Vitamin D Requirement, Functions, and Sources for Adolescents' Health
VerifiedAdded on 2022/09/18
|17
|4211
|30
Report
AI Summary
This report investigates the crucial role of vitamin D as a micronutrient for adolescents. It begins with an introduction to vitamin D, detailing its forms (D2 and D3), natural sources, and chemical structure. The report explores the biochemical functions of vitamin D, emphasizing its impact on calcium absorption, bone health, muscle function, and the immune system. Dietary requirements, including the Recommended Dietary Allowance (RDA), are presented, along with a table outlining the RDA for different age groups. Dietary sources of vitamin D, such as fatty fish, fortified foods, and supplements, are discussed. The report highlights the significance of vitamin D in adolescence for achieving peak bone mass. The report also mentions the role of vitamin D in several other functions such as cell formation and development. The report concludes with a discussion of the importance of vitamin D supplementation and the potential need for further research into its effects on health. The report is based on the research of peer reviewed articles from the last five years. The paper utilizes APA style citation both in the paper and on the reference page.

Running head: MICRONUTRIENT REQUIRED FOR THE ADOLESCENTS 1
Vitamin D Requirement for the Adolescents Ages
Firstname Lastname
Name of Institution
Vitamin D Requirement for the Adolescents Ages
Firstname Lastname
Name of Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 2
Vitamin D as a micronutrient Requirement for the Adolescents Ages
Introduction
Vitamin D is a class of fat soluble and non-nutrient soluble which is essential for enhancing
magnesium, calcium, and phosphorus and several other biochemical impacts. In individuals,
vitamin D3 (often referred as cholecalciferol) and vitamin D2 (termed as ergocalciferol) seem to
be the most significant molecules in this category. The vitamin D's principal natural source is the
breakdown of cholesterol cholecalciferol well into the skin via a chemical process based on
sunlight exposure (explicitly UVB radioactivity). It is possible to consume cholecalciferol as
well as ergocalciferol from either the food or supplements (NHS, 2019). Just a few foods,
including fatty fish flesh, comprise important quantities of vitamin D, and fish may not carry
plenty of vitamin D without sunshine and sometimes supplements to attain ideal vitamin D
concentration. Nutrient suggestions usually suppose all of a person's vitamin D is given by
mouth while exposure to sunlight is varying in the demographic and suggestions regarding the
quantity of secure sunlight are unsure given the danger of cancer.
In the event of skin development, vitamin D from food sources is not effective. In their studies
(Borel, Cano, & Caillaud, 2013) it was discovered that the protein receptor should still
hydroxylate to an active state. This can be done either in liver or even in the kidneys. Since other
mammal species can properly metabolize vitamin D under sufficient sunlight, it is not a
significant dietary component and not technically a vitamin. It can be considered a hormone with
vitamin D pro-hormone absorption that arises in the aggressive state of calcitriol, which then
produces effects at separate places through the nuclear transmitter (Feldman, et al., 2017).
Vitamin D as a micronutrient Requirement for the Adolescents Ages
Introduction
Vitamin D is a class of fat soluble and non-nutrient soluble which is essential for enhancing
magnesium, calcium, and phosphorus and several other biochemical impacts. In individuals,
vitamin D3 (often referred as cholecalciferol) and vitamin D2 (termed as ergocalciferol) seem to
be the most significant molecules in this category. The vitamin D's principal natural source is the
breakdown of cholesterol cholecalciferol well into the skin via a chemical process based on
sunlight exposure (explicitly UVB radioactivity). It is possible to consume cholecalciferol as
well as ergocalciferol from either the food or supplements (NHS, 2019). Just a few foods,
including fatty fish flesh, comprise important quantities of vitamin D, and fish may not carry
plenty of vitamin D without sunshine and sometimes supplements to attain ideal vitamin D
concentration. Nutrient suggestions usually suppose all of a person's vitamin D is given by
mouth while exposure to sunlight is varying in the demographic and suggestions regarding the
quantity of secure sunlight are unsure given the danger of cancer.
In the event of skin development, vitamin D from food sources is not effective. In their studies
(Borel, Cano, & Caillaud, 2013) it was discovered that the protein receptor should still
hydroxylate to an active state. This can be done either in liver or even in the kidneys. Since other
mammal species can properly metabolize vitamin D under sufficient sunlight, it is not a
significant dietary component and not technically a vitamin. It can be considered a hormone with
vitamin D pro-hormone absorption that arises in the aggressive state of calcitriol, which then
produces effects at separate places through the nuclear transmitter (Feldman, et al., 2017).
