University Name - VLAD Data Analysis and Action Plan for Stroke Unit
VerifiedAdded on 2021/05/31
|12
|3224
|128
Report
AI Summary
This report presents an analysis of VLAD data related to stroke in-hospital mortality, focusing on the interpretation of VLAD graphs, identification of underlying issues, and the development of an action plan to improve performance within a hospital's acute stroke unit. The analysis includes a breakdown of VLAD graph features, identification of issues indicated by the graph, and a detailed investigation into potential causes, categorized by professional personnel, processes of care, structures or resources, patient case mix, and data. The report proposes specific actions to address each issue, including improvements in coding and classification, case mix adjustments, structural enhancements, process optimization, and data integrity. Furthermore, the report outlines strategies for monitoring stroke management, including early patient mobilization, rehabilitation programs, and multidisciplinary team approaches. Finally, the report addresses the importance of patient experience feedback, proposing a four-stage process involving normative, structural, and organizational legitimacy, culminating in a comprehensive action plan to incorporate patient feedback into service improvements. The report aims to enhance patient care and outcomes within the hospital setting.

Running Head: ANALYSIS OF VLAD DATA 1
Analysis of VLAD Data
Unit Title
Student Name
University Name
Analysis of VLAD Data
Unit Title
Student Name
University Name
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Running Head: ANALYSIS OF VLAD DATA 2
Analysis of VLAD data (Stroke In-Hospital Mortality VLAD, Jul 2011 - Nov 2014) and
development of an action plan to improve performance (2000 words)
Note: There are 4 parts to this task. Please make sure you attempt all parts. You cannot
answer these questions without referring to the provided resource – VLADs for Dummies.
1. How are VLAD graphs interpreted? Explain the important features/aspects of a
VLAD graph? As an example, what does the red line, blue line, black line
indicate, what are the numbers, what does the y axis indicate, what are the level 1
to 3 limits for (Note: this is not an exhaustive list. There may be other features that
you should explain-what they are and what is their purpose)?
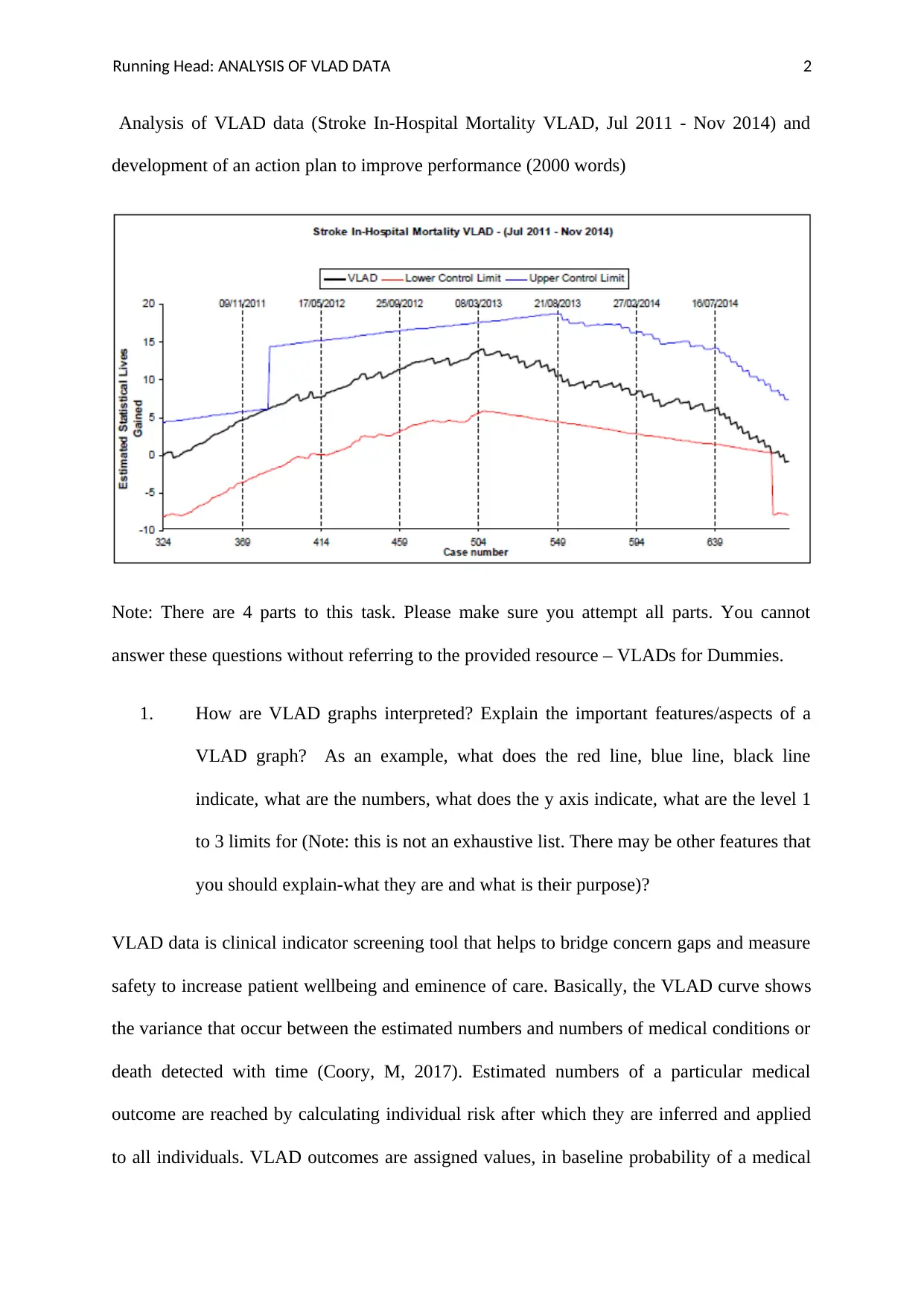
VLAD data is clinical indicator screening tool that helps to bridge concern gaps and measure
safety to increase patient wellbeing and eminence of care. Basically, the VLAD curve shows
the variance that occur between the estimated numbers and numbers of medical conditions or
death detected with time (Coory, M, 2017). Estimated numbers of a particular medical
outcome are reached by calculating individual risk after which they are inferred and applied
to all individuals. VLAD outcomes are assigned values, in baseline probability of a medical
