Healthcare Case Study: Management of Venous Ulcer in Mrs. A
VerifiedAdded on 2023/01/23
|12
|3354
|96
Case Study
AI Summary
This case study presents the case of Mrs. A, a 72-year-old woman with a three-year history of a venous ulcer on her left leg, complicated by rheumatoid arthritis, steroid-induced type 2 diabetes, and a history of neuropathic pain. The assignment details her medical history, including previous surgeries, medications, and allergies, providing a comprehensive overview of her health status. The assessment reveals the ulcer's characteristics, including size, exudate, odor, and appearance, alongside an evaluation of her pain levels and lifestyle factors. The diagnosis focuses on venous insufficiency, supported by vascular studies. The management plan encompasses assessment, treatment, and evaluation phases, emphasizing compression therapy, wound dressing, exercise, and pain management strategies. Challenges encountered during treatment, such as the patient's non-responsiveness to compression therapy due to nerve pain, are highlighted, along with the need for alternative approaches. The case study showcases the complexities of managing chronic wounds in elderly patients with multiple comorbidities, underscoring the importance of a holistic approach to care and the iterative process of treatment and evaluation.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction/Background Condition
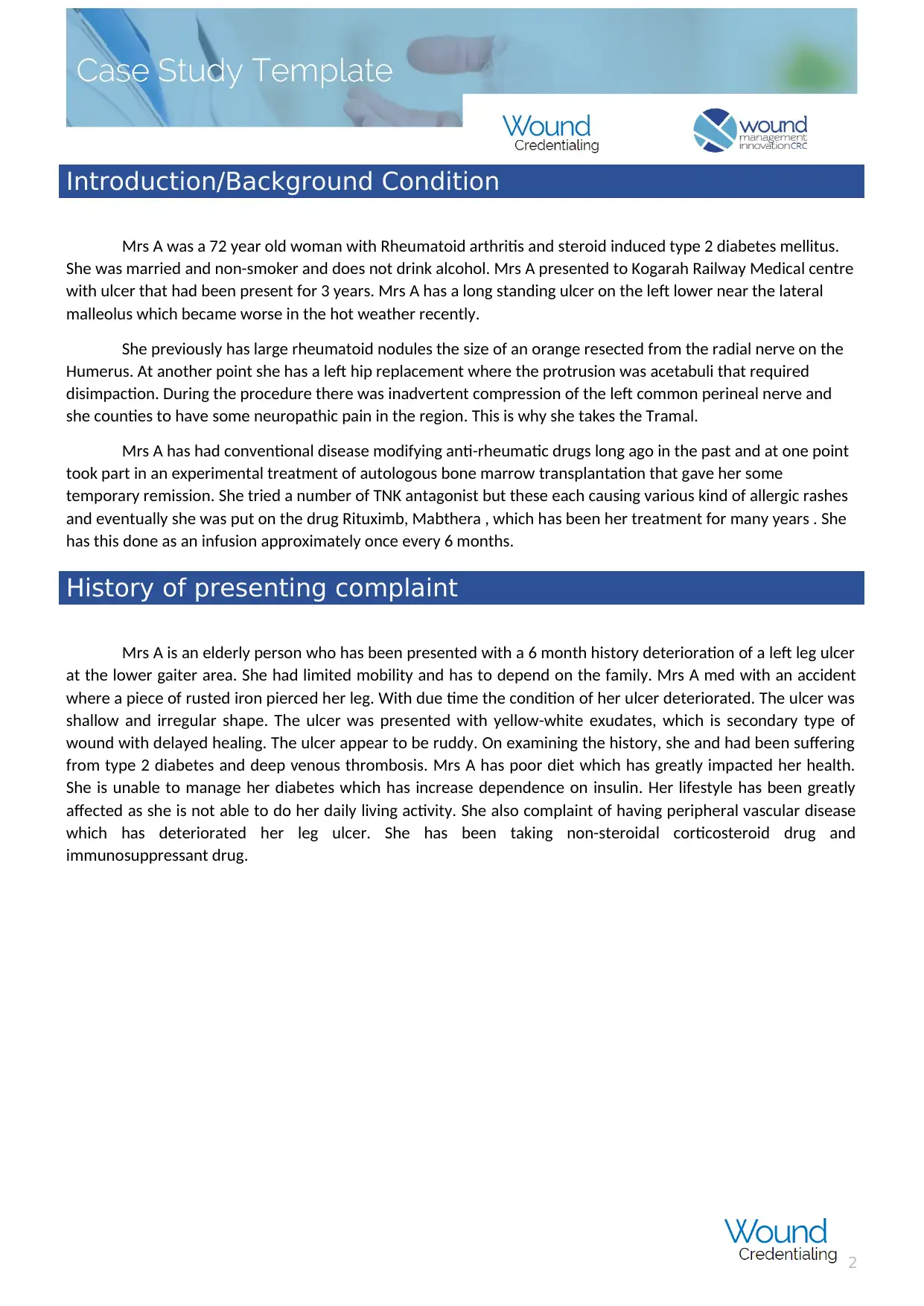
Mrs A was a 72 year old woman with Rheumatoid arthritis and steroid induced type 2 diabetes mellitus.
She was married and non-smoker and does not drink alcohol. Mrs A presented to Kogarah Railway Medical centre
with ulcer that had been present for 3 years. Mrs A has a long standing ulcer on the left lower near the lateral
malleolus which became worse in the hot weather recently.
She previously has large rheumatoid nodules the size of an orange resected from the radial nerve on the
Humerus. At another point she has a left hip replacement where the protrusion was acetabuli that required
disimpaction. During the procedure there was inadvertent compression of the left common perineal nerve and
she counties to have some neuropathic pain in the region. This is why she takes the Tramal.
Mrs A has had conventional disease modifying anti-rheumatic drugs long ago in the past and at one point
took part in an experimental treatment of autologous bone marrow transplantation that gave her some
temporary remission. She tried a number of TNK antagonist but these each causing various kind of allergic rashes
and eventually she was put on the drug Rituximb, Mabthera , which has been her treatment for many years . She
has this done as an infusion approximately once every 6 months.
