Detailed Report on Wound Healing: Inflammation, Hypoxia & Smoking
VerifiedAdded on 2023/06/08
|7
|1326
|199
Report
AI Summary
This report provides a detailed analysis of wound healing processes, focusing on the impact of hypoxia and inflammation. It discusses how hypoxia, caused by restricted blood supply, impairs wound healing by affecting cellular respiration and the function of Hypoxia-inducible factor-1. Strategies to improve oxygen delivery to ischemic tissues, such as oedema drainage and hyperbaric oxygen therapy, are also explored. The report includes a biological drawing illustrating neutrophil movement during inflammation and compares acute versus chronic inflammation, highlighting their differences and similarities. Furthermore, the report includes case studies, one examining the adverse effects of smoking on wound healing due to vasoconstriction and reduced oxygen perfusion, and another classifying a wound and describing the healing process by primary intention. The document concludes with relevant references.

Running Head: PART A – EXERCISES 1
Part A – Exercises
Author’s Name
Institution
Date
Part A – Exercises
Author’s Name
Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PART A – EXERCISES 2
Cellular Damage
How Hypoxia Affects Wound Healing
Proper wound healing requires oxygen. Hypoxia or anoxia due to restricted blood supply
causes a drop in oxygen levels in the wound region. Hypoxia can be due to obstruction of the
respiratory pathway, the inability of the cells to utilize oxygen for cellular respiration that causes
ischemia, transfer of oxygen across the surfaces of the lungs and defective transport of oxygen in
the blood. Ischemia caused by restriction of blood hence oxygen cannot freely reach the
damaged tissues hence reduced granulation, epithelialization and reduced stromal function hence
limiting the process of wound healing. Hypoxia causes malfunction of the sodium-potassium
pump which leads to depletion of energy hence inhibition of ATPase leading to loss of cell
division (Cerqueira, Pirraco & Marques, 2016).
Therefore, hypoxia causes poor wound healing since Hypoxia-inducible factor-1 which is
a regulator of homeostasis determines the wound healing outcomes. This factor contributes to all
the stages of wound healing which include the migration of the cell, survival of the cell in the
hypoxic conditions, the release of growth factor, cell division and the production and release of
the matrix to be laid on the healing wound throughout the healing process (Hong et al. 2014). In
a nutshell, lack of oxygen and blood supply negatively affects the process of wound healing as
seen in our case study.
How To Improve Oxygen Delivery To Injured Ischemic Tissues
Most of the important process that is involved in wound healing is dependent on oxygen.
Oxygen delivery to ischemic tissue can be done through draining of oedema to allow sufficient
blood supply that leads to the increase in the amount of oxygen that reaches the tissues. More
Cellular Damage
How Hypoxia Affects Wound Healing
Proper wound healing requires oxygen. Hypoxia or anoxia due to restricted blood supply
causes a drop in oxygen levels in the wound region. Hypoxia can be due to obstruction of the
respiratory pathway, the inability of the cells to utilize oxygen for cellular respiration that causes
ischemia, transfer of oxygen across the surfaces of the lungs and defective transport of oxygen in
the blood. Ischemia caused by restriction of blood hence oxygen cannot freely reach the
damaged tissues hence reduced granulation, epithelialization and reduced stromal function hence
limiting the process of wound healing. Hypoxia causes malfunction of the sodium-potassium
pump which leads to depletion of energy hence inhibition of ATPase leading to loss of cell
division (Cerqueira, Pirraco & Marques, 2016).
Therefore, hypoxia causes poor wound healing since Hypoxia-inducible factor-1 which is
a regulator of homeostasis determines the wound healing outcomes. This factor contributes to all
the stages of wound healing which include the migration of the cell, survival of the cell in the
hypoxic conditions, the release of growth factor, cell division and the production and release of
the matrix to be laid on the healing wound throughout the healing process (Hong et al. 2014). In
a nutshell, lack of oxygen and blood supply negatively affects the process of wound healing as
seen in our case study.
How To Improve Oxygen Delivery To Injured Ischemic Tissues
Most of the important process that is involved in wound healing is dependent on oxygen.
