Variant Creutzfeldt-Jakob Disease (vCJD) and Non-Prion RPDs Analysis
VerifiedAdded on 2021/09/10
|7
|1350
|460
Report
AI Summary
This report provides an in-depth analysis of Variant Creutzfeldt-Jakob Disease (vCJD), a rapidly progressive dementia. It begins with an introduction to vCJD, including its definition and progression, and then delves into the symptoms, which include behavioral and psychiatric features, as well as sensory abnormalities. The report explores the disease pathology, highlighting the role of prion protein (PrP) and genetic mutations. The diagnosis of vCJD is also discussed, referencing EEG and MRI reports, and the detection of misfolded proteins. The report also considers non-prion RPDs, specifically autoimmune encephalopathies, comparing their symptoms, pathology, and diagnostic methods. References to relevant studies and research papers are included throughout the analysis. The report aims to provide a comprehensive understanding of both vCJD and autoimmune encephalopathies.

Running head: RAPIDLY PROGRESSIVE DEMENTIAS (RPDs)
Rapidly Progressive Dementias (RPDs)
Name of the Student
Name of the University
Author Note
Rapidly Progressive Dementias (RPDs)
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1RAPIDLY PROGRESSIVE DEMENTIAS (RPDs)
Introduction
The following paper aims to analyse variant Creutzfeldt-Jakob Disease (vCJD) which
is a rapid progressive dementias (RPD). In doing so, the paper will relate the case study with
prior disease symptoms and resease behind occurrence and will also compare VCJD with
non-prion RPDs.
Variant Creutzfeldt-Jakob disease (vCJD)
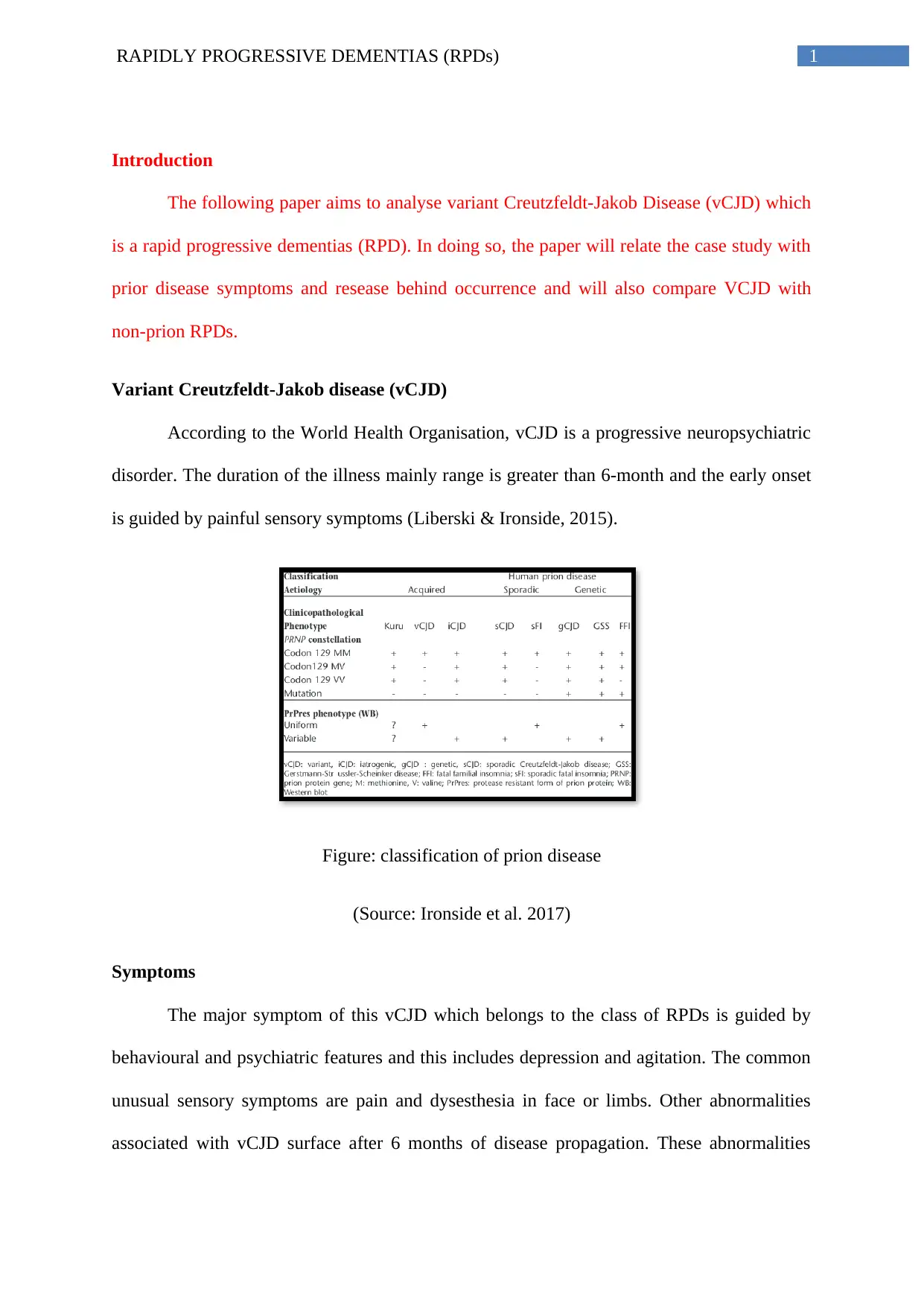
According to the World Health Organisation, vCJD is a progressive neuropsychiatric
disorder. The duration of the illness mainly range is greater than 6-month and the early onset
is guided by painful sensory symptoms (Liberski & Ironside, 2015).
Figure: classification of prion disease
(Source: Ironside et al. 2017)