History of presenting complaint
Mrs A is an elderly person who has been presented with a 6 month history deterioration of a left leg ulcer
at the lower gaiter area. She had limited mobility and has to depend on the family. Mrs A med with an accident
where a piece of rusted iron pierced her leg. With due time the condition of her ulcer deteriorated. The ulcer was
shallow and irregular shape. The ulcer was presented with yellow-white exudates, which is secondary type of
wound with delayed healing. The ulcer appear to be ruddy. On examining the history, she and had been suffering
from type 2 diabetes and deep venous thrombosis. Mrs A has poor diet which has greatly impacted her health.
She is unable to manage her diabetes which has increase dependence on insulin. Her lifestyle has been greatly
affected as she is not able to do her daily living activity. She also complaint of having peripheral vascular disease
which has deteriorated her leg ulcer. She has been taking non-steroidal corticosteroid drug and
immunosuppressant drug.
2
Mrs A was a 72 year old woman with Rheumatoid arthritis and steroid induced type 2 diabetes mellitus.
She was married and non-smoker and does not drink alcohol. Mrs A presented to Kogarah Railway Medical centre
with ulcer that had been present for 3 years. Mrs A has a long standing ulcer on the left lower near the lateral
malleolus which became worse in the hot weather recently.
She previously has large rheumatoid nodules the size of an orange resected from the radial nerve on the
Humerus. At another point she has a left hip replacement where the protrusion was acetabuli that required
disimpaction. During the procedure there was inadvertent compression of the left common perineal nerve and
she counties to have some neuropathic pain in the region. This is why she takes the Tramal.
Mrs A has had conventional disease modifying anti-rheumatic drugs long ago in the past and at one point
took part in an experimental treatment of autologous bone marrow transplantation that gave her some
temporary remission. She tried a number of TNK antagonist but these each causing various kind of allergic rashes
and eventually she was put on the drug Rituximb, Mabthera , which has been her treatment for many years . She
has this done as an infusion approximately once every 6 months.
History of presenting complaint
Mrs A is an elderly person who has been presented with a 6 month history deterioration of a left leg ulcer
at the lower gaiter area. She had limited mobility and has to depend on the family. Mrs A med with an accident
where a piece of rusted iron pierced her leg. With due time the condition of her ulcer deteriorated. The ulcer was
shallow and irregular shape. The ulcer was presented with yellow-white exudates, which is secondary type of
wound with delayed healing. The ulcer appear to be ruddy. On examining the history, she and had been suffering
from type 2 diabetes and deep venous thrombosis. Mrs A has poor diet which has greatly impacted her health.
She is unable to manage her diabetes which has increase dependence on insulin. Her lifestyle has been greatly
affected as she is not able to do her daily living activity. She also complaint of having peripheral vascular disease
which has deteriorated her leg ulcer. She has been taking non-steroidal corticosteroid drug and
immunosuppressant drug.
2
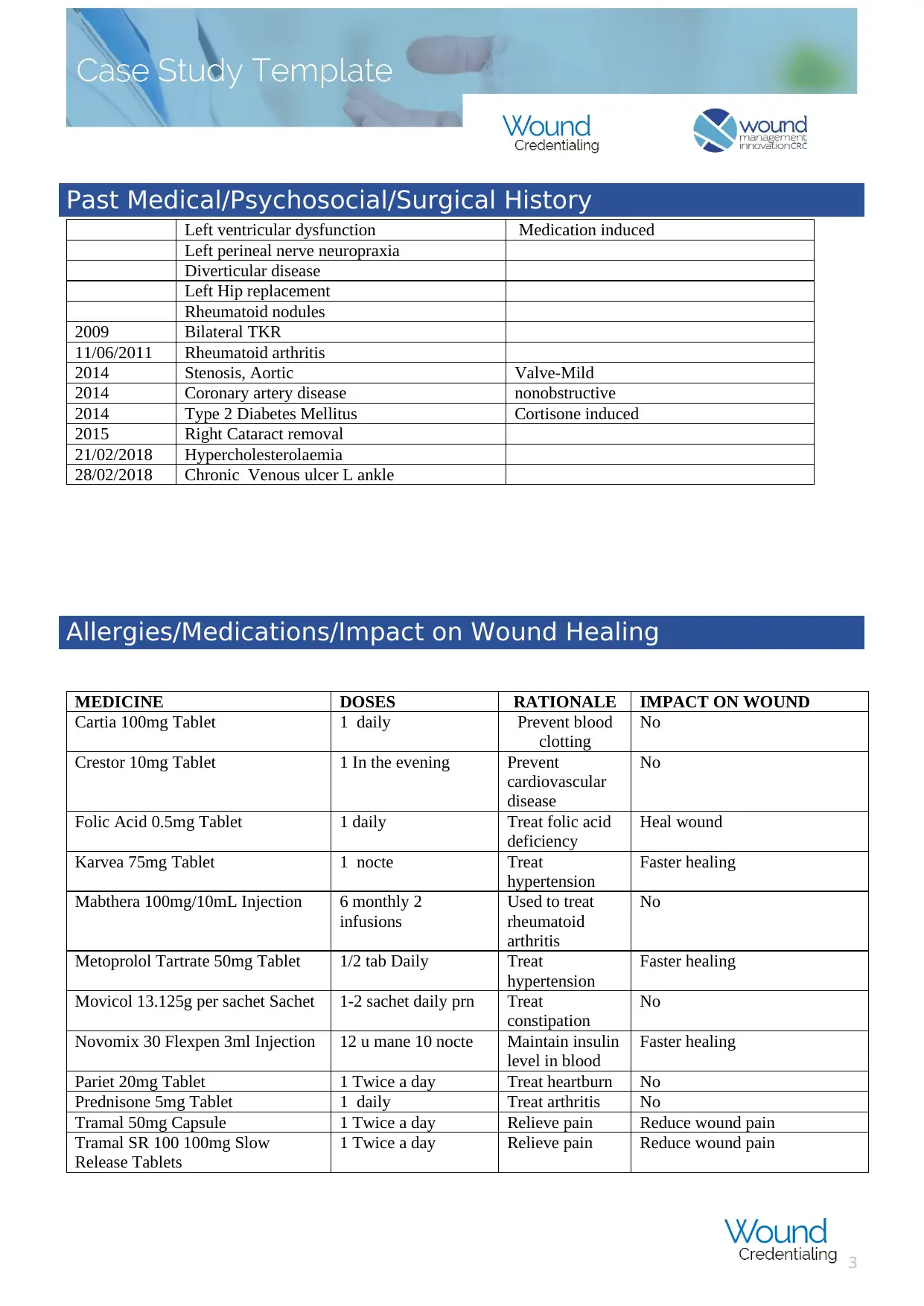
Past Medical/Psychosocial/Surgical History
Left ventricular dysfunction Medication induced
Left perineal nerve neuropraxia
Diverticular disease
Left Hip replacement
Rheumatoid nodules
2009 Bilateral TKR
11/06/2011 Rheumatoid arthritis
2014 Stenosis, Aortic Valve-Mild
2014 Coronary artery disease nonobstructive
2014 Type 2 Diabetes Mellitus Cortisone induced
2015 Right Cataract removal