Oxygen delivery to ischemic tissue can be done through draining of oedema to allow sufficient
blood supply that leads to the increase in the amount of oxygen that reaches the tissues. More
PART A – EXERCISES 3
rapid clearance of bacterial infection and resolution of inflammation also improves oxygen
delivery to the healing wounds. The other way to improve oxygen delivery to the wound region
is the application of hyperbaric oxygen therapy whereby oxygen is introduced into the tissues at
a higher pressure than the atmospheric pressure so that it can reach the ischemic tissues.
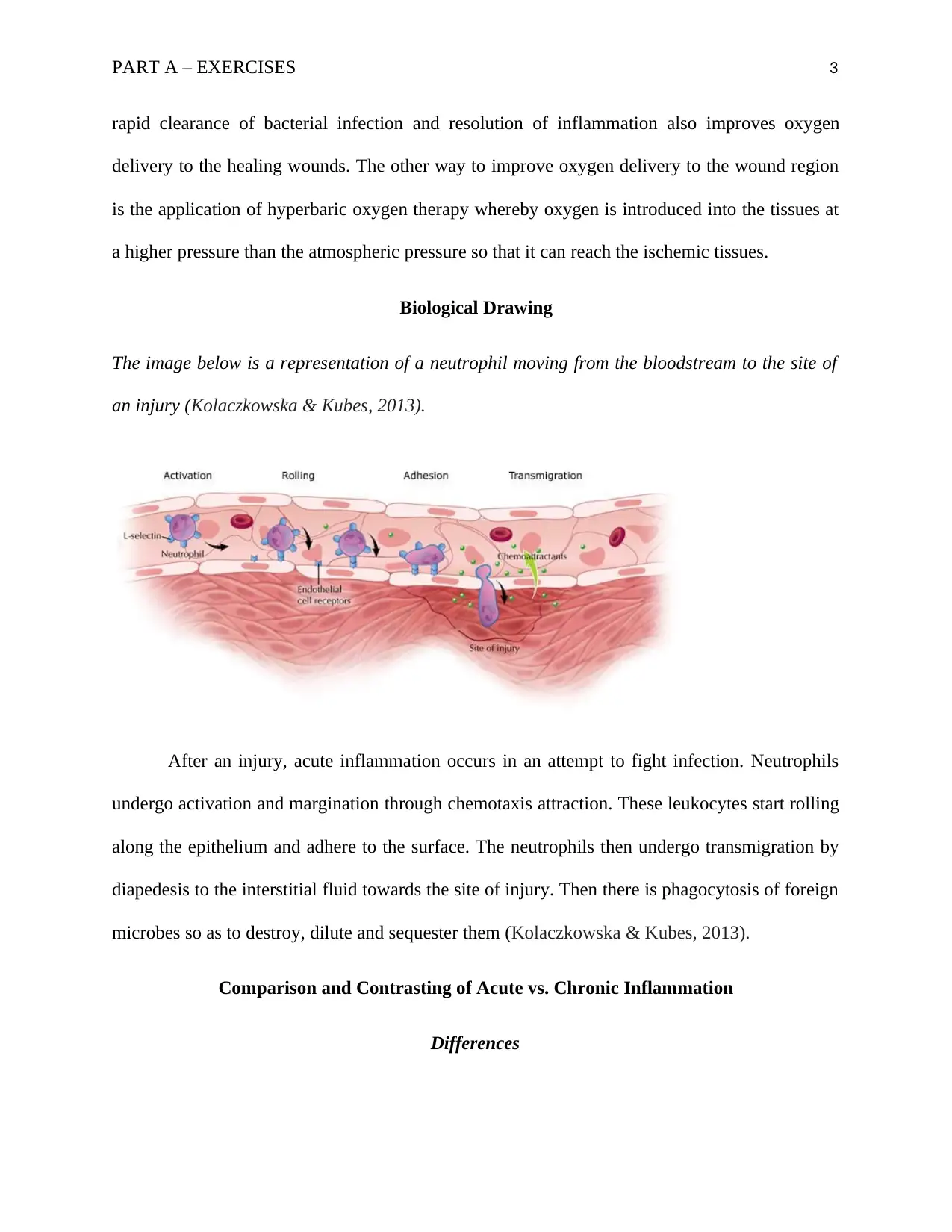
Biological Drawing