Analysis of VLAD data (Stroke In-Hospital Mortality VLAD, Jul 2011 - Nov 2014) and
development of an action plan to improve performance (2000 words)
Note: There are 4 parts to this task. Please make sure you attempt all parts. You cannot
answer these questions without referring to the provided resource – VLADs for Dummies.
1. How are VLAD graphs interpreted? Explain the important features/aspects of a
VLAD graph? As an example, what does the red line, blue line, black line
indicate, what are the numbers, what does the y axis indicate, what are the level 1
to 3 limits for (Note: this is not an exhaustive list. There may be other features that
you should explain-what they are and what is their purpose)?
VLAD data is clinical indicator screening tool that helps to bridge concern gaps and measure
safety to increase patient wellbeing and eminence of care. Basically, the VLAD curve shows
the variance that occur between the estimated numbers and numbers of medical conditions or
death detected with time (Coory, M, 2017). Estimated numbers of a particular medical
outcome are reached by calculating individual risk after which they are inferred and applied
to all individuals. VLAD outcomes are assigned values, in baseline probability of a medical
Running Head: ANALYSIS OF VLAD DATA 3
outcome occurring, the probability is represented by P, where P is between 0 and 1 (Liu, M,
2011). Interpretation of score include 0-1(10%) where an event is unlikely to occur and
0.9(90%) an event is highly likely to occur. All these are calculated through logistic
regression. Therefore, VLAD mark score is the accumulative aggregate score by time which
stands for accumulative variation between predictable and detected medical outcome (Lopez,
A, 2016).When variance exceeds zero then less outcomes than perceived occur, and when
below zero then there have been additional outcomes than anticipated. Charting VLAD is
made by scheming VLAD mark by time this tells developments with time. Subgroups like
trial arms and different hospitals can be plotted independently with various traces on the same
VLAD chart. On the chart the VLAD graph has various lines with different interpretation
(Noxez, L, 2009). Each dot characterises a patient who had a medical condition or disease.
When the patient lived the line travels upwards but when the patient perished the line travels
downwards. The probability of a patient dying directly impacts the degree of movement of
the line up or down. There are also three lines namely: VLAD black line; the lower control
limit represented by the red line and upper control limit represented by the blue line. The
upper and lower control limits represent the boundaries of acceptable differences (Murraf, M,
2012). Cases whereby the VLAD line touches any of the control lines the exact place where it
has touched is flagged. At this point it calls for an intervention approach to determine the
reasons for the difference from national score.