21/02/2018 Hypercholesterolaemia
28/02/2018 Chronic Venous ulcer L ankle
Allergies/Medications/Impact on Wound Healing
MEDICINE DOSES RATIONALE IMPACT ON WOUND
Cartia 100mg Tablet 1 daily Prevent blood
clotting
No
Crestor 10mg Tablet 1 In the evening Prevent
cardiovascular
disease
No
Folic Acid 0.5mg Tablet 1 daily Treat folic acid
deficiency
Heal wound
Karvea 75mg Tablet 1 nocte Treat
hypertension
Faster healing
Mabthera 100mg/10mL Injection 6 monthly 2
infusions
Used to treat
rheumatoid
arthritis
No
Metoprolol Tartrate 50mg Tablet 1/2 tab Daily Treat
hypertension
Faster healing
Movicol 13.125g per sachet Sachet 1-2 sachet daily prn Treat
constipation
No
Novomix 30 Flexpen 3ml Injection 12 u mane 10 nocte Maintain insulin
level in blood
Faster healing
Pariet 20mg Tablet 1 Twice a day Treat heartburn No
Prednisone 5mg Tablet 1 daily Treat arthritis No
Tramal 50mg Capsule 1 Twice a day Relieve pain Reduce wound pain
Tramal SR 100 100mg Slow
Release Tablets
1 Twice a day Relieve pain Reduce wound pain
3
Left ventricular dysfunction Medication induced
Left perineal nerve neuropraxia
Diverticular disease
Left Hip replacement
Rheumatoid nodules
2009 Bilateral TKR
11/06/2011 Rheumatoid arthritis
2014 Stenosis, Aortic Valve-Mild
2014 Coronary artery disease nonobstructive
2014 Type 2 Diabetes Mellitus Cortisone induced
2015 Right Cataract removal
21/02/2018 Hypercholesterolaemia
28/02/2018 Chronic Venous ulcer L ankle
Allergies/Medications/Impact on Wound Healing
MEDICINE DOSES RATIONALE IMPACT ON WOUND
Cartia 100mg Tablet 1 daily Prevent blood
clotting
No
Crestor 10mg Tablet 1 In the evening Prevent
cardiovascular
disease
No
Folic Acid 0.5mg Tablet 1 daily Treat folic acid
deficiency
Heal wound
Karvea 75mg Tablet 1 nocte Treat
hypertension
Faster healing
Mabthera 100mg/10mL Injection 6 monthly 2
infusions
Used to treat
rheumatoid
arthritis
No
Metoprolol Tartrate 50mg Tablet 1/2 tab Daily Treat
hypertension
Faster healing
Movicol 13.125g per sachet Sachet 1-2 sachet daily prn Treat
constipation
No
Novomix 30 Flexpen 3ml Injection 12 u mane 10 nocte Maintain insulin
level in blood
Faster healing
Pariet 20mg Tablet 1 Twice a day Treat heartburn No
Prednisone 5mg Tablet 1 daily Treat arthritis No
Tramal 50mg Capsule 1 Twice a day Relieve pain Reduce wound pain
Tramal SR 100 100mg Slow
Release Tablets
1 Twice a day Relieve pain Reduce wound pain
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
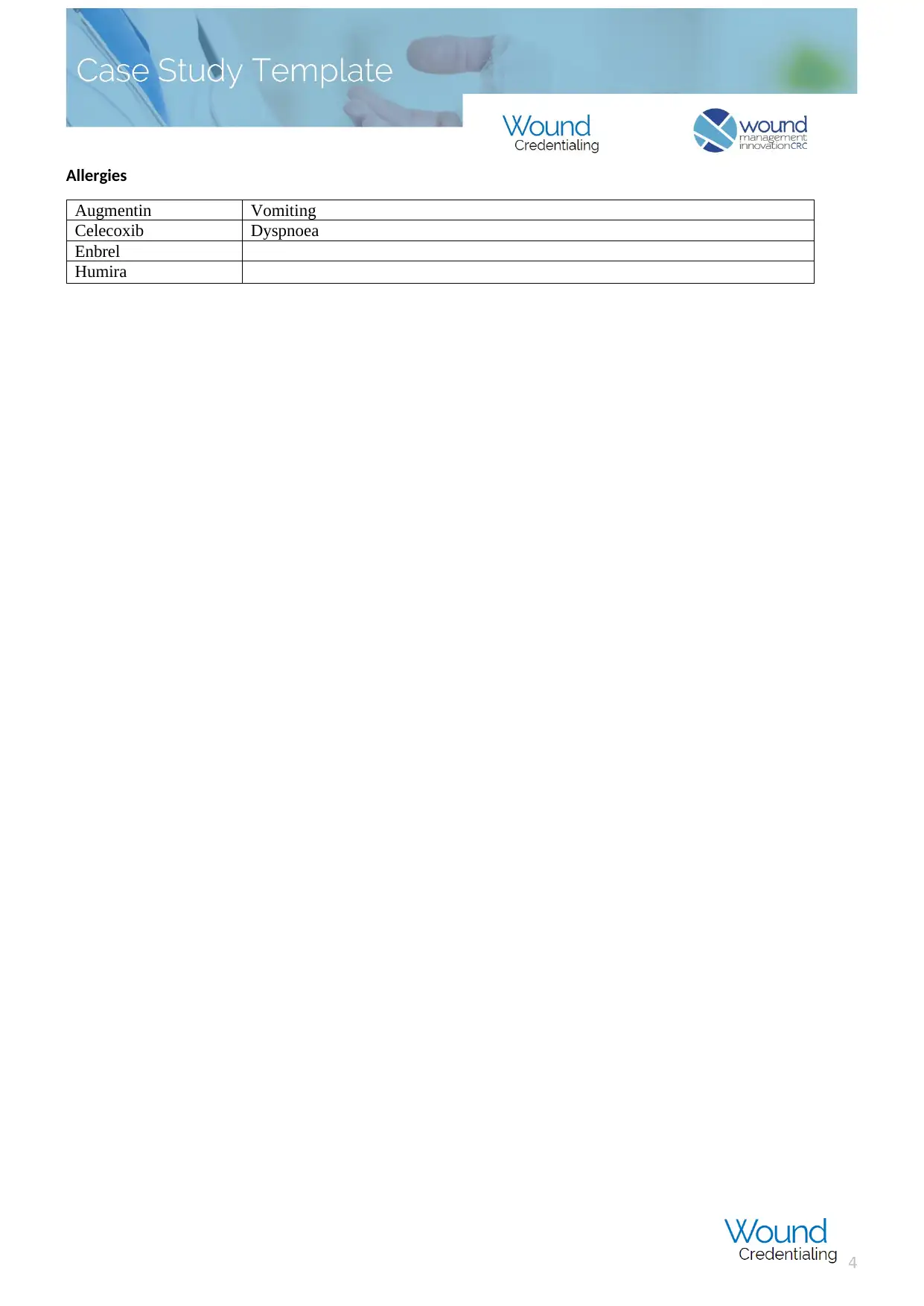
Allergies
Augmentin Vomiting
Celecoxib Dyspnoea
Enbrel
Humira
4
Augmentin Vomiting
Celecoxib Dyspnoea
Enbrel
Humira
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Focused Assessment
Measure- The size of the wound was of 7*6cm in diameter with 7 com deep infection.
Exudate- Based on the significant amount of erythema and maceration surrounding the wound, and the
appearance of a moist wound bed. The exudate was high and large discharge of the pus infected with the
bacteria.
Quality- The wound was showing with purulent consistent with heavy infection by the bacteria.
Odour- The wound as having strong and stingy odour. The exudate was yellow in colour which proved to be
infected and because of this, bad smell was emerging from the wound.
Appearance- The appearance of wound was red with 90% loose necrotic slough and 10% granulation was
observed around the wound circumference of wound bed. On assessment of the wound, the deeper structure
was not visible though it can be palpable. The patient has shown hyperkeratosis.
Suffering- The patient was suffering from severe pain at night which is due to compression of the left common
perineal nerve and she also have neuropathic pain in that region. The pain assessment was done using validated
pain tool accompanied with the wound history of the patient.
