). A formulation centered on evaluating
outcomes, and leads to changes in efficiency, is value-based healthcare (VBHC). Nevertheless,
as with applying research, VBHC does not provide a systematic approach to change.
In many patient policies, an important objective is an improvement in the quality of care
thus reducing costs (Baumhauer and Bozic 2016). Value-based health care (VBHC) seeks to
restructure healthcare and maximize consumer value. The ' satisfaction ' is defined in VBHC as
health outcomes related to costs that are relevant to the patient. Porter indicated that this aim can
be achieved by monitoring of outcomes and medical costs that can help to identify differences of
performance throughout the whole clinical process. Experts suggest that the increased capacity
can be established and the quality of care enhanced on the basis of this insight into outcomes.
VBHC is now used as a paradigm to enhance register results and to promote more effective
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3VALUE BASED-CARE
cohesion of care via optimization and reporting (Baumhauer and Bozic 2016). The current
framework of VBHC does not, however, have a systematic approach to enhancement execution.
Sometimes the concept is the only solution to improve results and reduce cost, but it remains
unclear how improvements should be implemented. The literature identifies a lack of a systemic
approach to VBHC and, in particular, a method to carry out improvements. Lack of systemic
approach reduces the significance of a research paper. Thus, the relationship between cost and
performance monitoring plays an important role in understanding the strength of a value based
service. Measuring performance and costs also proven to give valuable insights into functional
variability and duplication, which can strengthen procedures. There is scant information on the
application of VBHC improvement initiatives (Elf et al. 2017). An example in the context of the
orthopedics project was identified which improved the identification of variations in the hospital
stay. Another example, involving prostate cancer treatment, shows that results-based
improvement has led to a significant decrease in incontinence. However, many change programs
focused on established differences in outcomes have been introduced in the field of heart
treatment. Nevertheless, it was not mentioned how the enhancements were introduced. We have
therefore studied the implementation of VBHC improvement initiatives and whether there is an
added value to VBHC in a systems method of implementation. The insight that resulted might
enrich the VBHC concept (Baumhauer and Bozic 2016).
Objective
The aim is to investigate the implementation of improvement initiatives in the context of VBHC
cohesion of care via optimization and reporting (Baumhauer and Bozic 2016). The current
framework of VBHC does not, however, have a systematic approach to enhancement execution.
Sometimes the concept is the only solution to improve results and reduce cost, but it remains
unclear how improvements should be implemented. The literature identifies a lack of a systemic
approach to VBHC and, in particular, a method to carry out improvements. Lack of systemic
approach reduces the significance of a research paper. Thus, the relationship between cost and
performance monitoring plays an important role in understanding the strength of a value based
service. Measuring performance and costs also proven to give valuable insights into functional
variability and duplication, which can strengthen procedures. There is scant information on the
application of VBHC improvement initiatives (Elf et al. 2017). An example in the context of the
orthopedics project was identified which improved the identification of variations in the hospital
stay. Another example, involving prostate cancer treatment, shows that results-based
improvement has led to a significant decrease in incontinence. However, many change programs
focused on established differences in outcomes have been introduced in the field of heart
treatment. Nevertheless, it was not mentioned how the enhancements were introduced. We have
therefore studied the implementation of VBHC improvement initiatives and whether there is an
added value to VBHC in a systems method of implementation. The insight that resulted might
enrich the VBHC concept (Baumhauer and Bozic 2016).
Objective
The aim is to investigate the implementation of improvement initiatives in the context of VBHC
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4VALUE BASED-CARE
Research questions
How implementation science could be of added value for VBHC and vice versa?
Search strategy
In this report, various online libraries such as NCBI, PubMed, and Google Scholar were
used to identify the corresponding publications that rely on the terms of' value-based treatment,''
Value-based literature review.' The search approach for 2000 to 2019 was implemented in this
report. In fact, this report included only papers published in English. Any other records written in
non-English are exempt. This paper even used a variety of documents, including quantitative,
qualitative studies, respective websites and literary works reports.