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 3
Chemical Structure of Vitamin D
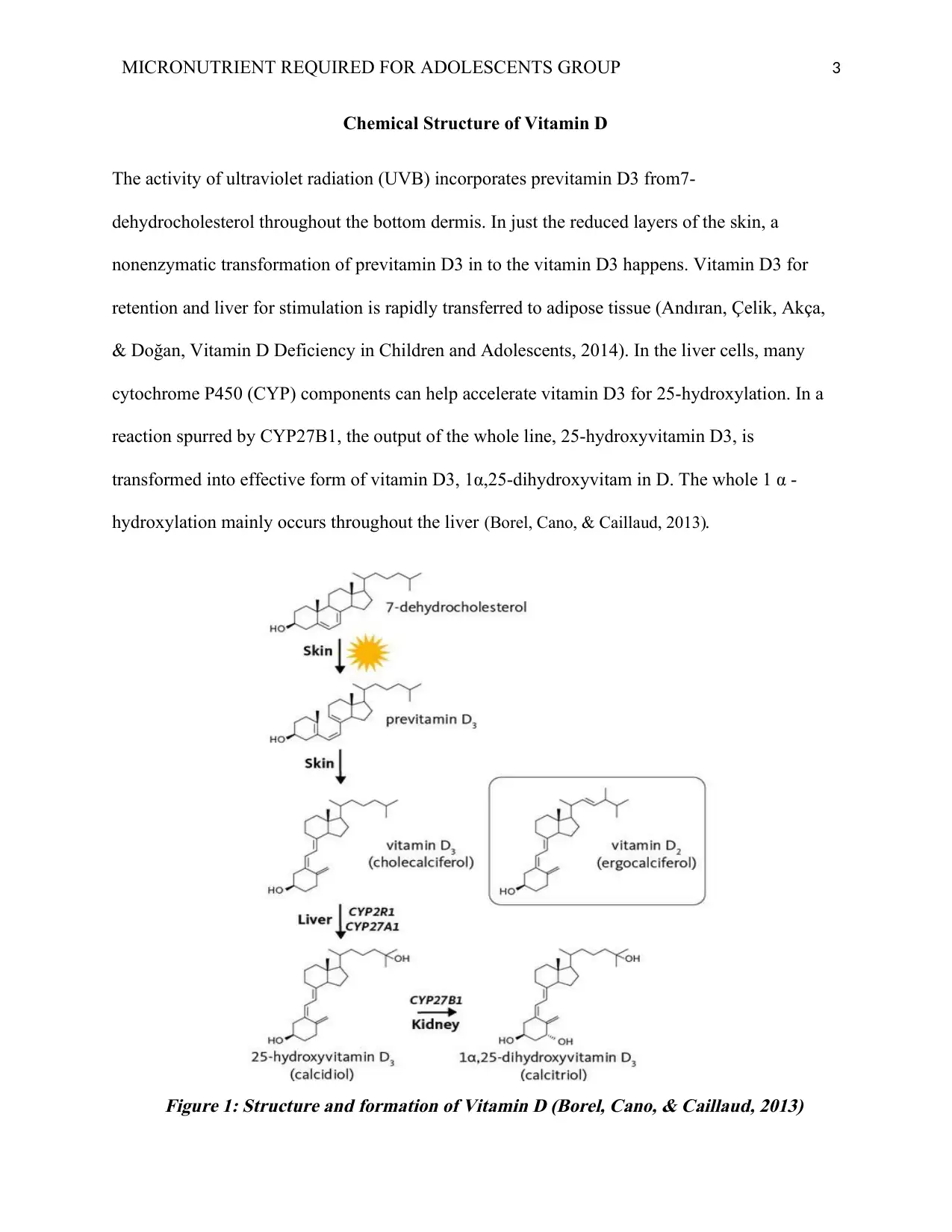
The activity of ultraviolet radiation (UVB) incorporates previtamin D3 from7-
dehydrocholesterol throughout the bottom dermis. In just the reduced layers of the skin, a
nonenzymatic transformation of previtamin D3 in to the vitamin D3 happens. Vitamin D3 for
retention and liver for stimulation is rapidly transferred to adipose tissue (Andıran, Çelik, Akça,
& Doğan, Vitamin D Deficiency in Children and Adolescents, 2014). In the liver cells, many
cytochrome P450 (CYP) components can help accelerate vitamin D3 for 25-hydroxylation. In a
reaction spurred by CYP27B1, the output of the whole line, 25-hydroxyvitamin D3, is
transformed into effective form of vitamin D3, 1α,25-dihydroxyvitam in D. The whole 1 α -
hydroxylation mainly occurs throughout the liver (Borel, Cano, & Caillaud, 2013).
Figure 1: Structure and formation of Vitamin D (Borel, Cano, & Caillaud, 2013)
Chemical Structure of Vitamin D
The activity of ultraviolet radiation (UVB) incorporates previtamin D3 from7-
dehydrocholesterol throughout the bottom dermis. In just the reduced layers of the skin, a
nonenzymatic transformation of previtamin D3 in to the vitamin D3 happens. Vitamin D3 for
retention and liver for stimulation is rapidly transferred to adipose tissue (Andıran, Çelik, Akça,
& Doğan, Vitamin D Deficiency in Children and Adolescents, 2014). In the liver cells, many
cytochrome P450 (CYP) components can help accelerate vitamin D3 for 25-hydroxylation. In a
reaction spurred by CYP27B1, the output of the whole line, 25-hydroxyvitamin D3, is
transformed into effective form of vitamin D3, 1α,25-dihydroxyvitam in D. The whole 1 α -
hydroxylation mainly occurs throughout the liver (Borel, Cano, & Caillaud, 2013).
Figure 1: Structure and formation of Vitamin D (Borel, Cano, & Caillaud, 2013)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 4
Functions of vitamin D
Vitamin D is just one of many foods to remain healthy in our lives. It enables the body among
many of the primary functions of the vitamin: absorb calcium. Vitamin D, together with calcium,
enables to construct bones and maintain bones firm and healthy, and blocks parathyroid hormone
discharge. This hormone superheats tissue, making the bones thin and fragile. In muscle function
as well as the immune system, vitamin D can play an important role. The digestive system is
really the protection system to your organs. It enables to safeguard it from diseases as well as
other diseases. Have shown that taking vitamin D every day reduces the likelihood of dropping
in the elderly.
Research has suggested that Vitamin D may help avoid cancers of the stomach, breast, and
nipple. Several studies are indeed available that may help avoid and treat diabetes, heart disease,
increased blood pressure, and various sclerosis. The findings of these research, however, is either
provisional or are under discussion. Even most of the scientists who performed these original
studies are careful to propose vitamin D for the avoidance of such illnesses without any lengthy-
term studies.
On sunlight exposure, vitamin D can indeed be formed in the skin and is then excreted into the
biologically active molecule called 1α,25-dihydroxyvitamin D well into the kidneys and liver.
The genes are activated and engaged in both skeletal and biological activities can be controlled
by linking to the vitamin D transmitter.
Vitamin D is vital to keep bone mineralization by influencing immune function of phosphate and
calcium. There are several non-skeletal impacts of vitamin D, especially on both the cellular,
Functions of vitamin D
Vitamin D is just one of many foods to remain healthy in our lives. It enables the body among
many of the primary functions of the vitamin: absorb calcium. Vitamin D, together with calcium,
enables to construct bones and maintain bones firm and healthy, and blocks parathyroid hormone
discharge. This hormone superheats tissue, making the bones thin and fragile. In muscle function
as well as the immune system, vitamin D can play an important role. The digestive system is
really the protection system to your organs. It enables to safeguard it from diseases as well as
other diseases. Have shown that taking vitamin D every day reduces the likelihood of dropping
in the elderly.
Research has suggested that Vitamin D may help avoid cancers of the stomach, breast, and
nipple. Several studies are indeed available that may help avoid and treat diabetes, heart disease,
increased blood pressure, and various sclerosis. The findings of these research, however, is either
provisional or are under discussion. Even most of the scientists who performed these original
studies are careful to propose vitamin D for the avoidance of such illnesses without any lengthy-
term studies.
On sunlight exposure, vitamin D can indeed be formed in the skin and is then excreted into the
biologically active molecule called 1α,25-dihydroxyvitamin D well into the kidneys and liver.
The genes are activated and engaged in both skeletal and biological activities can be controlled
by linking to the vitamin D transmitter.
