Effective Communication Plan for Optimal Wound Documentation
VerifiedAdded on 2021/06/14
|14
|1197
|79
Presentation
AI Summary
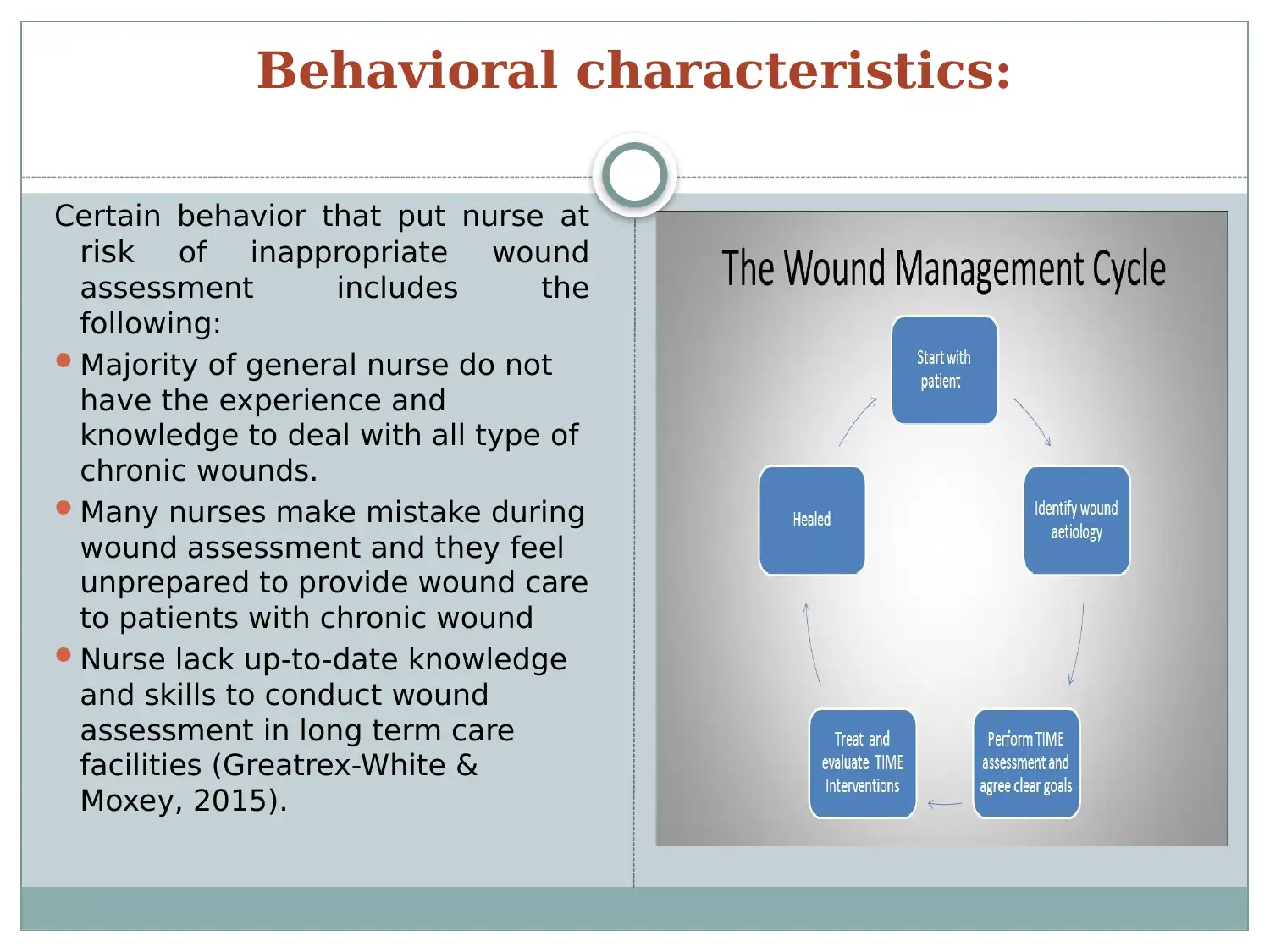
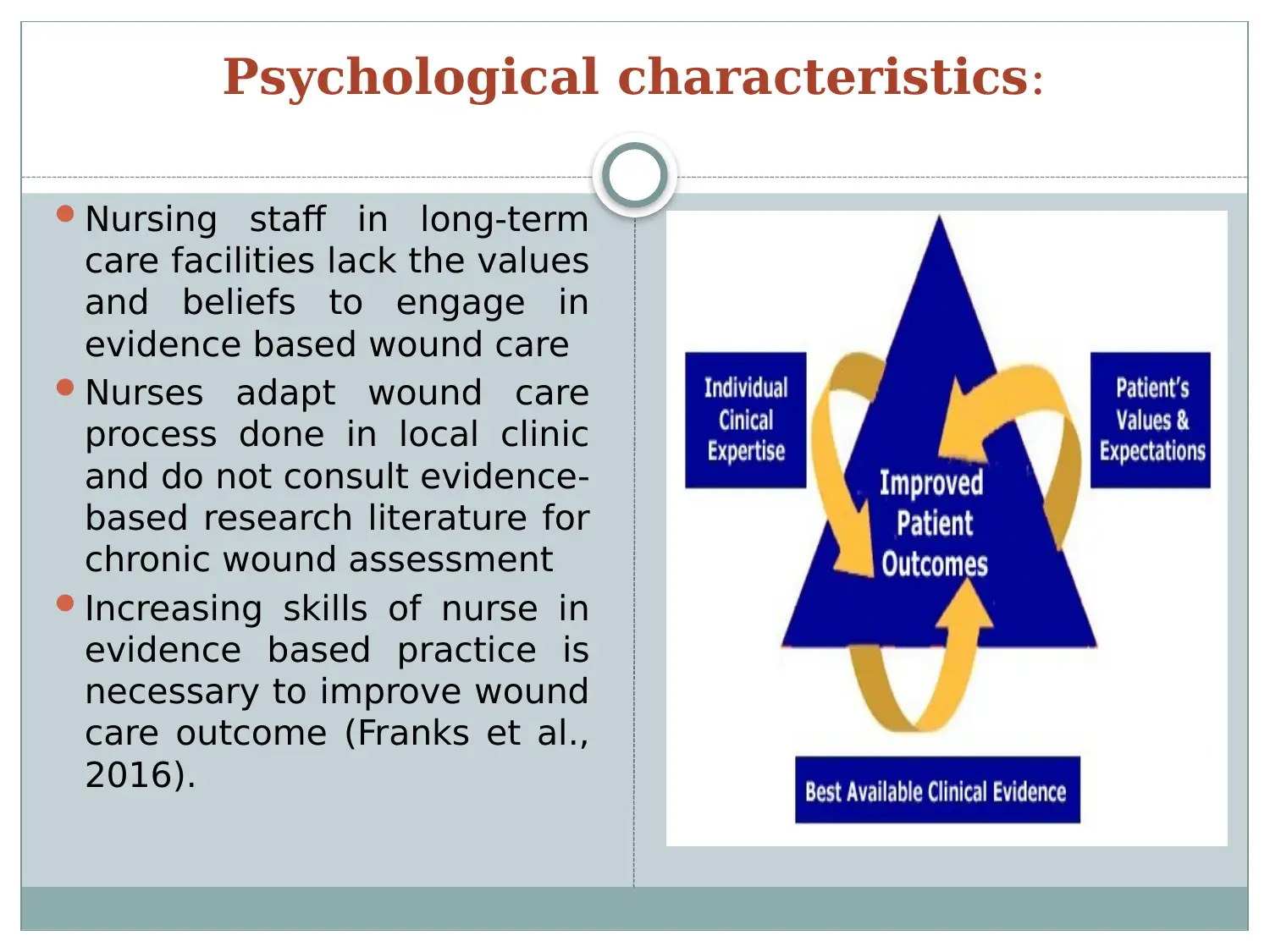
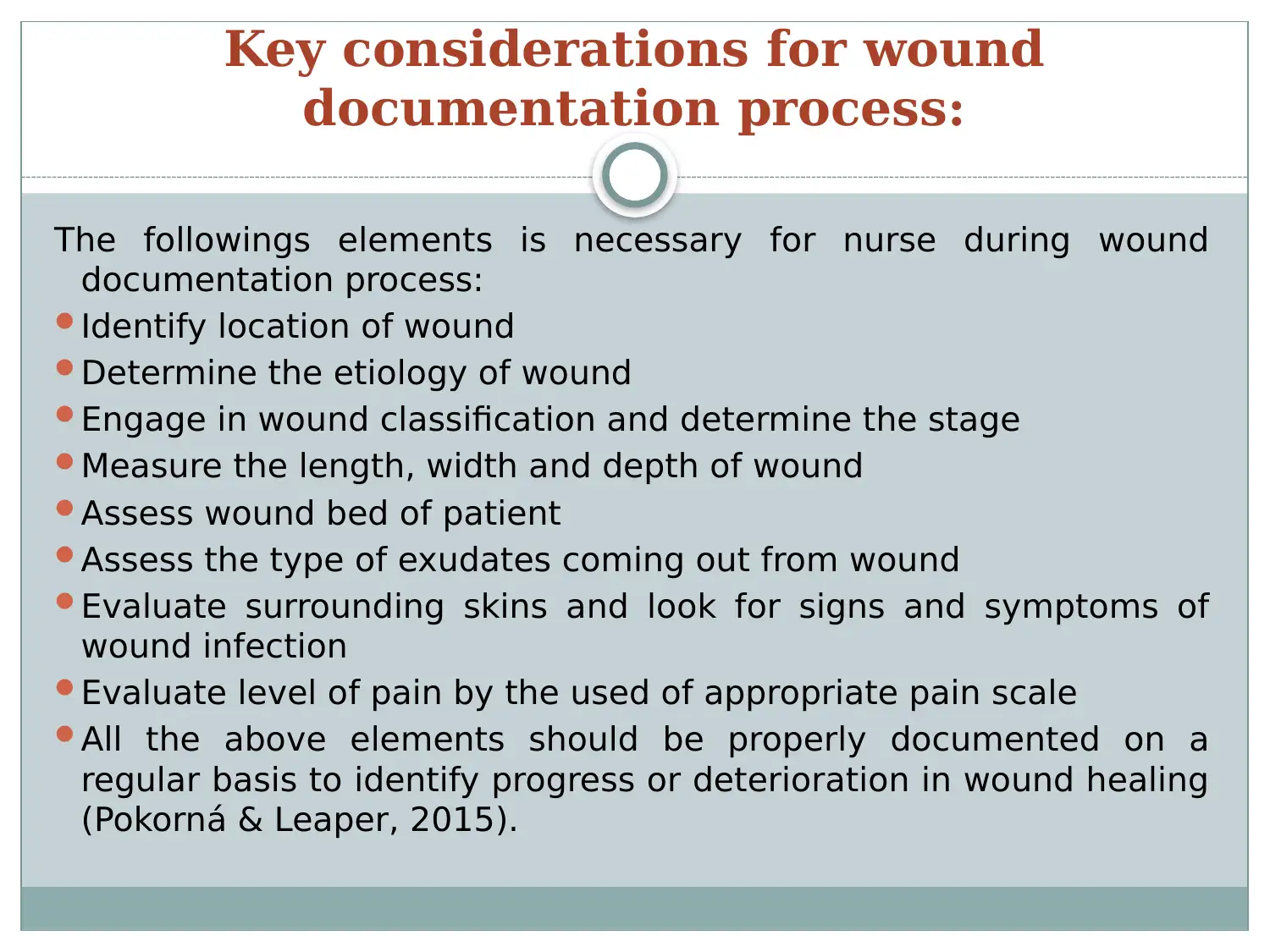