VLAD probes the following:
I. Medical indicators
II. It aims to find a particular result,
outcome occurring, the probability is represented by P, where P is between 0 and 1 (Liu, M,
2011). Interpretation of score include 0-1(10%) where an event is unlikely to occur and
0.9(90%) an event is highly likely to occur. All these are calculated through logistic
regression. Therefore, VLAD mark score is the accumulative aggregate score by time which
stands for accumulative variation between predictable and detected medical outcome (Lopez,
A, 2016).When variance exceeds zero then less outcomes than perceived occur, and when
below zero then there have been additional outcomes than anticipated. Charting VLAD is
made by scheming VLAD mark by time this tells developments with time. Subgroups like
trial arms and different hospitals can be plotted independently with various traces on the same
VLAD chart. On the chart the VLAD graph has various lines with different interpretation
(Noxez, L, 2009). Each dot characterises a patient who had a medical condition or disease.
When the patient lived the line travels upwards but when the patient perished the line travels
downwards. The probability of a patient dying directly impacts the degree of movement of
the line up or down. There are also three lines namely: VLAD black line; the lower control
limit represented by the red line and upper control limit represented by the blue line. The
upper and lower control limits represent the boundaries of acceptable differences (Murraf, M,
2012). Cases whereby the VLAD line touches any of the control lines the exact place where it
has touched is flagged. At this point it calls for an intervention approach to determine the
reasons for the difference from national score.
VLAD probes the following:
I. Medical indicators
II. It aims to find a particular result,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Running Head: ANALYSIS OF VLAD DATA 4
III. It creates boundaries of cut off for responsive increase or decrease,
IV. Observed period and
V. Exact location whereby the study was conducted.
VLAD utilises the logistic regression in calculating clinical indicator probability and its
outcome which is based on an individual patient. If the VLAD curves rise to above zero then
the first patient surviving is likely in comparison to the probability of the patient dying
(Kaira, L, 2014). If the VLAD curve decreases the likelihood of the first patient dying is
likely in comparison to the patient surviving. Hence, the remaining plots is applied to the
remaining patients. VLAD encapsulates a process of flagging which happens once a specified
level of difference is reached by three flagging levels. Once a VLAD flag happens on specific
place it means over a period there have been additional (or fewer) patients having the result
than estimated, upwards till the specific patient. The technique to look at this graph is to
originally express for flags and then view rearward from the flagging plug to figure out the
patients for evaluation. Flagging levels can happen at upper or lower levels. The level 3 flag
is the upper level, this indicates that the hospital’s result rate is lower than the national result
rate (Tan, H, 2015). The level 1 flag is the lower level flag shows that the hospital degree
exceeds the national result rate. Finally, level 2 flag is the medium level which rests at broad
level, staying inside the upper and lower control limits. This shows that that clinic’s outcome
rate is same as the national outcome rate.
III. It creates boundaries of cut off for responsive increase or decrease,
IV. Observed period and
V. Exact location whereby the study was conducted.
VLAD utilises the logistic regression in calculating clinical indicator probability and its
outcome which is based on an individual patient. If the VLAD curves rise to above zero then
the first patient surviving is likely in comparison to the probability of the patient dying
(Kaira, L, 2014). If the VLAD curve decreases the likelihood of the first patient dying is
likely in comparison to the patient surviving. Hence, the remaining plots is applied to the
remaining patients. VLAD encapsulates a process of flagging which happens once a specified
level of difference is reached by three flagging levels. Once a VLAD flag happens on specific
place it means over a period there have been additional (or fewer) patients having the result
than estimated, upwards till the specific patient. The technique to look at this graph is to
originally express for flags and then view rearward from the flagging plug to figure out the
patients for evaluation. Flagging levels can happen at upper or lower levels. The level 3 flag
is the upper level, this indicates that the hospital’s result rate is lower than the national result
rate (Tan, H, 2015). The level 1 flag is the lower level flag shows that the hospital degree
exceeds the national result rate. Finally, level 2 flag is the medium level which rests at broad
level, staying inside the upper and lower control limits. This shows that that clinic’s outcome
rate is same as the national outcome rate.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Running Head: ANALYSIS OF VLAD DATA 5
2. Describe the issues that are evident when you analyse this VLAD graph above, i.e.
what does the graph tell you?
