Workplace Violence Against Homecare Workers: A Cross-Sectional Study
VerifiedAdded on 2023/06/04
|13
|11142
|323
Report
AI Summary
This research article, published in BMC Public Health, presents a cross-sectional study on workplace violence experienced by homecare workers. The study, conducted in Oregon, investigated the prevalence of verbal aggression, workplace aggression, workplace violence, sexual harassment, and sexu...
R E S E A R C H A R T I C L E Open Access
Workplace violence against homecare workers
and its relationship with workers health
outcomes:a cross-sectionalstudy
Ginger C Hanson1*
, Nancy A Perrin1
, Helen Moss2
, Naima Laharnar3 and Nancy Glass4
Abstract
Background:Consumer-driven homecare models support aging and disabled individuals to live independent
through the services of homecare workers.Although these models have benefits,including autonomy and control
over services,little evidence exists about challenges homecare workers may face when providing services,including
workplace violence and the negative outcomes associated with workplace violence.This study investigates the
prevalence of workplace violence among homecare workers and examines the relationship between these
experiences and homecare worker stress,burnout,depression,and sleep.
Methods:We recruited female homecare workers in Oregon,the first US state to implement a consumer driven
homecare model,to complete an on-line or telephone survey with peer interviewers.The survey asked about
demographics and included measures to assess workplace violence,fear,stress,burnout,depression and sleep
problems.
Results:Homecare workers (n = 1,214) reported past-year incidents of verbalaggression (50.3% of respondents),
workplace aggression (26.9%),workplace violence (23.6%),sexualharassment (25.7%),and sexualaggression (12.8%).
Exposure was associated with greater stress (p < .001),depression (p < .001),sleep problems (p < .001),and burnout
(p < .001).Confidence in addressing workplace aggression buffered homecare workers against negative work
health outcomes.
Conclusions:To ensure homecare worker safety and positive health outcomes in the provision of services,it is
criticalto develop and implement preventive safety training programs with policies and procedures that sup
homecare workers who experience harassment and violence.
Keywords:Homecare,Workplace aggression,Workplace violence,Sexualharassment,Burnout
Background
Our global population is aging;this is true for developed
and developing nations alike [1].Reasons for this trend
include both declining fertility rates and increases in life
expectancy.The current life expectancy at birth is now
over 80 in 33 countries.Given the significance ofthis
trend,there is a need for health care policies thatwill
improve the quality of life for aging and disabled popula-
tion,their family and those caring for them.The elderly
and disabled have repeatedly expressed theirdesire to
have controlover care and remain active in their com-
munities,therefore,in an effortto meetthese appeals,
health care funding policies in mostwestern countries
for long-term care for elders and disabled persons are
shifting away from institutions,such as nursing homes
and long-term care settings to the client’s home [2].
One approach innovative to homecare is the consumer-
driven modelin the U.S.,or self-directed modelas it is
called in the UK [3].The consumer-driven model funded
through Federal/Stateentitlementprograms,such as
Medicaid/Medicare in the US,enables elderly ordis-
abled individuals in need of supportive care to continue
to live in their homes and communities while receiving
support with activities of daily living (ADLs).Homecare
* Correspondence:ginger.c.hanson@kpchr.org
1Research Data and Analysis Center,Center for Health Research,Portland,
Oregon,USA
Fulllist of author information is available at the end of the article
© 2015 Hanson et al.;licensee BioMed Central.This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/4.0),which permits unrestricted use,distribution,and
reproduction in any medium,provided the originalwork is properly credited.The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,
unless otherwise stated.
Hanson et al.BMC Public Health (2015) 15:11
DOI10.1186/s12889-014-1340-7
Workplace violence against homecare workers
and its relationship with workers health
outcomes:a cross-sectionalstudy
Ginger C Hanson1*
, Nancy A Perrin1
, Helen Moss2
, Naima Laharnar3 and Nancy Glass4
Abstract
Background:Consumer-driven homecare models support aging and disabled individuals to live independent
through the services of homecare workers.Although these models have benefits,including autonomy and control
over services,little evidence exists about challenges homecare workers may face when providing services,including
workplace violence and the negative outcomes associated with workplace violence.This study investigates the
prevalence of workplace violence among homecare workers and examines the relationship between these
experiences and homecare worker stress,burnout,depression,and sleep.
Methods:We recruited female homecare workers in Oregon,the first US state to implement a consumer driven
homecare model,to complete an on-line or telephone survey with peer interviewers.The survey asked about
demographics and included measures to assess workplace violence,fear,stress,burnout,depression and sleep
problems.
Results:Homecare workers (n = 1,214) reported past-year incidents of verbalaggression (50.3% of respondents),
workplace aggression (26.9%),workplace violence (23.6%),sexualharassment (25.7%),and sexualaggression (12.8%).
Exposure was associated with greater stress (p < .001),depression (p < .001),sleep problems (p < .001),and burnout
(p < .001).Confidence in addressing workplace aggression buffered homecare workers against negative work
health outcomes.
Conclusions:To ensure homecare worker safety and positive health outcomes in the provision of services,it is
criticalto develop and implement preventive safety training programs with policies and procedures that sup
homecare workers who experience harassment and violence.
Keywords:Homecare,Workplace aggression,Workplace violence,Sexualharassment,Burnout
Background
Our global population is aging;this is true for developed
and developing nations alike [1].Reasons for this trend
include both declining fertility rates and increases in life
expectancy.The current life expectancy at birth is now
over 80 in 33 countries.Given the significance ofthis
trend,there is a need for health care policies thatwill
improve the quality of life for aging and disabled popula-
tion,their family and those caring for them.The elderly
and disabled have repeatedly expressed theirdesire to
have controlover care and remain active in their com-
munities,therefore,in an effortto meetthese appeals,
health care funding policies in mostwestern countries
for long-term care for elders and disabled persons are
shifting away from institutions,such as nursing homes
and long-term care settings to the client’s home [2].
One approach innovative to homecare is the consumer-
driven modelin the U.S.,or self-directed modelas it is
called in the UK [3].The consumer-driven model funded
through Federal/Stateentitlementprograms,such as
Medicaid/Medicare in the US,enables elderly ordis-
abled individuals in need of supportive care to continue
to live in their homes and communities while receiving
support with activities of daily living (ADLs).Homecare
* Correspondence:ginger.c.hanson@kpchr.org
1Research Data and Analysis Center,Center for Health Research,Portland,
Oregon,USA
Fulllist of author information is available at the end of the article
© 2015 Hanson et al.;licensee BioMed Central.This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/4.0),which permits unrestricted use,distribution,and
reproduction in any medium,provided the originalwork is properly credited.The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,
unless otherwise stated.
Hanson et al.BMC Public Health (2015) 15:11
DOI10.1186/s12889-014-1340-7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
workers in the consumer-driven modelare employees
of the consumer rather than an organization/institution.
The homecareworkers,often non-licensed workers,
perform ADLs such as bathing and hygiene,dressing
and grooming,eating,elimination,mobility and cogni-
tion/behavior support,as wellas IADLs such as shop-
ping,housekeeping,mealpreparation,assistance with
medication and oxygen and transportation for their em-
ployer for an assigned number of hours daily [4].
The consumer-driven homecare model has a variety of
benefitsfor the consumer-employersand homecare
workers.For consumer employers,the modelsupports
the consumer’s autonomy and controlover who is hired
as their homecare worker and how the homecare worker
implementssupportfor the ADLs. Homecare workers
reportthatthey appreciate the informalwork environ-
ment ofthe home,the ability to negotiate flexible work
hours,and the meaningfulrelationships they can forge
with their consumer-employers [5].
Although there are benefits,the consumer-employer
and homecare worker relationship has the potentialfor
safety challenges.Specifically,given the weak labor mar-
ket position ofhomecare workers and their work in the
consumer employer’s home,our previous research has
demonstrated theirvulnerability to sexualharassment
and workplace violence [4].These socialand employ-
mentissues cannot be resolved in the same manner as
employmenthealth and safety issues within a hospital,
clinic or nursing home setting where employees have ac-
cessto employmentassistanceprograms,human re-
sourcesor security personnel.For homecare workers,
the workplace is the consumer employer’s home and the
perpetrator of sexual harassment and/or violence can be
eitherthe consumeremployeror a relative orfriend
with the consumeremployer.Further,limited training
initiatives aimed to prevent or respond to sexualharass-
ment and workplace violence are available to homecare
workers,and consumer-driven program policies often do
not specifically addresssexualharassmentand/orvio-
lence perpetrated by consumer employers or others in
the home against homecare workers.
Defining workplace violence
For our study,we used the definitions provided by Bar-
ling and colleagues [6],they defined four different types
of workplace violence thathomecare workers may ex-
perience:workplaceaggression,workplaceviolence,
sexualharassment,and sexualaggression.Workplace
aggression refers to acts ofnon-physicalaggression or
threats ofviolence in the work setting (e.g.cornering
someone,slamming a door,or threatening them with a
weapon).Some studies also categorize verbal aggression
(e.g.,yelling,insulting,belittling) separately from work-
place aggression [7-9]and we choseto follow this
convention.Workplaceviolencerefersto the occur-
rence ofphysicalassaultor physically threatening be-
havior (e.g.,hitting with a fist or other object,kicking,
biting,bumping with intentionalforce).Sexualharass-
ment is defined as the occurrence of acts of a sexual na-
ture that could be deemed offensive or intimidating,but
were not physical acts (e.g., sexual comments, unwanted
requests dates or sexualfavors,leaving sexually explicit
materialin view).SexualAggression was defined as the
occurrence ofacts ofa sexualnature involving physical
contact(e.g.,breaking personalboundaries,touching
someone in a sexual way).
Workplace violence in homecare
In the US,approximately 2 million workers are affected
by workplace violence annually [10].Workplace violence
in healthcare and socialservices occupations has been
recognizedgloballyas a major occupationalhazard
[11-14].Homicide is the number one cause ofdeath in
the workplace for nurses and employees in personal-care
facilities [15].Almost half of allnon-fatalassaults in US
workplaces occur in the healthcare or socialservice in-
dustries[14].In the U.K., wherea similarmodelof
homecare isbeing implemented,assaultswere among
the top causesof workplace injuriesresulting in 7 or
more days ofmissed work in both the healthcare and
residential care industries [16].
The threat of workplace violence is one of the top con-
cerns ofhome healthcare workers,ranking higher than
environmentalhazardsor transportation issues[17].
Severalfactors,including the lack ofa large nationally
representative sample and differencesin methodology
make it difficult to narrow in on the precise prevalence
of workplace violence,but looking across severalstudies
can offer some estimate.Survey results from severaldif-
ferentstudies have shown the percentage ofhomecare
workers experiencing any form of workplace violence to
be between 5-61% [7].Verbal aggression is the most per-
vasive,reportedby between18-59% of homecare
workers [6,7,17]:with the highest estimate coming from
a study that ask about abuse over the homecare worker’s
career [7] and the lower estimates coming from studies
that ask aboutthe occurrencein the last 6-months
[6,17].Workplaceaggression,or threatening behavior
were reported by 7-16% [6,7] of homecare workers,with
the highest percentage coming from a study that asked
about the occurrence over the homecare workers career
[7],and lower percentage coming from a study that re-
ported aboutthe occurrence in the last6 months [6].
Workplace violence orphysicalassaults were reported
by between 2-11% ofhomecare workers [6,17,18],with
the larger percentage coming from a broader definition
of workplaceviolencethat included being threatened
with a knife [6],and the smallerpercentagescoming
Hanson et al.BMC Public Health (2015) 15:11 Page 2 of 13
of the consumer rather than an organization/institution.
The homecareworkers,often non-licensed workers,
perform ADLs such as bathing and hygiene,dressing
and grooming,eating,elimination,mobility and cogni-
tion/behavior support,as wellas IADLs such as shop-
ping,housekeeping,mealpreparation,assistance with
medication and oxygen and transportation for their em-
ployer for an assigned number of hours daily [4].
The consumer-driven homecare model has a variety of
benefitsfor the consumer-employersand homecare
workers.For consumer employers,the modelsupports
the consumer’s autonomy and controlover who is hired
as their homecare worker and how the homecare worker
implementssupportfor the ADLs. Homecare workers
reportthatthey appreciate the informalwork environ-
ment ofthe home,the ability to negotiate flexible work
hours,and the meaningfulrelationships they can forge
with their consumer-employers [5].
Although there are benefits,the consumer-employer
and homecare worker relationship has the potentialfor
safety challenges.Specifically,given the weak labor mar-
ket position ofhomecare workers and their work in the
consumer employer’s home,our previous research has
demonstrated theirvulnerability to sexualharassment
and workplace violence [4].These socialand employ-
mentissues cannot be resolved in the same manner as
employmenthealth and safety issues within a hospital,
clinic or nursing home setting where employees have ac-
cessto employmentassistanceprograms,human re-
sourcesor security personnel.For homecare workers,
the workplace is the consumer employer’s home and the
perpetrator of sexual harassment and/or violence can be
eitherthe consumeremployeror a relative orfriend
with the consumeremployer.Further,limited training
initiatives aimed to prevent or respond to sexualharass-
ment and workplace violence are available to homecare
workers,and consumer-driven program policies often do
not specifically addresssexualharassmentand/orvio-
lence perpetrated by consumer employers or others in
the home against homecare workers.
Defining workplace violence
For our study,we used the definitions provided by Bar-
ling and colleagues [6],they defined four different types
of workplace violence thathomecare workers may ex-
perience:workplaceaggression,workplaceviolence,
sexualharassment,and sexualaggression.Workplace
aggression refers to acts ofnon-physicalaggression or
threats ofviolence in the work setting (e.g.cornering
someone,slamming a door,or threatening them with a
weapon).Some studies also categorize verbal aggression
(e.g.,yelling,insulting,belittling) separately from work-
place aggression [7-9]and we choseto follow this
convention.Workplaceviolencerefersto the occur-
rence ofphysicalassaultor physically threatening be-
havior (e.g.,hitting with a fist or other object,kicking,
biting,bumping with intentionalforce).Sexualharass-
ment is defined as the occurrence of acts of a sexual na-
ture that could be deemed offensive or intimidating,but
were not physical acts (e.g., sexual comments, unwanted
requests dates or sexualfavors,leaving sexually explicit
materialin view).SexualAggression was defined as the
occurrence ofacts ofa sexualnature involving physical
contact(e.g.,breaking personalboundaries,touching
someone in a sexual way).
Workplace violence in homecare
In the US,approximately 2 million workers are affected
by workplace violence annually [10].Workplace violence
in healthcare and socialservices occupations has been
recognizedgloballyas a major occupationalhazard
[11-14].Homicide is the number one cause ofdeath in
the workplace for nurses and employees in personal-care
facilities [15].Almost half of allnon-fatalassaults in US
workplaces occur in the healthcare or socialservice in-
dustries[14].In the U.K., wherea similarmodelof
homecare isbeing implemented,assaultswere among
the top causesof workplace injuriesresulting in 7 or
more days ofmissed work in both the healthcare and
residential care industries [16].
The threat of workplace violence is one of the top con-
cerns ofhome healthcare workers,ranking higher than
environmentalhazardsor transportation issues[17].
Severalfactors,including the lack ofa large nationally
representative sample and differencesin methodology
make it difficult to narrow in on the precise prevalence
of workplace violence,but looking across severalstudies
can offer some estimate.Survey results from severaldif-
ferentstudies have shown the percentage ofhomecare
workers experiencing any form of workplace violence to
be between 5-61% [7].Verbal aggression is the most per-
vasive,reportedby between18-59% of homecare
workers [6,7,17]:with the highest estimate coming from
a study that ask about abuse over the homecare worker’s
career [7] and the lower estimates coming from studies
that ask aboutthe occurrencein the last 6-months
[6,17].Workplaceaggression,or threatening behavior
were reported by 7-16% [6,7] of homecare workers,with
the highest percentage coming from a study that asked
about the occurrence over the homecare workers career
[7],and lower percentage coming from a study that re-
ported aboutthe occurrence in the last6 months [6].
Workplace violence orphysicalassaults were reported
by between 2-11% ofhomecare workers [6,17,18],with
the larger percentage coming from a broader definition
of workplaceviolencethat included being threatened
with a knife [6],and the smallerpercentagescoming
Hanson et al.BMC Public Health (2015) 15:11 Page 2 of 13
from studies that included general questions about phys-
ical assaults only [17,18].
Research has shown that workplace violence and sex-
ual harassment and sexual aggression often co-occur [6].
A meta-analysiscovering 86,578 participantsfrom 55
separate probability samplesacross a variety ofindus-
tries found that 58% of women reportexperiencing
sexually harassing behaviors atwork [19].Nurses are
believed to have a higher exposure to sexual harassment
than many other occupations;studies have found that
between 16-76% ofnurses’reportexperiencing sexual
harassment over their careers [20-27].Studies of home-
care workershavefound thatapproximately30% of
homecareworkersreported beingsexuallyharassed
[6,28].While reports ofworkplace violence and sexual
harassmentare high,scientists believe thatthe actual
prevalence may be even highergiven underreporting
bias [29].