Symptoms
The major symptom of this vCJD which belongs to the class of RPDs is guided by
behavioural and psychiatric features and this includes depression and agitation. The common
unusual sensory symptoms are pain and dysesthesia in face or limbs. Other abnormalities
associated with vCJD surface after 6 months of disease propagation. These abnormalities
Introduction
The following paper aims to analyse variant Creutzfeldt-Jakob Disease (vCJD) which
is a rapid progressive dementias (RPD). In doing so, the paper will relate the case study with
prior disease symptoms and resease behind occurrence and will also compare VCJD with
non-prion RPDs.
Variant Creutzfeldt-Jakob disease (vCJD)
According to the World Health Organisation, vCJD is a progressive neuropsychiatric
disorder. The duration of the illness mainly range is greater than 6-month and the early onset
is guided by painful sensory symptoms (Liberski & Ironside, 2015).
Figure: classification of prion disease
(Source: Ironside et al. 2017)
Symptoms
The major symptom of this vCJD which belongs to the class of RPDs is guided by
behavioural and psychiatric features and this includes depression and agitation. The common
unusual sensory symptoms are pain and dysesthesia in face or limbs. Other abnormalities
associated with vCJD surface after 6 months of disease propagation. These abnormalities
2RAPIDLY PROGRESSIVE DEMENTIAS (RPDs)
include cerebellar ataxia, dystonia, chorea, cognitive impairment and visual abnormalities.
The final stage of the disease is marked by the symptoms like akinetic mutism (Haïk &
Brandel, 2014).
Disease pathology
Apart from the stereotypic clinical features, the pathological phenotype of vCJD is
uniform in comparison to the other subtypes of CJD. However, Haïk and Brandel (2014)
highlighted that variations in the severity of the pathological lesions occurs with an increase
in the age of the individuals. The main causative agent of vCJD is the prior protein (PrP).