Undermining- Nothing was founded
Re-evaluate- For re-evaluation, three time the wound is dressed initially and weekly assessment of both pressure
injury healing, and ongoing risk assessment. In this wound frequent assessment at each dressing change need to
be monitor for resolution of infection or wound deterioration. The frequency of dressing changes is determined
by the wound management plan which will consider the exudate management.
Edge- The edge of the wound was irregular and wound bed appears moist. The surrounding skin is much
macerated from contact with moisture/exudate. Parts of the epidermis is sheering away. Peri wound erythema, is
evident, as would be expected with wound infection.
On assessing the wound of the patient it was observed that the she was having venous leg ulcer located in
the left lower gaiter region near the lateral malleolus. The size of the wound was determined which showed the
size of 7cmx6cm. On determination of etiology of the wound, ABI was noted to be 0.80 which showed venous
insufficiency. Hence it is Suitable for compression. No biopsy was done of the wound as it was not required. The
wound had adequate flow of blood which has been presented in the patient for 3 years. The wound was not
tunnelling or undermining and no bone was exposed, however it was having stingy odour. The odour was due to
large discharge of exudate from the wound and showed pale yellow coloration. On assessing the skin, it showed
large amount of necrotic, granulation and epithelial tissue. The edge of the wound was irregular. Previously
Betadine and Melolin was used as wound dressing and Changed every 2 days.
The patient was reported to have average nutrition intake and does not take any supplement. The fluid
intake is 2L per day. The patient was having normal limits of albumin and non-albumin levels. She was taking the
following medicine.
Cartia 100mg Tablet
Crestor 10mg Tablet
Folic Acid 0.5mg Tablet
Karvea 75mg Tablet
5
Measure- The size of the wound was of 7*6cm in diameter with 7 com deep infection.
Exudate- Based on the significant amount of erythema and maceration surrounding the wound, and the
appearance of a moist wound bed. The exudate was high and large discharge of the pus infected with the
bacteria.
Quality- The wound was showing with purulent consistent with heavy infection by the bacteria.
Odour- The wound as having strong and stingy odour. The exudate was yellow in colour which proved to be
infected and because of this, bad smell was emerging from the wound.
Appearance- The appearance of wound was red with 90% loose necrotic slough and 10% granulation was
observed around the wound circumference of wound bed. On assessment of the wound, the deeper structure
was not visible though it can be palpable. The patient has shown hyperkeratosis.
Suffering- The patient was suffering from severe pain at night which is due to compression of the left common
perineal nerve and she also have neuropathic pain in that region. The pain assessment was done using validated
pain tool accompanied with the wound history of the patient.
Undermining- Nothing was founded
Re-evaluate- For re-evaluation, three time the wound is dressed initially and weekly assessment of both pressure
injury healing, and ongoing risk assessment. In this wound frequent assessment at each dressing change need to
be monitor for resolution of infection or wound deterioration. The frequency of dressing changes is determined
by the wound management plan which will consider the exudate management.
Edge- The edge of the wound was irregular and wound bed appears moist. The surrounding skin is much
macerated from contact with moisture/exudate. Parts of the epidermis is sheering away. Peri wound erythema, is
evident, as would be expected with wound infection.