Literature review 800
In 2018, Colldén and Hellström conducted a study to examine how the Consolidated
Framework of Implementation Research (CFIR) can be driven by a theory of translation to
improve their awareness of the dynamic method of applying MIs. Two years of MI Value-Based
Health Care(VBHC) in a major Swedish hospital were the empirical basis of the research. A
methodological methodology was used in this longitudinal study undertaken by Colldén and
Hellström with the help of an insider investigator with unique data exposure, who began in 2015.
Field observations, documentation, and audio recordings of meetings and community thoughts,
abridged in an event data system organized through CFIR domains, form data sources. An
additional consultant was involved in a collaborative study to improve the methodology and
minimize potential bias. In recent years, VBHC is one sometimes known as MIs according to the
article. The key element of this MI is the concept of importance as outcomes that are essential for
Research questions
How implementation science could be of added value for VBHC and vice versa?
Search strategy
In this report, various online libraries such as NCBI, PubMed, and Google Scholar were
used to identify the corresponding publications that rely on the terms of' value-based treatment,''
Value-based literature review.' The search approach for 2000 to 2019 was implemented in this
report. In fact, this report included only papers published in English. Any other records written in
non-English are exempt. This paper even used a variety of documents, including quantitative,
qualitative studies, respective websites and literary works reports.
Literature review 800
In 2018, Colldén and Hellström conducted a study to examine how the Consolidated
Framework of Implementation Research (CFIR) can be driven by a theory of translation to
improve their awareness of the dynamic method of applying MIs. Two years of MI Value-Based
Health Care(VBHC) in a major Swedish hospital were the empirical basis of the research. A
methodological methodology was used in this longitudinal study undertaken by Colldén and
Hellström with the help of an insider investigator with unique data exposure, who began in 2015.
Field observations, documentation, and audio recordings of meetings and community thoughts,
abridged in an event data system organized through CFIR domains, form data sources. An
additional consultant was involved in a collaborative study to improve the methodology and
minimize potential bias. In recent years, VBHC is one sometimes known as MIs according to the
article. The key element of this MI is the concept of importance as outcomes that are essential for
5VALUE BASED-CARE
the patient with respect to care costs. The paper provides three directions to advise CFIR as
applying to MI: 1) proof reliability is not as important to MIs as to scientific and technological
innovations; 2) the adaptability of the MI is stronger; and 3) execution may be more effective
than planning and executing. It allows administrators not to abandon the initial ideas, but to take
advantage of the opportunity to adapt MIs to suit their organization.
There was another study conducted by Zipfel et al. (2019) which incorporated change
models to enhance the value of the value-based healthcare. To conduct this study, two cases of
heart care were evaluated – in one of the cases, the study was conducted without the
unambiguous use of a systematic implementation method and in another case, (ICM)
Implementation of Change Model was used (Zipfel et al. 2019). To assess the degree of which
the method was used, information was collected by searching different documents, semi-
structured interviews, and a focus group. A theory-driven qualitative analysis was done utilizing
the ICM as a key structure. The researchers observed that in both the cases result measures were
observed as a significant initial starting position for the execution and for observing moderations.
The researchers after completing the study concluded that the execution of the ICM enables the
effective application of quality-improvement creativities within.
In another study, Damberg et al. (2014) conducted a literature review where the
researchers summarized the available amount of knowledge regarding Value-based purchasing
(VBP) (Damberg et al. 2014). The information was collected from a set of published journals
and articles, a review of documents related to the VBP programs available to the public, and
discuss with an expert panel involving the VBP program sponsors, healthcare professionals and
healthcare systems, and academic researchers with VBP evaluation expertise. According to all
the gathered data, the researchers found that the VBP program sponsors have attained a huge
the patient with respect to care costs. The paper provides three directions to advise CFIR as
applying to MI: 1) proof reliability is not as important to MIs as to scientific and technological
innovations; 2) the adaptability of the MI is stronger; and 3) execution may be more effective
than planning and executing. It allows administrators not to abandon the initial ideas, but to take
advantage of the opportunity to adapt MIs to suit their organization.