The VLAD line moves up and touches the upper control limit between 09/11/2011 and
17/5/2012. The ‘flag’ shows that the hospital has a lesser mortality frequency than the
national regular average.
The VLAD line rests at broad level, staying inside the higher and lower control limits. This
shows that that hospital’s transience rate is the same to the national mortality rate.
The VLAD line moves down and touches the Lower control limit below. This ‘flag’ shows
that the hospital has a higher mortality rate than the national regular average (Cook, D, 2011).
3. You are the Director of the Acute Stroke Unit of a large hospital. Your CEO has
passed the above VLAD chart on to you. The CEO has asked to you investigate the issues
identified from the chart and to prepare a report to advise her on the following:
a. The underlying issues –what could be the causes of the problems evident in this chart?
Note: As you do not have access to the patient records you will need to use the pyramid of
investigation categories and describe potential causes for each category.
The underlying issues are as follows: Starting from professional bit of personnel this occurs
due to differences in commonality of personnel involved. The underlying issue is failure to
offer additional support for delivery of the best possible care (Arcavi, A, 2013). Secondly,
processes of care occur due to lack of enough reviews in service delivery in hospital
environments. This makes issues not to be identified due to both poor and inconsistent
monitoring and investigating alerts. Thirdly, structures or resources, this occurs through
application of different care pathways seen in the end of life care. Other notable differences
2. Describe the issues that are evident when you analyse this VLAD graph above, i.e.
what does the graph tell you?
The VLAD line moves up and touches the upper control limit between 09/11/2011 and
17/5/2012. The ‘flag’ shows that the hospital has a lesser mortality frequency than the
national regular average.
The VLAD line rests at broad level, staying inside the higher and lower control limits. This
shows that that hospital’s transience rate is the same to the national mortality rate.
The VLAD line moves down and touches the Lower control limit below. This ‘flag’ shows
that the hospital has a higher mortality rate than the national regular average (Cook, D, 2011).
3. You are the Director of the Acute Stroke Unit of a large hospital. Your CEO has
passed the above VLAD chart on to you. The CEO has asked to you investigate the issues
identified from the chart and to prepare a report to advise her on the following:
a. The underlying issues –what could be the causes of the problems evident in this chart?
Note: As you do not have access to the patient records you will need to use the pyramid of
investigation categories and describe potential causes for each category.
The underlying issues are as follows: Starting from professional bit of personnel this occurs
due to differences in commonality of personnel involved. The underlying issue is failure to
offer additional support for delivery of the best possible care (Arcavi, A, 2013). Secondly,
processes of care occur due to lack of enough reviews in service delivery in hospital
environments. This makes issues not to be identified due to both poor and inconsistent
monitoring and investigating alerts. Thirdly, structures or resources, this occurs through
application of different care pathways seen in the end of life care. Other notable differences
Running Head: ANALYSIS OF VLAD DATA 6
include lack of weekend discharges. Fourthly, it can be caused by patient case mix, this
happens due to unusual event that has happened in the specified time frame example poor
prognosis of patient who arrive in the hospital with an ambulance or delayed presentation of a
patient for medical action (Hayes, A, 2013). This is through atypical run of severely ill
patients. Lastly, data, this occurs when the hospital submits incorrect or unreliable data when
applied to dissimilar data codes from other hospitals. This alters hospital standardized
mortality rate through creating of poor coding depth that impacts subordinate codes.
b. What are the actions that you would put in place to investigate each of the issues or
problems that you have described in (a) above? Note: it may save time and be more logical to
answer (a) and (b) together.
First on coding and classification, I will encourage coders and clinicians to have closer work
processes to increases professional roles and limitations. Due to medical accuracy I will also
encourage clinicians to utilise medical audit tools to determine the best diagnosis and
procedural code. I will also encourage professional understanding of data entry staff and its
significance to the hospital (Lavados, P, 2017). Secondly, on the case mix, I will ensure that
co-morbidity is correct to arrive at true case mix of the patient. Thirdly, on Structure, I will
ensure that there is weekend discharges and nurse-led discharges. Fourthly, on process, I will
start to consider issues that relate to potential safety and quality. I will also ensure monitoring
and investigation alerts are working properly to identify issues on service delivery. Lastly, I
will ensure there is commonality in service delivery of personnel involved and ensure that I
offer extra support to guarantee highest state of care on patients.
c. What strategies will you now put in place to monitor stroke management within the
hospital?