On assessing the wound of the patient it was observed that the she was having venous leg ulcer located in
the left lower gaiter region near the lateral malleolus. The size of the wound was determined which showed the
size of 7cmx6cm. On determination of etiology of the wound, ABI was noted to be 0.80 which showed venous
insufficiency. Hence it is Suitable for compression. No biopsy was done of the wound as it was not required. The
wound had adequate flow of blood which has been presented in the patient for 3 years. The wound was not
tunnelling or undermining and no bone was exposed, however it was having stingy odour. The odour was due to
large discharge of exudate from the wound and showed pale yellow coloration. On assessing the skin, it showed
large amount of necrotic, granulation and epithelial tissue. The edge of the wound was irregular. Previously
Betadine and Melolin was used as wound dressing and Changed every 2 days.
The patient was reported to have average nutrition intake and does not take any supplement. The fluid
intake is 2L per day. The patient was having normal limits of albumin and non-albumin levels. She was taking the
following medicine.
Cartia 100mg Tablet
Crestor 10mg Tablet
Folic Acid 0.5mg Tablet
Karvea 75mg Tablet
5
Mabthera 100mg/10mL Injection
Metoprolol Tartrate 50mg Tablet
Movicol 13.125g per sachet Sachet
Novomix 30 Flexpen 3ml Injection
Pariet 20mg Tablet
Prednisone 5mg Tablet
Tramal 50mg Capsule
Tramal SR 100 100mg Slow Release Tablets
The patient's HgA1C 7.5% and complete blood count is HB 128. The history of patient tells that she is non-smoker
and does not consumes alcohol
Diagnosis
Full assessment of wound has been done of the patient to draw the diagnosis. On evaluating provisional
diagnosis of venous insufficiency has been determined. The doctor were not confirmed about the diagnosis hence
the present history, physical and social risk factor has been resolute. The patient had traumatic leg Injury due to
which she has become immobile. Though she also had diabetes and does not show any history of DVT reflect
towards arterial ulcer. However, the position of leg injury is at gaiter area which can be the reason for venous
ulcer. As 95% of the venous ulcer is that position. Therefore the differential diagnosis of type of ulcer can get
related to either arterial or venous ulcer. To get into definitive diagnosis vascular studies has been done which
showed left ABPI of 0.80, right ABPI of 1.0. To verify the vascular status, duplex ultrasound has been conducted.
6
Metoprolol Tartrate 50mg Tablet
Movicol 13.125g per sachet Sachet
Novomix 30 Flexpen 3ml Injection
Pariet 20mg Tablet
Prednisone 5mg Tablet
Tramal 50mg Capsule
Tramal SR 100 100mg Slow Release Tablets
The patient's HgA1C 7.5% and complete blood count is HB 128. The history of patient tells that she is non-smoker
and does not consumes alcohol
Diagnosis
Full assessment of wound has been done of the patient to draw the diagnosis. On evaluating provisional
diagnosis of venous insufficiency has been determined. The doctor were not confirmed about the diagnosis hence
the present history, physical and social risk factor has been resolute. The patient had traumatic leg Injury due to
which she has become immobile. Though she also had diabetes and does not show any history of DVT reflect
towards arterial ulcer. However, the position of leg injury is at gaiter area which can be the reason for venous
ulcer. As 95% of the venous ulcer is that position. Therefore the differential diagnosis of type of ulcer can get
related to either arterial or venous ulcer. To get into definitive diagnosis vascular studies has been done which
showed left ABPI of 0.80, right ABPI of 1.0. To verify the vascular status, duplex ultrasound has been conducted.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
While assessing the pain, the patient has complaint of having throbbing and heaviness in the leg. The patient also
had Toe pressure and refilling of capillary, which reflect towards venous insufficiency. After the evaluation, the
patient was showed clear feature of venous insufficiency in the lower left leg at the gaiter position. Leg ulceration
is often regarded as non-healing wound.
7
had Toe pressure and refilling of capillary, which reflect towards venous insufficiency. After the evaluation, the
patient was showed clear feature of venous insufficiency in the lower left leg at the gaiter position. Leg ulceration
is often regarded as non-healing wound.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Management & Evaluation Plan
The management of wound included four phases that need to be done for treating the ulcer. The phases
include assessment, treatment, evaluation and its management. The goal of wound management was of long
term related to wound healing to reduce the exudate, oedema and pain. Venous leg ulcer is one of the most
chronic condition of with poor healing tendency (1) On assessment it was found that, the size of wound is large
with yellow exudate and bad odour. By increasing the blood flow the, required nutrient can be reach at the site of
infection which can accelerate the rate of healing process (2) To reduce the consequence of oedema, pressure is
applied at the different site of capillaries. Therefore, for faster healing the compression therapy is the best option
to promote healing and managing the wound. In order to proceed with the therapy, caution need to take that
avoid any consequence of neuropathic pain (3). On applying the compression therapy initially with three layer,
Mrs A showed to develop left common perineal nerve pain. Therefore, two layer compression therapy is best
suited to treat her ulcer. The compression therapy used is reusable one. To initiate the therapy, it is important to
clean the wound with water and remove the dry skin especially at the edges. The antibacterial cleansing solution
is generally used as this will remove any bacterial infection (4)
Dressing of wound also proves to be effective in healing, however, dressing do not heal the wound alone,
and it need to be accompanied with the compression therapy. Dressing selection is important as patient may
develop allergies because of it. It should be kept in mind that wound need to be cleaned nicely and non-sticky.
High absorbent cotton dressing is used because the patient’s wound is showing high discharge of exudate. This
will also prevent bacterial infection (5)
In addition to the dressing and therapy, patient is encourage to include physical exercise in her daily live
activities. The exercise administered should be of low level. This will increase the blood flow and improve the
circulation. (6)
Further, pain management is also done by giving analgesic or other pain reliever (7). The patient was
receiving domiciliary care from her son and daughter, who helped her in performing physiotherapy and daily
living activities.
For the initial period of first week, nurse have not applied any stretch in the site of ulcer. When the time
came to apply compression therapy, Mrs A was not responding to the therapy as valve was not working and in
addition the calf was not able to be pumped. This was the most stressed condition in managing the wound of Mrs
A. There are many alternative present in today’s time, when patient is not able to take compression therapy.
Some of them are use of machine that is known to pump the sterile air into the boot that need to be applied in
the site of ulcer. However, these alternative are of high cost and not everyone is able to afford for the same.