Impact on work and health outcomes
Homecareworkers’experienceof workplaceviolence
and sexualharassment can impact their health both dir-
ectly and indirectly.The most severe possible direct ef-
fect is homicide of the homecare worker [30],but more
common directeffectsare nonfatalinjuries[31-33].
While the most severe forms ofviolence occur less fre-
quently,even less-severe formsof workplace violence
and sexualharassmentare associated with a variety of
negativeoutcomesfor women’sphysicaland mental
health [34].The indirectpersonalimpactof workplace
violence on women’s health can be understood using the
Lazarus and Folkman’s transactionalstress and coping
theory [35].According to this perspective,experiences
of workplaceviolencecan overwhelm thehomecare
worker’s coping resources resulting in prolonged stress
[36,37]and leadingto poorer mentaland physical
health outcomes.Severalstudieshave documented
health effectsof workplaceviolenceon health out-
comes,including depersonalization[38]; depression
[18]; flashbacks,sleeplessness,poorer mentalhealth
[39];traumatic stress disorder [40];emotionalexhaus-
tion [38],and poorer physical health [38].Health effects
of workplace violence and harassment can last for years
after the incident(s) [41].
Research has confirmed links between workplace vio-
lence and stressorssuch as fear of future violence
[7,36,42-47],and has demonstrated that fear is a path-
way by which workplaceviolencecan affect health
[6,36].In addition,homecare workers do notneed to
experience workplace violence to reportnegative out-
comes,as studieshave shown thatfear or perceived
threat of workplaceviolenceis associated with in-
creased physicalsymptoms,anxiety,and poorer mental
health [48].Fear or perceived threat may be precipitated
by witnessing or hearing about the negative experience
of another homecare worker.Based on the transactional
stress and coping theory,confidence in preventing and
responding to workplace violence may be considered a
resource thatincreases homecare workers capacity to
cope with the stress and helps buffer the negative im-
pacts on their health.A study conducted in one private
homecare agency found that 93% ofhomecare workers
were more confidentafter participating in violence-
prevention training [49].However,they did not go fur-
ther to examine the impact of the increase in confidence
on health outcomes.
Purpose
This study examines sexualharassmentand workplace
violenceprevalencein a consumer-drivenhomecare
model,where the potentialoutcomesfor homecare
workers who experience harassment and/or violence are
not fully understood.We examined the prevalence of
different types ofworkplace violence and sexualharass-
ment as defined above,and the association of workplace
violence,sexualharassment,and fear of violence or har-
assmenton homecare worker’swork and health out-
comes.Prevalence estimatesare criticalto supporting
efforts of homecare workers and their advocates,such as
labor unions,to develop training programs and policies
to preventsexualharassmentand workplace violence.
We also examined workers’confidencein preventing
and responding to sexual harassment and workplace vio-
lence as a moderator ofthe relationship between these
experiences and negative work (e.g.burnout) and health
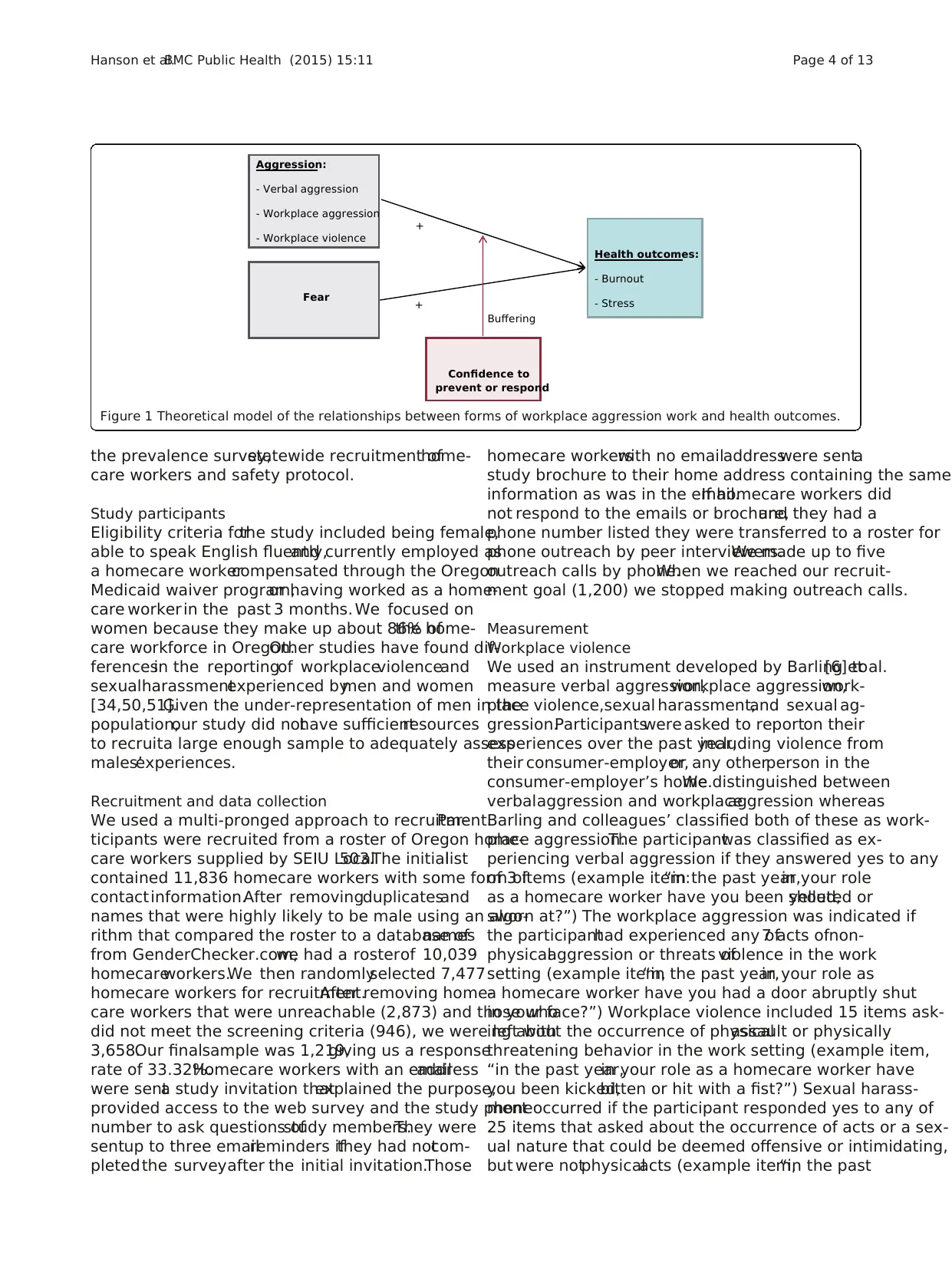
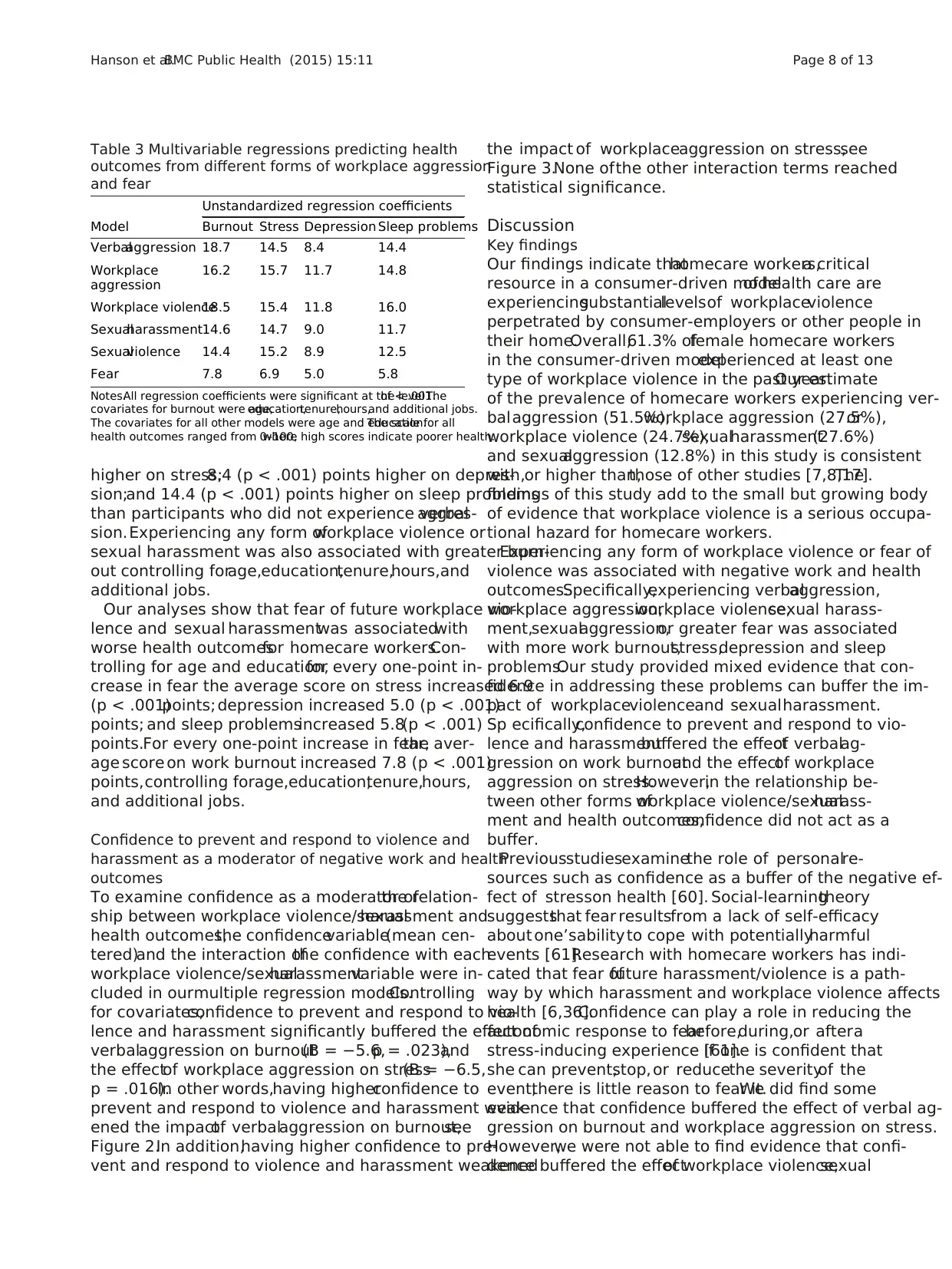
(e.g.depression)outcomes,see Figure 1.This informa-
tion is also importantto developing homecare worker
programs to reduce the negative outcomes often associ-
ated with experiencing harassment and violence.
Methods
We used a cross-sectionaldesign to explore the preva-
lence of workplace violence and sexual harassment expe-
rienced by homecareworkersin a consumer-driven
homecare modeland to understand how these experi-
ences related to homecare workers’work and health out-
comes.The study isin compliance with the Helsinki
Declaration and received oversight and approvalfor the
study from the IRBs at Johns Hopkins Medical Institutions
(#20685)and Oregon Health and Science University
(#4623).Our research was facilitated by a partnership
with the Oregon Homecare Commission (OHCC)and
with the Service Employees InternationalUnion (SEIU)
Local503,who also participated in our advisory board
along with members of the study team and representa-
tives for Oregon Department ofHuman Services DHS,
homecare workers,and consumer-employers.The ad-
visory board provided guidance on the development of
Hanson et al.BMC Public Health (2015) 15:11 Page 3 of 13
ical assaults only [17,18].
Research has shown that workplace violence and sex-
ual harassment and sexual aggression often co-occur [6].
A meta-analysiscovering 86,578 participantsfrom 55
separate probability samplesacross a variety ofindus-
tries found that 58% of women reportexperiencing
sexually harassing behaviors atwork [19].Nurses are
believed to have a higher exposure to sexual harassment
than many other occupations;studies have found that
between 16-76% ofnurses’reportexperiencing sexual
harassment over their careers [20-27].Studies of home-
care workershavefound thatapproximately30% of
homecareworkersreported beingsexuallyharassed
[6,28].While reports ofworkplace violence and sexual
harassmentare high,scientists believe thatthe actual
prevalence may be even highergiven underreporting
bias [29].
Impact on work and health outcomes
Homecareworkers’experienceof workplaceviolence
and sexualharassment can impact their health both dir-
ectly and indirectly.The most severe possible direct ef-
fect is homicide of the homecare worker [30],but more
common directeffectsare nonfatalinjuries[31-33].
While the most severe forms ofviolence occur less fre-
quently,even less-severe formsof workplace violence
and sexualharassmentare associated with a variety of
negativeoutcomesfor women’sphysicaland mental
health [34].The indirectpersonalimpactof workplace
violence on women’s health can be understood using the
Lazarus and Folkman’s transactionalstress and coping
theory [35].According to this perspective,experiences
of workplaceviolencecan overwhelm thehomecare
worker’s coping resources resulting in prolonged stress
[36,37]and leadingto poorer mentaland physical
health outcomes.Severalstudieshave documented
health effectsof workplaceviolenceon health out-
comes,including depersonalization[38]; depression
[18]; flashbacks,sleeplessness,poorer mentalhealth
[39];traumatic stress disorder [40];emotionalexhaus-
tion [38],and poorer physical health [38].Health effects
of workplace violence and harassment can last for years
after the incident(s) [41].
Research has confirmed links between workplace vio-
lence and stressorssuch as fear of future violence
[7,36,42-47],and has demonstrated that fear is a path-
way by which workplaceviolencecan affect health
[6,36].In addition,homecare workers do notneed to
experience workplace violence to reportnegative out-
comes,as studieshave shown thatfear or perceived
threat of workplaceviolenceis associated with in-
creased physicalsymptoms,anxiety,and poorer mental
health [48].Fear or perceived threat may be precipitated
by witnessing or hearing about the negative experience
of another homecare worker.Based on the transactional
stress and coping theory,confidence in preventing and
responding to workplace violence may be considered a
resource thatincreases homecare workers capacity to
cope with the stress and helps buffer the negative im-
pacts on their health.A study conducted in one private
homecare agency found that 93% ofhomecare workers
were more confidentafter participating in violence-
prevention training [49].However,they did not go fur-
ther to examine the impact of the increase in confidence
on health outcomes.
Purpose
This study examines sexualharassmentand workplace
violenceprevalencein a consumer-drivenhomecare
model,where the potentialoutcomesfor homecare
workers who experience harassment and/or violence are
not fully understood.We examined the prevalence of
different types ofworkplace violence and sexualharass-
ment as defined above,and the association of workplace
violence,sexualharassment,and fear of violence or har-
assmenton homecare worker’swork and health out-
comes.Prevalence estimatesare criticalto supporting
efforts of homecare workers and their advocates,such as
labor unions,to develop training programs and policies
to preventsexualharassmentand workplace violence.
We also examined workers’confidencein preventing
and responding to sexual harassment and workplace vio-
lence as a moderator ofthe relationship between these
experiences and negative work (e.g.burnout) and health
(e.g.depression)outcomes,see Figure 1.This informa-
tion is also importantto developing homecare worker
programs to reduce the negative outcomes often associ-
ated with experiencing harassment and violence.
Methods
We used a cross-sectionaldesign to explore the preva-
lence of workplace violence and sexual harassment expe-
rienced by homecareworkersin a consumer-driven
homecare modeland to understand how these experi-
ences related to homecare workers’work and health out-
comes.The study isin compliance with the Helsinki
Declaration and received oversight and approvalfor the
study from the IRBs at Johns Hopkins Medical Institutions
(#20685)and Oregon Health and Science University
(#4623).Our research was facilitated by a partnership
with the Oregon Homecare Commission (OHCC)and
with the Service Employees InternationalUnion (SEIU)
Local503,who also participated in our advisory board
along with members of the study team and representa-
tives for Oregon Department ofHuman Services DHS,
homecare workers,and consumer-employers.The ad-
visory board provided guidance on the development of
Hanson et al.BMC Public Health (2015) 15:11 Page 3 of 13
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
the prevalence survey,statewide recruitment ofhome-
care workers and safety protocol.
Study participants
Eligibility criteria forthe study included being female,
able to speak English fluently,and currently employed as
a homecare workercompensated through the Oregon
Medicaid waiver program,or having worked as a home-
care worker in the past 3 months. We focused on
women because they make up about 86% ofthe home-
care workforce in Oregon.Other studies have found dif-
ferencesin the reportingof workplaceviolenceand
sexualharassmentexperienced bymen and women
[34,50,51].Given the under-representation of men in the
population,our study did nothave sufficientresources
to recruita large enough sample to adequately assess
males’experiences.
Recruitment and data collection
We used a multi-pronged approach to recruitment.Par-
ticipants were recruited from a roster of Oregon home-
care workers supplied by SEIU Local503.The initiallist
contained 11,836 homecare workers with some form of
contactinformation.After removingduplicatesand
names that were highly likely to be male using an algo-
rithm that compared the roster to a database ofnames
from GenderChecker.com,we had a rosterof 10,039
homecareworkers.We then randomlyselected 7,477
homecare workers for recruitment.After removing home-
care workers that were unreachable (2,873) and those who
did not meet the screening criteria (946), we were left with
3,658.Our finalsample was 1,219,giving us a response
rate of 33.32%.Homecare workers with an emailaddress
were senta study invitation thatexplained the purpose,
provided access to the web survey and the study phone
number to ask questions ofstudy members.They were
sentup to three emailreminders ifthey had notcom-
pletedthe surveyafter the initial invitation.Those
homecare workerswith no emailaddresswere senta
study brochure to their home address containing the same
information as was in the email.If homecare workers did
not respond to the emails or brochure,and they had a
phone number listed they were transferred to a roster for
phone outreach by peer interviewers.We made up to five
outreach calls by phone.When we reached our recruit-
ment goal (1,200) we stopped making outreach calls.