MANAGEMENT AND PREVENTION SERVICES
include lack of weekend discharges. Fourthly, it can be caused by patient case mix, this
happens due to unusual event that has happened in the specified time frame example poor
prognosis of patient who arrive in the hospital with an ambulance or delayed presentation of a
patient for medical action (Hayes, A, 2013). This is through atypical run of severely ill
patients. Lastly, data, this occurs when the hospital submits incorrect or unreliable data when
applied to dissimilar data codes from other hospitals. This alters hospital standardized
mortality rate through creating of poor coding depth that impacts subordinate codes.
b. What are the actions that you would put in place to investigate each of the issues or
problems that you have described in (a) above? Note: it may save time and be more logical to
answer (a) and (b) together.
First on coding and classification, I will encourage coders and clinicians to have closer work
processes to increases professional roles and limitations. Due to medical accuracy I will also
encourage clinicians to utilise medical audit tools to determine the best diagnosis and
procedural code. I will also encourage professional understanding of data entry staff and its
significance to the hospital (Lavados, P, 2017). Secondly, on the case mix, I will ensure that
co-morbidity is correct to arrive at true case mix of the patient. Thirdly, on Structure, I will
ensure that there is weekend discharges and nurse-led discharges. Fourthly, on process, I will
start to consider issues that relate to potential safety and quality. I will also ensure monitoring
and investigation alerts are working properly to identify issues on service delivery. Lastly, I
will ensure there is commonality in service delivery of personnel involved and ensure that I
offer extra support to guarantee highest state of care on patients.
c. What strategies will you now put in place to monitor stroke management within the
hospital?
MANAGEMENT AND PREVENTION SERVICES
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Running Head: ANALYSIS OF VLAD DATA 7
I will initiate a process whereby the patients with stroke are mobilised as early as possible.
I will start a patient stroke rehabilitation programme whereby occupational therapists will
assist in patient’s personal act of daily living for those living with stroke (Ducket, S, 2017).
I will initiate and encourage threadmill training that aims at improving gait and speed in
people who are self-governing in walking at the beginning of treatment.
I will adopt the approach mechanism in regard to physiotherapists and give preferences to
individual patient needs.
I will encourage repetitive task training to improve gait, speed, functional ambulation this
should be done in regard safety and acceptability to the patient.
I will screen patients for visual problems and do referrals.
I will initiate nutritional monitoring after stroke using the following parameters like
biochemical status, swallowing status, weight loss monitoring, dependence and eating
assessment and nutrition intake.
I will offer services for electrical stimulation especially to supraspinatus and deltoid muscles
in shoulder subluxation stroke patients
I will set up a multidisciplinary team for stroke patients whereby they will be treated 24 hours
a day by specialists in stroke unit.
I will ensure routinely and timely provision of information to patient and care givers that
gives a set of education and counselling techniques.
ORGANIZATIONAL SERVICES
I will initiate a process whereby the patients with stroke are mobilised as early as possible.
I will start a patient stroke rehabilitation programme whereby occupational therapists will
assist in patient’s personal act of daily living for those living with stroke (Ducket, S, 2017).
I will initiate and encourage threadmill training that aims at improving gait and speed in
people who are self-governing in walking at the beginning of treatment.
I will adopt the approach mechanism in regard to physiotherapists and give preferences to
individual patient needs.
I will encourage repetitive task training to improve gait, speed, functional ambulation this
should be done in regard safety and acceptability to the patient.
I will screen patients for visual problems and do referrals.
I will initiate nutritional monitoring after stroke using the following parameters like
biochemical status, swallowing status, weight loss monitoring, dependence and eating
assessment and nutrition intake.
I will offer services for electrical stimulation especially to supraspinatus and deltoid muscles
in shoulder subluxation stroke patients
I will set up a multidisciplinary team for stroke patients whereby they will be treated 24 hours
a day by specialists in stroke unit.
I will ensure routinely and timely provision of information to patient and care givers that
gives a set of education and counselling techniques.