Vitamin D is vital to keep bone mineralization by influencing immune function of phosphate and
calcium. There are several non-skeletal impacts of vitamin D, especially on both the cellular,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 5
cardiovascular and cardiac systems ("Vitamin D and Macrophage Functions in Tuberculosis",
2015).
For proper bone growth and preservation, vitamin D is significant. Extreme defect in vitamin D
leads infants to rickets and adolescent osteomalacia.
Tertiary hyperparathyroidism may improve bone deterioration and catalyze osteoporosis relative
to insufficient vitamin D (Pharande, Pammi, Collins, Zhou & Abrams, 2015). Randomized
controlled clinical tests show that supplementing vitamin D with at least 800 IU / day should
reduce the likelihood of falling and fracturing in elderly people.
Through linking to vitamin D gene contained in several cells of the body, vitamin D may control
cell formation and development. Scientific studies have noted correlation among little sunlight
intake, bad condition of vitamin D and enhanced likelihood of colorectal as well as breast cancer
development (Grant, 2016). Randomized controlled tests are required to assess if vitamin D
supplementation could be used to prevent diseases such as cancer.
Different studies noted reverse correlations in both vitamin D identity and autoimmune disorder
proneness or extent, which include type 1 diabetes mellitus, sclerosis, osteoarthritis, as well as
lupus erythematosus.
The VDR is conveyed by pancreatic insulin-secreting neurons, as well as the findings of animal
research indicate even under circumstances of enhanced insulin demand, 1α,25-
dihydroxyvitamin D plays a major role in insulin production. Cross-sectional and subsequent
research indicates that inadequate vitamin D levels in type 2 diabetes mellitus (noninsulin-
dependent diabetes mellitus) might well adversely affect insulin release and glucose sensitivity.
cardiovascular and cardiac systems ("Vitamin D and Macrophage Functions in Tuberculosis",
2015).
For proper bone growth and preservation, vitamin D is significant. Extreme defect in vitamin D
leads infants to rickets and adolescent osteomalacia.
Tertiary hyperparathyroidism may improve bone deterioration and catalyze osteoporosis relative
to insufficient vitamin D (Pharande, Pammi, Collins, Zhou & Abrams, 2015). Randomized
controlled clinical tests show that supplementing vitamin D with at least 800 IU / day should
reduce the likelihood of falling and fracturing in elderly people.
Through linking to vitamin D gene contained in several cells of the body, vitamin D may control
cell formation and development. Scientific studies have noted correlation among little sunlight
intake, bad condition of vitamin D and enhanced likelihood of colorectal as well as breast cancer
development (Grant, 2016). Randomized controlled tests are required to assess if vitamin D
supplementation could be used to prevent diseases such as cancer.
Different studies noted reverse correlations in both vitamin D identity and autoimmune disorder
proneness or extent, which include type 1 diabetes mellitus, sclerosis, osteoarthritis, as well as
lupus erythematosus.
The VDR is conveyed by pancreatic insulin-secreting neurons, as well as the findings of animal
research indicate even under circumstances of enhanced insulin demand, 1α,25-
dihydroxyvitamin D plays a major role in insulin production. Cross-sectional and subsequent
research indicates that inadequate vitamin D levels in type 2 diabetes mellitus (noninsulin-
dependent diabetes mellitus) might well adversely affect insulin release and glucose sensitivity.
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 6
Phosphate as well as calcium metabolic regulations are strongly related, as well as serum
phosphate can also be controlled by calciotropic hormones, PTH or even 1α,25-
dihydroxyvitamin D. In specific, by promoting the production of a sodium-phosphate
cotransporter in the small intestine, 1α,25-dihydroxyvitamin D increases the intake of intestinal
phosphorus.
Dietary requirements for Vitamin D (RDA)
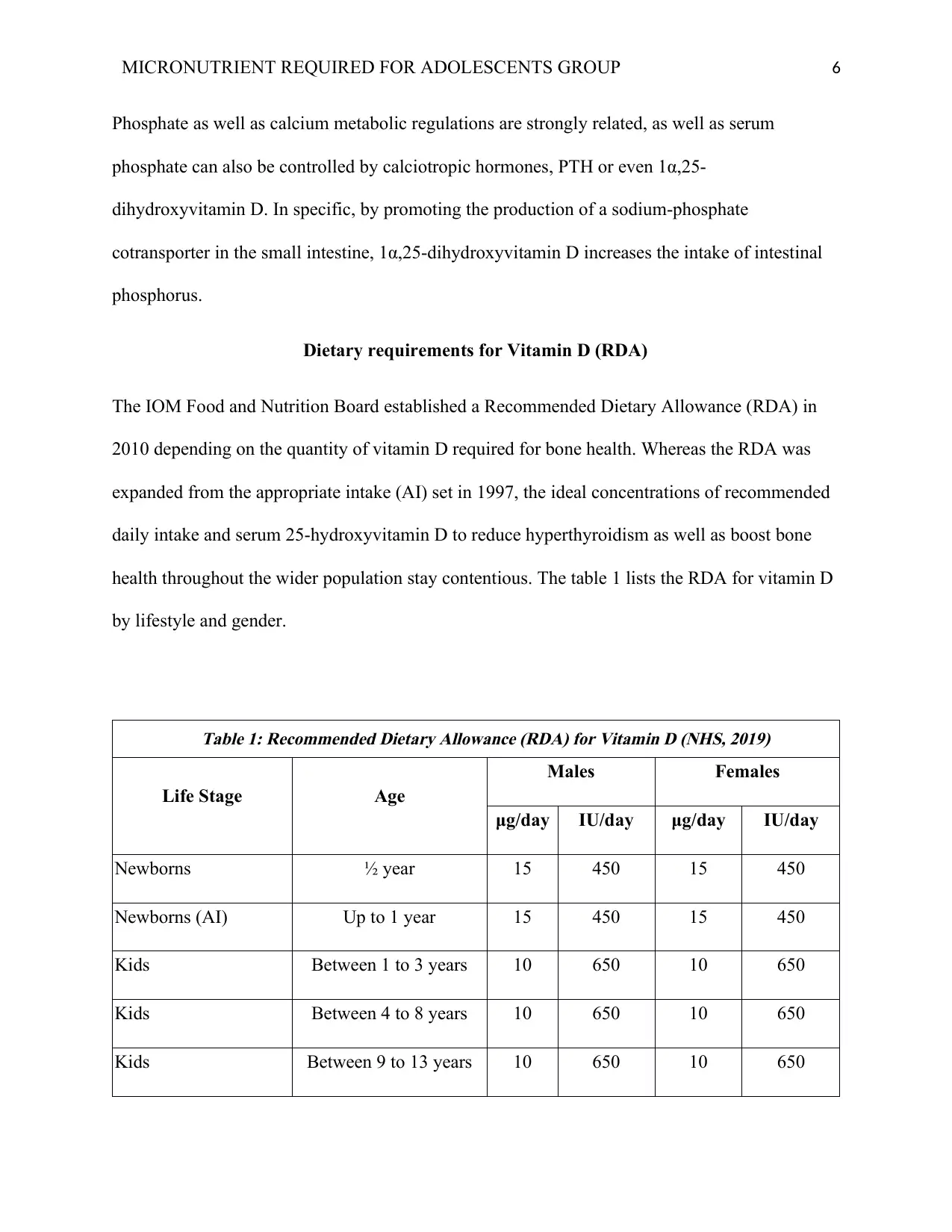
The IOM Food and Nutrition Board established a Recommended Dietary Allowance (RDA) in
2010 depending on the quantity of vitamin D required for bone health. Whereas the RDA was
expanded from the appropriate intake (AI) set in 1997, the ideal concentrations of recommended
daily intake and serum 25-hydroxyvitamin D to reduce hyperthyroidism as well as boost bone
health throughout the wider population stay contentious. The table 1 lists the RDA for vitamin D
by lifestyle and gender.