Therefore, on consultation with the GP and vascular surgeon, they confirmed that, compression therapy can be
given to the patient.
The management of wound was done for the period of three month with continue evaluation in every 7 th
day of the month. On managing the wound, initially the wound did not show any such healing process. It was
noted that her sugar level of blood is high enough. Nurse in consultation with the doctor, gave proper medicine to
control the blood sugar level. After period of one month, the wound started to show healing process, and
occurrence of dryness seem to appear. In next evaluation, pain assessment was done with slightly touching the
leg. It was noted that the level of pain has been decreased. All the healing process was noted and made a clear
record of it. To overcome the skin drying, ointment was given to moisture the skin.
8
The management of wound included four phases that need to be done for treating the ulcer. The phases
include assessment, treatment, evaluation and its management. The goal of wound management was of long
term related to wound healing to reduce the exudate, oedema and pain. Venous leg ulcer is one of the most
chronic condition of with poor healing tendency (1) On assessment it was found that, the size of wound is large
with yellow exudate and bad odour. By increasing the blood flow the, required nutrient can be reach at the site of
infection which can accelerate the rate of healing process (2) To reduce the consequence of oedema, pressure is
applied at the different site of capillaries. Therefore, for faster healing the compression therapy is the best option
to promote healing and managing the wound. In order to proceed with the therapy, caution need to take that
avoid any consequence of neuropathic pain (3). On applying the compression therapy initially with three layer,
Mrs A showed to develop left common perineal nerve pain. Therefore, two layer compression therapy is best
suited to treat her ulcer. The compression therapy used is reusable one. To initiate the therapy, it is important to
clean the wound with water and remove the dry skin especially at the edges. The antibacterial cleansing solution
is generally used as this will remove any bacterial infection (4)
Dressing of wound also proves to be effective in healing, however, dressing do not heal the wound alone,
and it need to be accompanied with the compression therapy. Dressing selection is important as patient may
develop allergies because of it. It should be kept in mind that wound need to be cleaned nicely and non-sticky.
High absorbent cotton dressing is used because the patient’s wound is showing high discharge of exudate. This
will also prevent bacterial infection (5)
In addition to the dressing and therapy, patient is encourage to include physical exercise in her daily live
activities. The exercise administered should be of low level. This will increase the blood flow and improve the
circulation. (6)
Further, pain management is also done by giving analgesic or other pain reliever (7). The patient was
receiving domiciliary care from her son and daughter, who helped her in performing physiotherapy and daily
living activities.
For the initial period of first week, nurse have not applied any stretch in the site of ulcer. When the time
came to apply compression therapy, Mrs A was not responding to the therapy as valve was not working and in
addition the calf was not able to be pumped. This was the most stressed condition in managing the wound of Mrs
A. There are many alternative present in today’s time, when patient is not able to take compression therapy.
Some of them are use of machine that is known to pump the sterile air into the boot that need to be applied in
the site of ulcer. However, these alternative are of high cost and not everyone is able to afford for the same.
Therefore, on consultation with the GP and vascular surgeon, they confirmed that, compression therapy can be
given to the patient.
The management of wound was done for the period of three month with continue evaluation in every 7 th
day of the month. On managing the wound, initially the wound did not show any such healing process. It was
noted that her sugar level of blood is high enough. Nurse in consultation with the doctor, gave proper medicine to
control the blood sugar level. After period of one month, the wound started to show healing process, and
occurrence of dryness seem to appear. In next evaluation, pain assessment was done with slightly touching the
leg. It was noted that the level of pain has been decreased. All the healing process was noted and made a clear
record of it. To overcome the skin drying, ointment was given to moisture the skin.
8
On the prescribed management of the wound, patient was cooperative enough and allowed the nurse to
assist her in giving compression therapy and in weekly changing of the dressing. The result was effective, at the
end of third month, the wound of the patient got completely cured and healed. The Patient and her family was
happy with the outcome.
Applicant’s Role
The action plan set for the patient was proved to be very effective. The kind of management given was
proved to influence the wound management of the leg ulcer. The therapy given to the patient has increased the
healing process. Nurse continuously monitored the blood sugar level of the patient to maintain and control the
diabetes (10). It is important to keep it at level as this will interrupt with the healing mechanism of the wound.
This action performed by the nurse has managed the wound effectively. Nurse also changed the dressing of the
wound in every their day. This step has reduce the prevalence of infection of wound. The patient has also
reported to have high exudate therefore, dressing chosen by the nurse has given effective result. The continuous
evaluation by the nurse, has increases the rate of healing process. By administration of the physiotherapy, the
circulation has increased and wound got healed faster. Therefore, by the above mentioned action, quality of life
of Mrs A has been improved. Now she is able to perform her daily living activities, ADL and live happily. She is now
able to move and visit various places.
Apart from giving compression therapy, local treatment of ulcer can also be done (8). For cleaning the
wound only drinking or saline solution are used as because many antiseptic chemical is known to slow down the
healing process. Assessment need to be done for the presence of any non-viable tissue, level of infection and
exudate (9). Additionally, nurse also need to have to good communication skill, so that the patient feels
comfortable with the treatment. This also build trust with the care provider, that the kind of treatment given is
good for their health.
Clinical teaching is also important as because, nurse needs to have food practical as well theoretical
knowledge about the type of wound and causes for better management of the wound (11). As per my experience
and knowledge I also mentored to other staff for care of the patient. I was acted as role model of wound
management. I did not suggested any strategies to the GP or vascular surgeon. There more experienced one.
9
assist her in giving compression therapy and in weekly changing of the dressing. The result was effective, at the
end of third month, the wound of the patient got completely cured and healed. The Patient and her family was
happy with the outcome.
Applicant’s Role
The action plan set for the patient was proved to be very effective. The kind of management given was
proved to influence the wound management of the leg ulcer. The therapy given to the patient has increased the
healing process. Nurse continuously monitored the blood sugar level of the patient to maintain and control the
diabetes (10). It is important to keep it at level as this will interrupt with the healing mechanism of the wound.