Measurement
Workplace violence
We used an instrument developed by Barling et al.[6] to
measure verbal aggression,workplace aggression,work-
place violence,sexual harassment,and sexual ag-
gression.Participantswere asked to reporton their
experiences over the past year,including violence from
their consumer-employer,or any otherperson in the
consumer-employer’s home.We distinguished between
verbalaggression and workplaceaggression whereas
Barling and colleagues’ classified both of these as work-
place aggression.The participantwas classified as ex-
periencing verbal aggression if they answered yes to any
of 3 items (example item:“in the past year,in your role
as a homecare worker have you been yelled,shouted or
sworn at?”) The workplace aggression was indicated if
the participanthad experienced any of7 acts ofnon-
physicalaggression or threats ofviolence in the work
setting (example item,“in the past year,in your role as
a homecare worker have you had a door abruptly shut
in your face?”) Workplace violence included 15 items ask-
ing about the occurrence of physicalassault or physically
threatening behavior in the work setting (example item,
“in the past year,in your role as a homecare worker have
you been kicked,bitten or hit with a fist?”) Sexual harass-
ment occurred if the participant responded yes to any of
25 items that asked about the occurrence of acts or a sex-
ual nature that could be deemed offensive or intimidating,
but were notphysicalacts (example item,“in the past
Aggression:
- Verbal aggression
- Workplace aggression
- Workplace violence
Health outcomes:
- Burnout
- Stress
Fear
Confidence to
prevent or respond
+
+
Buffering
Figure 1 Theoretical model of the relationships between forms of workplace aggression work and health outcomes.
Hanson et al.BMC Public Health (2015) 15:11 Page 4 of 13
care workers and safety protocol.
Study participants
Eligibility criteria forthe study included being female,
able to speak English fluently,and currently employed as
a homecare workercompensated through the Oregon
Medicaid waiver program,or having worked as a home-
care worker in the past 3 months. We focused on
women because they make up about 86% ofthe home-
care workforce in Oregon.Other studies have found dif-
ferencesin the reportingof workplaceviolenceand
sexualharassmentexperienced bymen and women
[34,50,51].Given the under-representation of men in the
population,our study did nothave sufficientresources
to recruita large enough sample to adequately assess
males’experiences.
Recruitment and data collection
We used a multi-pronged approach to recruitment.Par-
ticipants were recruited from a roster of Oregon home-
care workers supplied by SEIU Local503.The initiallist
contained 11,836 homecare workers with some form of
contactinformation.After removingduplicatesand
names that were highly likely to be male using an algo-
rithm that compared the roster to a database ofnames
from GenderChecker.com,we had a rosterof 10,039
homecareworkers.We then randomlyselected 7,477
homecare workers for recruitment.After removing home-
care workers that were unreachable (2,873) and those who
did not meet the screening criteria (946), we were left with
3,658.Our finalsample was 1,219,giving us a response
rate of 33.32%.Homecare workers with an emailaddress
were senta study invitation thatexplained the purpose,
provided access to the web survey and the study phone
number to ask questions ofstudy members.They were
sentup to three emailreminders ifthey had notcom-
pletedthe surveyafter the initial invitation.Those
homecare workerswith no emailaddresswere senta
study brochure to their home address containing the same
information as was in the email.If homecare workers did
not respond to the emails or brochure,and they had a
phone number listed they were transferred to a roster for
phone outreach by peer interviewers.We made up to five
outreach calls by phone.When we reached our recruit-
ment goal (1,200) we stopped making outreach calls.
Measurement
Workplace violence
We used an instrument developed by Barling et al.[6] to
measure verbal aggression,workplace aggression,work-
place violence,sexual harassment,and sexual ag-
gression.Participantswere asked to reporton their
experiences over the past year,including violence from
their consumer-employer,or any otherperson in the
consumer-employer’s home.We distinguished between
verbalaggression and workplaceaggression whereas
Barling and colleagues’ classified both of these as work-
place aggression.The participantwas classified as ex-
periencing verbal aggression if they answered yes to any
of 3 items (example item:“in the past year,in your role
as a homecare worker have you been yelled,shouted or
sworn at?”) The workplace aggression was indicated if
the participanthad experienced any of7 acts ofnon-
physicalaggression or threats ofviolence in the work
setting (example item,“in the past year,in your role as
a homecare worker have you had a door abruptly shut
in your face?”) Workplace violence included 15 items ask-
ing about the occurrence of physicalassault or physically
threatening behavior in the work setting (example item,
“in the past year,in your role as a homecare worker have
you been kicked,bitten or hit with a fist?”) Sexual harass-
ment occurred if the participant responded yes to any of
25 items that asked about the occurrence of acts or a sex-
ual nature that could be deemed offensive or intimidating,
but were notphysicalacts (example item,“in the past
Aggression:
- Verbal aggression
- Workplace aggression
- Workplace violence
Health outcomes:
- Burnout
- Stress
Fear
Confidence to
prevent or respond
+
+
Buffering
Figure 1 Theoretical model of the relationships between forms of workplace aggression work and health outcomes.
Hanson et al.BMC Public Health (2015) 15:11 Page 4 of 13
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
year,in your role as a homecare worker have you had
sexually explicit material left in view?”).The participant
was classified as experiencing SexualAggression if they
indicated that any 11 acts ofa sexualnature involving
physicalcontact(example item,“in the pastyear,in
your role as a homecare worker have you been touched
in a sexual way?”) had occurred.
Fear
For the purpose ofthis study,fear is defined asthe
worry thatone will experience some form ofviolence
while working asa homecare workers.We measured
fear by adapting the scale used by Barling et al.[6].After
each section ofthe questions(e.g.,workplace aggres-
sion),participantswere asked to indicate theiragree-
ment or disagreement with the statement,“I worry that I
will experience workplace aggression while performing
my dutiesas a homecare worker.”A similar question
was asked after the sections on workplace violence,sex-
ual harassment,and sexual aggression.These items were
rated on a 5-point Likert-typescaleranging from 1
(strongly disagree) to 5 (strongly agree).We calculated a
totalscore as the mean of these 4 items.The validity of
the Barling etal. scale hasbeen established in other
studieswith homecareworkers[6,36].The internal
consistency,or Cronbach’s alpha,for these items was .90
in our sample.
Burnout
We used a subset ofeight items from the work-related
burnoutand client-related burnoutsubscalesof the
Copenhagan Burnout Inventory (CBI) developed for the
PUMA study [52].The validityof this measurewas
established in a large sample ofhuman service workers
[53].In our sample the two subscales used in the PUMA
study were highly correlated.An exploratory-factor
analysisindicated thattherewas a singlefactor,see
Additionalfile 1.As a result,we collapsed them into a
single work related burnout scale.Work related burnout
can be defined as “a state of prolonged physical and psy-
chologicalexhaustion,which is perceived as related to
the person’s work” [54].An example item is,“thinking
aboutthe last4 weeks,is your work as a homecare
worker emotionally exhausting?”The items were mea-
sured on a 5-pointscale.We obtained a totalscore by
taking the mean of the items and then rescaling so that
the final score would range from 0–100.The Cronbach’s
alpha for this scale was .9.
Stress,depression and sleep
We measured stress,depression,and sleep using the
COPSOQ II [55].Each subscale had fouritems.The
introduction asked participants to think about how often
in the past 4 weeks they had experienced each item due
to working as a homecare worker.The developers of the
COPSOQ II describe stress as a personal state character-
ized by both heightened arousaland displeasure.An ex-
ampleitems is, “how often haveyou had problems
relaxing?” The COPSOQ IImeasure ofdepression was
designed to measure the levelof depressive symptoms
experienced by workers rather than to diagnose clinical
depression.An example item is,“how often have you felt
sad?”The sleep subscale is meantto be a measure of
generalsleeping troubles in a working population.An
example item is,“how often have you found ithard to
go to sleep?” All items were asked on a scale of 1 (not at
all),2 (a small part of the time),3 (part of the time),4 (a
large part of the time) or 5 (all the time).We obtained a
totalscore by taking the mean of the items and then re-
scaling so that the finalscore would range from 0–100.
The validity ofthese sub-scales has been established by
in previousresearch [56].The Cronbach’salphasfor
these scales were:α = .9stess, α = .8depression, and α = .9sleep.
Confidence
We measured an individual’s confidence thatshe could
preventand respond to workplace violence and sexual
harassmentusing a 19-item scale developed specifically
for this study.We developed an initial list of items based
on focus groups conducted by the study team with 83
homecare workers [4].Then we sent these items to five
subject-matter experts and asked them to rate the items
from 0–2 on clarity,relevance,and usability.We retained
items with a high mean on all three rating scales. The final
rating scale for the items was 1 (not at all confident),2 (a
little confident),3 (confident),or 4 (very confident).See
Additionalfile 2 for finalscale.Cronbach’s alpha for this
scale was .9.
Covariates
Age was measured in number ofyears.Education was
coded as 1 (8th grade or less),2 (some high school),3
(high school diploma or GED),4 (some college),5 (asso-
ciate’s degree or vocationalgraduate),6 (4 year college
degree/bachelor’sdegree),or 7 (post-Baccalaureate/
Master’s degree/Ph.D).Tenure was coded as the num-
ber ofyears the participant has worked as a homecare
worker.Hours worked was coded as the average num-
ber of hours worked weeklyas a homecare worker.
Additionaljobs was coded as 0 (no additionaljobs out-
side of homecare)or 1 (one or more jobs outside of
homecare).
Statistical analyses
We conducted three sets ofanalyses to answer the fol-
lowing questions:1) what is the prevalence ofdifferent
forms of workplaceviolenceand sexualharassment
among female homecare workers;2) are experiences of
Hanson et al.BMC Public Health (2015) 15:11 Page 5 of 13
sexually explicit material left in view?”).The participant
was classified as experiencing SexualAggression if they
indicated that any 11 acts ofa sexualnature involving
physicalcontact(example item,“in the pastyear,in
your role as a homecare worker have you been touched
in a sexual way?”) had occurred.
Fear
For the purpose ofthis study,fear is defined asthe
worry thatone will experience some form ofviolence
while working asa homecare workers.We measured
fear by adapting the scale used by Barling et al.[6].After
each section ofthe questions(e.g.,workplace aggres-
sion),participantswere asked to indicate theiragree-
ment or disagreement with the statement,“I worry that I
will experience workplace aggression while performing
my dutiesas a homecare worker.”A similar question
was asked after the sections on workplace violence,sex-
ual harassment,and sexual aggression.These items were
rated on a 5-point Likert-typescaleranging from 1
(strongly disagree) to 5 (strongly agree).We calculated a
totalscore as the mean of these 4 items.The validity of
the Barling etal. scale hasbeen established in other
studieswith homecareworkers[6,36].The internal
consistency,or Cronbach’s alpha,for these items was .90
in our sample.
Burnout
We used a subset ofeight items from the work-related
burnoutand client-related burnoutsubscalesof the
Copenhagan Burnout Inventory (CBI) developed for the
PUMA study [52].The validityof this measurewas
established in a large sample ofhuman service workers
[53].In our sample the two subscales used in the PUMA
study were highly correlated.An exploratory-factor
analysisindicated thattherewas a singlefactor,see
Additionalfile 1.As a result,we collapsed them into a
single work related burnout scale.Work related burnout
can be defined as “a state of prolonged physical and psy-
chologicalexhaustion,which is perceived as related to
the person’s work” [54].An example item is,“thinking
aboutthe last4 weeks,is your work as a homecare
worker emotionally exhausting?”The items were mea-
sured on a 5-pointscale.We obtained a totalscore by
taking the mean of the items and then rescaling so that
the final score would range from 0–100.The Cronbach’s
alpha for this scale was .9.
Stress,depression and sleep
We measured stress,depression,and sleep using the
COPSOQ II [55].Each subscale had fouritems.The
introduction asked participants to think about how often
in the past 4 weeks they had experienced each item due
to working as a homecare worker.The developers of the
COPSOQ II describe stress as a personal state character-
ized by both heightened arousaland displeasure.An ex-
ampleitems is, “how often haveyou had problems
relaxing?” The COPSOQ IImeasure ofdepression was
designed to measure the levelof depressive symptoms
experienced by workers rather than to diagnose clinical
depression.An example item is,“how often have you felt
sad?”The sleep subscale is meantto be a measure of
generalsleeping troubles in a working population.An
example item is,“how often have you found ithard to
go to sleep?” All items were asked on a scale of 1 (not at
all),2 (a small part of the time),3 (part of the time),4 (a
large part of the time) or 5 (all the time).We obtained a
totalscore by taking the mean of the items and then re-
scaling so that the finalscore would range from 0–100.
The validity ofthese sub-scales has been established by
in previousresearch [56].The Cronbach’salphasfor
these scales were:α = .9stess, α = .8depression, and α = .9sleep.
Confidence
We measured an individual’s confidence thatshe could
preventand respond to workplace violence and sexual
harassmentusing a 19-item scale developed specifically
for this study.We developed an initial list of items based
on focus groups conducted by the study team with 83
homecare workers [4].Then we sent these items to five
subject-matter experts and asked them to rate the items
from 0–2 on clarity,relevance,and usability.We retained
items with a high mean on all three rating scales. The final
rating scale for the items was 1 (not at all confident),2 (a
little confident),3 (confident),or 4 (very confident).See
Additionalfile 2 for finalscale.Cronbach’s alpha for this
scale was .9.
Covariates
Age was measured in number ofyears.Education was
coded as 1 (8th grade or less),2 (some high school),3
(high school diploma or GED),4 (some college),5 (asso-
ciate’s degree or vocationalgraduate),6 (4 year college
degree/bachelor’sdegree),or 7 (post-Baccalaureate/
Master’s degree/Ph.D).Tenure was coded as the num-
ber ofyears the participant has worked as a homecare
worker.Hours worked was coded as the average num-
ber of hours worked weeklyas a homecare worker.
Additionaljobs was coded as 0 (no additionaljobs out-
side of homecare)or 1 (one or more jobs outside of
homecare).
Statistical analyses
We conducted three sets ofanalyses to answer the fol-
lowing questions:1) what is the prevalence ofdifferent
forms of workplaceviolenceand sexualharassment
among female homecare workers;2) are experiences of
Hanson et al.BMC Public Health (2015) 15:11 Page 5 of 13
workplace violence and fearrelated to negative work
and health outcomes;and,3) are these effects moder-
ated by confidence in preventing and responding to
workplace violence.We computed prevalence asthe
percentof respondentsexperiencing each item,and
overallscores as the percentof respondents experien-
cing one or more items for each ofthe violence cate-
gories (i.e., verbalaggression,workplaceaggression,
workplace violence,sexualharassment,sexualaggres-
sion, and fear).Homecare workers providing services
for their spouseswere excludedfrom the sexual-
harassment analyses.Scores for scales with more than 3
items were computed using mean replacement from the
participant’s answered items if at least 75% of the ques-
tions were answered.
We used separate multiple regression analyses to re-
gress each violence scale on each health outcome (stress,
depression,and sleep) controlling for covariates.Poorer
health outcomes are associated with increased age and
lowersocioeconomic [57,58],for this reason,age and
education were included in allof the regression analyses
to partial out any confounding effects.Burnout is known
to be associated with work-related demographics[59].
Therefore,potentialwork related confounders including
tenure,number ofhours worked,and having additional
jobs,were also included in the model when burnout was
the outcome.