Table 1: Recommended Dietary Allowance (RDA) for Vitamin D (NHS, 2019)
Life Stage Age
Males Females
μg/day IU/day μg/day IU/day
Newborns ½ year 15 450 15 450
Newborns (AI) Up to 1 year 15 450 15 450
Kids Between 1 to 3 years 10 650 10 650
Kids Between 4 to 8 years 10 650 10 650
Kids Between 9 to 13 years 10 650 10 650
Phosphate as well as calcium metabolic regulations are strongly related, as well as serum
phosphate can also be controlled by calciotropic hormones, PTH or even 1α,25-
dihydroxyvitamin D. In specific, by promoting the production of a sodium-phosphate
cotransporter in the small intestine, 1α,25-dihydroxyvitamin D increases the intake of intestinal
phosphorus.
Dietary requirements for Vitamin D (RDA)
The IOM Food and Nutrition Board established a Recommended Dietary Allowance (RDA) in
2010 depending on the quantity of vitamin D required for bone health. Whereas the RDA was
expanded from the appropriate intake (AI) set in 1997, the ideal concentrations of recommended
daily intake and serum 25-hydroxyvitamin D to reduce hyperthyroidism as well as boost bone
health throughout the wider population stay contentious. The table 1 lists the RDA for vitamin D
by lifestyle and gender.
Table 1: Recommended Dietary Allowance (RDA) for Vitamin D (NHS, 2019)
Life Stage Age
Males Females
μg/day IU/day μg/day IU/day
Newborns ½ year 15 450 15 450
Newborns (AI) Up to 1 year 15 450 15 450
Kids Between 1 to 3 years 10 650 10 650
Kids Between 4 to 8 years 10 650 10 650
Kids Between 9 to 13 years 10 650 10 650
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 7
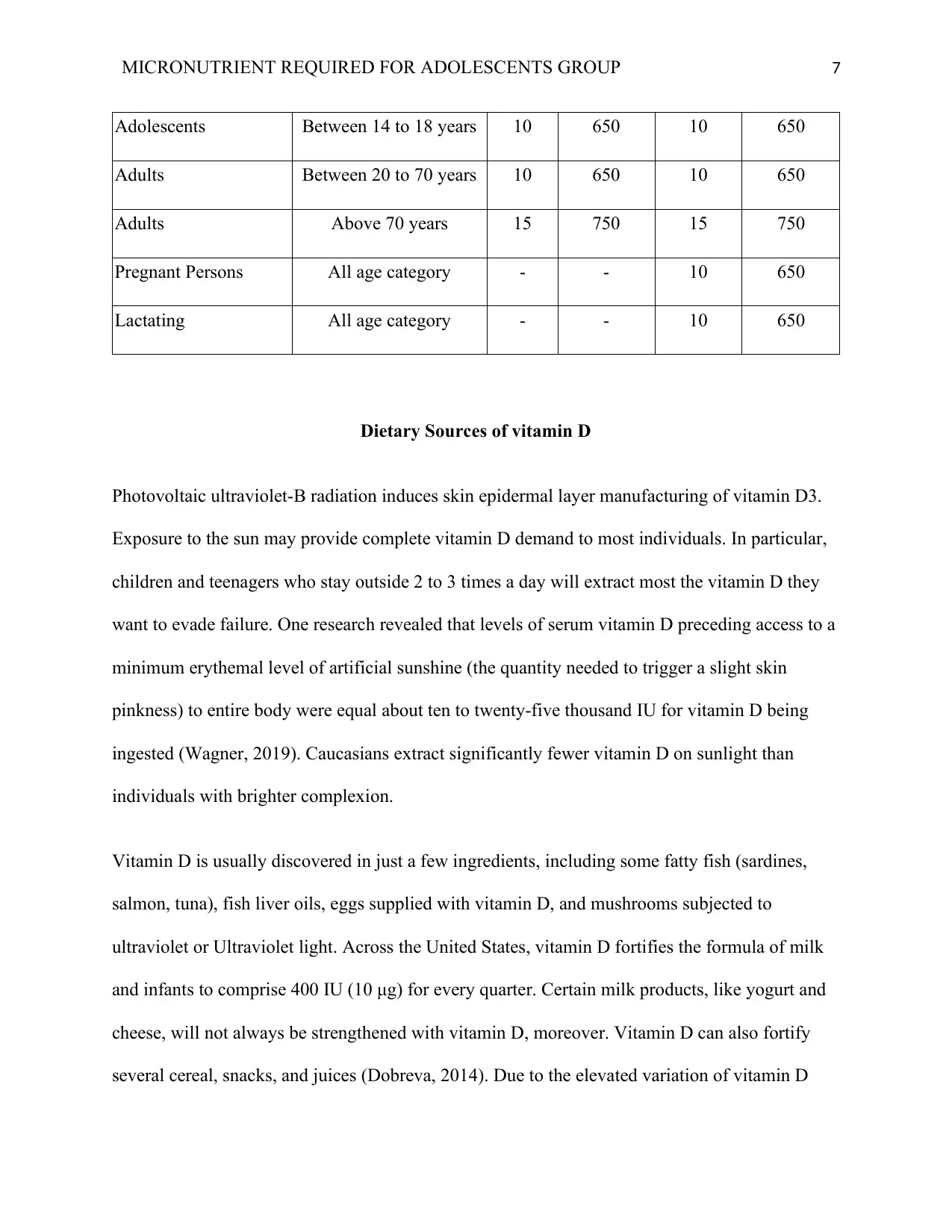
Adolescents Between 14 to 18 years 10 650 10 650
Adults Between 20 to 70 years 10 650 10 650
Adults Above 70 years 15 750 15 750
Pregnant Persons All age category - - 10 650
Lactating All age category - - 10 650
Dietary Sources of vitamin D
Photovoltaic ultraviolet-B radiation induces skin epidermal layer manufacturing of vitamin D3.