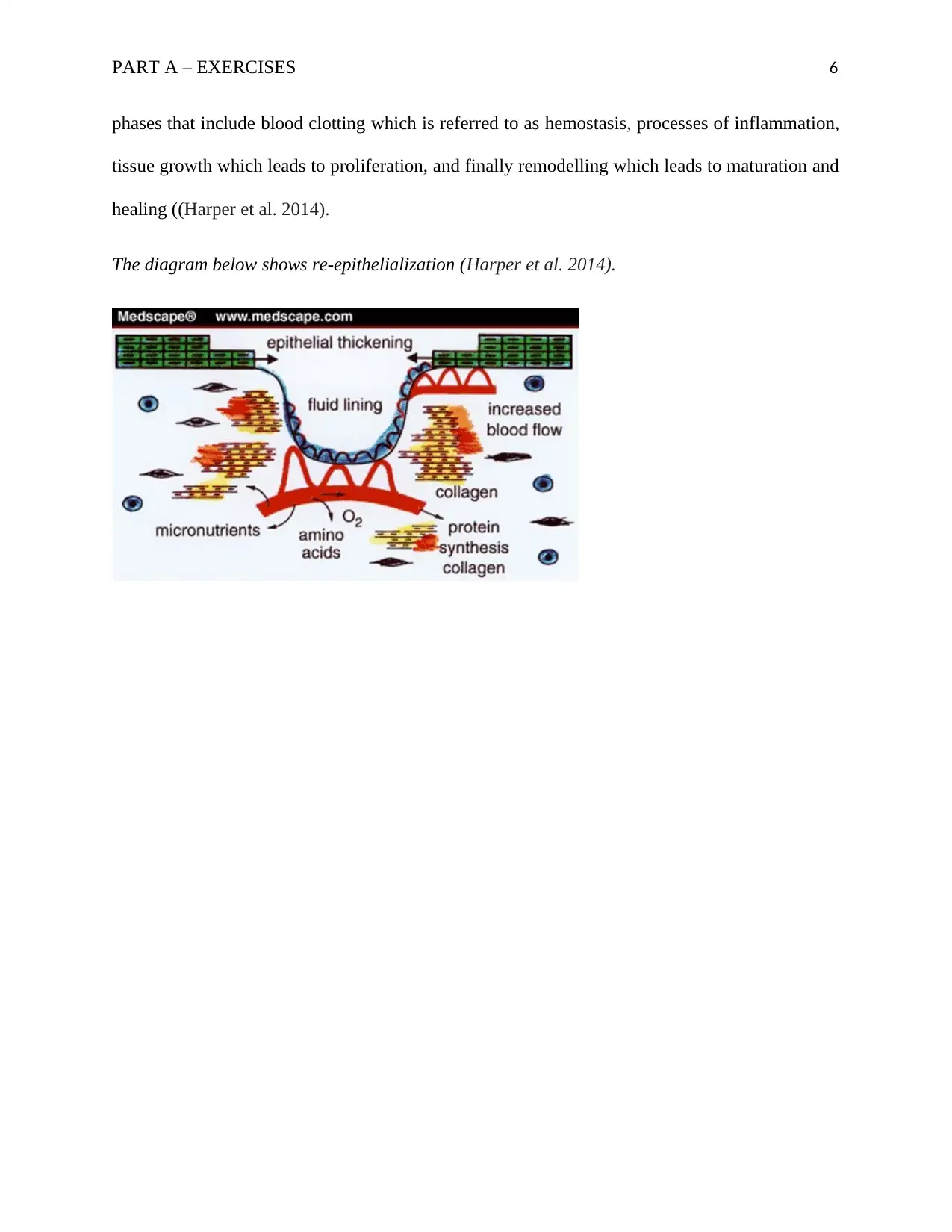
The image below is a representation of a neutrophil moving from the bloodstream to the site of
an injury (Kolaczkowska & Kubes, 2013).
After an injury, acute inflammation occurs in an attempt to fight infection. Neutrophils
undergo activation and margination through chemotaxis attraction. These leukocytes start rolling
along the epithelium and adhere to the surface. The neutrophils then undergo transmigration by
diapedesis to the interstitial fluid towards the site of injury. Then there is phagocytosis of foreign
microbes so as to destroy, dilute and sequester them (Kolaczkowska & Kubes, 2013).