Results
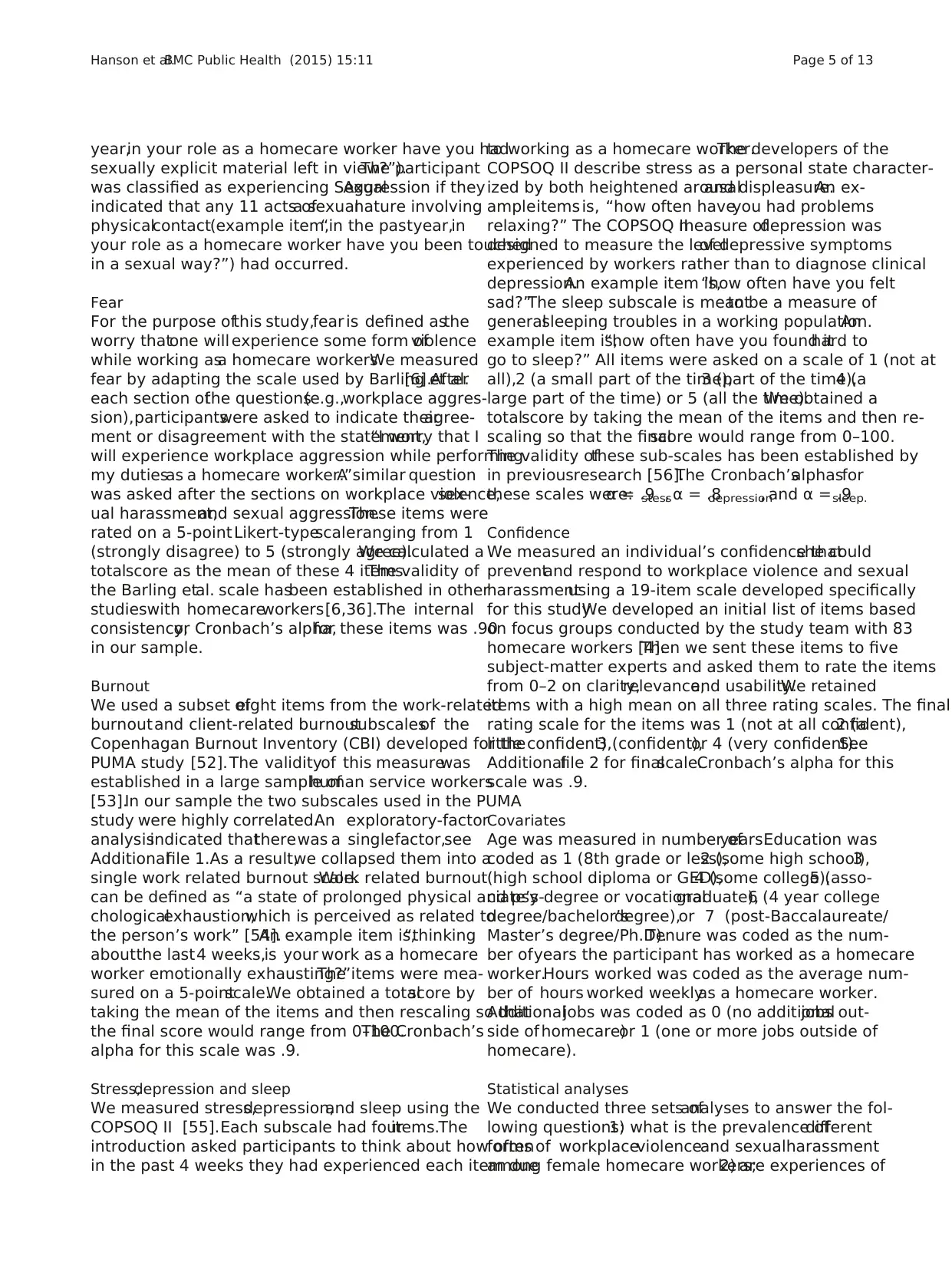
Table 1 shows demographic and work characteristics of
the 1,214 homecare workers who completed the survey.
Participants ranged in age from 19 to 80,with a mean
age of 47.30(SD = 13.8).The majorityof homecare
workers were White (85.4%),with 6.7% self-reported as
Hispanic or Latina. Almost all of the participants
(93.1%)had a high schooldiploma or GED,and 25.1%
had a college or vocationaldegree.Participants reported
having worked,on average,7. 9 (SD = 7.3)yearsas a
homecare worker.Twenty-one percentof participants
lived with their consumer-employer.The average num-
ber of hours worked perweek was33.5 (SD = 27.6).
Thirty-one participants worked for more than one con-
sumer/employer,with the average working for between
1–2 consumer-employers(M = 1.5,SD = .8).The over-
whelming majority ofhomecare workers provided ser-
vices for someone other than their spouse atleastpart
of the time (97.9%).
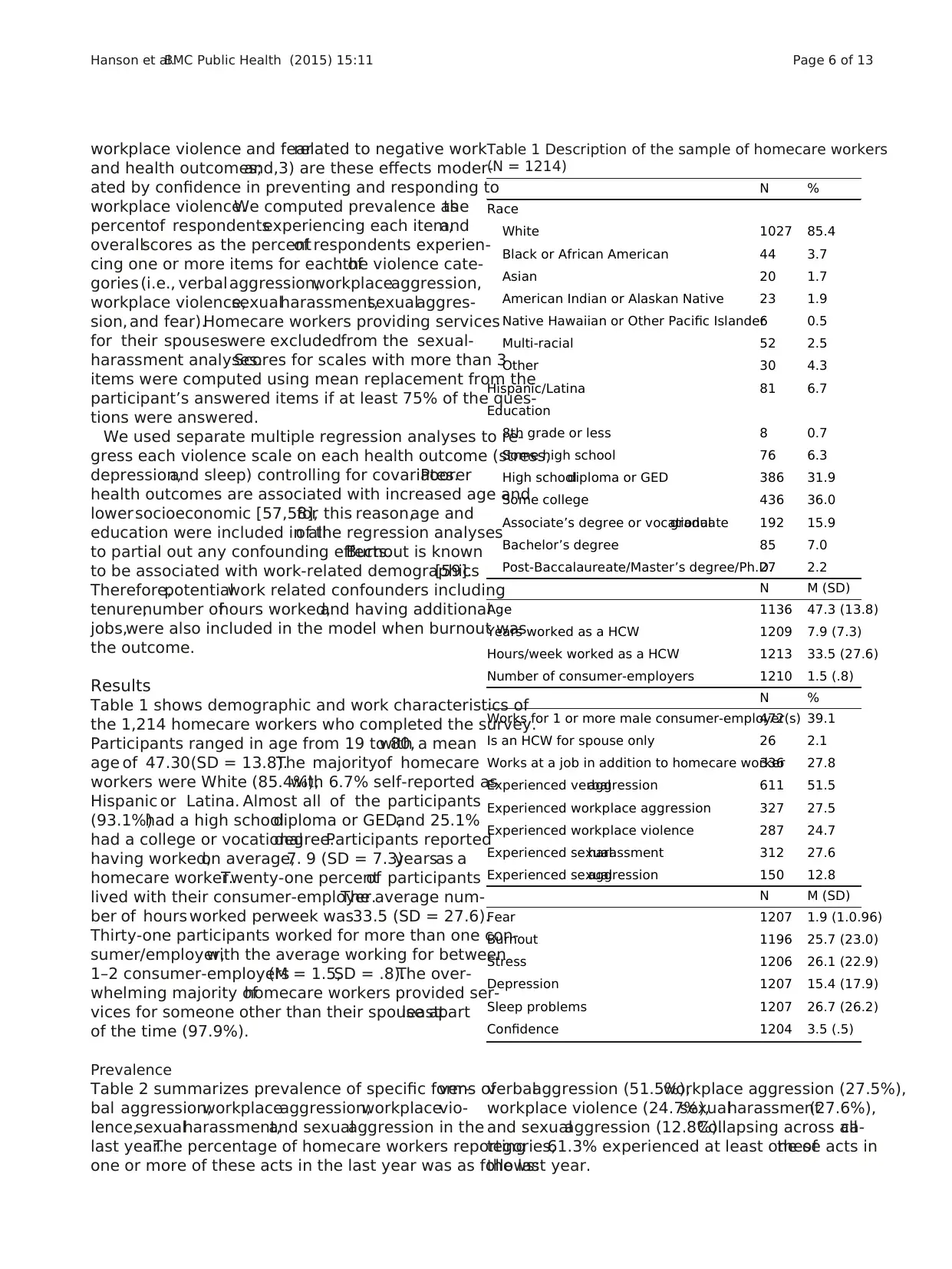
Prevalence
Table 2 summarizes prevalence of specific forms ofver-
bal aggression,workplaceaggression,workplacevio-
lence,sexualharassment,and sexualaggression in the
last year.The percentage of homecare workers reporting
one or more of these acts in the last year was as follows:
verbalaggression (51.5%),workplace aggression (27.5%),
workplace violence (24.7%),sexualharassment(27.6%),
and sexualaggression (12.8%).Collapsing across allca-
tegories,61.3% experienced at least one ofthese acts in
the last year.
Table 1 Description of the sample of homecare workers
(N = 1214)
N %
Race
White 1027 85.4
Black or African American 44 3.7
Asian 20 1.7
American Indian or Alaskan Native 23 1.9
Native Hawaiian or Other Pacific Islander6 0.5
Multi-racial 52 2.5
Other 30 4.3
Hispanic/Latina 81 6.7
Education
8th grade or less 8 0.7
Some high school 76 6.3
High schooldiploma or GED 386 31.9
Some college 436 36.0
Associate’s degree or vocationalgraduate 192 15.9
Bachelor’s degree 85 7.0
Post-Baccalaureate/Master’s degree/Ph.D.27 2.2
N M (SD)
Age 1136 47.3 (13.8)
Years worked as a HCW 1209 7.9 (7.3)
Hours/week worked as a HCW 1213 33.5 (27.6)
Number of consumer-employers 1210 1.5 (.8)
N %
Works for 1 or more male consumer-employer(s)472 39.1
Is an HCW for spouse only 26 2.1
Works at a job in addition to homecare worker336 27.8
Experienced verbalaggression 611 51.5
Experienced workplace aggression 327 27.5
Experienced workplace violence 287 24.7
Experienced sexualharassment 312 27.6
Experienced sexualaggression 150 12.8
N M (SD)
Fear 1207 1.9 (1.0.96)
Burnout 1196 25.7 (23.0)
Stress 1206 26.1 (22.9)
Depression 1207 15.4 (17.9)
Sleep problems 1207 26.7 (26.2)
Confidence 1204 3.5 (.5)
Hanson et al.BMC Public Health (2015) 15:11 Page 6 of 13
and health outcomes;and,3) are these effects moder-
ated by confidence in preventing and responding to
workplace violence.We computed prevalence asthe
percentof respondentsexperiencing each item,and
overallscores as the percentof respondents experien-
cing one or more items for each ofthe violence cate-
gories (i.e., verbalaggression,workplaceaggression,
workplace violence,sexualharassment,sexualaggres-
sion, and fear).Homecare workers providing services
for their spouseswere excludedfrom the sexual-
harassment analyses.Scores for scales with more than 3
items were computed using mean replacement from the
participant’s answered items if at least 75% of the ques-
tions were answered.
We used separate multiple regression analyses to re-
gress each violence scale on each health outcome (stress,
depression,and sleep) controlling for covariates.Poorer
health outcomes are associated with increased age and
lowersocioeconomic [57,58],for this reason,age and
education were included in allof the regression analyses
to partial out any confounding effects.Burnout is known
to be associated with work-related demographics[59].
Therefore,potentialwork related confounders including
tenure,number ofhours worked,and having additional
jobs,were also included in the model when burnout was
the outcome.
Results
Table 1 shows demographic and work characteristics of
the 1,214 homecare workers who completed the survey.
Participants ranged in age from 19 to 80,with a mean
age of 47.30(SD = 13.8).The majorityof homecare
workers were White (85.4%),with 6.7% self-reported as
Hispanic or Latina. Almost all of the participants
(93.1%)had a high schooldiploma or GED,and 25.1%
had a college or vocationaldegree.Participants reported
having worked,on average,7. 9 (SD = 7.3)yearsas a
homecare worker.Twenty-one percentof participants
lived with their consumer-employer.The average num-
ber of hours worked perweek was33.5 (SD = 27.6).
Thirty-one participants worked for more than one con-
sumer/employer,with the average working for between
1–2 consumer-employers(M = 1.5,SD = .8).The over-
whelming majority ofhomecare workers provided ser-
vices for someone other than their spouse atleastpart
of the time (97.9%).
Prevalence
Table 2 summarizes prevalence of specific forms ofver-
bal aggression,workplaceaggression,workplacevio-
lence,sexualharassment,and sexualaggression in the
last year.The percentage of homecare workers reporting
one or more of these acts in the last year was as follows:
verbalaggression (51.5%),workplace aggression (27.5%),
workplace violence (24.7%),sexualharassment(27.6%),
and sexualaggression (12.8%).Collapsing across allca-
tegories,61.3% experienced at least one ofthese acts in
the last year.
Table 1 Description of the sample of homecare workers
(N = 1214)
N %
Race
White 1027 85.4
Black or African American 44 3.7
Asian 20 1.7
American Indian or Alaskan Native 23 1.9
Native Hawaiian or Other Pacific Islander6 0.5
Multi-racial 52 2.5
Other 30 4.3
Hispanic/Latina 81 6.7
Education
8th grade or less 8 0.7
Some high school 76 6.3
High schooldiploma or GED 386 31.9
Some college 436 36.0
Associate’s degree or vocationalgraduate 192 15.9
Bachelor’s degree 85 7.0
Post-Baccalaureate/Master’s degree/Ph.D.27 2.2
N M (SD)
Age 1136 47.3 (13.8)
Years worked as a HCW 1209 7.9 (7.3)
Hours/week worked as a HCW 1213 33.5 (27.6)
Number of consumer-employers 1210 1.5 (.8)
N %
Works for 1 or more male consumer-employer(s)472 39.1
Is an HCW for spouse only 26 2.1
Works at a job in addition to homecare worker336 27.8
Experienced verbalaggression 611 51.5
Experienced workplace aggression 327 27.5
Experienced workplace violence 287 24.7
Experienced sexualharassment 312 27.6
Experienced sexualaggression 150 12.8
N M (SD)
Fear 1207 1.9 (1.0.96)
Burnout 1196 25.7 (23.0)
Stress 1206 26.1 (22.9)
Depression 1207 15.4 (17.9)
Sleep problems 1207 26.7 (26.2)
Confidence 1204 3.5 (.5)
Hanson et al.BMC Public Health (2015) 15:11 Page 6 of 13
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
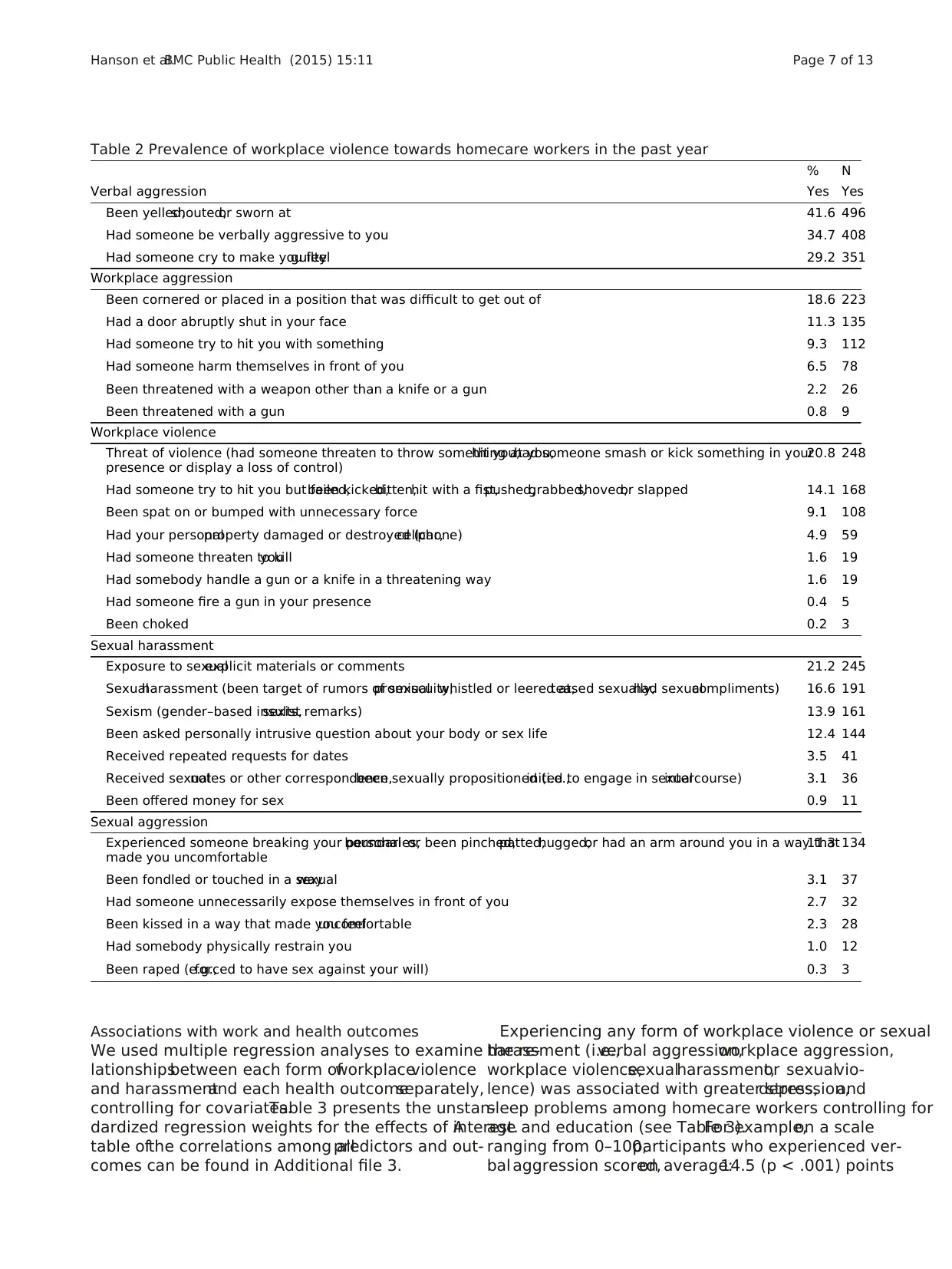
Associations with work and health outcomes
We used multiple regression analyses to examine the re-
lationshipsbetween each form ofworkplaceviolence
and harassmentand each health outcomeseparately,
controlling for covariates.Table 3 presents the unstan-
dardized regression weights for the effects of interest.A
table ofthe correlations among allpredictors and out-
comes can be found in Additional file 3.