Exposure to the sun may provide complete vitamin D demand to most individuals. In particular,
children and teenagers who stay outside 2 to 3 times a day will extract most the vitamin D they
want to evade failure. One research revealed that levels of serum vitamin D preceding access to a
minimum erythemal level of artificial sunshine (the quantity needed to trigger a slight skin
pinkness) to entire body were equal about ten to twenty-five thousand IU for vitamin D being
ingested (Wagner, 2019). Caucasians extract significantly fewer vitamin D on sunlight than
individuals with brighter complexion.
Vitamin D is usually discovered in just a few ingredients, including some fatty fish (sardines,
salmon, tuna), fish liver oils, eggs supplied with vitamin D, and mushrooms subjected to
ultraviolet or Ultraviolet light. Across the United States, vitamin D fortifies the formula of milk
and infants to comprise 400 IU (10 μg) for every quarter. Certain milk products, like yogurt and
cheese, will not always be strengthened with vitamin D, moreover. Vitamin D can also fortify
several cereal, snacks, and juices (Dobreva, 2014). Due to the elevated variation of vitamin D
Adolescents Between 14 to 18 years 10 650 10 650
Adults Between 20 to 70 years 10 650 10 650
Adults Above 70 years 15 750 15 750
Pregnant Persons All age category - - 10 650
Lactating All age category - - 10 650
Dietary Sources of vitamin D
Photovoltaic ultraviolet-B radiation induces skin epidermal layer manufacturing of vitamin D3.
Exposure to the sun may provide complete vitamin D demand to most individuals. In particular,
children and teenagers who stay outside 2 to 3 times a day will extract most the vitamin D they
want to evade failure. One research revealed that levels of serum vitamin D preceding access to a
minimum erythemal level of artificial sunshine (the quantity needed to trigger a slight skin
pinkness) to entire body were equal about ten to twenty-five thousand IU for vitamin D being
ingested (Wagner, 2019). Caucasians extract significantly fewer vitamin D on sunlight than
individuals with brighter complexion.
Vitamin D is usually discovered in just a few ingredients, including some fatty fish (sardines,
salmon, tuna), fish liver oils, eggs supplied with vitamin D, and mushrooms subjected to
ultraviolet or Ultraviolet light. Across the United States, vitamin D fortifies the formula of milk
and infants to comprise 400 IU (10 μg) for every quarter. Certain milk products, like yogurt and
cheese, will not always be strengthened with vitamin D, moreover. Vitamin D can also fortify
several cereal, snacks, and juices (Dobreva, 2014). Due to the elevated variation of vitamin D
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 8
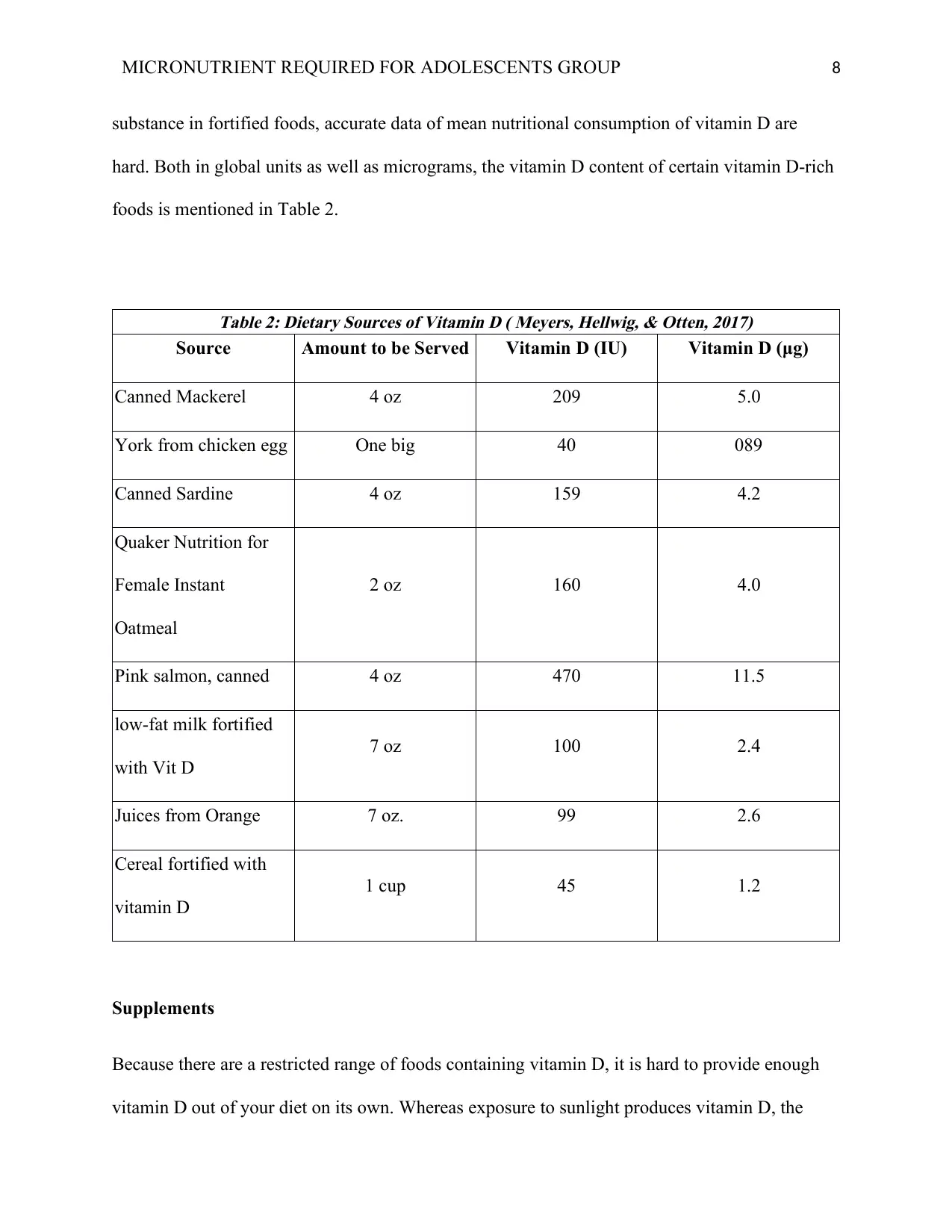
substance in fortified foods, accurate data of mean nutritional consumption of vitamin D are
hard. Both in global units as well as micrograms, the vitamin D content of certain vitamin D-rich
foods is mentioned in Table 2.