PrPc is the normal isoform of the disease while PrPd is the isoforrm of the misfolded (d
signifies for disease). The gene encoding PrP (PrPNP) is present in the polymphic nature in at
codon 129 (Val or Met). The Mutation of Met (methionine) is mutated to Valine (Val) at the
polymorphic codon leading to the disease development. The mutated isoform of the protein
(PrP) is abnormally mutated and thus leads to the accumulation of these abnormally folded
proteins in the brain leading to the disease development (Haïk & Brandel, 2014).
include cerebellar ataxia, dystonia, chorea, cognitive impairment and visual abnormalities.
The final stage of the disease is marked by the symptoms like akinetic mutism (Haïk &
Brandel, 2014).
Disease pathology
Apart from the stereotypic clinical features, the pathological phenotype of vCJD is
uniform in comparison to the other subtypes of CJD. However, Haïk and Brandel (2014)
highlighted that variations in the severity of the pathological lesions occurs with an increase
in the age of the individuals. The main causative agent of vCJD is the prior protein (PrP).
PrPc is the normal isoform of the disease while PrPd is the isoforrm of the misfolded (d
signifies for disease). The gene encoding PrP (PrPNP) is present in the polymphic nature in at
codon 129 (Val or Met). The Mutation of Met (methionine) is mutated to Valine (Val) at the
polymorphic codon leading to the disease development. The mutated isoform of the protein
(PrP) is abnormally mutated and thus leads to the accumulation of these abnormally folded
proteins in the brain leading to the disease development (Haïk & Brandel, 2014).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

3RAPIDLY PROGRESSIVE DEMENTIAS (RPDs)
Figure: Mutation in Prion Disease
(Source: Haïk & Brandel, 2014)
Diagnosis
The analysis of the EEG reports of the patients suffering of vCJD highlighted that
abnormalities are mainly detected during later stages of diseases however those abnormalities
are non-specific. The analysis of the MRI reports of individuals suffering from vCJD
highlighted abnormality in the posterior thalamic region. The deposition of the mis-folded
protein gives rise to florid plaques in the cerebral and cerebellar cortex that stains intensively
in immunohistochemistry test (Haïk & Brandel, 2014).Autospy can also be regarded as an
important detection method for prion disease as used in the case study of Susan (Ironside,
Figure: Mutation in Prion Disease
(Source: Haïk & Brandel, 2014)
Diagnosis
The analysis of the EEG reports of the patients suffering of vCJD highlighted that
abnormalities are mainly detected during later stages of diseases however those abnormalities
are non-specific. The analysis of the MRI reports of individuals suffering from vCJD
highlighted abnormality in the posterior thalamic region. The deposition of the mis-folded
protein gives rise to florid plaques in the cerebral and cerebellar cortex that stains intensively
in immunohistochemistry test (Haïk & Brandel, 2014).Autospy can also be regarded as an
important detection method for prion disease as used in the case study of Susan (Ironside,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4RAPIDLY PROGRESSIVE DEMENTIAS (RPDs)
Ritchie & Head, 2017). Furthermore, urine can also be used for the detection of the VCJD.
According to the study conducted by Moda et al. (2014) people suffering from vCJD as
traces of prion protein excreted through urine.
In relation to the case study it can be said that development of the prion disease in
case of Susan is not solely associated with the contamination arising from beef products
afflicted with bovine spongiform encephalopathy. Other source of the development of prion
disease might be hormonal treatment which she received during 1979-1983 for Turner’s
syndrome. According to Cali et al. (2015) administration of prion contaminated human
growth hormone results in the development of CDJ. This human growth hormone acquired
CJD has similar symptoms and pathology of MRI reports as compared to mad cow disease or
bovine spongiform encephalopathy.
Non-prion RPD
The non-prion RPD selected is autoimmune encephalopathies. According to
Geschwind (2016), aside from prion diseases, few of the common cause of RPD are regarded
as the atypical presentation of neurodegenerative disorders. One of the common examples of
atypical neurodegenerative disorder is autoimmune encephalopathies (Geschwind, 2016).