There was another study conducted by Zipfel et al. (2019) which incorporated change
models to enhance the value of the value-based healthcare. To conduct this study, two cases of
heart care were evaluated – in one of the cases, the study was conducted without the
unambiguous use of a systematic implementation method and in another case, (ICM)
Implementation of Change Model was used (Zipfel et al. 2019). To assess the degree of which
the method was used, information was collected by searching different documents, semi-
structured interviews, and a focus group. A theory-driven qualitative analysis was done utilizing
the ICM as a key structure. The researchers observed that in both the cases result measures were
observed as a significant initial starting position for the execution and for observing moderations.
The researchers after completing the study concluded that the execution of the ICM enables the
effective application of quality-improvement creativities within.
In another study, Damberg et al. (2014) conducted a literature review where the
researchers summarized the available amount of knowledge regarding Value-based purchasing
(VBP) (Damberg et al. 2014). The information was collected from a set of published journals
and articles, a review of documents related to the VBP programs available to the public, and
discuss with an expert panel involving the VBP program sponsors, healthcare professionals and
healthcare systems, and academic researchers with VBP evaluation expertise. According to all
the gathered data, the researchers found that the VBP program sponsors have attained a huge
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6VALUE BASED-CARE
amount of experience through trial and error as they work to operate the VBP notion in the real-
world environment; though they are not being recorded appropriately as it is a new concept, and
researchers believe that VBP is advantageous to experiments during the early phase of VBP
development.
In another research paper conducted by Elf et al. (2017), the researchers tried to assess
the effectiveness of the value-based healthcare in the lives of the people living with complex and
long-term health conditions (Elf et al. 2017). The researchers concluded that in the value-based
health services related consequence measures with an associated compensation model are
thought to move development towards better quality. This progress has the ability to support the
healthcare-service provision with patient-centered care in an effort to take the patient’s
standpoint into account. The researchers also concluded that strategies should be formed to
administer the evaluation procedure regarding which consequence links to which performance. It
is particularly specific in disjointed healthcare organizations and for patients with chronic and
multi-setting-care requirements. Therefore, healthcare organizations strive to develop value-
based care which must cooperate outside of the organizational limitations to form clear patient
relationships.
Methodology
The methodology of this study involves a combination of primary research data as well as
internal healthcare industry expertise to conceptualize the overall framework, indicator list, and
research focus. As it is a research proposal, the information has been collected after thorough
research and assessment from a wide range of online databases like NCBI and Google scholar.
Both these databases are effective for searching existing literatures based on the topic of
amount of experience through trial and error as they work to operate the VBP notion in the real-
world environment; though they are not being recorded appropriately as it is a new concept, and
researchers believe that VBP is advantageous to experiments during the early phase of VBP
development.
In another research paper conducted by Elf et al. (2017), the researchers tried to assess
the effectiveness of the value-based healthcare in the lives of the people living with complex and
long-term health conditions (Elf et al. 2017). The researchers concluded that in the value-based
health services related consequence measures with an associated compensation model are
thought to move development towards better quality. This progress has the ability to support the
healthcare-service provision with patient-centered care in an effort to take the patient’s
standpoint into account. The researchers also concluded that strategies should be formed to
administer the evaluation procedure regarding which consequence links to which performance. It
is particularly specific in disjointed healthcare organizations and for patients with chronic and
multi-setting-care requirements. Therefore, healthcare organizations strive to develop value-
based care which must cooperate outside of the organizational limitations to form clear patient
relationships.
Methodology
The methodology of this study involves a combination of primary research data as well as
internal healthcare industry expertise to conceptualize the overall framework, indicator list, and
research focus. As it is a research proposal, the information has been collected after thorough
research and assessment from a wide range of online databases like NCBI and Google scholar.