Table 2: Dietary Sources of Vitamin D ( Meyers, Hellwig, & Otten, 2017)
Source Amount to be Served Vitamin D (IU) Vitamin D (μg)
Canned Mackerel 4 oz 209 5.0
York from chicken egg One big 40 089
Canned Sardine 4 oz 159 4.2
Quaker Nutrition for
Female Instant
Oatmeal
2 oz 160 4.0
Pink salmon, canned 4 oz 470 11.5
low-fat milk fortified
with Vit D
7 oz 100 2.4
Juices from Orange 7 oz. 99 2.6
Cereal fortified with
vitamin D
1 cup 45 1.2
Supplements
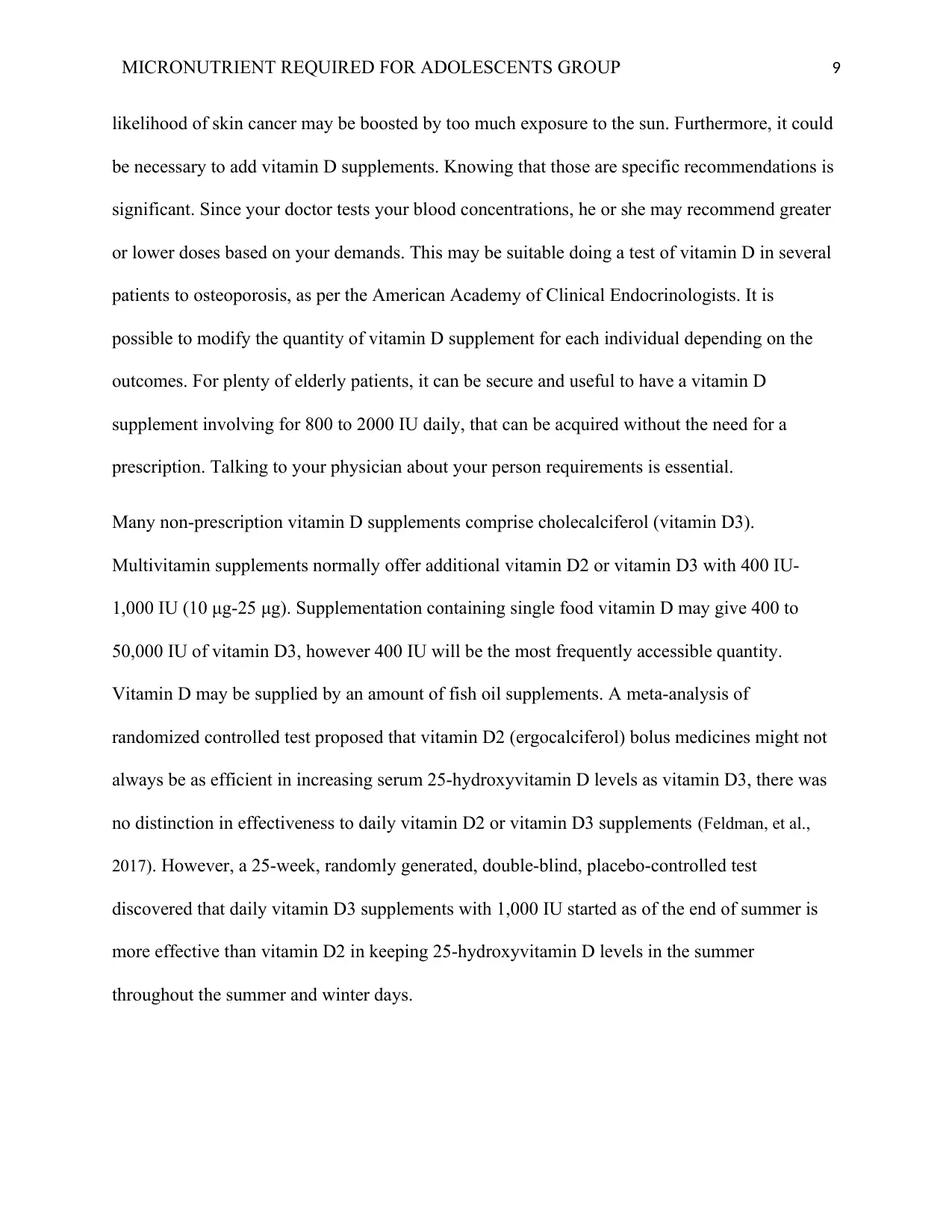
Because there are a restricted range of foods containing vitamin D, it is hard to provide enough
vitamin D out of your diet on its own. Whereas exposure to sunlight produces vitamin D, the
substance in fortified foods, accurate data of mean nutritional consumption of vitamin D are
hard. Both in global units as well as micrograms, the vitamin D content of certain vitamin D-rich
foods is mentioned in Table 2.