ORGANIZATIONAL SERVICES
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Running Head: ANALYSIS OF VLAD DATA 8
I will ensure that I provide a specialised and coordinated multidisciplinary team to
specifically mainten stroke patients in the stroke unit. Specialisation increases service
provision and improves advanced practice.
I will provide individual generic rehabilitation on circumstances whereby stroke unit
admission is not possible.
I will synergize a core multidisciplinary team which will intervene where services like
occupational therapy, speech and language therapy, physiotherapy services are needed.
I will provide timely active involvement process for patient and caregivers (Chenatia, H,
2011).
4. The quality manager has recommended that you also consider patient experience feedback
as part of your investigation. How would you respond to this request?
I will initiate a process that follows the following processes:
Stage one: Normative legitimacy which expresses their openness and positive response to
feedback from their patients through ward teams. I will assure the quality team on authentic
improvements and acting on patient feedback.
Stage two: Structural legitimacy which I will look for autonomy, ownership and resource
factors. After I have received sufficient data collected from patients, I will create and enact
change based on patient feedback. I will look for autonomic sense of change from the staff
which can be acted on at an individual level. The staff should own the issues raised by the
I will ensure that I provide a specialised and coordinated multidisciplinary team to
specifically mainten stroke patients in the stroke unit. Specialisation increases service
provision and improves advanced practice.
I will provide individual generic rehabilitation on circumstances whereby stroke unit
admission is not possible.
I will synergize a core multidisciplinary team which will intervene where services like
occupational therapy, speech and language therapy, physiotherapy services are needed.
I will provide timely active involvement process for patient and caregivers (Chenatia, H,
2011).
4. The quality manager has recommended that you also consider patient experience feedback
as part of your investigation. How would you respond to this request?
I will initiate a process that follows the following processes:
Stage one: Normative legitimacy which expresses their openness and positive response to
feedback from their patients through ward teams. I will assure the quality team on authentic
improvements and acting on patient feedback.
Stage two: Structural legitimacy which I will look for autonomy, ownership and resource
factors. After I have received sufficient data collected from patients, I will create and enact
change based on patient feedback. I will look for autonomic sense of change from the staff
which can be acted on at an individual level. The staff should own the issues raised by the
Running Head: ANALYSIS OF VLAD DATA 9
patient and I will allocate the resources for improvement of services through change (Guest,
R, 2012).
Stage three: I will look into organizational readiness to the change through inter-departmental
working and partnership to get to consistent progress. On the other hand, I will build the
capacity of superior hospital organisation and levels of organization goodwill, provision and
enable staff effort on advancement (Bergstand, M, 2011). The intervention strategies geared
at facilitating an organization to be ready for change include: increasing trust levels in the
processes to be initiated, autonomous collection feedback on quality by research team, peer
training, motivation and support (Kessler, R, 2017).
Stage four: I will initiate an action plan in the following ways:
I will assemble all hospital management and review the due process and provide governance
through the following processes:
I will institute the governance process which specifies the personnel notified, implementers
of variation review report, monitoring and evaluation of the actions of review.
I will encourage the clinicians and coding staff to offer leadership to the review process.
I will start a review process in a timely and perform due care. Which touches on potential
issues raised to data, case mixes in hospitals, investigate structure in hospitals and ensure that
processes of care are followed and issues of professional care are looked into
(Andrianopoulos, N, 2012).
I will nominate key issue identified and initiate appropriate action.
I will disseminate data and lessons received to personnel involved in stroke management.
I will identify actions that are geared towards improvement of service delivery.
patient and I will allocate the resources for improvement of services through change (Guest,
R, 2012).
Stage three: I will look into organizational readiness to the change through inter-departmental
working and partnership to get to consistent progress. On the other hand, I will build the
capacity of superior hospital organisation and levels of organization goodwill, provision and
enable staff effort on advancement (Bergstand, M, 2011). The intervention strategies geared
at facilitating an organization to be ready for change include: increasing trust levels in the
processes to be initiated, autonomous collection feedback on quality by research team, peer
training, motivation and support (Kessler, R, 2017).
Stage four: I will initiate an action plan in the following ways:
I will assemble all hospital management and review the due process and provide governance
through the following processes:
I will institute the governance process which specifies the personnel notified, implementers
of variation review report, monitoring and evaluation of the actions of review.