Experiencing any form of workplace violence or sexual
harassment (i.e.,verbal aggression,workplace aggression,
workplace violence,sexualharassment,or sexualvio-
lence) was associated with greater stress,depression,and
sleep problems among homecare workers controlling for
age and education (see Table 3).For example,on a scale
ranging from 0–100,participants who experienced ver-
bal aggression scored,on average:14.5 (p < .001) points
Table 2 Prevalence of workplace violence towards homecare workers in the past year
% N
Verbal aggression Yes Yes
Been yelled,shouted,or sworn at 41.6 496
Had someone be verbally aggressive to you 34.7 408
Had someone cry to make you feelguilty 29.2 351
Workplace aggression
Been cornered or placed in a position that was difficult to get out of 18.6 223
Had a door abruptly shut in your face 11.3 135
Had someone try to hit you with something 9.3 112
Had someone harm themselves in front of you 6.5 78
Been threatened with a weapon other than a knife or a gun 2.2 26
Been threatened with a gun 0.8 9
Workplace violence
Threat of violence (had someone threaten to throw something at you,hit you,had someone smash or kick something in your
presence or display a loss of control)
20.8 248
Had someone try to hit you but failed,been kicked,bitten,hit with a fist,pushed,grabbed,shoved,or slapped 14.1 168
Been spat on or bumped with unnecessary force 9.1 108
Had your personalproperty damaged or destroyed (car,cellphone) 4.9 59
Had someone threaten to killyou 1.6 19
Had somebody handle a gun or a knife in a threatening way 1.6 19
Had someone fire a gun in your presence 0.4 5
Been choked 0.2 3
Sexual harassment
Exposure to sexualexplicit materials or comments 21.2 245
Sexualharassment (been target of rumors of sexualpromiscuity,whistled or leered at,teased sexually,had sexualcompliments) 16.6 191
Sexism (gender–based insults,sexist remarks) 13.9 161
Been asked personally intrusive question about your body or sex life 12.4 144
Received repeated requests for dates 3.5 41
Received sexualnotes or other correspondence,been sexually propositioned (i.e.,inited to engage in sexualintercourse) 3.1 36
Been offered money for sex 0.9 11
Sexual aggression
Experienced someone breaking your personalboundaries,or been pinched,patted,hugged,or had an arm around you in a way that
made you uncomfortable
11.3 134
Been fondled or touched in a sexualway 3.1 37
Had someone unnecessarily expose themselves in front of you 2.7 32
Been kissed in a way that made you feeluncomfortable 2.3 28
Had somebody physically restrain you 1.0 12
Been raped (e.g.,forced to have sex against your will) 0.3 3
Hanson et al.BMC Public Health (2015) 15:11 Page 7 of 13
We used multiple regression analyses to examine the re-
lationshipsbetween each form ofworkplaceviolence
and harassmentand each health outcomeseparately,
controlling for covariates.Table 3 presents the unstan-
dardized regression weights for the effects of interest.A
table ofthe correlations among allpredictors and out-
comes can be found in Additional file 3.
Experiencing any form of workplace violence or sexual
harassment (i.e.,verbal aggression,workplace aggression,
workplace violence,sexualharassment,or sexualvio-
lence) was associated with greater stress,depression,and
sleep problems among homecare workers controlling for
age and education (see Table 3).For example,on a scale
ranging from 0–100,participants who experienced ver-
bal aggression scored,on average:14.5 (p < .001) points
Table 2 Prevalence of workplace violence towards homecare workers in the past year
% N
Verbal aggression Yes Yes
Been yelled,shouted,or sworn at 41.6 496
Had someone be verbally aggressive to you 34.7 408
Had someone cry to make you feelguilty 29.2 351
Workplace aggression
Been cornered or placed in a position that was difficult to get out of 18.6 223
Had a door abruptly shut in your face 11.3 135
Had someone try to hit you with something 9.3 112
Had someone harm themselves in front of you 6.5 78
Been threatened with a weapon other than a knife or a gun 2.2 26
Been threatened with a gun 0.8 9
Workplace violence
Threat of violence (had someone threaten to throw something at you,hit you,had someone smash or kick something in your
presence or display a loss of control)
20.8 248
Had someone try to hit you but failed,been kicked,bitten,hit with a fist,pushed,grabbed,shoved,or slapped 14.1 168
Been spat on or bumped with unnecessary force 9.1 108
Had your personalproperty damaged or destroyed (car,cellphone) 4.9 59
Had someone threaten to killyou 1.6 19
Had somebody handle a gun or a knife in a threatening way 1.6 19
Had someone fire a gun in your presence 0.4 5
Been choked 0.2 3
Sexual harassment
Exposure to sexualexplicit materials or comments 21.2 245
Sexualharassment (been target of rumors of sexualpromiscuity,whistled or leered at,teased sexually,had sexualcompliments) 16.6 191
Sexism (gender–based insults,sexist remarks) 13.9 161
Been asked personally intrusive question about your body or sex life 12.4 144
Received repeated requests for dates 3.5 41
Received sexualnotes or other correspondence,been sexually propositioned (i.e.,inited to engage in sexualintercourse) 3.1 36
Been offered money for sex 0.9 11
Sexual aggression
Experienced someone breaking your personalboundaries,or been pinched,patted,hugged,or had an arm around you in a way that
made you uncomfortable
11.3 134
Been fondled or touched in a sexualway 3.1 37
Had someone unnecessarily expose themselves in front of you 2.7 32
Been kissed in a way that made you feeluncomfortable 2.3 28
Had somebody physically restrain you 1.0 12
Been raped (e.g.,forced to have sex against your will) 0.3 3
Hanson et al.BMC Public Health (2015) 15:11 Page 7 of 13
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
higher on stress;8.4 (p < .001) points higher on depres-
sion;and 14.4 (p < .001) points higher on sleep problems
than participants who did not experience verbalaggres-
sion.Experiencing any form ofworkplace violence or
sexual harassment was also associated with greater burn-
out controlling forage,education,tenure,hours,and
additional jobs.
Our analyses show that fear of future workplace vio-
lence and sexual harassmentwas associatedwith
worse health outcomesfor homecare workers.Con-
trolling for age and education,for every one-point in-
crease in fear the average score on stress increased 6.9
(p < .001)points; depression increased 5.0 (p < .001)
points; and sleep problemsincreased 5.8(p < .001)
points.For every one-point increase in fear,the aver-
age score on work burnout increased 7.8 (p < .001)
points,controlling forage,education,tenure,hours,
and additional jobs.
Confidence to prevent and respond to violence and
harassment as a moderator of negative work and health
outcomes
To examine confidence as a moderator ofthe relation-
ship between workplace violence/sexualharassment and
health outcomes,the confidencevariable(mean cen-
tered)and the interaction ofthe confidence with each
workplace violence/sexualharassmentvariable were in-
cluded in ourmultiple regression models.Controlling
for covariates,confidence to prevent and respond to vio-
lence and harassment significantly buffered the effect of
verbalaggression on burnout(B = −5.6,p = .023),and
the effectof workplace aggression on stress(B = −6.5,
p = .016).In other words,having higherconfidence to
prevent and respond to violence and harassment weak-
ened the impactof verbalaggression on burnout,see
Figure 2.In addition,having higher confidence to pre-
vent and respond to violence and harassment weakened
the impact of workplaceaggression on stress,see
Figure 3.None ofthe other interaction terms reached
statistical significance.
Discussion
Key findings
Our findings indicate thathomecare workers,a critical
resource in a consumer-driven modelof health care are
experiencingsubstantiallevelsof workplaceviolence
perpetrated by consumer-employers or other people in
their home.Overall,61.3% offemale homecare workers
in the consumer-driven modelexperienced at least one
type of workplace violence in the past year.Our estimate
of the prevalence of homecare workers experiencing ver-
balaggression (51.5%),workplace aggression (27.5%),or
workplace violence (24.7%),sexualharassment(27.6%)
and sexualaggression (12.8%) in this study is consistent
with,or higher than,those of other studies [7,8,17].The
findings of this study add to the small but growing body
of evidence that workplace violence is a serious occupa-
tional hazard for homecare workers.
Experiencing any form of workplace violence or fear of
violence was associated with negative work and health
outcomes.Specifically,experiencing verbalaggression,
workplace aggression,workplace violence,sexual harass-
ment,sexualaggression,or greater fear was associated
with more work burnout,stress,depression and sleep
problems.Our study provided mixed evidence that con-
fidence in addressing these problems can buffer the im-
pact of workplaceviolenceand sexualharassment.
Sp ecifically,confidence to prevent and respond to vio-
lence and harassmentbuffered the effectof verbalag-
gression on work burnoutand the effectof workplace
aggression on stress.However,in the relationship be-
tween other forms ofworkplace violence/sexualharass-
ment and health outcomes,confidence did not act as a
buffer.
Previousstudiesexaminethe role of personalre-
sources such as confidence as a buffer of the negative ef-
fect of stresson health [60]. Social-learningtheory
suggeststhat fear resultsfrom a lack of self-efficacy
about one’sability to cope with potentiallyharmful
events [61].Research with homecare workers has indi-
cated that fear offuture harassment/violence is a path-
way by which harassment and workplace violence affects
health [6,36].Confidence can play a role in reducing the
autonomic response to fearbefore,during,or aftera
stress-inducing experience [61].If one is confident that
she can prevent,stop, or reducethe severityof the
event,there is little reason to fear it.We did find some
evidence that confidence buffered the effect of verbal ag-
gression on burnout and workplace aggression on stress.
However,we were not able to find evidence that confi-
dence buffered the effectof workplace violence,sexual
Table 3 Multivariable regressions predicting health
outcomes from different forms of workplace aggression
and fear
Unstandardized regression coefficients
Model Burnout Stress Depression Sleep problems
Verbalaggression 18.7 14.5 8.4 14.4
Workplace
aggression
16.2 15.7 11.7 14.8
Workplace violence18.5 15.4 11.8 16.0
Sexualharassment14.6 14.7 9.0 11.7
Sexualviolence 14.4 15.2 8.9 12.5
Fear 7.8 6.9 5.0 5.8
Notes.All regression coefficients were significant at the levelof < .001.The
covariates for burnout were age,education,tenure,hours,and additional jobs.
The covariates for all other models were age and education.The scale for all
health outcomes ranged from 0–100,where high scores indicate poorer health.
Hanson et al.BMC Public Health (2015) 15:11 Page 8 of 13
sion;and 14.4 (p < .001) points higher on sleep problems
than participants who did not experience verbalaggres-
sion.Experiencing any form ofworkplace violence or
sexual harassment was also associated with greater burn-
out controlling forage,education,tenure,hours,and
additional jobs.
Our analyses show that fear of future workplace vio-
lence and sexual harassmentwas associatedwith
worse health outcomesfor homecare workers.Con-
trolling for age and education,for every one-point in-
crease in fear the average score on stress increased 6.9
(p < .001)points; depression increased 5.0 (p < .001)
points; and sleep problemsincreased 5.8(p < .001)
points.For every one-point increase in fear,the aver-
age score on work burnout increased 7.8 (p < .001)
points,controlling forage,education,tenure,hours,
and additional jobs.
Confidence to prevent and respond to violence and
harassment as a moderator of negative work and health
outcomes
To examine confidence as a moderator ofthe relation-
ship between workplace violence/sexualharassment and
health outcomes,the confidencevariable(mean cen-
tered)and the interaction ofthe confidence with each
workplace violence/sexualharassmentvariable were in-
cluded in ourmultiple regression models.Controlling
for covariates,confidence to prevent and respond to vio-
lence and harassment significantly buffered the effect of
verbalaggression on burnout(B = −5.6,p = .023),and
the effectof workplace aggression on stress(B = −6.5,
p = .016).In other words,having higherconfidence to
prevent and respond to violence and harassment weak-
ened the impactof verbalaggression on burnout,see
Figure 2.In addition,having higher confidence to pre-
vent and respond to violence and harassment weakened
the impact of workplaceaggression on stress,see
Figure 3.None ofthe other interaction terms reached
statistical significance.
Discussion
Key findings
Our findings indicate thathomecare workers,a critical
resource in a consumer-driven modelof health care are
experiencingsubstantiallevelsof workplaceviolence
perpetrated by consumer-employers or other people in
their home.Overall,61.3% offemale homecare workers
in the consumer-driven modelexperienced at least one
type of workplace violence in the past year.Our estimate
of the prevalence of homecare workers experiencing ver-
balaggression (51.5%),workplace aggression (27.5%),or
workplace violence (24.7%),sexualharassment(27.6%)
and sexualaggression (12.8%) in this study is consistent
with,or higher than,those of other studies [7,8,17].The
findings of this study add to the small but growing body
of evidence that workplace violence is a serious occupa-
tional hazard for homecare workers.
Experiencing any form of workplace violence or fear of
violence was associated with negative work and health
outcomes.Specifically,experiencing verbalaggression,
workplace aggression,workplace violence,sexual harass-
ment,sexualaggression,or greater fear was associated
with more work burnout,stress,depression and sleep
problems.Our study provided mixed evidence that con-
fidence in addressing these problems can buffer the im-
pact of workplaceviolenceand sexualharassment.
Sp ecifically,confidence to prevent and respond to vio-
lence and harassmentbuffered the effectof verbalag-
gression on work burnoutand the effectof workplace
aggression on stress.However,in the relationship be-
tween other forms ofworkplace violence/sexualharass-
ment and health outcomes,confidence did not act as a
buffer.
Previousstudiesexaminethe role of personalre-
sources such as confidence as a buffer of the negative ef-
fect of stresson health [60]. Social-learningtheory
suggeststhat fear resultsfrom a lack of self-efficacy
about one’sability to cope with potentiallyharmful
events [61].Research with homecare workers has indi-
cated that fear offuture harassment/violence is a path-
way by which harassment and workplace violence affects
health [6,36].Confidence can play a role in reducing the
autonomic response to fearbefore,during,or aftera
stress-inducing experience [61].If one is confident that
she can prevent,stop, or reducethe severityof the
event,there is little reason to fear it.We did find some
evidence that confidence buffered the effect of verbal ag-
gression on burnout and workplace aggression on stress.
However,we were not able to find evidence that confi-
dence buffered the effectof workplace violence,sexual
Table 3 Multivariable regressions predicting health
outcomes from different forms of workplace aggression
and fear
Unstandardized regression coefficients
Model Burnout Stress Depression Sleep problems
Verbalaggression 18.7 14.5 8.4 14.4
Workplace
aggression
16.2 15.7 11.7 14.8
Workplace violence18.5 15.4 11.8 16.0
Sexualharassment14.6 14.7 9.0 11.7
Sexualviolence 14.4 15.2 8.9 12.5
Fear 7.8 6.9 5.0 5.8
Notes.All regression coefficients were significant at the levelof < .001.The
covariates for burnout were age,education,tenure,hours,and additional jobs.
The covariates for all other models were age and education.The scale for all
health outcomes ranged from 0–100,where high scores indicate poorer health.