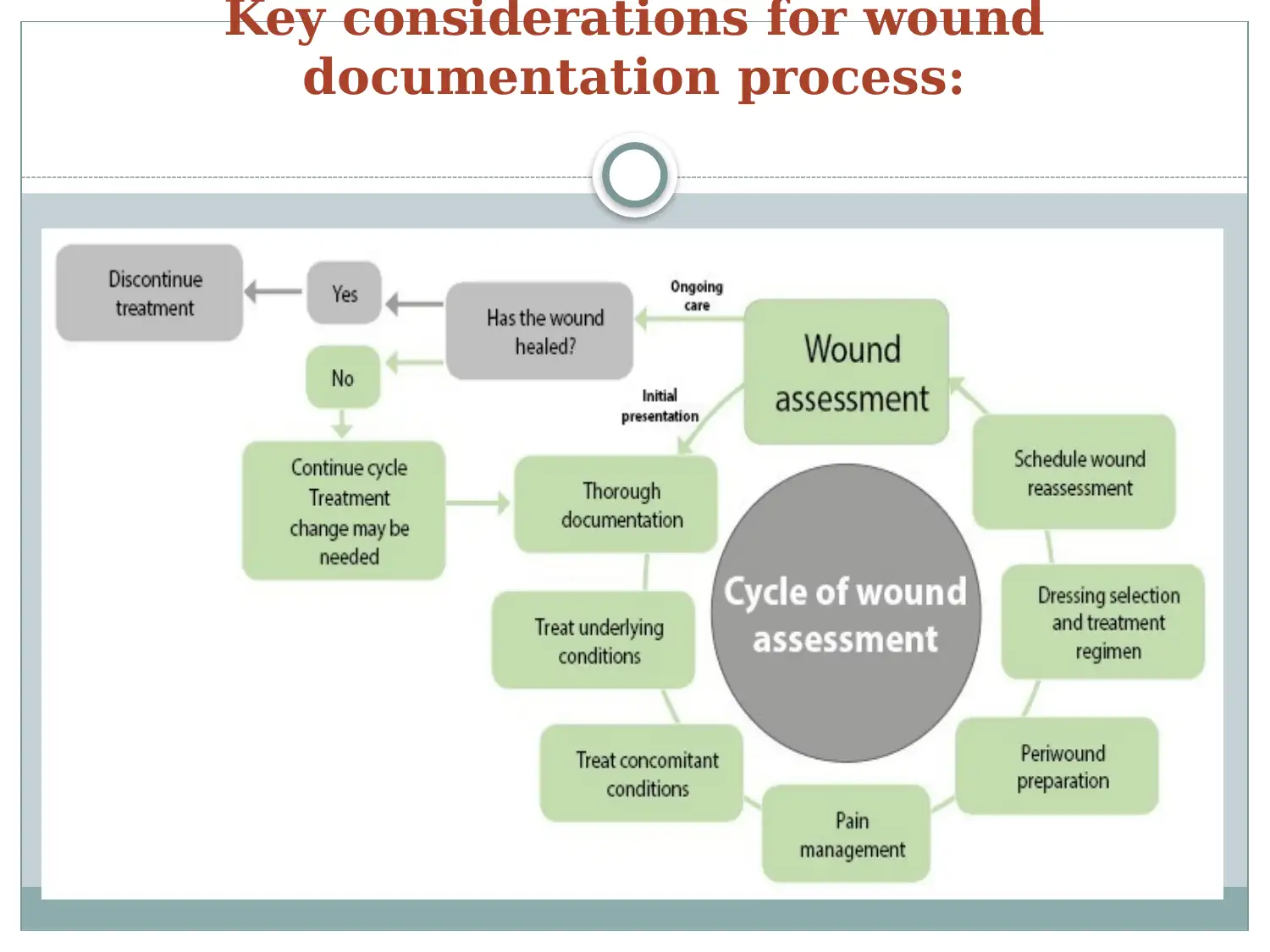
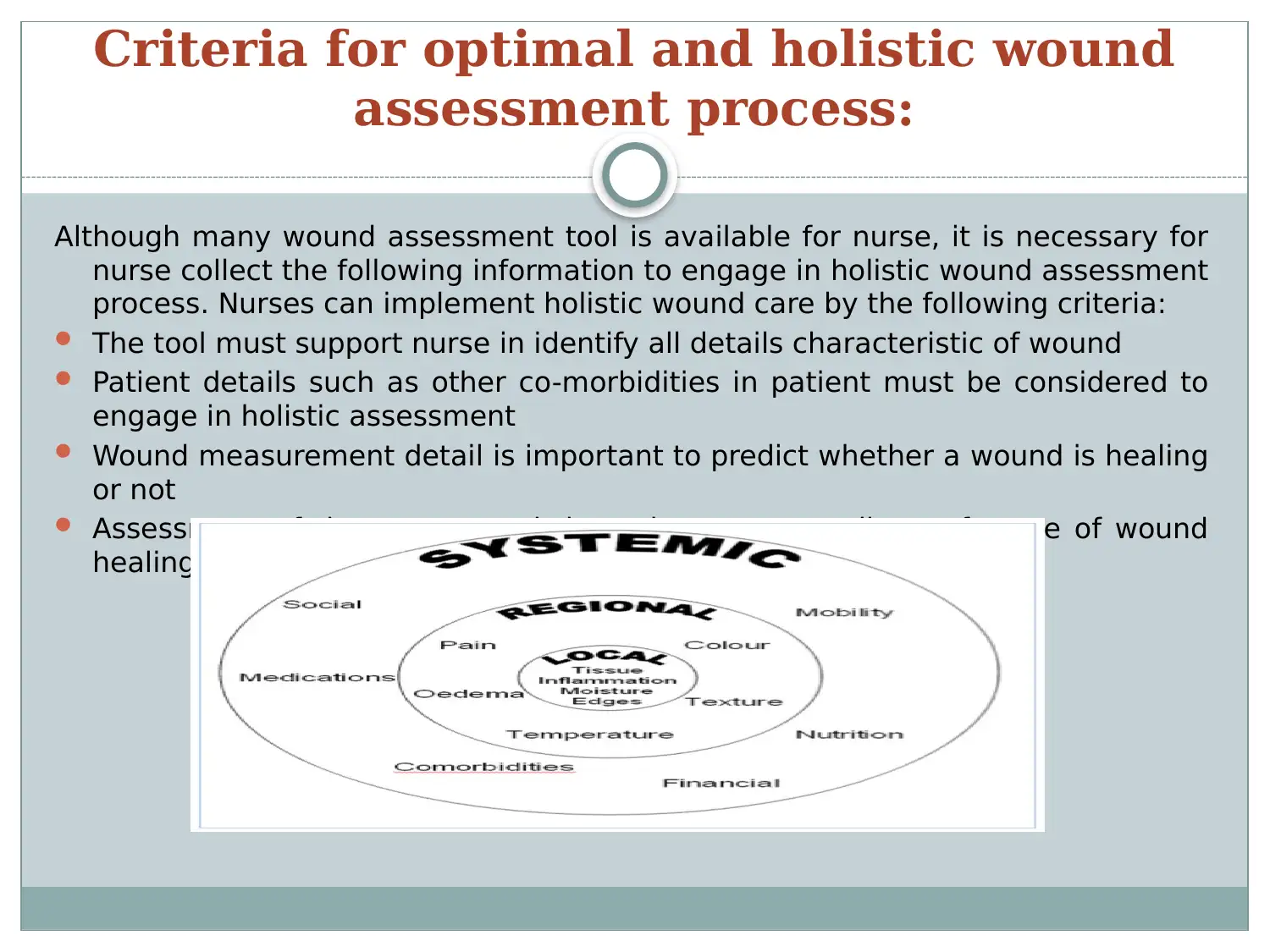
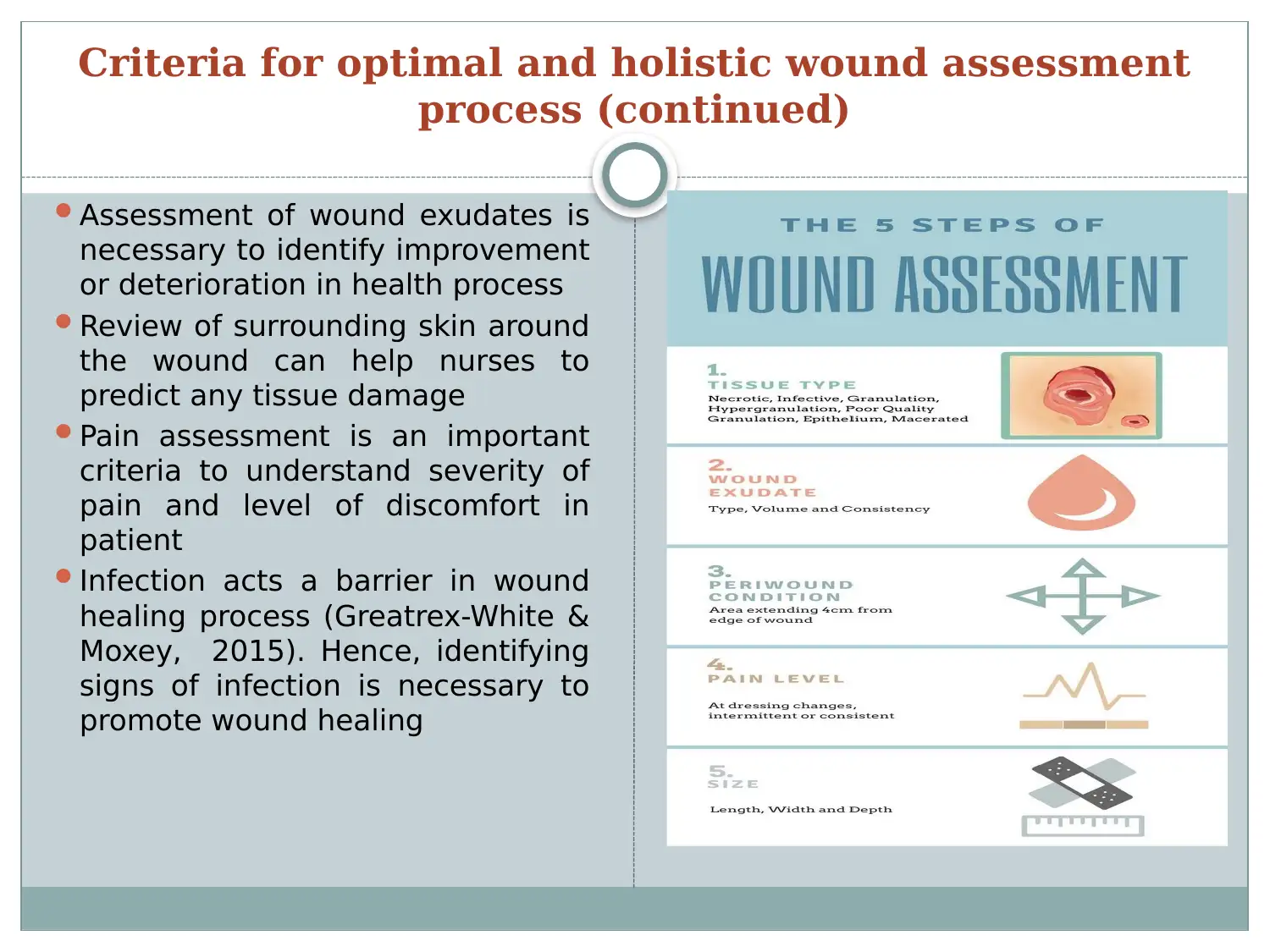
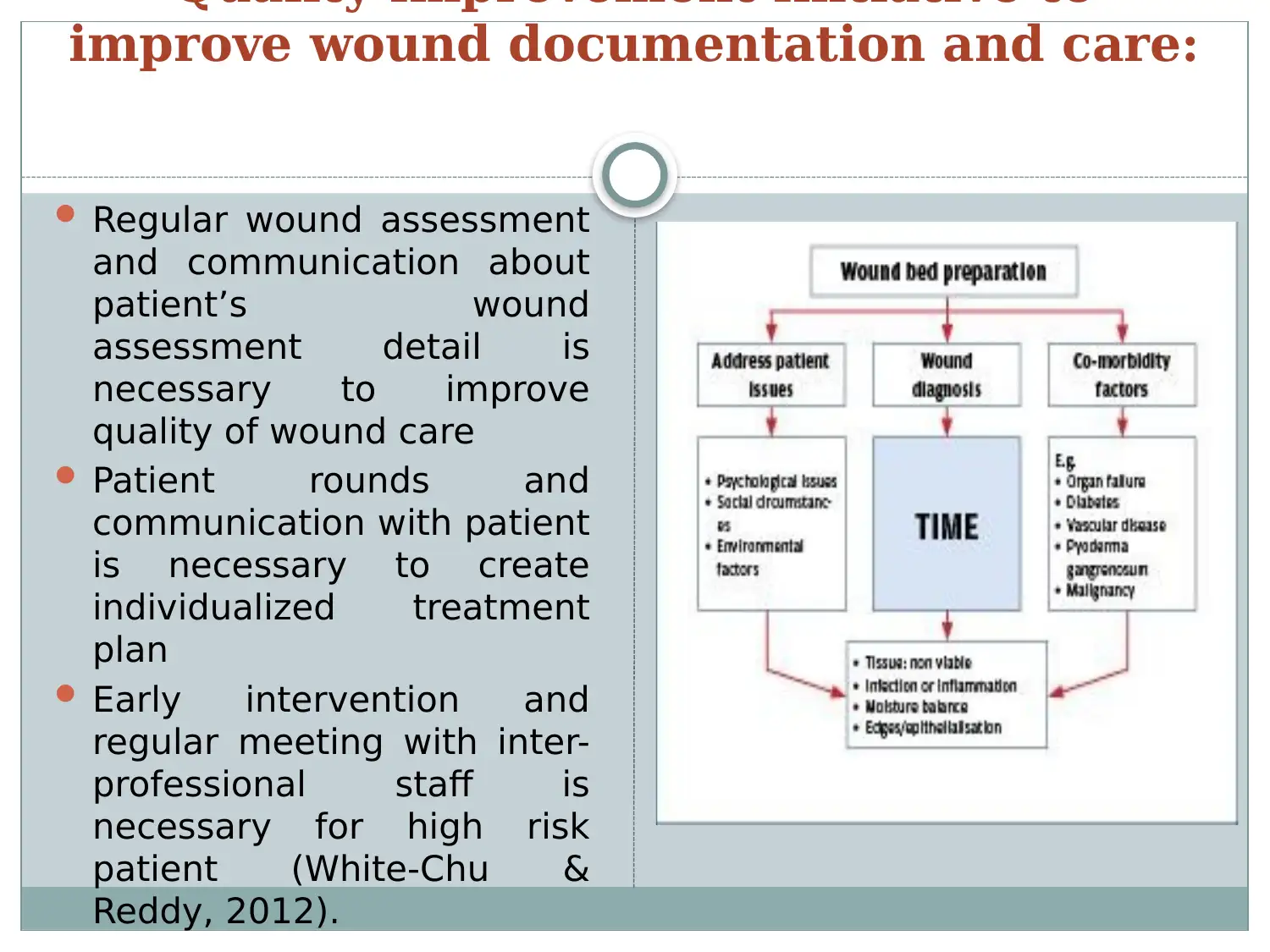
This presentation provides a detailed communication plan for effective wound documentation in long-term care facilities. It addresses the importance of comprehensive wound assessment, including identifying wound location, etiology, classification, and measurement. The plan emphasizes the need for holistic assessment, considering patient comorbidities, tissue type, exudates, surrounding skin, pain levels, and infection signs. Key considerations include the use of optimal assessment tools and regular communication among inter-professional staff. The presentation highlights the behavioral and psychological characteristics of nursing staff, addressing the need for up-to-date knowledge and skills in evidence-based practice. Quality improvement initiatives, such as regular wound assessment, patient rounds, and early intervention, are discussed to improve the quality of wound care. The plan also details approaches to enhance inter-professional collaboration, emphasizing team-based wound management, optimal communication formats, regular team briefings, and timely information handover. The presentation aims to improve nursing documentation, patient outcomes, and the overall quality of life for residents in long-term care facilities. References to relevant literature are included to support the recommendations.
1 out of 14







![[object Object]](/_next/static/media/star-bottom.7253800d.svg)