I will encourage the clinicians and coding staff to offer leadership to the review process.
I will start a review process in a timely and perform due care. Which touches on potential
issues raised to data, case mixes in hospitals, investigate structure in hospitals and ensure that
processes of care are followed and issues of professional care are looked into
(Andrianopoulos, N, 2012).
I will nominate key issue identified and initiate appropriate action.
I will disseminate data and lessons received to personnel involved in stroke management.
I will identify actions that are geared towards improvement of service delivery.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Running Head: ANALYSIS OF VLAD DATA
10
I will inform the board and get assurance on highest level governance.
REFERENCES
Duckett, S. J., Coory, M., & Sketcher-Baker, K. (2007). Identifying variations in quality of
care in Queensland hospitals. Medical Journal of Australia, 187(10), 571.
Cook, D. A., Coory, M., & Webster, R. A. (2011). Exponentially weighted moving average
charts to compare observed and expected values for monitoring risk-adjusted hospital
indicators. BMJ quality & safety, 20(6), 469-474.
Coory, M., Duckett, S., & Sketcher-Baker, K. (2007). Using control charts to monitor quality
of hospital care with administrative data. International Journal for Quality in Health
Care, 20(1), 31-39.
Chenaitia, H., Massa, H., Toesca, R., Michelet, P., Auffray, J. P., & Gariboldi, V. (2011).
Mobile cardio-respiratory support in prehospital emergency medicine. European Journal of
Emergency Medicine, 18(2), 99-101.
Andrianopoulos, N., Jolley, D., Evans, S. M., Brand, C. A., & Cameron, P. A. (2012).
Application of variable life adjusted displays (VLAD) on Victorian admitted episodes dataset
(VAED). BMC health services research, 12(1), 278.
Tan, H. B., Cross, S. F., & Goodacre, S. W. (2005). Application of variable life adjusted
display (VLAD) in early detection of deficiency in trauma care. Emergency medicine
journal, 22(10), 726-728.
10
I will inform the board and get assurance on highest level governance.
REFERENCES
Duckett, S. J., Coory, M., & Sketcher-Baker, K. (2007). Identifying variations in quality of
care in Queensland hospitals. Medical Journal of Australia, 187(10), 571.
Cook, D. A., Coory, M., & Webster, R. A. (2011). Exponentially weighted moving average
charts to compare observed and expected values for monitoring risk-adjusted hospital
indicators. BMJ quality & safety, 20(6), 469-474.
Coory, M., Duckett, S., & Sketcher-Baker, K. (2007). Using control charts to monitor quality
of hospital care with administrative data. International Journal for Quality in Health
Care, 20(1), 31-39.
Chenaitia, H., Massa, H., Toesca, R., Michelet, P., Auffray, J. P., & Gariboldi, V. (2011).
Mobile cardio-respiratory support in prehospital emergency medicine. European Journal of
Emergency Medicine, 18(2), 99-101.
Andrianopoulos, N., Jolley, D., Evans, S. M., Brand, C. A., & Cameron, P. A. (2012).
Application of variable life adjusted displays (VLAD) on Victorian admitted episodes dataset
(VAED). BMC health services research, 12(1), 278.
Tan, H. B., Cross, S. F., & Goodacre, S. W. (2005). Application of variable life adjusted
display (VLAD) in early detection of deficiency in trauma care. Emergency medicine
journal, 22(10), 726-728.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Running Head: ANALYSIS OF VLAD DATA
11
Noyez, L. (2009). Control charts, Cusum techniques and funnel plots. A review of methods
for monitoring performance in healthcare. Interactive cardiovascular and thoracic
surgery, 9(3), 494-499.
Guest, R. V., Chandrabalan, V. V., Murray, G. D., & Auld, C. D. (2012). Application of
Variable Life Adjusted Display (VLAD) to risk-adjusted mortality of esophagogastric cancer
surgery. World journal of surgery, 36(1), 104-108.
Arcavi, A. (2003). The role of visual representations in the learning of
mathematics. Educational studies in mathematics, 52(3), 215-241.
Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T., & Murray, C. J. (2006). Global and
regional burden of disease and risk factors, 2001: systematic analysis of population health
data. The Lancet, 367(9524), 1747-1757.