Comparison and Contrasting of Acute vs. Chronic Inflammation
Differences
rapid clearance of bacterial infection and resolution of inflammation also improves oxygen
delivery to the healing wounds. The other way to improve oxygen delivery to the wound region
is the application of hyperbaric oxygen therapy whereby oxygen is introduced into the tissues at
a higher pressure than the atmospheric pressure so that it can reach the ischemic tissues.
Biological Drawing
The image below is a representation of a neutrophil moving from the bloodstream to the site of
an injury (Kolaczkowska & Kubes, 2013).
After an injury, acute inflammation occurs in an attempt to fight infection. Neutrophils
undergo activation and margination through chemotaxis attraction. These leukocytes start rolling
along the epithelium and adhere to the surface. The neutrophils then undergo transmigration by
diapedesis to the interstitial fluid towards the site of injury. Then there is phagocytosis of foreign
microbes so as to destroy, dilute and sequester them (Kolaczkowska & Kubes, 2013).
Comparison and Contrasting of Acute vs. Chronic Inflammation
Differences
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PART A – EXERCISES 4
Acute inflammation has a fast commencement and takes a short duration of time while chronic
inflammation is an extended period reaction.
Acute inflammation results into secretion of serotonin, histamines and prostaglandin while
chronic inflammation results into production of macrophages, fibroblasts and lymphocytes.
Diseases that result from acute inflammation include a sore throat, sinusitis, bronchitis and
tonsillitis while chronic inflammation leads to rheumatoid arthritis, sinusitis, Cohn’s disease and
TB.
Acute inflammation is non-specific while chronic inflammation is specific since it involves
acquired immunity.
In acute inflammation, there are cardinal signs such loss of function, swelling, redness, pain and
heat while in chronic inflammation has no any cardinal signs.
Oedema and fluid exudation are present in acute inflammation while there are fibrosis and
angiogenesis in chronic inflammation.
The systemic manifestation in acute inflammation has a high fever while chronic inflammation
has low ranking fever, appetite loss and loss of weight.
The causative agents for acute inflammation include tissue necrosis, immune response, chemical
damages and invasions by pathogens while the causative agents of chronic inflammation are the
continuous infection, foreign bodies and autoimmunity disorders (Kumar, Abbas & Aster,
2017).
Similarities
Both forms of inflammation involve immune cells, blood vessels and molecular mediators.
Acute inflammation has a fast commencement and takes a short duration of time while chronic
inflammation is an extended period reaction.
Acute inflammation results into secretion of serotonin, histamines and prostaglandin while
chronic inflammation results into production of macrophages, fibroblasts and lymphocytes.
Diseases that result from acute inflammation include a sore throat, sinusitis, bronchitis and
tonsillitis while chronic inflammation leads to rheumatoid arthritis, sinusitis, Cohn’s disease and
TB.
Acute inflammation is non-specific while chronic inflammation is specific since it involves
acquired immunity.
In acute inflammation, there are cardinal signs such loss of function, swelling, redness, pain and
heat while in chronic inflammation has no any cardinal signs.
Oedema and fluid exudation are present in acute inflammation while there are fibrosis and
angiogenesis in chronic inflammation.
The systemic manifestation in acute inflammation has a high fever while chronic inflammation
has low ranking fever, appetite loss and loss of weight.
The causative agents for acute inflammation include tissue necrosis, immune response, chemical
damages and invasions by pathogens while the causative agents of chronic inflammation are the
continuous infection, foreign bodies and autoimmunity disorders (Kumar, Abbas & Aster,
2017).
Similarities
Both forms of inflammation involve immune cells, blood vessels and molecular mediators.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PART A – EXERCISES 5
Acute and chronic inflammation both aims at removing the causes of cell damage, clearing all
the necrotic cells and damaged tissues so that tissues can start recovering (Kumar, Abbas &
Aster, 2013).
Case Study 1
How smoking affect wound healing
Smoking has adverse effects on wound healing. This is because smoking causes many negative
effects such as premalignant lesions and cancers. Tobacco smoking is associated with the
production and release of catecholamines that causes vasoconstriction and decreased tissue
perfusion hence oxygen and nutrients cannot reach the site of injury to promote wound healing.
Smoking reduces wound healing since it suppresses the innate as well as the host responses
which affects the function of the neutrophils which is the major line of defence against many
infections. Therefore, the association between the delayed healing of wounds and smoking.