Symptoms
The main symptoms of autoimmune encephalopathies are loss of memory, altered
level of cognition, fluctuation of mood and difficulty in retaining new information. The other
symptoms of autoimmune encephalopathy include psychoss, dystona chorea, hyperekplexia,
status epilepticus, fasciobrachial dystonic seizures, neuromyotonia, muscle spasms,
fasculations, exaggerated startle, stiff-person syndrome, delirum and myoclonus. The
psychiatric manifestations are common during the early phase of life (Lancaster, 2016).
Ritchie & Head, 2017). Furthermore, urine can also be used for the detection of the VCJD.
According to the study conducted by Moda et al. (2014) people suffering from vCJD as
traces of prion protein excreted through urine.
In relation to the case study it can be said that development of the prion disease in
case of Susan is not solely associated with the contamination arising from beef products
afflicted with bovine spongiform encephalopathy. Other source of the development of prion
disease might be hormonal treatment which she received during 1979-1983 for Turner’s
syndrome. According to Cali et al. (2015) administration of prion contaminated human
growth hormone results in the development of CDJ. This human growth hormone acquired
CJD has similar symptoms and pathology of MRI reports as compared to mad cow disease or
bovine spongiform encephalopathy.
Non-prion RPD
The non-prion RPD selected is autoimmune encephalopathies. According to
Geschwind (2016), aside from prion diseases, few of the common cause of RPD are regarded
as the atypical presentation of neurodegenerative disorders. One of the common examples of
atypical neurodegenerative disorder is autoimmune encephalopathies (Geschwind, 2016).
Symptoms
The main symptoms of autoimmune encephalopathies are loss of memory, altered
level of cognition, fluctuation of mood and difficulty in retaining new information. The other
symptoms of autoimmune encephalopathy include psychoss, dystona chorea, hyperekplexia,
status epilepticus, fasciobrachial dystonic seizures, neuromyotonia, muscle spasms,
fasculations, exaggerated startle, stiff-person syndrome, delirum and myoclonus. The
psychiatric manifestations are common during the early phase of life (Lancaster, 2016).
5RAPIDLY PROGRESSIVE DEMENTIAS (RPDs)
Pathology
The pathology is autoimmune encephalopathies is mainly dominated by the formation
antibodies for the intracellular antigens (anti-Hu). These disorders are mainly associated with
cancer disease development and mainly involve the T-cell responses targeting the neurons
(Lancaster, 2016). The prognosis of the disease is poor due to irreversible damage of the
neurons. Another form of the autoimmune encephaloathies leads to the development of
antibodies against extracellular epitopes of the ion channels and NMDA receptors. The auto-
antibodies which are generated in this disorder are regarded to be directly pathogenic for
causing reversible effects over the synaptic neurons with neuronal death (Lancaster, 2016).
Diagnosis
The main mode of detection or the diagnosis of autoimmune encephalopathies is
biomarkers (Lancaster, 2016). Other diagnostic approaches that are used for the diagnosis of
autoimmune encephalopathies include autoantibody testing (Graus et al., 2016). The most
sensitive auto-antibody is NMDAR antibody (Graus et al., 2016). Brain imaging through
MRI is also used for the diagnosis of autoimmune encepathopathies (Lancaster, 2016).
Pathology
The pathology is autoimmune encephalopathies is mainly dominated by the formation
antibodies for the intracellular antigens (anti-Hu). These disorders are mainly associated with
cancer disease development and mainly involve the T-cell responses targeting the neurons
(Lancaster, 2016). The prognosis of the disease is poor due to irreversible damage of the
neurons. Another form of the autoimmune encephaloathies leads to the development of
antibodies against extracellular epitopes of the ion channels and NMDA receptors. The auto-
antibodies which are generated in this disorder are regarded to be directly pathogenic for
causing reversible effects over the synaptic neurons with neuronal death (Lancaster, 2016).