This action performed by the nurse has managed the wound effectively. Nurse also changed the dressing of the
wound in every their day. This step has reduce the prevalence of infection of wound. The patient has also
reported to have high exudate therefore, dressing chosen by the nurse has given effective result. The continuous
evaluation by the nurse, has increases the rate of healing process. By administration of the physiotherapy, the
circulation has increased and wound got healed faster. Therefore, by the above mentioned action, quality of life
of Mrs A has been improved. Now she is able to perform her daily living activities, ADL and live happily. She is now
able to move and visit various places.
Apart from giving compression therapy, local treatment of ulcer can also be done (8). For cleaning the
wound only drinking or saline solution are used as because many antiseptic chemical is known to slow down the
healing process. Assessment need to be done for the presence of any non-viable tissue, level of infection and
exudate (9). Additionally, nurse also need to have to good communication skill, so that the patient feels
comfortable with the treatment. This also build trust with the care provider, that the kind of treatment given is
good for their health.
Clinical teaching is also important as because, nurse needs to have food practical as well theoretical
knowledge about the type of wound and causes for better management of the wound (11). As per my experience
and knowledge I also mentored to other staff for care of the patient. I was acted as role model of wound
management. I did not suggested any strategies to the GP or vascular surgeon. There more experienced one.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
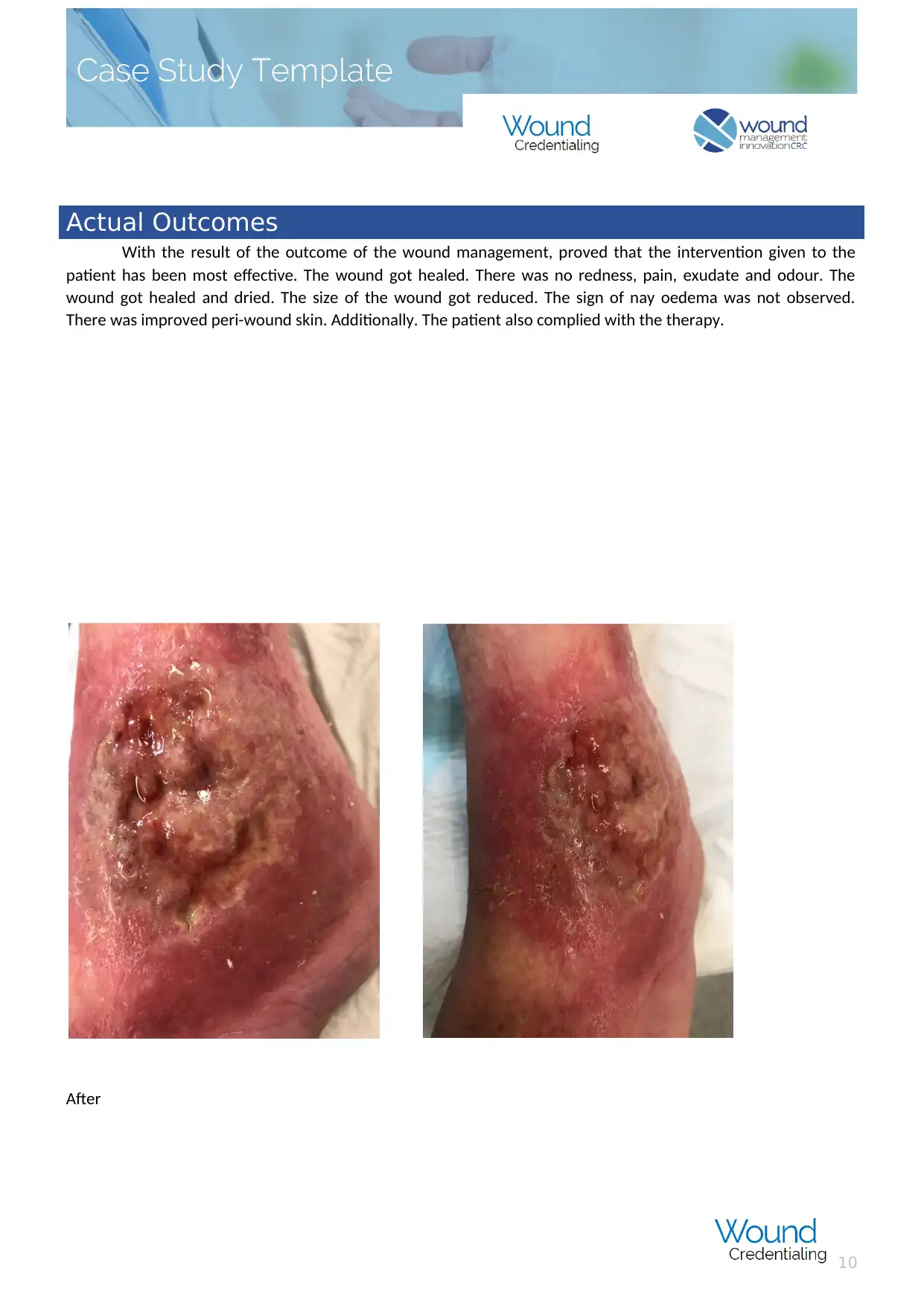
Actual Outcomes
With the result of the outcome of the wound management, proved that the intervention given to the
patient has been most effective. The wound got healed. There was no redness, pain, exudate and odour. The
wound got healed and dried. The size of the wound got reduced. The sign of nay oedema was not observed.
There was improved peri-wound skin. Additionally. The patient also complied with the therapy.
After
10
With the result of the outcome of the wound management, proved that the intervention given to the
patient has been most effective. The wound got healed. There was no redness, pain, exudate and odour. The
wound got healed and dried. The size of the wound got reduced. The sign of nay oedema was not observed.
There was improved peri-wound skin. Additionally. The patient also complied with the therapy.