Carbon monoxide produced when tobacco burns produce capillary blood flow hence delaying
wound healing. Nicotine has several adverse effects on wound healing by reducing the
proliferation of RBCs, macrophages and fibroblasts. Nicotine also increases adhesiveness which
leads to the formation of a micro cloth that elevates the risk of microvascular occlusion and
tissue ischemia. It also results in cutaneous vasoconstriction. The rise of carboxyhemoglobin
levels causes the oxygen curve to shift to the left hence oxygen is not able to dissociate from
RBCs (Harper, Young & McNaught, 2014).
Case Study 2
The wound can be classified as partial thickness. The wound healing process in this case
study is healing by primary intention. Healing by primary intention involves various predictable
Acute and chronic inflammation both aims at removing the causes of cell damage, clearing all
the necrotic cells and damaged tissues so that tissues can start recovering (Kumar, Abbas &
Aster, 2013).
Case Study 1
How smoking affect wound healing
Smoking has adverse effects on wound healing. This is because smoking causes many negative
effects such as premalignant lesions and cancers. Tobacco smoking is associated with the
production and release of catecholamines that causes vasoconstriction and decreased tissue
perfusion hence oxygen and nutrients cannot reach the site of injury to promote wound healing.
Smoking reduces wound healing since it suppresses the innate as well as the host responses
which affects the function of the neutrophils which is the major line of defence against many
infections. Therefore, the association between the delayed healing of wounds and smoking.
Carbon monoxide produced when tobacco burns produce capillary blood flow hence delaying
wound healing. Nicotine has several adverse effects on wound healing by reducing the
proliferation of RBCs, macrophages and fibroblasts. Nicotine also increases adhesiveness which
leads to the formation of a micro cloth that elevates the risk of microvascular occlusion and
tissue ischemia. It also results in cutaneous vasoconstriction. The rise of carboxyhemoglobin
levels causes the oxygen curve to shift to the left hence oxygen is not able to dissociate from
RBCs (Harper, Young & McNaught, 2014).
Case Study 2
The wound can be classified as partial thickness. The wound healing process in this case
study is healing by primary intention. Healing by primary intention involves various predictable