Diagnosis
The main mode of detection or the diagnosis of autoimmune encephalopathies is
biomarkers (Lancaster, 2016). Other diagnostic approaches that are used for the diagnosis of
autoimmune encephalopathies include autoantibody testing (Graus et al., 2016). The most
sensitive auto-antibody is NMDAR antibody (Graus et al., 2016). Brain imaging through
MRI is also used for the diagnosis of autoimmune encepathopathies (Lancaster, 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

6RAPIDLY PROGRESSIVE DEMENTIAS (RPDs)
References
Cali, I., Miller, C. J., Parisi, J. E., Geschwind, M. D., Gambetti, P., & Schonberger, L. B.
(2015). Distinct pathological phenotypes of Creutzfeldt-Jakob disease in recipients of
prion-contaminated growth hormone. Acta neuropathologica communications, 3(1),
37.
Geschwind, M. D. (2016). Rapidly progressive dementia. Continuum: Lifelong Learning in
Neurology, 22(2 Dementia), 510.
Graus, F., Titulaer, M. J., Balu, R., Benseler, S., Bien, C. G., Cellucci, T., ... & Glaser, C. A.
(2016). A clinical approach to diagnosis of autoimmune encephalitis. The Lancet
Neurology, 15(4), 391-404.
Haïk, S., & Brandel, J. P. (2014). Infectious prion diseases in humans: cannibalism,
iatrogenicity and zoonoses. Infection, Genetics and Evolution, 26, 303-312.
Ironside, J. W., Ritchie, D. L., & Head, M. W. (2017). Prion diseases. In Handbook of
clinical neurology (Vol. 145, pp. 393-403). Elsevier.
Lancaster, E. (2016). The diagnosis and treatment of autoimmune encephalitis. Journal of
Clinical Neurology, 12(1), 1-13.
Liberski, P. P., & Ironside, J. W. (2015). Prion Diseases. In Neurobiology of Brain
Disorders (pp. 356-374).
Moda, F., Gambetti, P., Notari, S., Concha-Marambio, L., Catania, M., Park, K. W., ... &
Ironside, J. (2014). Prions in the urine of patients with variant Creutzfeldt–Jakob
disease. New England Journal of Medicine, 371(6), 530-539.
References
Cali, I., Miller, C. J., Parisi, J. E., Geschwind, M. D., Gambetti, P., & Schonberger, L. B.
(2015). Distinct pathological phenotypes of Creutzfeldt-Jakob disease in recipients of
prion-contaminated growth hormone. Acta neuropathologica communications, 3(1),
37.
Geschwind, M. D. (2016). Rapidly progressive dementia. Continuum: Lifelong Learning in
Neurology, 22(2 Dementia), 510.
Graus, F., Titulaer, M. J., Balu, R., Benseler, S., Bien, C. G., Cellucci, T., ... & Glaser, C. A.
(2016). A clinical approach to diagnosis of autoimmune encephalitis. The Lancet
Neurology, 15(4), 391-404.
Haïk, S., & Brandel, J. P. (2014). Infectious prion diseases in humans: cannibalism,
iatrogenicity and zoonoses. Infection, Genetics and Evolution, 26, 303-312.
Ironside, J. W., Ritchie, D. L., & Head, M. W. (2017). Prion diseases. In Handbook of
clinical neurology (Vol. 145, pp. 393-403). Elsevier.
Lancaster, E. (2016). The diagnosis and treatment of autoimmune encephalitis. Journal of
Clinical Neurology, 12(1), 1-13.
Liberski, P. P., & Ironside, J. W. (2015). Prion Diseases. In Neurobiology of Brain
Disorders (pp. 356-374).
Moda, F., Gambetti, P., Notari, S., Concha-Marambio, L., Catania, M., Park, K. W., ... &
Ironside, J. (2014). Prions in the urine of patients with variant Creutzfeldt–Jakob
disease. New England Journal of Medicine, 371(6), 530-539.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