Both these databases are effective for searching existing literatures based on the topic of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7VALUE BASED-CARE
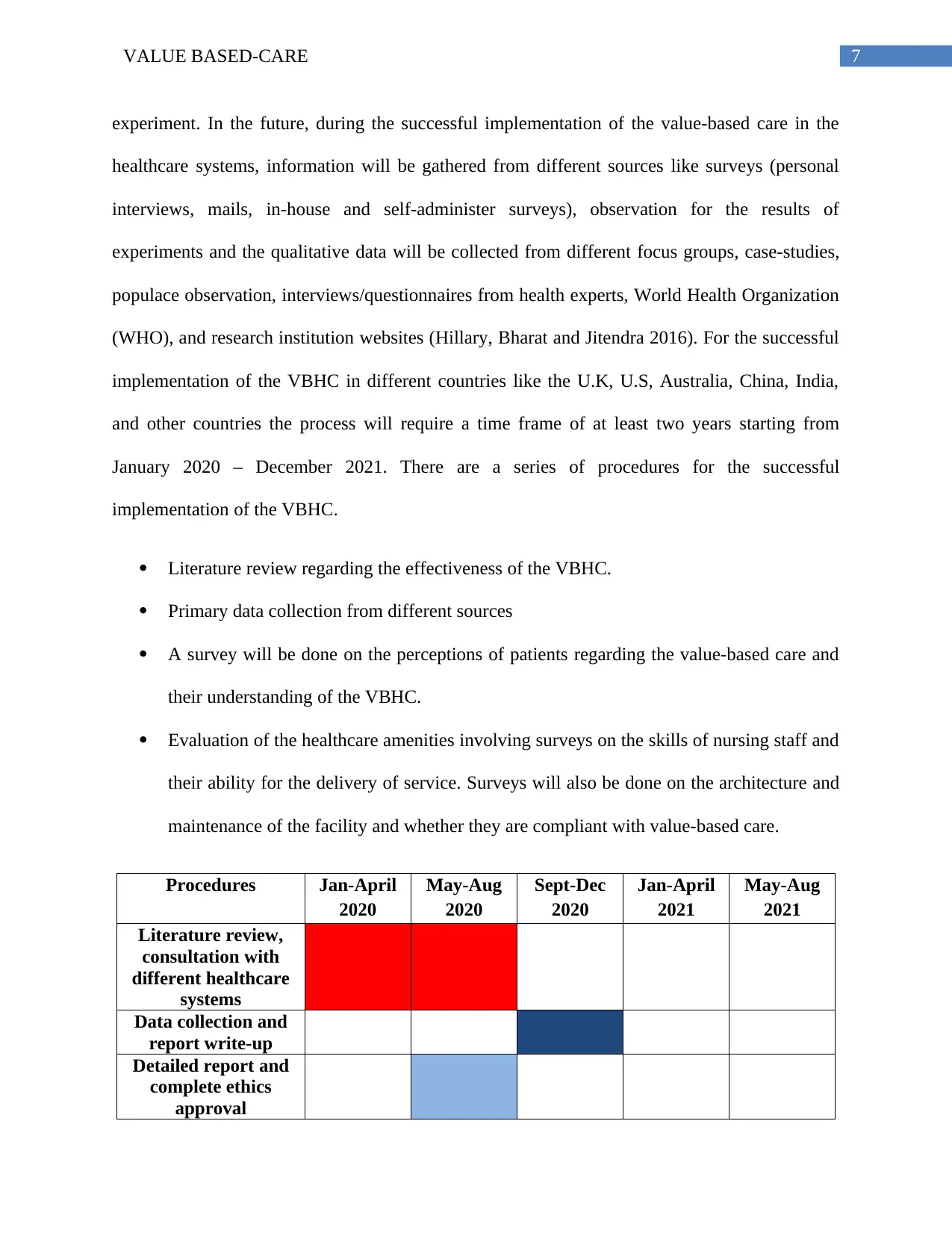
experiment. In the future, during the successful implementation of the value-based care in the
healthcare systems, information will be gathered from different sources like surveys (personal
interviews, mails, in-house and self-administer surveys), observation for the results of
experiments and the qualitative data will be collected from different focus groups, case-studies,
populace observation, interviews/questionnaires from health experts, World Health Organization
(WHO), and research institution websites (Hillary, Bharat and Jitendra 2016). For the successful
implementation of the VBHC in different countries like the U.K, U.S, Australia, China, India,
and other countries the process will require a time frame of at least two years starting from
January 2020 – December 2021. There are a series of procedures for the successful
implementation of the VBHC.