Table 2: Dietary Sources of Vitamin D ( Meyers, Hellwig, & Otten, 2017)
Source Amount to be Served Vitamin D (IU) Vitamin D (μg)
Canned Mackerel 4 oz 209 5.0
York from chicken egg One big 40 089
Canned Sardine 4 oz 159 4.2
Quaker Nutrition for
Female Instant
Oatmeal
2 oz 160 4.0
Pink salmon, canned 4 oz 470 11.5
low-fat milk fortified
with Vit D
7 oz 100 2.4
Juices from Orange 7 oz. 99 2.6
Cereal fortified with
vitamin D
1 cup 45 1.2
Supplements
Because there are a restricted range of foods containing vitamin D, it is hard to provide enough
vitamin D out of your diet on its own. Whereas exposure to sunlight produces vitamin D, the
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 9
likelihood of skin cancer may be boosted by too much exposure to the sun. Furthermore, it could
be necessary to add vitamin D supplements. Knowing that those are specific recommendations is
significant. Since your doctor tests your blood concentrations, he or she may recommend greater
or lower doses based on your demands. This may be suitable doing a test of vitamin D in several
patients to osteoporosis, as per the American Academy of Clinical Endocrinologists. It is
possible to modify the quantity of vitamin D supplement for each individual depending on the
outcomes. For plenty of elderly patients, it can be secure and useful to have a vitamin D
supplement involving for 800 to 2000 IU daily, that can be acquired without the need for a
prescription. Talking to your physician about your person requirements is essential.
Many non-prescription vitamin D supplements comprise cholecalciferol (vitamin D3).
Multivitamin supplements normally offer additional vitamin D2 or vitamin D3 with 400 IU-
1,000 IU (10 μg-25 μg). Supplementation containing single food vitamin D may give 400 to
50,000 IU of vitamin D3, however 400 IU will be the most frequently accessible quantity.
Vitamin D may be supplied by an amount of fish oil supplements. A meta-analysis of
randomized controlled test proposed that vitamin D2 (ergocalciferol) bolus medicines might not
always be as efficient in increasing serum 25-hydroxyvitamin D levels as vitamin D3, there was
no distinction in effectiveness to daily vitamin D2 or vitamin D3 supplements (Feldman, et al.,
2017). However, a 25-week, randomly generated, double-blind, placebo-controlled test
discovered that daily vitamin D3 supplements with 1,000 IU started as of the end of summer is
more effective than vitamin D2 in keeping 25-hydroxyvitamin D levels in the summer
throughout the summer and winter days.
likelihood of skin cancer may be boosted by too much exposure to the sun. Furthermore, it could
be necessary to add vitamin D supplements. Knowing that those are specific recommendations is
significant. Since your doctor tests your blood concentrations, he or she may recommend greater
or lower doses based on your demands. This may be suitable doing a test of vitamin D in several
patients to osteoporosis, as per the American Academy of Clinical Endocrinologists. It is
possible to modify the quantity of vitamin D supplement for each individual depending on the
outcomes. For plenty of elderly patients, it can be secure and useful to have a vitamin D
supplement involving for 800 to 2000 IU daily, that can be acquired without the need for a
prescription. Talking to your physician about your person requirements is essential.
Many non-prescription vitamin D supplements comprise cholecalciferol (vitamin D3).
Multivitamin supplements normally offer additional vitamin D2 or vitamin D3 with 400 IU-
1,000 IU (10 μg-25 μg). Supplementation containing single food vitamin D may give 400 to
50,000 IU of vitamin D3, however 400 IU will be the most frequently accessible quantity.
Vitamin D may be supplied by an amount of fish oil supplements. A meta-analysis of
randomized controlled test proposed that vitamin D2 (ergocalciferol) bolus medicines might not
always be as efficient in increasing serum 25-hydroxyvitamin D levels as vitamin D3, there was
no distinction in effectiveness to daily vitamin D2 or vitamin D3 supplements (Feldman, et al.,
2017). However, a 25-week, randomly generated, double-blind, placebo-controlled test
discovered that daily vitamin D3 supplements with 1,000 IU started as of the end of summer is
more effective than vitamin D2 in keeping 25-hydroxyvitamin D levels in the summer
throughout the summer and winter days.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 10
The role of Vitamin D on Adolescence
Both men and women in the earlier to mid-21st century achieve their maximum bone mass and
skeleton endurance and keep them by their mid-40s. While people had no influence over inherent
variables that assist assess their bone mass, including sex, family history, and race, other
extrinsic variables are also predictors of bone mass, such as diet, body mass, hormonal mixture
of a specific individual, disease and diagnosis, physical exercise, and behavior choices.
Healthcare providers should therefore enable patients to practice frequently, keep good weight,
eat healthily, and take vitamins on a regular basis.
According to (Al-Shaar, Mneimneh, Nabulsi, Malouf & Fuleihan, 2014), vitamin D is generated
linearly at distinct locations of the body and plays a key role in adolescent health, especially in
born development. Certain roles, though, are arising. The risk of rickets, osteomalacia and
coronary heart disease is boosted when the serum level of vitamin D is quite low. There is indeed
a high incidence of low vitamin D in adolescents, particularly in women and also in winter, with
a reduced incidence than those in summer. Though there is no common consensus on the low
values required for excellent health, serum 25-hydroxyvitamin D [ 25(OH)D] concentrations
below 20 ng / mL may be considered a disease with vitamin D deficiency, as well as
concentrations between 20-30 ng / mL can be the vitamin D deficiency range. Bone mass
accumulative changes in kids and adolescents, decreased muscle power, adverse cardiovascular
results, insulin resistance and obesity, and neurological disorders have been correlated with
moderate low concentrations (Bjelakovic, Nikolova, Bjelakovic & Gluud, 2017). Appropriate
preventive policies are required all across adolescent years to ensure appropriate concentrations
of vitamin D.
The role of Vitamin D on Adolescence
Both men and women in the earlier to mid-21st century achieve their maximum bone mass and
skeleton endurance and keep them by their mid-40s. While people had no influence over inherent
variables that assist assess their bone mass, including sex, family history, and race, other
extrinsic variables are also predictors of bone mass, such as diet, body mass, hormonal mixture
of a specific individual, disease and diagnosis, physical exercise, and behavior choices.
Healthcare providers should therefore enable patients to practice frequently, keep good weight,
eat healthily, and take vitamins on a regular basis.