After
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Evidence/References
1. Langemo D, Haesler E, Naylor W, Tippett A, Young T. Evidence-based guidelines for pressure ulcer
management at the end of life. International journal of palliative nursing. 2015 May 2;21(5):225-32.
https://doi.org/10.12968/ijpn.2015.21.5.225
2. Posthauer ME, Banks M, Dorner B, Schols JM. The role of nutrition for pressure ulcer management:
national pressure ulcer advisory panel, European pressure ulcer advisory panel, and pan pacific pressure
injury alliance white paper. Advances in skin & wound care. 2015 Apr 1;28(4):175-88. doi:
10.1097/01.ASW.0000461911.31139.62
11
1. Langemo D, Haesler E, Naylor W, Tippett A, Young T. Evidence-based guidelines for pressure ulcer
management at the end of life. International journal of palliative nursing. 2015 May 2;21(5):225-32.
https://doi.org/10.12968/ijpn.2015.21.5.225
2. Posthauer ME, Banks M, Dorner B, Schols JM. The role of nutrition for pressure ulcer management:
national pressure ulcer advisory panel, European pressure ulcer advisory panel, and pan pacific pressure
injury alliance white paper. Advances in skin & wound care. 2015 Apr 1;28(4):175-88. doi:
10.1097/01.ASW.0000461911.31139.62
11
3. Franks PJ, Barker J, Collier M, Gethin G, Haesler E, Jawien A, Laeuchli S, Mosti G, Probst S, Weller C.
Management of patients with venous leg ulcers: challenges and current best practice. Journal of wound
care. 2016 Jun 1; 25(Sup6):S1-67. https://doi.org/10.12968/jowc.2016.25.Sup6.S1
4. Pascarella L, Shortell CK. Medical management of venous ulcers. InSeminars in vascular surgery 2015 Mar
1 (Vol. 28, No. 1, pp. 21-28). WB Saunders. https://doi.org/10.1053/j.semvascsurg.2015.06.001
5. Adderley UJ, Thompson C. Community nurses’ judgement for the management of venous leg ulceration: A
judgement analysis. International journal of nursing studies. 2015 Jan 1;52(1):345-54.
https://doi.org/10.1016/j.ijnurstu.2014.09.004
6. Guest JF, Fuller GW, Vowden P. Venous leg ulcer management in clinical practice in the UK: costs and
outcomes. International wound journal. 2018 Feb 1; 15(1):29-37. https://doi.org/10.1111/iwj.12814
7. Alavi A, Sibbald RG, Phillips TJ, Miller OF, Margolis DJ, Marston W, Woo K, Romanelli M, Kirsner RS.
What's new: Management of venous leg ulcers: Treating venous leg ulcers. Journal of the American
Academy of Dermatology. 2016 Apr 1; 74(4):643-64. https://doi.org/10.1016/j.jaad.2015.03.059
8. Weller CD, Buchbinder R, Johnston RV. Interventions for helping people adhere to compression
treatments for venous leg ulceration. Cochrane database of systematic reviews. 2016(3).
doi/10.1002/14651858.CD008378.pub3/abstract
9. Marola S, Ferrarese A, Solej M, Enrico S, Nano M, Martino V. Management of venous ulcers: State of the
art. International Journal of Surgery. 2016 Sep 1; 33:S132-4. https://doi.org/10.1016/j.ijsu.2016.06.015
10. Powers JG, Higham C, Broussard K, Phillips TJ. Wound healing and treating wounds: Chronic wound care
and management. Journal of the American Academy of Dermatology. 2016 Apr 1;74(4):607-25.
https://doi.org/10.1016/j.jaad.2015.08.070
11. Loubet P, Lescure FX, Lepage L, Kirsch M, Armand-Lefevre L, Bouadma L, Lariven S, Duval X, Yazdanpanah
Y, Joly V. Endocarditis due to gram-negative bacilli at a French teaching hospital over a 6-year period:
clinical characteristics and outcome. Infectious Diseases. 2015 Dec 2;47(12):889-95.
https://doi.org/10.3109/23744235.2015.1075660.
12
Management of patients with venous leg ulcers: challenges and current best practice. Journal of wound
care. 2016 Jun 1; 25(Sup6):S1-67. https://doi.org/10.12968/jowc.2016.25.Sup6.S1
4. Pascarella L, Shortell CK. Medical management of venous ulcers. InSeminars in vascular surgery 2015 Mar
1 (Vol. 28, No. 1, pp. 21-28). WB Saunders. https://doi.org/10.1053/j.semvascsurg.2015.06.001
5. Adderley UJ, Thompson C. Community nurses’ judgement for the management of venous leg ulceration: A
judgement analysis. International journal of nursing studies. 2015 Jan 1;52(1):345-54.
https://doi.org/10.1016/j.ijnurstu.2014.09.004
6. Guest JF, Fuller GW, Vowden P. Venous leg ulcer management in clinical practice in the UK: costs and
outcomes. International wound journal. 2018 Feb 1; 15(1):29-37. https://doi.org/10.1111/iwj.12814
7. Alavi A, Sibbald RG, Phillips TJ, Miller OF, Margolis DJ, Marston W, Woo K, Romanelli M, Kirsner RS.
What's new: Management of venous leg ulcers: Treating venous leg ulcers. Journal of the American
Academy of Dermatology. 2016 Apr 1; 74(4):643-64. https://doi.org/10.1016/j.jaad.2015.03.059
8. Weller CD, Buchbinder R, Johnston RV. Interventions for helping people adhere to compression
treatments for venous leg ulceration. Cochrane database of systematic reviews. 2016(3).
doi/10.1002/14651858.CD008378.pub3/abstract
9. Marola S, Ferrarese A, Solej M, Enrico S, Nano M, Martino V. Management of venous ulcers: State of the
art. International Journal of Surgery. 2016 Sep 1; 33:S132-4. https://doi.org/10.1016/j.ijsu.2016.06.015
10. Powers JG, Higham C, Broussard K, Phillips TJ. Wound healing and treating wounds: Chronic wound care
and management. Journal of the American Academy of Dermatology. 2016 Apr 1;74(4):607-25.
https://doi.org/10.1016/j.jaad.2015.08.070
11. Loubet P, Lescure FX, Lepage L, Kirsch M, Armand-Lefevre L, Bouadma L, Lariven S, Duval X, Yazdanpanah
Y, Joly V. Endocarditis due to gram-negative bacilli at a French teaching hospital over a 6-year period:
clinical characteristics and outcome. Infectious Diseases. 2015 Dec 2;47(12):889-95.
https://doi.org/10.3109/23744235.2015.1075660.
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