Literature review regarding the effectiveness of the VBHC.
Primary data collection from different sources
A survey will be done on the perceptions of patients regarding the value-based care and
their understanding of the VBHC.
Evaluation of the healthcare amenities involving surveys on the skills of nursing staff and
their ability for the delivery of service. Surveys will also be done on the architecture and
maintenance of the facility and whether they are compliant with value-based care.
Procedures Jan-April
2020
May-Aug
2020
Sept-Dec
2020
Jan-April
2021
May-Aug
2021
Literature review,
consultation with
different healthcare
systems
Data collection and
report write-up
Detailed report and
complete ethics
approval
experiment. In the future, during the successful implementation of the value-based care in the
healthcare systems, information will be gathered from different sources like surveys (personal
interviews, mails, in-house and self-administer surveys), observation for the results of
experiments and the qualitative data will be collected from different focus groups, case-studies,
populace observation, interviews/questionnaires from health experts, World Health Organization
(WHO), and research institution websites (Hillary, Bharat and Jitendra 2016). For the successful
implementation of the VBHC in different countries like the U.K, U.S, Australia, China, India,
and other countries the process will require a time frame of at least two years starting from
January 2020 – December 2021. There are a series of procedures for the successful
implementation of the VBHC.
Literature review regarding the effectiveness of the VBHC.
Primary data collection from different sources
A survey will be done on the perceptions of patients regarding the value-based care and
their understanding of the VBHC.
Evaluation of the healthcare amenities involving surveys on the skills of nursing staff and
their ability for the delivery of service. Surveys will also be done on the architecture and
maintenance of the facility and whether they are compliant with value-based care.
Procedures Jan-April
2020
May-Aug
2020
Sept-Dec
2020
Jan-April
2021
May-Aug
2021
Literature review,
consultation with
different healthcare
systems
Data collection and
report write-up
Detailed report and
complete ethics