Hanson et al.BMC Public Health (2015) 15:11 Page 8 of 13
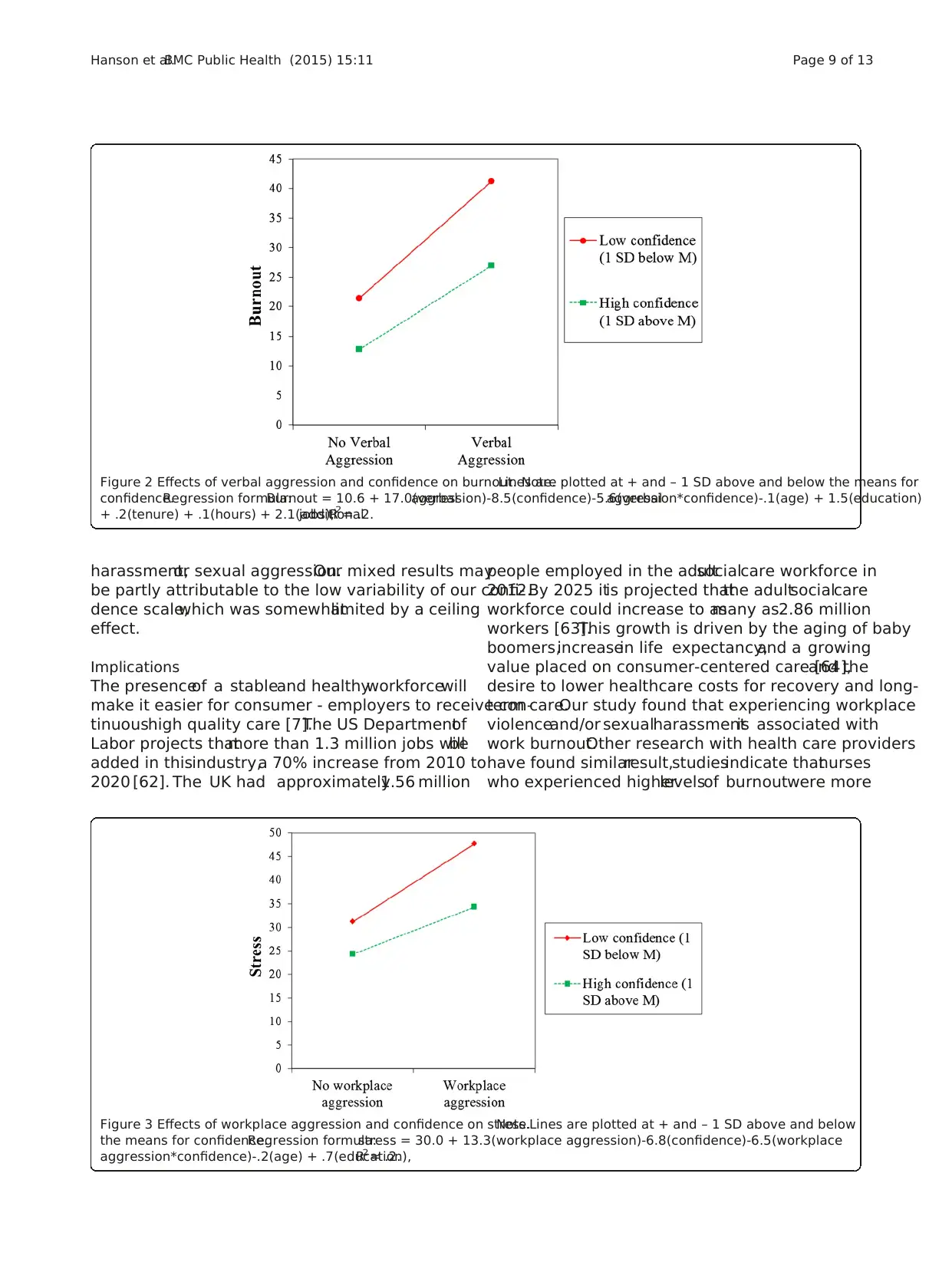
harassment,or sexual aggression.Our mixed results may
be partly attributable to the low variability of our confi-
dence scale,which was somewhatlimited by a ceiling
effect.
Implications
The presenceof a stableand healthyworkforcewill
make it easier for consumer - employers to receive con-
tinuoushigh quality care [7].The US Departmentof
Labor projects thatmore than 1.3 million jobs willbe
added in thisindustry,a 70% increase from 2010 to
2020 [62]. The UK had approximately1.56 million
people employed in the adultsocialcare workforce in
2012.By 2025 itis projected thatthe adultsocialcare
workforce could increase to asmany as2.86 million
workers [63].This growth is driven by the aging of baby
boomers,increasein life expectancy,and a growing
value placed on consumer-centered care [64],and the
desire to lower healthcare costs for recovery and long-
term care.Our study found that experiencing workplace
violenceand/or sexualharassmentis associated with
work burnout.Other research with health care providers
have found similarresult,studiesindicate thatnurses
who experienced higherlevelsof burnoutwere more
Figure 3 Effects of workplace aggression and confidence on stress.Note.Lines are plotted at + and – 1 SD above and below
the means for confidence.Regression formula:stress = 30.0 + 13.3(workplace aggression)-6.8(confidence)-6.5(workplace
aggression*confidence)-.2(age) + .7(education),R2 = .2.
Figure 2 Effects of verbal aggression and confidence on burnout. Note.Lines are plotted at + and – 1 SD above and below the means for
confidence.Regression formula:Burnout = 10.6 + 17.0(verbalaggression)-8.5(confidence)-5.6(verbalaggression*confidence)-.1(age) + 1.5(education)
+ .2(tenure) + .1(hours) + 2.1(additionaljobs),R2 = .2.
Hanson et al.BMC Public Health (2015) 15:11 Page 9 of 13
be partly attributable to the low variability of our confi-
dence scale,which was somewhatlimited by a ceiling
effect.
Implications
The presenceof a stableand healthyworkforcewill
make it easier for consumer - employers to receive con-
tinuoushigh quality care [7].The US Departmentof
Labor projects thatmore than 1.3 million jobs willbe
added in thisindustry,a 70% increase from 2010 to
2020 [62]. The UK had approximately1.56 million
people employed in the adultsocialcare workforce in
2012.By 2025 itis projected thatthe adultsocialcare
workforce could increase to asmany as2.86 million
workers [63].This growth is driven by the aging of baby
boomers,increasein life expectancy,and a growing
value placed on consumer-centered care [64],and the
desire to lower healthcare costs for recovery and long-
term care.Our study found that experiencing workplace
violenceand/or sexualharassmentis associated with
work burnout.Other research with health care providers
have found similarresult,studiesindicate thatnurses
who experienced higherlevelsof burnoutwere more
Figure 3 Effects of workplace aggression and confidence on stress.Note.Lines are plotted at + and – 1 SD above and below
the means for confidence.Regression formula:stress = 30.0 + 13.3(workplace aggression)-6.8(confidence)-6.5(workplace
aggression*confidence)-.2(age) + .7(education),R2 = .2.
Figure 2 Effects of verbal aggression and confidence on burnout. Note.Lines are plotted at + and – 1 SD above and below the means for
confidence.Regression formula:Burnout = 10.6 + 17.0(verbalaggression)-8.5(confidence)-5.6(verbalaggression*confidence)-.1(age) + 1.5(education)
+ .2(tenure) + .1(hours) + 2.1(additionaljobs),R2 = .2.
Hanson et al.BMC Public Health (2015) 15:11 Page 9 of 13
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
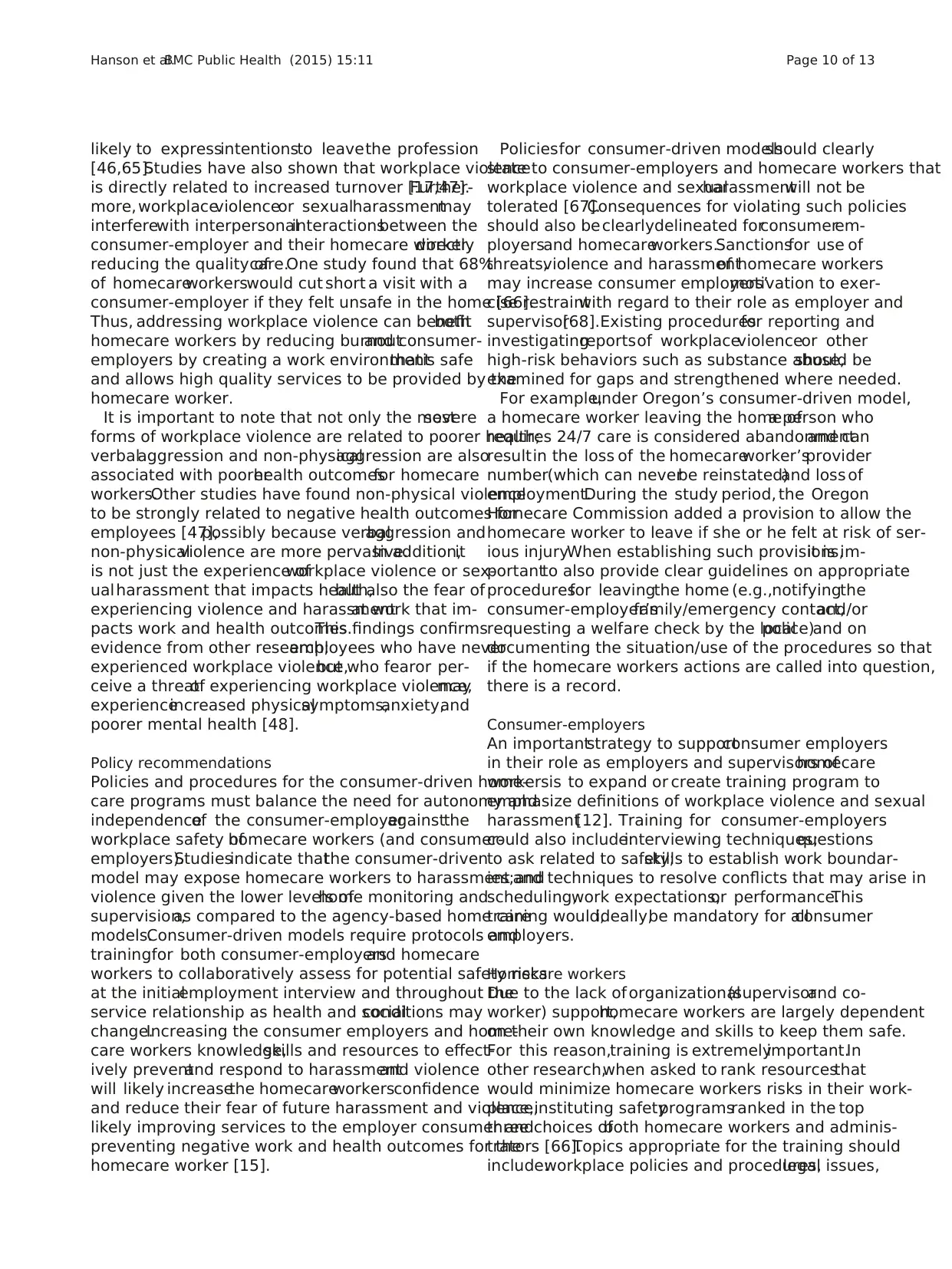
likely to expressintentionsto leavethe profession
[46,65].Studies have also shown that workplace violence
is directly related to increased turnover [17,47].Further-
more, workplaceviolenceor sexualharassmentmay
interferewith interpersonalinteractionsbetween the
consumer-employer and their homecare worker,directly
reducing the quality ofcare.One study found that 68%
of homecareworkerswould cut short a visit with a
consumer-employer if they felt unsafe in the home [66].
Thus, addressing workplace violence can benefitboth
homecare workers by reducing burnoutand consumer-
employers by creating a work environmentthatis safe
and allows high quality services to be provided by the
homecare worker.
It is important to note that not only the mostsevere
forms of workplace violence are related to poorer health;
verbalaggression and non-physicalaggression are also
associated with poorerhealth outcomesfor homecare
workers.Other studies have found non-physical violence
to be strongly related to negative health outcomes for
employees [47],possibly because verbalaggression and
non-physicalviolence are more pervasive.In addition,it
is not just the experience ofworkplace violence or sex-
ual harassment that impacts health,but also the fear of
experiencing violence and harassmentat work that im-
pacts work and health outcomes.This findings confirms
evidence from other research;employees who have never
experienced workplace violence,but who fearor per-
ceive a threatof experiencing workplace violence,may
experienceincreased physicalsymptoms,anxiety,and
poorer mental health [48].
Policy recommendations
Policies and procedures for the consumer-driven home-
care programs must balance the need for autonomy and
independenceof the consumer-employeragainstthe
workplace safety ofhomecare workers (and consumer-
employers).Studiesindicate thatthe consumer-driven
model may expose homecare workers to harassment and
violence given the lower levels ofhome monitoring and
supervision,as compared to the agency-based home care
models.Consumer-driven models require protocols and
trainingfor both consumer-employersand homecare
workers to collaboratively assess for potential safety risks
at the initialemployment interview and throughout the
service relationship as health and socialconditions may
change.Increasing the consumer employers and home-
care workers knowledge,skills and resources to effect-
ively preventand respond to harassmentand violence
will likely increasethe homecareworkersconfidence
and reduce their fear of future harassment and violence,
likely improving services to the employer consumer and
preventing negative work and health outcomes for the
homecare worker [15].
Policiesfor consumer-driven modelsshould clearly
state to consumer-employers and homecare workers that
workplace violence and sexualharassmentwill not be
tolerated [67].Consequences for violating such policies
should also beclearlydelineated forconsumerem-
ployersand homecareworkers.Sanctionsfor use of
threats,violence and harassmentof homecare workers
may increase consumer employers’motivation to exer-
cise restraintwith regard to their role as employer and
supervisor[68].Existing proceduresfor reporting and
investigatingreportsof workplaceviolenceor other
high-risk behaviors such as substance abuse,should be
examined for gaps and strengthened where needed.
For example,under Oregon’s consumer-driven model,
a homecare worker leaving the home ofa person who
requires 24/7 care is considered abandonmentand can
resultin the loss of the homecareworker’sprovider
number(which can neverbe reinstated)and loss of
employment.During the study period, the Oregon
Homecare Commission added a provision to allow the
homecare worker to leave if she or he felt at risk of ser-
ious injury.When establishing such provisions,it is im-
portantto also provide clear guidelines on appropriate
proceduresfor leavingthe home (e.g.,notifyingthe
consumer-employer’sfamily/emergency contact,and/or
requesting a welfare check by the localpolice)and on
documenting the situation/use of the procedures so that
if the homecare workers actions are called into question,
there is a record.
Consumer-employers
An importantstrategy to supportconsumer employers
in their role as employers and supervisors ofhomecare
workersis to expand or create training program to
emphasize definitions of workplace violence and sexual
harassment[12]. Training for consumer-employers
could also include:interviewing techniques;questions
to ask related to safety;skills to establish work boundar-
ies;and techniques to resolve conflicts that may arise in
scheduling,work expectations,or performance.This
training would,ideally,be mandatory for allconsumer
employers.
Homecare workers
Due to the lack of organizational(supervisorand co-
worker) support,homecare workers are largely dependent
on their own knowledge and skills to keep them safe.
For this reason,training is extremelyimportant.In
other research,when asked to rank resourcesthat
would minimize homecare workers risks in their work-
place,instituting safetyprogramsranked in the top
three choices ofboth homecare workers and adminis-
trators [66].Topics appropriate for the training should
include:workplace policies and procedures,legal issues,
Hanson et al.BMC Public Health (2015) 15:11 Page 10 of 13
[46,65].Studies have also shown that workplace violence
is directly related to increased turnover [17,47].Further-
more, workplaceviolenceor sexualharassmentmay
interferewith interpersonalinteractionsbetween the
consumer-employer and their homecare worker,directly
reducing the quality ofcare.One study found that 68%
of homecareworkerswould cut short a visit with a
consumer-employer if they felt unsafe in the home [66].
Thus, addressing workplace violence can benefitboth
homecare workers by reducing burnoutand consumer-
employers by creating a work environmentthatis safe
and allows high quality services to be provided by the
homecare worker.
It is important to note that not only the mostsevere
forms of workplace violence are related to poorer health;
verbalaggression and non-physicalaggression are also
associated with poorerhealth outcomesfor homecare
workers.Other studies have found non-physical violence
to be strongly related to negative health outcomes for
employees [47],possibly because verbalaggression and
non-physicalviolence are more pervasive.In addition,it
is not just the experience ofworkplace violence or sex-
ual harassment that impacts health,but also the fear of
experiencing violence and harassmentat work that im-
pacts work and health outcomes.This findings confirms
evidence from other research;employees who have never
experienced workplace violence,but who fearor per-
ceive a threatof experiencing workplace violence,may
experienceincreased physicalsymptoms,anxiety,and
poorer mental health [48].
Policy recommendations
Policies and procedures for the consumer-driven home-
care programs must balance the need for autonomy and
independenceof the consumer-employeragainstthe
workplace safety ofhomecare workers (and consumer-
employers).Studiesindicate thatthe consumer-driven
model may expose homecare workers to harassment and
violence given the lower levels ofhome monitoring and
supervision,as compared to the agency-based home care
models.Consumer-driven models require protocols and
trainingfor both consumer-employersand homecare
workers to collaboratively assess for potential safety risks
at the initialemployment interview and throughout the
service relationship as health and socialconditions may
change.Increasing the consumer employers and home-
care workers knowledge,skills and resources to effect-
ively preventand respond to harassmentand violence
will likely increasethe homecareworkersconfidence
and reduce their fear of future harassment and violence,
likely improving services to the employer consumer and
preventing negative work and health outcomes for the
homecare worker [15].
Policiesfor consumer-driven modelsshould clearly
state to consumer-employers and homecare workers that
workplace violence and sexualharassmentwill not be
tolerated [67].Consequences for violating such policies
should also beclearlydelineated forconsumerem-
ployersand homecareworkers.Sanctionsfor use of
threats,violence and harassmentof homecare workers
may increase consumer employers’motivation to exer-
cise restraintwith regard to their role as employer and
supervisor[68].Existing proceduresfor reporting and
investigatingreportsof workplaceviolenceor other
high-risk behaviors such as substance abuse,should be
examined for gaps and strengthened where needed.
For example,under Oregon’s consumer-driven model,
a homecare worker leaving the home ofa person who
requires 24/7 care is considered abandonmentand can
resultin the loss of the homecareworker’sprovider
number(which can neverbe reinstated)and loss of
employment.During the study period, the Oregon
Homecare Commission added a provision to allow the
homecare worker to leave if she or he felt at risk of ser-
ious injury.When establishing such provisions,it is im-
portantto also provide clear guidelines on appropriate
proceduresfor leavingthe home (e.g.,notifyingthe
consumer-employer’sfamily/emergency contact,and/or
requesting a welfare check by the localpolice)and on
documenting the situation/use of the procedures so that
if the homecare workers actions are called into question,
there is a record.