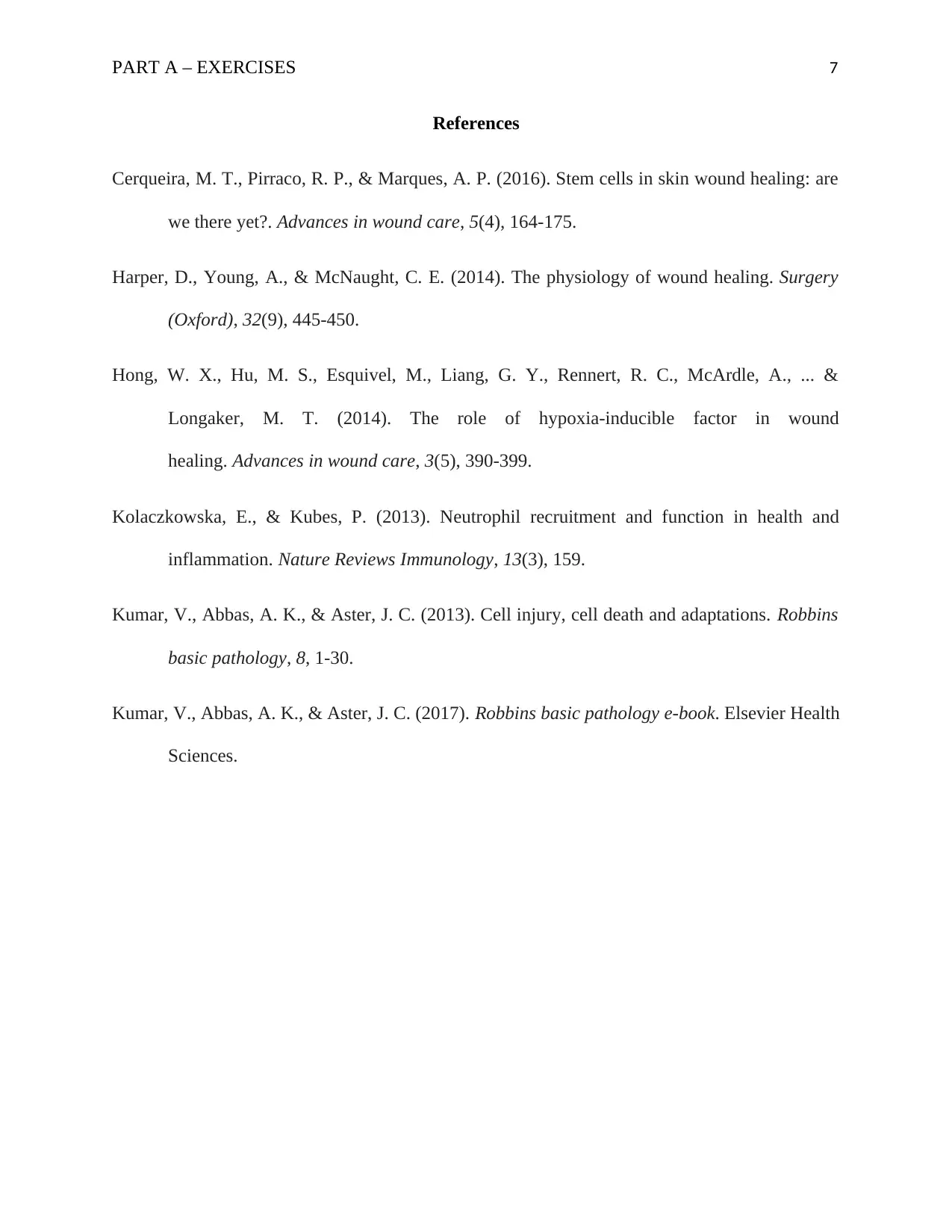
PART A – EXERCISES 6
phases that include blood clotting which is referred to as hemostasis, processes of inflammation,
tissue growth which leads to proliferation, and finally remodelling which leads to maturation and
healing ((Harper et al. 2014).
The diagram below shows re-epithelialization (Harper et al. 2014).
phases that include blood clotting which is referred to as hemostasis, processes of inflammation,
tissue growth which leads to proliferation, and finally remodelling which leads to maturation and
healing ((Harper et al. 2014).
The diagram below shows re-epithelialization (Harper et al. 2014).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PART A – EXERCISES 7
References
Cerqueira, M. T., Pirraco, R. P., & Marques, A. P. (2016). Stem cells in skin wound healing: are
we there yet?. Advances in wound care, 5(4), 164-175.
Harper, D., Young, A., & McNaught, C. E. (2014). The physiology of wound healing. Surgery
(Oxford), 32(9), 445-450.
Hong, W. X., Hu, M. S., Esquivel, M., Liang, G. Y., Rennert, R. C., McArdle, A., ... &
Longaker, M. T. (2014). The role of hypoxia-inducible factor in wound
healing. Advances in wound care, 3(5), 390-399.
Kolaczkowska, E., & Kubes, P. (2013). Neutrophil recruitment and function in health and
inflammation. Nature Reviews Immunology, 13(3), 159.
Kumar, V., Abbas, A. K., & Aster, J. C. (2013). Cell injury, cell death and adaptations. Robbins
basic pathology, 8, 1-30.
Kumar, V., Abbas, A. K., & Aster, J. C. (2017). Robbins basic pathology e-book. Elsevier Health
Sciences.
References
Cerqueira, M. T., Pirraco, R. P., & Marques, A. P. (2016). Stem cells in skin wound healing: are
we there yet?. Advances in wound care, 5(4), 164-175.
Harper, D., Young, A., & McNaught, C. E. (2014). The physiology of wound healing. Surgery
(Oxford), 32(9), 445-450.
Hong, W. X., Hu, M. S., Esquivel, M., Liang, G. Y., Rennert, R. C., McArdle, A., ... &
Longaker, M. T. (2014). The role of hypoxia-inducible factor in wound
healing. Advances in wound care, 3(5), 390-399.
Kolaczkowska, E., & Kubes, P. (2013). Neutrophil recruitment and function in health and
inflammation. Nature Reviews Immunology, 13(3), 159.
Kumar, V., Abbas, A. K., & Aster, J. C. (2013). Cell injury, cell death and adaptations. Robbins
basic pathology, 8, 1-30.
Kumar, V., Abbas, A. K., & Aster, J. C. (2017). Robbins basic pathology e-book. Elsevier Health
Sciences.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