approval
8VALUE BASED-CARE
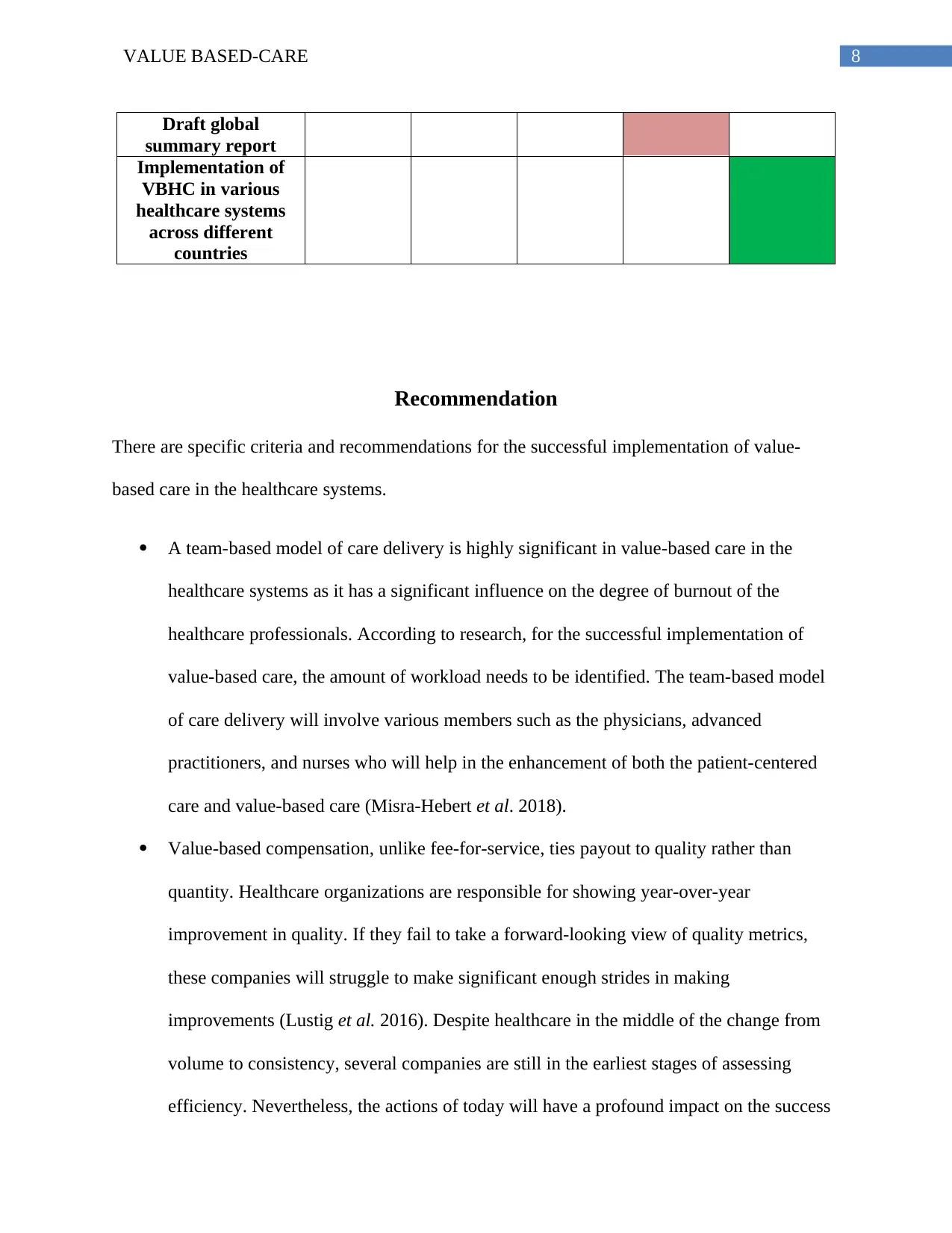
Draft global
summary report
Implementation of
VBHC in various
healthcare systems
across different
countries
Recommendation
There are specific criteria and recommendations for the successful implementation of value-
based care in the healthcare systems.
A team-based model of care delivery is highly significant in value-based care in the
healthcare systems as it has a significant influence on the degree of burnout of the
healthcare professionals. According to research, for the successful implementation of
value-based care, the amount of workload needs to be identified. The team-based model
of care delivery will involve various members such as the physicians, advanced
practitioners, and nurses who will help in the enhancement of both the patient-centered
care and value-based care (Misra-Hebert et al. 2018).
Value-based compensation, unlike fee-for-service, ties payout to quality rather than
quantity. Healthcare organizations are responsible for showing year-over-year
improvement in quality. If they fail to take a forward-looking view of quality metrics,
these companies will struggle to make significant enough strides in making
improvements (Lustig et al. 2016). Despite healthcare in the middle of the change from
volume to consistency, several companies are still in the earliest stages of assessing
efficiency. Nevertheless, the actions of today will have a profound impact on the success
Draft global
summary report
Implementation of
VBHC in various
healthcare systems
across different
countries
Recommendation
There are specific criteria and recommendations for the successful implementation of value-
based care in the healthcare systems.
A team-based model of care delivery is highly significant in value-based care in the
healthcare systems as it has a significant influence on the degree of burnout of the
healthcare professionals. According to research, for the successful implementation of
value-based care, the amount of workload needs to be identified. The team-based model
of care delivery will involve various members such as the physicians, advanced
practitioners, and nurses who will help in the enhancement of both the patient-centered
care and value-based care (Misra-Hebert et al. 2018).