Consumer-employers
An importantstrategy to supportconsumer employers
in their role as employers and supervisors ofhomecare
workersis to expand or create training program to
emphasize definitions of workplace violence and sexual
harassment[12]. Training for consumer-employers
could also include:interviewing techniques;questions
to ask related to safety;skills to establish work boundar-
ies;and techniques to resolve conflicts that may arise in
scheduling,work expectations,or performance.This
training would,ideally,be mandatory for allconsumer
employers.
Homecare workers
Due to the lack of organizational(supervisorand co-
worker) support,homecare workers are largely dependent
on their own knowledge and skills to keep them safe.
For this reason,training is extremelyimportant.In
other research,when asked to rank resourcesthat
would minimize homecare workers risks in their work-
place,instituting safetyprogramsranked in the top
three choices ofboth homecare workers and adminis-
trators [66].Topics appropriate for the training should
include:workplace policies and procedures,legal issues,
Hanson et al.BMC Public Health (2015) 15:11 Page 10 of 13
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
identifying warning signs ofviolence,safety planning,as-
sertive communication,conflictresolution,de-escalation
of conflict, and self-care [29,69,70].
Limitations
Our study design was cross-sectional,which was an ad-
equate and efficientway to assess prevalence,but pre-
cludes our ability to determine a causaldirection of the
relationship between workplace violence,sexualharass-
ment,and health outcomes.Our 33% response rate was
not unexpected given some ofthe barriers to reaching
this population,such as income and housing insecurity,
that impact their access to consistent and reliable phone
and internet services.Given this response rate,we can-
not rule outthe possibility thatrespondents may have
been more likely to experience workplace violence than
non-respondents.However,we were careful during
recruitmentto emphasizethe importanceof hearing
from all workers,whetheror not they had experience
workplaceviolence.There is also the possibilitythat
participants may under-report exposure,wanting to give
socially desirableresponsesto sensitivequestions.
Healthcare workerstend to under-reportviolentinci-
dents,in part because they see such incidents as “part of
the job” [71,72].Also, while we eliminated participants
providingservicesfor only their spousesfrom the
sexual-harassmentanalyses,we did not ask whethera
homecare worker was providing services to an intimate
partner or ex-intimate partner.However,we do not sus-
pectthatasking aboutintimate or ex-intimate partners
would have increased significantly the smallnumber of
homecare workers (2.14%) who provided services only to
a spouse orpartner.This assumption is supported by
the percentage of homecare workers in our study report-
ing sexualharassment,which is similar to,if not lower
than,otherstudieswe reviewed [21-23,25,26].Finally,
the focus ofthis study was on homecare workers from
Oregon’s consumer-driven model,thus the findings may
not be generalizableto homecareworkersworking
under different models,such as private or agency-based
models.
Conclusions
As our global population ages,the importanceof
retaining a health workforce of homecare workers is of
increasingimportance.Homecaremodelssimilar to
Oregon’s consumer-driven modelare existin the UK
and in several US states including California,Connecticut,
Illinion,Maryland,Massachusetts,Minnesota,Missouri,
and Washington.Given this,we feelthat our study find-
ings may be usefulto policy makers in a wide variety of
locations who are currently using or may be considering a
similar modelof homecare.Our research adds to the lit-
erature demonstrating that homecare workers are at high
risk ofexposure to incidents ofworkplace violence and
sexualharassment,and that these experiences are related
to increased stress,depression,burnout,and sleeping
problems.In order to ensure homecare worker safety and
positive health outcomes for both worker and consumer-
employer,it is necessary to develop preventive safety pol-
icies and proceduresand provideprevention training.
More research is needed to understand how best to inter-
vene to reduce homecare workers’exposure to workplace
violence and sexualharassment.Homecare worker train-
ings should be designed to increase confidence and cap-
acity to plan for safety,establish and maintain appropriate
work boundaries,and de-escalate violence and harassing
situations.
Additional files
Additional file 1: Exploratory factor analysis on burnout.
Additional file 2: Confidence in preventing and responding to
sexual harassment and workplace violent scale.
Additional file 3: Correlations among covariates,predictors,
moderators,and outcomes.
Competing interests
The authors declare that they have no competing interests.
Authors’contributions
GH participated in the design and coordination of the study,carried out
statisticalanalyses,and led the writing of the manuscript.NP participated in
the design of the study,helped in acquiring funding,acted as the senior
statistician,and helped draft the manuscript.HM participated in the design
of the study,facilitated and maintained relationships with community
partners,and helped draft the manuscript.NL helped draft the manuscript.
NG was the senior investigator who led in the design of the study and
acquisition of funding,facilitated and maintained relationships with
community partners,and helped draft the manuscript.Allauthors read and
approved the finalmanuscript.
Acknowledgements
This research is supported by the NationalInstitute for OccupationalHealth
and Safety research grant R01 OH009080.The authors thank the members of
our advisory board for allof their support including their valuable input
during the development of the survey and recruitment strategies.Additional
thanks to the Service Employees InternationalUnion Local503 for providing
the recruitment roster for the study.Finally,specialthanks to allof the
homecare workers who participated in the study and shared their time and
perspective.
Author details
1Research Data and Analysis Center,Center for Health Research,Portland,
Oregon,USA.2Labor Education and Research Center,University of Oregon,
Portland,Oregon,USA.3Oregon Institute of OccupationalHealth Sciences,
Oregon Health & Science University,Portland,Oregon,USA.4Schoolof
Nursing,Johns Hopkins University,Baltimore,Maryland,USA.
Received:16 October 2014 Accepted:22 December 2014
References
1. United Nations Population Fund (UNFPA).United Nations Population Fund
(UNFPA).Aging in the 21st century:a celebration and a challenge:Executive
summary,2012.New York and London;2012.
Hanson et al.BMC Public Health (2015) 15:11 Page 11 of 13
sertive communication,conflictresolution,de-escalation
of conflict, and self-care [29,69,70].
Limitations
Our study design was cross-sectional,which was an ad-
equate and efficientway to assess prevalence,but pre-
cludes our ability to determine a causaldirection of the
relationship between workplace violence,sexualharass-
ment,and health outcomes.Our 33% response rate was
not unexpected given some ofthe barriers to reaching
this population,such as income and housing insecurity,
that impact their access to consistent and reliable phone
and internet services.Given this response rate,we can-
not rule outthe possibility thatrespondents may have
been more likely to experience workplace violence than
non-respondents.However,we were careful during
recruitmentto emphasizethe importanceof hearing
from all workers,whetheror not they had experience
workplaceviolence.There is also the possibilitythat
participants may under-report exposure,wanting to give
socially desirableresponsesto sensitivequestions.
Healthcare workerstend to under-reportviolentinci-
dents,in part because they see such incidents as “part of
the job” [71,72].Also, while we eliminated participants
providingservicesfor only their spousesfrom the
sexual-harassmentanalyses,we did not ask whethera
homecare worker was providing services to an intimate
partner or ex-intimate partner.However,we do not sus-
pectthatasking aboutintimate or ex-intimate partners
would have increased significantly the smallnumber of
homecare workers (2.14%) who provided services only to
a spouse orpartner.This assumption is supported by
the percentage of homecare workers in our study report-
ing sexualharassment,which is similar to,if not lower
than,otherstudieswe reviewed [21-23,25,26].Finally,
the focus ofthis study was on homecare workers from
Oregon’s consumer-driven model,thus the findings may
not be generalizableto homecareworkersworking
under different models,such as private or agency-based
models.
Conclusions
As our global population ages,the importanceof
retaining a health workforce of homecare workers is of
increasingimportance.Homecaremodelssimilar to
Oregon’s consumer-driven modelare existin the UK
and in several US states including California,Connecticut,
Illinion,Maryland,Massachusetts,Minnesota,Missouri,
and Washington.Given this,we feelthat our study find-
ings may be usefulto policy makers in a wide variety of
locations who are currently using or may be considering a
similar modelof homecare.Our research adds to the lit-
erature demonstrating that homecare workers are at high
risk ofexposure to incidents ofworkplace violence and
sexualharassment,and that these experiences are related
to increased stress,depression,burnout,and sleeping
problems.In order to ensure homecare worker safety and
positive health outcomes for both worker and consumer-
employer,it is necessary to develop preventive safety pol-
icies and proceduresand provideprevention training.
More research is needed to understand how best to inter-
vene to reduce homecare workers’exposure to workplace
violence and sexualharassment.Homecare worker train-
ings should be designed to increase confidence and cap-
acity to plan for safety,establish and maintain appropriate
work boundaries,and de-escalate violence and harassing
situations.
Additional files
Additional file 1: Exploratory factor analysis on burnout.
Additional file 2: Confidence in preventing and responding to
sexual harassment and workplace violent scale.
Additional file 3: Correlations among covariates,predictors,
moderators,and outcomes.
Competing interests
The authors declare that they have no competing interests.
Authors’contributions
GH participated in the design and coordination of the study,carried out
statisticalanalyses,and led the writing of the manuscript.NP participated in
the design of the study,helped in acquiring funding,acted as the senior
statistician,and helped draft the manuscript.HM participated in the design
of the study,facilitated and maintained relationships with community
partners,and helped draft the manuscript.NL helped draft the manuscript.
NG was the senior investigator who led in the design of the study and
acquisition of funding,facilitated and maintained relationships with
community partners,and helped draft the manuscript.Allauthors read and
approved the finalmanuscript.
Acknowledgements
This research is supported by the NationalInstitute for OccupationalHealth
and Safety research grant R01 OH009080.The authors thank the members of
our advisory board for allof their support including their valuable input
during the development of the survey and recruitment strategies.Additional
thanks to the Service Employees InternationalUnion Local503 for providing
the recruitment roster for the study.Finally,specialthanks to allof the
homecare workers who participated in the study and shared their time and
perspective.
Author details
1Research Data and Analysis Center,Center for Health Research,Portland,
Oregon,USA.2Labor Education and Research Center,University of Oregon,
Portland,Oregon,USA.3Oregon Institute of OccupationalHealth Sciences,
Oregon Health & Science University,Portland,Oregon,USA.4Schoolof
Nursing,Johns Hopkins University,Baltimore,Maryland,USA.
Received:16 October 2014 Accepted:22 December 2014
References
1. United Nations Population Fund (UNFPA).United Nations Population Fund
(UNFPA).Aging in the 21st century:a celebration and a challenge:Executive
summary,2012.New York and London;2012.
Hanson et al.BMC Public Health (2015) 15:11 Page 11 of 13
2. Bettio F,Verashchagina A.Long-Term Care for the elderly:Provisions and
providers in 33 European countries.2012.[http://ec.europa.eu/justice/gen-
der-equality/files/elderly_care_en.pdf]
3. Francis J.UKHCA Summary paper:An overview of the UK domiciliary care sector.
No.3083104 [http://www.ukhca.co.uk/pdfs/domiciliarycaresectoroverview.pdf]
4. NakaishiL,Moss H,Weinstein M,Perrin N,Rose L,Anger WK,et al.Exploring
workplace violence among home care workers in a consumer-driven home
health care program.Workplace Health Saf.2013;61:441–50.
5. Howes C.Love,money,or flexibility:what motivates people to work in
consumer-directed home care? Gerontologist.2008;48(Spec No 1):46–59.
6. Barling J,Rogers AG,Kelloway EK.Behind closed doors:in-home workers’
experience of sexualharassment and workplace violence.J Occup Health
Psychol.2001;6:255–69.
7. Canton AN,Sherman MF,Magda LA,Westra LJ,Pearson JM,Raveis VH,et al.
Violence,job satisfaction,and employment intentions among home
healthcare registered nurses.Home Healthc Nurse.2009;27:364–73.
8. McPhaulK,Lipscomb J,Johnson J.Assessing risk for violence on home
health visits.Home Healthc Nurse.2010;28:278–89.
9. ChappellD,Di Martino V.Violence at Work.InternationalLabour Office:
Geneva,Switzerland;2006.
10. U.S.Department of Labor OccupationalSafety and Health Administration.
Workplace Violence Fact Sheet.2002.
11. Camerino D,Estryn-Behar M,Conway PM,van Der Heijden BI,Hasselhorn
HM.Work-related factors and violence among nursing staff in the European
NEXT study:a longitudinalcohort study.Int J Nurs Stud.2008;45:35–50.
12. Rippon TJ.Aggression and violence in health care professions.J Adv Nurs.
2000;31:452–60.
13. McPhaulKM,Lipscomb JA.Workplace violence in health care:recognized
but not regulated.Online J Issues Nurs.2004;9:7.
14. Occupational Safety and Health Administration.Guidelines for preventing
workplace violence for health care and social service workers.[www.osha.gov]
15. Distasio CA.Violence against home care providers–stop it before it starts.
Caring.2000;19:14–8.
16. Health and Safety Executive.Health and safety in human health and social
care in Great Britain,2013 [http://www.hse.gov.uk/statistics/industry/
healthservices/health.pdf]
17. Sherman MF,Gershon RR,Samar SM,Pearson JM,Canton AN,Damsky MR.
Safety factors predictive of job satisfaction and job retention among home
healthcare aides.J Occup Environ Med.2008;50:1430–41.
18. Geiger-Brown J,Muntaner C,McPhaulK,Lipscomb J,Trinkoff A.Abuse and
violence during home care work as predictor of worker depression.Home
Health Care Serv Q.2007;26:59–77.
19. Ilies R,Hauserman N,Schwochau S,StibalJ. Reported incidence rates of
work-related sexualharassment in the United States:Using meta-analysis to
explain reported rate disparities.PersonnelPsychology.2003;56:607–31.
20. Chuang SC,Lin HM.Nurses confronting sexualharassment in the medical
environment.Stud Health TechnolInform.2006;122:349–52.
21. Finnis SJ,Robbins I.Sexualharassment of nurses:an occupationalhazard?
J Clin Nurs.1994;3:87–95.
22. Grieco A.Scope and nature of sexualharassment in nursing.J Sex Res.
1987;23:261–6.
23. Kinross L.Nurse assault:overcoming the barriers to prevention.The Nursing
Report.Can Nurs Manage.1992;49:4–8.
24. Libbus MK,Bowman KG.Sexualharassment of female registered nurses in
hospitals.J Nurs Adm.1994;24:26–31.
25. Preston A.Sexualharassment survey:sufferers in silence.Nurs Stand.
1990;5:62–3.
26. Valente SM,Bullough V.Sexualharassment of nurses in the workplace.J
Nurs Care Qual.2004;19:234–41.
27. Williams MF.Violence and sexualharassment:impact on registered nurses
in the workplace.AAOHN J.1996;44:73–7.
28. Rogers JL,Maurizio SJ.Prevalence of sexualharassment among rural
community care workers.Home Healthc Nurse.1993;11:37–40.
29. FarrellG,Cubit K.Nurses under threat:a comparison of content of 28
aggression management programs.Int J Ment Health Nurs.2005;14:44–53.
30. Janicak CA.RegionalVariations in Workplace Homicide Rates.Compensation
and Working Conditions.2003.
31. Bensley L,Nelson N,Kaufman J,Silverstein B,Kalat J.Study of Assaults on
Staff in Washington State Hospitals-FinalReport.1993.
32. Foley M.Violence in Washington Workplaces,1995–2000.Washington:
Olympia;2002.
33. McGovern P,Kochevar L,Lohman W,Zaidman B,Gerberich SG,Nyman J,
et al.The cost of work-related physicalassaults in Minnesota.Health Serv
Res.2000;35:663–86.
34. Fitzgerald LF.Sexualharassment.Violence against women in the workplace.
Am Psychol.1993;48:1070–6.
35. Lazarus RS,Folkman S.Stress,Appraisal,and Coping.New York,NY:Springer
Publishing Company;1984.
36. Rogers KA,Kelloway EK.Violence at work:personaland organizational
outcomes.J Occup Health Psychol.1997;2:63–71.
37. Denton MA,Zeytinoglu IU,Davies S.Working in clients’homes:the impact
on the mentalhealth and well-being of visiting home care workers.Home
Health Care Serv Q.2002;21:1–27.
38. Bussing A,Hoge T.Aggression and violence against home care workers.
J Occup Health Psychol.2004;9:206–19.
39. Rospenda KM,Richman JA,Shannon CA.Prevalence and mentalhealth
correlates of harassment and discrimination in the workplace:results from a
nationalstudy.J Interpers Violence.2009;24:819–43.
40. Matthews LR.Effect of staff debriefing on posttraumatic stress symptoms after
assaults by community housing residents.Psychiatr Serv.1998;49:207–12.
41. Findorff-Dennis MJ,McGovern PM,BullM,Hung J.Work related assaults.
The impact on victims.AAOHN J.1999;47:456–65.
42. Atawneh FA,Zahid MA,Al-SahlawiKS,Shahid AA,Al-Farrah MH.Violence
against nurses in hospitals:prevalence and effects.Br J Nurs.2003;12:102–7.
43. Walsh BR,Clark E.Post-trauma symptoms in health workers following
physicaland verbalaggression.Work Stress.2003;17:170–81.
44. Holz CL.When professionalkindness is misunderstood:boundaries and
stalking issues:a case study for the home health clinician.Home Healthc
Nurse.2009;27:410–6.