According to (Al-Shaar, Mneimneh, Nabulsi, Malouf & Fuleihan, 2014), vitamin D is generated
linearly at distinct locations of the body and plays a key role in adolescent health, especially in
born development. Certain roles, though, are arising. The risk of rickets, osteomalacia and
coronary heart disease is boosted when the serum level of vitamin D is quite low. There is indeed
a high incidence of low vitamin D in adolescents, particularly in women and also in winter, with
a reduced incidence than those in summer. Though there is no common consensus on the low
values required for excellent health, serum 25-hydroxyvitamin D [ 25(OH)D] concentrations
below 20 ng / mL may be considered a disease with vitamin D deficiency, as well as
concentrations between 20-30 ng / mL can be the vitamin D deficiency range. Bone mass
accumulative changes in kids and adolescents, decreased muscle power, adverse cardiovascular
results, insulin resistance and obesity, and neurological disorders have been correlated with
moderate low concentrations (Bjelakovic, Nikolova, Bjelakovic & Gluud, 2017). Appropriate
preventive policies are required all across adolescent years to ensure appropriate concentrations
of vitamin D.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 11
Both bone mass and density boost and achieve the maximum bone mass content (BMC) by all
the end of the second century of life throughout adolescence (Magge, Prasad, Zemel & Kelly,
2018). In adolescents, there may be demographic variations in the accrual of bone mass owing to
genetic and environmental factors and even the phases of puberty and lifestyle choices, along
with physical activity, size, weight, lean body mass and food. A research study used dual-energy
X-ray absorptiometry to evaluate bone mass for up to four years at various locations in
Australian, African, Latino and Caucasian people between ages 9 to 5 years. Black people had
higher mean concentrations of area bone mineral density (BMD) as well as volumetric BMD at
all skeletal locations evaluated of many women. Of many Australian and Caucasian women,
femoral neck volumetric BMD was smaller than those in Hispanic people. There is really limited
information readily accessible on the connection among 25(OH)D levels and bone turnover
markers in adolescent girls (Saggese, et al., 2015). The serum concentration of adolescent vitamin
D is an integral factor for gaining bone mass. Rickets are correlated with prolonged very small
serum concentrations of 25(OH)D, although inadequate concentrations (< 50 nmol / L) change
the intake of calcium and bone mineralized. Serum calcium and vitamin D are correlated with
complete body or hip BMD, and when modified of age, gender and swimming relationships are
decreased.
The consequences of low level of vitamin D on muscle activity are indeed obvious in post
menarche women forward to weight change. Vitamin D seemed to affect brain function in many
respects before changes in the bone mass can be detected (De Souza Silva, 2016). Young ladies
with appropriate status of vitamin D had greater muscle power comparative to those with bad
status of vitamin D.
Both bone mass and density boost and achieve the maximum bone mass content (BMC) by all
the end of the second century of life throughout adolescence (Magge, Prasad, Zemel & Kelly,
2018). In adolescents, there may be demographic variations in the accrual of bone mass owing to
genetic and environmental factors and even the phases of puberty and lifestyle choices, along
with physical activity, size, weight, lean body mass and food. A research study used dual-energy
X-ray absorptiometry to evaluate bone mass for up to four years at various locations in
Australian, African, Latino and Caucasian people between ages 9 to 5 years. Black people had
higher mean concentrations of area bone mineral density (BMD) as well as volumetric BMD at
all skeletal locations evaluated of many women. Of many Australian and Caucasian women,
femoral neck volumetric BMD was smaller than those in Hispanic people. There is really limited
information readily accessible on the connection among 25(OH)D levels and bone turnover
markers in adolescent girls (Saggese, et al., 2015). The serum concentration of adolescent vitamin
D is an integral factor for gaining bone mass. Rickets are correlated with prolonged very small
serum concentrations of 25(OH)D, although inadequate concentrations (< 50 nmol / L) change
the intake of calcium and bone mineralized. Serum calcium and vitamin D are correlated with
complete body or hip BMD, and when modified of age, gender and swimming relationships are
decreased.
The consequences of low level of vitamin D on muscle activity are indeed obvious in post
menarche women forward to weight change. Vitamin D seemed to affect brain function in many
respects before changes in the bone mass can be detected (De Souza Silva, 2016). Young ladies
with appropriate status of vitamin D had greater muscle power comparative to those with bad
status of vitamin D.
MICRONUTRIENT REQUIRED FOR ADOLESCENTS GROUP 12
Vitamin D seems to affect brain function and brain development. In specific, throughout the
brain and spinal cord, this vitamin may play an immunomodulatory function. Hypocalcemia-
induced tetany might be correlated to deficiency of vitamin D in kids and adolescent (Aydogan,
Onder & Aycan, 2016). This state may bring signs and symptoms like losing sensation on face,
hands and fingers. There will be, indeed, no particular scientific research of particular
neurological impairment and vitamin D concentrations in kids as well as adolescents.
Conclusion
Adolescents requires the finest nutritional circumstances of vitamin D for their optimum
development and growth and to avoid the morbid circumstances outlined. Epidemiological
studies are required in order to identify the best dosages of vitamin D grounded on the
environmental variables mentioned in this research, in order to maintain adequate concentrations
of vitamin from intrauterine life as well as during the stages of adolescents for the
commencement of the highest possible health.
Efficient precautionary approaches are required to ensure appropriate concentrations of vitamin
D all across adolescence, considering the geographical location, time of the year, pollution
concentrations, skin features, eating habits and body weight, with a perspective to ensuring
optimum health during these stages and preventing problems in adults. The positive impact of
mild sunlight requires to be renewed welcomed in order to provide all people with vitamin D
required to ensure perfect health. Furthermore, owing to the danger of skin cancer, extended
exposure to the sun is not proposed. Furthermore, a healthy diet is stated because nutrients lots of
vitamin D are better assimilated than supplements
Vitamin D seems to affect brain function and brain development. In specific, throughout the
brain and spinal cord, this vitamin may play an immunomodulatory function. Hypocalcemia-
induced tetany might be correlated to deficiency of vitamin D in kids and adolescent (Aydogan,
Onder & Aycan, 2016). This state may bring signs and symptoms like losing sensation on face,
hands and fingers. There will be, indeed, no particular scientific research of particular
neurological impairment and vitamin D concentrations in kids as well as adolescents.
Conclusion
Adolescents requires the finest nutritional circumstances of vitamin D for their optimum
development and growth and to avoid the morbid circumstances outlined. Epidemiological
studies are required in order to identify the best dosages of vitamin D grounded on the
environmental variables mentioned in this research, in order to maintain adequate concentrations
of vitamin from intrauterine life as well as during the stages of adolescents for the
commencement of the highest possible health.
Efficient precautionary approaches are required to ensure appropriate concentrations of vitamin
D all across adolescence, considering the geographical location, time of the year, pollution
concentrations, skin features, eating habits and body weight, with a perspective to ensuring
optimum health during these stages and preventing problems in adults. The positive impact of
mild sunlight requires to be renewed welcomed in order to provide all people with vitamin D
required to ensure perfect health. Furthermore, owing to the danger of skin cancer, extended
exposure to the sun is not proposed. Furthermore, a healthy diet is stated because nutrients lots of
vitamin D are better assimilated than supplements
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