Value-based compensation, unlike fee-for-service, ties payout to quality rather than
quantity. Healthcare organizations are responsible for showing year-over-year
improvement in quality. If they fail to take a forward-looking view of quality metrics,
these companies will struggle to make significant enough strides in making
improvements (Lustig et al. 2016). Despite healthcare in the middle of the change from
volume to consistency, several companies are still in the earliest stages of assessing
efficiency. Nevertheless, the actions of today will have a profound impact on the success
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9VALUE BASED-CARE
or loss of tomorrow in which therapeutic effectiveness rises. Providers must have a
strategy to achieve benefits over the lifetime of these contracts during their involvement
in risk-based agreements with payers (French, Guzman et al. 2016).
Healthcare providers will need to take greater responsibility for the treatment of the
individual through different care environments depending on the appropriate level of
acuity to meet the ultimate goals of value-based clinical. While the process of moving
away from the inconsistency synonymous with episodic, fee-for-service services can take
some time, in the near term, it now needs the commitment of these organizations to
identify areas where coordination and collaboration with other sections of the spectrum of
treatment can minimize care costs although maintaining a high quality of care.
Alternative models of reimbursement emphasized post-acute as a means of reducing
costs. These models can be used for the establishment of value based service for value
based treatment. The value-based treatment should be able to optimize the patient's
transition from the acute back home, ideally being able to move the patient to lower-care,
lower-cost environments earlier in the process while still ensuring the patient's health
(Hillary, Bharat and Jitendra 2016).
Conclusion
As this study reveals, several countries are still in the earliest stages of building the
enabling climate for realigning the importance of care provision. In many instances, discrete
programs are introduced and seldom form part of a structured value-based healthcare plan.
Nevertheless, while only a few countries are making significant strides to reconcile their
healthcare systems with VBHC's specific concepts, others are taking the first steps forward to
or loss of tomorrow in which therapeutic effectiveness rises. Providers must have a
strategy to achieve benefits over the lifetime of these contracts during their involvement
in risk-based agreements with payers (French, Guzman et al. 2016).
Healthcare providers will need to take greater responsibility for the treatment of the
individual through different care environments depending on the appropriate level of
acuity to meet the ultimate goals of value-based clinical. While the process of moving
away from the inconsistency synonymous with episodic, fee-for-service services can take
some time, in the near term, it now needs the commitment of these organizations to
identify areas where coordination and collaboration with other sections of the spectrum of
treatment can minimize care costs although maintaining a high quality of care.
Alternative models of reimbursement emphasized post-acute as a means of reducing
costs. These models can be used for the establishment of value based service for value
based treatment. The value-based treatment should be able to optimize the patient's
transition from the acute back home, ideally being able to move the patient to lower-care,
lower-cost environments earlier in the process while still ensuring the patient's health
(Hillary, Bharat and Jitendra 2016).
Conclusion
As this study reveals, several countries are still in the earliest stages of building the
enabling climate for realigning the importance of care provision. In many instances, discrete
programs are introduced and seldom form part of a structured value-based healthcare plan.
Nevertheless, while only a few countries are making significant strides to reconcile their
healthcare systems with VBHC's specific concepts, others are taking the first steps forward to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10VALUE BASED-CARE
reorganize their healthcare systems around the individual, with a greater focus on value
distribution.
A group of partners to embrace value-based treatment delivery and achieve long-term
success. Through ongoing support for physicians and treatment managers, a consistent
dedication to long-term strategic change, and an accurate alignment of internal and external
priorities, healthcare institutions have an opportunity to improve the quality and value of care
provided by their professionals. However, it is encouraging to see that some of the elements
needed to adopt VBHC are beginning to be put in place by countries. When technology advances
and innovative value-based solutions take hold in affluent nations, countries that are still invested
in improving their health systems have the opportunity to move immediately to value-based
treatment, conserve valuable resources and deliver better long-term care, leading to better results
for their residents.
reorganize their healthcare systems around the individual, with a greater focus on value
distribution.