Kessler, R. C., Andrews, G., Mroczek, D., Ustun, B., & Wittchen, H. U. (1998). The world
health organization composite international diagnostic interview short‐form (cidi‐
sf). International journal of methods in psychiatric research, 7(4), 171-185.
Murray, C. J. (1994). Quantifying the burden of disease: the technical basis for disability-
adjusted life years. Bulletin of the World health Organization, 72(3), 429.
Hayes, A. J., Leal, J., Gray, A. M., Holman, R. R., & Clarke, P. M. (2013). UKPDS outcomes
model 2: a new version of a model to simulate lifetime health outcomes of patients with type
2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study:
UKPDS 82. Diabetologia, 56(9), 1925-1933.
Bergstrand, M., Hooker, A. C., Wallin, J. E., & Karlsson, M. O. (2011). Prediction-corrected
visual predictive checks for diagnosing nonlinear mixed-effects models. The AAPS
journal, 13(2), 143-151.
11
Noyez, L. (2009). Control charts, Cusum techniques and funnel plots. A review of methods
for monitoring performance in healthcare. Interactive cardiovascular and thoracic
surgery, 9(3), 494-499.
Guest, R. V., Chandrabalan, V. V., Murray, G. D., & Auld, C. D. (2012). Application of
Variable Life Adjusted Display (VLAD) to risk-adjusted mortality of esophagogastric cancer
surgery. World journal of surgery, 36(1), 104-108.
Arcavi, A. (2003). The role of visual representations in the learning of
mathematics. Educational studies in mathematics, 52(3), 215-241.
Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T., & Murray, C. J. (2006). Global and
regional burden of disease and risk factors, 2001: systematic analysis of population health
data. The Lancet, 367(9524), 1747-1757.
Kessler, R. C., Andrews, G., Mroczek, D., Ustun, B., & Wittchen, H. U. (1998). The world
health organization composite international diagnostic interview short‐form (cidi‐
sf). International journal of methods in psychiatric research, 7(4), 171-185.
Murray, C. J. (1994). Quantifying the burden of disease: the technical basis for disability-
adjusted life years. Bulletin of the World health Organization, 72(3), 429.
Hayes, A. J., Leal, J., Gray, A. M., Holman, R. R., & Clarke, P. M. (2013). UKPDS outcomes
model 2: a new version of a model to simulate lifetime health outcomes of patients with type
2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study:
UKPDS 82. Diabetologia, 56(9), 1925-1933.
Bergstrand, M., Hooker, A. C., Wallin, J. E., & Karlsson, M. O. (2011). Prediction-corrected
visual predictive checks for diagnosing nonlinear mixed-effects models. The AAPS
journal, 13(2), 143-151.
Running Head: ANALYSIS OF VLAD DATA
12
Liu, M., Wu, B., Wang, W. Z., Lee, L. M., Zhang, S. H., & Kong, L. Z. (2007). Stroke in
China: epidemiology, prevention, and management strategies. The Lancet Neurology, 6(5),
456-464.
Lavados, P. M., Hennis, A. J., Fernandes, J. G., Medina, M. T., Legetic, B., Hoppe, A., ... &
Salinas, R. (2007). Stroke epidemiology, prevention, and management strategies at a regional
level: Latin America and the Caribbean. The Lancet Neurology, 6(4), 362-372.
Kalra, L., Evans, A., Perez, I., Knapp, M., Donaldson, N., & Swift, C. G. (2000). Alternative
strategies for stroke care: a prospective randomised controlled trial. The Lancet, 356(9233),
894-899.
12
Liu, M., Wu, B., Wang, W. Z., Lee, L. M., Zhang, S. H., & Kong, L. Z. (2007). Stroke in
China: epidemiology, prevention, and management strategies. The Lancet Neurology, 6(5),
456-464.
Lavados, P. M., Hennis, A. J., Fernandes, J. G., Medina, M. T., Legetic, B., Hoppe, A., ... &
Salinas, R. (2007). Stroke epidemiology, prevention, and management strategies at a regional
level: Latin America and the Caribbean. The Lancet Neurology, 6(4), 362-372.
Kalra, L., Evans, A., Perez, I., Knapp, M., Donaldson, N., & Swift, C. G. (2000). Alternative
strategies for stroke care: a prospective randomised controlled trial. The Lancet, 356(9233),
894-899.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.