45. Inoue M,Tsukano K,Muraoka M,Kaneko F,Okamura H.Psychological
impact of verbalabuse and violence by patients on nurses working in
psychiatric departments.Psychiatry Clin Neurosci.2006;60:29–36.
46. Leiter MP,Harvie PL.Burnout among mentalhealth workers:a review and a
research agenda.Int J Soc Psychiatry.1996;42:90–101.
47. Gerberich SG,Church TR,McGovern PM,Hansen HE,Nachreiner NM,Geisser
MS,et al.An epidemiologicalstudy of the magnitude and consequences of
work related violence:the Minnesota Nurses’Study.Occup Environ Med.
2004;61:495–503.
48. HallJK,Specter PE.Relationships of work stress measures for employees
with the same job.Work Stress.1991;5:29–35.
49. Durkin N,Wilson C.The value and impact of violence prevention training in
a home healthcare setting.Home Healthc Nurse Manag.1998;2:22–8.
50. Cortina LM,Magley VJ,Williams JH,Langhout RD.Incivility in the workplace:
incidence and impact.J Occup Health Psychol.2001;6:64–80.
51. Hegney D,Plank A,Parker V.Workplace violence in nursing in Queensland,
Australia:a self-reported study.Int J Nurs Pract.2003;9:261–8.
52. Borritz M,Rugulies R,Bjorner JB,Villadsen E,Mikkelsen OA,Kristensen TS.
Burnout among employees in human service work:design and baseline
findings of the PUMA study.Scand J Public Health.2006;34:49–58.
53. Kristensen TS,Borrotz M,Villadsen E,Christensen KB.The Copenhagen
burnout inventory:a new toolfor the assessment of burnout.Work Stress.
2005;19:192–207.
54. Borritz M,Kristensen T.Copenhagen Burnout Inventory (English Version) used in
the PUMA study.[http://www.arbejdsmiljoforskning.dk/upload/CBI-scales.pdf]
55. Pejtersen JH,Kristensen TS,Borg V,Bjorner JB.The second version of the
Copenhagen psychosocial questionnaire.Scand J Public Health.2010;38:8–24.
56. National Research Centre for the Working Environment.The construction of
the COPSOQ II.[http://www.arbejdsmiljoforskning.dk/~/media/
Spoergeskemaer/copsoq/uk/construction-of-the-scales-of-copsoq-ii-22-6.pdf#
57. Ross CE,Wu CL.Education,age,and the cumulative advantage in health.
J Health Soc Behav.1996;37:104–20.
58. NationalCenter for Health Statistics.Healthy People 2010 FinalReview.
Hyattsville,MD.[http://www.cdc.gov/nchs/data/hpdata2010/
hp2010_final_review.pdf]
59. Maslach C,SchaufeliWB,Leiter MP.Job burnout.Annu Rev Psychol.
2001;52:397–422.
60. Holahan CJ,Moos RH.Life stress and health:personality,coping,and family
support in stress resistance.J Pers Soc Psychol.1985;49:739–47.
61. Bandura A.Self-efficacy mechanism in human agency.Am Psychol.
1982;37:122–47.
62. Lockard CB,Wolf M.Occupationalemployment projections to.Mon Labor
Rev.2012;2020:84–108.
Hanson et al.BMC Public Health (2015) 15:11 Page 12 of 13
providers in 33 European countries.2012.[http://ec.europa.eu/justice/gen-
der-equality/files/elderly_care_en.pdf]
3. Francis J.UKHCA Summary paper:An overview of the UK domiciliary care sector.
No.3083104 [http://www.ukhca.co.uk/pdfs/domiciliarycaresectoroverview.pdf]
4. NakaishiL,Moss H,Weinstein M,Perrin N,Rose L,Anger WK,et al.Exploring
workplace violence among home care workers in a consumer-driven home
health care program.Workplace Health Saf.2013;61:441–50.
5. Howes C.Love,money,or flexibility:what motivates people to work in
consumer-directed home care? Gerontologist.2008;48(Spec No 1):46–59.
6. Barling J,Rogers AG,Kelloway EK.Behind closed doors:in-home workers’
experience of sexualharassment and workplace violence.J Occup Health
Psychol.2001;6:255–69.
7. Canton AN,Sherman MF,Magda LA,Westra LJ,Pearson JM,Raveis VH,et al.
Violence,job satisfaction,and employment intentions among home
healthcare registered nurses.Home Healthc Nurse.2009;27:364–73.
8. McPhaulK,Lipscomb J,Johnson J.Assessing risk for violence on home
health visits.Home Healthc Nurse.2010;28:278–89.
9. ChappellD,Di Martino V.Violence at Work.InternationalLabour Office:
Geneva,Switzerland;2006.
10. U.S.Department of Labor OccupationalSafety and Health Administration.
Workplace Violence Fact Sheet.2002.
11. Camerino D,Estryn-Behar M,Conway PM,van Der Heijden BI,Hasselhorn
HM.Work-related factors and violence among nursing staff in the European
NEXT study:a longitudinalcohort study.Int J Nurs Stud.2008;45:35–50.
12. Rippon TJ.Aggression and violence in health care professions.J Adv Nurs.
2000;31:452–60.
13. McPhaulKM,Lipscomb JA.Workplace violence in health care:recognized
but not regulated.Online J Issues Nurs.2004;9:7.
14. Occupational Safety and Health Administration.Guidelines for preventing
workplace violence for health care and social service workers.[www.osha.gov]
15. Distasio CA.Violence against home care providers–stop it before it starts.
Caring.2000;19:14–8.
16. Health and Safety Executive.Health and safety in human health and social
care in Great Britain,2013 [http://www.hse.gov.uk/statistics/industry/
healthservices/health.pdf]
17. Sherman MF,Gershon RR,Samar SM,Pearson JM,Canton AN,Damsky MR.
Safety factors predictive of job satisfaction and job retention among home
healthcare aides.J Occup Environ Med.2008;50:1430–41.
18. Geiger-Brown J,Muntaner C,McPhaulK,Lipscomb J,Trinkoff A.Abuse and
violence during home care work as predictor of worker depression.Home
Health Care Serv Q.2007;26:59–77.
19. Ilies R,Hauserman N,Schwochau S,StibalJ. Reported incidence rates of
work-related sexualharassment in the United States:Using meta-analysis to
explain reported rate disparities.PersonnelPsychology.2003;56:607–31.
20. Chuang SC,Lin HM.Nurses confronting sexualharassment in the medical
environment.Stud Health TechnolInform.2006;122:349–52.
21. Finnis SJ,Robbins I.Sexualharassment of nurses:an occupationalhazard?
J Clin Nurs.1994;3:87–95.
22. Grieco A.Scope and nature of sexualharassment in nursing.J Sex Res.
1987;23:261–6.
23. Kinross L.Nurse assault:overcoming the barriers to prevention.The Nursing
Report.Can Nurs Manage.1992;49:4–8.
24. Libbus MK,Bowman KG.Sexualharassment of female registered nurses in
hospitals.J Nurs Adm.1994;24:26–31.
25. Preston A.Sexualharassment survey:sufferers in silence.Nurs Stand.
1990;5:62–3.
26. Valente SM,Bullough V.Sexualharassment of nurses in the workplace.J
Nurs Care Qual.2004;19:234–41.
27. Williams MF.Violence and sexualharassment:impact on registered nurses
in the workplace.AAOHN J.1996;44:73–7.
28. Rogers JL,Maurizio SJ.Prevalence of sexualharassment among rural
community care workers.Home Healthc Nurse.1993;11:37–40.
29. FarrellG,Cubit K.Nurses under threat:a comparison of content of 28
aggression management programs.Int J Ment Health Nurs.2005;14:44–53.
30. Janicak CA.RegionalVariations in Workplace Homicide Rates.Compensation
and Working Conditions.2003.
31. Bensley L,Nelson N,Kaufman J,Silverstein B,Kalat J.Study of Assaults on
Staff in Washington State Hospitals-FinalReport.1993.
32. Foley M.Violence in Washington Workplaces,1995–2000.Washington:
Olympia;2002.
33. McGovern P,Kochevar L,Lohman W,Zaidman B,Gerberich SG,Nyman J,
et al.The cost of work-related physicalassaults in Minnesota.Health Serv
Res.2000;35:663–86.
34. Fitzgerald LF.Sexualharassment.Violence against women in the workplace.
Am Psychol.1993;48:1070–6.
35. Lazarus RS,Folkman S.Stress,Appraisal,and Coping.New York,NY:Springer
Publishing Company;1984.
36. Rogers KA,Kelloway EK.Violence at work:personaland organizational
outcomes.J Occup Health Psychol.1997;2:63–71.
37. Denton MA,Zeytinoglu IU,Davies S.Working in clients’homes:the impact
on the mentalhealth and well-being of visiting home care workers.Home
Health Care Serv Q.2002;21:1–27.
38. Bussing A,Hoge T.Aggression and violence against home care workers.
J Occup Health Psychol.2004;9:206–19.
39. Rospenda KM,Richman JA,Shannon CA.Prevalence and mentalhealth
correlates of harassment and discrimination in the workplace:results from a
nationalstudy.J Interpers Violence.2009;24:819–43.
40. Matthews LR.Effect of staff debriefing on posttraumatic stress symptoms after
assaults by community housing residents.Psychiatr Serv.1998;49:207–12.
41. Findorff-Dennis MJ,McGovern PM,BullM,Hung J.Work related assaults.
The impact on victims.AAOHN J.1999;47:456–65.
42. Atawneh FA,Zahid MA,Al-SahlawiKS,Shahid AA,Al-Farrah MH.Violence
against nurses in hospitals:prevalence and effects.Br J Nurs.2003;12:102–7.
43. Walsh BR,Clark E.Post-trauma symptoms in health workers following
physicaland verbalaggression.Work Stress.2003;17:170–81.
44. Holz CL.When professionalkindness is misunderstood:boundaries and
stalking issues:a case study for the home health clinician.Home Healthc
Nurse.2009;27:410–6.
45. Inoue M,Tsukano K,Muraoka M,Kaneko F,Okamura H.Psychological
impact of verbalabuse and violence by patients on nurses working in
psychiatric departments.Psychiatry Clin Neurosci.2006;60:29–36.
46. Leiter MP,Harvie PL.Burnout among mentalhealth workers:a review and a
research agenda.Int J Soc Psychiatry.1996;42:90–101.
47. Gerberich SG,Church TR,McGovern PM,Hansen HE,Nachreiner NM,Geisser
MS,et al.An epidemiologicalstudy of the magnitude and consequences of
work related violence:the Minnesota Nurses’Study.Occup Environ Med.
2004;61:495–503.
48. HallJK,Specter PE.Relationships of work stress measures for employees
with the same job.Work Stress.1991;5:29–35.
49. Durkin N,Wilson C.The value and impact of violence prevention training in
a home healthcare setting.Home Healthc Nurse Manag.1998;2:22–8.
50. Cortina LM,Magley VJ,Williams JH,Langhout RD.Incivility in the workplace:
incidence and impact.J Occup Health Psychol.2001;6:64–80.
51. Hegney D,Plank A,Parker V.Workplace violence in nursing in Queensland,
Australia:a self-reported study.Int J Nurs Pract.2003;9:261–8.
52. Borritz M,Rugulies R,Bjorner JB,Villadsen E,Mikkelsen OA,Kristensen TS.
Burnout among employees in human service work:design and baseline
findings of the PUMA study.Scand J Public Health.2006;34:49–58.
53. Kristensen TS,Borrotz M,Villadsen E,Christensen KB.The Copenhagen
burnout inventory:a new toolfor the assessment of burnout.Work Stress.
2005;19:192–207.
54. Borritz M,Kristensen T.Copenhagen Burnout Inventory (English Version) used in
the PUMA study.[http://www.arbejdsmiljoforskning.dk/upload/CBI-scales.pdf]
55. Pejtersen JH,Kristensen TS,Borg V,Bjorner JB.The second version of the
Copenhagen psychosocial questionnaire.Scand J Public Health.2010;38:8–24.
56. National Research Centre for the Working Environment.The construction of
the COPSOQ II.[http://www.arbejdsmiljoforskning.dk/~/media/
Spoergeskemaer/copsoq/uk/construction-of-the-scales-of-copsoq-ii-22-6.pdf#
57. Ross CE,Wu CL.Education,age,and the cumulative advantage in health.
J Health Soc Behav.1996;37:104–20.
58. NationalCenter for Health Statistics.Healthy People 2010 FinalReview.
Hyattsville,MD.[http://www.cdc.gov/nchs/data/hpdata2010/
hp2010_final_review.pdf]
59. Maslach C,SchaufeliWB,Leiter MP.Job burnout.Annu Rev Psychol.
2001;52:397–422.
60. Holahan CJ,Moos RH.Life stress and health:personality,coping,and family
support in stress resistance.J Pers Soc Psychol.1985;49:739–47.
61. Bandura A.Self-efficacy mechanism in human agency.Am Psychol.
1982;37:122–47.
62. Lockard CB,Wolf M.Occupationalemployment projections to.Mon Labor
Rev.2012;2020:84–108.
Hanson et al.BMC Public Health (2015) 15:11 Page 12 of 13
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
63. Carers UK.Growing the care market:Turning a demographic challenge into
an economic opportunity.[http://socialwelfare.bl.uk/subject-areas/services-
activity/social-work-care-services/carersuk/future121.aspx]
64. White-Chu EF,Graves WJ,Godfrey SM,Bonner A,Sloane P.Beyond the
medicalmodel:the culture change revolution in long-term care.J Am Med
Dir Assoc.2009;10:370–8.
65. Raquepaw JM,Miller RS.Psychotherapist burnout:a componentialanalysis.
ProfessionalPsychology:Research and Practice.1989;20:32–6.
66. Kendra MA,Weiker A,Simon S,Grant A,Shullick D.Safety concerns affecting
delivery of home health care.Public Health Nurs.1996;13:83–9.
67. Letizia JM,Cassagrande K.Workplace violence:a continued to homecare
employers and employees.Home Health Care Management & Practice.
2005;17:327–9.
68. Dekker I,Barling J.Personaland organizationalpredictors of workplace
sexualharassment of women by men.J Occup Health Psychol.1998;3:7–18.
69. Beech B,Leather P.Workplace violence in the health care sector:a review
of staff training and integration of training evaluation models.Aggression
Violent Behav.2006;11:12–43.
70. Runyan CW,Zakocs RC,Zwerling C.Administrative and behavioral
interventions for workplace violence prevention.Am J Prev Med.
2000;18:116–27.
71. Fazzone PA,Barloon LF,McConnellSJ,Chitty JA.Personalsafety,violence,
and home health.Public Health Nurs.2000;17:43–52.
72. Flynn L.The State of the Nursing Workforce in New Jersey:Findings from a
Statewide Survey of Registered Nurses.Newark,NJ:New Jersey:
Collaborating Center for Nursing;2007.
Submit your next manuscript to BioMed Central
and take full advantage of:
• Convenient online submission
• Thorough peer review
• No space constraints or color figure charges
• Immediate publication on acceptance
• Inclusion in PubMed, CAS, Scopus and Google Scholar
• Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Hanson et al.BMC Public Health (2015) 15:11 Page 13 of 13
an economic opportunity.[http://socialwelfare.bl.uk/subject-areas/services-
activity/social-work-care-services/carersuk/future121.aspx]
64. White-Chu EF,Graves WJ,Godfrey SM,Bonner A,Sloane P.Beyond the
medicalmodel:the culture change revolution in long-term care.J Am Med
Dir Assoc.2009;10:370–8.
65. Raquepaw JM,Miller RS.Psychotherapist burnout:a componentialanalysis.
ProfessionalPsychology:Research and Practice.1989;20:32–6.
66. Kendra MA,Weiker A,Simon S,Grant A,Shullick D.Safety concerns affecting
delivery of home health care.Public Health Nurs.1996;13:83–9.
67. Letizia JM,Cassagrande K.Workplace violence:a continued to homecare
employers and employees.Home Health Care Management & Practice.
2005;17:327–9.
68. Dekker I,Barling J.Personaland organizationalpredictors of workplace
sexualharassment of women by men.J Occup Health Psychol.1998;3:7–18.
69. Beech B,Leather P.Workplace violence in the health care sector:a review
of staff training and integration of training evaluation models.Aggression
Violent Behav.2006;11:12–43.
70. Runyan CW,Zakocs RC,Zwerling C.Administrative and behavioral
interventions for workplace violence prevention.Am J Prev Med.
2000;18:116–27.
71. Fazzone PA,Barloon LF,McConnellSJ,Chitty JA.Personalsafety,violence,
and home health.Public Health Nurs.2000;17:43–52.
72. Flynn L.The State of the Nursing Workforce in New Jersey:Findings from a
Statewide Survey of Registered Nurses.Newark,NJ:New Jersey:
Collaborating Center for Nursing;2007.
Submit your next manuscript to BioMed Central
and take full advantage of:
• Convenient online submission
• Thorough peer review
• No space constraints or color figure charges
• Immediate publication on acceptance
• Inclusion in PubMed, CAS, Scopus and Google Scholar
• Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Hanson et al.BMC Public Health (2015) 15:11 Page 13 of 13
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.