A group of partners to embrace value-based treatment delivery and achieve long-term
success. Through ongoing support for physicians and treatment managers, a consistent
dedication to long-term strategic change, and an accurate alignment of internal and external
priorities, healthcare institutions have an opportunity to improve the quality and value of care
provided by their professionals. However, it is encouraging to see that some of the elements
needed to adopt VBHC are beginning to be put in place by countries. When technology advances
and innovative value-based solutions take hold in affluent nations, countries that are still invested
in improving their health systems have the opportunity to move immediately to value-based
treatment, conserve valuable resources and deliver better long-term care, leading to better results
for their residents.
11VALUE BASED-CARE
References
Baumhauer, J.F. and Bozic, K.J., 2016. Value-based healthcare: patient-reported outcomes in
clinical decision making. Clinical Orthopaedics and Related Research®, 474(6), pp.1375-1378.
Britto, M.T., Fuller, S.C., Kaplan, H.C., Kotagal, U., Lannon, C., Margolis, P.A., Muething,
S.E., Schoettker, P.J. and Seid, M., 2018. Using a network organisational architecture to support
the development of Learning Healthcare Systems. BMJ Qual Saf, 27(11), pp.937-946.
Colldén, C. and Hellström, A., 2018. Value-based healthcare translated: a complementary view
of implementation. BMC health services research, 18(1), p.681.
Damberg, C.L., Sorbero, M.E., Lovejoy, S.L., Martsolf, G.R., Raaen, L. and Mandel, D., 2014.
Measuring success in health care value-based purchasing programs: Findings from an
environmental scan, literature review, and expert panel discussions. Rand health quarterly, 4(3).
Elf, M., Flink, M., Nilsson, M., Tistad, M., von Koch, L. and Ytterberg, C., 2017. The case of
value-based healthcare for people living with complex long-term conditions. BMC health
services research, 17(1), p.24.
French, K. E., Guzman, A. B., Rubio, A. C., Frenzel, J. C., & Feeley, T. W. (2016, September).
Value based care and bundled payments: Anesthesia care costs for outpatient oncology surgery
using time-driven activity-based costing. In Healthcare (Vol. 4, No. 3, pp. 173-180). Elsevier.
Hillary, W., Justin, G., Bharat, M. and Jitendra, M., 2016. Value based healthcare. Advances in
Management, 9(1), p.1.
References
Baumhauer, J.F. and Bozic, K.J., 2016. Value-based healthcare: patient-reported outcomes in
clinical decision making. Clinical Orthopaedics and Related Research®, 474(6), pp.1375-1378.
Britto, M.T., Fuller, S.C., Kaplan, H.C., Kotagal, U., Lannon, C., Margolis, P.A., Muething,
S.E., Schoettker, P.J. and Seid, M., 2018. Using a network organisational architecture to support
the development of Learning Healthcare Systems. BMJ Qual Saf, 27(11), pp.937-946.
Colldén, C. and Hellström, A., 2018. Value-based healthcare translated: a complementary view
of implementation. BMC health services research, 18(1), p.681.
Damberg, C.L., Sorbero, M.E., Lovejoy, S.L., Martsolf, G.R., Raaen, L. and Mandel, D., 2014.
Measuring success in health care value-based purchasing programs: Findings from an
environmental scan, literature review, and expert panel discussions. Rand health quarterly, 4(3).
Elf, M., Flink, M., Nilsson, M., Tistad, M., von Koch, L. and Ytterberg, C., 2017. The case of
value-based healthcare for people living with complex long-term conditions. BMC health
services research, 17(1), p.24.
French, K. E., Guzman, A. B., Rubio, A. C., Frenzel, J. C., & Feeley, T. W. (2016, September).
Value based care and bundled payments: Anesthesia care costs for outpatient oncology surgery
using time-driven activity-based costing. In Healthcare (Vol. 4, No. 3, pp. 173-180). Elsevier.
Hillary, W., Justin, G., Bharat, M. and Jitendra, M., 2016. Value based healthcare. Advances in
Management, 9(1), p.1.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




